Community-Based Participatory Obesity Prevention Interventions in Rural Communities: A Scoping Review
Abstract
1. Introduction
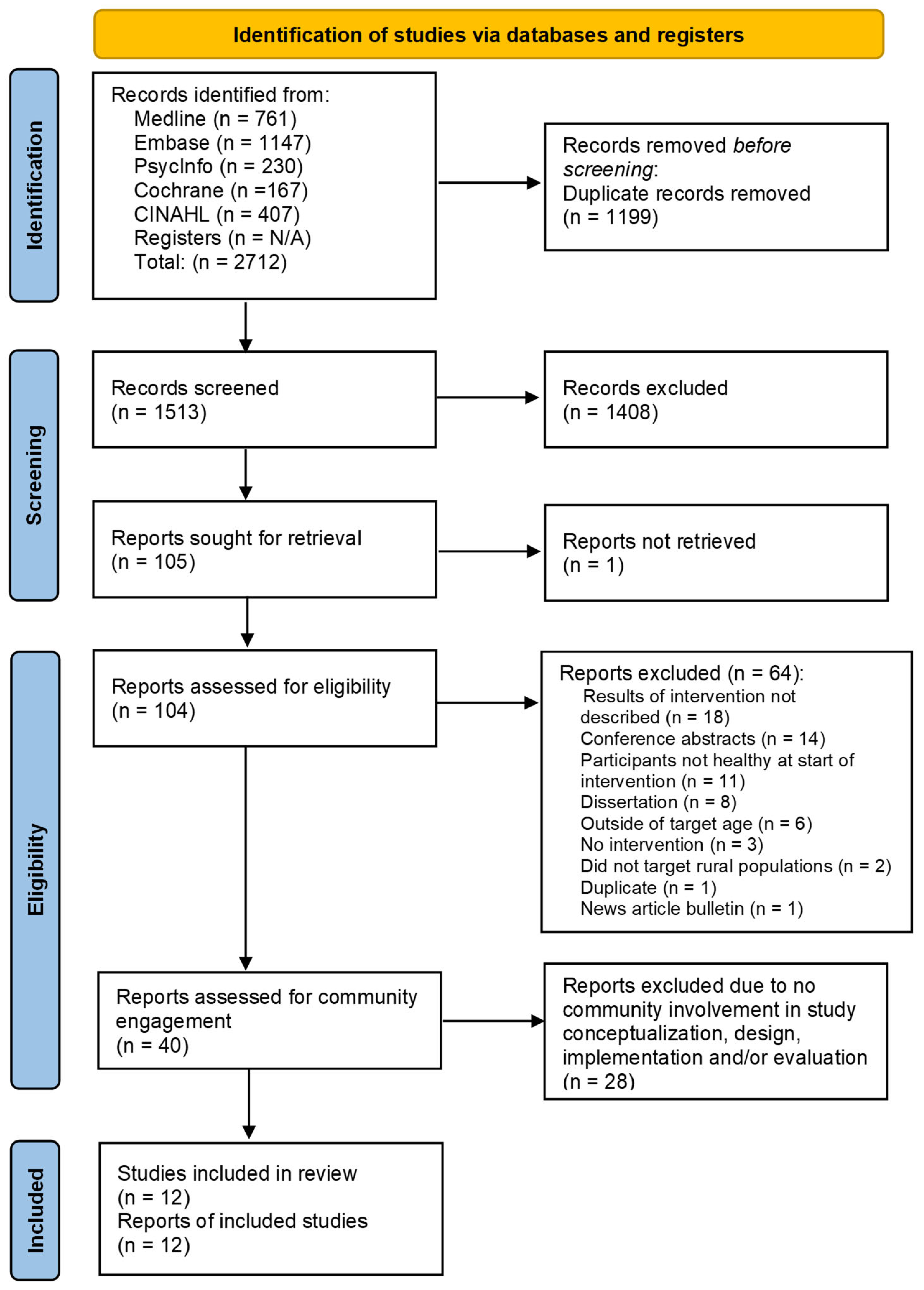
2. Materials and Methods
2.1. Data Sources
2.2. Data Collection Procedures
3. Results
3.1. Study Characteristics
| Author(s) (Year of Publication) | Intervention Name | Geographic Location | Socio-Economic Status | Research Design | Target Audience |
|---|---|---|---|---|---|
| Askelson, N.M., et al. (2019) [42] | None | Iowa | 28.5% of students received free/reduced-price lunch | Quasi-experimental (pre/post—one group) | Middle School Students |
| Belansky, E.S., et al. (2006) [31] | INPAP | Colorado | 67% of students were eligible for free/reduced-price lunch | Quasi-experimental—3 groups | 2nd–3rd-grade students |
| Belansky, E.S., et al. (2013) [33]; Belansky, E.S., et al. (2009) [32] | School Environment Project | Colorado | An average of 69% of students at each school received free/reduced-price lunch | Pair randomized design: 5 schools receiving the AIM intervention and 5 schools receiving the SHI intervention | Elementary school students |
| Canavera, M., et al. (2008) [34] | None | Kentucky | An average of 32% of students at each school received free/reduced-price lunch | Quasi-experimental (pre/post—one group) | 5th-grade students |
| de la Torre, A., et al. (2013) [43]; Sadeghi, B., et al. (2019) [44] | Niños Sanos, Familia Sana | California | 58.9% of students were below the poverty line | Two groups (intervention and control)—quasi-experimental | 3–8-year-old children of Mexican origin |
| Donnelly, J.E., et al. (1996) [46] | None | Nebraska | Not reported | Two groups (intervention and control)—quasi-experimental | 3rd–5th-grade students |
| Greening, L., et al. (2011) [37] | TEAM Mississippi | Mississippi | Treatment group median income: USD 30,713 Control group median income: USD 29,904 | Two groups (intervention and control)—randomized | 6–10-year-old children |
| Gustafson, A., et al. (2017) [35]; Gustafson, A., et al. (2019) [36] for outcomes | Go Big and Bring it Home | Kentucky and North Carolina | Not Reported | Two groups (intervention and control)—randomized | 14–16-year-old adolescents |
| Hawley, S.R., et al. (2006) [45] | Pilot Community Prevention Program | Kansas | Not reported | Quasi-experimental (pre/post—one group) | 6th-grade students |
| Lynch, W.C., et al. (2012) [44]; Eldridge, G., et al. (2016) [43] | 4-Health | Montana | Not Reported | Two groups (intervention and control)—quasi-experimental | Families with 8–12-year-old children |
| Schetzina, K.E., et al. (2009) [39]; Schetzina, K.E., et al. (2009) [40] | Winning with Wellness | Tennessee | More than 50% of students were economically disadvantaged | Quasi-experimental (pre/post—one group) | 3rd–4th-grade students |
| Smith, L.H., et al. (2014) [38] | Sodabriety | Ohio | 40% of students received free/reduced-price lunch | Quasi-experimental (pre/post—one group) | 9th–12th-grade students |
3.2. Intervention Characteristics
3.3. Reported Outcomes
3.4. Review Question #1: To What Extent Were Stakeholders Engaged in the Research Process?
3.5. Research Question #2: How Were the Target Audience (K-12th Graders) and/or Their Parents/Caregivers Involved in the Research?
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 22 April 2024).
- Stierman, B.; Afful, J.; Carroll, M.D.; Chen, T.C.; Davy, O.; Fink, S.; Fryar, C.D.; Gu, Q.; Hales, C.M.; Hughes, J.P.; et al. National Health and Nutrition Examination Survey 2017–March 2020 prepandemic data files development of files and prevalence estimates for selected health outcomes. Natl. Health Stat. Rep. 2021, 158, 1–20. [Google Scholar] [CrossRef]
- Mahmood, N.; Sanchez-Vaznaugh, E.V.; Matsuzaki, M.; Sánchez, B.N. Racial/ethnic disparities in childhood obesity: The role of school segregation. Obesity 2022, 30, 1116–1125. [Google Scholar] [CrossRef] [PubMed]
- U.S. Census Bureau. New Census Data Show Differences Between Urban and Rural Populations. Available online: https://www.census.gov/newsroom/press-releases/2016/cb16-210.html (accessed on 15 April 2024).
- U.S. Census Bureau. Nation’s Urban and Rural Populations Shift following 2020 Census. Available online: https://www.census.gov/newsroom/press-releases/2022/urban-rural-populations.html (accessed on 15 April 2024).
- United Nations; Department of Economic and Social Affairs; Population Division. World Urbanization Prospects: The 2018 Revision (ST/ESA/SER.A/420); United Nations: New York, NY, USA, 2019; Available online: https://population.un.org/wup/Publications/Files/WUP2018-Report.pdf (accessed on 17 June 2024).
- Johnson, J.A., III; Johnson, A.M. Urban-rural differences in childhood and adolescent obesity in the United States: A systematic review and meta-analysis. Child. Obes. 2015, 11, 233–241. [Google Scholar] [CrossRef]
- Zgodic, A.; Eberth, J.M.; Breneman, C.B.; Wende, M.E.; Kaczynski, A.T.; Liese, A.D.; McLain, A.C. Estimates of childhood overweight and obesity at the region, state, and county levels: A multilevel small-area estimation approach. Am. J. Epidemiol. 2021, 190, 2618–2629. [Google Scholar] [CrossRef]
- National Heart Lung and Blood Institute. Overweight and Obesity Causes and Risk Factors. Available online: https://www.nhlbi.nih.gov/health/overweight-and-obesity/causes (accessed on 15 April 2024).
- Davis, A.M.; Boles, R.E.; James, R.L.; Sullivan, D.K.; Donnelly, J.E.; Swirczynski, D.L.; Goetz, J. Health behaviors and weight status among urban and rural children. Rural Remote Health 2008, 8, 810. [Google Scholar] [CrossRef]
- Joens-Matre, R.R.; Welk, G.J.; Calabro, M.A.; Russell, D.W.; Nicklay, E.; Hensley, L.D. Rural-urban differences in physical activity, physical fitness, and overweight prevalence of children. J. Rural Health 2008, 24, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.H.; Jones, S.J.; Sun, H.; Probst, J.C.; Merchant, A.T.; Cavicchia, P. Diet, physical activity, and sedentary behaviors as risk factors for childhood obesity: An urban and rural comparison. Child. Obes. 2012, 8, 440–448. [Google Scholar] [CrossRef]
- Liu, J.; Bennett, K.J.; Harun, N.; Probst, J.C. Urban-rural differences in overweight status and physical inactivity among US children aged 10–17 years. J. Rural Health 2008, 24, 407–415. [Google Scholar] [CrossRef]
- Singh, G.K.; Kogan, M.D.; Van Dyck, P.C.; Siahpush, M. Racial/ethnic, socioeconomic, and behavioral determinants of childhood and adolescent obesity in the United States: Analyzing independent and joint associations. Ann. Epidemiol. 2008, 18, 682–695. [Google Scholar] [CrossRef]
- Wattelez, G.; Frayon, S.; Caillaud, C.; Galy, O. Physical activity in adolescents living in rural and urban New Caledonia: The role of socioenvironmental factors and the association with weight status. Front. Public Health 2021, 9, 623685. [Google Scholar] [CrossRef]
- Crouch, E.; Abshire, D.A.; Wirth, M.D.; Hung, P.; Benavidez, G.A. Rural-urban differences in overweight and obesity, physical activity, and food security among children and adolescents. Prev. Chronic Dis. 2023, 20, E92. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.M.; Bennett, K.J.; Befort, C.; Nollen, N. Obesity and related health behaviors among urban and rural children in the United States: Data from the National Health And Nutrition Examination Survey 2003–2004 and 2005–2006. J. Pediatr. Psychol. 2011, 36, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Euler, R.; Jimenez, E.Y.; Sanders, S.; Kuhlemeier, A.; Van Horn, M.L.; Cohen, D.; Gonzales-Pacheco, D.; Kong, A.S. Rural-urban differences in baseline dietary intake and physical activity levels of adolescents. Prev. Chronic Dis. 2019, 16, E01. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.S.; Robinson, J.; Hinton, E.; Gordy, X.Z.; Gamble, A.; Compretta, C.; Holmes, M.E.; Ravola, M. School-based obesity prevention programs in rural communities: A scoping review. JBI Evid. Synth. 2022, 20, 2936–2985. [Google Scholar] [CrossRef] [PubMed]
- Wallerstein, N.; Duran, B. Community-based participatory research contributions to intervention research: The intersection of science and practice to improve health equity. Am. J. Public Health 2010, 100 (Suppl. S1), S40–S46. [Google Scholar] [CrossRef] [PubMed]
- McCloskey, D.J.; McDonald, M.A.; Cook, J.; Heurtin-Roberts, S.; Updegrove, S.; Sampson, D.; Gutter, S.; Eder, M. Community engagement: Definitions and organizing concepts from the literature. In Principles of Community Engagement, 2nd ed.; Clinical and Translational Science Awards (CTSA) Consortium Community Engagement Key Function Committee Task Force on the Principles of Community Engagement, Ed.; U.S. Government Publishing Office: Washington, DC, USA, 2011; pp. 1–42. [Google Scholar]
- O’Mara-Eves, A.; Brunton, G.; Oliver, S.; Kavanagh, J.; Jamal, F.; Thomas, J. The effectiveness of community engagement in public health interventions for disadvantaged groups: A meta-analysis. BMC Public Health 2015, 15, 129. [Google Scholar] [CrossRef] [PubMed]
- Eder, M.M.; D’Alonzo, K.T.; Yonas, M.A.; Oetzel, J.G. Editorial: Examining community-engaged and participatory research programs and projects. Front. Public Health 2023, 11, 1239670. [Google Scholar] [CrossRef] [PubMed]
- Rural Health Information Hub. Community-Based Participatory Research Strategies for Addressing SDOH. Available online: https://www.ruralhealthinfo.org/toolkits/sdoh/4/research-strategies (accessed on 15 April 2024).
- Duea, S.R.; Zimmerman, E.B.; Vaughn, L.M.; Dias, S.; Harris, J. A guide to selecting participatory research methods based on project and partnership goals. J. Particip. Res. Methods 2022, 3. [Google Scholar] [CrossRef]
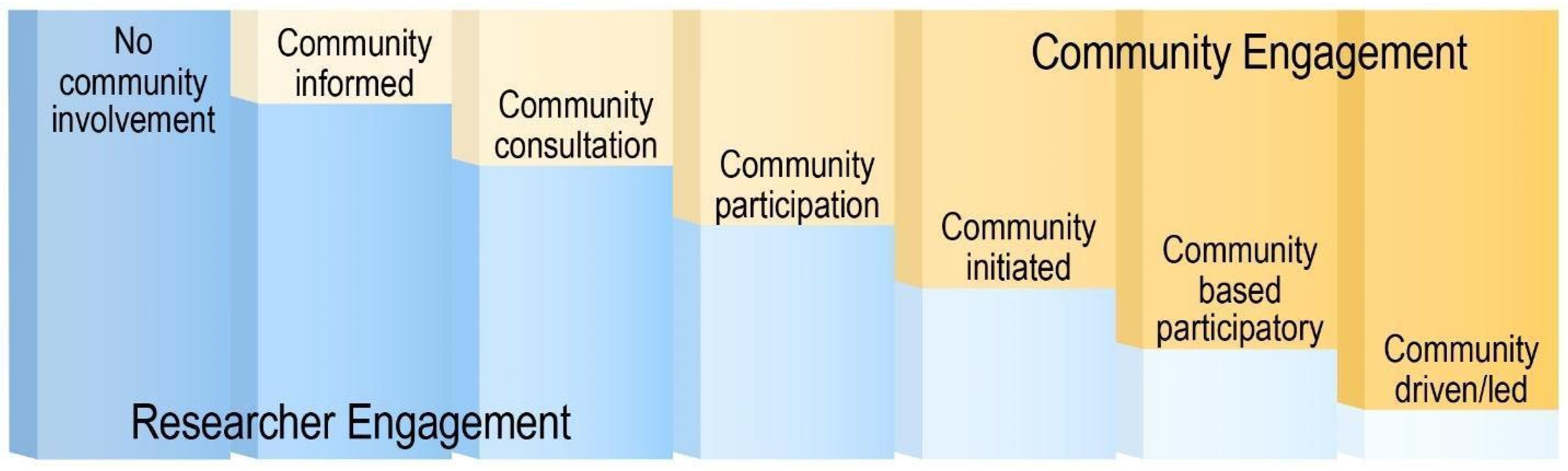
- Key, K.D.; Furr-Holden, D.; Lewis, E.Y.; Cunningham, R.; Zimmerman, M.A.; Johnson-Lawrence, V.; Selig, S. The continuum of community engagement in research: A roadmap for understanding and assessing progress. Prog. Community Health Partnersh. 2019, 13, 427–434. [Google Scholar] [CrossRef]
- Elbers, S.; van Gessel, C.; Renes, R.J.; van der Lugt, R.; Wittink, H.; Hermsen, S. Innovation in pain rehabilitation using co-design methods during the development of a relapse prevention intervention: Case study. J. Med. Internet Res. 2021, 23, e18462. [Google Scholar] [CrossRef]
- Tanner, A.; Kim, S.H.; Friedman, D.B.; Foster, C.; Bergeron, C.D. Barriers to medical research participation as perceived by clinical trial investigators: Communicating with rural and African American communities. J. Health Commun. 2015, 20, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Ratcliffe, M.; Burd, C.; Holder, K.; Fields, A. Defining Rural at the U.S. Census Bureau. ACSGEO-1. 2016. Available online: https://www2.census.gov/geo/pdfs/reference/ua/Defining_Rural.pdf (accessed on 15 April 2024).
- Belansky, E.S.; Romaniello, C.; Morin, C.; Uyeki, T.; Sawyer, R.L.; Scarbro, S.; Auld, G.W.; Crane, L.; Reynolds, K.; Hamman, R.F.; et al. Adapting and implementing a long-term nutrition and physical activity curriculum to a rural, low-income, biethnic community. J. Nutr. Educ. Behav. 2006, 38, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Belansky, E.S.; Cutforth, N.; Delong, E.; Ross, C.; Scarbro, S.; Gilbert, L.; Beatty, B.; Marshall, J.A. Early impact of the federally mandated Local Wellness Policy on physical activity in rural, low-income elementary schools in Colorado. J. Public Health Policy 2009, 30 (Suppl. S1), S141–S160. [Google Scholar] [CrossRef] [PubMed]
- Belansky, E.S.; Cutforth, N.; Chavez, R.; Crane, L.A.; Waters, E.; Marshall, J.A. Adapted intervention mapping: A strategic planning process for increasing physical activity and healthy eating opportunities in schools via environment and policy change. J. Sch. Health 2013, 83, 194–205. [Google Scholar] [CrossRef] [PubMed]
- Canavera, M.; Sharma, M.; Murnan, J. Development and pilot testing a social cognitive theory-based intervention to prevent childhood obesity among elementary students in rural Kentucky. Int. Q. Community Health Educ. 2008, 29, 57–70. [Google Scholar] [CrossRef] [PubMed]
- Gustafson, A.; Jilcott Pitts, S.; McDonald, J.; Ford, H.; Connelly, P.; Gillespie, R.; Liu, E.; Bush, H.; Brancato, C.; Babatande, T.; et al. Direct effects of the home, school, and consumer food environments on the association between food purchasing patterns and dietary intake among rural adolescents in Kentucky and North Carolina, 2017. Int. J. Env. Res. Public Health 2017, 14, 1255. [Google Scholar] [CrossRef] [PubMed]
- Gustafson, A.; Jilcott Pitts, S.B.; McQuerry, K.; Babtunde, O.; Mullins, J. A mentor-led text-messaging intervention increases intake of fruits and vegetables and goal setting for healthier dietary consumption among rural adolescents in Kentucky and North Carolina, 2017. Nutrients 2019, 11, 593. [Google Scholar] [CrossRef] [PubMed]
- Greening, L.; Harrell, K.T.; Low, A.K.; Fielder, C.E. Efficacy of a school-based childhood obesity intervention program in a rural southern community: TEAM Mississippi Project. Obesity 2011, 19, 1213–1219. [Google Scholar] [CrossRef]
- Smith, L.H.; Holloman, C. Piloting “sodabriety”: A school-based intervention to impact sugar-sweetened beverage consumption in rural Appalachian high schools. J. Sch. Health 2014, 84, 177–184. [Google Scholar] [CrossRef]
- Schetzina, K.E.; Dalton III, W.T.; Lowe, E.F.; Azzazy, N.; Vonwerssowetz, K.M.; Givens, C.; Stern, H.P. Developing a coordinated school health approach to child obesity prevention in rural Appalachia: Results of focus groups with teachers, parents, and students. Rural. Remote Health 2009, 9, 1157. [Google Scholar] [CrossRef] [PubMed]
- Schetzina, K.E.; Dalton, W.T., 3rd; Lowe, E.F.; Azzazy, N.; VonWerssowetz, K.M.; Givens, C.; Pfortmiller, D.T.; Stern, H.P. A coordinated school health approach to obesity prevention among Appalachian youth: The Winning with Wellness Pilot Project. Fam. Community Health 2009, 32, 271–285. [Google Scholar] [CrossRef]
- Appalachian Research Commission. About the Appalachian Region. Available online: https://www.arc.gov/about-the-appalachian-region/#:~:text=The%20Region%E2%80%99s%2026.3%20million%20residents,and%20all%20of%20West%20Virginia (accessed on 15 April 2024).
- Askelson, N.M.; Brady, P.; Ryan, G.; Meier, C.; Ortiz, C.; Scheidel, C.; Delger, P. Actively involving middle school students in the implementation of a pilot of a behavioral economics-based lunchroom intervention in rural schools. Health Promot. Pract. 2019, 20, 675–683. [Google Scholar] [CrossRef] [PubMed]
- de la Torre, A.; Sadeghi, B.; Green, R.D.; Kaiser, L.L.; Flores, Y.G.; Jackson, C.F.; Shaikh, U.; Whent, L.; Schaefer, S.E. Niños Sanos, Familia Sana: Mexican immigrant study protocol for a multifaceted CBPR intervention to combat childhood obesity in two rural California towns. BMC Public Health 2013, 13, 1033. [Google Scholar] [CrossRef]
- Sadeghi, B.; Kaiser, L.L.; Hanbury, M.M.; Tseregounis, I.E.; Shaikh, U.; Gomez-Camacho, R.; Cheung, R.C.Y.; Aguilera, A.L.; Whent, L.; de la Torre, A. A three-year multifaceted intervention to prevent obesity in children of Mexican-heritage. BMC Public Health 2019, 19, 582. [Google Scholar] [CrossRef]
- Hawley, S.R.; Beckman, H.; Bishop, T. Development of an obesity prevention and management program for children and adolescents in a rural setting. J. Community Health Nurs. 2006, 23, 69–80. [Google Scholar] [CrossRef]
- Donnelly, J.E.; Jacobsen, D.J.; Whatley, J.E.; Hill, J.O.; Swift, L.L.; Cherrington, A.; Polk, B.; Tran, Z.V.; Reed, G. Nutrition and physical activity program to attenuate obesity and promote physical and metabolic fitness in elementary school children. Obes. Res. 1996, 4, 229–243. [Google Scholar] [CrossRef]
- Eldridge, G.; Paul, L.; Bailey, S.J.; Ashe, C.B.; Martz, J.; Lynch, W. Effects of parent-only childhood obesity prevention programs on BMIz and body image in rural preteens. Body Image 2016, 16, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Lynch, W.C.; Martz, J.; Eldridge, G.; Bailey, S.J.; Benke, C.; Paul, L. Childhood obesity prevention in rural settings: Background, rationale, and study design of ‘4-Health,’ a parent-only intervention. BMC Public Health 2012, 12, 255. [Google Scholar] [CrossRef]
- Dong, Y.; Ma, Y.; Dong, B.; Zou, Z.; Hu, P.; Wang, Z.; Yang, Y.; Song, Y.; Ma, J. Geographical variation and urban-rural disparity of overweight and obesity in Chinese school-aged children between 2010 and 2014: Two successive national cross-sectional surveys. BMJ Open 2019, 9, e025559. [Google Scholar] [CrossRef]
- Gu, D.; Andreev, K.; Dupre, M.E. Major trends in population growth around the world. China CDC Wkly. 2021, 3, 604–613. [Google Scholar] [CrossRef] [PubMed]
- Polidano, K.; Parton, L.; Agampodi, S.B.; Agampodi, T.C.; Haileselassie, B.H.; Lalani, J.M.G.; Mota, C.; Price, H.P.; Rodrigues, S.; Tafere, G.R.; et al. Community engagement in cutaneous leishmaniasis research in Brazil, Ethiopia, and Sri Lanka: A decolonial approach for global health. Front. Public Health 2022, 10, 823844. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Agriculture—Economic Research Service. Rural America at a Glance—2017 Edition. Economic Information Bulletin 182. 2017. Available online: https://www.ers.usda.gov/webdocs/publications/85740/eib-182.pdf?v=43054 (accessed on 3 April 2024).
- National Academies of Science Engineering and Medicine. Achieving Rural Health Equity and Well-Being: Proceedings of a Workshop; The National Academies: Washington, DC, USA, 2018. [Google Scholar]
- Economic Research Service—U.S. Department of Agriculture. Counties with Continuous High Poverty since 1960 Are Largely Rural. Available online: https://www.ers.usda.gov/data-products/chart-gallery/gallery/chart-detail/?chartId=105425 (accessed on 4 May 2023).
- Economic Research Service—U.S. Department of Agriculture. Rural Poverty & Well-Being. Available online: https://www.ers.usda.gov/topics/rural-economy-population/rural-poverty-well-being/#geography (accessed on 4 May 2023).
- Henning-Smith, C.; Evenson, A.; Corbett, A.; Kozhimannil, K.; Moscovice, I. Rural Transportation: Challenges and Opportunities. Policy Brief. Available online: https://rhrc.umn.edu/wp-content/files_mf/1518734252UMRHRCTransportationChallenges.pdf (accessed on 13 May 2024).
- Agency for Healthcare Research and Quality. National Healthcare Quality and Disparities Report Chartbook on Rural Healthcare. AHRQ Pub. No. 22-0010. Rockville, MD: U.S. Department of Health and Human Services. 2021. Available online: https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/chartbooks/2019-qdr-rural-chartbook.pdf (accessed on 5 May 2024).
- Rural Health Information Hub. Rural Hunger and Access to Healthy Food: Why Do Food Deserts Exist in Rural Areas? Available online: https://www.ruralhealthinfo.org/topics/food-and-hunger#food-deserts (accessed on 2 November 2023).
- Ko, L.K.; Enzler, C.; Perry, C.K.; Rodriguez, E.; Mariscal, N.; Linde, S.; Duggan, C. Food availability and food access in rural agricultural communities: Use of mixed methods. BMC Public Health 2018, 18, 634. [Google Scholar] [CrossRef] [PubMed]
- Hansen, A.Y.; Umstattd Meyer, M.R.; Lenardson, J.D.; Hartley, D. Built environments and active living in rural and remote areas: A review of the literature. Curr. Obes. Rep. 2015, 4, 484–493. [Google Scholar] [CrossRef] [PubMed]
- Fergusson, D.; Monfaredi, Z.; Pussegoda, K.; Garritty, C.; Lyddiatt, A.; Shea, B.; Duffett, L.; Ghannad, M.; Montroy, J.; Murad, M.H.; et al. The prevalence of patient engagement in published trials: A systematic review. Res. Involv. Engagem. 2018, 4, 17. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.; Miranda, J.; Callender, C.; Dave, J.M.; Appiah, G.; Musaad, S.M.A. See me, hear me, know me: Perspectives on diet and physical activity influences among teens living in rural Texas communities. Nutrients 2023, 15, 4695. [Google Scholar] [CrossRef] [PubMed]
- Allen, H.; Callender, C.; Thompson, D. Promoting health equity: Identifying parent and child reactions to a culturally-grounded obesity prevention program specifically designed for Black girls using community-engaged research. Children 2023, 10, 417. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Hladek, M.D.; Ejem, D. One size fits all—An underappreciated health inequity. JAMA Intern. Med. 2024, 184, 7–8. [Google Scholar] [CrossRef] [PubMed]
- Lu, A.S.; Green, M.C.; Alon, D. The effect of animated Sci-Fi characters’ racial presentation on narrative engagement, wishful identification, and physical activity intention among children. J. Commun. 2024, 74, 160–172. [Google Scholar] [CrossRef]
- Jacob, C.M.; Hardy-Johnson, P.L.; Inskip, H.M.; Morris, T.; Parsons, C.M.; Barrett, M.; Hanson, M.; Woods-Townsend, K.; Baird, J. A systematic review and meta-analysis of school-based interventions with health education to reduce body mass index in adolescents aged 10 to 19 years. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 1. [Google Scholar] [CrossRef]
- Andrade, J.; Lotton, J.; Andrade, J. Systematic review: Frameworks used in school-based interventions, the impact on Hispanic children’s obesity-related outcomes. J. Sch. Health 2018, 88, 847–858. [Google Scholar] [CrossRef] [PubMed]
- Barlow, S.E.; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007, 120 (Suppl. S4), S164–S192. [Google Scholar] [CrossRef]
- Daniels, S.R.; Arnett, D.K.; Eckel, R.H.; Gidding, S.S.; Hayman, L.L.; Kumanyika, S.; Robinson, T.N.; Scott, B.J.; St Jeor, S.; Williams, C.L. Overweight in children and adolescents: Pathophysiology, consequences, prevention, and treatment. Circulation 2005, 111, 1999–2012. [Google Scholar] [CrossRef] [PubMed]
- Gruber, K.J.; Haldeman, L.A. Using the family to combat childhood and adult obesity. Prev. Chronic Dis. 2009, 6, A106. [Google Scholar] [PubMed]
- Schrempft, S.; van Jaarsveld, C.H.; Fisher, A.; Fildes, A.; Wardle, J. Maternal characteristics associated with the obesogenic quality of the home environment in early childhood. Appetite 2016, 107, 392–397. [Google Scholar] [CrossRef] [PubMed]
- Freeman, E.; Fletcher, R.; Collins, C.E.; Morgan, P.J.; Burrows, T.; Callister, R. Preventing and treating childhood obesity: Time to target fathers. Int. J. Obes. 2012, 36, 12–15. [Google Scholar] [CrossRef] [PubMed]
- Johnson, B.E.; Ray, W.A. Family systems theory. In Encyclopedia of Family Studies; Shehan, C.L., Ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2016; pp. 1–5. [Google Scholar]
- Kitzman-Ulrich, H.; Wilson, D.K.; St George, S.M.; Lawman, H.; Segal, M.; Fairchild, A. The integration of a family systems approach for understanding youth obesity, physical activity, and dietary programs. Clin. Child. Fam. Psychol. Rev. 2010, 13, 231–253. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, S.G.; Arnold, E.M.; Irby, M.B.; Boles, K.A.; Skelton, J.A. Family systems theory and obesity treatment: Applications for clinicians. Infant. Child. Adolesc. Nutr. 2014, 6, 24–29. [Google Scholar] [CrossRef]
- Dave, J.M.; Chen, T.A.; Castro, A.N.; White, M.; Onugha, E.A.; Zimmerman, S.; Thompson, D. Regional variability in the prevalence of food insecurity and diet quality among United States children. Nutrients 2024, 16, 224. [Google Scholar] [CrossRef]
- Budig, K.; Diez, J.; Conde, P.; Sastre, M.; Hernán, M.; Franco, M. Photovoice and empowerment: Evaluating the transformative potential of a participatory action research project. BMC Public Health 2018, 18, 432. [Google Scholar] [CrossRef]
- Thompson, D.; Callender, C.; Dave, J.M.; Jibaja-Weiss, M.L.; Montealegre, J.R. Health equity in action: Using community engaged research to update an intervention promoting a healthy home food environment to Black/African American families. Cancer Causes Control 2024, 35, 311–321. [Google Scholar] [CrossRef]
- Hailemariam, M.; Bustos, T.; Montgomery, B.; Barajas, R.; Evans, L.B.; Drahota, A. Evidence-based intervention sustainability strategies: A systematic review. Implement. Sci. 2019, 14, 57. [Google Scholar] [CrossRef] [PubMed]
- Grow, H.M.; Hencz, P.; Verbovski, M.J.; Gregerson, L.; Liu, L.L.; Dossett, L.; Larison, C.; Saelens, B.E. Partnering for success and sustainability in community-based child obesity intervention: Seeking to help families ACT! Fam. Community Health 2014, 37, 45–59. [Google Scholar] [CrossRef] [PubMed]
- McDavitt, B.; Bogart, L.M.; Mutchler, M.G.; Wagner, G.J.; Green, H.D., Jr.; Lawrence, S.J.; Mutepfa, K.D.; Nogg, K.A. Dissemination as dialogue: Building trust and sharing research findings through community engagement. Prev. Chronic Dis. 2016, 13, E38. [Google Scholar] [CrossRef] [PubMed]
- Harris, A.D.; McGregor, J.C.; Perencevich, E.N.; Furuno, J.P.; Zhu, J.; Peterson, D.E.; Finkelstein, J. The use and interpretation of quasi-experimental studies in medical informatics. J. Am. Med. Inf. Assoc. 2006, 13, 16–23. [Google Scholar] [CrossRef] [PubMed]
| Author(s) (Year of Publication) | Intervention Focus | Intervention Setting | Duration | Components | Theoretical Framework | Implementer |
|---|---|---|---|---|---|---|
| Askelson, N. M., et al. (2019) [42] | Diet | School—lunchroom | 1 Academic Year | Cafeteria changes in food and prompts from foodservice staff | Behavioral Economics | Students, foodservice staff |
| Belansky, E. S., et al. (2006) [31] | Physical Activity and Diet | School | 2 Years | Classroom based nutrition and PA lessons; 10 home visits that included fun activities and coaching techniques to motivate family members to make behavioral changes | Social Cognitive Theory, Piaget Cognitive Development Theory | Resource teachers, classroom teachers, and family advisor |
| Belansky, E. S., et al. (2013) [33]; Belansky, E. S., et al. (2009) [32] | Physical Activity and Diet | School | 3 Academic Semesters | Implemented environmental and policy changes using AIM or SHI; AIM schools included 12 meetings led by trained, external facilitators with school task force while SHI schools had no external facilitation but were instead given a self-assessment and planning tool | Social Cognitive Theory | AIM—School task force led by external facilitator, SHI—School health team which included principal and a team of school staff |
| Canavera, M., et al. (2008) [34] | Physical Activity, Diet, and Watching less TV | School (PE class) | 12 Weeks | Four modules that focused on PA, fruit/vegetable consumption, limiting television use, and replacing sweetened beverages with water | Social Cognitive Theory | Physical education or Health education teachers |
| de la Torre, et al. (2013) [43]; Sadeghi, et al. (2019) [44] | Physical Activity and Diet | School | 3 Years | Nutrition education was provided on family nights and in school; the SPARK PA Program was implemented; families were provided with a monthly fruit and vegetable voucher worth USD 25/month; community art tools and strategies were used to engage community members | Social Cognitive Theory, Health Belief Model | Local health educators, local teachers, and the University of California Cooperative Extension |
| Donnelly, J. E., et al. (1996) [46] | Physical Activity and Diet | School | 2 Academic Years | Used existing programming (Lunchpower program) to enhance PA, create grade-specific nutrition education, and a modified school lunch program | Not mentioned | Classroom teachers and cafeteria staff |
| Greening, L., et al. (2011) [37] | Physical Activity and Diet | School and Community | 8 Months | Monthly nutrition and PA events for families; foodservice equipment changes; two 45 min PA sessions/week; incorporation of classroom nutrition lectures | Social Learning Theory | Dietitians, educators from the Department of Education, and school faculty |
| Gustafson, A. (2017) [35]; Gustafson, A. (2019) [36] for outcomes | Diet | Virtual | 1 Academic Semester | Text messages were sent two times a week to encourage healthy food purchasing; weekly challenges were given as well | Social Cognitive Theory | Undergraduate students |
| Hawley, S. R., et al. (2006) [45] | Physical Activity and Diet | School | 6 Weeks | Five 40 min sessions in PE class; community family event that provided a fitness option and education on nutrition and exercise | Principles of behavior change—Transtheoretical model | Unclear |
| Lynch et al. (2012) [48]; Eldridge (2016) [47] | Physical Activity and Diet | County Extension Office | 8 Months | Ten, 90 min, face-to-face meetings covering healthy eating, PA, stress management, and effective parenting strategies; take-home materials such as handouts and recipes were given; control group received written information from USDA sources | Social Cognitive Theory, Health at Every Size approach, Social Marketing Theory | County agents |
| Schetzina, K.E., et al. (2009) [39]; Schetzina, K.E., et al. (2009) [40] | Physical Activity and Diet | School | 18 Months | Nutrition services which included a series of interactive Go, Slow, and Whoa lesson plans; classroom health education lessons; increased PA during the school day; health screenings and referrals for students; counseling and psychological services; changes to the cafeteria menu and school environment; health promotion for staff; involvement of parents and community in promoting healthy behavior changes | Coordinated School Health Model | Classroom teachers, school health staff, school administration, parents |
| Smith, L. H., et al. (2014) [38] | Diet | School | 30 Days | Promotional campaign which included a commercial flier, T-shirts, and posters; daily announcements about the benefits of limiting sweetened beverage consumption; distribution of nylon goody bags with promotional items; wellness presentations | Not mentioned | The Teen Advisory Council which consisted of teachers and students |
| Community Engagement Level | Example |
|---|---|
| Community-Informed | Statewide or national data used to determine intervention focus, content, mode |
| Community Consultation | Interviews or focus groups conducted to identify needs and to shape an intervention; researcher determines intervention focus (e.g., diet, physical activity) |
| Community Participation | Community advisory board to guide changes to a previously developed intervention |
| Community-Initiated | A community coalition approaches researchers to assist them with developing an intervention |
| Community-Based Participatory Research | Researchers and community jointly identify a need, determine how to address it, develop the intervention, assist in recruitment, evaluation and/or interpretation |
| Community-Driven/Community-Led | Community coalition identifies a problem, determines how to address it; may consult with a researcher for advice or questions, but community drives the research and makes decisions |
| Stakeholder Level | Definition | Example |
|---|---|---|
| Level 1 | Target audience | School-aged children |
| Level 2 | Caregivers | Parents |
| Level 3 | Intervention implementers | Teachers or school staff |
| Level 4 | Community members not included in levels 1–3 | City managers or local elected officials |
| Author(s) (Year of Publication) | Stakeholder Involvement | Community Engagement Level | Participants in Community Engaged Research | Stakeholder Level a |
|---|---|---|---|---|
| Askelson, N.M., et al. (2019) [42] | Student group assisted in planning, implementing, and evaluating changes to lunchroom. Food service staff collaborated with students to review lunchroom assessments and jointly identify and plan changes. | CBPR | Students and food service staff | 1, 3 |
| Belansky, E.S., et al. (2006) [31] | Rural-based teachers and nutrition educators adapted lessons for culturally relevance | Community Participation | Teachers and nutrition educators | 3 |
| Belansky, E.S., et al. (2013) [33]; Belansky, E.S., et al. (2009) [32] | A steering committee consisting of school personnel made decisions on research design, school recruitment strategies, intervention plans, evaluation and dissemination plans, and other related matters. In AIM schools, a task force consisting of the principal, food service manager, parent(s), and school nurse evaluated the school environment and selected/implemented changes. In SHI schools, school staff were responsible for planning and implementing changes. | CBPR | Parents and school personnel including principal, foodservice manager, and school nurse | 2, 3, 4 |
| Canavera, M., et al. (2008) [34] | Focus groups consisting of parents and children were used to gather information on physical activity behaviors, watching television, and fruit/vegetable/water intake | Community Consultation | Parents and students | 1, 2 |
| de laTorre, A., et al. (2013) [43]; Sadeghi, B., et al. (2019) [44] | Research team conducted focused meetings with various community leaders; research team presented proposed research at town hall meetings to gather feedback; a Community Advisory Council comprising stakeholders from each community including representatives such as city managers, school superintendents, teachers, principals, school nurses, food service managers, local health facility representatives, religious leaders, community health outreach workers (promotores), and a representative from a major local supermarket was formed | Community Participation | Various community leaders including city managers, local elected officials, school superintendents and boards, teachers, religious leaders, local healthcare professionals, principals, school nurses, food service managers, local health facility representatives, community health outreach workers (promotores), and a representative from a major local supermarket | 3, 4 |
| Donnelly, J.E., et al. (1996) [46] | Kitchen staff helped plan meals to reflect Lunchpower; teachers helped develop and deliver nutrition education and physical activity program | Community Participation | Kitchen staff, teachers | 3 |
| Greening, L., et al. (2011) [37] | Focus groups were held with community residents to obtain their input on treatment activities that would complement the community’s activities. Parents completed a dietary habit questionnaire for their children and teachers incorporated health information in their lectures | Community-Informed | Parents, teachers, community members | 2, 3, 4 |
| Gustafson, A. (2017) [35]; Gustafson, A. (2019) for outcomes [36] | Student survey aimed to gather information about the adolescents’ food purchasing patterns, dietary intake, home food availability, and demographics | Community-Informed | Students | 1 |
| Hawley, S.R., et al. (2006) [45] | Community meetings were conducted to determine barriers to addressing youth obesity; director of the local recreation commission was interviewed; community church completed a survey | Community Consultation | Community members | 4 |
| Lynch, W.C., et al. (2012) [48]; Eldridge, G., (2016) [47] | Focus groups with parents were used to identify concerns regarding child obesity, interest in participating, and time constraints | Community Consultation | Parents | 2 |
| Schetzina, K.E., et al. (2009) [40]; Schetzina, K.E., et al. (2009) [39] | Focus groups with students, teachers, and parents were used to understand perceptions on institutional guidelines concerning nutrition and physical activity; a coalition consisting of educators, healthcare providers, parents, community members, and researchers designed the intervention and met monthly to discuss the results and make needed modifications | Community Participation | Educators, healthcare providers, parents, students, teachers and community members | 1, 2, 3, 4 |
| Smith, L.H., et al. (2014) [38] | A community survey was completed by community residents, school personnel, teens, and parents to identify health concerns; teachers and students were responsible for developing and delivering the intervention | CBPR | Students, parents, school staff, and community residents | 1, 2, 3, 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dhanjani, S.; Allen, H.; Varman, B.; Callender, C.; Dave, J.M.; Thompson, D. Community-Based Participatory Obesity Prevention Interventions in Rural Communities: A Scoping Review. Nutrients 2024, 16, 2201. https://doi.org/10.3390/nu16142201
Dhanjani S, Allen H, Varman B, Callender C, Dave JM, Thompson D. Community-Based Participatory Obesity Prevention Interventions in Rural Communities: A Scoping Review. Nutrients. 2024; 16(14):2201. https://doi.org/10.3390/nu16142201
Chicago/Turabian StyleDhanjani, Saagar, Haley Allen, Beatriz Varman, Chishinga Callender, Jayna M. Dave, and Debbe Thompson. 2024. "Community-Based Participatory Obesity Prevention Interventions in Rural Communities: A Scoping Review" Nutrients 16, no. 14: 2201. https://doi.org/10.3390/nu16142201
APA StyleDhanjani, S., Allen, H., Varman, B., Callender, C., Dave, J. M., & Thompson, D. (2024). Community-Based Participatory Obesity Prevention Interventions in Rural Communities: A Scoping Review. Nutrients, 16(14), 2201. https://doi.org/10.3390/nu16142201









