Association between Salt-Related Knowledge, Attitudes, and Behaviours and 24 h Urinary Salt Excretion in Nepal
Highlights
- The average daily salt intake in Nepal was 13.28 g, more than double the WHO's recommended 5 g. Nearly all participants (98%) exceeded this limit.
- Although 83% were aware of the risks of a high salt intake and 87% recognized the need to reduce it, only 10% took steps to control their consumption.
- Self-perceived high salt intake was linked to higher urinary salt levels, frequent addition of extra salt, and processed food consumption, whereas those who were aware of low salt intake were more likely to take actions to reduce salt intake.
- The high salt intake underscores the urgent need for national reduction programs to meet the WHO's target of a 30% reduction in population salt intake by 2025 and to lower hypertension and cardiovascular risks.
- The gap between awareness and action indicates a need for public health efforts that promote practical changes, such as reducing added salt and limiting processed foods.
- Interventions should focus on high-risk groups, including those who perceive their intake as normal or high, using community programs, salt-restriction tools, and healthcare counseling to drive behavior change.
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Sample Size Calculations
2.3. Measurements
2.3.1. Salt-Related Knowledge, Attitudes, and Behaviours
2.3.2. Twenty-Four-Hour Urine Collection
2.3.3. Socio-Demographic Characteristics (Covariates)
2.4. Statistical Analysis
2.5. Ethical Approval
3. Results
3.1. Socio-Demographic Characteristics
3.2. Mean 24 h Urinary Salt Excretion
3.3. Association between Socio-Demographic Characteristics and Salt-Related Knowledge Attitudes and Behaviours (Bivariate Analysis)
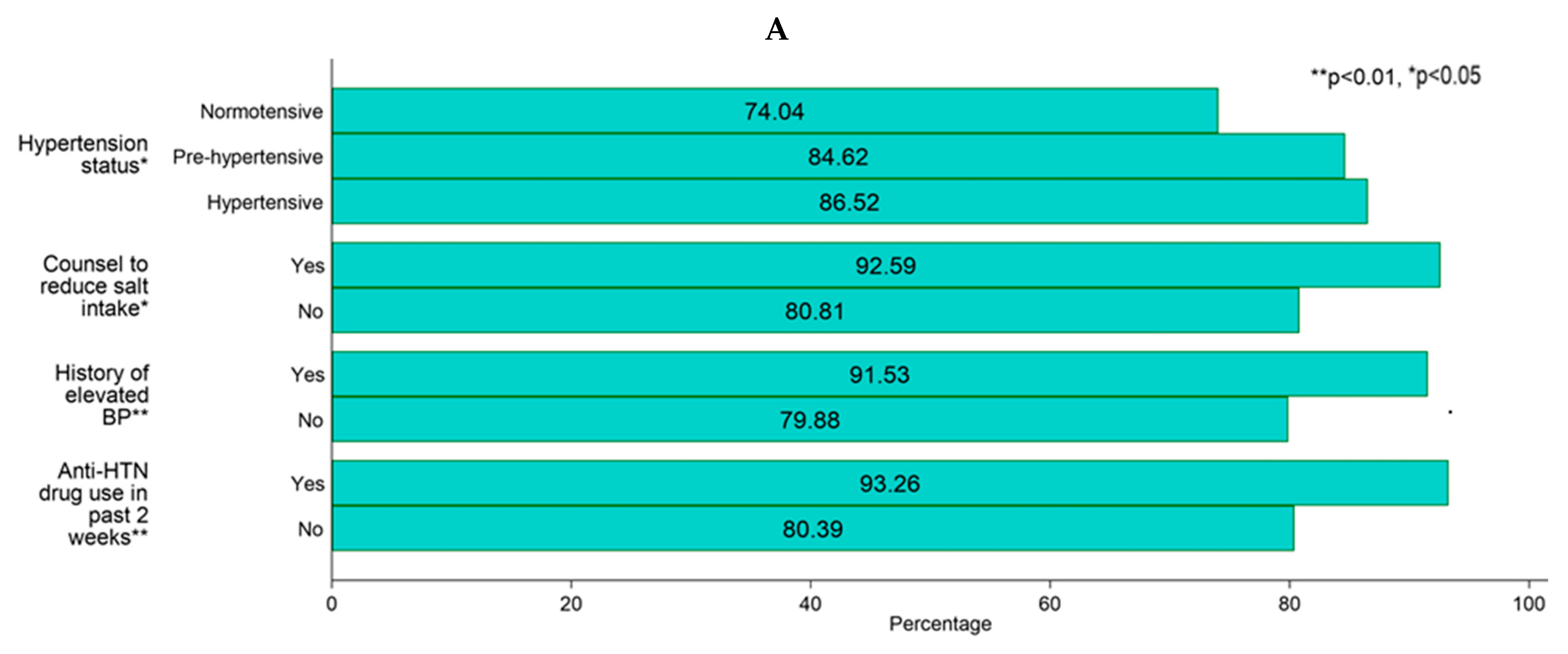
3.3.1. Association with Salt-Related Knowledge and Attitudes
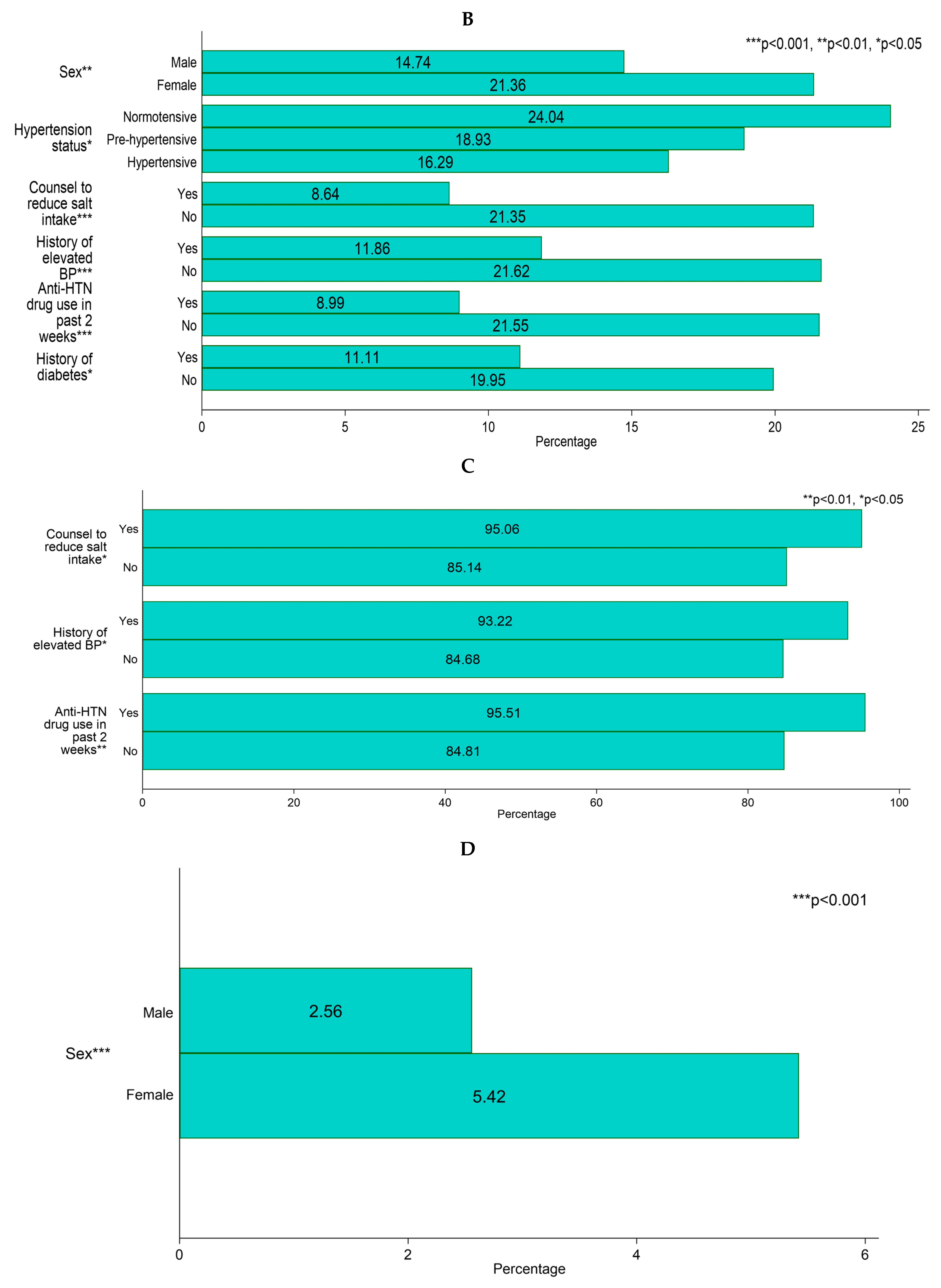
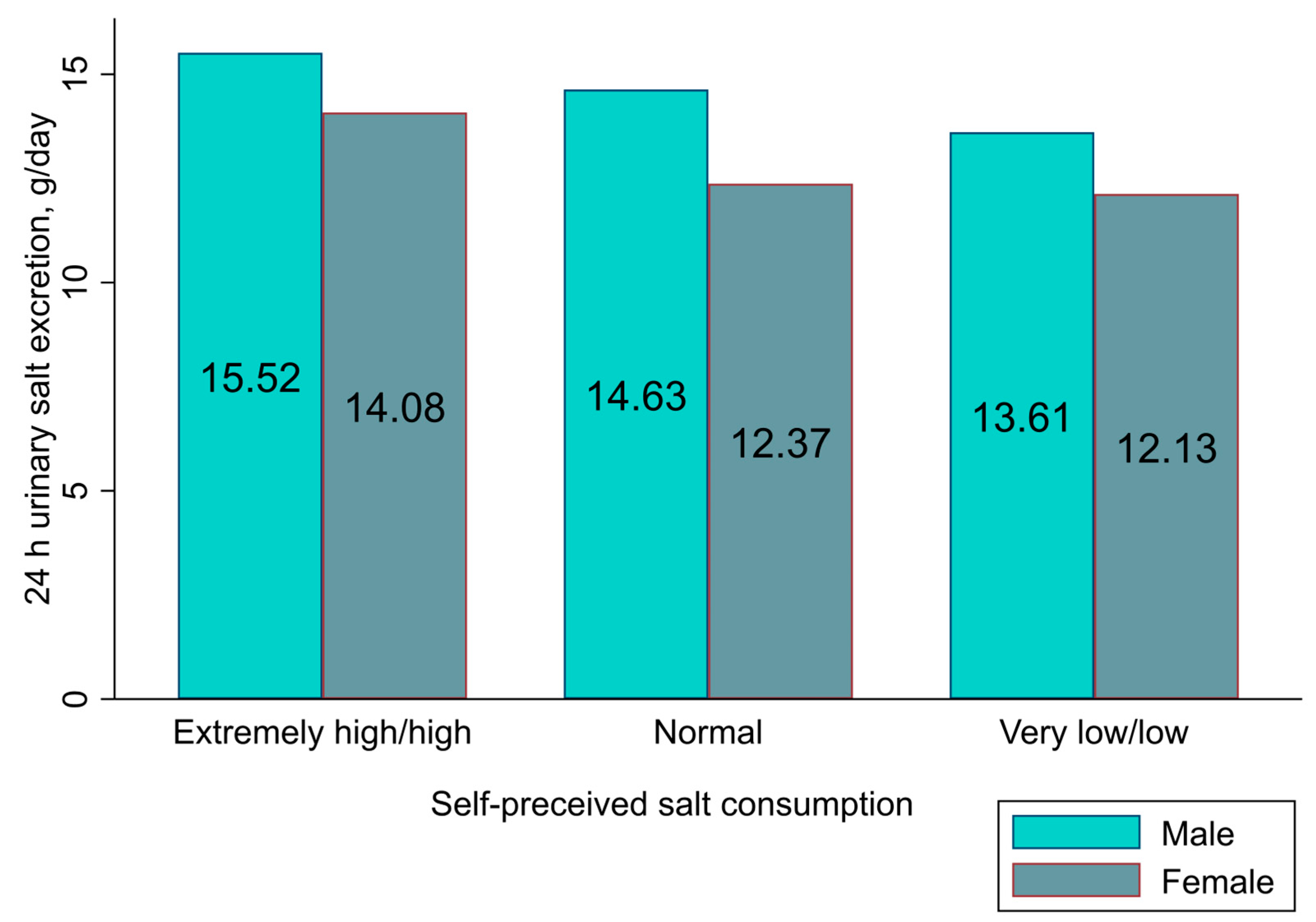
3.3.2. Association with Salt-Related Behaviours
3.4. Association between Socio-Demographic Characteristics and Salt-Related Knowledge, Attitudes, and Salt-Related Behaviours (Logistic Regression)
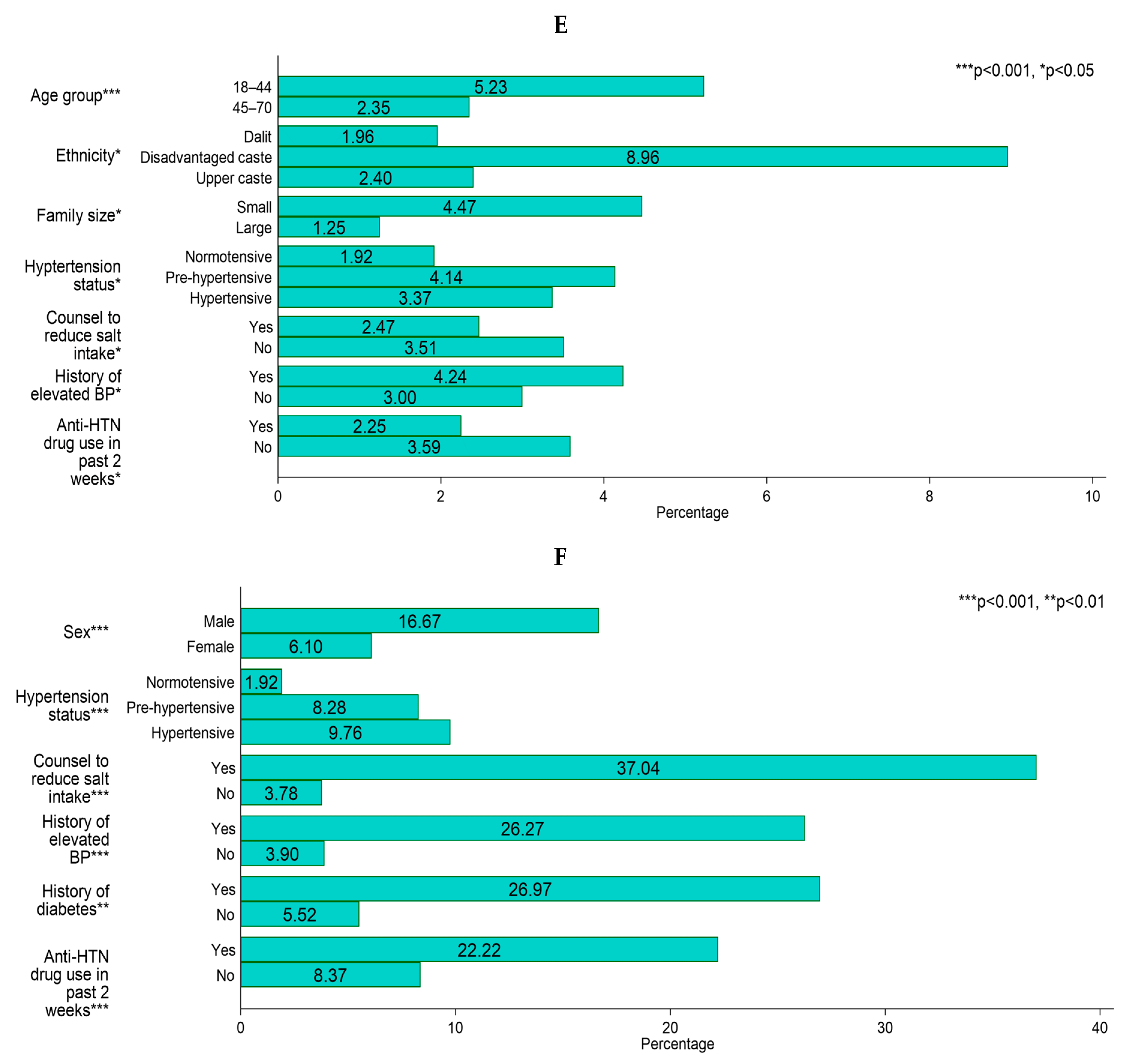
3.5. Association between Salt Related Knowledge, Attitudes, and Behaviours and 24 h Urinary Salt Excretion (General Linear Model)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Guideline: Sodium Intake for Adults and Children; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- The INTERSALT Co-operative Research Group. Intersalt: An international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ 1988, 297, 319–328. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; Li, J.; MacGregor, G.A. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013, 346, f1325. [Google Scholar] [CrossRef] [PubMed]
- Institute for Health Metrics and Evaluation. Country Profile—Nepal. Available online: http://www.healthdata.org/nepal/ (accessed on 11 November 2023).
- World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- Powles, J.; Fahimi, S.; Micha, R.; Khatibzadeh, S.; Shi, P.; Ezzati, M.; Engell, R.E.; Lim, S.S.; Danaei, G.; Mozaffarian, D. Global, regional and national sodium intakes in 1990 and 2010: A systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013, 3, e003733. [Google Scholar] [CrossRef] [PubMed]
- Ghimire, K.; Mishra, S.R.; Satheesh, G.; Neupane, D.; Sharma, A.; Panda, R.; Kallestrup, P.; Mclachlan, C.S. Salt intake and salt-reduction strategies in South Asia: From evidence to action. J. Clin. Hypertens. 2021, 23, 1815–1829. [Google Scholar] [CrossRef]
- Santos, J.A.; Tekle, D.; Rosewarne, E.; Flexner, N.; Cobb, L.; Al-Jawaldeh, A.; Kim, W.J.; Breda, J.; Whiting, S.; Campbell, N. A systematic review of salt reduction initiatives around the world: A midterm evaluation of progress towards the 2025 global non-communicable diseases salt reduction target. Adv. Nutr. 2021, 12, 1768–1780. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Reducing Salt Intake in Populations: Report of a WHO Forum and Technical Meeting, 5–7 October 2006, Paris, France; WHO: Geneva, Switzerland, 2007. [Google Scholar]
- Land, M.-A.; Wu, J.H.; Selwyn, A.; Crino, M.; Woodward, M.; Chalmers, J.; Webster, J.; Nowson, C.; Jeffery, P.; Smith, W. Effects of a community-based salt reduction program in a regional Australian population. BMC Public Health 2016, 16, 388. [Google Scholar] [CrossRef] [PubMed]
- Do, H.T.P.; Santos, J.A.; Trieu, K.; Petersen, K.; Le, M.B.; Lai, D.T.; Bauman, A.; Webster, J. Effectiveness of a Communication for Behavioral Impact (COMBI) intervention to reduce salt intake in a Vietnamese Province based on estimations from spot urine samples. J. Clin. Hypertens. 2016, 18, 1135–1142. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Xu, A.-Q.; Ma, J.-X.; Shi, X.-M.; Guo, X.-L.; Engelgau, M.; Yan, L.-X.; Li, Y.; Li, Y.-C.; Wang, H.-C. Dietary sodium intake: Knowledge, attitudes and practices in Shandong Province, China, 2011. PLoS ONE 2013, 8, e58973. [Google Scholar] [CrossRef] [PubMed]
- Neupane, D.; Rijal, A.; Henry, M.E.; Kallestrup, P.; Koirala, B.; Mclachlan, C.S.; Ghimire, K.; Zhao, D.; Sharma, S.; Pokharel, Y. Mean dietary salt intake in Nepal: A population survey with 24-hour urine collections. J. Clin. Hypertens. 2020, 22, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Ghimire, K.; McLachlan, C.S.; Mishra, S.R.; Kallestrup, P.; Neupane, D. Estimating mean population salt intake using spot urine samples in Nepal: A cross-sectional study. J. Hypertens. 2023, 10, 1097. [Google Scholar] [CrossRef] [PubMed]
- Neupane, D.; McLachlan, C.S.; Christensen, B.; Karki, A.; Perry, H.B.; Kallestrup, P. Community-based intervention for blood pressure reduction in Nepal (COBIN trial): Study protocol for a cluster-randomized controlled trial. Trials 2016, 17, 292. [Google Scholar] [CrossRef] [PubMed]
- National Statistics Office. National Population and Housing Census 2021 (National Report); National Statistics Office: Kathmandu, Nepal, 2023. [Google Scholar]
- Rahi, S. Research design and methods: A systematic review of research paradigms, sampling issues and instruments development. Int. J. Econ. Manag. Sci. 2017, 6, 13901. [Google Scholar] [CrossRef]
- World Health Organization. The WHO STEPwise Approach to Noncommunicable Disease Risk Factor Surveillance (STEPS); World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- National Institutes of Health. Clinical guidelines for the identification, evaluation, and treatment of overweight and obesity in adults-the evidence report. Obes. Res. 1998, 6, 51S–209S. [Google Scholar]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T., Jr. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA 2003, 289, 2560–2571. [Google Scholar] [CrossRef] [PubMed]
- Dhimal, M.; Bista, B.; Bahttarai, S.; Dixit, L.P.; Hyder, M.K.A.; Agrawal, N.; Rani, M.; Jha, A.K. Report of Non-Communicable Disease Risk Factors: STEPS Survey Nepal 2019; Nepal Health Research Council: Kathmandu, Nepal, 2020. [Google Scholar]
- Johnson, C.; Mohan, S.; Rogers, K.; Shivashankar, R.; Thout, S.R.; Gupta, P.; He, F.J.; MacGregor, G.A.; Webster, J.; Krishnan, A. The association of knowledge and behaviours related to salt with 24-h urinary salt excretion in a population from North and South India. Nutrients 2017, 9, 144. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; Fang, L.; Xu, J.; Chen, X.; Bai, Y.; Wu, J.; Wu, L.; Zhong, J. The association of knowledge, attitudes and behaviors related to salt with 24-h urinary sodium, potassium excretion and hypertensive status. Sci. Rep. 2022, 12, 13901. [Google Scholar] [CrossRef] [PubMed]
- Cheong, S.M.; Ambak, R.; Othman, F.; He, F.J.; Salleh, R.; Mohd Sallehudin, S.; Palaniveloo, L.; Ganapathy, S.S. Knowledge, perception, and practice related to sodium intake among Malaysian adults: Findings from the Malaysian Community Salt Study (MyCoSS). J. Health Popul. Nutr. 2021, 40, 5. [Google Scholar] [CrossRef] [PubMed]
- Jarrar, A.H.; Stojanovska, L.; Apostolopoulos, V.; Cheikh Ismail, L.; Feehan, J.; Ohuma, E.O.; Ahmad, A.Z.; Alnoaimi, A.A.; Al Khaili, L.S.; Allowch, N.H. Assessment of sodium knowledge and urinary sodium excretion among regions of the united arab emirates: A cross-sectional study. Nutrients 2020, 12, 2747. [Google Scholar] [CrossRef] [PubMed]
- Land, M.-A.; Webster, J.; Christoforou, A.; Johnson, C.; Trevena, H.; Hodgins, F.; Chalmers, J.; Woodward, M.; Barzi, F.; Smith, W. The association of knowledge, attitudes and behaviours related to salt with 24-hour urinary sodium excretion. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 47. [Google Scholar] [CrossRef] [PubMed]
- Webster, J.; Su’a, S.A.F.; Ieremia, M.; Bompoint, S.; Johnson, C.; Faeamani, G.; Vaiaso, M.; Snowdon, W.; Land, M.A.; Trieu, K. Salt intakes, knowledge, and behavior in Samoa: Monitoring salt-consumption patterns through the World Health Organization’s Surveillance of Noncommunicable Disease Risk Factors (STEPS). J. Clin. Hypertens. 2016, 18, 884–891. [Google Scholar] [CrossRef] [PubMed]
- Saje, S.M.; Endris, B.S.; Nagasa, B.; Ashebir, G.; Gebreyesus, S.H. Dietary sodium and potassium intake: Knowledge, attitude and behaviour towards dietary salt intake among adults in Addis Ababa, Ethiopia. Public Health Nutr. 2021, 24, 3451–3459. [Google Scholar] [CrossRef] [PubMed]
- Claro, R.M.; Linders, H.; Ricardo, C.Z.; Legetic, B.; Campbell, N.R. Consumer attitudes, knowledge, and behavior related to salt consumption in sentinel countries of the Americas. Rev. Panam. Salud Pública 2012, 32, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Alawwa, I.; Dagash, R.; Saleh, A.; Ahmad, A. Dietary salt consumption and the knowledge, attitudes and behavior of healthy adults: A cross-sectional study from Jordan. Libyan J. Med. 2018, 13, 1479602. [Google Scholar] [CrossRef]
- Mahat, D.; Isa, Z.M.; Tamil, A.M.; Mahmood, M.I.; Othman, F.; Ambak, R. The association of knowledge, attitude and practice with 24 hours urinary sodium excretion among Malay healthcare staff in Malaysia. Int. J. Public Health Res. 2017, 7, 860–870. [Google Scholar]
- Fan, F.; Li, Y.; Li, L.; Nie, X.; Zhang, P.; Li, Y.; Luo, R.; Zhang, G.; Wang, L.; He, F.J. Salt-Related Knowledge, Attitudes, and Behaviors and Their Relationship with 24-Hour Urinary Sodium Excretion in Chinese Adults. Nutrients 2022, 14, 4404. [Google Scholar] [CrossRef] [PubMed]
- Variyam, J.N.; Shim, Y.; Blaylock, J. Consumer misperceptions of diet quality. J. Nutr. Educ. 2001, 33, 314–321. [Google Scholar] [CrossRef]
- Baranowski, T.; Perry, C.L.; Parcel, G.S. How individuals, environments, and health behavior interact. Health Behav. Health Educ. Theory Res. Pract. 2002, 3, 165–184. [Google Scholar]
- Patel, D.; Cogswell, M.E.; John, K.; Creel, S.; Ayala, C. Knowledge, attitudes, and behaviors related to sodium intake and reduction among adult consumers in the United States. Am. J. Health Promot. 2017, 31, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Nasreddine, L.; Akl, C.; Al-Shaar, L.; Almedawar, M.M.; Isma’eel, H. Consumer knowledge, attitudes and salt-related behavior in the Middle-East: The case of Lebanon. Nutrients 2014, 6, 5079–5102. [Google Scholar] [CrossRef] [PubMed]
- Treciokiene, I.; Postma, M.; Nguyen, T.; Fens, T.; Petkevicius, J.; Kubilius, R.; Gulbinovic, J.; Taxis, K. Healthcare professional-led interventions on lifestyle modifications for hypertensive patients–a systematic review and meta-analysis. BMC Fam. Pract. 2021, 22, 63. [Google Scholar] [CrossRef] [PubMed]
- Greaves, C.J.; Sheppard, K.E.; Abraham, C.; Hardeman, W.; Roden, M.; Evans, P.H.; Schwarz, P. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health 2011, 11, 119. [Google Scholar] [CrossRef] [PubMed]
- Sarmugam, R.; Worsley, A.; Wang, W. An examination of the mediating role of salt knowledge and beliefs on the relationship between socio-demographic factors and discretionary salt use: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 25. [Google Scholar] [CrossRef]
- Brown, I.J.; Tzoulaki, I.; Candeias, V.; Elliott, P. Salt intakes around the world: Implications for public health. Int. J. Epidemiol. 2009, 38, 791–813. [Google Scholar] [CrossRef] [PubMed]
- Ghimire, K.; Adhikari, T.B.; Rijal, A.; Kallestrup, P.; Henry, M.E.; Neupane, D. Knowledge, attitudes, and practices related to salt consumption in Nepal: Findings from the community-based management of non-communicable diseases project in Nepal (COBIN). J. Clin. Hypertens. 2019, 21, 739–748. [Google Scholar] [CrossRef] [PubMed]
- Shao, S.; Hua, Y.; Yang, Y.; Liu, X.; Fan, J.; Zhang, A.; Xiang, J.; Li, M.; Yan, L.L. Salt reduction in China: A state-of-the-art review. Risk Manag. Healthc. Policy 2017, 10, 17. [Google Scholar] [CrossRef] [PubMed]
- Li, K.-C.; Huang, L.; Tian, M.; Di Tanna, G.L.; Yu, J.; Zhang, X.; Yin, X.; Liu, Y.; Hao, Z.; Zhou, B. Cost-Effectiveness of a Household Salt Substitution Intervention: Findings From 20 995 Participants of the Salt Substitute and Stroke Study. Circulation 2022, 145, 1534–1541. [Google Scholar] [CrossRef] [PubMed]
- Ide, N.; Ajenikoko, A.; Steele, L.; Cohn, J.; Curtis, C.; Frieden, T.R.; Cobb, L.K. Priority actions to advance population sodium reduction. Nutrients 2020, 12, 2543. [Google Scholar] [CrossRef] [PubMed]
- Hyseni, L.; Elliot-Green, A.; Lloyd-Williams, F.; Kypridemos, C.; O’Flaherty, M.; McGill, R.; Orton, L.; Bromley, H.; Cappuccio, F.P.; Capewell, S. Systematic review of dietary salt reduction policies: Evidence for an effectiveness hierarchy? PLoS ONE 2017, 12, e0177535. [Google Scholar] [CrossRef] [PubMed]
- McLaren, L.; Sumar, N.; Barberio, A.M.; Trieu, K.; Lorenzetti, D.L.; Tarasuk, V.; Webster, J.; Campbell, N.R. Population-level interventions in government jurisdictions for dietary sodium reduction. Cochrane Database Syst. Rev. 2016, 9, CD010166. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Potassium Intake for Adults and Children; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Jafar, T.H.; Islam, M.; Hatcher, J.; Hashmi, S.; Bux, R.; Khan, A.; Poulter, N.; Badruddin, S.; Chaturvedi, N. Community based lifestyle intervention for blood pressure reduction in children and young adults in developing country: Cluster randomised controlled trial. BMJ 2010, 340, c2641. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Kerry, S.M.; Micah, F.B.; Plange-Rhule, J.; Eastwood, J.B. A community programme to reduce salt intake and blood pressure in Ghana [ISRCTN88789643]. BMC Public Health 2006, 6, 13. [Google Scholar] [CrossRef] [PubMed]
- Neupane, D.; McLachlan, C.S.; Mishra, S.R.; Olsen, M.H.; Perry, H.B.; Karki, A.; Kallestrup, P. Effectiveness of a lifestyle intervention led by female community health volunteers versus usual care in blood pressure reduction (COBIN): An open-label, cluster-randomised trial. Lancet Glob. Health 2018, 6, e66–e73. [Google Scholar] [CrossRef] [PubMed]
- Wyness, L.A.; Butriss, J.L.; Stanner, S.A. Reducing the population’s sodium intake: The UK Food Standards Agency’s salt reduction programme. Public Health Nutr. 2012, 15, 254–261. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Mean or (n) | SD or (%) |
|---|---|---|
| Age (years) | 49.60 | 9.82 |
| Weight (kg) | 63.70 | 11.59 |
| Height (cm) | 156.03 | (8.2 |
| BMI (kg/m2) | 26.15 | 428 |
| Systolic blood pressure (mm Hg) | 129.06 | 18.03 |
| Diastolic blood pressure (mm Hg) | 83.37 | 10.26 |
| Hypertension | (178) | (39.47) |
| Diabetes (self-reported) | (45) | (10.90) |
| 24 h urine | ||
| Sodium (g/day) | 5.31 | 1.89 |
| Potassium (g/day) | 1.94 | 0.77 |
| Creatinine (mg/day) | 1232.77 | 524.94 |
| Sodium-to-potassium ratio | 5.04 | 2.04 |
| Urine volume (mL/day) | 2584.03 | 1100.14 |
| Salt excretion, g/day | 13.28 | 4.72 |
| Proportion with ≥5 g/day | (441) | (97.78) |
| Characteristics | Total, n (%) | Mean (±SD) Salt Intake (g/day) * | Proportion of Participants with Salt-Related Knowledge and Attitudes (%) * | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Knowledge | Attitudes | ||||||||
| High Salt Intake Causes Health Problems | Self-Perceived Salt Intake | Importance of Lowering Salt Intake | |||||||
| Yes | No † | Extremely High/ High | Normal | Very Low/ Low | Very Important/ Somewhat Important | Not Important ¶ | |||
| Age, years | |||||||||
| 18–44 | 153 (33.92) | 14.34 (4.91) | 86.93 | 13.07 | 22.88 | 57.52 | 19.61 | 86.93 | 13.07 |
| 45–70 | 298 (66.08) | 12.73 (4.53) | 80.87 | 19.13 | 17.11 | 53.69 | 29.19 | 86.91 | 13.09 |
| p-value | <0.01 | 0.10 | 0.06 | 0.10 | |||||
| Sex | |||||||||
| Male | 156 (34.59) | 14.40 (5.06) | 84.62 | 15.38 | 14.74 | 50 | 35.26 | 89.10 | 10.90 |
| Female | 295 (65.41) | 12.69 (4.43) | 82.03 | 17.97 | 21.36 | 57.63 | 21.02 | 85.76 | 14.24 |
| p-value | <0.01 | 0.49 | <0.01 | 0.32 | |||||
| Ethnicity | |||||||||
| Dalit | 51 (11.31) | 12.90 (5.45) | 76.47 | 23.53 | 19.61 | 45.10 | 35.29 | 84.31 | 15.69 |
| Disadvantaged caste | 67 (14.86) | 13.12 (5.04) | 80.60 | 19.40 | 22.39 | 62.69 | 14.93 | 83.58 | 16.42 |
| Upper caste | 333 (73.84) | 13.37 (4.54) | 84.38 | 15.62 | 18.32 | 54.95 | 26.73 | 87.99 | 12.01 |
| p-value | 0.76 | 0.32 | 0.13 | 0.52 | |||||
| Highest education | |||||||||
| Primary level | 265 (58.76) | 12.70 (4.74) | 79.62 | 20.38 | 20 | 56.98 | 23.02 | 85.28 | 14.72 |
| Higher secondary level | 158 (35.03) | 14.12 (4.78) | 87.97 | 12.03 | 18.99 | 53.16 | 27.85 | 88.61 | 11.39 |
| University level | 28 (6.21) | 14.08 (3.16) | 85.71 | 14.29 | 10.71 | 46.43 | 42.86 | 92.86 | 7.14 |
| p-value | <0.01 | 0.08 | 0.20 | 0.45 | |||||
| BMI | |||||||||
| Underweight | 17 (3.78) | 12.64 (4.26) | 82.35 | 17.65 | 11.76 | 47.06 | 41.18 | 88.24 | 11.76 |
| Normal | 159 (35.33) | 12.82 (4.50) | 82.39 | 17.61 | 20.13 | 57.86 | 22.01 | 86.16 | 13.84 |
| Overweight | 192 (42.67) | 13.42 (4.61) | 84.90 | 15.10 | 17.19 | 52.60 | 30.21 | 89.58 | 10.42 |
| Obese | 82 (18.22) | 13.86 (5.34) | 80.49 | 19.51 | 23.17 | 56.10 | 20.73 | 82.93 | 17.07 |
| p-value | 0.36 | 0.79 | 0.34 | 0.47 | |||||
| Family size | |||||||||
| Small (≤4 people) | 291 (64.52) | 13.02 (4.67) | 82.13 | 17.87 | 19.93 | 55.67 | 24.40 | 85.22 | 14.78 |
| Large (>4 people) | 160 (35.48) | 13.76 (4.78) | 84.38 | 15.63 | 17.50 | 53.75 | 28.75 | 90 | 10 |
| p-value | 0.11 | 0.54 | 0.57 | 0.15 | |||||
| HTN status | |||||||||
| Normotensive | 104 (23.06) | 13.39 (4.81) | 74.04 | 25.96 | 24.04 | 61.54 | 14.42 | 79.81 | 20.19 |
| Pre-hypertensive | 169 (37.47) | 13.17 (4.59) | 84.62 | 15.38 | 18.93 | 57.99 | 23.08 | 88.76 | 11.24 |
| Hypertensive | 178 (39.47) | 13.32 (4.81) | 86.52 | 13.48 | 16.29 | 48.31 | 35.39 | 89.33 | 10.67 |
| p-value | 0.92 | <0.05 | <0.05 | 0.05 | |||||
| Counsel to reduce dietary salt | |||||||||
| Yes | 81 (17.96) | 13.20 (5.08) | 92.59 | 7.41 | 8.64 | 43.21 | 48.15 | 95.06 | 4.94 |
| No | 370 (82.04) | 13.30 (4.64) | 80.81 | 19.19 | 21.35 | 57.57 | 21.08 | 85.14 | 14.86 |
| p-value | 0.87 | <0.05 | <0.001 | <0.05 | |||||
| History of elevated BP | |||||||||
| Yes | 118 (26.16) | 13.25 (4.87) | 91.53 | 8.47 | 11.86 | 44.07 | 44.07 | 93.22 | 6.78 |
| No | 333 (73.84) | 13.29 (4.67) | 79.88 | 20.12 | 21.62 | 58.86 | 19.52 | 84.68 | 15.32 |
| p-value | 0.94 | <0.01 | <0.001 | <0.05 | |||||
| Anti-HTN drug use in the past 2 weeks | |||||||||
| Yes | 89 (19.73) | 12.99 (4.42) | 93.26 | 6.74 | 8.99 | 43.82 | 47.19 | 95.51 | 4.49 |
| No | 362 (80.27) | 13.35 (4.79) | 80.39 | 19.61 | 21.55 | 57.73 | 20.72 | 84.81 | 15.19 |
| p-value | 0.5120 | <0.01 | <0.001 | <0.01 | |||||
| History of diabetes | |||||||||
| Yes | 45 (10.90) | 13.71 (3.82) | 91.11 | 8.89 | 11.11 | 43.90 | 44.44 | 93.33 | 6.67 |
| No | 368 (89.10) | 13.27 (4.74) | 82.61 | 20.11 | 19.76 | 55.16 | 24.73 | 86.41 | 13.59 |
| p-value | 0.55 | 0.20 | <0.05 | 0.24 | |||||
| Characteristics | Proportion of Participants with Salt-Related Behaviours (%) * | |||||||
|---|---|---|---|---|---|---|---|---|
| Add Extra Salt | Processed Food Consumption | Take Actions to Control Salt | ||||||
| Always/Often | Sometimes | Rarely/Never | Always/Often | Sometimes | Rarely/Never | Yes | No | |
| Age, years | ||||||||
| 18–44 | 6.54 | 19.61 | 73.86 | 5.23 | 64.05 | 30.72 | 6.54 | 93.46 |
| 45–70 | 3.36 | 17.79 | 78.86 | 2.35 | 44.63 | 53.02 | 11.41 | 88.59 |
| p-value | 0.25 | <0.001 | 0.10 | |||||
| Sex | ||||||||
| Male | 2.56 | 9.62 | 87.82 | 2.56 | 45.51 | 51.92 | 16.67 | 83.33 |
| Female | 5.42 | 23.05 | 71.53 | 3.73 | 54.24 | 42.03 | 6.10 | 93.90 |
| p-value | <0.001 | 0.13 | <0.001 | |||||
| Ethnicity | ||||||||
| Dalit | 7.84 | 19.61 | 72.55 | 1.96 | 54.90 | 43.14 | 15.69 | 84.31 |
| Disadvantaged caste | 2.99 | 28.36 | 68.66 | 8.96 | 59.70 | 31.34 | 10.45 | 89.55 |
| Upper caste | 4.20 | 16.22 | 79.58 | 2.40 | 48.95 | 48.65 | 8.71 | 91.29 |
| p-value | 0.12 | <0.05 | 0.29 | |||||
| Highest education | ||||||||
| Primary level | 4.91 | 20.38 | 74.72 | 3.40 | 49.06 | 47.55 | 9.43 | 90.57 |
| Higher secondary level | 3.80 | 17.72 | 78.48 | 3.80 | 56.33 | 39.87 | 10.13 | 89.87 |
| University level | 3.57 | 3.57 | 92.86 | 0 | 42.86 | 57.14 | 10.71 | 89.29 |
| p-value | 0.20 | 0.37 | 0.90 | |||||
| BMI | ||||||||
| Underweight | 0 | 17.65 | 82.35 | 0 | 29.41 | 70.59 | 23.53 | 76.47 |
| Normal | 4.40 | 20.75 | 74.84 | 1.89 | 52.83 | 45.28 | 8.18 | 91.82 |
| Overweight | 3.65 | 18.23 | 78.13 | 3.13 | 52.08 | 44.79 | 11.46 | 88.54 |
| Obese | 7.32 | 14.63 | 78.05 | 7.32 | 51.22 | 41.46 | 6.10 | 93.90 |
| p-value | 0.77 | 0.18 | 0.11 | |||||
| Family size | ||||||||
| Small (≤ four people) | 4.12 | 19.59 | 76.29 | 4.47 | 46.74 | 48.80 | 9.62 | 90.38 |
| Large (>four people) | 5 | 16.25 | 78.75 | 1.25 | 59.38 | 39.38 | 10 | 90 |
| p-value | 0.66 | <0.05 | 0.90 | |||||
| HTN status | ||||||||
| Normotensive | 6.73 | 19.23 | 74.04 | 1.92 | 60.58 | 37.50 | 1.92 | 98.08 |
| Pre-hypertensive | 4.14 | 21.89 | 73.96 | 4.14 | 54.44 | 41.42 | 8.28 | 91.72 |
| Hypertensive | 3.37 | 14.61 | 82.02 | 3.37 | 42.70 | 53.93 | 9.76 | 90.24 |
| p-value | 0.26 | <0.05 | <0.001 | |||||
| Counsel to reduce dietary salt | ||||||||
| Yes | 3.70 | 9.88 | 86.42 | 2.47 | 37.04 | 60.49 | 37.04 | 62.96 |
| No | 4.59 | 20.27 | 75.14 | 3.51 | 54.32 | 42.16 | 3.78 | 96.22 |
| p-value | 0.07 | <0.05 | <0.001 | |||||
| History of elevated BP | ||||||||
| Yes | 2.54 | 12.71 | 84.75 | 4.24 | 40.68 | 55.08 | 26.27 | 73.73 |
| No | 5.11 | 20.42 | 74.47 | 3 | 54.95 | 42.04 | 3.90 | 96.10 |
| p-value | 0.08 | <0.05 | <0.001 | |||||
| Anti-HTN drug use in past 2 weeks | ||||||||
| Yes | 3.37 | 10.11 | 86.52 | 2.25 | 39.33 | 58.43 | 26.97 | 73.03 |
| No | 4.70 | 20.44 | 74.86 | 3.59 | 54.14 | 42.27 | 5.52 | 94.48 |
| p-value | 0.054 | <0.05 | <0.001 | |||||
| History of diabetes | ||||||||
| Yes | 0 | 17.78 | 82.22 | 2.22 | 37.78 | 60 | 22.22 | 77.78 |
| No | 4.62 | 17.93 | 77.45 | 3.80 | 54.08 | 42.12 | 8.15 | 91.85 |
| p-value | 0.44 | 0.07 | <0.01 | |||||
| Salt-Related Knowledge and Attitudes | Salt-Related Behaviours † | |||||
|---|---|---|---|---|---|---|
| Adding Extra Salt Always a | Consuming Processed Food Always a | Taking Actions to Control Salt ¥ | ||||
| AOR † | 95% CI | AOR † | 95% CI | AOR † | 95% CI | |
| High salt intake causes health problems | ||||||
| No b | 1.00 (Ref.) | |||||
| Yes | 0.60 | 0.33, 1.09 | 1.73 | 0.99, 3.02 | 3.19 | 0.65, 15.70 |
| Self-perceived salt consumption ¥ | ||||||
| Normal | 1.00 (Ref.) | |||||
| Very low/low | 0.47 | 0.22, 1.01 | 0.60 | 0.36, 0.98 * | 4.22 | 1.90, 9.37 *** |
| Extremely high/high c | 3.59 | 2.03, 6.33 *** | 1.90 | 1.06, 3.40 * | 0.14 | 0.01, 2.58 |
| Importance of lowering salt intake | ||||||
| Not important d | 1.00 (Ref.) | |||||
| Very Important/somewhat important | 1.06 | 0.53, 2.14 | 1.61 | 0.87, 2.97 | 5.44 | 0.60, 49.19 |
| Salt-Related KAB | n (%) | Adjusted Estimate † | ||
|---|---|---|---|---|
| Mean Salt Intake (g/day) | 95% CI | p-Value | ||
| Knowledge | ||||
| High salt intake causes health problems | ||||
| Yes | 374 (82.93) | 13.28 | 12.82, 13.75 | 0.78 |
| No a | 77 (17.07) | 13.14 | 12.11, 14.17 | |
| Attitudes | ||||
| Self-perceived salt consumption | ||||
| Extremely high/high | 86 (19.07) | 14.42 | 13.45, 15.39 | 0.03 * |
| Normal | 248 (54.99) | 13.11 | 12.54, 13.67 | |
| Very low/low | 117 (25.94) | 12.73 | 11.89, 13.65 | |
| Importance of lowering salt intake | ||||
| Very important/somewhat important | 392 (86.92) | 13.33 | 12.87, 13.78 | 0.42 |
| Not important b | 59 (13.08) | 12.81 | 11.63, 13.99 | |
| Behaviours | ||||
| Add extra salt | ||||
| Always/often | 20 (4.43) | 14.67 | 12.66, 16.68 | 0.36 |
| Sometimes | 83 (18.40) | 13.00 | 12.31, 14.30 | |
| Rarely/never | 348 (77.16) | 13.17 | 12.69, 13.65 | |
| Processed food consumption | ||||
| Always/often | 15 (3.33) | 14.57 | 12.23, 16.91 | 0.53 |
| Sometimes | 231 (51.22) | 13.23 | 12.64, 13.83 | |
| Rarely/never | 205 (45.45) | 13.19 | 12.55, 13.83 | |
| Take actions to control salt intake | ||||
| Yes | 44 (9.76) | 13.51 | 12.15, 14.89 | 0.70 |
| No | 407 (90.24) | 13.23 | 12.79, 13.67 | |
| If yes, what are theyc(n = 44)? | ||||
| Avoid eating processed foods | ||||
| Yes | 14 (31.82) | 13.88 | 10.37, 17.39 | 0.88 |
| No | 30 (68.18) | 13.53 | 11.30, 15.76 | |
| Check salt/sodium labelling on food | ||||
| Yes | 11 (25) | 15.61 | 11.83, 19.39 | 0.25 |
| No | 33 (75) | 12.99 | 10.97, 15.01 | |
| Buy low-salt/sodium alternatives | ||||
| Yes | 1 (2.27) | 12.72 | 0.60, 24.85 | 0.88 |
| No | 43 (97.73) | 13.67 | 11.94, 15.40 | |
| Avoid out-of-home dinning | ||||
| Yes | 9 (20.45) | 16.25 | 12.06, 20.43 | 0.18 |
| No | 35 (79.55) | 12.98 | 11.04, 14.91 | |
| Avoid adding extra salt | ||||
| Yes | 36 (81.82) | 14.10 | 12.18, 16.02 | 0.33 |
| No | 8 (18.18) | 11.60 | 7.09, 16.10 | |
| Use small spoon | ||||
| Yes | 10 (22.73) | 15.83 | 11.93, 19.73 | 0.22 |
| No | 34 (77.27) | 13.00 | 11.03, 14.97 | |
| Apply other measures | ||||
| Yes | 9 (20.45) | 11.76 | 7.65, 15.86 | 0.31 |
| No | 35 (79.55) | 14.13 | 12.19, 16.07 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghimire, K.; Mishra, S.R.; Neupane, D.; Kallestrup, P.; McLachlan, C.S. Association between Salt-Related Knowledge, Attitudes, and Behaviours and 24 h Urinary Salt Excretion in Nepal. Nutrients 2024, 16, 1928. https://doi.org/10.3390/nu16121928
Ghimire K, Mishra SR, Neupane D, Kallestrup P, McLachlan CS. Association between Salt-Related Knowledge, Attitudes, and Behaviours and 24 h Urinary Salt Excretion in Nepal. Nutrients. 2024; 16(12):1928. https://doi.org/10.3390/nu16121928
Chicago/Turabian StyleGhimire, Kamal, Shiva Raj Mishra, Dinesh Neupane, Per Kallestrup, and Craig S. McLachlan. 2024. "Association between Salt-Related Knowledge, Attitudes, and Behaviours and 24 h Urinary Salt Excretion in Nepal" Nutrients 16, no. 12: 1928. https://doi.org/10.3390/nu16121928
APA StyleGhimire, K., Mishra, S. R., Neupane, D., Kallestrup, P., & McLachlan, C. S. (2024). Association between Salt-Related Knowledge, Attitudes, and Behaviours and 24 h Urinary Salt Excretion in Nepal. Nutrients, 16(12), 1928. https://doi.org/10.3390/nu16121928






