Association between Dietary Patterns and Cardiometabolic Multimorbidity among Chinese Rural Older Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Assessment of CMM
2.3. Dietary Assessment
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Characteristics of Study Participants
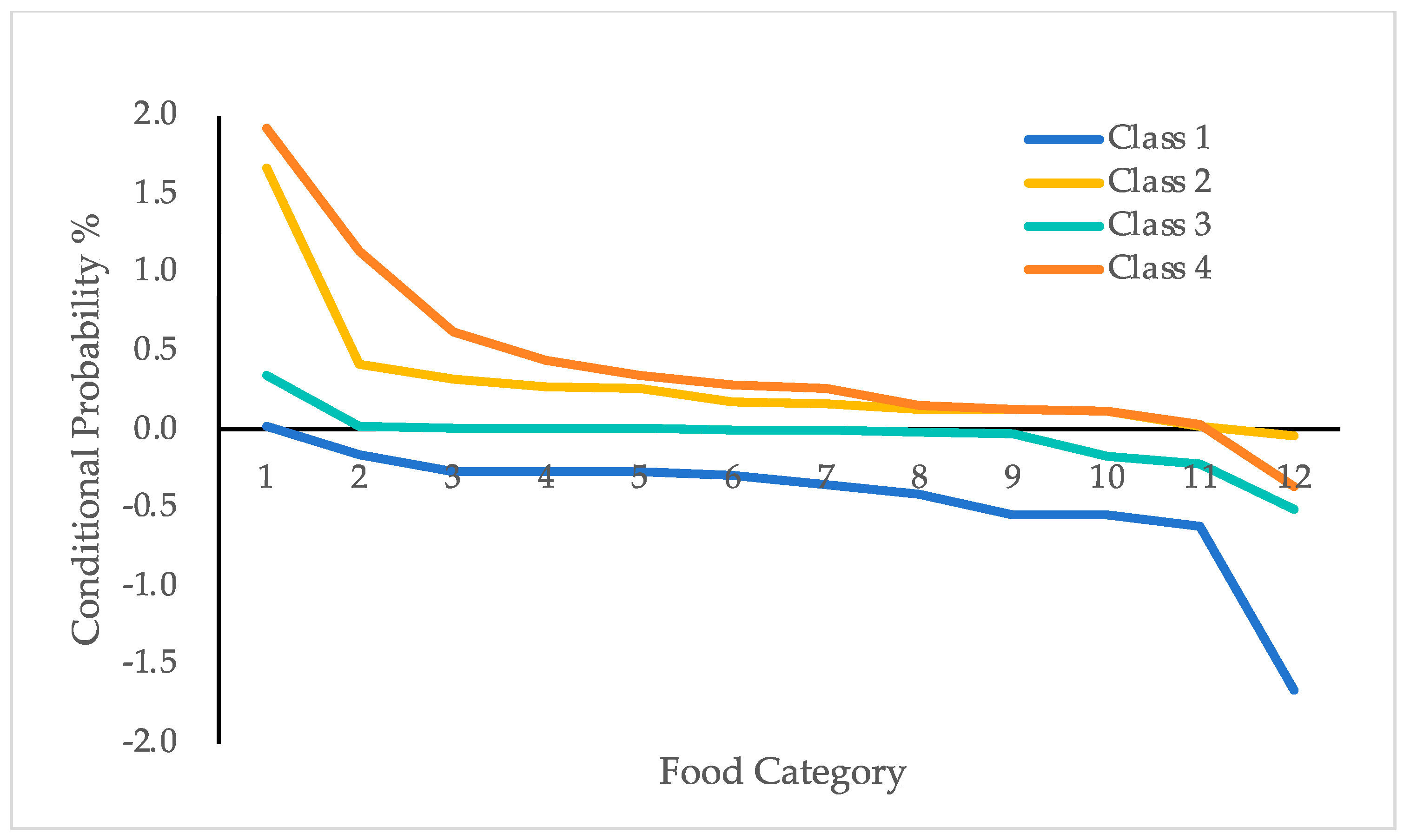
3.2. Latent Profile Analysis Dietary Patterns
3.3. Prevalence of CMM by Dietary Patterns
3.4. Association between Dietary Patterns and the Prevalence of CMM among Rarul Older Adults
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Whitty, C.J.M.; MacEwen, C.; Goddard, A.; Alderson, D.; Marshall, M.; Calderwood, C.; Atherton, F.; McBride, M.; Atherton, J.; Stokes-Lampard, H.; et al. Rising to the challenge of multimorbidity. BMJ 2020, 368, l6964. [Google Scholar] [CrossRef] [PubMed]
- Bodenheimer, T.; Lorig, K.; Holman, H.; Grumbach, K. Patient self-management of chronic disease in primary care. JAMA 2002, 288, 2469–2475. [Google Scholar] [CrossRef] [PubMed]
- Di Angelantonio, E.; Kaptoge, S.; Wormser, D.; Willeit, P.; Butterworth, A.S.; Bansal, N.; O’Keeffe, L.M.; Gao, P.; Wood, A.M.; Burgess, S.; et al. Association of Cardiometabolic Multimorbidity With Mortality. JAMA 2015, 314, 52–60. [Google Scholar] [CrossRef]
- Canoy, D.; Tran, J.; Zottoli, M.; Ramakrishnan, R.; Hassaine, A.; Rao, S.; Li, Y.; Salimi-Khorshidi, G.; Norton, R.; Rahimi, K. Association between cardiometabolic disease multimorbidity and all-cause mortality in 2 million women and men registered in UK general practices. BMC Med. 2021, 19, 258. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.T.; Luo, Y.; Han, L.; Wang, K.; Yao, S.S.; Su, H.X.; Chen, S.; Cao, G.Y.; De Fries, C.M.; Chen, Z.S.; et al. Patterns of cardiometabolic multimorbidity and the risk of depressive symptoms in a longitudinal cohort of middle-aged and older Chinese. J. Affect. Disord. 2022, 301, 1–7. [Google Scholar] [CrossRef]
- Xiao, L.X.; Wang, Z.Y.; Li, J.T.; Wang, H.M.; Hao, Y.M.; Zhou, P.; Huang, Y.L.; Deng, Q.J.; Hao, Y.C.; Yang, N.; et al. Association of cardiometabolic multimorbidity with all-cause and cardiovascular disease mortality among Chinese hypertensive patients. J. Geriatr. Cardiol. 2024, 21, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.T.; Sun, Z.J.; Lyu, J.; Li, L.M. progress in research on the association between lifestyle and cardiometabolic comorbidities. Chin. J. Control Prev. 2021, 25, 266–270. (In Chinese) [Google Scholar]
- Macmahon, S. Multimorbidity: A Priority for Global Health Research; The Academy of Medical Sciences: London, UK, 2018. [Google Scholar]
- Fan, J.; Sun, Z.; Yu, C.; Guo, Y.; Pei, P.; Yang, L.; Chen, Y.; Du, H.; Sun, D.; Pang, Y.; et al. Multimorbidity patterns and association with mortality in 0.5 million Chinese adults. Chin. Med. J. 2022, 135, 648–657. [Google Scholar] [CrossRef]
- Dove, A.; Guo, J.; Marseglia, A.; Fastbom, J.; Vetrano, D.L.; Fratiglioni, L.; Pedersen, N.L.; Xu, W. Cardiometabolic multimorbidity and incident dementia: The Swedish twin registry. Eur. Heart J. 2023, 44, 573–582. [Google Scholar] [CrossRef]
- Lu, Z.; Ntlapo, N.; Tilly, M.J.; Geurts, S.; Aribas, E.; Ikram, M.K.; de Groot, N.M.S.; Kavousi, M. Burden of cardiometabolic disorders and lifetime risk of new-onset atrial fibrillation among men and women: The Rotterdam Study. Eur. J. Prev. Cardiol. 2024, 31, 1141–1149. [Google Scholar] [CrossRef]
- Imaiso, J. Significant Differences in Elderly Health between Urban and Rural Communities: A Literature Review. Health 2019, 11, 567–577. [Google Scholar] [CrossRef]
- Liu, B.P.; Zhu, J.H.; Wan, L.P.; Zhao, Z.Y.; Wang, X.; Jia, C.X. The Impact of Physical Activity Intensity on the Dynamic Progression of Cardiometabolic Multimorbidity: Prospective Cohort Study Using UK Biobank Data. JMIR Public Health Surveill. 2023, 9, e46991. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Zhang, S.; Zeng, P.; Wang, T. Influence of social deprivation on morbidity and all-cause mortality of cardiometabolic multi-morbidity: A cohort analysis of the UK Biobank cohort. BMC Public Health 2023, 23, 2177. [Google Scholar] [CrossRef] [PubMed]
- DeSalvo, K.B.; Olson, R.; Casavale, K.O. Dietary Guidelines for Americans. JAMA 2016, 315, 457–458. [Google Scholar] [CrossRef] [PubMed]
- Harrison, S.; Couture, P.; Lamarche, B. Diet Quality, Saturated Fat and Metabolic Syndrome. Nutrients 2020, 12, 3232. [Google Scholar] [CrossRef] [PubMed]
- Farvid, M.S.; Sidahmed, E.; Spence, N.D.; Mante Angua, K.; Rosner, B.A.; Barnett, J.B. Consumption of red meat and processed meat and cancer incidence: A systematic review and meta-analysis of prospective studies. Eur. J. Epidemiol. 2021, 36, 937–951. [Google Scholar] [CrossRef]
- Qin, A.; Wang, M.; Xu, L. Increased Intake of Vegetables and Fruits Improves Cognitive Function among Chinese Oldest Old: 10-Year Follow-Up Study. Nutrients 2023, 15, 2147. [Google Scholar] [CrossRef]
- Cavallo, D.N.; Horino, M.; McCarthy, W.J. Adult Intake of Minimally Processed Fruits and Vegetables: Associations with Cardiometabolic Disease Risk Factors. J. Acad. Nutr. Diet. 2016, 116, 1387–1394. [Google Scholar] [CrossRef]
- Pei, Z.; Zhang, J.; Qin, W.; Hu, F.; Zhao, Y.; Zhang, X.; Cong, X.; Liu, C.; Xu, L. Association between Dietary Patterns and Depression in Chinese Older Adults: A Longitudinal Study Based on CLHLS. Nutrients 2022, 14, 5230. [Google Scholar] [CrossRef]
- Chen, Y.C.; Jung, C.C.; Chen, J.H.; Chiou, J.M.; Chen, T.F.; Chen, Y.F.; Tang, S.C.; Yeh, S.J.; Lee, M.S. Association of Dietary Patterns With Global and Domain-Specific Cognitive Decline in Chinese Elderly. J. Am. Geriatr. Soc. 2017, 65, 1159–1167. [Google Scholar] [CrossRef]
- World Health Organization. Draft action plan for the prevention and control of noncommunicable diseases 2013–2020. In WHO Global NCD Action Plan 2013–2020; World Health Organization: Geneva Switzerland, 2013. [Google Scholar]
- Vasto, S.; Scapagnini, G.; Rizzo, C.; Monastero, R.; Marchese, A.; Caruso, C. Mediterranean diet and longevity in Sicily: Survey in a Sicani Mountains population. Rejuvenation Res. 2012, 15, 184–188. [Google Scholar] [CrossRef]
- Mente, A.; Dehghan, M.; Rangarajan, S.; O’Donnell, M.; Hu, W.; Dagenais, G.; Wielgosz, A.; Lear, S.A.; Wei, L.; Diaz, R.; et al. Diet, cardiovascular disease, and mortality in 80 countries. Eur. Heart J. 2023, 44, 2560–2579. [Google Scholar] [CrossRef] [PubMed]
- Kopelman, P.G. Obesity as a medical problem. Nature 2000, 404, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Kivimäki, M.; Kuosma, E.; Ferrie, J.E.; Luukkonen, R.; Nyberg, S.T.; Alfredsson, L.; Batty, G.D.; Brunner, E.J.; Fransson, E.; Goldberg, M.; et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: Pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health 2017, 2, e277–e285. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, Q.; Hao, W.; Zhu, D. Long-Term Food Variety and Dietary Patterns Are Associated with Frailty among Chinese Older Adults: A Cohort Study Based on CLHLS from 2014 to 2018. Nutrients 2022, 14, 4279. [Google Scholar] [CrossRef] [PubMed]
- Ford, T.; Lipson, J.; Miller, L. Spiritually grounded character: A latent profile analysis. Front. Psychol. 2022, 13, 1061416. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Liang, J.; Hong, C.; Liang, R.; Luo, Y. Cardiometabolic multimorbidity, lifestyle behaviours, and cognitive function: A multicohort study. Lancet Healthy Longev. 2023, 4, e265–e273. [Google Scholar] [CrossRef]
- Chen, W.; Wang, X.; Chen, J.; You, C.; Ma, L.; Zhang, W.; Li, D. Household air pollution, adherence to a healthy lifestyle, and risk of cardiometabolic multimorbidity: Results from the China health and retirement longitudinal study. Sci. Total Environ. 2023, 855, 158896. [Google Scholar] [CrossRef]
- Zhang, J.; Sun, Y. Meta-analysis of the prevalence and influencing factors of cardiovascular metabolic comorbidity in middle-aged and elderly. Chin. J. Geriatr. Care 2023, 21, 9–15. (In Chinese) [Google Scholar]
- Qin, X.; Chen, C.; Wang, J.; Cai, A.; Feng, X.; Jiang, X.; Feng, Y. Association of adiposity indices with cardiometabolic multimorbidity among 101,973 chinese adults: A cross-sectional study. BMC Cardiovasc. Disord. 2023, 23, 514. [Google Scholar] [CrossRef] [PubMed]
- Guo, D.; Ding, R.X.; He, P. Prevalence and influencing factors of cardiometabolic multmorbidity in Chinese elderly. Chin. J. Prev. Contr. Chron. Dis. 2023, 31, 101–105. (In Chinese) [Google Scholar]
- Zhao, Y.; Zhang, H.; Liu, X.; Desloge, A.; Wang, Q.; Zhao, S.; Song, L.; Tzoulaki, I. The prevalence of cardiometabolic multimorbidity and its associations with health outcomes among women in China. Front. Cardiovasc. Med. 2023, 10, 922932. [Google Scholar] [CrossRef]
- Kim, J.; Baek, Y.; Jeong, K.; Lee, S. Association of Dietary Factors With Grip Strength, Body Fat, and Prevalence of Sarcopenic Obesity in Rural Korean Elderly With Cardiometabolic Multimorbidity. Front. Nutr. 2022, 9, 910481. [Google Scholar] [CrossRef] [PubMed]
- Amirkalali, B.; Fakhrzadeh, H.; Sharifi, F.; Kelishadi, R.; Zamani, F.; Asayesh, H.; Safiri, S.; Samavat, T.; Qorbani, M. Prevalence of Metabolic Syndrome and Its Components in the Iranian Adult Population: A Systematic Review and Meta-Analysis. Iran Red Crescent. Med. J. 2015, 17, e24723. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, M.; Bhuket, T.; Torres, S.; Liu, B.; Wong, R.J. Prevalence of the metabolic syndrome in the United States, 2003-2012. JAMA 2015, 313, 1973–1974. [Google Scholar] [CrossRef]
- Sakakibara, B.M.; Obembe, A.O.; Eng, J.J. The prevalence of cardiometabolic multimorbidity and its association with physical activity, diet, and stress in Canada: Evidence from a population-based cross-sectional study. BMC Public Health 2019, 19, 1361. [Google Scholar] [CrossRef]
- Satija, A.; Bhupathiraju, S.N.; Rimm, E.B.; Spiegelman, D.; Chiuve, S.E.; Borgi, L.; Willett, W.C.; Manson, J.E.; Sun, Q.; Hu, F.B. Plant-Based Dietary Patterns and Incidence of Type 2 Diabetes in US Men and Women: Results from Three Prospective Cohort Studies. PLoS Med. 2016, 13, e1002039. [Google Scholar] [CrossRef]
- Liu, R.H. Health-promoting components of fruits and vegetables in the diet. Adv. Nutr. 2013, 4, 384s–392s. [Google Scholar] [CrossRef]
- Yahia, E.M. Contribution of Fruits and Vegetables to Human Nutrition and Health. In Postharvest Physiology and Biochemistry of Fruits and Vegetables; Elsevier: Amsterdam, The Netherlands, 2019; pp. 19–45. [Google Scholar]
- Han, Y.; Hu, Y.; Yu, C.; Guo, Y.; Pei, P.; Yang, L.; Chen, Y.; Du, H.; Sun, D.; Pang, Y.; et al. Lifestyle, cardiometabolic disease, and multimorbidity in a prospective Chinese study. Eur. Heart J. 2021, 42, 3374–3384. [Google Scholar] [CrossRef]
- Dhalwani, N.N.; Zaccardi, F.; O’Donovan, G.; Carter, P.; Hamer, M.; Yates, T.; Davies, M.; Khunti, K. Association Between Lifestyle Factors and the Incidence of Multimorbidity in an Older English Population. J. Gerontol. A Biol. Sci. Med. Sci. 2017, 72, 528–534. [Google Scholar] [CrossRef]
- Ruel, G.; Shi, Z.; Zhen, S.; Zuo, H.; Kröger, E.; Sirois, C.; Lévesque, J.F.; Taylor, A.W. Association between nutrition and the evolution of multimorbidity: The importance of fruits and vegetables and whole grain products. Clin. Nutr. 2014, 33, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Veldheer, S.; Tuan, W.J.; Al-Shaar, L.; Wadsworth, M.; Sinoway, L.; Schmitz, K.H.; Sciamanna, C.; Gao, X. Gardening Is Associated With Better Cardiovascular Health Status Among Older Adults in the United States: Analysis of the 2019 Behavioral Risk Factor Surveillance System Survey. J. Acad. Nutr. Diet 2023, 123, 761–769.e3. [Google Scholar] [CrossRef] [PubMed]
- Guasch-Ferré, M.; Willett, W.C. The Mediterranean diet and health: A comprehensive overview. J. Intern. Med. 2021, 290, 549–566. [Google Scholar] [CrossRef]
- Blesso, C.N. Egg phospholipids and cardiovascular health. Nutrients 2015, 7, 2731–2747. [Google Scholar] [CrossRef]
- Becerra-Tomás, N.; Babio, N.; Martínez-González, M.; Corella, D.; Estruch, R.; Ros, E.; Fitó, M.; Serra-Majem, L.; Salaverria, I.; Lamuela-Raventós, R.M.; et al. Replacing red meat and processed red meat for white meat, fish, legumes or eggs is associated with lower risk of incidence of metabolic syndrome. Clin. Nutr. 2016, 35, 1442–1449. [Google Scholar] [CrossRef]
- Anderson, A.L.; Harris, T.B.; Tylavsky, F.A.; Perry, S.E.; Houston, D.K.; Lee, J.S.; Kanaya, A.M.; Sahyoun, N.R. Dietary patterns, insulin sensitivity and inflammation in older adults. Eur. J. Clin. Nutr. 2012, 66, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Riccardi, G.; Giosuè, A.; Calabrese, I.; Vaccaro, O. Dietary recommendations for prevention of atherosclerosis. Cardiovasc. Res. 2022, 118, 1188–1204. [Google Scholar] [CrossRef]
- Shimazu, T.; Kuriyama, S.; Hozawa, A.; Ohmori, K.; Sato, Y.; Nakaya, N.; Nishino, Y.; Tsubono, Y.; Tsuji, I. Dietary patterns and cardiovascular disease mortality in Japan: A prospective cohort study. Int. J. Epidemiol. 2007, 36, 600–609. [Google Scholar] [CrossRef]
- Kim, Y.S.; Xun, P.; He, K. Fish consumption, long-chain omega-3 polyunsaturated fatty acid intake and risk of metabolic syndrome: A meta-analysis. Nutrients 2015, 7, 2085–2100. [Google Scholar] [CrossRef]
- Appleby, P.N.; Davey, G.K.; Key, T.J. Hypertension and blood pressure among meat eaters, fish eaters, vegetarians and vegans in EPIC-Oxford. Public Health Nutr. 2002, 5, 645–654. [Google Scholar] [CrossRef]
- Wang, L.; Manson, J.E.; Buring, J.E.; Sesso, H.D. Meat intake and the risk of hypertension in middle-aged and older women. J. Hypertens 2008, 26, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Svetkey, L.P.; Simons-Morton, D.; Vollmer, W.M.; Appel, L.J.; Conlin, P.R.; Ryan, D.H.; Ard, J.; Kennedy, B.M. Effects of dietary patterns on blood pressure: Subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Arch. Intern. Med. 1999, 159, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Dietary Guidelines Advisory Committee. USDA Nutrition Evidence Systematic Reviews. In Dietary Patterns and Risk of Cardiovascular Disease: A Systematic Review; USDA: Alexandria, VA, USA, 2020. [Google Scholar]
- Darmon, N.; Drewnowski, A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: A systematic review and analysis. Nutr. Rev. 2015, 73, 643–660. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total (n = 3331) | CMM (n = 1487) | NO-CMM (n = 1844) | t/χ2 | p |
|---|---|---|---|---|---|
| Age (years) | 70.89 (5.88) | 71.32 (5.69) | 70.54 (6.01) | −3.85 | <0.001 |
| Sex | 52.63 | <0.001 | |||
| Male | 1388 (41.67%) | 517 (37.25%) | 871 (62.75%) | ||
| Female | 1943 (58.33%) | 970 (49.92%) | 973 (50.08%) | ||
| Highest education | 14.09 | 0.003 | |||
| Illiteracy | 1452 (43.59%) | 691 (47.59%) | 761 (52.41%) | ||
| Primary School | 1127 (33.83%) | 491 (43.57%) | 636 (56.43%) | ||
| Middle school | 565 (16.96%) | 240 (42.48%) | 325 (57.52%) | ||
| High school and higher | 187 (5.61%) | 65 (34.76%) | 122 (65.24%) | ||
| Marital status | 6.21 | 0.013 | |||
| With a spouse | 2539 (23.78%) | 384 (48.48%) | 408 (51.52%) | ||
| Without a spouse | 792 (76.22%) | 1103 (43.44%) | 1436 (56.56%) | ||
| Live arrangement | 5.26 | 0.072 | |||
| Living alone | 626 (18.79%) | 302 (48.24%) | 324 (51.76%) | ||
| Living only with spouse | 2205 (66.20%) | 977 (44.31%) | 1228 (55.69%) | ||
| Living with spouse and children | 500 (15.01%) | 208 (41.60%) | 292 (58.40%) | ||
| Personal income | 33.29 | <0.001 | |||
| Q1 | 1794 (53.86%) | 880 (49.05%) | 914 (50.95%) | ||
| Q2 | 892 (26.78%) | 368 (41.26%) | 524 (58.74%) | ||
| Q3 | 645 (19.36%) | 239 (37.05%) | 406 (62.95%) | ||
| Smoking status | 30.61 | <0.001 | |||
| Smoker | 949 (28.49%) | 352 (37.09%) | 597 (62.91%) | ||
| Non-smoker | 2382 (71.51%) | 1135 (47.65%) | 1247 (52.35%) | ||
| Drinking status | 31.64 | <0.001 | |||
| Drinker | 1006 (30.20%) | 375 (37.28%) | 631 (62.72%) | ||
| Non-drinker | 2325 (69.80%) | 1112 (47.83%) | 1213 (52.17%) | ||
| Present occupation | 47.30 | <0.001 | |||
| No | 1711 (51.37%) | 862 (50.38%) | 849 (49.62%) | ||
| Farming | 1380 (41.42%) | 537 (38.91%) | 843 (61.09%) | ||
| Non-farming occupations | 240 (7.21%) | 88 (36.67%) | 152 (63.33%) | ||
| Medical insurance type | 1.60 | 0.451 | |||
| UEBMI | 87 (2.61%) | 38 (43.68%) | 49 (56.32%) | ||
| RBMI | 3189 (95.74%) | 1429 (44.81%) | 1760 (55.19%) | ||
| Others | 55 (1.65%) | 20 (36.36%) | 35 (63.64%) | ||
| Online frequency | 1.20 | 0.550 | |||
| Never | 2528 (75.89%) | 316 (42.88%) | 421 (57.12%) | ||
| 1~4 times per month | 66 (1.98%) | 30 (45.45%) | 36 (54.55%) | ||
| Every day | 737 (22.13%) | 1141 (45.13%) | 1387 (54.87%) | ||
| Obesity status | 85.71 | <0.001 | |||
| Underweight | 110 (3.30%) | 33 (30.00%) | 77 (70.00%) | ||
| Normal | 1309 (39.30%) | 485 (37.05%) | 824 (62.95%) | ||
| Overweight | 1356 (40.71%) | 646 (47.64%) | 710 (52.36%) | ||
| Obesity | 556 (16.69%) | 323 (58.09%) | 233 (41.91%) | ||
| Amount of exercise | 0.85 | 0.652 | |||
| Little | 2491 (74.78%) | 1121 (45.00%) | 1370 (55.00%) | ||
| Middle | 804 (24.14%) | 352 (43.78%) | 452 (56.22%) | ||
| Big | 36 (1.08%) | 14 (38.89%) | 22 (61.11%) |
| Class | Loglikelihood | AIC | BIC | aBIC | Entropy | LMRT (p) | BLRT (p) | Class Probability (%) |
|---|---|---|---|---|---|---|---|---|
| 1 | −56,711.82 | 113,471.64 | 113,618.31 | 113,542.05 | — | — | — | 1.00 |
| 2 | −55,772.74 | 111,619.48 | 111,845.59 | 111,728.02 | 0.61 | <0.001 | <0.001 | 0.49/0.51 |
| 3 | −54,357.39 | 108,814.78 | 109,120.33 | 108,961.46 | 0.90 | <0.001 | <0.001 | 0.23/0.59/0.18 |
| 4 | −54,008.12 | 108,142.24 | 108,527.24 | 108,327.06 | 0.88 | <0.001 | <0.001 | 0.17/0.23/0.53/0.07 |
| 5 | −53,628.85 | 107,409.71 | 107,874.15 | 107,632.66 | 0.88 | 0.007 | 0.007 | 0.20/0.02/0.62/0.07/0.09 |
| Class | n | (%) | Attribution Probability | |||
|---|---|---|---|---|---|---|
| Class 1 | Class 2 | Class 3 | Class 4 | |||
| Class 1 | 571 | 17.14 | 0.91 | 0.00 | 0.08 | 0.00 |
| Class 2 | 754 | 22.64 | 0.00 | 0.99 | 0.01 | 0.00 |
| Class 3 | 1770 | 53.14 | 0.04 | 0.01 | 0.92 | 0.03 |
| Class 4 | 236 | 7.08 | 0.01 | 0.02 | 0.10 | 0.88 |
| Variable | CMM | NO-CMM | χ2 | p |
|---|---|---|---|---|
| Class 1 | 276 (48.34%) | 295 (51.66%) | 8.37 | 0.03 |
| Class 2 | 353 (46.82%) | 401 (53.18%) | ||
| Class 3 | 764 (43.16%) | 1006 (56.84%) | ||
| Class 4 | 94 (39.83%) | 142 (60.17%) |
| Heading | Crude Model 1 | Adjusted Model 2 | ||
|---|---|---|---|---|
| OR (95%CI) | p | OR (95%CI) | p | |
| Dietary patterns | ||||
| Class 1 | Ref. | Ref. | ||
| Class 2 | 0.94 (0.76–1.17) | 0.583 | 0.87 (0.69–1.10) | 0.252 |
| Class 3 | 0.81 (0.67–0.98) | 0.031 | 0.80 (0.66–0.98) | 0.028 |
| Class 4 | 0.71 (0.52–0.96) | 0.028 | 0.70 (0.51–0.97) | 0.034 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, F.; Qin, W.; Xu, L. Association between Dietary Patterns and Cardiometabolic Multimorbidity among Chinese Rural Older Adults. Nutrients 2024, 16, 2830. https://doi.org/10.3390/nu16172830
Hu F, Qin W, Xu L. Association between Dietary Patterns and Cardiometabolic Multimorbidity among Chinese Rural Older Adults. Nutrients. 2024; 16(17):2830. https://doi.org/10.3390/nu16172830
Chicago/Turabian StyleHu, Fangfang, Wenzhe Qin, and Lingzhong Xu. 2024. "Association between Dietary Patterns and Cardiometabolic Multimorbidity among Chinese Rural Older Adults" Nutrients 16, no. 17: 2830. https://doi.org/10.3390/nu16172830
APA StyleHu, F., Qin, W., & Xu, L. (2024). Association between Dietary Patterns and Cardiometabolic Multimorbidity among Chinese Rural Older Adults. Nutrients, 16(17), 2830. https://doi.org/10.3390/nu16172830





