Abstract
The systematic review and meta-analysis were conducted to ascertain the prevalence of anemia, iron deficiency (ID), and iron deficiency anemia (IDA) among Chinese pregnant women. A total of 722 articles on maternal anemia during pregnancy published between January 2010 and December 2020 were compiled, and a systematic review and meta-analysis were conducted on 57 eligible studies including 1,376,204 pregnant women to ascertain the prevalence of anemia and the prevalence in different subgroups. The results showed that the prevalence of anemia, ID, and IDA among pregnant women in China were 30.7% (95% CI: 26.6%, 34.7%), 45.6% (95% CI: 37.0%, 54.2%), and 17.3% (95% CI: 13.9%, 20.7%), respectively. All prevalence increased with the progression of the pregnancy. There were sizable regional variations in the prevalence of anemia, ID, and IDA. Generally, lower prevalence was observed in the economically more advanced eastern region of the country, while the prevalence of ID was higher in the eastern region than that in the western region. The prevalence of anemia and IDA in rural areas was higher than that in urban areas, but ID prevalence was higher in urban areas. In conclusion, the regional differences and urban–rural disparities in the prevalence of anemia indicate the need for more context-specific interventions to prevent and treat anemia. It was found that dietary factors were one of the major causes of anemia, and iron-containing supplements and nutrition counseling could be effective interventions to reduce the prevalence of anemia, ID, and IDA among Chinese pregnant women.
1. Introduction
Anemia is a condition in which the volume of red blood cells in the peripheral circulation is lower than the normal range, obstructing adequate oxygen from being transported to tissues, thus obstructing the normal physiological functions of the body. Anemia significantly affects population health, impairs physical and cognitive growth, and eventually impacts socioeconomic development. It is a serious public health problem globally, especially in low- and middle-income countries [1].
About a quarter of the world’s population suffers from anemia. Children and women, especially pregnant women, are at higher risk [2,3]. Based on different causes, anemia can be classified into three types: nutritional anemia, disease-related anemia, and anemia caused by genetic factors [4]. The deficiency in iron, folate, vitamin B12, vitamin A, vitamin C, and other nutrients can cause nutritional anemia, and it is common in low- and middle-income countries [5]. Iron deficiency (ID) is one of the main causes of anemia, accounting for about 50% of all anemic cases [6]. The occurrence of ID and iron deficiency anemia (IDA) can be affected by geographical, cultural, dietary, and economic factors, as well as genetic factors (e.g., single-nucleotide polymorphisms of gene TMPRSS6) [7,8]. IDA during pregnancy is associated with adverse health outcomes for both mothers and babies, including premature delivery, infants who are small for gestational age, low birth weight, or even perinatal death [5,9,10]. The common prevention and treatment of ID and IDA during pregnancy include iron-containing supplements, medicines, and nutrition counseling on dietary practices [2,11,12].
In China, some national surveys, routine data reporting systems, and research studies [13,14,15] have assessed the prevalence of anemia among pregnant women in recent years. However, the published data have been inconsistent. Many of the studies were conducted within confined geographical areas, some had small sample sizes or data collected from population-based cross-sectional surveys or management information systems of health facilities, and others did not report data on anemia rates in different trimesters. In this paper, the objective is to conduct a systematic review and meta-analysis using data derived from available studies to establish the prevalence and pattern of ID and IDA among pregnant women across China, in order to inform and facilitate the design and implementation of targeted interventions.
2. Methods
The systematic review and meta-analysis were conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Figure 1). Two researchers independently searched through English databases (Medline, PubMed, Embase, Web of Science, and Science Direct) and Chinese databases (China National Knowledge Infrastructure, Wanfang, and Chongqing VIP). Relevant studies published between 1 January 2010 and 31 December 2020 were gathered using a combination of Medical Subject Headings (MeSH) and free-text terms including the following: (anemia OR hemoglobin) AND (pregnancy OR maternal OR pregnant OR perinatal OR prenatal) AND (Chinese OR china) AND (prevalence OR epidemiology). The review was not registered, and no protocol was prepared.
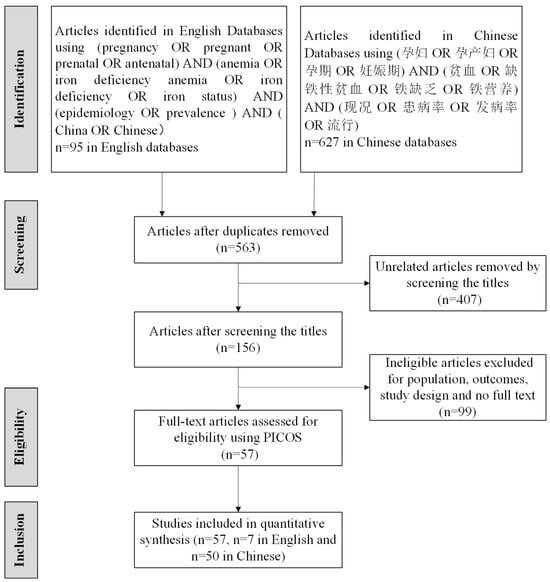
Figure 1.
PRISMA flow diagram. 孕妇: pregnant women; 孕产妇: pregnant and maternity women; 孕期 or 妊娠期: pregnancy; 贫血: anemia; 缺铁性贫血: iron deficiency anemia; 铁缺乏: iron deficiency; 铁营养: iron nutrition status; 现况OR患病率 OR 流行: prevalence; 发病率: incidence.
2.1. Search Strategy and Selection Criteria
Criteria of inclusion and exclusion were applied to the selection of articles; please see Participant, Intervention, Comparison, Outcome Study (PICOs) in Table 1. Two researchers independently reviewed the titles, abstracts, and the full text to exclude studies that did not meet the inclusion criteria. The detailed screening process of articles is shown in Figure 1.

Table 1.
The inclusion and exclusion criteria for article selection.
2.2. Primary Outcome
The primary outcomes were the prevalence of anemia, ID, and IDA. The WHO diagnostic criteria of anemia among pregnant women were applied: anemia was defined as a hemoglobin (Hb) level of less than 110 g/L [16], with mild anemia ranging between an Hb level of 100 and 109 g/L, moderate anemia ranging between an Hb level of 70 and 99 g/L, and severe anemia defined as an Hb level of less than 70 g/L [10]. For the diagnosis of ID among pregnant women, the cutoff recommended in the Diagnosis and Treatment of Iron Deficiency and Iron Deficiency Anemia in Pregnancy issued by the Perinatal Branch of the Chinese Medical Association in 2014 was applied: serum ferritin (SF) of less than 20 µg/L. IDA was defined as an Hb level of less than 110 g/L and an SF value of less than 20 µg/L [17].
2.3. Quality Assessment and Data Collection
Two researchers independently extracted and reviewed the data from all the selected articles (Table S1), including the authors, year of publication, year of investigation, study location, economic condition of the study location, study design, sampling strategies, sample size, diagnostic criteria of anemia, ID and IDA, prevalence of anemia, ID, and IDA among pregnant women, and whether the Hb level was adjusted according to altitude and smoking status. Any disagreements were resolved by consensus or involving a third researcher. The quality assessment of the studies included in this research was carried out per standard requirements.
2.4. Data Analysis
Firstly, we tested the heterogeneity of prevalence estimates reported in included studies with the Cochran Q test and I2 index. The heterogeneity existed among studies if Cochran Q showed a p < 0.10 and I2 > 50% [18]. According to the I2 statistic, heterogeneity was categorized into 3 levels: I2 < 25% taken as low heterogeneity, 25–75% as moderate heterogeneity, and >75% as high heterogeneity [19]. Then, based on the result of the heterogeneity test, a fixed- or random-effects model was selected for the estimate of the pooled prevalence of anemia, ID, and IDA among pregnant women and 95% confidence intervals (CIs). All statistical analyses were carried out using Stata version 12.0 (StataCorp, College Station, TX, USA) and SPSS version 22.0 (SPSS Inc., Chicago, IL, USA).
3. Results
3.1. The Characteristics of Eligible Studies
A total of 57 studies that reported on the prevalence of anemia, ID, or IDA, with a total sample size of 1,376,204 pregnant women, were included in the meta-analysis. The geographic location of the studies spanned the entire country and covered 23 of China’s 34 provinces, autonomous regions, municipalities, and special administrative regions. According to the National Bureau of Statistics, mainland China can be classified into three regions—eastern, central, and western (Figure 2). Many economic and human development indicators are lower in the western region than in the central and eastern regions [20,21]. In this study, the provinces and municipalities of Hebei [22,23,24], Beijing [13,25,26], Tianjin [27], Shandong [28], Jiangsu [29,30,31,32,33], Shanghai [34], Zhejiang [35,36,37,38], Fujian [39], Guangdong [13,33,40], Hainan [41], and Liaoning [42,43,44] represent the eastern region; the provinces of Henan [45,46], Hubei [47], Hunan [48,49], Anhui [50], and Jilin [42,51,52,53] represent the central region; and the provinces, autonomous regions, and municipalities of Chongqing [54,55,56], Sichuan [13,56,57], Shaanxi [58,59], Yunnan [60], Guizhou [58,61], Guangxi Zhuang Autonomous Region [58,61], Ningxia Hui Autonomous Region [62,63,64,65], Tibet Autonomous Region [66,67], and Xinjiang Uygur Autonomous Region [68] represent the western region. Detailed information on the included studies is described in Tables S2–S4.

Figure 2.
The geographic location of the studies included in the meta-analysis.
3.2. Prevalence of Anemia among Pregnant Women in China
3.2.1. Pooled Prevalence
The prevalence of anemia among pregnant women reported by the 36 studies varied widely. The meta-analysis showed that the pooled prevalence of anemia was 30.7% (95% CI: 26.6%, 34.7%). Among anemic cases, roughly half were mild (15.8%; 95% CI: 14.0%, 17.6%), close to 40% were moderate (11.8%; 95% CI: 8.9%, 14.7%), and about 4% were severe (1.1%; 95% CI: 0.8%, 1.5%) (Table 2). Global data show that the prevalence of anemia varies by trimester and geographic location [69]. Therefore, the meta-analysis was conducted to compute the prevalence of anemia among pregnant women in the subgroups as well. However, after the stratification by severity, trimesters, regions, and residence, the I2 statistic varied from 99.3% to 100%, implying the existence of the heterogeneity among included studies.

Table 2.
The prevalence of anemia among pregnant women in China by subgroups.
3.2.2. Prevalence by Trimester
The physical decrease in Hb concentration occurs during pregnancy because the expansion of plasma volume exceeds the increase in the red blood cell volume. Therefore, the trimester that pregnant women are in is one of the influencing factors of anemia [70]. As shown in Table 2, a higher proportion of women in their third trimester were anemic in comparison with those in the first and second trimesters.
3.2.3. Prevalence by Region and by Residence
The prevalence of anemia among pregnant women varied greatly in different regions (shown in Table 2). The subgroup meta-analysis by region showed an increasing trend in the prevalence of anemia among pregnant women from eastern areas to central and western regions. In addition, the prevalence of anemia among pregnant women residing in rural areas was more than double that of pregnant women in urban areas. However, one exception was found in the data collected in Henan Province where the prevalence of anemia among pregnant women in rural areas was lower than that of pregnant women in urban areas (19.6% in rural areas versus 31.5% in urban areas) [71].
3.3. Prevalence of ID among Pregnant Women in China
3.3.1. Pooled Prevalence
A total of 11 studies were included in this meta-analysis on the prevalence of ID among pregnant women in China. The meta-analysis showed that the pooled prevalence of ID was 45.6% (95% CI: 37.0%, 54.2%), suggesting nearly half of the pregnant women in China suffered from ID (Table 3). The heterogeneity existed among studies with I2 between 98.8% and 99.90%.

Table 3.
The prevalence of ID among pregnant women in China by subgroups.
3.3.2. Prevalence by Trimester
Based on the data available, it was found that about a quarter of the pregnant women in their first trimester suffered from ID, while slightly over half of the pregnant women in their third trimester suffered from ID.
3.3.3. Prevalence by Region and by Residence
Contrary to the patterns observed in the prevalence of anemia, the prevalence of ID was higher among pregnant women in the eastern region than the western region and higher among pregnant women residing in urban areas than those in rural areas.
3.4. Prevalence of IDA among Pregnant Women in China
3.4.1. The Pooled IDA Prevalence
The meta-analysis of the 17 studies included in this research showed that the prevalence of IDA among all pregnant women in China was 17.3% (95% CI: 13.9, 20.7) (Table 4). The heterogeneity existed among studies with I2 between 98.6% and 99.90%.

Table 4.
The prevalence of IDA among Chinese pregnant women by subgroups.
3.4.2. Prevalence by Trimester
Similar to the patterns observed in the prevalence of anemia and ID, the subgroup meta-analysis by trimester showed that the prevalence of IDA increased steadily from the first trimester to the third trimester. However, the prevalence of IDA in each trimester was lower than that of anemia and ID in the corresponding trimester.
3.4.3. Prevalence by Region and by Residence
The subgroup meta-analysis by regions was conducted for the pooled prevalence of IDA in the eastern, central, and western regions of China. The prevalence among pregnant women in the central region was higher than both the eastern and western regions. The prevalence of IDA among pregnant women residing in rural areas was found to be nearly twice as high as that in urban areas.
4. Discussion
The 57 studies included in this research collectively sampled 1,376,204 pregnant women who lived in 23 of China’s 34 provinces, autonomous regions, municipalities, and special administrative regions. Our analysis found that the prevalence of anemia, ID, and IDA in pregnant women in China varied by region, urban and rural areas, and the trimester. Moreover, this research found that the prevalence of anemia among pregnant women in China was 30.7%, with roughly half of the cases classified as mild. In comparison, the prevalence of ID and IDA were 45.6% and 17.3%, respectively.
4.1. Anemia, ID, and IDA Prevalence among Pregnant Women in China
According to the WHO classification [10], the prevalence of anemia among pregnant women in China (30.7%) found during this research would be classified as a “moderate” public health problem (20.0–39.9%). This was higher than the 13.6% stated in the “Report on nutrition and chronic diseases of Chinese residents (2020)” published by the China Nutrition and Health Surveillance (CNHS) [72].
In western China, the prevalence of anemia among pregnant women (38.2%) would be close to being regarded as a “severe” public health problem (>40.0%), despite China’s rapid economic development in recent decades. At the national level, although the prevalence of anemia among pregnant women was lower than the global average (36.5%), it was higher than the prevalence in most BRICS countries that shared a similar developing economic situation with China, namely Brazil (19.1%), Russia (23.4%), India (50.1%), and South Africa (30.8%) [73]. The prevalence of anemia among Western pregnant women (38.2%) was close to that in Southeast Asia (37.5%) but lower than that in South Asia (46.7%) [74]. The GDP per capita in China’s most economically developed cities, such as Beijing, Guangzhou, and Shanghai, is comparable to that of high-income countries, according to classification of the World Bank [75]. Yet, our analysis revealed that the prevalence of anemia in those cities was still much higher (19.3%, 38.8%, and 37.3%, respectively, compared to 17.2% in high-income countries) [13,34]. This indicates that the government of China needs to also allocate funding to prevent maternal anemia in the developed areas of the country.
The high prevalence of ID (45.6%) indicates that nearly half of the pregnant women in China suffer from ID. Significantly, the prevalence in China is much higher than what was found among pregnant women in the second trimester in Switzerland (31.8%) and among pregnant women during the third trimester in America (18.5%) [76,77]. SF is an effective indicator to reflect the status of iron stores. Screening for SF should be routinely performed in pregnant women to trigger intervention to prevent the occurrence of IDA during pregnancy [78]. In addition, our findings also suggest that the iron reserves among women of childbearing age in China could be low before conception, indicating the importance of iron supplementation during the pre-pregnancy period to prevent ID and IDA during pregnancy.
4.2. Regional Differences in the Prevalence of Anemia, ID, and IDA among Pregnant Women in China
The significant differences in the prevalence of anemia by region suggest its association with overall socioeconomic status [79], including the quality of medical care services, income levels, dietary diversity and quality, and education level, particularly among pregnant women.
Previous research showed that dietary diversity among residents in rural areas was low, especially in poorer areas where the diet consisted of mainly grains with inadequate intake of animal-based foods and fruits [80,81,82]. One study conducted in the rural areas of northern Shaanxi Province (e.g., western region of China) found that the diet of pregnant women primarily comprised grains and cereals, with an inadequate intake of meat, eggs, milk, fruits, and vegetables [83]. Another study reported that more than 70% of pregnant women had an inadequate intake of fruits and vegetables, and over 90% had a low intake of soybeans, milk, and aquatic products in selected rural poor areas in Anhui Province [84]. In regard to ID, our findings suggest that the prevalence of ID was higher in the economically more developed eastern region and in urban areas, which appeared to be counterintuitive. The following reasons might offer some explanations. Firstly, in terms of screening capacity, only 62.5% of health facilities in China are able to assess SF [85], and fewer facilities in rural areas and the western region had the necessary laboratory equipment, which could lead to the missed reporting of ID cases in these areas. Since ID could lead to IDA and IDA accounted for roughly 50% of anemia globally [1], it is advisable to include SF in the routine testing conducted as part of antenatal and postnatal health care. Secondly, the differences in the varied intake of iron-rich, animal-sourced foods are independent of socioeconomic status. In the eastern region, especially along the coast, the main animal-sourced foods for pregnant women are aquatic foods, instead of red meat, animal offal, and blood, which are richer in heme iron [86]. In comparison, the main animal-sourced foods available in the western region is red meat [87]. For the prevalence of IDA, the regional variation was smaller than that of the prevalence of anemia and ID. Our findings show that the prevalence of IDA in the eastern region of the country is slightly higher than that in the western region. This is consistent, albeit at a smaller magnitude, with the prevalence of ID found in the eastern and western regions.
4.3. Other Influencing Factors of Anemia among Pregnant Women in China
Our analysis found that over half (56%) of the cases of anemia in pregnant women were due to ID, which is very close to global estimates [1]. While prioritizing IDA among pregnant women, attention should also be paid to other causes of anemia. The nutritional status of FA among pregnant women has remarkably improved after the national FA supplementation program for preventing neural tube defects took effect in 2009 [88]. Nonetheless, one cross-sectional study conducted in northwestern China showed that about 12.1% of women in late pregnancy were deficient in FA, and 69.6% of the women were deficient in vitamin B12 [89]. According to the CNHS 2015, 1.2% of pregnant women had a vitamin A deficiency in China, a 10.5% marginal deficiency, while only 0.8% of pregnant women in urban areas had a vitamin A deficiency, a 7.5% marginal deficiency [90,91]. The CNHS2010-2012 found that the average intake of vitamin C was 80.1 mg/d among pregnant women, which was lower than the recommended Dietary Reference Intake (100 mg per day) [92]. Thus, a higher percentage of people could have inadequate vitamin C intake in western China, particularly in the northern part of the region (such as Shaanxi Province), where the availability of fresh vegetables and fruits is limited due to prolonged cold weather [59]. Additionally, thalassemia caused by genetic deficiency is prevalent in areas to the south of the Yangtze River, including Guangdong Province, Guangxi Zhuang Autonomous Region, and Yunnan Province. It was reported that 17.4% of pregnant women carry thalassemia genes [93]. A previous study showed that 18.2% of pregnant women in the Guangxi Zhuang Autonomous Region suffered from thalassemia, and routine screening was performed for pregnant women in areas with a high prevalence of thalassemia [94]. Furthermore, clinicians play a crucial role in reducing anemia among pregnant women. Once a pregnant woman is diagnosed with anemia or ID or IDA, doctors should promptly provide appropriate dietary and iron supplementation recommendations to correct anemia and ID or IDA in a timely manner, aiming for a favorable pregnancy outcome. In the literature included in this meta-analysis, doctors in all studies provided appropriate dietary and nutritional supplement recommendations to anemic pregnant women.
4.4. Quality of Data and Studies
There remain certain quality issues with the studies included in this research despite the application of the inclusion and exclusion criteria. The Hb values could not be adjusted according to the altitude or the smoking status of the pregnant women in some of studies included, as this information was not collected. Therefore, the prevalence of anemia or IDA could be underestimated. Moreover, there were variations in the methods used to take blood samples and assess Hb values, which may have introduced additional variables in the meta-analysis.
5. Recommendations
This meta-analysis and literature review suggest that some program and policy changes could further reduce the prevalence of anemia, ID, and IDA among pregnant women in China. Official standards or guidelines are needed to standardize the lab test protocol and methods for Hb and SF, and SF screening should be a compulsory item in routine antenatal care or basic public health services. Moreover, the must-test items on preventive and therapeutic measures for anemia, ID, and IDA (including iron supplement and nutrition counseling) should be specified in guidelines, appropriate indicators for monitoring should be identified, and the collection, reporting, analysis, and feedback on monitoring data should be required. It is advisable that the official standards or guidelines are issued by the National Health Commission, as this would hold the health services at all levels accountable and have implications for the health insurance scheme. Lastly, prevention and treatment measures, such as multi-micronutrient supplements, should be developed according to the plausible determinants and etiology of anemia among pregnant women residing in different areas in China.
6. Conclusions
In conclusion, this study found that the prevalence of anemia among pregnant women in China was 30.7%, with half of the cases categorized as mild (15.8%). During pregnancy, close to half of the women were diagnosed with ID, and close to 20% of them had IDA. In general, the prevalence of anemia, ID, and IDA were higher in the economically less developed western region and in rural areas, with some exceptions for ID. Program and policy changes are recommended to further reduce the prevalence of anemia, ID, and IDA, including the standardization of lab and diagnostic methods, stipulation of indicators and the relevant reporting mechanisms, requirement of SF screening in antenatal care services, and development of preventive and treatment measures tailored to different contexts in China. Additionally, iron-containing supplements and nutrition counseling could be effective interventions to reduce the prevalence of anemia, ID, and IDA among pregnant women in China.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/nu16121854/s1; Table S1: Quality assessment questions for the studies included; Table S2: Characteristics of the studies included on the prevalence of anemia among pregnant women in China; Table S3: Characteristics of the studies included on the prevalence of ID among pregnant women in China; Table S4: Characteristics of the studies included on the prevalence of IDA among pregnant women in China.
Author Contributions
Conceptualization, data curation, funding acquisition, supervision, and project administration: Y.X. Methodology, formal analysis, validation, and writing—original draft: Y.Z. Formal analysis and writing—review and editing: Y.X., Y.L., Y.Y., X.H. and S.C. Methodology and writing—review and editing: W.Y., H.S., Y.P. and Z.W. Project administration and supervision: A.N., Y.Y., X.H. and S.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the UNICEF Office for China (grant Number: 2022-702-12-MN-4.1). The funding source had no involvement in the study design, the collection, analysis or interpretation of data, the writing of the report, or in the decision to submit the paper for publication.
Data Availability Statement
Datasets are available through the corresponding author upon reasonable request. The data are not publicly available due to privacy reasons.
Acknowledgments
The authors sincerely thank the panel of experts who have provided constructive comments for the development and finalization of this manuscript and thank the study sponsor Anuradha Narayan for project administration and supervision.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Stevens, G.A.; Finucane, M.M.; De-Regil, L.M.; Paciorek, C.J.; Flaxman, S.R.; Branca, F.; Pena-Rosas, J.P.; Bhutta, Z.A.; Ezzati, M.; Nutrition Impact Model Study Group. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995-2011: A systematic analysis of population-representative data. Lancet Glob. Health 2013, 1, e16–e25. [Google Scholar] [CrossRef] [PubMed]
- Mattei, D.; Pietrobelli, A. Micronutrients and Brain Development. Curr. Nutr. Rep. 2019, 8, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Pena-Rosas, J.P.; De-Regil, L.M.; Gomez Malave, H.; Flores-Urrutia, M.C.; Dowswell, T. Intermittent oral iron supplementation during pregnancy. Cochrane Database Syst. Rev. 2015, 2015, Cd009997. [Google Scholar] [CrossRef] [PubMed]
- Chaparro, C.M.; Suchdev, P.S. Anemia epidemiology, pathophysiology, and etiology in low- and middle-income countries. Ann. N. Y. Acad. Sci. 2019, 1450, 15–31. [Google Scholar] [CrossRef] [PubMed]
- Breymann, C. Iron Deficiency Anemia in Pregnancy. Semin. Hematol. 2015, 52, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Kassebaum, N.J.; GBD 2013 Anemia Collaborators. The Global Burden of Anemia. Hematol. Oncol. Clin. North Am. 2016, 30, 247–308. [Google Scholar] [CrossRef]
- An, P.; Wu, Q.; Wang, H.; Guan, Y.; Mu, M.; Liao, Y.; Zhou, D.; Song, P.; Wang, C.; Meng, L.; et al. TMPRSS6, but not TF, TFR2 or BMP2 variants are associated with increased risk of iron-deficiency anemia. Hum. Mol. Genet. 2012, 21, 2124–2131. [Google Scholar] [CrossRef]
- Gan, W.; Guan, Y.; Wu, Q.; An, P.; Zhu, J.; Lu, L.; Jing, L.; Yu, Y.; Ruan, S.; Xie, D.; et al. Association of TMPRSS6 polymorphisms with ferritin, hemoglobin, and type 2 diabetes risk in a Chinese Han population. Am. J. Clin. Nutr. 2012, 95, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Santos, D.C.C.; Angulo-Barroso, R.M.; Li, M.; Bian, Y.; Sturza, J.; Richards, B.; Lozoff, B. Timing, duration, and severity of iron deficiency in early development and motor outcomes at 9 months. Eur. J. Clin. Nutr. 2018, 72, 332–341. [Google Scholar] [CrossRef]
- Kang, Y.; Dang, S.; Zeng, L.; Wang, D.; Li, Q.; Wang, J.; Ouzhu, L.; Yan, H. Multi-micronutrient supplementation during pregnancy for prevention of maternal anaemia and adverse birth outcomes in a high-altitude area: A prospective cohort study in rural Tibet of China. Br. J. Nutr. 2017, 118, 431–440. [Google Scholar] [CrossRef]
- Pena-Rosas, J.P.; De-Regil, L.M.; Garcia-Casal, M.N.; Dowswell, T. Daily oral iron supplementation during pregnancy. Cochrane Database Syst. Rev. 2015, 12, Cd004736. [Google Scholar] [CrossRef] [PubMed]
- Derbyshire, E.; Obeid, R. Choline, Neurological Development and Brain Function: A Systematic Review Focusing on the First 1000 Days. Nutrients 2020, 12, 1731. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; on behalf of the Gestational diabetes mellitus Prevalence Survey (GPS) study Group; Wei, Y.; Zhu, W.; Wang, C.; Su, R.; Feng, H.; Yang, H. Prevalence, risk factors and associated adverse pregnancy outcomes of anaemia in Chinese pregnant women: A multicentre retrospective study. BMC Pregnancy Childbirth 2018, 18, 111. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Huang, A.; Yang, Q.; Zhao, W.; Di, J. Prevalence and Risk Factors of Anemia of Pregnant Women—6 Provinces in China, 2014-2018. China CDC Wkly. 2020, 2, 225–229. [Google Scholar] [CrossRef]
- Wu, Y.; Ye, H.; Liu, J.; Ma, Q.; Yuan, Y.; Pang, Q.; Liu, J.; Kong, C.; Liu, M. Prevalence of anemia and sociodemographic characteristics among pregnant and non-pregnant women in southwest China: A longitudinal observational study. BMC Pregnancy Childbirth 2020, 20, 535. [Google Scholar] [CrossRef] [PubMed]
- Cormack, B.E.; Harding, J.E.; Miller, S.P.; Bloomfield, F.H. The Influence of Early Nutrition on Brain Growth and Neurodevelopment in Extremely Preterm Babies: A Narrative Review. Nutrients 2019, 11, 2029. [Google Scholar] [CrossRef] [PubMed]
- Perinatal Branch of Chinese Medical Association. Diagnosis and Treatment of Iron Deficiency and Iron Deficiency Anemia in Pregnancy. Chin. J. Perinat. Med. 2014, 17, 4. [Google Scholar]
- Garrido-Miguel, M.; Cavero-Redondo, I.; Álvarez-Bueno, C.; Rodríguez-Artalejo, F.; Moreno, L.A.; Ruiz, J.R.; Ahrens, W.; Martínez-Vizcaíno, V. Prevalence and Trends of Overweight and Obesity in European Children From 1999 to 2016: A Systematic Review and Meta-analysis. JAMA Pediatr. 2019, 173, e192430. [Google Scholar] [CrossRef] [PubMed]
- Mogire, R.M.; Mutua, A.; Kimita, W.; Kamau, A.; Bejon, P.; Pettifor, J.M.; Adeyemo, A.; Williams, T.N.; Atkinson, S.H. Prevalence of vitamin D deficiency in Africa: A systematic review and meta-analysis. Lancet Glob. Health 2020, 8, e134–e142. [Google Scholar] [CrossRef] [PubMed]
- Adam, I.; Ibrahim, Y.; Elhardello, O. Prevalence, types and determinants of anemia among pregnant women in Sudan: A systematic review and meta-analysis. BMC Hematol. 2018, 18, 31. [Google Scholar] [CrossRef]
- He, G. A survey on the prevalence of iron deficiency and iron deficiency anemia during pregnancy in some cities of China. Chin. J. Obstet. Gynecol. 2018, 53, 761–767. [Google Scholar]
- Ning, F. Clinical Investigation on the Incidence of Iron Deficiency and Iron Deficiency Anemia During Pregnancy and Study on the Timing of Preventive Iron Supplementation. Master’s Thesis, Hebei Medical University, Shijiazhuang, China, 2015. [Google Scholar]
- Li, M.; Zhao, Y.; Zhang, Y. A survey on malnutrition anemia among pregnant women in Qinhuangdao City. J. Prev. Med. Chin. People’s Lib. Army 2019, 37, 131–132. [Google Scholar]
- Li, J. Survey and Analysis of Anemia Status in 1558 Pregnant Women. J. Hebei Med. Univ. 2011, 32, 1223–1224. [Google Scholar]
- Lu, S.; Zhang, X.; Hu, M.; Dong, S.; Peng, Y.; Teng, Y. Analysis of Hemoglobin Nutrition Status in Late Pregnancy Women in Beijing. China Foods Nutr. 2018, 24, 83–86. [Google Scholar]
- Wang, B. Survey on Anemia among Pregnant Women in the Jurisdiction of Beijing Tiantan Community Health Service Center in 2013. J. Reprod. Med. 2014, 23, 586–588. [Google Scholar]
- Xiao, H.; Yin, S. Analysis of Serum Ferritin Levels and Anemia Prevalence Characteristics in Pregnant Women at Different Gestational Ages. Matern. Child Health Care China 2019, 34, 4886–4888. [Google Scholar]
- Wang, Y.; Wang, J.; Wu, H. Anemia in different stages of pregnancy and folic acid supplementation. J. Mod. Instrum. Mediccal Treat. 2019, 25, 77–80. [Google Scholar]
- Feng, P.; Jia, F.; Yu, Q.; Wang, K.; Li, N.; Yang, L.; Shen, J.; Wan, Q.; Xu, Y.; Zhang, M.; et al. A Study on Iron Deficiency and Anemia during Pregnancy in Kunshan City. Adv. Clin. Med. 2020, 10, 562–567. [Google Scholar] [CrossRef]
- Gao, H.; Shi, J.; Zhang, D.; Shen, P.; Guo, Y.; Zhou, S. Investigation and Analysis of the Prevalence of Anemia among Residents in Ningbo City. Chin. J. Health Lab. Technol. 2019, 29, 623–626. [Google Scholar]
- Yu, J. Investigation on Serum Ferritin Levels and Incidence of Iron Deficiency Anemia in Pregnant Women in the Middle and Late Stages of Pregnancy in Zhangjiagang Area. Master’s Degree, Soochow University, Taipei, Taiwan, 2017. [Google Scholar]
- Lan, M. Investigation on the Prevalence of Anemia and Serum Ferritin Levels in 3262 Pregnant Women in the Middle and Late Stages of Pregnancy. Master’s Thesis, Nanjing University, Nanjing, China, 2016. [Google Scholar]
- Yuan, X.; Hu, H.; Zhang, M.; Long, W.; Liu, J.; Jiang, J.; Yu, B. Iron deficiency in late pregnancy and its associations with birth outcomes in Chinese pregnant women: A retrospective cohort study. Nutr. Metab. 2019, 16, 30. [Google Scholar] [CrossRef]
- Tang, L.; Zhang, X.J.; Tang, Z.H. Investigation of gestational anaemia in Shanghai, 2016. Lab. Med. Clin. 2020, 35, 116–119. [Google Scholar]
- Sun, L.; Xu, R.; Peng, J.; Gong, T.; Liu, J.; Wu, Q.; Wang, J. Analysis of Health Care and Health Status of Pregnant and Lying-in Women in Suzhou City from 2014 to 2017. China Health Ind. 2019, 16, 180–181, 184. [Google Scholar] [CrossRef]
- Qian, L.; Hong, Z. Serum Ferritin Levels, Prevalence of Iron Deficiency Anemia, and Their Impact on Pregnancy Outcomes among Pregnant Women in the Middle and Late Stages of Pregnancy in Yueqing Area. Matern. Child Health Care China 2020, 35, 995–998. [Google Scholar]
- Kong, J.; Chen, L. Analysis of the Incidence and Prevention Measures of Common Complications such as Hypertensive Disorders in Pregnancy, Diabetes, and Anemia in 2000 Pregnant Women. Matern. Child Health Care China 2019, 34, 5112–5115. [Google Scholar]
- Shao, Y.; Wu, H.; Jiang, W.; Pu, L.; Huang, M.; Shao, B.; Mo, M.; Wang, S.; Shen, Y.; Yu, Y. Study on the Relationship between Hemoglobin Content and Blood Pressure in Pregnant Women in Zhoushan Island Area. Matern. Child Health Care China 2019, 34, 2438–2443. [Google Scholar]
- Fu, L.; Zhang, Q. Current Analysis of Iron Deficiency Anemia and Iron Deficiency during Pregnancy in Xiamen City. Chin. Foreign Med. Res. 2020, 18, 175–178. [Google Scholar]
- Chen, Y.; Li, M.; Pan, H.; Chen, X.M.; Lin, Q.M. Analysis of complications/complications in 51327 pregnant women. Jilin Med. Sci. 2017, 38, 2278–2280. [Google Scholar]
- Huang, X.; Yu, Z.; Zhang, F. Survey and Analysis of Anemia Status of 517 Pregnant Women in Lingshui County, Hainan Province. Clin. Med. Eng. 2011, 18, 1466–1467, 1470. [Google Scholar] [CrossRef]
- Yang, L.; Li, J.; Dong, S. Epidemiological Investigation of Anemia among Pregnant Women in Shenyang Area. Matern. Child Health Care China 2012, 27, 5559–5560. [Google Scholar]
- Yu, J.; Yang, L. Analysis of the Anemia Status of Pregnant and Lying-in Women in Shenyang in 2009. Chin. J. Rural. Med. Pharm. 2012, 19, 23–24. [Google Scholar]
- Li, M. Investigation and Study on the Prevalence of Iron Deficiency and Iron Deficiency Anemia among 1562 Pregnant Women in Dalian City. Master’s Thesis, Dalian Medical University, Dalian, China, 2019. [Google Scholar]
- Luo, H.; Shi, N.; Guo, P.; Zhai, S.S.; Pan, C.; Wang, X.H. Correlation Study of Serum Iron and Serum Ferritin Levels in Pregnant Women. Chin. J. Women Child. Health 2019, 10, 35–38. [Google Scholar]
- Li, F. Analysis of Anemia Status and Related Factors among Pregnant Women. Chin. J. Health Care Nutr. (Mid-Month Ed.) 2012, 7, 270. [Google Scholar]
- Nuerbiye, D. Investigation and Study on the Prevalence of Iron Deficiency and Iron Deficiency Anemia among Pregnant Women in Wuhan Area. World Latest Med. Inf. Dig. (Electronic Edition) 2019, 19, 192. [Google Scholar]
- Tan, J.; He, G.; Qi, Y.; Yang, H.; Xiong, Y.; Liu, C.; Wang, W.; Zou, K.; Lee, A.H.; Sun, X.; et al. Prevalence of anemia and iron deficiency anemia in Chinese pregnant women (IRON WOMEN): A national cross-sectional survey. BMC Pregnancy Childbirth 2020, 20, 670. [Google Scholar] [CrossRef] [PubMed]
- Ye, C.; Li, T.; Li, P. Analysis of the Occurrence and Influencing Factors of Iron Deficiency Anemia in Pregnant Women. South China J. Prev. Med. 2020, 46, 477–480. [Google Scholar]
- Yang, Y.Y.; Fang, Y.H.; Wang, X.; Zhang, Y.; Liu, X.-J.; Yin, Z.-Z. A retrospective cohort study of risk factors and pregnancy outcomes in 14,014 Chinese pregnant women. Medicine 2018, 97, e11748. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y. Epidemiological Analysis of Monitoring Data on Critical Pregnant Women in Jilin Province in 2017. Master’s Degree, Jilin University, Changchun, China, 2019. [Google Scholar]
- Huang, L.; Kang, Y.; Jiang, T.; Liu, C.X.; Qiao, C. Cross-sectional Survey on the Status of Iron Deficiency and Iron Deficiency Anemia among Pregnant Women in Urban Shenyang. Chin. J. Pract. Gynecol. Obstet. 2017, 33, 751–754. [Google Scholar] [CrossRef]
- Liu, J.; Yang, J.; Sun, C. Investigation and Analysis of the Current Status and Related Factors of Iron Deficiency Anemia during Pregnancy in Jilin Province. Matern. Child Health Care China 2016, 31, 3144–3146. [Google Scholar]
- Xie, M. Study on the Distribution of Diseases and Influencing Factors of Pregnancy Outcomes among Pregnant Women in Chongqing Area. Master’s Degree, Chongqing Medical University, Chongqing, China, 2020. [Google Scholar]
- Lan, Y.; Huang, R. Analysis of Anemia Status and Causes among 1000 Pregnant Women in the Second Trimester. Chongqing Med. 2014, 43, 2792–2794. [Google Scholar]
- Yang, M.; He, L.; Shi, L.; Tan, J.; Gao, Y.; Zhou, W.; Liu, X.L.; Liu, X.H.; Chen, M. Current Status Investigation and Multi-factor Analysis of Iron Deficiency and Iron Deficiency Anemia during Pregnancy in Urban Areas of Sichuan and Chongqing. J. Pract. Obstet. Gynecol. 2018, 34, 840–843. [Google Scholar]
- Kuang, L.; Song, J.; Yin, J. Analysis of Iron Deficiency and Iron Deficiency Anemia during Pregnancy among Pregnant Women in Santai County. Te Bie Jian Kang 2019, 13, 166. [Google Scholar] [CrossRef]
- Wang, H.; Tang, W.; Zhu, J.; Liang, J.; Mou, W.; Liu, Z.; Li, M.R.; Shen, L.Q. Prevalence and Influencing Factors of Anemia among Pregnant Women in Three Western Provinces of China. Matern. Child Health Care China 2016, 31, 2019–2022. [Google Scholar]
- Liu, H. Investigation on the Prevalence of Iron Deficiency and Iron Deficiency Anemia among Pregnant Women in Shaanxi Area. Shaanxi Med. J. 2018, 47, 943–946. [Google Scholar]
- Yang, H. Investigation of Anemia among Rural Tibetan Pregnant Women with Gestational Complications in Yunnan Tibetan Areas. Health Soft Sci. 2013, 27, 499–501. [Google Scholar]
- Ma, A.G.; Schouten, E.G.; Wang, Y.; Xu, R.-X.; Zheng, M.-C.; Li, Y.; Wang, Q.; Sun, Y. Micronutrient status in anemic and non-anemic Chinese women in the third trimester of pregnancy. Asia Pac. J. Clin. Nutr. 2009, 18, 41–47. [Google Scholar] [PubMed]
- Wang, G.; Hou, W.; Zhang, H. Investigation and Analysis of Anemia during Pregnancy from 2013 to 2014. Mother Baby World 2016, 85. Available online: https://d.wanfangdata.com.cn/periodical/mysj201614078 (accessed on 28 May 2022).
- He, Y.; Chen, H.; Gao, M.; He, Y.; Li, G.; Pan, Y. Analysis of the Current Status and Influencing Factors of Anemia among Pregnant Women in Haiyuan Area of Ningxia. J. Ningxia Med. Univ. 2015, 37, 556–558. [Google Scholar]
- Gao, L.; Shen, D.; Yang, W. Investigation and Analysis of the Current Status and Related Factors of Iron Deficiency Anemia among 2405 Pregnant Women. J. Hubei Univ. Natl. (Med. Ed.) 2017, 34, 39–41. [Google Scholar]
- Ma, H. Analysis of the Adverse Effects of Iron Deficiency Anemia during Pregnancy on Mothers and Infants in High Altitude Areas. Qinghai Med. J. 2019, 49, 28–30. [Google Scholar]
- Kang, J.; Li, Z.; Dang, N. Investigation of Hemoglobin Levels among Rural Tibetan Pregnant Women in Lhasa. Chin. J. Prev. Med. 2014, 48, 396–400. [Google Scholar]
- Zhou, X. Study on Pregnancy Complications and Their Influencing Factors among 2136 Pregnant Women in Lhasa. Master’s Degree, Huazhong University of Science and Technology, Wuhan, China, 2019. [Google Scholar]
- Shi, P.; Liu, X.; Yang, J.; Han, M.; Zhao, X. Investigation on the Prevalence of Pregnancy Complications with Anemia among Pregnant Women in Nilka Area of Xinjiang. Chin. Foreign Med. Res. 2016, 14, 163–164. [Google Scholar]
- Georgieff, M.K. Iron deficiency in pregnancy. Am. J. Obstet. Gynecol. 2020, 223, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Churchill, D.; Nair, M.; Stanworth, S.J.; Knight, M. The change in haemoglobin concentration between the first and third trimesters of pregnancy: A population study. BMC Pregnancy Childbirth 2019, 19, 359. [Google Scholar] [CrossRef] [PubMed]
- Qi, M.J.; Gao, L.; Wang, K.; Zhou, S.S.; Feng, S.X.; Kang, K. Analysis on anemia status and its influencing factors in pregnant women. Chin. J. Woman Child Health 2020, 31, 1204–1208. [Google Scholar]
- Pedersen, T.L.; Smilowitz, J.T.; Winter, C.K.; Emami, S.; Schmidt, R.J.; Bennett, D.H.; Hertz-Picciotto, I.; Taha, A.Y. Quantification of Nonpersistent Pesticides in Small Volumes of Human Breast Milk with Ultrahigh Performance Liquid Chromatography Coupled to Tandem Mass Spectrometry. J. Agric. Food Chem. 2021, 69, 6676–6689. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.Y.; Wen, Q.H.; Liu, Z.X.; Huang, J.Y. Investigation and analysis of iron deficiency anemia of pregnant women in Dongguan. Lab. Med. Clin. 2019, 16, 1703–1705. [Google Scholar]
- Camaschella, C. Iron-deficiency anemia. N. Engl. J. Med. 2015, 372, 1832–1843. [Google Scholar] [CrossRef] [PubMed]
- Businge, C.B.; Longo-Mbenza, B.; Kengne, A.P. The prevalence of insufficient iodine intake in pregnancy in Africa: Protocol for a systematic review and meta-analysis. Syst. Rev. 2019, 8, 209. [Google Scholar] [CrossRef] [PubMed]
- Cogswell, M.E.; Parvanta, I.; Ickes, L.; Yip, R.; Brittenham, G.M. Iron supplementation during pregnancy, anemia, and birth weight: A randomized controlled trial. Am. J. Clin. Nutr. 2003, 78, 773–781. [Google Scholar] [CrossRef]
- Bencaiova, G.; Burkhardt, T.; Breymann, C. Anemia--prevalence and risk factors in pregnancy. Eur. J. Intern. Med. 2012, 23, 529–533. [Google Scholar] [CrossRef]
- Loy, S.L.; Lim, L.M.; Chan, S.Y.; Tan, P.T.; Chee, Y.L.; Quah, P.L.; Chan, J.K.Y.; Tan, K.H.; Yap, F.; Godfrey, K.M.; et al. Iron status and risk factors of iron deficiency among pregnant women in Singapore: A cross-sectional study. BMC Public Health 2019, 19, 397. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Pang, X.; Daun, Y.; Bi, Y.; Wang, J.; Yin, S.A.; Yang, L.C.; Yang, Z.Y. Prevalence and related factors of anemia in pregnant women in China during 2010-2012. Chin. J. Prev. Med. 2018, 52, 21–25. [Google Scholar]
- Zheng, M.; Yin, J.Z.; Li, Y.; Luo, X.Y.; Qian, C.F.; Shi, A.P. Investigation on nutritional knowledge and attitude and dietary behavior of poor rural women of middle and late pregnancy. Matern. Child Health Care China 2010, 25, 3458–3461. [Google Scholar]
- Gao, H.; Stiller, C.K.; Scherbaum, V.; Biesalski, H.K.; Wang, Q.; Hormann, E.; Bellows, A.C. Dietary intake and food habits of pregnant women residing in urban and rural areas of Deyang City, Sichuan Province, China. Nutrients 2013, 5, 2933–2954. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Feng, X.Y.; Luo, B.R. Investigation on the status of pregnant women’s dietary behavior in poverty-stricken rural areas of Sichuan Province. Matern. Child Health Care China 2016, 31, 3823–3827. [Google Scholar]
- Fan, X.; Li, X.L.; Ma, L.P.; Xue, C.L.; Liu, Y.L.; Li, Z.X.; Yang, H.G.; Zhang, Y.P. A study on the status of pregnant women complicated with anemia in a county of northern Shaanxi. Chin. J. Health Stat. 2014, 31, 294–296. [Google Scholar]
- Zhang, W.M.; Wang, X.Q.; Bo, Q.L.; Ruan, L.; Wang, H.J.; Sun, S.B.; Gao, Y.L.; Wang, S.F. Cross-sectional investigation and study on dietary situation among urban and rural pregnant women in Anhui province. Matern. Child Health Care China 2015, 30, 5633–5636. [Google Scholar]
- Lange, S.; Probst, C.; Gmel, G.; Rehm, J.; Burd, L.; Popova, S. Global Prevalence of Fetal Alcohol Spectrum Disorder Among Children and Youth: A Systematic Review and Meta-analysis. JAMA Pediatr. 2017, 171, 948–956. [Google Scholar] [CrossRef] [PubMed]
- Lou, H.Q.; Wan, C.H.; Wu, Z. Investigation and analysis of dietary nutrition status of pregnant women in Nantong city. Matern. Child Health Care China 2014, 29, 761–762. [Google Scholar]
- Tuerxunjiang, M.; Wang, X.; Camila, T.; Yang, Y.Q.; Dilihuomaer, ·W.; Pu, J.F.; Wang, L.; Yan, L.Q.Z. Follow-up study on diet, folic acid and iron status in 358 cases of Uygur pregnant women from Xinjiang Kashi. J. Hyg. Res. 2017, 46, 563–568. [Google Scholar] [CrossRef]
- Liu, J.; Li, Z.; Ye, R.; Ren, A.; Liu, J. Folic acid supplementation and risk for congenital hydrocephalus in China. Public Health Nutr. 2021, 24, 4238–4244. [Google Scholar] [CrossRef]
- Du, Y.J.; Li, J.; Wang, H.L.; Du, J.Y.; Qu, P.F.; Zhang, R.; Guo, L.Q.; Yan, H.; Dang, S.N. Epidemiological characteristics of serum vitamin B(12) and folate levels in women awaiting delivery. Zhonghua Liu Xing Bing Xue Za Zhi=Zhonghua Liuxingbingxue Zazhi 2020, 41, 1359–1364. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Wang, L.J.; Wang, R.; Hu, Y.C.; Li, W.D.; Mao, D.Q.; Huang, J.; Yang, L.C. Vitamin A nutrition status among pregnant women in rural China in 2015. Wei Sheng Yan Jiu=J. Hyg. Res. 2021, 50, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Wang, R.; Li, W.; Mao, D.Q.; Hu, Y.C.; Yang, L.C. Vitamin A nutritional status and its changing trends in Chinese urban pregnant women. Acta Nutr. Sin. 2020, 42, 542–546. [Google Scholar]
- He, Y.N.; Wang, Z.; Zhao, L.Y.; Fang, Y.H.; Yang, X.G.; Zhao, W.H. Dietary intake of vitamin in Chinese population from 2010 to 2012. Acta Nutr. Sin. 2017, 39, 112–115. [Google Scholar]
- Li, B. The evaluation on epidemiology and prevention status of thalassemia in Guangdong Province. Ph.D. Thesis, Southern Medical University, Guangzhou, China, 2015. [Google Scholar]
- Wu, H.Z.; Chang, Z.Y.; Wei, F.L.; Lu, C.H.; Lu, X.C. Prenatal screening and fetal diagnosis of thalassemia. Chin. J. Birth Health Hered. 2007, 50–51. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).