Psychological Effects of Nasogastric Tube (NGT) in Patients with Anorexia Nervosa: A Systematic Review
Abstract
1. Introduction
- Severe Malnutrition and Weight Loss: When patients present with severe malnutrition or have lost a significant amount of weight (typically more than 15–20% of their body weight), nutritional support through an NGT may be necessary to prevent further health deterioration and to stabilize the patient’s condition. This is especially critical when oral intake is insufficient to meet the caloric and nutritional needs required for recovery.
- Failure of Oral Refeeding: If patients are non-compliant with dietary therapy or oral refeeding plans, an NGT can ensure that they receive the necessary nutrients. This approach helps in overcoming the resistance to eating commonly observed in AN, thereby facilitating weight gain and nutritional rehabilitation.
- Critical Clinical Condition: In cases where patients are in a life-threatening condition due to complications such as electrolyte imbalances, cardiovascular instability, or severe organ dysfunction, immediate nutritional intervention via NGT is crucial to support vital functions and initiate the recovery process.
2. Review Methodology
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
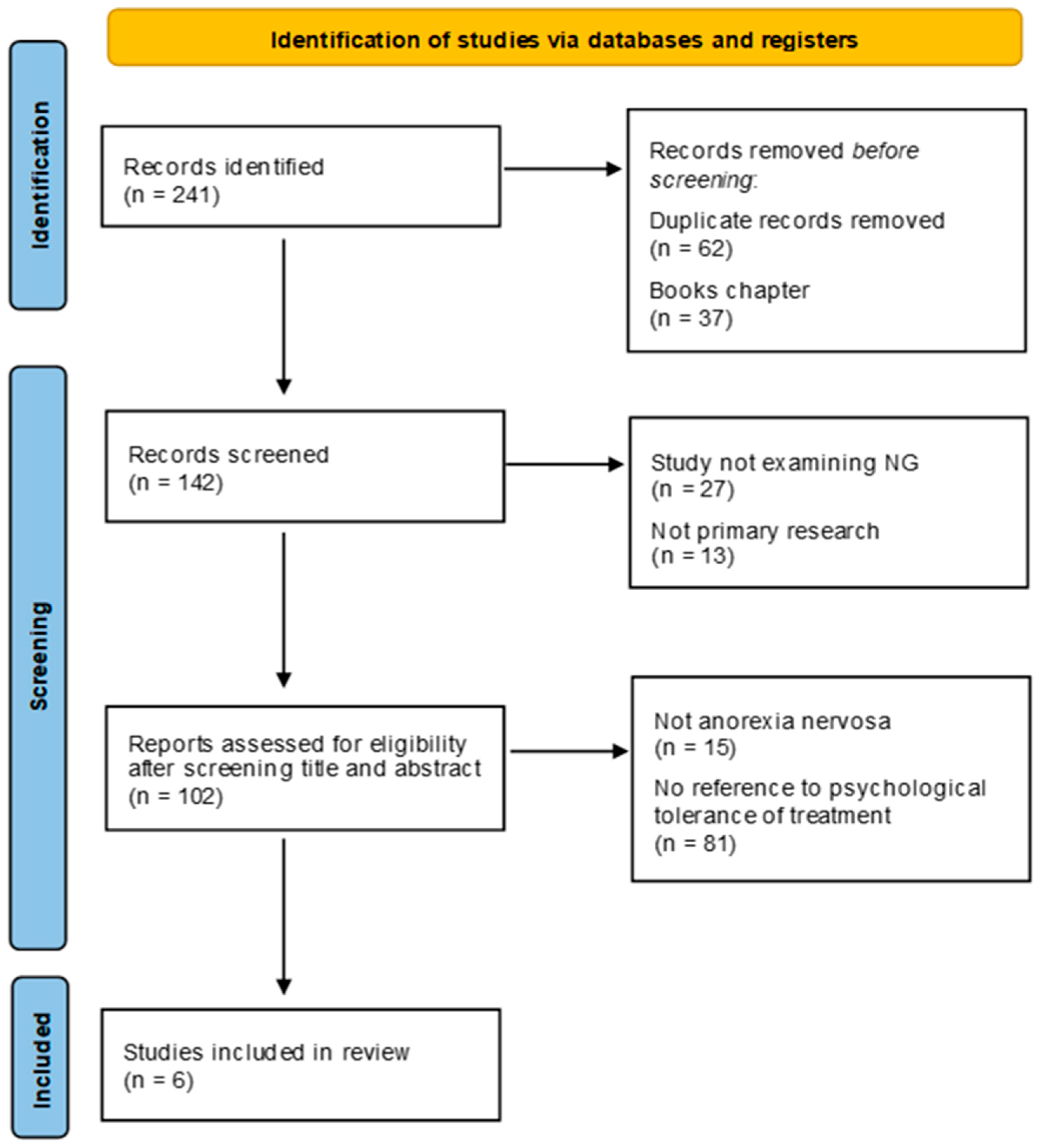
2.3. Study Selection
2.4. Data Extraction
2.5. Quality Assessment
3. Results
3.1. Analytic Description of the Studies
3.2. General Comments on the Studies
3.3. Quality of Studies
4. Discussion
4.1. Study Characteristics
4.2. NGT Tolerability
4.3. NGT Treatment Steps
4.4. Others’ Points of View: Parents and Medical Staff
4.5. Recommendations for Further Research
4.6. Limits of the Study
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Hudson, J.I.; Hiripi, E.; Pope, H.G., Jr.; Kessler, R.C. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol. Psychiatry 2007, 61, 348–358. [Google Scholar] [CrossRef]
- Arcelus, J.; Mitchell, A.J.; Wales, J.; Nielsen, S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch. Gen. Psychiatry 2011, 68, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Agostino, H.; Burstein, B.; Moubayed, D.; Taddeo, D.; Grady, R.; Vyver, E.; Dimitropoulos, G.; Dominic, A.; Coelho, J.S. Trends in the Incidence of New-Onset Anorexia Nervosa and Atypical Anorexia Nervosa among Youth During the COVID-19 Pandemic in Canada. JAMA Netw. Open 2021, 4, e2137395. [Google Scholar] [CrossRef] [PubMed]
- Haripersad, Y.V.; Kannegiesser-Bailey, M.; Morton, K.; Skeldon, S.; Shipton, N.; Edwards, K.; Newton, R.; Newell, A.; Stevenson, P.G.; Martin, A.C. Outbreak of Anorexia Nervosa Admissions during the COVID-19 Pandemic. Arch. Dis. Child. 2021, 106, e15. [Google Scholar] [CrossRef]
- Murray, S.B.; Quintana, D.S.; Loeb, K.L.; Griffiths, S.; Le Grange, D. Treatment outcomes for anorexia nervosa: A systematic review and meta-analysis of randomized controlled trials. Psychol. Med. 2019, 49, 535–544. [Google Scholar] [CrossRef] [PubMed]
- Treasure, J.; Todd, G. Interpersonal Maintaining Factors in Eating Disorder: Skill Sharing Interventions for Carers. In Bio-Psycho-Social Contributions to Understanding Eating Disorders; Springer: Cham, Switzerland, 2016. [Google Scholar] [CrossRef]
- Lock, J.D.; Fitzpatrick, K.K. Anorexia nervosa. BMJ Clin. Evid. 2009, 2009, 1011. [Google Scholar]
- Abbate-Daga, G.; Amianto, F.; Delsedime, N.; De-Bacco, C.; Fassino, S. Resistance to treatment and change in anorexia nervosa: A clinical overview. BMC Psychiatry 2013, 13, 294. [Google Scholar] [CrossRef]
- American Psychiatric Association. Practice Guideline for the Treatment of Patients with Eating Disorders, 3rd ed.; American Psychiatric Association: Washington, DC, USA, 2020. [Google Scholar]
- Royal College of Psychiatrists. Guidelines for the Nutritional Management of Anorexia Nervosa in Children and Adolescents. 2017. Available online: https://www.rcpsych.ac.uk/docs/default-source/improving-care/better-mh-policy/college-reports/cr168.pdf (accessed on 2 February 2024).
- Kells, M.; Kelly-Weeder, S. Nasogastric Tube Feeding for Individuals with Anorexia Nervosa: An Integrative Review. J. Am. Psychiatr. Nurses Assoc. 2016, 22, 449–468. [Google Scholar] [CrossRef]
- Marchili, M.R.; Diamanti, A.; Zanna, V.; Spina, G.; Mascolo, C.; Roversi, M.; Guarnieri, B.; Mirra, G.; Testa, G.; Raucci, U.; et al. Early Naso-Gastric Feeding and Outcomes of Anorexia Nervosa Patients. Nutrients 2023, 15, 490. [Google Scholar] [CrossRef]
- Agostino, H.; Erdstein, J.; Di Meglio, G. Shifting Paradigms: Continuous Nasogastric Feeding with High Caloric Intakes in Anorexia Nervosa. J. Adolesc. Health 2013, 53, 590–594. [Google Scholar] [CrossRef]
- Madden, S.; Miskovic-Wheatley, J.; Wallis, A.; Kohn, M.; Lock, J.; Le Grange, D.; Jo, B.; Clarke, S.; Rhodes, P.; Hay, P.; et al. A Randomized Controlled Trial of In-Patient Treatment for Anorexia Nervosa in Medically Unstable Adolescents. Psychol. Med. 2015, 45, 415–427. [Google Scholar] [CrossRef]
- Parker, E.K.; Faruquie, S.S.; Anderson, G.; Gomes, L.; Kennedy, A.; Wearne, C.M.; Kohn, M.R.; Clarke, S.D. Higher Caloric Refeeding Is Safe in Hospitalised Adolescent Patients with Restrictive Eating Disorders. J. Nutr. Metab. 2016, 2016, 5168978. [Google Scholar] [CrossRef]
- Rigaud, D.; Boulier, A.; Tallonneau, I.; Brindisi, M.C.; Rozen, R. Body Fluid Retention and Body Weight Change in Anorexia Nervosa Patients during Refeeding. Clin. Nutr. 2010, 29, 749–755. [Google Scholar] [CrossRef] [PubMed]
- Pruccoli, J.; Pelusi, M.; Romagnoli, G.; Malaspina, E.; Moscano, F.; Parmeggiani, A. Timing of Psychopharmacological and Nutritional Interventions in the Inpatient Treatment of Anorexia Nervosa: An Observational Study. Brain Sci. 2021, 11, 1242. [Google Scholar] [CrossRef] [PubMed]
- Rigaud, D.; Brondel, L.; Poupard, A.T.; Talonneau, I.; Brun, J.M. A Randomized Trial on the Efficacy of a 2-Month Tube Feeding Regimen in Anorexia Nervosa: A 1-year follow-up study. Clin. Nutr. 2007, 26, 421–429. [Google Scholar] [CrossRef]
- Zuercher, J.; Cumella, E.; Woods, B.; Eberly, M.; Carr, J. Efficacy of Voluntary Nasogastric Tube Feeding in Female Inpatients with Anorexia Nervosa. J. Parenter. Enter. Nutr. 2003, 27, 268–276. [Google Scholar] [CrossRef]
- Sanderson, S.; Tatt, I.D.; Higgins, J.P.T. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: A systematic review and annotated bibliography. Int. J. Epidemiol. 2007, 36, 666–676. [Google Scholar] [CrossRef]
- Bayes, A.; Madden, S. Early Onset Eating Disorders in Male Adolescents: A Series of 10 Inpatients. Australas. Psychiatry 2011, 19, 526–530. [Google Scholar] [CrossRef]
- Rigaud, D.J.; Brayer, V.; Roblot, A.; Brindisi, M.; Vergès, B. Efficacy of Tube Feeding in Binge-Eating/Vomiting Patients. J. Parenter. Enter. Nutr. 2011, 35, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, S.M.; Douglas, J.W.; Lawrence, J.C. Enteral Nutrition via Nasogastric Tube for Refeeding Patients with Anorexia Nervosa: A Systematic Review. Nutr. Clin. Pract. 2019, 34, 359–370. [Google Scholar] [CrossRef]
- Falcoski, P.; Philpot, U.; Tan, J.; Hudson, L.D.; Fuller, S.J. Nasogastric Tube Feeding in Line with New Dietetic Guidelines for the Treatment of Anorexia Nervosa in a Specialist Children and Adolescent Inpatient Unit: A Case Series. J. Hum. Nutr. Diet. 2021, 34, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Matthews-Rensch, K.; Young, A.; Cutmore, C.; Davis, A.; Jeffrey, S.; Patterson, S. Acceptability of Using a Nasogastric Refeeding Protocol with Adult Patients with Medically Unstable Eating Disorders. J. Eval. Clin. Pract. 2023, 29, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Fuller, S.J.; Tan, J.; De Costa, H.; Nicholls, D. Nasogastric Tube Feeding under Physical Restraint: Comprehensive Audit and Case Series across In-Patient Mental Health Units in England. BJPsych Bull. 2023, 47, 322–327. [Google Scholar] [CrossRef]
- Halse, C.; Boughtwood, D.; Clarke, S.; Honey, A.; Kohn, M.; Madden, S. Illuminating Multiple Perspectives: Meanings of Nasogastric Feeding in Anorexia Nervosa. Eur. Eat. Disord. Rev. 2005, 13, 264–272. [Google Scholar] [CrossRef]
- Neiderman, M.; Farley, A.; Richardson, J.; Lask, B. Nasogastric Feeding in Children and Adolescents with Eating Disorders: Toward Good Practice. Int. J. Eat. Disord. 2001, 29, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Blikshavn, T.; Halvorsen, I.; Rø, Ø. Physical Restraint during Inpatient Treatment of Adolescent Anorexia Nervosa: Frequency, Clinical Correlates, and Associations with Outcome at Five-Year Follow-Up. J. Eat. Disord. 2020, 8, 20. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.O.; Hope, T.; Stewart, A.; Fitzpatrick, R. Control and Compulsory Treatment in Anorexia Nervosa: The Views of Patients and Parents. Int. J. Law Psychiatry 2003, 26, 627–645. [Google Scholar] [CrossRef] [PubMed]
- Cusack, P.; Cusack, F.P.; McAndrew, S.; McKeown, M.; Duxbury, J. An Integrative Review Exploring the Physical and Psychological Harm Inherent in Using Restraint in Mental Health Inpatient Settings. Int. J. Ment. Health Nurs. 2018, 27, 1162–1176. [Google Scholar] [CrossRef] [PubMed]
- Mac Donald, B.; Gustafsson, S.A.; Bulik, C.M.; Clausen, L. Living and Leaving a Life of Coercion: A Qualitative Interview Study of Patients with Anorexia Nervosa and Multiple Involuntary Treatment Events. J. Eat. Disord. 2023, 11, 40. [Google Scholar] [CrossRef]
- Amianto, F.; Northoff, G.; Daga, G.A.; Fassino, S.; Tasca, G.A. Is Anorexia Nervosa a Disorder of the Self? A Psychological Approach. Front. Psychol. 2016, 7, 849. [Google Scholar] [CrossRef]
- Pearson, S.D.; Raeke, L.H. Patients’ Trust in Physicians: Many Theories, Few Measures, and Little Data. J. Gen. Intern. Med. 2000, 15, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-S.; Liao, F.-T.; Huang, L.-C.; Chen, S.-L. The Treatment Experience of Anorexia Nervosa in Adolescents from Healthcare Professionals’ Perspective: A Qualitative Study. Int. J. Environ. Res. Public Health 2023, 20, 794. [Google Scholar] [CrossRef] [PubMed]
- Oketah, N.O.; Hur, J.O.; Talebloo, J.; Cheng, C.M.; Nagata, J.M. Parents’ Perspectives of Anorexia Nervosa Treatment in Adolescents: A Systematic Review and Metasynthesis of Qualitative Data. J. Eat. Disord. 2023, 11, 193. [Google Scholar] [CrossRef] [PubMed]
- Whitney, J.L.; Keitel, M.A.; Cummings, M.P.; Ponterotto, J.G.; Ott, E. Caring for Sons with Anorexia: The Perspective of Mothers. J. Child Fam. Stud. 2023, 32, 2637–2651. [Google Scholar] [CrossRef]
- Duclos, J.; Piva, G.; Riquin, É.; Lalanne, C.; Meilleur, D.; Blondin, S.; Berthoz, S.; Mattar, L.; Roux, H.; Thiébaud, M.-R.; et al. Caregivers in Anorexia Nervosa: Is Grief Underlying Parental Burden? Eat. Weight. Disord. 2023, 28, 16. [Google Scholar] [CrossRef] [PubMed]
- Anastasiadou, D.; Medina-Pradas, C.; Sepulveda, A.R.; Treasure, J. A systematic Review of Family Caregiving in Eating Disorders. Eat. Behav. 2014, 15, 464–477. [Google Scholar] [CrossRef] [PubMed]
- Gilburt, H.; Rose, D.; Slade, M. The Importance of Relationships in Mental Health Care: A Qualitative Study of Service Users’ Experiences of Psychiatric Hospital Admission in the UK. BMC Health Serv. Res. 2008, 8, 92. [Google Scholar] [CrossRef] [PubMed]
- Wufong, E.; Rhodes, P.; Conti, J. “We Don’t Really Know What Else We Can Do”: Parent Experiences When Adolescent Distress Persists after the Maudsley and Family-Based Therapies for Anorexia Nervosa. J. Eat. Disord. 2019, 7, 5. [Google Scholar] [CrossRef] [PubMed]
- Mensi, M.M.; Orlandi, M.; Rogantini, C.; Provenzi, L.; Chiappedi, M.; Criscuolo, M.; Castiglioni, M.C.; Zanna, V.; Borgatti, R. Assessing Family Functioning before and after an Integrated Multidisciplinary Family Treatment for Adolescents with Restrictive Eating Disorders. Front. Psychiatry 2021, 12, 653047. [Google Scholar] [CrossRef]
- Amianto, F.; Bertorello, A.; Spalatro, A.; Milazzo, M.; Signa, C.; Cavarero, S.; Daga, G.A.; Fassino, S. Adlerian Parental Counseling in Eating Disorders: Preliminary data of a controlled clinical trial. Eat. Weight. Disord. 2014, 19, 303–314. [Google Scholar] [CrossRef]
- Monteleone, A.M.; Pellegrino, F.; Croatto, G.; Carfagno, M.; Hilbert, A.; Treasure, J.; Wade, T.; Bulik, C.M.; Zipfel, S.; Hay, P.; et al. Treatment of Eating Disorders: A Systematic Meta-Review of Meta-Analyses and Network Meta-Analyses. Neurosci. Biobehav. Rev. 2022, 142, 104857. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, J.E.; Peterson, C.B. Anorexia Nervosa. N. Engl. J. Med. 2020, 382, 1343–1351. [Google Scholar] [CrossRef] [PubMed]
- Maia, B.B.; Campelo, F.G.; Rodrigues, E.C.G.; Oliveira-Cardoso, É.A.; dos Santos, M.A. Perceptions of Health Professionals in Providing Care for People with Anorexia Nervosa and Bulimia Nervosa: A Systematic Review and Meta-Synthesis of Qualitative Studies. Cadernos Saúde Públ. 2023, 39, e00223122. [Google Scholar] [CrossRef] [PubMed]
| Study | Design | Country | Setting | Aims |
|---|---|---|---|---|
| Bayes and Madden (2011) [22] | Retrospective case series | Australia | Hospital | To describe the demographic and clinical features of male inpatients with early-onset eating disorders |
| Rigaud et al. (2011) [23] | Prospective cohort study | France | Outpatient service | Abstinence from binge eating/purging episodes, improvements in nutritional status, psychological and quality of life Improvements |
| Blikshavn et al. (2020) [24] | Quantitative study of follow-up | Norway | Regional, specialized adolescent eating disorders inpatient unit offering a family-based inpatient treatment | To describe the frequency of physical restraint in a specialized program for adolescents with AN, and to examine if meal-related physical restraint (forced nasogastric tube feeding) was related to 5-year outcome |
| Falcoski et al. (2021) [25] | Case series | UK | Hospital (specialist eating disorders unit for children and adolescents) | To illustrate practices in line with new dietetic guidelines for NGT feeding under restraint |
| Matthews-Rensch et al. (2022) [26] | Qualitative exploratory study | Australia | Tertiary hospital | To describe the acceptability of a nasogastric refeeding protocol with adult patients with medically unstable eating disorders and the staff involved in their treatment |
| Fuller et al. (2023) [27] | Comprehensive audit and case series | UK | n.a. | To identify the clinical characteristics of patients receiving nasogastric tube (NGT) feeding under physical restraint |
| Study | Sample | Age in Years | Gender | Length Stay (Average) | Diagnosis |
|---|---|---|---|---|---|
| Bayes and Madden (2011) [22] | 10 | 12.8 (10.6–14.5) | Male (100%) | 36.3 days | AN (30%) EDNOS (70%) |
| Rigaud et al. (2011) [23] | 103 | 27.4 (19.3–35.5) | Female (100%) | n.a. | AN (35%) BN (65%) |
| Blikshavn et al. [24] | 38 | 15.9 (SD = 1.9) | Female (89.5%) Male (10.5%) | 20.3 | AN (100%) |
| Falcoski et al. [25] | 3 | 11 (33%) 14 (67%) | Female (67%) Male (33%) | n.a. | AN (67%) Atypical AN (33%) |
| Matthews-Rensch et al. (2022) [26] | 8 | 22 (18–27) | Female (100%) | n.a. | AN (75%) Atypical AN (12.5%) OSFED (12.5%) |
| Fuller et al. (2023) [27] | 143 | 19.02 (SD = 7.9) | Females (77.6%) Males (1.4%) Gender different from that they were born with (21%) | 29.1 weeks | AN (68.5–75.7%) BN (0.7–3.2%) OSFED (6.7–9.1%) Others |
| Study | Aims | Sample Size | Justified Sample Size? | Level of Evidence |
|---|---|---|---|---|
| Bayes and Madden (2011) [22] | Aims are clear and the study design is appropriate. | 10 | The study sample is too small and not representative of the reference population. | Case series |
| Rigaud et al. (2011) [23] | Aims are clear and the study design is appropriate. | 103 | Sample size is suitable. | Cohort study |
| Blikshavn et al. (2020) [24] | Aims are clear and the study design is appropriate. | 38 | The study sample is too small and not representative of the reference population. | Cohort study |
| Falcoski et al. (2021) [25] | Aims are clear and the study design is appropriate. | 3 | The study sample is too small and not representative of the reference population. | Case series |
| Matthews-Rensch et al. (2022) [26] | Aims are clear and the study design is appropriate. | 8 | The study sample is too small and not representative of the reference population. | Cohort study |
| Fuller et al. (2023) [27] | Aims are clear and the study design is appropriate. | 143 | Sample size is suitable. | Case series |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amianto, F.; Oliaro, T.; Righettoni, F.; Davico, C.; Marcotulli, D.; Vitiello, B. Psychological Effects of Nasogastric Tube (NGT) in Patients with Anorexia Nervosa: A Systematic Review. Nutrients 2024, 16, 2316. https://doi.org/10.3390/nu16142316
Amianto F, Oliaro T, Righettoni F, Davico C, Marcotulli D, Vitiello B. Psychological Effects of Nasogastric Tube (NGT) in Patients with Anorexia Nervosa: A Systematic Review. Nutrients. 2024; 16(14):2316. https://doi.org/10.3390/nu16142316
Chicago/Turabian StyleAmianto, Federico, Tomaso Oliaro, Francesca Righettoni, Chiara Davico, Daniele Marcotulli, and Benedetto Vitiello. 2024. "Psychological Effects of Nasogastric Tube (NGT) in Patients with Anorexia Nervosa: A Systematic Review" Nutrients 16, no. 14: 2316. https://doi.org/10.3390/nu16142316
APA StyleAmianto, F., Oliaro, T., Righettoni, F., Davico, C., Marcotulli, D., & Vitiello, B. (2024). Psychological Effects of Nasogastric Tube (NGT) in Patients with Anorexia Nervosa: A Systematic Review. Nutrients, 16(14), 2316. https://doi.org/10.3390/nu16142316





