Diet and Nutrients in Rare Neurological Disorders: Biological, Biochemical, and Pathophysiological Evidence
Abstract
1. Introduction
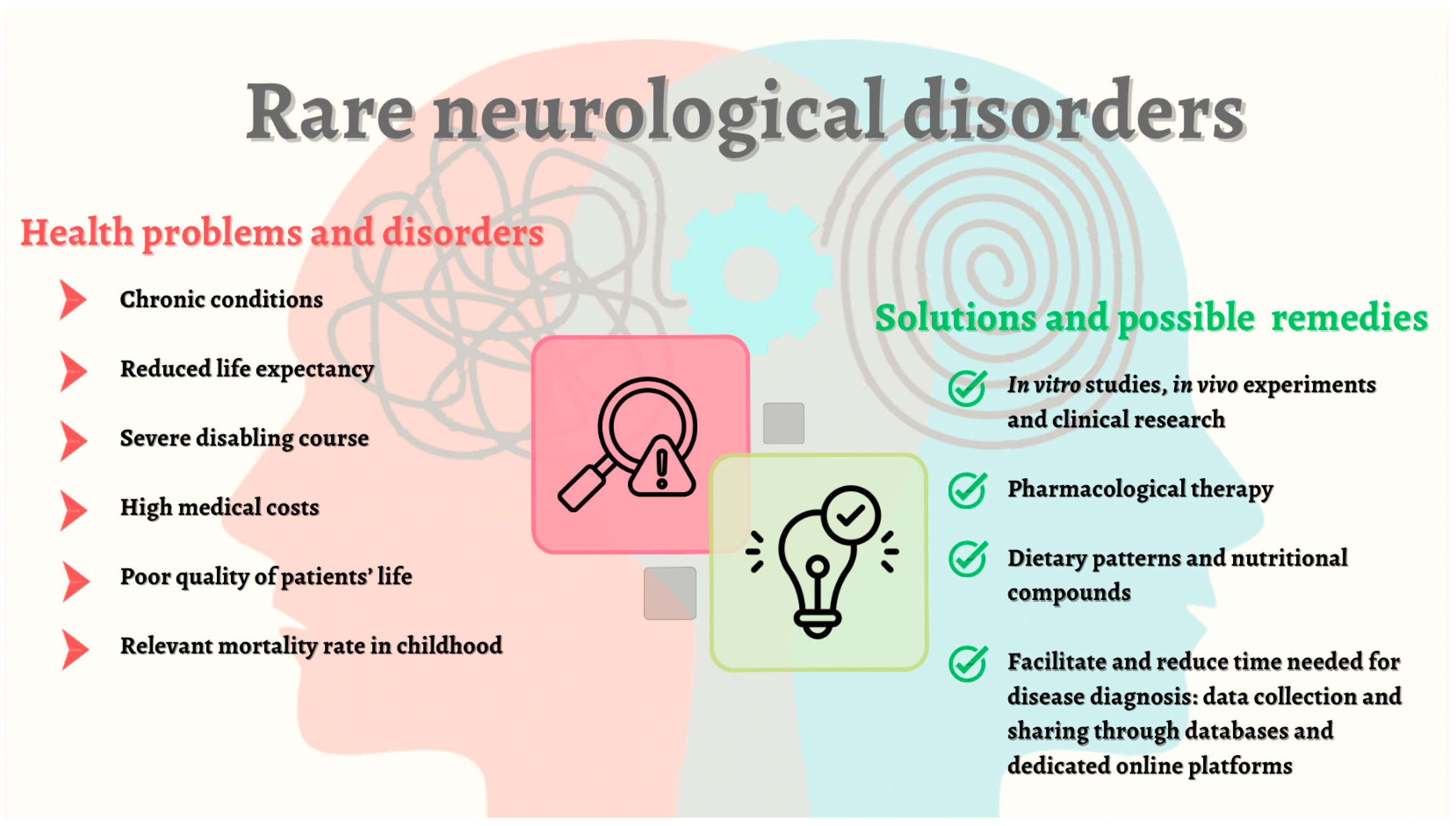
2. Rare Disorders: Lights and Shadows
Rare Neurological Disorders
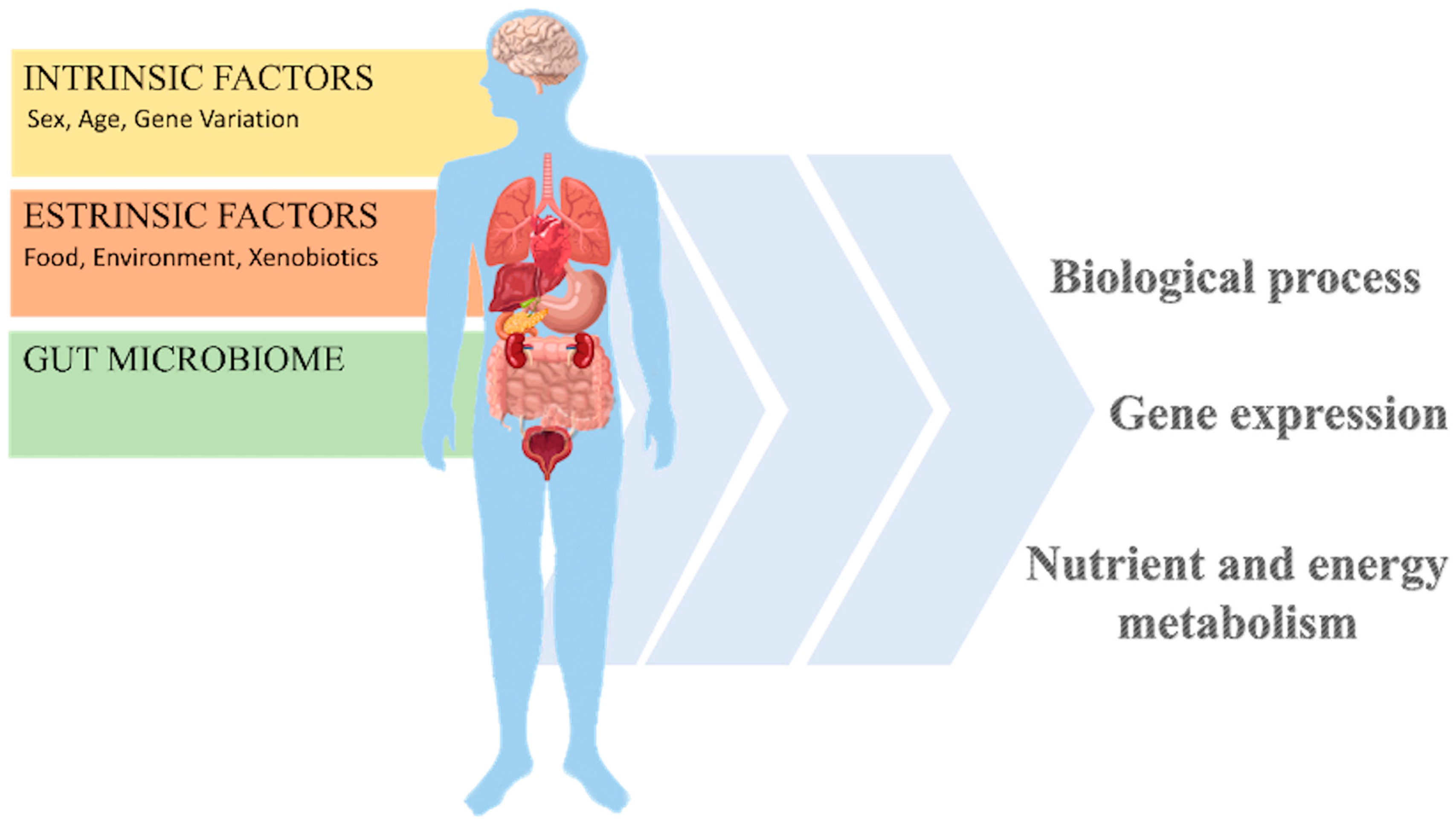
3. The Alimentary Wellness for a Global Health
3.1. Nutritional Interventions: What Are They?
3.1.1. The Nutrient Supplementation in Neurological Illness
3.1.2. The Dietary Modification in Neurological Illness
4. Nutritional Interventions for Rare Neurological Disorders: What Is the Right Model?
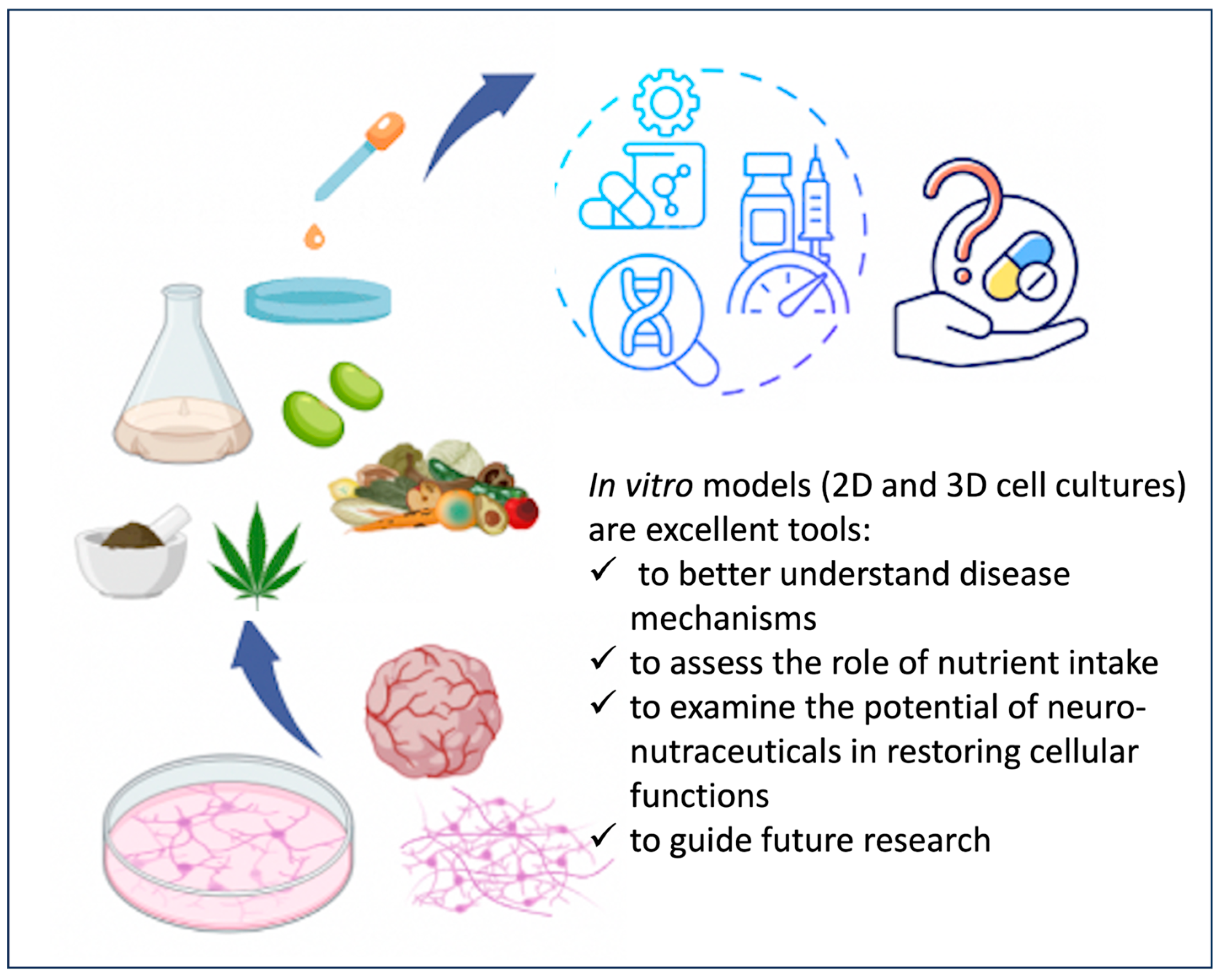
4.1. In Vitro Models for Testing Nutritional Interventions in Rare Neurological Disorders
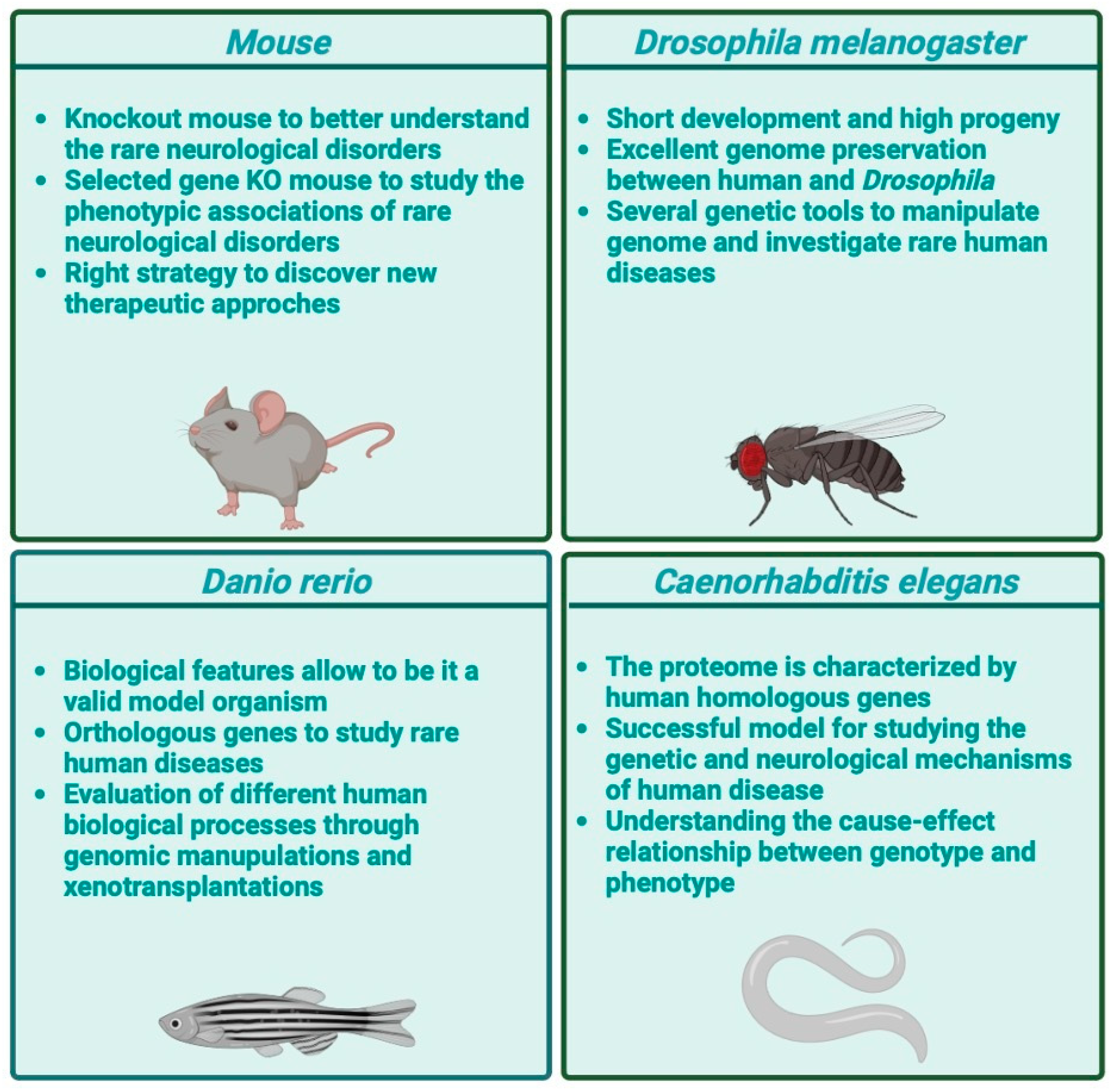
4.2. In Vivo Models for Testing Nutritional Interventions in Rare Neurological Disorders
4.2.1. Nonhuman Primate Genetic Models
4.2.2. Rodents
4.2.3. Caenorhabditis elegans (C. elegans)
4.2.4. Drosophila melanogaster
4.2.5. Zebrafish (Danio rerio)
4.3. Clinical Research for Testing Nutritional Interventions in Rare Neurological Disorders
5. Diet and Nutrient Intake in Rare Neurological Disorders
5.1. Rare Pervasive Developmental Disorder
5.1.1. Angelman Syndrome
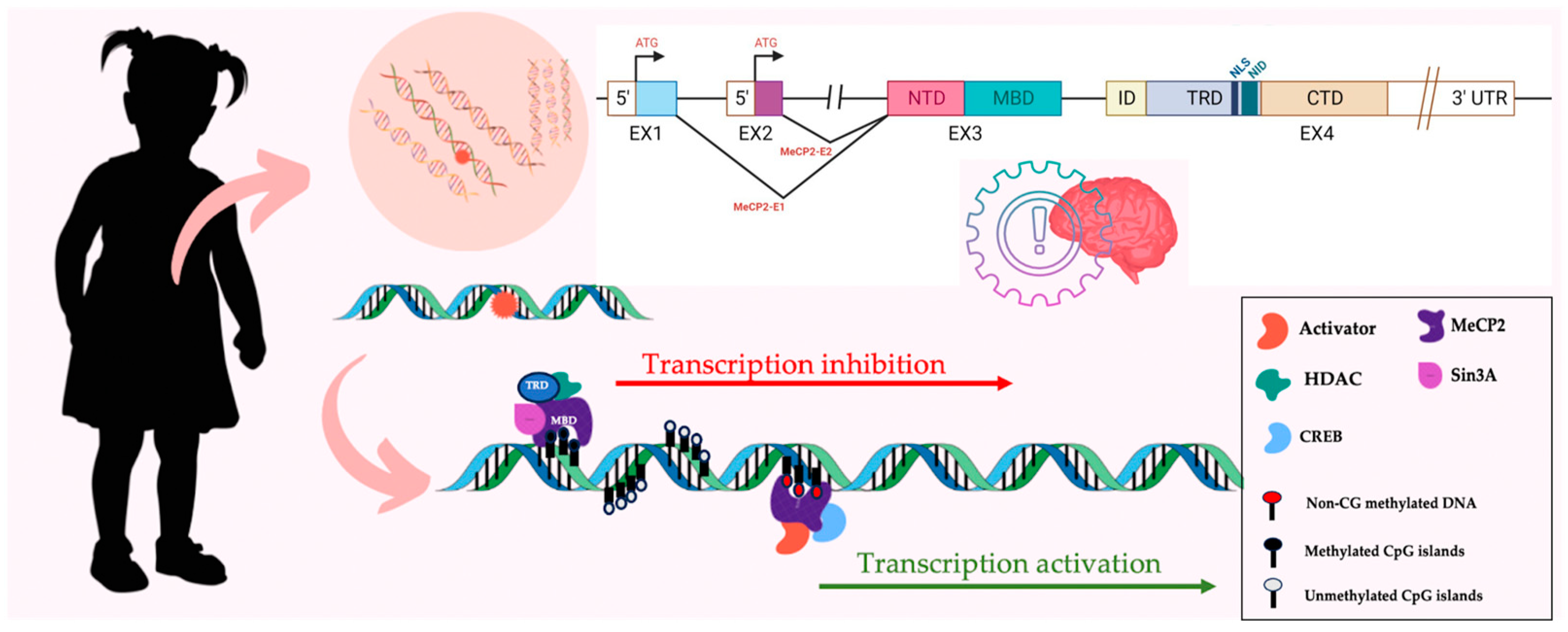
5.1.2. Rett Syndrome
| Nutritional Interventions for Rett Syndrome | ||
|---|---|---|
| Nutrients or Neuro-Nutraceutical Substance | Effects | |
| Nutrient supplementation | Vitamin D 1 | Reduction in vitamin D deficiency [183] |
| ω-3 polyunsaturated fatty acids 1 | Improvement in inflammatory status [200,201] | |
| Triheptanoin 2,3 | Amelioration of mitochondrial function, motor function and social interaction [202] | |
| Choline 2 | Modulation of neuronal plasticity, possibly leading to behavioral changes. | |
| Probiotic 1 | Amelioration of neurological outcomes [188] | |
| Cannabidivarin 2 | Rescue cognitive deficits and delay of neurological and motor defects [204,205] | |
| Cannabidiol 1 | Antiepileptic actions | |
| Creatine monohydrate 1 | Increase in DNA methylation [192] | |
| Type of diet | Effects | |
| Dietary modification | Ketogenic diet 1,2 | Antiepileptic actions [206,207,208] |
5.2. Rare Leukodystrophies
5.2.1. Krabbe Disease
5.2.2. Pelizaeus–Merzbacher Disease
5.2.3. Miscellaneous
5.3. Rare Genetic Epilepsy
5.4. Rare Forms of Ataxia
5.5. Rare Brain Tumors
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vigo, D.; Thornicroft, G.; Atun, R. Estimating the True Global Burden of Mental Illness. Lancet Psychiatry 2016, 3, 171–178. [Google Scholar] [CrossRef] [PubMed]
- WHO Over 1 in 3 People Affected by Neurological Conditions, the Leading Cause of Illness and Disability Worldwide. Available online: https://www.who.int/news/item/14-03-2024-over-1-in-3-people-affected-by-neurological-conditions--the-leading-cause-of-illness-and-disability-worldwide (accessed on 30 May 2024).
- Steinmetz, J.D.; Seeher, K.M.; Schiess, N.; Nichols, E.; Cao, B.; Servili, C.; Cavallera, V.; Cousin, E.; Hagins, H.; Moberg, M.E.; et al. Global, Regional, and National Burden of Disorders Affecting the Nervous System, 1990–2021: A Systematic Analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 2024, 23, 344–381. [Google Scholar] [CrossRef]
- Kouzani, A.Z.; Sillitoe, R.V. Medical Devices in Neurology. In Encyclopedia of Biomedical Engineering; Narayan, R., Ed.; Elsevier: Oxford, UK, 2019; pp. 409–413. ISBN 978-0-12-805144-3. [Google Scholar]
- Chan, J.K.N.; Correll, C.U.; Wong, C.S.M.; Chu, R.S.T.; Fung, V.S.C.; Wong, G.H.S.; Lei, J.H.C.; Chang, W.C. Life Expectancy and Years of Potential Life Lost in People with Mental Disorders: A Systematic Review and Meta-Analysis. EClinicalMedicine 2023, 65, 102294. [Google Scholar] [CrossRef] [PubMed]
- Intersectoral Global Action Plan on Epilepsy and Other Neurological Disorders; WHO: Geneva, Switzerland, 2023.
- Mao, X.-Y.; Yin, X.-X.; Guan, Q.-W.; Xia, Q.-X.; Yang, N.; Zhou, H.-H.; Liu, Z.-Q.; Jin, W.-L. Dietary Nutrition for Neurological Disease Therapy: Current Status and Future Directions. Pharmacol. Ther. 2021, 226, 107861. [Google Scholar] [CrossRef] [PubMed]
- Lee, H. The Importance of Nutrition in Neurological Disorders and Nutrition Assessment Methods. Brain Neurorehabilit. 2022, 15, e1. [Google Scholar] [CrossRef]
- Kivipelto, M.; Mangialasche, F.; Ngandu, T. Lifestyle Interventions to Prevent Cognitive Impairment, Dementia and Alzheimer Disease. Nat. Rev. Neurol. 2018, 14, 653–666. [Google Scholar] [CrossRef]
- Provensi, G.; Schmidt, S.D.; Boehme, M.; Bastiaanssen, T.F.S.; Rani, B.; Costa, A.; Busca, K.; Fouhy, F.; Strain, C.; Stanton, C.; et al. Preventing Adolescent Stress-Induced Cognitive and Microbiome Changes by Diet. Proc. Natl. Acad. Sci. USA 2019, 116, 9644–9651. [Google Scholar] [CrossRef]
- Franco, P. Orphan Drugs: The Regulatory Environment. Drug Discov. Today 2013, 18, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Aronson, J. Rare Diseases, Orphan Drugs, and Orphan Diseases. BMJ 2006, 333, 127. [Google Scholar] [CrossRef]
- Jinnah, H.A.; Albanese, A.; Bhatia, K.P.; Cardoso, F.; Da Prat, G.; De Koning, T.J.; Espay, A.J.; Fung, V.; Garcia-Ruiz, P.J.; Gershanik, O.; et al. Treatable Inherited Rare Movement Disorders. Mov. Disord. 2018, 33, 21–35. [Google Scholar] [CrossRef]
- Federico, A. Rare Neurological Diseases: A Pandora’s Box for Neurology (an European and Italian Perspective). Rev. Neurol. 2013, 169, S12–S17. [Google Scholar] [CrossRef] [PubMed]
- Maroilley, T.; Tarailo-Graovac, M. Uncovering Missing Heritability in Rare Diseases. Genes 2019, 10, 275. [Google Scholar] [CrossRef] [PubMed]
- García, J.-C.; Bustos, R.-H. The Genetic Diagnosis of Neurodegenerative Diseases and Therapeutic Perspectives. Brain Sci. 2018, 8, 222. [Google Scholar] [CrossRef]
- Schaaf, J.; Sedlmayr, M.; Schaefer, J.; Storf, H. Diagnosis of Rare Diseases: A Scoping Review of Clinical Decision Support Systems. Orphanet J. Rare Dis. 2020, 15, 263. [Google Scholar] [CrossRef]
- Matilla-Dueñas, A.; Corral-Juan, M.; Rodríguez-Palmero Seuma, A.; Vilas, D.; Ispierto, L.; Morais, S.; Sequeiros, J.; Alonso, I.; Volpini, V.; Serrano-Munuera, C.; et al. Rare Neurodegenerative Diseases: Clinical and Genetic Update. In Rare Diseases Epidemiology: Update and Overview; Posada De La Paz, M., Taruscio, D., Groft, S.C., Eds.; Advances in Experimental Medicine and Biology; Springer International Publishing: Cham, Switzerland, 2017; Volume 1031, pp. 443–496. ISBN 978-3-319-67142-0. [Google Scholar]
- Schieppati, A.; Henter, J.I.; Daina, E.; Aperia, A. Why Rare Diseases Are an Important Medical and Social Issue. Lancet 2008, 371, 2039–2041. [Google Scholar] [CrossRef]
- The Lancet Neurology. Rare Advances for Rare Diseases. Lancet Neurol. 2017, 16, 1. [Google Scholar] [CrossRef]
- Sintila, S.-A.; Boziki, M.; Bakirtzis, C.; Stardeli, T.; Smyrni, N.; Nikolaidis, I.; Parissis, D.; Afrantou, T.; Karapanayiotides, T.; Koutroulou, I.; et al. The Experience of a Tertiary Reference Hospital in the Study of Rare Neurological Diseases. Medicina 2023, 59, 266. [Google Scholar] [CrossRef] [PubMed]
- Meekings, K.N.; Williams, C.S.M.; Arrowsmith, J.E. Orphan Drug Development: An Economically Viable Strategy for Biopharma R&D. Drug Discov. Today 2012, 17, 660–664. [Google Scholar] [CrossRef]
- Orphanet. Available online: https://www.orpha.net.
- Painous, C.; Van Os, N.J.H.; Delamarre, A.; Michailoviene, I.; Marti, M.J.; Van De Warrenburg, B.P.; Meissner, W.G.; Utkus, A.; Reinhard, C.; Graessner, H.; et al. Management of Rare Movement Disorders in Europe: Outcome of Surveys of the European Reference Network for Rare Neurological Diseases. Eur. J. Neurol. 2020, 27, 1493–1500. [Google Scholar] [CrossRef]
- European Reference Networks. Available online: http://www.Ern-Rnd.Eu.
- ERN-ITHACA. European Reference Network for Rare Malformation Syndromes, Intellectual and Other Neurodevelopmental Disorders. Available online: https://Ern-Ithaca.Eu.
- March, P.A. Diseases of the Brain and Cranial Nerves. In Saunders Manual of Small Animal Practice; Elsevier: Amsterdam, The Netherlands, 2006; pp. 1249–1276. ISBN 978-0-7216-0422-0. [Google Scholar]
- Frederiksen, S.D.; Avramović, V.; Maroilley, T.; Lehman, A.; Arbour, L.; Tarailo-Graovac, M. Rare Disorders Have Many Faces: In Silico Characterization of Rare Disorder Spectrum. Orphanet J. Rare Dis. 2022, 17, 76. [Google Scholar] [CrossRef]
- Krieg, S.I.; Krägeloh-Mann, I.; Groeschel, S.; Beck-Wödl, S.; Husain, R.A.; Schöls, L.; Kehrer, C. Natural History of Krabbe Disease–a Nationwide Study in Germany Using Clinical and MRI Data. Orphanet J. Rare Dis. 2020, 15, 243. [Google Scholar] [CrossRef] [PubMed]
- Amelot, A.; Terrier, L.-M.; Cognacq, G.; Jecko, V.; Marlier, B.; Seizeur, R.; Emery, E.; Bauchet, L.; Roualdes, V.; Voirin, J.; et al. Natural History of Spinal Cord Metastasis from Brain Glioblastomas. J. Neurooncol. 2023, 162, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Lim, A.Z.; Ng, Y.S.; Blain, A.; Jiminez-Moreno, C.; Alston, C.L.; Nesbitt, V.; Simmons, L.; Santra, S.; Wassmer, E.; Blakely, E.L.; et al. Natural History of Leigh Syndrome: A Study of Disease Burden and Progression. Ann. Neurol. 2022, 91, 117–130. [Google Scholar] [CrossRef]
- Gillette-Guyonnet, S.; Secher, M.; Vellas, B. Nutrition and Neurodegeneration: Epidemiological Evidence and Challenges for Future Research. Br. J. Clin. Pharmacol. 2013, 75, 738–755. [Google Scholar] [CrossRef]
- Chen, Y.; Michalak, M.; Agellon, L.B. Importance of Nutrients and Nutrient Metabolism on Human Health. Yale J. Biol. Med. 2018, 91, 95–103. [Google Scholar]
- Nasri, H.; Baradaran, A.; Shirzad, H.; Rafieian-Kopaei, M. New Concepts in Nutraceuticals as Alternative for Pharmaceuticals. Int. J. Prev. Med. 2014, 5, 1487–1499. [Google Scholar]
- Kearney, P.M.; Whelton, M.; Reynolds, K.; Muntner, P.; Whelton, P.K.; He, J. Global Burden of Hypertension: Analysis of Worldwide Data. Lancet 2005, 365, 217–223. [Google Scholar] [CrossRef]
- Kelly, T.; Yang, W.; Chen, C.-S.; Reynolds, K.; He, J. Global Burden of Obesity in 2005 and Projections to 2030. Int. J. Obes. 2008, 32, 1431–1437. [Google Scholar] [CrossRef] [PubMed]
- Shaw, J.E.; Sicree, R.A.; Zimmet, P.Z. Global Estimates of the Prevalence of Diabetes for 2010 and 2030. Diabetes Res. Clin. Pract. 2010, 87, 4–14. [Google Scholar] [CrossRef]
- Stanaway, J.D.; Afshin, A.; Gakidou, E.; Lim, S.S.; Abate, D.; Abate, K.H.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; et al. Global, Regional, and National Comparative Risk Assessment of 84 Behavioural, Environmental and Occupational, and Metabolic Risks or Clusters of Risks for 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- World Health Organization. Healthy Diet 2015. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet/ (accessed on 2 August 2024).
- Van Der Knaap, J.A.; Verrijzer, C.P. Undercover: Gene Control by Metabolites and Metabolic Enzymes. Genes Dev. 2016, 30, 2345–2369. [Google Scholar] [CrossRef] [PubMed]
- Donald, B. Chapter5: Nutrients as Regulators of Gene Expression. In Scientific Advances in Animal Nutrition: Promise for the New Century: Proceedings of a Symposium; National Academies Press: Washington, DC, USA, 2001; p. 102997152024. Available online: https://nap.nationalacademies.org/read/10299/chapter/7 (accessed on 15 June 2024).
- Johnston, J.D.; Ordovás, J.M.; Scheer, F.A.; Turek, F.W. Circadian Rhythms, Metabolism, and Chrononutrition in Rodents and Humans. Adv. Nutr. 2016, 7, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Dallman, M.F. Stress-Induced Obesity and the Emotional Nervous System. Trends Endocrinol. Metab. 2010, 21, 159–165. [Google Scholar] [CrossRef]
- Feil, R.; Fraga, M.F. Epigenetics and the Environment: Emerging Patterns and Implications. Nat. Rev. Genet. 2012, 13, 97–109. [Google Scholar] [CrossRef]
- Kyrou, I.; Tsigos, C. Stress Hormones: Physiological Stress and Regulation of Metabolism. Curr. Opin. Pharmacol. 2009, 9, 787–793. [Google Scholar] [CrossRef]
- Jaenisch, R.; Bird, A. Epigenetic Regulation of Gene Expression: How the Genome Integrates Intrinsic and Environmental Signals. Nat. Genet. 2003, 33, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Nicolia, V.; Lucarelli, M.; Fuso, A. Environment, Epigenetics and Neurodegeneration: Focus on Nutrition in Alzheimer’s Disease. Exp. Gerontol. 2015, 68, 8–12. [Google Scholar] [CrossRef]
- Ordovás, J.M.; Smith, C.E. Epigenetics and Cardiovascular Disease. Nat. Rev. Cardiol. 2010, 7, 510–519. [Google Scholar] [CrossRef]
- Teslovich, T.M.; Musunuru, K.; Smith, A.V.; Edmondson, A.C.; Stylianou, I.M.; Koseki, M.; Pirruccello, J.P.; Ripatti, S.; Chasman, D.I.; Willer, C.J.; et al. Biological, Clinical and Population Relevance of 95 Loci for Blood Lipids. Nature 2010, 466, 707–713. [Google Scholar] [CrossRef]
- Estrada, J.A.; Contreras, I. Nutritional Modulation of Immune and Central Nervous System Homeostasis: The Role of Diet in Development of Neuroinflammation and Neurological Disease. Nutrients 2019, 11, 1076. [Google Scholar] [CrossRef]
- Bhatara, V.S.; Bernstein, B.; Fazili, S. Complementary and Integrative Treatments of Aggressiveness/Emotion Dysregulation: Associated with Disruptive Disorders and Disruptive Mood Dysregulation Disorder. Child Adolesc. Psychiatr. Clin. N. Am. 2023, 32, 297–315. [Google Scholar] [CrossRef] [PubMed]
- Swierz, M.J.; Storman, D.; Jasinska, K.W.; Storman, M.; Staskiewicz, W.; Gorecka, M.; Skuza, A.; Tobola, P.; Bala, M.M. Systematic Review and Meta-Analysis of Perioperative Behavioral Lifestyle and Nutritional Interventions in Bariatric Surgery: A Call for Better Research and Reporting. Surg. Obes. Relat. Dis. 2020, 16, 2088–2104. [Google Scholar] [CrossRef] [PubMed]
- Cobley, J.N.; Fiorello, M.L.; Bailey, D.M. 13 Reasons Why the Brain Is Susceptible to Oxidative Stress. Redox Biol. 2018, 15, 490–503. [Google Scholar] [CrossRef]
- Gómez-Pinilla, F. Brain Foods: The Effects of Nutrients on Brain Function. Nat. Rev. Neurosci. 2008, 9, 568–578. [Google Scholar] [CrossRef]
- Holton, K.F. Micronutrients May Be a Unique Weapon Against the Neurotoxic Triad of Excitotoxicity, Oxidative Stress and Neuroinflammation: A Perspective. Front. Neurosci. 2021, 15, 726457. [Google Scholar] [CrossRef]
- Lahoda Brodska, H.; Klempir, J.; Zavora, J.; Kohout, P. The Role of Micronutrients in Neurological Disorders. Nutrients 2023, 15, 4129. [Google Scholar] [CrossRef] [PubMed]
- Poulose, S.M.; Miller, M.G.; Scott, T.; Shukitt-Hale, B. Nutritional Factors Affecting Adult Neurogenesis and Cognitive Function. Adv. Nutr. 2017, 8, 804–811. [Google Scholar] [CrossRef]
- Smith, A.D.; Smith, S.M.; de Jager, C.A.; Whitbread, P.; Johnston, C.; Agacinski, G.; Oulhaj, A.; Bradley, K.M.; Jacoby, R.; Refsum, H. Homocysteine-Lowering by B Vitamins Slows the Rate of Accelerated Brain Atrophy in Mild Cognitive Impairment: A Randomized Controlled Trial. PLoS ONE 2010, 5, e12244. [Google Scholar] [CrossRef]
- Zhang, L.; Chen, X.; Chen, Y.; Yan, J.; Huang, G.; Li, W. A Comparative Study Evaluating the Effectiveness of Folate-Based B Vitamin Intervention on Cognitive Function of Older Adults under Mandatory Folic Acid Fortification Policy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2024, 16, 2199. [Google Scholar] [CrossRef]
- Grundman, M. Vitamin E and Alzheimer Disease: The Basis for Additional Clinical Trials. Am. J. Clin. Nutr. 2000, 71, 630S–636S. [Google Scholar] [CrossRef]
- Pierrot-Deseilligny, C.; Souberbielle, J.-C. Vitamin D and Multiple Sclerosis: An Update. Mult. Scler. Relat. Disord. 2017, 14, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Mavar, M.; Sorić, T.; Bagarić, E.; Sarić, A.; Matek Sarić, M. The Power of Vitamin D: Is the Future in Precision Nutrition through Personalized Supplementation Plans? Nutrients 2024, 16, 1176. [Google Scholar] [CrossRef]
- Dales, J.-P.; Desplat-Jégo, S. Metal Imbalance in Neurodegenerative Diseases with a Specific Concern to the Brain of Multiple Sclerosis Patients. Int. J. Mol. Sci. 2020, 21, 9105. [Google Scholar] [CrossRef]
- Barbagallo, M.; Dominguez, L.J. Magnesium and Aging. Curr. Pharm. Des. 2010, 16, 832–839. [Google Scholar] [CrossRef] [PubMed]
- McCann, J.C.; Ames, B.N. An Overview of Evidence for a Causal Relation between Iron Deficiency during Development and Deficits in Cognitive or Behavioral Function. Am. J. Clin. Nutr. 2007, 85, 931–945. [Google Scholar] [CrossRef]
- Parkin, P.C.; Borkhoff, C.M.; Macarthur, C.; Abdullah, K.; Birken, C.S.; Fehlings, D.; Koroshegyi, C.; Maguire, J.L.; Mamak, E.; Mamdani, M.; et al. Randomized Trial of Oral Iron and Diet Advice versus Diet Advice Alone in Young Children with Nonanemic Iron Deficiency. J. Pediatr. 2021, 233, 233–240.e1. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.C.; Evans, D.A.; Tangney, C.C.; Bienias, J.L.; Wilson, R.S. Fish Consumption and Cognitive Decline with Age in a Large Community Study. Arch. Neurol. 2005, 62, 1849–1853. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, J.; Qiu, J.; Li, Y.; Wang, J.; Jiao, J. Intakes of Fish and Polyunsaturated Fatty Acids and Mild-to-Severe Cognitive Impairment Risks: A Dose-Response Meta-Analysis of 21 Cohort Studies. Am. J. Clin. Nutr. 2016, 103, 330–340. [Google Scholar] [CrossRef]
- Duarte, G.M.; De Araújo, F.E.A.; Da Rocha, J.M.C.; Idalina Neta, F.; Do Rego, A.C.M.; Araújo Filho, I.; Pinheiro, F.I.; De Azevedo, E.P.; Cobucci, R.N.; Guzen, F.P. Neuroprotective Potential of Seed Extracts: Review of In Vitro and In Vivo Studies. Nutrients 2023, 15, 2502. [Google Scholar] [CrossRef]
- Wang, S.; Luo, Q.; Zhou, Y.; Fan, P. CLG from Hemp Seed Inhibits LPS-Stimulated Neuroinflammation in BV2 Microglia by Regulating NF-κB and Nrf-2 Pathways. ACS Omega 2019, 4, 16517–16523. [Google Scholar] [CrossRef]
- Wang, S.; Luo, Q.; Fan, P. Cannabisin F from Hemp (Cannabis sativa) Seed Suppresses Lipopolysaccharide-Induced Inflammatory Responses in BV2 Microglia as SIRT1 Modulator. Int. J. Mol. Sci. 2019, 20, 507. [Google Scholar] [CrossRef] [PubMed]
- Bhuiyan, M.I.H.; Kim, J.Y.; Ha, T.J.; Kim, S.Y.; Cho, K.-O. Anthocyanins Extracted from Black Soybean Seed Coat Protect Primary Cortical Neurons against in Vitro Ischemia. Biol. Pharm. Bull. 2012, 35, 999–1008. [Google Scholar] [CrossRef]
- Ramírez-Salazar, S.A.; Herren, C.; McCartney, J.; Ortiz García, J.G. Dietary Insights in Neurological Diseases. Curr. Neurol. Neurosci. Rep. 2021, 21, 55. [Google Scholar] [CrossRef] [PubMed]
- Francis, H.M.; Stevenson, R.J. Potential for Diet to Prevent and Remediate Cognitive Deficits in Neurological Disorders. Nutr. Rev. 2018, 76, 204–217. [Google Scholar] [CrossRef]
- Chamoun, E.; Mutch, D.M.; Allen-Vercoe, E.; Buchholz, A.C.; Duncan, A.M.; Spriet, L.L.; Haines, J.; Ma, D.W.L.; on behalf of the Guelph Family Health Study. A Review of the Associations between Single Nucleotide Polymorphisms in Taste Receptors, Eating Behaviors, and Health. Crit. Rev. Food Sci. Nutr. 2018, 58, 194–207. [Google Scholar] [CrossRef]
- Gardener, H.; Caunca, M.R. Mediterranean Diet in Preventing Neurodegenerative Diseases. Curr. Nutr. Rep. 2018, 7, 10–20. [Google Scholar] [CrossRef]
- Estruch, R. Anti-Inflammatory Effects of the Mediterranean Diet: The Experience of the PREDIMED Study. Proc. Nutr. Soc. 2010, 69, 333–340. [Google Scholar] [CrossRef]
- Scarmeas, N.; Stern, Y.; Tang, M.-X.; Mayeux, R.; Luchsinger, J.A. Mediterranean Diet and Risk for Alzheimer’s Disease. Ann. Neurol. 2006, 59, 912–921. [Google Scholar] [CrossRef] [PubMed]
- Alcalay, R.N.; Gu, Y.; Mejia-Santana, H.; Cote, L.; Marder, K.S.; Scarmeas, N. The Association between Mediterranean Diet Adherence and Parkinson’s Disease. Mov. Disord. 2012, 27, 771–774. [Google Scholar] [CrossRef]
- Maraki, M.I.; Yannakoulia, M.; Stamelou, M.; Stefanis, L.; Xiromerisiou, G.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.M.; Sakka, P.; Anastasiou, C.A.; et al. Mediterranean Diet Adherence Is Related to Reduced Probability of Prodromal Parkinson’s Disease. Mov. Disord. 2019, 34, 48–57. [Google Scholar] [CrossRef]
- Metcalfe-Roach, A.; Yu, A.C.; Golz, E.; Cirstea, M.; Sundvick, K.; Kliger, D.; Foulger, L.H.; Mackenzie, M.; Finlay, B.B.; Appel-Cresswell, S. MIND and Mediterranean Diets Associated with Later Onset of Parkinson’s Disease. Mov. Disord. 2021, 36, 977–984. [Google Scholar] [CrossRef] [PubMed]
- Wahls, T.L. Dietary Approaches to Treating Multiple Sclerosis-Related Symptoms. Phys. Med. Rehabil. Clin. 2022, 33, 605–620. [Google Scholar] [CrossRef] [PubMed]
- Krikorian, R.; Shidler, M.D.; Summer, S.S.; Sullivan, P.G.; Duker, A.P.; Isaacson, R.S.; Espay, A.J. Nutritional Ketosis for Mild Cognitive Impairment in Parkinson’s Disease: A Controlled Pilot Trial. Clin. Park. Relat. Disord. 2019, 1, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Chen, S.; Huang, X.; Tong, H.; Niu, H.; Lu, L. Neuroprotective Effect of a Medium-Chain Triglyceride Ketogenic Diet on MPTP-Induced Parkinson’s Disease Mice: A Combination of Transcriptomics and Metabolomics in the Substantia Nigra and Fecal Microbiome. Cell Death Discov. 2023, 9, 251. [Google Scholar] [CrossRef]
- Krikorian, R.; Shidler, M.D.; Dangelo, K.; Couch, S.C.; Benoit, S.C.; Clegg, D.J. Dietary Ketosis Enhances Memory in Mild Cognitive Impairment. Neurobiol. Aging 2012, 33, 425.e19–425.e27. [Google Scholar] [CrossRef]
- Ko, A.; Kwon, H.E.; Kim, H.D. Updates on the Ketogenic Diet Therapy for Pediatric Epilepsy. Biomed. J. 2022, 45, 19–26. [Google Scholar] [CrossRef]
- Ruan, Y.; Chen, L.; She, D.; Chung, Y.; Ge, L.; Han, L. Ketogenic Diet for Epilepsy: An Overview of Systematic Review and Meta-Analysis. Eur. J. Clin. Nutr. 2022, 76, 1234–1244. [Google Scholar] [CrossRef]
- Verrotti, A.; Iapadre, G.; Di Francesco, L.; Zagaroli, L.; Farello, G. Diet in the Treatment of Epilepsy: What We Know So Far. Nutrients 2020, 12, 2645. [Google Scholar] [CrossRef]
- Wells, J.; Swaminathan, A.; Paseka, J.; Hanson, C. Efficacy and Safety of a Ketogenic Diet in Children and Adolescents with Refractory Epilepsy-A Review. Nutrients 2020, 12, 1809. [Google Scholar] [CrossRef]
- Mazurek, D.; Wyka, J. Down Syndrome--Genetic and Nutritional Aspects of Accompanying Disorders. Rocz. Panstw. Zakl. Hig. 2015, 66, 189–194. [Google Scholar]
- Duarte, A.C.; Costa, E.C.; Filipe, H.A.L.; Saraiva, S.M.; Jacinto, T.; Miguel, S.P.; Ribeiro, M.P.; Coutinho, P. Animal-Derived Products in Science and Current Alternatives. Biomater. Adv. 2023, 151, 213428. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C.; Teng, Y. Is It Time to Start Transitioning from 2D to 3D Cell Culture? Front. Mol. Biosci. 2020, 7, 33. [Google Scholar] [CrossRef]
- Kim, J.; Koo, B.-K.; Knoblich, J.A. Human Organoids: Model Systems for Human Biology and Medicine. Nat. Rev. Mol. Cell Biol. 2020, 21, 571–584. [Google Scholar] [CrossRef]
- Lee, H.-K.; Sanchez, C.V.; Chen, M.; Morin, P.J.; Wells, J.M.; Hanlon, E.B.; Xia, W. Three Dimensional Human Neuro-Spheroid Model of Alzheimer’s Disease Based on Differentiated Induced Pluripotent Stem Cells. PLoS ONE 2016, 11, e0163072. [Google Scholar] [CrossRef] [PubMed]
- Benchoua, A.; Lasbareilles, M.; Tournois, J. Contribution of Human Pluripotent Stem Cell-Based Models to Drug Discovery for Neurological Disorders. Cells 2021, 10, 3290. [Google Scholar] [CrossRef]
- Ma, K.; Gauthier, L.O.; Cheung, F.; Huang, S.; Lek, M. High-Throughput Assays to Assess Variant Effects on Disease. Dis. Model. Mech. 2024, 17, dmm050573. [Google Scholar] [CrossRef]
- Lee, D.D.H.; Cardinale, D.; Nigro, E.; Butler, C.R.; Rutman, A.; Fassad, M.R.; Hirst, R.A.; Moulding, D.; Agrotis, A.; Forsythe, E.; et al. Higher Throughput Drug Screening for Rare Respiratory Diseases: Readthrough Therapy in Primary Ciliary Dyskinesia. Eur. Respir. J. 2021, 58, 2000455. [Google Scholar] [CrossRef] [PubMed]
- Bellomo, F.; Medina, D.L.; De Leo, E.; Panarella, A.; Emma, F. High-Content Drug Screening for Rare Diseases. J. Inherit. Metab. Dis. 2017, 40, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.W.; Doh, I.; Nam, D.-H. Unified 2D and 3D Cell-Based High-Throughput Screening Platform Using a Micropillar/Microwell Chip. Sens. Actuators Chem. 2016, 228, 523–528. [Google Scholar] [CrossRef]
- Yamamoto, S.; Kanca, O.; Wangler, M.F.; Bellen, H.J. Integrating Non-Mammalian Model Organisms in the Diagnosis of Rare Genetic Diseases in Humans. Nat. Rev. Genet. 2024, 25, 46–60. [Google Scholar] [CrossRef]
- Cabasso, O.; Kuppuramalingam, A.; Lelieveld, L.; Van der Lienden, M.; Boot, R.; Aerts, J.M.; Horowitz, M. Animal Models for the Study of Gaucher Disease. Int. J. Mol. Sci. 2023, 24, 16035. [Google Scholar] [CrossRef] [PubMed]
- Vallender, E.J.; Hotchkiss, C.E.; Lewis, A.D.; Rogers, J.; Stern, J.A.; Peterson, S.M.; Ferguson, B.; Sayers, K. Nonhuman Primate Genetic Models for the Study of Rare Diseases. Orphanet J. Rare Dis. 2023, 18, 20. [Google Scholar] [CrossRef] [PubMed]
- Phillips, K.A.; Bales, K.L.; Capitanio, J.P.; Conley, A.; Czoty, P.W.; ‘t Hart, B.A.; Hopkins, W.D.; Hu, S.-L.; Miller, L.A.; Nader, M.A.; et al. Why Primate Models Matter. Am. J. Primatol. 2014, 76, 801–827. [Google Scholar] [CrossRef] [PubMed]
- Bryda, E.C. The Mighty Mouse: The Impact of Rodents on Advances in Biomedical Research. Mo. Med. 2013, 110, 207–211. [Google Scholar]
- Doyle, A.; McGarry, M.P.; Lee, N.A.; Lee, J.J. The Construction of Transgenic and Gene Knockout/Knockin Mouse Models of Human Disease. Transgenic Res. 2012, 21, 327–349. [Google Scholar] [CrossRef]
- Bergen, W.G.; Mersmann, H.J. Comparative Aspects of Lipid Metabolism: Impact on Contemporary Research and Use of Animal Models1. J. Nutr. 2005, 135, 2499–2502. [Google Scholar] [CrossRef]
- Duchen, L.W.; Eicher, E.M.; Jacobs, J.M.; Scaravilli, F.; Teixeira, F. Hereditary Leucodystrophy in the Mouse: The New Mutant Twitcher. Brain 1980, 103, 695–710. [Google Scholar] [CrossRef]
- Da Silva-Buttkus, P.; Spielmann, N.; Klein-Rodewald, T.; Schütt, C.; Aguilar-Pimentel, A.; Amarie, O.V.; Becker, L.; Calzada-Wack, J.; Garrett, L.; Gerlini, R.; et al. Knockout Mouse Models as a Resource for the Study of Rare Diseases. Mamm. Genome 2023, 34, 244–261. [Google Scholar] [CrossRef]
- Julkowska, D.; Austin, C.P.; Cutillo, C.M.; Gancberg, D.; Hager, C.; Halftermeyer, J.; Jonker, A.H.; Lau, L.P.L.; Norstedt, I.; Rath, A.; et al. The Importance of International Collaboration for Rare Diseases Research: A European Perspective. Gene Ther. 2017, 24, 562–571. [Google Scholar] [CrossRef]
- Monaco, L.; Zanello, G.; Baynam, G.; Jonker, A.H.; Julkowska, D.; Hartman, A.L.; O’Connor, D.; Wang, C.M.; Wong-Rieger, D.; Pearce, D.A. Research on Rare Diseases: Ten Years of Progress and Challenges at IRDiRC. Nat. Rev. Drug Discov. 2022, 21, 319–320. [Google Scholar] [CrossRef]
- Kropp, P.A.; Bauer, R.; Zafra, I.; Graham, C.; Golden, A. Caenorhabditis elegans for Rare Disease Modeling and Drug Discovery: Strategies and Strengths. Dis. Model. Mech. 2021, 14, dmm049010. [Google Scholar] [CrossRef] [PubMed]
- O’Kane, C.J. Modelling Human Diseases in Drosophila and Caenorhabditis. Semin. Cell Dev. Biol. 2003, 14, 3–10. [Google Scholar] [CrossRef]
- Lai, C.-H.; Chou, C.-Y.; Ch’ang, L.-Y.; Liu, C.-S.; Lin, W. Identification of Novel Human Genes Evolutionarily Conserved in Caenorhabditis elegans by Comparative Proteomics. Genome Res. 2000, 10, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Schafer, W.R. Deciphering the Neural and Molecular Mechanisms of C. elegans Behavior. Curr. Biol. 2005, 15, R723–R729. [Google Scholar] [CrossRef]
- Paix, A.; Folkmann, A.; Rasoloson, D.; Seydoux, G. High Efficiency, Homology-Directed Genome Editing in Caenorhabditis elegans Using CRISPR-Cas9 Ribonucleoprotein Complexes. Genetics 2015, 201, 47–54. [Google Scholar] [CrossRef]
- Paix, A.; Schmidt, H.; Seydoux, G. Cas9-Assisted Recombineering in C. elegans: Genome Editing Using in vivo Assembly of Linear DNAs. Nucleic Acids Res. 2016, 44, e128. [Google Scholar] [CrossRef]
- Aoyagi, K.; Rossignol, E.; Hamdan, F.F.; Mulcahy, B.; Xie, L.; Nagamatsu, S.; Rouleau, G.A.; Zhen, M.; Michaud, J.L. A Gain-of-Function Mutation in NALCN in a Child with Intellectual Disability, Ataxia, and Arthrogryposis. Hum. Mutat. 2015, 36, 753–757. [Google Scholar] [CrossRef] [PubMed]
- Lange, K.I.; Tsiropoulou, S.; Kucharska, K.; Blacque, O.E. Interpreting the Pathogenicity of Joubert Syndrome Missense Variants in Caenorhabditis elegans. Dis. Model. Mech. 2021, 14, dmm046631. [Google Scholar] [CrossRef]
- Bachmann-Gagescu, R.; Dempsey, J.C.; Phelps, I.G.; O’Roak, B.J.; Knutzen, D.M.; Rue, T.C.; Ishak, G.E.; Isabella, C.R.; Gorden, N.; Adkins, J.; et al. Joubert Syndrome: A Model for Untangling Recessive Disorders with Extreme Genetic Heterogeneity. J. Med. Genet. 2015, 52, 514–522. [Google Scholar] [CrossRef]
- Jia, F.; Cui, M.; Than, M.T.; Han, M. Developmental Defects of Caenorhabditis elegans Lacking Branched-Chain α-Ketoacid Dehydrogenase Are Mainly Caused by Monomethyl Branched-Chain Fatty Acid Deficiency. J. Biol. Chem. 2016, 291, 2967–2973. [Google Scholar] [CrossRef]
- Verheyen, E.M. The Power of Drosophila in Modeling Human Disease Mechanisms. Dis. Model. Mech. 2022, 15, dmm049549. [Google Scholar] [CrossRef] [PubMed]
- Adams, M.D.; Celniker, S.E.; Holt, R.A.; Evans, C.A.; Gocayne, J.D.; Amanatides, P.G.; Scherer, S.E.; Li, P.W.; Hoskins, R.A.; Galle, R.F.; et al. The Genome Sequence of Drosophila melanogaster. Science 2000, 287, 2185–2195. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Flockhart, I.; Vinayagam, A.; Bergwitz, C.; Berger, B.; Perrimon, N.; Mohr, S.E. An Integrative Approach to Ortholog Prediction for Disease-Focused and Other Functional Studies. BMC Bioinform. 2011, 12, 357. [Google Scholar] [CrossRef]
- Reiter, L.T.; Potocki, L.; Chien, S.; Gribskov, M.; Bier, E. A Systematic Analysis of Human Disease-Associated Gene Sequences in Drosophila melanogaster. Genome Res. 2001, 11, 1114–1125. [Google Scholar] [CrossRef]
- Bellen, H.J.; Wangler, M.F.; Yamamoto, S. The Fruit Fly at the Interface of Diagnosis and Pathogenic Mechanisms of Rare and Common Human Diseases. Hum. Mol. Genet. 2019, 28, R207–R214. [Google Scholar] [CrossRef]
- Harnish, J.M.; Deal, S.L.; Chao, H.-T.; Wangler, M.F.; Yamamoto, S. In Vivo Functional Study of Disease-Associated Rare Human Variants Using Drosophila. J. Vis. Exp. 2019, 150. [Google Scholar] [CrossRef]
- Kanca, O.; Bellen, H.J.; Schnorrer, F. Gene Tagging Strategies to Assess Protein Expression, Localization, and Function in Drosophila. Genetics 2017, 207, 389–412. [Google Scholar] [CrossRef]
- Mele, S.; Martelli, F.; Lin, J.; Kanca, O.; Christodoulou, J.; Bellen, H.J.; Piper, M.D.W.; Johnson, T.K. Drosophila as a Diet Discovery Tool for Treating Amino Acid Disorders. Trends Endocrinol. Metab. 2023, 34, 85–105. [Google Scholar] [CrossRef] [PubMed]
- Martelli, F.; Quig, A.; Mele, S.; Lin, J.; Fulton, T.L.; Wansbrough, M.; Barlow, C.K.; Schittenhelm, R.B.; Johnson, T.K.; Piper, M.D.W. A Defined Diet for Pre-Adult Drosophila melanogaster. Sci. Rep. 2024, 14, 6974. [Google Scholar] [CrossRef]
- Baxendale, S.; Van Eeden, F.; Wilkinson, R. The Power of Zebrafish in Personalised Medicine. In Personalised Medicine; El-Khamisy, S., Ed.; Advances in Experimental Medicine and Biology; Springer International Publishing: Cham, Switzerland, 2017; Volume 1007, pp. 179–197. ISBN 978-3-319-60731-3. [Google Scholar]
- Howe, K.; Clark, M.D.; Torroja, C.F.; Torrance, J.; Berthelot, C.; Muffato, M.; Collins, J.E.; Humphray, S.; McLaren, K.; Matthews, L.; et al. The Zebrafish Reference Genome Sequence and Its Relationship to the Human Genome. Nature 2013, 496, 498–503. [Google Scholar] [CrossRef]
- Choi, T.-Y.; Choi, T.-I.; Lee, Y.-R.; Choe, S.-K.; Kim, C.-H. Zebrafish as an Animal Model for Biomedical Research. Exp. Mol. Med. 2021, 53, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Son, M.; Kim, D.Y.; Kim, C.-H. Disease Modeling of Rare Neurological Disorders in Zebrafish. Int. J. Mol. Sci. 2022, 23, 3946. [Google Scholar] [CrossRef]
- Crouzier, L.; Richard, E.M.; Sourbron, J.; Lagae, L.; Maurice, T.; Delprat, B. Use of Zebrafish Models to Boost Research in Rare Genetic Diseases. Int. J. Mol. Sci. 2021, 22, 13356. [Google Scholar] [CrossRef] [PubMed]
- Sloan, J.L.; Achilly, N.P.; Arnold, M.L.; Catlett, J.L.; Blake, T.; Bishop, K.; Jones, M.; Harper, U.; English, M.A.; Anderson, S.; et al. The Vitamin B12 Processing Enzyme, Mmachc, Is Essential for Zebrafish Survival, Growth and Retinal Morphology. Hum. Mol. Genet. 2020, 29, 2109–2123. [Google Scholar] [CrossRef] [PubMed]
- Rath, A.; Salamon, V.; Peixoto, S.; Hivert, V.; Laville, M.; Segrestin, B.; Neugebauer, E.A.M.; Eikermann, M.; Bertele, V.; Garattini, S.; et al. A Systematic Literature Review of Evidence-Based Clinical Practice for Rare Diseases: What Are the Perceived and Real Barriers for Improving the Evidence and How Can They Be Overcome? Trials 2017, 18, 556. [Google Scholar] [CrossRef]
- Chang, X.; Zhang, J.; Jiang, Y.; Shang, M.; Wu, Y. A Survey of Registered Pharmacological Clinical Trials on Rare Neurological Diseases in Children in 2010–2020. Front. Pediatr. 2022, 10, 963601. [Google Scholar] [CrossRef]
- Lumsden, J.M.; Urv, T.K. The Rare Diseases Clinical Research Network: A Model for Clinical Trial Readiness. Ther. Adv. Rare Dis. 2023, 4, 26330040231219272. [Google Scholar] [CrossRef]
- U.S. Food & Drug Administration. Rare Diseases: Natural History Studies for Drug Development 2019. Available online: https://www.Fda.Gov/Regulatory-Information/Search-Fda-Guidance-Documents/Rare-Diseases-Natural-History-Studies-Drug-Development (accessed on 28 June 2024).
- U.S. Food & Drug Administration. FDA Approves Givosiran for Acute Hepatic Porphyria: U.S. Food and Drug Administration. Available online: https://www.Fda.Gov/Drugs/Resources-Information-Approved-Drugs/Fda-Approves-Givosiran-Acute-Hepatic-Porphyria (accessed on 18 December 2023).
- Al-Horani, R.A.; Chiles, R. First Therapeutic Approval for Eosinophilic Esophagitis. Gastroenterol. Insights 2022, 13, 238–244. [Google Scholar] [CrossRef]
- U.S. Food & Drug Administration. FDA Approves First Treatment for Rett Syndrome. Available online: https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-first-treatment-rett-syndrome (accessed on 18 June 2024).
- Piwek, L.; Ellis, D.A.; Andrews, S.; Joinson, A. The Rise of Consumer Health Wearables: Promises and Barriers. PLoS Med. 2016, 13, e1001953. [Google Scholar] [CrossRef]
- Youn, B.-Y.; Ko, Y.; Moon, S.; Lee, J.; Ko, S.-G.; Kim, J.-Y. Digital Biomarkers for Neuromuscular Disorders: A Systematic Scoping Review. Diagnostics 2021, 11, 1275. [Google Scholar] [CrossRef]
- Sica, M.; Tedesco, S.; Crowe, C.; Kenny, L.; Moore, K.; Timmons, S.; Barton, J.; O’Flynn, B.; Komaris, D.-S. Continuous Home Monitoring of Parkinson’s Disease Using Inertial Sensors: A Systematic Review. PLoS ONE 2021, 16, e0246528. [Google Scholar] [CrossRef] [PubMed]
- Vienne-Jumeau, A.; Quijoux, F.; Vidal, P.-P.; Ricard, D. Wearable Inertial Sensors Provide Reliable Biomarkers of Disease Severity in Multiple Sclerosis: A Systematic Review and Meta-Analysis. Ann. Phys. Rehabil. Med. 2020, 63, 138–147. [Google Scholar] [CrossRef] [PubMed]
- Ricotti, V.; Kadirvelu, B.; Selby, V.; Festenstein, R.; Mercuri, E.; Voit, T.; Faisal, A.A. Wearable Full-Body Motion Tracking of Activities of Daily Living Predicts Disease Trajectory in Duchenne Muscular Dystrophy. Nat. Med. 2023, 29, 95–103. [Google Scholar] [CrossRef]
- Liu, X.; Chen, H.; Zhong, Y.; Lee, T.-Y.; Han, W.; Yu, D.; Liu, H.; Ji, J. Diet Therapy in Patients with Rare Diseases: A Scoping Review. J. Hum. Nutr. Diet. 2023, 36, 742–753. [Google Scholar] [CrossRef] [PubMed]
- Camp, K.M.; Lloyd-Puryear, M.A.; Yao, L.; Groft, S.C.; Parisi, M.A.; Mulberg, A.; Gopal-Srivastava, R.; Cederbaum, S.; Enns, G.M.; Ershow, A.G.; et al. Expanding Research to Provide an Evidence Base for Nutritional Interventions for the Management of Inborn Errors of Metabolism. Mol. Genet. Metab. 2013, 109, 319–328. [Google Scholar] [CrossRef]
- Kishino, T.; Lalande, M.; Wagstaff, J. UBE3A/E6-AP Mutations Cause Angelman Syndrome. Nat. Genet. 1997, 15, 70–73. [Google Scholar] [CrossRef] [PubMed]
- Samanta, D. Epilepsy in Angelman Syndrome: A Scoping Review. Brain Dev. 2021, 43, 32–44. [Google Scholar] [CrossRef]
- Stein, D.; Chetty, M.; Rho, J.M. A “Happy” Toddler Presenting with Sudden, Life-Threatening Seizures. Semin. Pediatr. Neurol. 2010, 17, 35–38. [Google Scholar] [CrossRef]
- Evangeliou, A.; Doulioglou, V.; Haidopoulou, K.; Aptouramani, M.; Spilioti, M.; Varlamis, G. Ketogenic Diet in a Patient with Angelman Syndrome. Pediatr. Int. 2010, 52, 831–834. [Google Scholar] [CrossRef]
- Grocott, O.R.; Herrington, K.S.; Pfeifer, H.H.; Thiele, E.A.; Thibert, R.L. Low Glycemic Index Treatment for Seizure Control in Angelman Syndrome: A Case Series from the Center for Dietary Therapy of Epilepsy at the Massachusetts General Hospital. Epilepsy Behav. EB 2017, 68, 45–50. [Google Scholar] [CrossRef]
- Thibert, R.L.; Pfeifer, H.H.; Larson, A.M.; Raby, A.R.; Reynolds, A.A.; Morgan, A.K.; Thiele, E.A. Low Glycemic Index Treatment for Seizures in Angelman Syndrome. Epilepsia 2012, 53, 1498–1502. [Google Scholar] [CrossRef] [PubMed]
- Ciarlone, S.L.; Grieco, J.C.; D’Agostino, D.P.; Weeber, E.J. Ketone Ester Supplementation Attenuates Seizure Activity, and Improves Behavior and Hippocampal Synaptic Plasticity in an Angelman Syndrome Mouse Model. Neurobiol. Dis. 2016, 96, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Romero, L.O.; Caires, R.; Kaitlyn Victor, A.; Ramirez, J.; Sierra-Valdez, F.J.; Walsh, P.; Truong, V.; Lee, J.; Mayor, U.; Reiter, L.T.; et al. Linoleic Acid Improves PIEZO2 Dysfunction in a Mouse Model of Angelman Syndrome. Nat. Commun. 2023, 14, 1167. [Google Scholar] [CrossRef] [PubMed]
- Herber, D.L.; Weeber, E.J.; D’Agostino, D.P.; Duis, J. Evaluation of the Safety and Tolerability of a Nutritional Formulation in Patients with ANgelman Syndrome (FANS): Study Protocol for a Randomized Controlled Trial. Trials 2020, 21, 60. [Google Scholar] [CrossRef] [PubMed]
- Carson, R.P.; Herber, D.L.; Pan, Z.; Phibbs, F.; Key, A.P.; Gouelle, A.; Ergish, P.; Armour, E.A.; Patel, S.; Duis, J. Nutritional Formulation for Patients with Angelman Syndrome: A Randomized, Double-Blind, Placebo-Controlled Study of Exogenous Ketones. J. Nutr. 2021, 151, 3628–3636. [Google Scholar] [CrossRef]
- Bird, L.M.; Tan, W.-H.; Bacino, C.A.; Peters, S.U.; Skinner, S.A.; Anselm, I.; Barbieri-Welge, R.; Bauer-Carlin, A.; Gentile, J.K.; Glaze, D.G.; et al. A Therapeutic Trial of Pro-Methylation Dietary Supplements in Angelman Syndrome. Am. J. Med. Genet. Part A 2011, 155, 2956–2963. [Google Scholar] [CrossRef]
- Han, J.; Bichell, T.J.; Golden, S.; Anselm, I.; Waisbren, S.; Bacino, C.A.; Peters, S.U.; Bird, L.M.; Kimonis, V. A Placebo-Controlled Trial of Folic Acid and Betaine in Identical Twins with Angelman Syndrome. Orphanet J. Rare Dis. 2019, 14, 232. [Google Scholar] [CrossRef]
- Neul, J.L.; Benke, T.A.; Marsh, E.D.; Skinner, S.A.; Merritt, J.; Lieberman, D.N.; Standridge, S.; Feyma, T.; Heydemann, P.; Peters, S.; et al. The Array of Clinical Phenotypes of Males with Mutations in Methyl-CpG Binding Protein 2. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2019, 180, 55–67. [Google Scholar] [CrossRef]
- Hagberg, B. Rett’s Syndrome: Prevalence and Impact on Progressive Severe Mental Retardation in Girls. Acta Paediatr. Scand. 1985, 74, 405–408. [Google Scholar] [CrossRef]
- Neul, J.L.; Kaufmann, W.E.; Glaze, D.G.; Christodoulou, J.; Clarke, A.J.; Bahi-Buisson, N.; Leonard, H.; Bailey, M.E.S.; Schanen, N.C.; Zappella, M.; et al. Rett Syndrome: Revised Diagnostic Criteria and Nomenclature. Ann. Neurol. 2010, 68, 944–950. [Google Scholar] [CrossRef]
- Neul, J.L.; Lane, J.B.; Lee, H.-S.; Geerts, S.; Barrish, J.O.; Annese, F.; Baggett, L.M.; Barnes, K.; Skinner, S.A.; Motil, K.J.; et al. Developmental Delay in Rett Syndrome: Data from the Natural History Study. J. Neurodev. Disord. 2014, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Hagberg, B. Clinical Manifestations and Stages of Rett Syndrome. Ment. Retard. Dev. Disabil. Res. Rev. 2002, 8, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Percy, A.K.; Neul, J.L.; Glaze, D.G.; Motil, K.J.; Skinner, S.A.; Khwaja, O.; Lee, H.-S.; Lane, J.B.; Barrish, J.O.; Annese, F.; et al. Rett Syndrome Diagnostic Criteria: Lessons from the Natural History Study. Ann. Neurol. 2010, 68, 951–955. [Google Scholar] [CrossRef] [PubMed]
- Chahrour, M.; Zoghbi, H.Y. The Story of Rett Syndrome: From Clinic to Neurobiology. Neuron 2007, 56, 422–437. [Google Scholar] [CrossRef]
- Amir, R.E.; Van den Veyver, I.B.; Wan, M.; Tran, C.Q.; Francke, U.; Zoghbi, H.Y. Rett Syndrome Is Caused by Mutations in X-Linked MECP2, Encoding Methyl-CpG-Binding Protein 2. Nat. Genet. 1999, 23, 185–188. [Google Scholar] [CrossRef]
- Good, K.V.; Vincent, J.B.; Ausió, J. MeCP2: The Genetic Driver of Rett Syndrome Epigenetics. Front. Genet. 2021, 12, 620859. [Google Scholar] [CrossRef]
- Frullanti, E.; Papa, F.T.; Grillo, E.; Clarke, A.; Ben-Zeev, B.; Pineda, M.; Bahi-Buisson, N.; Bienvenu, T.; Armstrong, J.; Roche Martinez, A.; et al. Analysis of the Phenotypes in the Rett Networked Database. Int. J. Genom. 2019, 2019, 6956934. [Google Scholar] [CrossRef]
- Palmieri, M.; Pozzer, D.; Landsberger, N. Advanced Genetic Therapies for the Treatment of Rett Syndrome: State of the Art and Future Perspectives. Front. Neurosci. 2023, 17, 1172805. [Google Scholar] [CrossRef]
- Cohen, D.R.S.; Matarazzo, V.; Palmer, A.M.; Tu, Y.; Jeon, O.-H.; Pevsner, J.; Ronnett, G.V. Expression of MeCP2 in Olfactory Receptor Neurons Is Developmentally Regulated and Occurs before Synaptogenesis. Mol. Cell. Neurosci. 2003, 22, 417–429. [Google Scholar] [CrossRef]
- Belichenko, P.V.; Wright, E.E.; Belichenko, N.P.; Masliah, E.; Li, H.H.; Mobley, W.C.; Francke, U. Widespread Changes in Dendritic and Axonal Morphology in Mecp2-Mutant Mouse Models of Rett Syndrome: Evidence for Disruption of Neuronal Networks. J. Comp. Neurol. 2009, 514, 240–258. [Google Scholar] [CrossRef]
- Kishi, N.; Macklis, J.D. Dissecting MECP2 Function in the Central Nervous System. J. Child Neurol. 2005, 20, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Fasolino, M.; Zhou, Z. The Crucial Role of DNA Methylation and MeCP2 in Neuronal Function. Genes 2017, 8, 141. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.C.; Archer, H.L.; Colley, J.P.; Ravn, K.; Nielsen, J.B.; Kerr, A.; Williams, E.; Christodoulou, J.; Gécz, J.; Jardine, P.E.; et al. Early Onset Seizures and Rett-like Features Associated with Mutations in CDKL5. Eur. J. Hum. Genet. EJHG 2005, 13, 1113–1120. [Google Scholar] [CrossRef]
- Philippe, C.; Amsallem, D.; Francannet, C.; Lambert, L.; Saunier, A.; Verneau, F.; Jonveaux, P. Phenotypic Variability in Rett Syndrome Associated with FOXG1 Mutations in Females. J. Med. Genet. 2010, 47, 59–65. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Neul, J.L.; Percy, A.K.; Benke, T.A.; Berry-Kravis, E.M.; Glaze, D.G.; Marsh, E.D.; Lin, T.; Stankovic, S.; Bishop, K.M.; Youakim, J.M. Trofinetide for the Treatment of Rett Syndrome: A Randomized Phase 3 Study. Nat. Med. 2023, 29, 1468–1475. [Google Scholar] [CrossRef]
- Singh, A.; Balasundaram, M.K.; Gupta, D. Trofinetide in Rett Syndrome: A Brief Review of Safety and Efficacy. Intractable Rare Dis. Res. 2023, 12, 262–266. [Google Scholar] [CrossRef]
- Czerwonogrodzka-Senczyna, A.; Milewska, M.; Kwiecień, P.; Szczałuba, K. Diet and Nutritional Status of Polish Girls with Rett Syndrome-A Case-Control Study. Nutrients 2023, 15, 3334. [Google Scholar] [CrossRef]
- Lotan, M.; Zysman, L. The Digestive System and Nutritional Considerations for Individuals with Rett Syndrome. Sci. World J. 2006, 6, 1737–1749. [Google Scholar] [CrossRef]
- Motil, K.J.; Barrish, J.O.; Lane, J.; Geerts, S.P.; Annese, F.; McNair, L.; Percy, A.K.; Skinner, S.A.; Neul, J.L.; Glaze, D.G. Vitamin D Deficiency Is Prevalent in Girls and Women with Rett Syndrome. J. Pediatr. Gastroenterol. Nutr. 2011, 53, 569–574. [Google Scholar] [CrossRef]
- Haas, R.H.; Dixon, S.D.; Sartoris, D.J.; Hennessy, M.J. Osteopenia in Rett Syndrome. J. Pediatr. 1997, 131, 771–774. [Google Scholar] [CrossRef]
- Motil, K.J.; Barrish, J.O.; Neul, J.L.; Glaze, D.G. Low Bone Mineral Mass Is Associated with Decreased Bone Formation and Diet in Females with Rett Syndrome. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 386. [Google Scholar] [CrossRef]
- Borghi, E.; Borgo, F.; Severgnini, M.; Savini, M.N.; Casiraghi, M.C.; Vignoli, A. Rett Syndrome: A Focus on Gut Microbiota. Int. J. Mol. Sci. 2017, 18, 344. [Google Scholar] [CrossRef] [PubMed]
- Gallucci, A.; Patterson, K.; Weit, A.; Van Der Pol, W.; Dubois, L.; Percy, A.; Morrow, C.; Campbell, S.; Olsen, M. Microbial Community Changes in a Female Rat Model of Rett Syndrome. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 109, 110259. [Google Scholar] [CrossRef]
- Wong, L.C.; Hsu, C.J.; Wu, Y.T.; Chu, H.F.; Lin, J.H.; Wang, H.P.; Hu, S.C.; Tsai, Y.C.; Tsai, W.C.; Lee, W.T. Investigating the impact of probiotic on neurological outcomes in Rett syndrome: A randomized, double-blind, and placebo-controlled pilot study. Autism 2024, 28, 2267–2281. [Google Scholar] [CrossRef] [PubMed]
- Chin, E.W.M.; Marcy, G.; Yoon, S.-I.; Ma, D.; Rosales, F.J.; Augustine, G.J.; Goh, E.L.K. Choline Ameliorates Disease Phenotypes in Human iPSC Models of Rett Syndrome. Neuromolecular Med. 2016, 18, 364–377. [Google Scholar] [CrossRef] [PubMed]
- Nag, N.; Berger-Sweeney, J.E. Postnatal Dietary Choline Supplementation Alters Behavior in a Mouse Model of Rett Syndrome. Neurobiol. Dis. 2007, 26, 473–480. [Google Scholar] [CrossRef]
- Nag, N.; Ward, B.; Berger-Sweeney, J.E. Nutritional Factors in a Mouse Model of Rett Syndrome. Neurosci. Biobehav. Rev. 2009, 33, 586–592. [Google Scholar] [CrossRef]
- Freilinger, M.; Dunkler, D.; Lanator, I.; Item, C.B.; Mühl, A.; Fowler, B.; Bodamer, O.A. Effects of Creatine Supplementation in Rett Syndrome: A Randomized, Placebo-Controlled Trial. J. Dev. Behav. Pediatr. JDBP 2011, 32, 454–460. [Google Scholar] [CrossRef]
- Cortelazzo, A.; Pietri, T.; De Felice, C.; Leoncini, S.; Guerranti, R.; Signorini, C.; Timperio, A.M.; Zolla, L.; Ciccoli, L.; Hayek, J. Proteomic Analysis of the Rett Syndrome Experimental Model mecp2Q63X Mutant Zebrafish. J. Proteom. 2017, 154, 128–133. [Google Scholar] [CrossRef]
- Gold, W.A.; Williamson, S.L.; Kaur, S.; Hargreaves, I.P.; Land, J.M.; Pelka, G.J.; Tam, P.P.L.; Christodoulou, J. Mitochondrial Dysfunction in the Skeletal Muscle of a Mouse Model of Rett Syndrome (RTT): Implications for the Disease Phenotype. Mitochondrion 2014, 15, 10–17. [Google Scholar] [CrossRef]
- De Felice, C.; Ciccoli, L.; Leoncini, S.; Signorini, C.; Rossi, M.; Vannuccini, L.; Guazzi, G.; Latini, G.; Comporti, M.; Valacchi, G.; et al. Systemic Oxidative Stress in Classic Rett Syndrome. Free Radic. Biol. Med. 2009, 47, 440–448. [Google Scholar] [CrossRef] [PubMed]
- De Felice, C.; Della Ragione, F.; Signorini, C.; Leoncini, S.; Pecorelli, A.; Ciccoli, L.; Scalabrì, F.; Marracino, F.; Madonna, M.; Belmonte, G.; et al. Oxidative Brain Damage in Mecp2-Mutant Murine Models of Rett Syndrome. Neurobiol. Dis. 2014, 68, 66–77. [Google Scholar] [CrossRef] [PubMed]
- Nagy, G.; Ackerman, S. Cholesterol Metabolism and Rett Syndrome Pathogenesis. Fac. Res. 2013 2013, 45, 965–967. [Google Scholar] [CrossRef]
- Signorini, C.; De Felice, C.; Leoncini, S.; Giardini, A.; D’Esposito, M.; Filosa, S.; Della Ragione, F.; Rossi, M.; Pecorelli, A.; Valacchi, G.; et al. F4-Neuroprostanes Mediate Neurological Severity in Rett Syndrome. Clin. Chim. Acta 2011, 412, 1399–1406. [Google Scholar] [CrossRef]
- Leoncini, S.; De Felice, C.; Signorini, C.; Pecorelli, A.; Durand, T.; Valacchi, G.; Ciccoli, L.; Hayek, J. Oxidative Stress in Rett Syndrome: Natural History, Genotype, and Variants. Redox Rep. 2011, 16, 145–153. [Google Scholar] [CrossRef]
- Signorini, C.; De Felice, C.; Leoncini, S.; Durand, T.; Galano, J.-M.; Cortelazzo, A.; Zollo, G.; Guerranti, R.; Gonnelli, S.; Caffarelli, C.; et al. Altered Erythrocyte Membrane Fatty Acid Profile in Typical Rett Syndrome: Effects of Omega-3 Polyunsaturated Fatty Acid Supplementation. Prostaglandins Leukot. Essent. Fatty Acids 2014, 91, 183–193. [Google Scholar] [CrossRef]
- De Felice, C.; Signorini, C.; Durand, T.; Ciccoli, L.; Leoncini, S.; D’Esposito, M.; Filosa, S.; Oger, C.; Guy, A.; Bultel-Poncé, V.; et al. Partial Rescue of Rett Syndrome by ω-3 Polyunsaturated Fatty Acids (PUFAs) Oil. Genes Nutr. 2012, 7, 447–458. [Google Scholar] [CrossRef] [PubMed]
- Park, M.J.; Aja, S.; Li, Q.; Degano, A.L.; Penati, J.; Zhuo, J.; Roe, C.R.; Ronnett, G.V. Anaplerotic Triheptanoin Diet Enhances Mitochondrial Substrate Use to Remodel the Metabolome and Improve Lifespan, Motor Function, and Sociability in MeCP2-Null Mice. PLoS ONE 2014, 9, e109527. [Google Scholar] [CrossRef]
- Mouro, F.M.; Miranda-Lourenço, C.; Sebastião, A.M.; Diógenes, M.J. From Cannabinoids and Neurosteroids to Statins and the Ketogenic Diet: New Therapeutic Avenues in Rett Syndrome? Front. Neurosci. 2019, 13, 680. [Google Scholar] [CrossRef]
- Zamberletti, E.; Gabaglio, M.; Piscitelli, F.; Brodie, J.S.; Woolley-Roberts, M.; Barbiero, I.; Tramarin, M.; Binelli, G.; Landsberger, N.; Kilstrup-Nielsen, C.; et al. Cannabidivarin Completely Rescues Cognitive Deficits and Delays Neurological and Motor Defects in Male Mecp2 Mutant Mice. J. Psychopharmacol. 2019, 33, 894–907. [Google Scholar] [CrossRef]
- Vigli, D.; Cosentino, L.; Raggi, C.; Laviola, G.; Woolley-Roberts, M.; De Filippis, B. Chronic Treatment with the Phytocannabinoid Cannabidivarin (CBDV) Rescues Behavioural Alterations and Brain Atrophy in a Mouse Model of Rett Syndrome. Neuropharmacology 2018, 140, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Haas, R.H.; Rice, M.A.; Trauner, D.A.; Merritt, T.A.; Opitz, J.M.; Reynolds, J.F. Therapeutic Effects of a Ketogenic Diet in Rett Syndrome. Am. J. Med. Genet. 1986, 25, 225–246. [Google Scholar] [CrossRef] [PubMed]
- Liebhaber, G.M.; Riemann, E.; Matthias Baumeister, F.A. Ketogenic Diet in Rett Syndrome. J. Child Neurol. 2003, 18, 74–75. [Google Scholar] [CrossRef] [PubMed]
- van der Louw, E.; van den Hurk, D.; Neal, E.; Leiendecker, B.; Fitzsimmon, G.; Dority, L.; Thompson, L.; Marchió, M.; Dudzińska, M.; Dressler, A.; et al. Ketogenic Diet Guidelines for Infants with Refractory Epilepsy. Eur. J. Paediatr. Neurol. 2016, 20, 798–809. [Google Scholar] [CrossRef] [PubMed]
- Rogawski, M.A.; Löscher, W.; Rho, J.M. Mechanisms of Action of Antiseizure Drugs and the Ketogenic Diet. Cold Spring Harb. Perspect. Med. 2016, 6, a022780. [Google Scholar] [CrossRef] [PubMed]
- Masino, S.A.; Li, T.; Theofilas, P.; Sandau, U.S.; Ruskin, D.N.; Fredholm, B.B.; Geiger, J.D.; Aronica, E.; Boison, D. A Ketogenic Diet Suppresses Seizures in Mice through Adenosine A1 Receptors. J. Clin. Investig. 2011, 121, 2679–2683. [Google Scholar] [CrossRef]
- Miyatake, T.; Suzuki, K. Globoid Cell Leukodystrophy: Additional Deficiency of Psychosine Galactosidase. Biochem. Biophys. Res. Commun. 1972, 48, 539–543. [Google Scholar] [CrossRef]
- Suzuki, K. Twenty Five Years of the “Psychosine Hypothesis”: A Personal Perspective of Its History and Present Status. Neurochem. Res. 1998, 23, 251–259. [Google Scholar] [CrossRef]
- Won, J.-S.; Singh, A.K.; Singh, I. Biochemical, Cell Biological, Pathological, and Therapeutic Aspects of Krabbe’s Disease. J. Neurosci. Res. 2016, 94, 990–1006. [Google Scholar] [CrossRef]
- Graziano, A.C.E.; Parenti, R.; Avola, R.; Cardile, V. Krabbe Disease: Involvement of Connexin43 in the Apoptotic Effects of Sphingolipid Psychosine on Mouse Oligodendrocyte Precursors. Apoptosis Int. J. Program. Cell Death 2016, 21, 25–35. [Google Scholar] [CrossRef]
- Avola, R.; Graziano, A.C.E.; Pannuzzo, G.; Alvares, E.; Cardile, V. Krabbe’s Leukodystrophy: Approaches and Models in Vitro. J. Neurosci. Res. 2016, 94, 1284–1292. [Google Scholar] [CrossRef] [PubMed]
- Ida, H.; Eto, Y.; Maekawa, K. Biochemical Pathogenesis of Demyelination in Globoid Cell Leukodystrophy (Krabbe’s Disease): The Effects of Psychosine upon Oligodendroglial Cell Culture. Acta Paediatr. Jpn. 1990, 32, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Gowrishankar, S.; Cologna, S.M.; Givogri, M.I.; Bongarzone, E.R. Deregulation of Signalling in Genetic Conditions Affecting the Lysosomal Metabolism of Cholesterol and Galactosyl-Sphingolipids. Neurobiol. Dis. 2020, 146, 105142. [Google Scholar] [CrossRef] [PubMed]
- Escolar, M.L.; West, T.; Dallavecchia, A.; Poe, M.D.; LaPoint, K. Clinical Management of Krabbe Disease. J. Neurosci. Res. 2016, 94, 1118–1125. [Google Scholar] [CrossRef]
- Pannuzzo, G.; Cardile, V.; Costantino-Ceccarini, E.; Alvares, E.; Mazzone, D.; Perciavalle, V. A Galactose-Free Diet Enriched in Soy Isoflavones and Antioxidants Results in Delayed Onset of Symptoms of Krabbe Disease in Twitcher Mice. Mol. Genet. Metab. 2010, 100, 234–240. [Google Scholar] [CrossRef]
- Paintlia, M.K.; Singh, I.; Singh, A.K. Effect of Vitamin D3 Intake on the Onset of Disease in a Murine Model of Human Krabbe Disease. J. Neurosci. Res. 2015, 93, 28–42. [Google Scholar] [CrossRef] [PubMed]
- Signorini, C.; Pannuzzo, G.; Graziano, A.C.E.; Moretti, E.; Collodel, G.; Cardile, V. Dietary Supplementation with N-3 Polyunsaturated Fatty Acids Delays the Phenotypic Manifestation of Krabbe Disease and Partially Restores Lipid Mediator Production in the Brain—Study in a Mouse Model of the Disease. Int. J. Mol. Sci. 2024, 25, 7149. [Google Scholar] [CrossRef]
- Signorini, C.; Cardile, V.; Pannuzzo, G.; Graziano, A.C.E.; Durand, T.; Galano, J.-M.; Oger, C.; Leoncini, S.; Cortelazzo, A.; Lee, J.C.-Y.; et al. Increased Isoprostanoid Levels in Brain from Murine Model of Krabbe Disease–Relevance of Isoprostanes, Dihomo-Isoprostanes and Neuroprostanes to Disease Severity. Free Radic. Biol. Med. 2019, 139, 46–54. [Google Scholar] [CrossRef]
- Berardi, A.S.; Pannuzzo, G.; Graziano, A.; Costantino-Ceccarini, E.; Piomboni, P.; Luddi, A. Pharmacological Chaperones Increase Residual β-Galactocerebrosidase Activity in Fibroblasts from Krabbe Patients. Mol. Genet. Metab. 2014, 112, 294–301. [Google Scholar] [CrossRef]
- Graziano, A.C.E.; Pannuzzo, G.; Avola, R.; Cardile, V. Chaperones as Potential Therapeutics for Krabbe Disease. J. Neurosci. Res. 2016, 94, 1220–1230. [Google Scholar] [CrossRef]
- Inoue, K. PLP1-Related Inherited Dysmyelinating Disorders: Pelizaeus-Merzbacher Disease and Spastic Paraplegia Type 2. Neurogenetics 2005, 6, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Bahrambeigi, V.; Song, X.; Sperle, K.; Beck, C.R.; Hijazi, H.; Grochowski, C.M.; Gu, S.; Seeman, P.; Woodward, K.J.; Carvalho, C.M.B.; et al. Distinct Patterns of Complex Rearrangements and a Mutational Signature of Microhomeology Are Frequently Observed in PLP1 Copy Number Gain Structural Variants. Genome Med. 2019, 11, 80. [Google Scholar] [CrossRef] [PubMed]
- Cailloux, F.; Gauthier-Barichard, F.; Mimault, C.; Isabelle, V.; Courtois, V.; Giraud, G.; Dastugue, B.; Boespflug-Tanguy, O. Genotype-Phenotype Correlation in Inherited Brain Myelination Defects Due to Proteolipid Protein Gene Mutations. Clinical European Network on Brain Dysmyelinating Disease. Eur. J. Hum. Genet. EJHG 2000, 8, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Saher, G.; Rudolphi, F.; Corthals, K.; Ruhwedel, T.; Schmidt, K.-F.; Löwel, S.; Dibaj, P.; Barrette, B.; Möbius, W.; Nave, K.-A. Therapy of Pelizaeus-Merzbacher Disease in Mice by Feeding a Cholesterol-Enriched Diet. Nat. Med. 2012, 18, 1130–1135. [Google Scholar] [CrossRef]
- Stumpf, S.K.; Berghoff, S.A.; Trevisiol, A.; Spieth, L.; Düking, T.; Schneider, L.V.; Schlaphoff, L.; Dreha-Kulaczewski, S.; Bley, A.; Burfeind, D.; et al. Ketogenic Diet Ameliorates Axonal Defects and Promotes Myelination in Pelizaeus–Merzbacher Disease. Acta Neuropathol. 2019, 138, 147–161. [Google Scholar] [CrossRef]
- Epplen, D.B.; Prukop, T.; Nientiedt, T.; Albrecht, P.; Arlt, F.A.; Stassart, R.M.; Kassmann, C.M.; Methner, A.; Nave, K.-A.; Werner, H.B.; et al. Curcumin Therapy in a Plp1 Transgenic Mouse Model of Pelizaeus-Merzbacher Disease. Ann. Clin. Transl. Neurol. 2015, 2, 787–796. [Google Scholar] [CrossRef]
- Ünalp, A.; Köse, M.; Karaoğlu, P.; Güzin, Y.; Yılmaz, Ü. A Rare Case of Hypomyelinating Leukodystrophy-14 Benefiting from Ketogenic Diet Therapy. Turk. J. Pediatr. 2022, 64, 747–753. [Google Scholar] [CrossRef]
- Murofushi, Y.; Hayakawa, I.; Abe, Y.; Ohto, T.; Murayama, K.; Suzuki, H.; Takenouchi, T.; Kosaki, K.; Kubota, M. Ketogenic Diet for KARS-Related Mitochondrial Dysfunction and Progressive Leukodystrophy. Neuropediatrics 2021, 53, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Pavone, P.; Polizzi, A.; Marino, S.D.; Corsello, G.; Falsaperla, R.; Marino, S.; Ruggieri, M. West Syndrome: A Comprehensive Review. Neurol. Sci. 2020, 41, 3547–3562. [Google Scholar] [CrossRef]
- Kim, H.J.; Yang, D.; Kim, S.H.; Kim, B.; Kim, H.D.; Lee, J.S.; Choi, J.R.; Lee, S.-T.; Kang, H.-C. The Phenotype and Treatment of SCN2A-Related Developmental and Epileptic Encephalopathy. Epileptic Disord. 2020, 22, 563–570. [Google Scholar] [CrossRef]
- Anwar, A.; Saleem, S.; Patel, U.K.; Arumaithurai, K.; Malik, P. Dravet Syndrome: An Overview. Cureus 2019, 11, e5006. [Google Scholar] [CrossRef] [PubMed]
- Strzelczyk, A.; Schubert-Bast, S. Expanding the Treatment Landscape for Lennox-Gastaut Syndrome: Current and Future Strategies. CNS Drugs 2021, 35, 61–83. [Google Scholar] [CrossRef] [PubMed]
- Zuberi, S.M.; Wirrell, E.; Yozawitz, E.; Wilmshurst, J.M.; Specchio, N.; Riney, K.; Pressler, R.; Auvin, S.; Samia, P.; Hirsch, E.; et al. ILAE Classification and Definition of Epilepsy Syndromes with Onset in Neonates and Infants: Position Statement by the ILAE Task Force on Nosology and Definitions. Epilepsia 2022, 63, 1349–1397. [Google Scholar] [CrossRef] [PubMed]
- Ramantani, G.; Bölsterli, B.K.; Alber, M.; Klepper, J.; Korinthenberg, R.; Kurlemann, G.; Tibussek, D.; Wolff, M.; Schmitt, B. Treatment of Infantile Spasm Syndrome: Update from the Interdisciplinary Guideline Committee Coordinated by the German-Speaking Society of Neuropediatrics. Neuropediatrics 2022, 53, 389–401. [Google Scholar] [CrossRef]
- Neal, E.G.; Chaffe, H.; Schwartz, R.H.; Lawson, M.S.; Edwards, N.; Fitzsimmons, G.; Whitney, A.; Cross, J.H. The Ketogenic Diet for the Treatment of Childhood Epilepsy: A Randomised Controlled Trial. Lancet Neurol. 2008, 7, 500–506. [Google Scholar] [CrossRef]
- Caraballo, R.; Vaccarezza, M.; Cersósimo, R.; Rios, V.; Soraru, A.; Arroyo, H.; Agosta, G.; Escobal, N.; Demartini, M.; Maxit, C.; et al. Long-Term Follow-up of the Ketogenic Diet for Refractory Epilepsy: Multicenter Argentinean Experience in 216 Pediatric Patients. Seizure 2011, 20, 640–645. [Google Scholar] [CrossRef]
- Sharma, S.; Sankhyan, N.; Gulati, S.; Agarwala, A. Use of the Modified Atkins Diet in Infantile Spasms Refractory to First-Line Treatment. Seizure 2012, 21, 45–48. [Google Scholar] [CrossRef]
- Ko, A.; Jung, D.E.; Kim, S.H.; Kang, H.-C.; Lee, J.S.; Lee, S.T.; Choi, J.R.; Kim, H.D. The Efficacy of Ketogenic Diet for Specific Genetic Mutation in Developmental and Epileptic Encephalopathy. Front. Neurol. 2018, 9, 530. [Google Scholar] [CrossRef] [PubMed]
- Møller, R.S.; Dahl, H.A.; Helbig, I. The Contribution of next Generation Sequencing to Epilepsy Genetics. Expert Rev. Mol. Diagn. 2015, 15, 1531–1538. [Google Scholar] [CrossRef]
- Griffin, A.; Hamling, K.R.; Hong, S.; Anvar, M.; Lee, L.P.; Baraban, S.C. Preclinical Animal Models for Dravet Syndrome: Seizure Phenotypes, Comorbidities and Drug Screening. Front. Pharmacol. 2018, 9, 573. [Google Scholar] [CrossRef]
- Dutton, S.B.B.; Sawyer, N.T.; Kalume, F.; Jumbo-Lucioni, P.; Borges, K.; Catterall, W.A.; Escayg, A. Protective Effect of the Ketogenic Diet in Scn1a Mutant Mice. Epilepsia 2011, 52, 2050–2056. [Google Scholar] [CrossRef] [PubMed]
- Jancovski, N.; Baldwin, T.; Orford, M.; Li, M.; Jones, G.D.; Burbano, L.E.; Rutherford, T.; Reid, C.; Heales, S.; Eaton, S.; et al. Protective Effects of Medium Chain Triglyceride Diet in a Mouse Model of Dravet Syndrome. Epilepsia 2021, 62, 3131–3142. [Google Scholar] [CrossRef] [PubMed]
- Miljanovic, N.; Potschka, H. The Impact of Scn1a Deficiency and Ketogenic Diet on the Intestinal Microbiome: A Study in a Genetic Dravet Mouse Model. Epilepsy Res. 2021, 178, 106826. [Google Scholar] [CrossRef]
- Mu, C.; Choudhary, A.; Mayengbam, S.; Barrett, K.T.; Rho, J.M.; Shearer, J.; Scantlebury, M.H. Seizure Modulation by the Gut Microbiota and Tryptophan-Kynurenine Metabolism in an Animal Model of Infantile Spasms. EBioMedicine 2022, 76, 103833. [Google Scholar] [CrossRef]
- Maa, E.; Figi, P. The Case for Medical Marijuana in Epilepsy. Epilepsia 2014, 55, 783–786. [Google Scholar] [CrossRef]
- Porter, B.E.; Jacobson, C. Report of a Parent Survey of Cannabidiol-Enriched Cannabis Use in Pediatric Treatment-Resistant Epilepsy. Epilepsy Behav. 2013, 29, 574–577. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, J.S.; Stella, N.; Catterall, W.A.; Westenbroek, R.E. Cannabidiol Attenuates Seizures and Social Deficits in a Mouse Model of Dravet Syndrome. Proc. Natl. Acad. Sci. USA 2017, 114, 11229–11234. [Google Scholar] [CrossRef]
- Thiele, E.A.; Marsh, E.D.; French, J.A.; Mazurkiewicz-Beldzinska, M.; Benbadis, S.R.; Joshi, C.; Lyons, P.D.; Taylor, A.; Roberts, C.; Sommerville, K.; et al. Cannabidiol in Patients with Seizures Associated with Lennox-Gastaut Syndrome (GWPCARE4): A Randomised, Double-Blind, Placebo-Controlled Phase 3 Trial. Lancet 2018, 391, 1085–1096. [Google Scholar] [CrossRef]
- Devinsky, O.; Cross, J.H.; Laux, L.; Marsh, E.; Miller, I.; Nabbout, R.; Scheffer, I.E.; Thiele, E.A.; Wright, S. Trial of Cannabidiol for Drug-Resistant Seizures in the Dravet Syndrome. N. Engl. J. Med. 2017, 376, 2011–2020. [Google Scholar] [CrossRef]
- Filla, A.; De Michele, G.; Cavalcanti, F.; Pianese, L.; Monticelli, A.; Campanella, G.; Cocozza, S. The Relationship between Trinucleotide (GAA) Repeat Length and Clinical Features in Friedreich Ataxia. Am. J. Hum. Genet. 1996, 59, 554–560. [Google Scholar]
- Tai, G.; Corben, L.A.; Yiu, E.M.; Milne, S.C.; Delatycki, M.B. Progress in the Treatment of Friedreich Ataxia. Neurol. Neurochir. Pol. 2018, 52, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Voullaire, L.; Sandi, C.; Pook, M.A.; Ioannou, P.A.; Delatycki, M.B.; Sarsero, J.P. Pharmacological Screening Using an FXN-EGFP Cellular Genomic Reporter Assay for the Therapy of Friedreich Ataxia. PLoS ONE 2013, 8, e55940. [Google Scholar] [CrossRef] [PubMed]
- Yiu, E.M.; Tai, G.; Peverill, R.E.; Lee, K.J.; Croft, K.D.; Mori, T.A.; Scheiber-Mojdehkar, B.; Sturm, B.; Praschberger, M.; Vogel, A.P.; et al. An Open-Label Trial in Friedreich Ataxia Suggests Clinical Benefit with High-Dose Resveratrol, without Effect on Frataxin Levels. J. Neurol. 2015, 262, 1344–1353. [Google Scholar] [CrossRef] [PubMed]
- Hadjivassiliou, M.; Zis, P.; Sanders, D.S.; Hoggard, N.; Sarrigiannis, P.G. Stiff Person Syndrome and Gluten Sensitivity. Nutrients 2021, 13, 1373. [Google Scholar] [CrossRef] [PubMed]
- Hadjivassiliou, M. Gluten Ataxia in Perspective: Epidemiology, Genetic Susceptibility and Clinical Characteristics. Brain 2003, 126, 685–691. [Google Scholar] [CrossRef]
- Yadav, S.K.; Ir, R.; Jeewon, R.; Doble, M.; Hyde, K.D.; Kaliappan, I.; Jeyaraman, R.; Reddi, R.N.; Krishnan, J.; Li, M.; et al. A Mechanistic Review on Medicinal Mushrooms-Derived Bioactive Compounds: Potential Mycotherapy Candidates for Alleviating Neurological Disorders. Planta Med. 2020, 86, 1161–1175. [Google Scholar] [CrossRef]
- Kluger, B.; Triolo, P.; Jones, W.; Jankovic, J. The Therapeutic Potential of Cannabinoids for Movement Disorders. Mov. Disord. 2015, 30, 313–327. [Google Scholar] [CrossRef]
- Gómez-Ruiz, M.; Rodríguez-Cueto, C.; Luna-Piñel, E.; Hernández-Gálvez, M.; Fernández-Ruiz, J. Endocannabinoid System in Spinocerebellar Ataxia Type-3 and Other Autosomal-Dominant Cerebellar Ataxias: Potential Role in Pathogenesis and Expected Relevance as Neuroprotective Targets. Front. Mol. Neurosci. 2019, 12, 94. [Google Scholar] [CrossRef]
- Stephens, G.J. Does Modulation of the Endocannabinoid System Have Potential Therapeutic Utility in Cerebellar Ataxia? J. Physiol. 2016, 594, 4631–4641. [Google Scholar] [CrossRef]
- Rodríguez-Cueto, C.; Benito, C.; Fernández-Ruiz, J.; Romero, J.; Hernández-Gálvez, M.; Gómez-Ruiz, M. Changes in CB(1) and CB(2) Receptors in the Post-Mortem Cerebellum of Humans Affected by Spinocerebellar Ataxias. Br. J. Pharmacol. 2014, 171, 1472–1489. [Google Scholar] [CrossRef]
- Rodríguez-Cueto, C.; Hernández-Gálvez, M.; Hillard, C.J.; Maciel, P.; García-García, L.; Valdeolivas, S.; Pozo, M.A.; Ramos, J.A.; Gómez-Ruiz, M.; Fernández-Ruiz, J. Dysregulation of the Endocannabinoid Signaling System in the Cerebellum and Brainstem in a Transgenic Mouse Model of Spinocerebellar Ataxia Type-3. Neuroscience 2016, 339, 191–209. [Google Scholar] [CrossRef] [PubMed]
- Ranjbar, H.; Soti, M.; Janahmadi, M.; Kohlmeier, K.A.; Sheibani, V.; Ahmadi-Zeidabadi, M.; Shabani, M. Modulation of the CB1 Cannabinoid Receptor Has Potential Therapeutic Utility in the 3-Acetylpyridine Cerebellar Ataxia Rat Model. Exp. Brain Res. 2022, 240, 2339–2348. [Google Scholar] [CrossRef] [PubMed]
- Louis, D.N.; Perry, A.; Wesseling, P.; Brat, D.J.; Cree, I.A.; Figarella-Branger, D.; Hawkins, C.; Ng, H.K.; Pfister, S.M.; Reifenberger, G.; et al. The 2021 WHO Classification of Tumors of the Central Nervous System: A Summary. Neuro-Oncology 2021, 23, 1231–1251. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Liu, Y.; Kyritsis, A.P.; Bondy, M.L. Molecular Epidemiology of Primary Brain Tumors. Neurotherapeutics 2009, 6, 427–435. [Google Scholar] [CrossRef]
- Archer, T.C.; Mahoney, E.L.; Pomeroy, S.L. Medulloblastoma: Molecular Classification-Based Personal Therapeutics. Neurotherapeutics 2017, 14, 265–273. [Google Scholar] [CrossRef]
- Cavalheiro, S.; Valsechi, L.C.; Dastoli, P.A.; Nicácio, J.M.; Cappellano, A.M.; Saba da Silva, N.; Silva da Costa, M.D. Outcomes and surgical approaches for pineal region tumors in children: 30 years’ experience. J. Neurosurg. Pediatr. 2023, 32, 184–193. [Google Scholar] [CrossRef]
- Ogiwara, H.; Dipatri, A.J.; Alden, T.D.; Bowman, R.M.; Tomita, T. Choroid Plexus Tumors in Pediatric Patients. Br. J. Neurosurg. 2012, 26, 32–37. [Google Scholar] [CrossRef]
- Viaene, A.N.; Santi, M.; Hawkins, C. Pediatric Glial Tumors. Pediatr. Dev. Pathol. 2022, 25, 46–58. [Google Scholar] [CrossRef]
- Bielecka, J.; Markiewicz-Żukowska, R. The Influence of Nutritional and Lifestyle Factors on Glioma Incidence. Nutrients 2020, 12, 1812. [Google Scholar] [CrossRef]
- Heydari, M.; Shayanfar, M.; Sharifi, G.; Saneei, P.; Sadeghi, O.; Esmaillzadeh, A. The Association between Dietary Total Antioxidant Capacity and Glioma in Adults. Nutr. Cancer 2021, 73, 1947–1956. [Google Scholar] [CrossRef]
- Tedeschi-Blok, N.; Lee, M.; Sison, J.D.; Miike, R.; Wrensch, M. Inverse Association of Antioxidant and Phytoestrogen Nutrient Intake with Adult Glioma in the San Francisco Bay Area: A Case-Control Study. BMC Cancer 2006, 6, 148. [Google Scholar] [CrossRef] [PubMed]
- Dubrow, R.; Darefsky, A.S.; Park, Y.; Mayne, S.T.; Moore, S.C.; Kilfoy, B.; Cross, A.J.; Sinha, R.; Hollenbeck, A.R.; Schatzkin, A.; et al. Dietary Components Related to N-Nitroso Compound Formation: A Prospective Study of Adult Glioma. Cancer Epidemiol Biomarkers Prev. 2010, 19, 1709–1722. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; La Vecchia, C.; Negri, E.; Chatenoud, L.; Bosetti, C.; Jia, X.; Liu, R.; Huang, G.; Bi, D.; Wang, C. Diet and Brain Cancer in Adults: A Case-Control Study in Northeast China. Int. J. Cancer 1999, 81, 20–23. [Google Scholar] [CrossRef]
- Ni, Y.-J.; Huang, Y.-Q.; Yu, L.; Zhang, X.-Y.; Zhu, Q.; Shu, L.; Zhang, L. Associations between Dietary Antioxidant Vitamins and Risk of Glioma: An Updated Systematic Review and Meta-Analysis of Observational Studies. Front. Nutr. 2024, 11, 1428528. [Google Scholar] [CrossRef]
- Zhou, S.; Wang, X.; Tan, Y.; Qiu, L.; Fang, H.; Li, W. Association between Vitamin C Intake and Glioma Risk: Evidence from a Meta-Analysis. Neuroepidemiology 2015, 44, 39–44. [Google Scholar] [CrossRef]
- Lv, W.; Zhong, X.; Xu, L.; Han, W. Association between Dietary Vitamin A Intake and the Risk of Glioma: Evidence from a Meta-Analysis. Nutrients 2015, 7, 8897–8904. [Google Scholar] [CrossRef]
- LIANG, C.; YANG, L.; GUO, S. All-Trans Retinoic Acid Inhibits Migration, Invasion and Proliferation, and Promotes Apoptosis in Glioma Cells in Vitro. Oncol. Lett. 2015, 9, 2833–2838. [Google Scholar] [CrossRef]
- Bouterfa, H.; Picht, T.; Keß, D.; Herbold, C.; Noll, E.; Black, P.M.; Roosen, K.; Tonn, J.C. Retinoids Inhibit Human Glioma Cell Proliferation and Migration in Primary Cell Cultures But Not in Established Cell Lines. Neurosurgery 2000, 46, 419. [Google Scholar] [CrossRef] [PubMed]
- Naidu, K.A.; Tang, J.L.; Naidu, K.A.; Prockop, L.D.; Nicosia, S.V.; Coppola, D. Antiproliferative and Apoptotic Effect of Ascorbyl Stearate in Human Glioblastoma Multiforme Cells: Modulation of Insulin-like Growth Factor-I Receptor (IGF-IR) Expression. J. Neurooncol. 2001, 54, 15–22. [Google Scholar] [CrossRef]
- Dal Bello, S.; Valdemarin, F.; Martinuzzi, D.; Filippi, F.; Gigli, G.L.; Valente, M. Ketogenic Diet in the Treatment of Gliomas and Glioblastomas. Nutrients 2022, 14, 3851. [Google Scholar] [CrossRef]
- Clontz, A.D. Ketogenic Therapies for Glioblastoma: Understanding the Limitations in Transitioning from Mice to Patients. Front. Nutr. 2023, 10, 1110291. [Google Scholar] [CrossRef] [PubMed]
- Poff, A.; Koutnik, A.P.; Egan, K.M.; Sahebjam, S.; D’Agostino, D.; Kumar, N.B. Targeting the Warburg Effect for Cancer Treatment: Ketogenic Diets for Management of Glioma. Semin. Cancer Biol. 2019, 56, 135–148. [Google Scholar] [CrossRef] [PubMed]
- Abdelwahab, M.G.; Fenton, K.E.; Preul, M.C.; Rho, J.M.; Lynch, A.; Stafford, P.; Scheck, A.C. The Ketogenic Diet Is an Effective Adjuvant to Radiation Therapy for the Treatment of Malignant Glioma. PLoS ONE 2012, 7, e36197. [Google Scholar] [CrossRef]
- Stafford, P.; Abdelwahab, M.G.; Kim, D.Y.; Preul, M.C.; Rho, J.M.; Scheck, A.C. The Ketogenic Diet Reverses Gene Expression Patterns and Reduces Reactive Oxygen Species Levels When Used as an Adjuvant Therapy for Glioma. Nutr. Metab. 2010, 7, 74. [Google Scholar] [CrossRef]
- Sargaço, B.; Oliveira, P.A.; Antunes, M.L.; Moreira, A.C. Effects of the Ketogenic Diet in the Treatment of Gliomas: A Systematic Review. Nutrients 2022, 14, 1007. [Google Scholar] [CrossRef]
- Schreck, K.C.; Hsu, F.-C.; Berrington, A.; Henry-Barron, B.; Vizthum, D.; Blair, L.; Kossoff, E.H.; Easter, L.; Whitlow, C.T.; Barker, P.B.; et al. Feasibility and Biological Activity of a Ketogenic/Intermittent-Fasting Diet in Patients with Glioma. Neurology 2021, 97, e953–e963. [Google Scholar] [CrossRef]
- Martin-McGill, K.J.; Marson, A.G.; Tudur Smith, C.; Jenkinson, M.D. Ketogenic Diets as an Adjuvant Therapy in Glioblastoma (the KEATING Trial): Study Protocol for a Randomised Pilot Study. Pilot Feasibility Stud. 2017, 3, 67. [Google Scholar] [CrossRef] [PubMed]
- Klein, P.; Tyrlikova, I.; Zuccoli, G.; Tyrlik, A.; Maroon, J.C. Treatment of Glioblastoma Multiforme with “Classic” 4:1 Ketogenic Diet Total Meal Replacement. Cancer Metab. 2020, 8, 24. [Google Scholar] [CrossRef]
- Rieger, J.; Bähr, O.; Maurer, G.D.; Hattingen, E.; Franz, K.; Brucker, D.; Walenta, S.; Kämmerer, U.; Coy, J.F.; Weller, M.; et al. ERGO: A Pilot Study of Ketogenic Diet in Recurrent Glioblastoma. Int. J. Oncol. 2014, 44, 1843–1852. [Google Scholar] [CrossRef]
- Voss, M.; Wagner, M.; von Mettenheim, N.; Harter, P.N.; Wenger, K.J.; Franz, K.; Bojunga, J.; Vetter, M.; Gerlach, R.; Glatzel, M.; et al. ERGO2: A Prospective, Randomized Trial of Calorie-Restricted Ketogenic Diet and Fasting in Addition to Reirradiation for Malignant Glioma. Int. J. Radiat. Oncol. Biol. Phys. 2020, 108, 987–995. [Google Scholar] [CrossRef]
- Frebourg, T.; Barbier, N.; Yan, Y.X.; Garber, J.E.; Dreyfus, M.; Fraumeni, J.; Li, F.P.; Friend, S.H. Germ-Line P53 Mutations in 15 Families with Li-Fraumeni Syndrome. Am. J. Hum. Genet. 1995, 56, 608–615. [Google Scholar] [PubMed]
- Lombardi, C.; Ganguly, A.; Bunin, G.R.; Azary, S.; Alfonso, V.; Ritz, B.; Heck, J.E. Maternal Diet during Pregnancy and Unilateral Retinoblastoma. Cancer Causes Control 2015, 26, 387–397. [Google Scholar] [CrossRef] [PubMed]
- Pogoda, J.M.; Preston-Martin, S.; Howe, G.; Lubin, F.; Mueller, B.A.; Holly, E.A.; Filippini, G.; Peris-Bonet, R.; McCredie, M.R.E.; Cordier, S.; et al. An International Case-Control Study of Maternal Diet during Pregnancy and Childhood Brain Tumor Risk: A Histology-Specific Analysis by Food Group. Ann. Epidemiol. 2009, 19, 148–160. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Ye, J.; Shi, S.; Luo, C.; Wang, T.; Liu, Y.; Ye, J.; Sun, X.; Ke, Y.; Hou, C. Maternal Smoking, Consumption of Alcohol, and Caffeinated Beverages during Pregnancy and the Risk of Childhood Brain Tumors: A Meta-Analysis of Observational Studies. BMC Public Health 2024, 24, 1238. [Google Scholar] [CrossRef]
| Nutritional Interventions Krabbe Disease | ||
|---|---|---|
| Nutrients or Neuro-Nutraceutical Substance | Effects | |
| Nutrient supplementation | Vitamin D3 1 | Delay symptoms onset [220] |
| n-3 polyunsaturated fatty acids 1 | Slow the phenotypic presentation [221] | |
| Soy isoflavones and antioxidants (coenzyme Q10, glutathione and isoflavonoids 1 | Delay symptoms onset [219] | |
| 3′,4′,7-Trihydroxyisoflavone 2 | Pharmacological chaperone [223,224] | |
| Type of diet | Effects | |
| Dietary modification | Galactose-free diet 1 | Delay symptoms onset [219] |
| Clinical Trials for Ketogenic Diet in Gliomas | ||
|---|---|---|
| Status | Clinical Trial ID/Name | Results |
| Withdrawn | NCT05373381 The KetoGlioma (Ketogenic Glioma) Study | Study is on hold indefinitely due to funding issues |
| Unknown status | NCT03278249 Feasibility Study of Modified Atkins Ketogenic Diet in the Treatment of Newly Diagnosed Malignant Glioma | |
| NCT02939378 Ketogenic Diet Adjunctive to Salvage Chemotherapy for Recurrent Glioblastoma: a Pilot Study | ||
| Terminated | NCT02046187 Ketogenic Diet with Radiation and Chemotherapy for Newly Diagnosed Glioblastoma | Excessive protocol deviations due to strict nature of diet requirements |
| Completed | NCT02286167 Glioma Modified Atkins-based Diet in Patients with Glioblastoma | Production of ketonuria and significant systemic and cerebral metabolic changes in participants [290] |
| NCT03075514 Ketogenic Diets as an Adjuvant Therapy in Glioblastoma | No posted results, only a linked paper with trial description [291] | |
| NCT02302235 Ketogenic Diet Treatment Adjunctive to Radiation and Chemotherapy in Glioblastoma Multiforme: a Pilot Study NCT01865162 Ketogenic Diet as Adjunctive Treatment in Refractory/End-stage Glioblastoma Multiforme: a Pilot Study (KGDinGBM) | Diet was well tolerated. The small sample size limits efficacy conclusions [292]. | |
| NCT00575146 Ketogenic Diet for Recurrent Glioblastoma | Diet was feasible and safe but probably has no significant clinical activity when used as single agent in recurrent glioma [293]. | |
| NCT01754350 Calorie-restricted, Ketogenic Diet and Transient Fasting During Reirradiation for Patients With Recurrent Glioblastoma | Diet was feasible and effective in inducing ketosis in heavily pretreated patients with recurrent glioma, but failed to increase the efficacy of reirradiation [294]. | |
| Recruiting | NCT05708352 A Phase 2 Study of the Ketogenic Diet vs. Standard Anti-cancer Diet Guidance for Patients With Glioblastoma in Combination With Standard-of-care Treatment | |
| NCT04691960 A Pilot Study of Ketogenic Diet and Metformin in Glioblastoma: Feasibility and Metabolic Imaging | ||
| NCT05564949 A Ketogenic Diet as a Complementary Treatment on Patients With High-grade Gliomas and Brain Metastases | ||
| NCT05183204 Paxalisib With a High Fat, Low Carb Diet and Metformin for Glioblastoma | ||
| NCT04730869 Metabolic Therapy Program In Conjunction With Standard Treatment For Glioblastoma | ||
| Active, not recruiting | NCT03451799 Ketogenic Diet in Combination With Standard-of-care Radiation and Temozolomide for Patients With Glioblastoma | |
| NCT01535911 Pilot Study of a Metabolic Nutritional Therapy for the Management of Primary Brain Tumors | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Briglia, M.; Allia, F.; Avola, R.; Signorini, C.; Cardile, V.; Romano, G.L.; Giurdanella, G.; Malaguarnera, R.; Bellomo, M.; Graziano, A.C.E. Diet and Nutrients in Rare Neurological Disorders: Biological, Biochemical, and Pathophysiological Evidence. Nutrients 2024, 16, 3114. https://doi.org/10.3390/nu16183114
Briglia M, Allia F, Avola R, Signorini C, Cardile V, Romano GL, Giurdanella G, Malaguarnera R, Bellomo M, Graziano ACE. Diet and Nutrients in Rare Neurological Disorders: Biological, Biochemical, and Pathophysiological Evidence. Nutrients. 2024; 16(18):3114. https://doi.org/10.3390/nu16183114
Chicago/Turabian StyleBriglia, Marilena, Fabio Allia, Rosanna Avola, Cinzia Signorini, Venera Cardile, Giovanni Luca Romano, Giovanni Giurdanella, Roberta Malaguarnera, Maria Bellomo, and Adriana Carol Eleonora Graziano. 2024. "Diet and Nutrients in Rare Neurological Disorders: Biological, Biochemical, and Pathophysiological Evidence" Nutrients 16, no. 18: 3114. https://doi.org/10.3390/nu16183114
APA StyleBriglia, M., Allia, F., Avola, R., Signorini, C., Cardile, V., Romano, G. L., Giurdanella, G., Malaguarnera, R., Bellomo, M., & Graziano, A. C. E. (2024). Diet and Nutrients in Rare Neurological Disorders: Biological, Biochemical, and Pathophysiological Evidence. Nutrients, 16(18), 3114. https://doi.org/10.3390/nu16183114










