Food Insecurity Associated with Higher Stress, Depressive Symptoms, and Lower Diet Quality among Women Caregivers in North Carolina
Abstract
1. Introduction
2. Methods
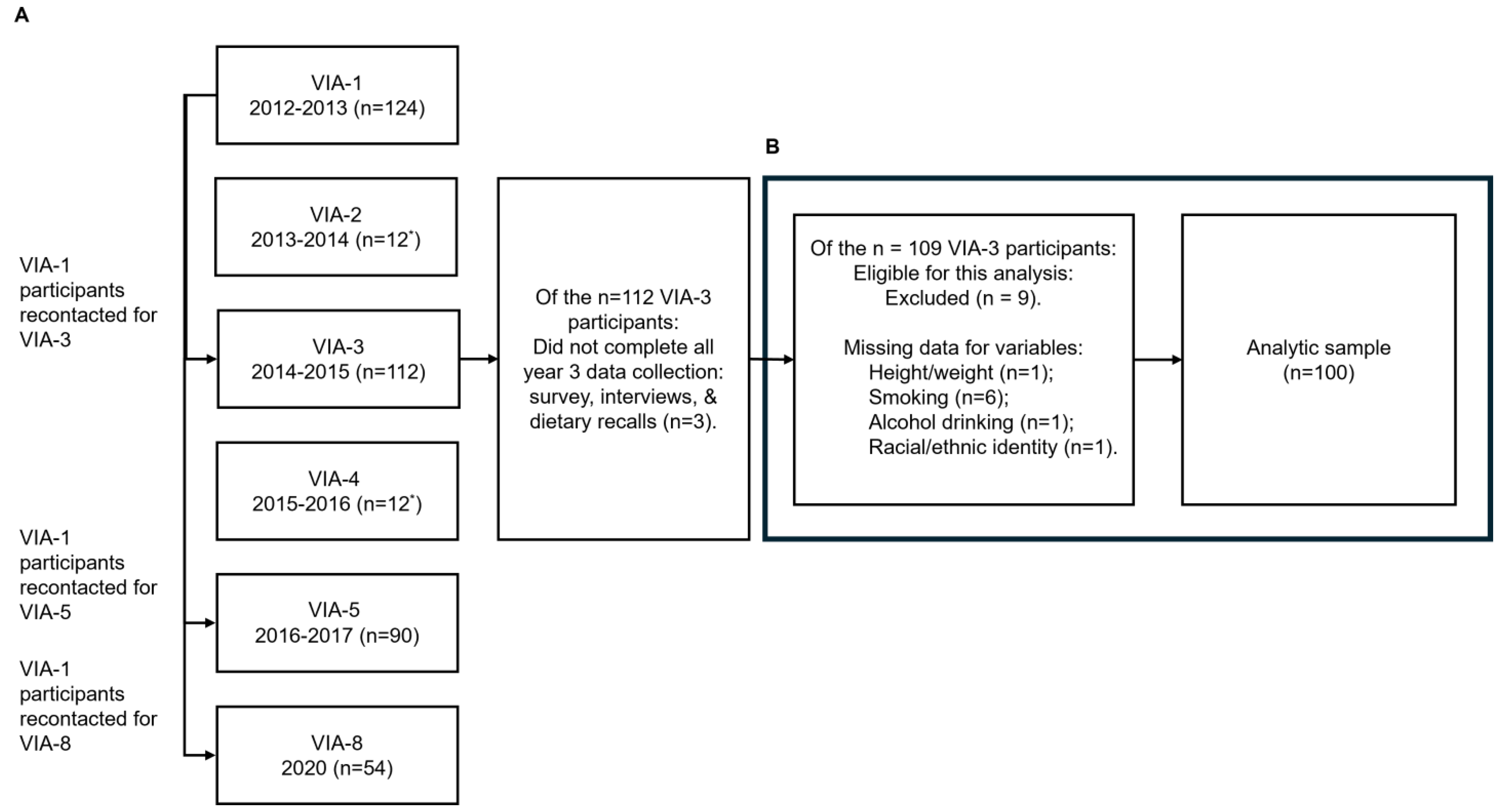
2.1. Study Design
2.2. Study Team and Training
2.3. Sample and Recruitment
2.4. Measures
2.4.1. Sociodemographic Characteristics
2.4.2. Physical Activity
2.4.3. Smoking and Alcoholic Beverage Consumption
2.4.4. Total Energy Intake and Diet Quality
2.4.5. Weight, Height, and Body Mass Index
2.4.6. Food Insecurity
2.4.7. Stress and Depression
2.5. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Associations of Food Insecurity with Perceived Stress, Depressive Symptoms
3.3. Associations of Food Insecurity with Diet Quality and Weight Status
3.4. Associations of Food Insecurity with Clinical Depression and Obesity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Economic Research Service (ERS), U.S. Department of Agriculture (USDA). Food Security in the U.S.: Measurement. ERS.USDA.gov. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/measurement/ (accessed on 28 June 2024).
- Fischer, E.P.L.T.; Reichert, A.; Alsopp, M.; Harvey, T.S. Reframing Childhood Obesity: Cultural Insights on Nutrition, Weight, and Food Systems; Vanderbilt Cultural Contexts of Health & Wellbeing Initiative: Nashville, TN, USA, 2022; p. 52. Available online: https://www.vanderbilt.edu/cultural-contexts-health/wp-content/uploads/sites/350/2022/06/Reframing-Childhood-Obesity-CCH-Report.pdf (accessed on 10 July 2024).
- Bowen, S.; Elliott, S.; Hardison-Moody, A. The structural roots of food insecurity: How racism is a fundamental cause of food insecurity. Sociol. Compass 2021, 15, e12846. [Google Scholar] [CrossRef]
- Pourmotabbed, A.; Moradi, S.; Babaei, A.; Ghavami, A.; Mohammadi, H.; Jalili, C.; Symonds, M.E.; Miraghajani, M. Food insecurity and mental health: A systematic review and meta-analysis. Public Health Nutr. 2020, 23, 1778–1790. [Google Scholar] [CrossRef]
- Johnson, C.M.; Sharkey, J.R.; Lackey, M.J.; Adair, L.S.; Aiello, A.E.; Bowen, S.K.; Fang, W.; Flax, V.L.; Ammerman, A.S. Relationship of food insecurity to women’s dietary outcomes: A systematic review. Nutr. Rev. 2018, 76, 910–928. [Google Scholar] [CrossRef] [PubMed]
- Lopes, S.O.; Abrantes, L.C.S.; Azevedo, F.M.; Morais, N.S.; Morais, D.C.; Gonçalves, V.S.S.; Fontes, E.A.F.; Franceschini, S.; Priore, S.E. Food insecurity and micronutrient deficiency in adults: A systematic review and meta-analysis. Nutrients 2023, 15, 1074. [Google Scholar] [CrossRef] [PubMed]
- Brandt, E.J.; Mozaffarian, D.; Leung, C.W.; Berkowitz, S.A.; Murthy, V.L. Diet and food and nutrition insecurity and cardiometabolic disease. Circ. Res. 2023, 132, 1692–1706. [Google Scholar] [CrossRef] [PubMed]
- Te Vazquez, J.; Feng, S.N.; Orr, C.J.; Berkowitz, S.A. Food insecurity and cardiometabolic conditions: A review of recent research. Curr. Nutr. Rep. 2021, 10, 243–254. [Google Scholar] [CrossRef] [PubMed]
- Laraia, B.A. Food insecurity and chronic disease. Adv. Nutr. 2013, 4, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Rabbitt, M.H.L.J.; Burke, M.P.; Coleman, A. Household Food Security in the United States in 2022 (ERR-325). Economic Research Service (ERS), U.S. Department of Agriculture (USDA). ERS.USDA.gov. 2023. Available online: https://www.ers.usda.gov/publications/pub-details/?pubid=107702 (accessed on 10 July 2024).
- U.S. Department of Agriculture (USDA). Priorities. Available online: https://www.usda.gov/priorities (accessed on 28 June 2024).
- Seligman, H.K.; Levi, R.; Adebiyi, V.O.; Coleman-Jensen, A.; Guthrie, J.F.; Frongillo, E.A. Assessing and monitoring nutrition security to promote healthy dietary intake and outcomes in the United States. Annu. Rev. Nutr. 2023, 43, 409–429. [Google Scholar] [CrossRef]
- Thorndike, A.N.; Gardner, C.D.; Kendrick, K.B.; Seligman, H.K.; Yaroch, A.L.; Gomes, A.V.; Ivy, K.N.; Scarmo, S.; Cotwright, C.J.; Schwartz, M.B. Strengthening U.S. food policies and programs to promote equity in nutrition security: A policy statement from the American Heart Association. Circulation 2022, 145, e1077–e1093. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Fleischhacker, S.; Andrés, J.R. Prioritizing nutrition security in the U.S. JAMA 2021, 325, 1605–1606. [Google Scholar] [CrossRef]
- Herman, D.R.; Westfall, M.; Bashir, M.; Afulani, P. Food insecurity and mental distress among WIC-eligible women in the United States: A cross-sectional study. J. Acad. Nutr. Diet 2024, 124, 65–79. [Google Scholar] [CrossRef]
- Bruening, M.; Dinour, L.M.; Chavez, J.B.R. Food insecurity and emotional health in the USA: A systematic narrative review of longitudinal research. Public Health Nutr. 2017, 20, 3200–3208. [Google Scholar] [CrossRef] [PubMed]
- Maynard, M.; Andrade, L.; Packull-McCormick, S.; Perlman, C.M.; Leos-Toro, C.; Kirkpatrick, S.I. Food insecurity and mental health among females in high-income countries. Int. J. Environ. Res. Public Health 2018, 15, 1424. [Google Scholar] [CrossRef] [PubMed]
- Myers, C.A. Food insecurity and psychological distress: A review of the recent literature. Curr. Nutr. Rep. 2020, 9, 107–118. [Google Scholar] [CrossRef]
- Wang, W.; Liu, Y.; Li, Y.; Luo, B.; Lin, Z.; Chen, K.; Liu, Y. Dietary patterns and cardiometabolic health: Clinical evidence and mechanism. MedComm 2023, 4, e212. [Google Scholar] [CrossRef]
- Thomas, M.K.; Lammert, L.J.; Beverly, E.A. Food insecurity and its impact on body weight, type 2 diabetes, cardiovascular disease, and mental health. Curr. Cardiovasc. Risk Rep. 2021, 15, 15. [Google Scholar] [CrossRef]
- Moradi, S.; Mirzababaei, A.; Dadfarma, A.; Rezaei, S.; Mohammadi, H.; Jannat, B.; Mirzaei, K. Food insecurity and adult weight abnormality risk: A systematic review and meta-analysis. Eur. J. Nutr. 2019, 58, 45–61. [Google Scholar] [CrossRef]
- Elliott, S.; Satterfield, S.; Solorzano, G.; Bowen, S.; Hardison-Moody, A.; Williams, L. Disenfranchised: How lower-income mothers navigated COVID-19 pandemic aid to put food on the table. Socius 2021, 7, 23780231211031690. [Google Scholar] [CrossRef]
- Nutrition Coordinating Center (NCC). Food Amount Reporting Booklet. Available online: https://www.ncc.umn.edu/products/support/food-amount-reporting-booklets/ (accessed on 1 May 2024).
- U.S. Centers for Disease Control and Prevention (CDC). National Health and Nutrition Examination Survey (NHANES): Anthropometry Procedures Manual. CDC.gov. Available online: https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/manuals.aspx?BeginYear=2017 (accessed on 1 May 2024).
- Leung, C.W.; Epel, E.S.; Ritchie, L.D.; Crawford, P.B.; Laraia, B.A. Food insecurity is inversely associated with diet quality of lower-income adults. J. Acad. Nutr. Diet 2014, 114, 1943–1953.e1942. [Google Scholar] [CrossRef] [PubMed]
- Stults-Kolehmainen, M.A.; Sinha, R. The effects of stress on physical activity and exercise. Sports Med. 2014, 44, 81–121. [Google Scholar] [CrossRef]
- American Heart Association. American Heart Association Recommendations for Physical Activity in Adults and Kids. Heart.org. Available online: https://www.heart.org/en/healthy-living/fitness/fitness-basics/aha-recs-for-physical-activity-in-adults (accessed on 1 June 2024).
- U.S. Department of Health and Human Services (HHS). Physical Activity Guidelines—Current Guidelines. Health.gov. Available online: https://health.gov/our-work/nutrition-physical-activity/physical-activity-guidelines/current-guidelines (accessed on 1 June 2024).
- Blackwell, A.K.M.; Lee, I.; Scollo, M.; Wakefield, M.; Munafò, M.R.; Marteau, T.M. Should cigarette pack sizes be capped? Addiction 2020, 115, 802–809. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services (HHS). CFR—Code of Federal Regulations Title 21. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=1140.16#:~:text=(1)%20Except%20as%20otherwise%20provided,the%20retailer%20and%20the%20consumer (accessed on 1 June 2024).
- U.S. Centers for Disease Control and Prevention (CDC). Alcohol Use and Your Health. Available online: https://www.cdc.gov/alcohol/about-alcohol-use/index.html (accessed on 1 June 2024).
- U.S. Centers for Disease Control and Prevention (CDC). National Health and Nutrition Examination Survey (NHANES): MEC In-Person Dietary Interviewers Procedures Manual. CDC.gov. Available online: https://www.cdc.gov/nchs/data/nhanes/2017-2018/manuals/2017_MEC_In-Person_Dietary_Interviewers_Manual.pdf (accessed on 1 May 2024).
- U.S. Centers for Disease Control and Prevention (CDC). What Counts as a Cup? CDC.gov. Available online: http://www.cdc.gov/nutrition/everyone/fruitsvegetables/cup.html (accessed on 1 May 2024).
- Guenther, P.M.; Kirkpatrick, S.I.; Reedy, J.; Krebs-Smith, S.M.; Buckman, D.W.; Dodd, K.W.; Casavale, K.O.; Carroll, R.J. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J. Nutr. 2014, 144, 399–407. [Google Scholar] [CrossRef]
- Guenther, P.M.; Casavale, K.O.; Reedy, J.; Kirkpatrick, S.I.; Hiza, H.A.; Kuczynski, K.J.; Kahle, L.L.; Krebs-Smith, S.M. Update of the healthy eating index: HEI-2010. J. Acad. Nutr. Diet 2013, 113, 569–580. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Agriculture (USDA), U.S. Department of Health and Human Services (HHS). 2010 Dietary Guidelines. Available online: https://www.dietaryguidelines.gov/about-dietary-guidelines/previous-editions/2010-dietary-guidelines (accessed on 1 May 2024).
- National Cancer Institute (NCI), D.o.C.C.P.S. Healthy Eating Index SAS Code. Available online: https://epi.grants.cancer.gov/hei/sas-code.html (accessed on 28 June 2024).
- Ludwig, D.A.; Landy, D.C.; Kurtz, J.M.; Miller, T.L. Using SAS to Expand the Application of Standard Measures and Guide Statistical Explorations: Creating Healthy Eating Index Scores Using Nutrition Data System for Research Output. In Proceedings of the SAS Global Forum 2013, Seattle, WA, USA, 20–22 June 2013; p. 12. [Google Scholar]
- Miller, P.E.; Mitchell, D.C.; Harala, P.L.; Pettit, J.M.; Smiciklas-Wright, H.; Hartman, T.J. Development and evaluation of a method for calculating the Healthy Eating Index-2005 using the Nutrition Data System for Research. Public Health Nutr. 2011, 14, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Nutrition Coordinating Center (NCC). Guide to Creating Variables Needed to Calculate Scores for Each Component of the Health Eating Index-2010. Available online: https://www.ncc.umn.edu/ncc-news/ncc-news-fall-2014/#firstarticle (accessed on 1 May 2024).
- U.S. Centers for Disease Control and Prevention (CDC). About Adult BMI. Available online: https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html (accessed on 1 May 2024).
- Economic Research Service (ERS), U.S. Department of Agriculture (USDA). Survey Tools: U.S. Adult Food Security Survey Module. ERS.USDA.gov. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/survey-tools/#adult (accessed on 28 June 2024).
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Cohen, S. Perceived stress in a probability sample of the United States. In The Social Psychology of Health; Oskamp, S.S.S., Ed.; Sage Publications: Thousand Oaks, CA, USA, 1988; pp. 31–67. [Google Scholar]
- Medvedev, O.N.; Krägeloh, C.U.; Siegert, R.J.; Singh, N.N. (Eds.) Handbook of Assessment in Mindfulness Research; Springer: Berlin/Heidelberg, Germany, 2022. [Google Scholar]
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- CESD-R The Center for Epidemiologic Studies Depression Scale Revised. Available online: https://cesd-r.com/ (accessed on 1 June 2024).
- Eaton, W.W.; Muntaner, C.; Smith, C.; Tien, A.; Ybarra, M.; Maruish, M.E. Center for Epidemiologic Studies Depression Scale: Review and revision (CESD and CESD-R). In The Use of Psychological Testing for Treatment Planning and Outcomes Assessment, 3rd ed.; Maruish, M., Ed.; Lawrence Erlbaum: Mahwah, NJ, USA, 2004; pp. 363–377. [Google Scholar]
- Loh, I.H.; Oddo, V.M.; Otten, J. Food insecurity is associated with depression among a vulnerable workforce: Early care and education workers. Int. J. Environ. Res. Public Health 2020, 18, 170. [Google Scholar] [CrossRef]
- Butler, L.; Popkin, B.M.; Poti, J.M. Associations of alcoholic beverage consumption with dietary intake, waist circumference, and body mass index in US adults: National Health and Nutrition Examination Survey 2003–2012. J. Acad. Nutr. Diet 2018, 118, 409–420.e403. [Google Scholar] [CrossRef]
- Butler, J.L.; Gordon-Larsen, P.; Steffen, L.M.; Shikany, J.M.; Jacobs, D.R., Jr.; Popkin, B.M.; Poti, J.M. Associations of 5-year changes in alcoholic beverage intake with 5-year changes in waist circumference and BMI in the Coronary Artery Risk Development in Young Adults (CARDIA) study. PLoS ONE 2023, 18, e0281722. [Google Scholar] [CrossRef] [PubMed]
- Alvidrez, J.; Castille, D.; Laude-Sharp, M.; Rosario, A.; Tabor, D. The National Institute on Minority Health and Health Disparities Research Framework. Am. J. Public Health 2019, 109, S16–S20. [Google Scholar] [CrossRef] [PubMed]
- Golovaty, I.; Tien, P.C.; Price, J.C.; Sheira, L.; Seligman, H.; Weiser, S.D. Food insecurity may be an independent risk factor associated with nonalcoholic fatty liver disease among low-income adults in the United States. J. Nutr. 2020, 150, 91–98. [Google Scholar] [CrossRef]
- Chiu, D.T.; Parker, J.E.; Wiley, C.R.; Epel, E.S.; Laraia, B.A.; Leung, C.W.; Tomiyama, A.J. Food insecurity, poor diet, and metabolic measures: The roles of stress and cortisol. Appetite 2024, 197, 107294. [Google Scholar] [CrossRef]
- Wiss, D.A.; Brewerton, T.D. Adverse childhood experiences and adult obesity: A systematic review of plausible mechanisms and meta-analysis of cross-sectional studies. Physiol Behav. 2020, 223, 112964. [Google Scholar] [CrossRef]
- Arenas, D.J.; Thomas, A.; Wang, J.; DeLisser, H.M. A systematic review and meta-analysis of depression, anxiety, and sleep disorders in US adults with food insecurity. J. Gen. Intern. Med. 2019, 34, 2874–2882. [Google Scholar] [CrossRef]
- Sidebottom, A.C.; Hellerstedt, W.L.; Harrison, P.A.; Hennrikus, D. An examination of prenatal and postpartum depressive symptoms among women served by urban community health centers. Arch. Women’s Ment. Health 2014, 17, 27–40. [Google Scholar] [CrossRef]
- Breland, J.Y.; Donalson, R.; Dinh, J.V.; Maguen, S. Trauma exposure and disordered eating: A qualitative study. Women Health 2018, 58, 160–174. [Google Scholar] [CrossRef]
- Kaiser, B.; Gemesi, K.; Holzmann, S.L.; Wintergerst, M.; Lurz, M.; Hauner, H.; Groh, G.; Böhm, M.; Krcmar, H.; Holzapfel, C.; et al. Stress-induced hyperphagia: Empirical characterization of stress-overeaters. BMC Public Health 2022, 22, 100. [Google Scholar] [CrossRef]
- Hill, D.; Conner, M.; Clancy, F.; Moss, R.; Wilding, S.; Bristow, M.; O’Connor, D.B. Stress and eating behaviours in healthy adults: A systematic review and meta-analysis. Health Psychol. Rev. 2021, 16, 280–304. [Google Scholar] [CrossRef]
- Pan, L.; Sherry, B.; Njai, R.; Blanck, H.M. Food insecurity is associated with obesity among US adults in 12 states. J. Acad. Nutr. Diet 2012, 112, 1403–1409. [Google Scholar] [CrossRef]
- Dhurandhar, E.J. The food-insecurity obesity paradox: A resource scarcity hypothesis. Physiol Behav. 2016, 162, 88–92. [Google Scholar] [CrossRef]
- Leung, C.W.; Williams, D.R.; Villamor, E. Very low food security predicts obesity predominantly in California Hispanic men and women. Public Health Nutr. 2012, 15, 2228–2236. [Google Scholar] [CrossRef][Green Version]
- Brostow, D.P.; Gunzburger, E.; Abbate, L.M.; Brenner, L.A.; Thomas, K.S. Mental illness, not obesity status, is associated with food insecurity among the elderly in the Health and Retirement Study. J. Nutr. Gerontol. Geriatr. 2019, 38, 149–172. [Google Scholar] [CrossRef]
- Gaines-Turner, T.; Simmons, J.C.; Chilton, M. Recommendations from SNAP participants to improve wages and end stigma. Am. J. Public Health 2019, 109, 1664–1667. [Google Scholar] [CrossRef]
- Turan, J.M.; Elafros, M.A.; Logie, C.H.; Banik, S.; Turan, B.; Crockett, K.B.; Pescosolido, B.; Murray, S.M. Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Med. 2019, 17, 7. [Google Scholar] [CrossRef]
- Stangl, A.L.; Earnshaw, V.A.; Logie, C.H.; Van Brakel, W.C.; Simbayi, L.; Barré, I.; Dovidio, J.F. The Health Stigma and Discrimination Framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019, 17, 31. [Google Scholar] [CrossRef]
- Barnidge, E.K.; Stenmark, S.H.; DeBor, M.; Seligman, H.K. The right to food: Building upon “food is medicine”. Am. J. Prev. Med. 2020, 59, 611–614. [Google Scholar] [CrossRef]
- Chilton, M.; Rose, D. A rights-based approach to food insecurity in the United States. Am. J. Public Health 2009, 99, 1203–1211. [Google Scholar] [CrossRef]
- Eder, M.; Henninger, M.; Durbin, S.; Iacocca, M.O.; Martin, A.; Gottlieb, L.M.; Lin, J.S. Screening and interventions for social risk factors: Technical brief to support the US Preventive Services Task Force. JAMA 2021, 326, 1416–1428. [Google Scholar] [CrossRef]
- Knifton, L.; Inglis, G. Poverty and mental health: Policy, practice and research implications. BJPsych Bull. 2020, 44, 193–196. [Google Scholar] [CrossRef]
- Phojanakong, P.; Welles, S.; Dugan, J.; Booshehri, L.; Brown Weida, E.; Chilton, M. Trauma-informed financial empowerment programming improves food security among families with young children. J. Nutr. Educ. Behav. 2020, 52, 465–473. [Google Scholar] [CrossRef]
- Bowen, S.; Hardison-Moody, A. Improving unequal food access requires understanding and addressing the social inequalities that contribute to it. Am. J. Public Health 2023, 113, 353–355. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total | Participants Experiencing Food Security | Participants Experiencing Food Insecurity | p |
|---|---|---|---|---|
| n (%) | 100 (100%) | 58 (58%) | 42 (42%) | 0.1082 |
| Age, years (mean ± SD) | 36.9 ± 9.8 | 35.4 ± 9.3 | 39.1 ± 10.1 | 0.0612 |
| Race or Ethnicity [N (%)] | 0.007 | |||
| White | 33 (33%) | 12 (20.7%) | 21 (50%) j | |
| Black/African American | 42 (42%) | 30 (51.7%) | 12 (28.6%) | |
| Latina/Hispanic | 25 (25%) | 16 (27.6%) | 9 (21.4%) | |
| Birthplace [N (%)] | 0.544 | |||
| U.S. | 78 (78%) | 44 (75.9%) | 34 (81%) | |
| Outside of U.S. | 22 (22%) | 14 (24.1%) | 8 (19.1%) | |
| Education [N (%)] | 0.426 | |||
| <High school | 31 (31%) | 15 (25.9%) | 16 (38.1%) | |
| High school | 29 (29%) | 18 (31%) | 11 (26.2%) | |
| >Highschool | 40 (40%) | 25 (43.1%) | 15 (35.7%) | |
| Physical Activity [N (%)] b | 0.791 | |||
| None | 60 (60%) | 16 (27.6%) | 28.6%) | |
| 1–4 days/week | 23 (23%) | 23 (39.7%) | 14 (33.3%) | |
| ≥5 days/week | 17 (17%) | 19 (32.8%) | 16 (38.1%) | |
| Smoking [N (%)] c | 0.198 | |||
| None | 61 (61%) | 35 (60.3%) | 25 (59.5%) | |
| <10 cigarettes/day | 18 (18%) | 16 (27.6%) | 7 (16.7%) | |
| ≥10 cigarettes/day | 21 (21%) | 7 (12.1%) | 10 (23.8%) | |
| Alcohol [N (%)] d | 0.957 | |||
| None | 17 (17%) | 35 (60.3%) | 26 (61.9%) | |
| ≤1 drink/day | 25 (25%) | 11 (19%) | 7 (16.7%) | |
| >1 drink/day | 58 (58%) | 12 (20.7%) | 9 (21.4%) | |
| Total Energy Intake, kcal/day (mean ± SD) e | 1755.3 ± 531.4 | 1726.9 ± 475.8 | 1794.9 ± 467 | 0.5286 |
| Diet quality (mean ± SD) f | 51.2 ± 17.4 | 54.4 ± 17.3 | 46.8 ± 16.7 | 0.0307 |
| BMI, kg/m2 (mean ± SD) g | 33.4 ± 8.8 | 33.1 ± 8.8 | 33.7 ± 8.8 | 0.7457 |
| BMI Category kg/m2 [N (%)] | 0.973 | |||
| 18.5 to 24.9 | 17 (17%) | 10 (17.2%) | 7 (16.7%) | |
| 25.0 to 29.9 | 25 (25%) | 14 (24.1%) | 11 (26.2%) | |
| ≥30.0 | 58 (58%) | 34 (58.6%) | 24 (57.1%) | |
| Depressive Symptoms (mean ± SD) h | 19.1 ± 7.0 | 17.8 ± 5.8 | 21 ± 8.2 | 0.0243 |
| Depression [N (%)] h | 0.973 | |||
| No clinical depression | 33 (33%) | 21 (36.2%) | 12 (28.6%) | |
| Clinically significant depression | 67 (67%) | 37 (63.8%) | 30 (71.4%) | |
| Stress (mean ± SD) i | 15.2 ± 8.0 | 12.3 ± 7.4 | 19.2 ± 7.2 | 0.0000 |
| FSSM Affirmative Responses (mean ± SD) | 2.5 ± 2.5 | 0.62 ± 0.77 | 5.07 ± 1.76 | 0.0000 |
| Unadjusted | Model 1 b | |||||
|---|---|---|---|---|---|---|
| A: Stress | β | 95% CI | Beta | β | 95% CI | Beta |
| Food Secure | Ref | Ref | ||||
| Food Insecure | 6.90 | 3.96, 9.84 | 0.43 | 7.51 | 4.19, 10.84 | 0.46 |
| Unadjusted | Model 1 b | |||||
| B: Depressive Symptoms | β | 95% CI | Beta | β | 95% CI | Beta |
| Food Secure | Ref | Ref | ||||
| Food Insecure | 3.18 | 0.27, 6.09 | 0.23 | 3.55 | 0.54, 6.56 | 0.25 |
| Unadjusted | Model 1 b | Model 2 c | |||||||
|---|---|---|---|---|---|---|---|---|---|
| A: Diet Quality | β | 95% CI | Beta | β | 95% CI | Beta | β | 95% CI | Beta |
| Food secure | Ref | Ref | |||||||
| Food insecure | −7.58 | −14.45, −0.72 | −0.22 | −8.96 | −14.66, −3.27 | −0.26 | −9.70 | −16.06, −3.34 | −0.28 |
| Unadjusted | Model 3 d | Model 4 e | |||||||
| B: Weight Status | β | 95% CI | Beta | β | 95% CI | Beta | β | 95% CI | Beta |
| Food secure | Ref | Ref | Ref | ||||||
| Food insecure | 0.58 | −2.95, 4.11 | 0.03 | 0.07 | −3.78, 3.91 | 0.00 | −0.27 | −4.59, 4.05 | −0.02 |
| Unadjusted | Model 1 b | Model 2 c | ||||
|---|---|---|---|---|---|---|
| A: Clinical Depression | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Food Secure | 1.00 | 1.00 | 1.00 | |||
| Food Insecure | 1.42 | 0.60, 3.36 | 1.42 | 0.50, 4.01 | 0.42 | 0.11, 1.65 |
| Unadjusted | Model 3 d | Model 4 e | ||||
| B: Obesity | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Food Secure | 1.00 | 1.00 | 1.00 | |||
| Food Insecure | 0.94 | 0.42, 2.11 | 0.73 | 0.26, 2.05 | 0.67 | 0.22, 2.07 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Butler, J.L.; Johnson, C.M.; Hardison-Moody, A.; Bowen, S.K. Food Insecurity Associated with Higher Stress, Depressive Symptoms, and Lower Diet Quality among Women Caregivers in North Carolina. Nutrients 2024, 16, 2491. https://doi.org/10.3390/nu16152491
Butler JL, Johnson CM, Hardison-Moody A, Bowen SK. Food Insecurity Associated with Higher Stress, Depressive Symptoms, and Lower Diet Quality among Women Caregivers in North Carolina. Nutrients. 2024; 16(15):2491. https://doi.org/10.3390/nu16152491
Chicago/Turabian StyleButler, J. Lauren, Cassandra M. Johnson, Annie Hardison-Moody, and Sarah K. Bowen. 2024. "Food Insecurity Associated with Higher Stress, Depressive Symptoms, and Lower Diet Quality among Women Caregivers in North Carolina" Nutrients 16, no. 15: 2491. https://doi.org/10.3390/nu16152491
APA StyleButler, J. L., Johnson, C. M., Hardison-Moody, A., & Bowen, S. K. (2024). Food Insecurity Associated with Higher Stress, Depressive Symptoms, and Lower Diet Quality among Women Caregivers in North Carolina. Nutrients, 16(15), 2491. https://doi.org/10.3390/nu16152491







