Iodine Status of Infants and Toddlers under 2 Years of Age and Its Association with Feeding Behaviors and Maternal Iodine Status in Shanghai: A Quantile Regression Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection and Measurements
2.3. Analysis of Iodine Status
2.4. Definitions and Classifications of Relevant Indicators
2.5. Statistical Analysis
3. Results
3.1. Characteristics of Infants and Toddlers and Their Mothers
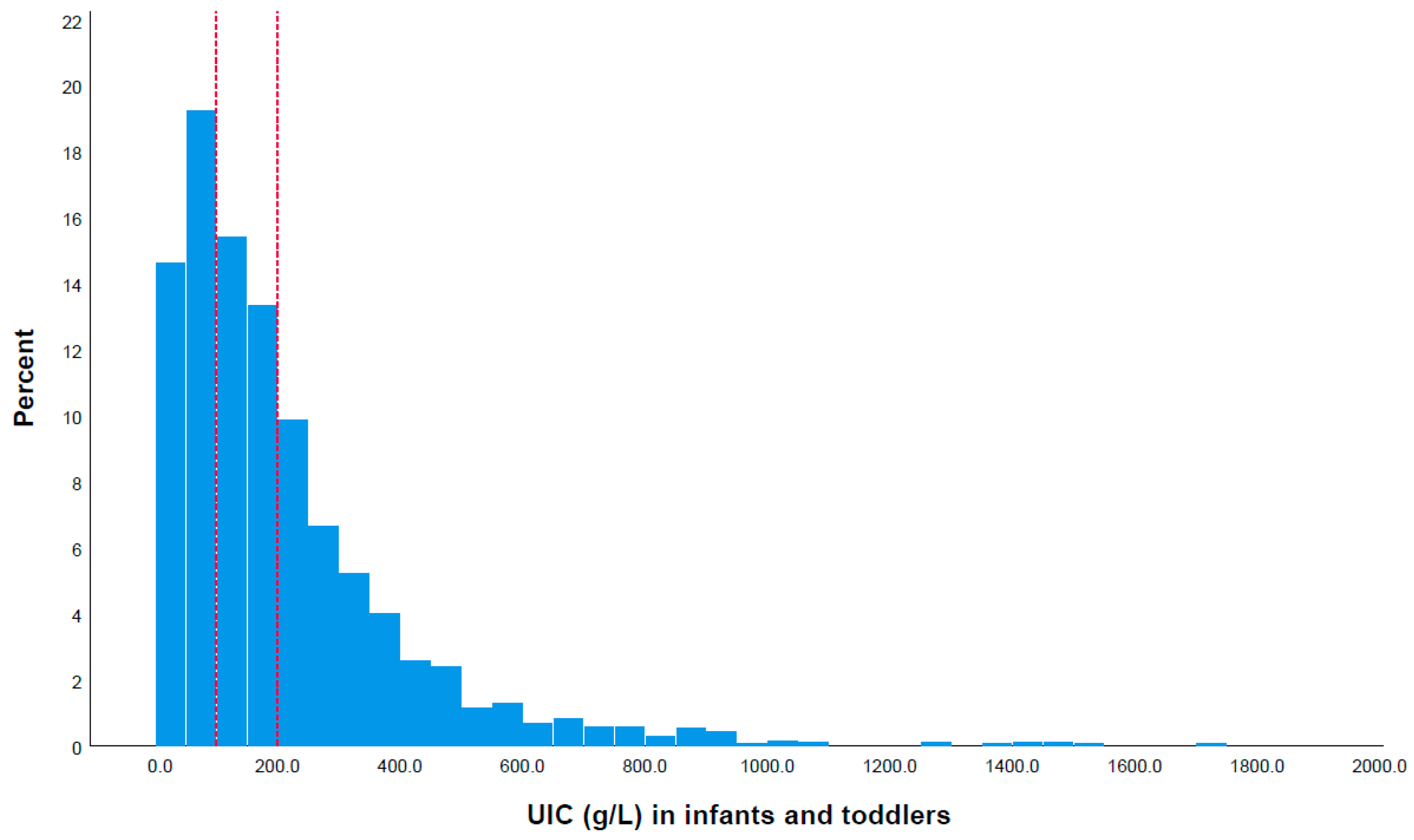
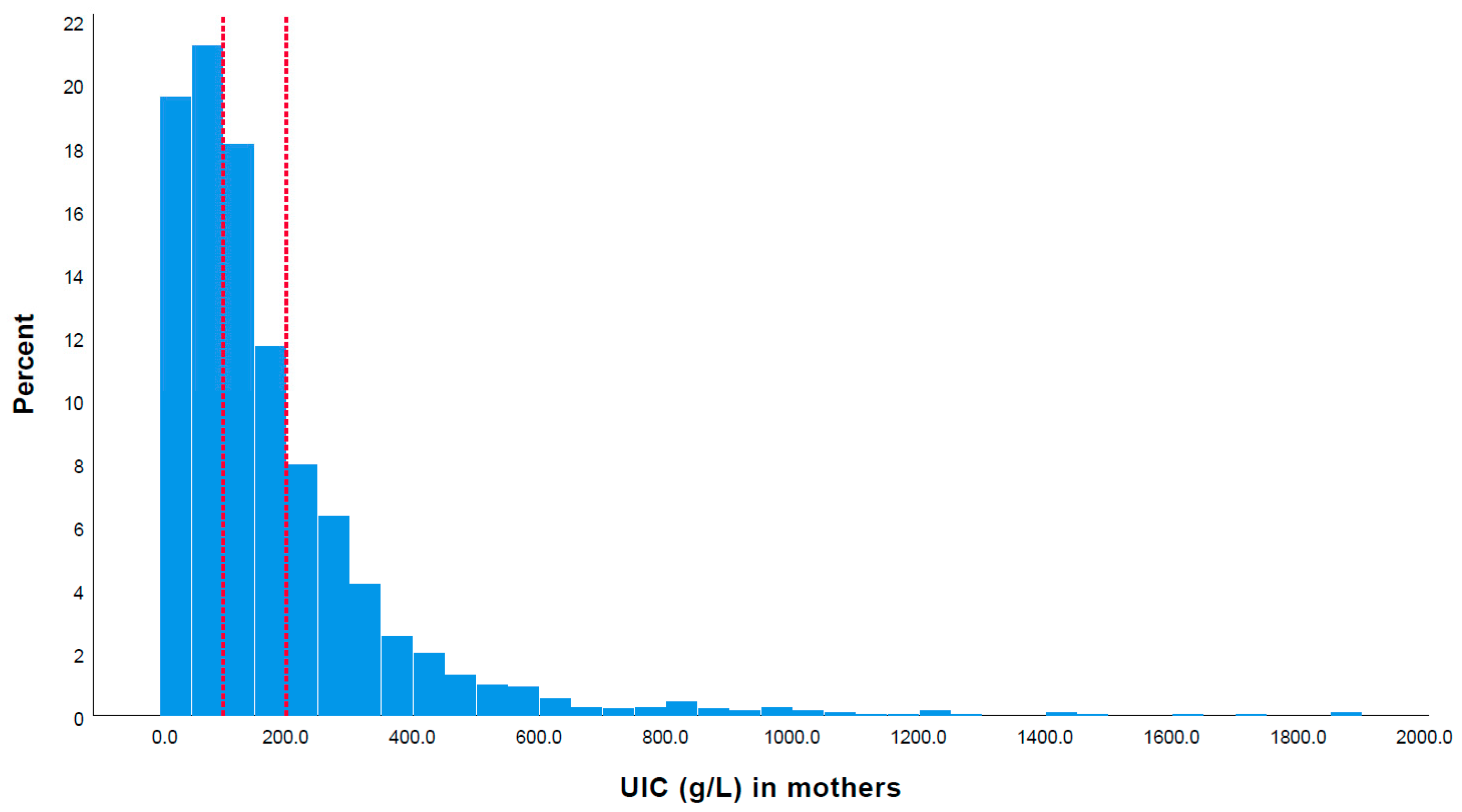
3.2. Iodine Status of Young Children and Mothers
3.3. The Relationship between Children’s UIC and Feeding Behaviors and the Frequency of Intake of Iodine-Rich Foods
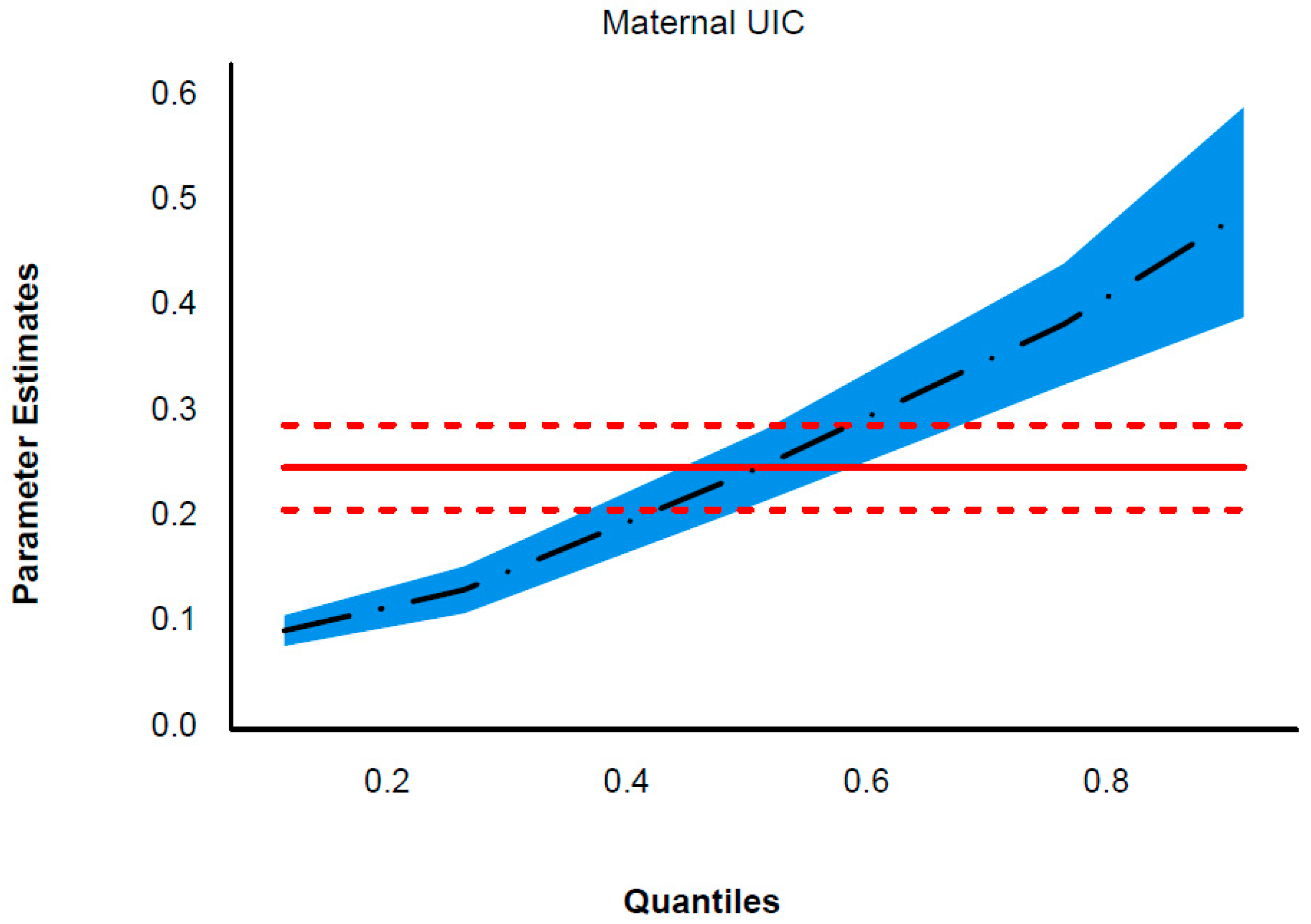
3.4. Correlation between the Iodine Status of Infants and Toddlers and Their Mothers
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Croce, L.; Chiovato, L.; Tonacchera, M.; Petrosino, E.; Tanda, M.L.; Moleti, M.; Magri, F.; Olivieri, A.; Pearce, E.N.; Rotondi, M. Iodine status and supplementation in pregnancy: An overview of the evidence provided by meta-analyses. Rev. Endocr. Metab. Disord. 2023, 24, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Bath, S.C. The effect of iodine deficiency during pregnancy on child development. Proc. Nutr. Soc. 2019, 78, 150–160. [Google Scholar] [CrossRef] [PubMed]
- Björnholm, L.; Orell, O.; Kerkelä, M.; Honka, U.; Laasonen, S.; Riekki, T.; Surcel, H.M.; Suvanto, E.; Veijola, J. Maternal Thyroid Function During Pregnancy and Offspring White Matter Microstructure in Early Adulthood: A Prospective Birth Cohort Study. Thyroid 2023, 33, 1245–1254. [Google Scholar] [CrossRef] [PubMed]
- Morreale de Escobar, G.; Obregon, M.J.; Escobar del Rey, F. Role of thyroid hormone during early brain development. Eur. J. Endocrinol. 2004, 151 (Suppl. S3), U25–U37. [Google Scholar] [CrossRef] [PubMed]
- Thaker, V.V.; Leung, A.M.; Braverman, L.E.; Brown, R.S.; Levine, B. Iodine-induced hypothyroidism in full-term infants with congenital heart disease: More common than currently appreciated? J. Clin. Endocrinol. Metab. 2014, 99, 3521–3526. [Google Scholar] [CrossRef]
- Cross, C.; Moriarty, H.; Coakley, J. Prevalence of Iodine Deficiency in Infants and Young Children in Western Sydney, Australia: A Cross-Sectional Analysis. ICAN Infant Child Adolesc. Nutr. 2010, 2, 284–287. [Google Scholar] [CrossRef]
- Hetzel, B.S. The development of a global program for the elimination of brain damage due to iodine deficiency. Asia Pac. J. Clin. Nutr. 2012, 21, 164–170. [Google Scholar] [PubMed]
- Bougma, K.; Aboud, F.E.; Harding, K.B.; Marquis, G.S. Iodine and mental development of children 5 years old and under: A systematic review and meta-analysis. Nutrients 2013, 5, 1384–1416. [Google Scholar] [CrossRef] [PubMed]
- Dineva, M.; Fishpool, H.; Rayman, M.P.; Mendis, J.; Bath, S.C. Systematic review and meta-analysis of the effects of iodine supplementation on thyroid function and child neurodevelopment in mildly-to-moderately iodine-deficient pregnant women. Am. J. Clin. Nutr. 2020, 112, 389–412. [Google Scholar] [CrossRef]
- Bakken, K.S.; Aarsland, T.E.; Groufh-Jacobsen, S.; Solvik, B.S.; Gjengedal, E.L.F.; Henjum, S.; Strand, T.A. Adequate Urinary Iodine Concentration among Infants in the Inland Area of Norway. Nutrients 2021, 13, 1826. [Google Scholar] [CrossRef]
- König, F.; Andersson, M.; Hotz, K.; Aeberli, I.; Zimmermann, M.B. Ten Repeat Collections for Urinary Iodine from Spot Samples or 24-Hour Samples Are Needed to Reliably Estimate Individual Iodine Status in Women. J. Nutr. 2011, 141, 2049–2054. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Wu, Y.; Lin, L.; Tan, L.; Shen, J.; Pearce, E.N.; Guo, X.; Wang, W.; Bian, J.; Jiang, W.; et al. 24-Hour Urine Samples Are More Reproducible Than Spot Urine Samples for Evaluation of Iodine Status in School-Age Children. J. Nutr. 2016, 146, 142–146. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; The United Nations Children’s Fund; The International Council for Control of Iodine Deficiency Disorders. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Program Managers. Available online: https://apps.who.int/iris/bitstream/handle/10665/43781/9789241595827_eng.pdf (accessed on 2 April 2024).
- Liu, Z.; Lin, Y.; Wu, J.; Chen, D.; Wu, X.; Lan, Y.; Chen, Z. Is the urinary iodine/creatinine ratio applicable to assess short term individual iodine status in Chinese adults? Comparison of iodine estimates from 24-h urine and timed-spot urine samples in different periods of the day. Nutr. Metab. 2022, 19, 27. [Google Scholar] [CrossRef] [PubMed]
- de Benoist, B.; McLean, E.; Andersson, M.; Rogers, L. Iodine deficiency in 2007: Global progress since 2003. Food Nutr. Bull. 2008, 29, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Li, Y.; Teng, D.; Shi, X.; Yan, L.; Yang, J.; Yao, Y.; Ye, Z.; Ba, J.; Chen, B.; et al. The Characteristics of Iodine Nutrition Status in China After 20 Years of Universal Salt Iodization: An Epidemiology Study Covering 31 Provinces. Thyroid 2021, 31, 1858–1867. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Zheng, C.; Zheng, W.; Wan, Z.; Bu, Y.; Zhang, G.; Ding, S.; Wang, E.; Zhai, D.; Ma, Z.F. Mild-to-moderate iodine deficiency in a sample of pregnant women and salt iodine concentration from Zhejiang province, China. Environ. Geochem. Health 2020, 42, 3811–3818. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Ma, Z.F.; Lu, Y.; Pan, B.; Shao, J.; Wang, L.; Du, Y.; Zhao, Q. Assessment of Iodine Status among Pregnant Women and Neonates Using Neonatal Thyrotropin (TSH) in Mainland China after the Introduction of New Revised Universal Salt Iodisation (USI) in 2012: A Re-Emergence of Iodine Deficiency? Int. J. Endocrinol. 2019, 2019, 3618169. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Li, M.; Liu, X.; Wu, M.; Zhang, J.; Zhao, L.; Ding, G.; Yang, X. Evaluation of Iodine Nutritional Status Among Pregnant Women in China. Thyroid 2020, 30, 443–450. [Google Scholar] [CrossRef]
- Tian, W.; Yan, W.; Liu, Y.; Zhou, F.; Wang, H.; Sun, W. The Status and Knowledge of Iodine among Pregnant Women in Shanghai. Biol. Trace Elem. Res. 2021, 199, 4489–4497. [Google Scholar] [CrossRef]
- Yan, W.; Bao, C.; Tian, W.; Sun, W. Assessment of the Iodine Status of Lactating Women and Infants in Shanghai, China. Biol. Trace Elem. Res. 2023, 201, 5512–5520. [Google Scholar] [CrossRef]
- Holla-Bhar, R.; Iellamo, A.; Gupta, A.; Smith, J.P.; Dadhich, J.P. Investing in breastfeeding—The world breastfeeding costing initiative. Int. Breastfeed. J. 2015, 10, 8. [Google Scholar] [CrossRef] [PubMed]
- Andersson, M.; de Benoist, B.; Delange, F.; Zupan, J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: Conclusions and recommendations of the Technical Consultation. Public Health Nutr. 2007, 10, 1606–1611. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Wang, Z.; Sun, Z.; Shi, Z.; Song, Q.; Cui, X.; Shen, L.; Qu, M.; Mai, S.; Zang, J. The Interactive Effects of Severe Vitamin D Deficiency and Iodine Nutrition Status on the Risk of Thyroid Disorder in Pregnant Women. Nutrients 2022, 14, 4484. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Jin, W.; Zhu, Z.; Cui, X.; Song, Q.; Shi, Z.; Wu, C.; Zang, J.; Guo, C. Relationship of household cooking salt and eating out on iodine status of pregnant women in environmental iodine-deficient coastal areas of China. Br. J. Nutr. 2020, 124, 971–978. [Google Scholar] [CrossRef] [PubMed]
- WHO. Child Growth Standards: Software. Available online: https://www.who.int/tools/child-growth-standards/software (accessed on 1 April 2024).
- Chen, X.; Wu, C.; Wang, Z.; Wu, C.; Guo, Y.; Zhu, X.; Hu, Y.P.; Shi, Z.; Song, Q.; Cui, X.; et al. Iodine nutrition status and thyroid autoimmunity during pregnancy: A cross-sectional study of 4635 pregnant women. Nutr. J. 2022, 21, 7. [Google Scholar] [CrossRef] [PubMed]
- WHO. Iodine Deficiency. Available online: https://www.who.int/data/nutrition/nlis/info/iodine-deficiency (accessed on 2 April 2024).
- Brantsæter, A.L.; Abel, M.H.; Haugen, M.; Meltzer, H.M. Risk of suboptimal iodine intake in pregnant Norwegian women. Nutrients 2013, 5, 424–440. [Google Scholar] [CrossRef] [PubMed]
- Aakre, I.; Markhus, M.W.; Kjellevold, M.; Moe, V.; Smith, L.; Dahl, L. Sufficient iodine status among Norwegian toddlers 18 months of age—Cross-sectional data from the Little in Norway study. Food Nutr. Res. 2018, 62, 1443–1452. [Google Scholar] [CrossRef] [PubMed]
- Delange, F.; Heidemann, P.; Bourdoux, P.; Larsson, A.; Vigneri, R.; Klett, M.; Beckers, C.; Stubbe, P. Regional variations of iodine nutrition and thyroid function during the neonatal period in Europe. Biol. Neonate 1986, 49, 322–330. [Google Scholar] [CrossRef]
- Pearce, E.N.; Leung, A.M.; Blount, B.C.; Bazrafshan, H.R.; He, X.; Pino, S.; Valentin-Blasini, L.; Braverman, L.E. Breast milk iodine and perchlorate concentrations in lactating Boston-area women. J. Clin. Endocrinol. Metab. 2007, 92, 1673–1677. [Google Scholar] [CrossRef]
- Rossi, L.; Branca, F. Salt iodisation and public health campaigns to eradicate iodine deficiency disorders in Armenia. Public Health Nutr. 2003, 6, 463–469. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, Z.; Ge, P.; Wang, Y.; Wang, S. Iodine status and thyroid function of pregnant, lactating women and infants (0-1 yr) residing in areas with an effective Universal Salt Iodization program. Asia Pac. J. Clin. Nutr. 2009, 18, 34–40. [Google Scholar] [PubMed]
- Osei, J.; Baumgartner, J.; Rothman, M.; Matsungo, T.M.; Covic, N.; Faber, M.; Smuts, C.M. Iodine status and associations with feeding practices and psychomotor milestone development in six-month-old South African infants. Matern. Child Nutr. 2017, 13, e12408. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zhu, L.; Li, X.F.; Zheng, H.M.; Wang, Z.; Hao, Z.Y.; Liu, Y. Maternal iodine status during lactation and infant weight and length in Henan Province, China. BMC Pregnancy Childbirth 2017, 17, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Gordon, J.H.; Leung, A.M.; Hale, A.R.; Pearce, E.N.; Braverman, L.E.; He, X.; Belfort, M.B.; Nelson, S.M.; Brown, R.S. No difference in urinary iodine concentrations between Boston-area breastfed and formula-fed infants. Thyroid 2014, 24, 1309–1313. [Google Scholar] [CrossRef] [PubMed]
- Thomassen, R.A.; Kvammen, J.A.; Eskerud, M.B.; Júlíusson, P.B.; Henriksen, C.; Rugtveit, J. Iodine Status and Growth In 0-2-Year-Old Infants With Cow’s Milk Protein Allergy. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 806–811. [Google Scholar] [CrossRef]
- Andersson, M.; Aeberli, I.; Wüst, N.; Piacenza, A.M.; Bucher, T.; Henschen, I.; Haldimann, M.; Zimmermann, M.B. The Swiss iodized salt program provides adequate iodine for school children and pregnant women, but weaning infants not receiving iodine-containing complementary foods as well as their mothers are iodine deficient. J. Clin. Endocrinol. Metab. 2010, 95, 5217–5224. [Google Scholar] [CrossRef]
- Jin, Y.; Coad, J.; Skeaff, S.A.; Zhou, S.J.; Brough, L. Iodine status of postpartum women and their infants aged 3, 6 and 12 months: Mother and Infant Nutrition Investigation (MINI). Br. J. Nutr. 2022, 127, 570–579. [Google Scholar] [CrossRef] [PubMed]
- Mulrine, H.M.; Skeaff, S.A.; Ferguson, E.L.; Gray, A.R.; Valeix, P. Breast-milk iodine concentration declines over the first 6 mo postpartum in iodine-deficient women. Am. J. Clin. Nutr. 2010, 92, 849–856. [Google Scholar] [CrossRef]
- Murray, C.W.; Egan, S.K.; Kim, H.; Beru, N.; Bolger, P.M. US Food and Drug Administration’s Total Diet Study: Dietary intake of perchlorate and iodine. J. Expo. Sci. Environ. Epidemiol. 2008, 18, 571–580. [Google Scholar] [CrossRef]
- Skeaff, S.A.; Ferguson, E.L.; McKenzie, J.E.; Valeix, P.; Gibson, R.S.; Thomson, C.D. Are breast-fed infants and toddlers in New Zealand at risk of iodine deficiency? Nutrition 2005, 21, 325–331. [Google Scholar] [CrossRef]
- Trumbo, P.R. FDA regulations regarding iodine addition to foods and labeling of foods containing added iodine. Am. J. Clin. Nutr. 2016, 104 (Suppl. S3), 864s–867s. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Gao, H.; Zhang, X.; Zhu, M.; Liang, D.; Xiang, X. Comparative study on the essential composition content of commercial follow-up formula for older infant with the requirements in the new national food safety standard in China from 2017 to 2022. Wei Sheng Yan Jiu 2023, 52, 394–398. [Google Scholar] [CrossRef] [PubMed]
- Mason, J.B.; Deitchler, M.; Gilman, A.; Gillenwater, K.; Shuaib, M.; Hotchkiss, D.; Mason, K.; Mock, N.; Sethuraman, K. Iodine fortification is related to increased weight-for-age and birthweight in children in Asia. Food Nutr. Bull. 2002, 23, 292–308. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Sun, J.; Huang, J.; Huo, J.S. Prevalence of Malnutrition and Associated Factors of Stunting among 6-23-Month-Old Infants in Central Rural China in 2019. Int. J. Environ. Res. Public Health 2021, 18, 8165. [Google Scholar] [CrossRef] [PubMed]
- Abel, M.H.; Caspersen, I.H.; Meltzer, H.M.; Haugen, M.; Brandlistuen, R.E.; Aase, H.; Alexander, J.; Torheim, L.E.; Brantsæter, A.L. Suboptimal Maternal Iodine Intake Is Associated with Impaired Child Neurodevelopment at 3 Years of Age in the Norwegian Mother and Child Cohort Study. J. Nutr. 2017, 147, 1314–1324. [Google Scholar] [CrossRef]
- Nazeri, P.; Mirmiran, P.; Hedayati, M.; Mehrabi, Y.; Delshad, H.; Azizi, F. Can postpartum maternal urinary iodine be used to estimate iodine nutrition status of newborns? Br. J. Nutr. 2016, 115, 1226–1231. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Liu, J.; Lu, W.; Jia, W.; Li, Q.; Traore, S.S.; Lyu, Q. Iodine Deficiency of Breastfeeding Mothers and Infants from 2012 to 2019 in Zhengzhou, China. Biol. Trace Elem. Res. 2023, 201, 4298–4306. [Google Scholar] [CrossRef]
- Liu, S.; Sharp, A.; Villanueva, E.; Ma, Z.F. Breast Milk Iodine Concentration (BMIC) as a Biomarker of Iodine Status in Lactating Women and Children < 2 Years of Age: A Systematic Review. Nutrients 2022, 14, 1691–1712. [Google Scholar] [CrossRef]
- Andersen, S.L.; Møller, M.; Laurberg, P. Iodine concentrations in milk and in urine during breastfeeding are differently affected by maternal fluid intake. Thyroid 2014, 24, 764–772. [Google Scholar] [CrossRef]
| Characteristics | n | % | Mean ± SD or Median (P25–P75) | Children’s UIC (μg/L) | rs | p-Value | ||
|---|---|---|---|---|---|---|---|---|
| Median | P25 | P75 | ||||||
| Infants and toddlers | 2282 | - | - | 152.1 | 75.8 | 268.3 | ||
| Gender | 2282 | - | - | |||||
| Boys | 1203 | 52.7 | - | 148.7 | 72.8 | 261.9 | 0.213 | |
| Girls | 1079 | 47.3 | - | 155.3 | 79.7 | 279.5 | ||
| Age group | 2281 | - | 12.9 ± 1.3 | 0.897 | ||||
| 6–11 months | 1591 | 69.7 | - | 152.1 | 74.2 | 273.9 | ||
| 12–23 months | 69.0 | 30.2 | - | 152.1 | 83.6 | 250.8 | ||
| Gestational age at birth, (completed weeks) | 2233 | - | 39 (38–40) | −0.002 | 0.930 | |||
| Weight-for-length/height, z-score | 2244 | - | 0.6 ± 0.982 | 0.010 | 0.642 | |||
| <−2 (wasted) | 15 | 0.7 | −2.73 ± 0.80 | 181.5 | 65.7 | 234.4 | 0.941 | |
| >2 (overweight) | 161 | 7.1 | 2.71 ± 0.69 | 151.0 | 81.3 | 288.2 | ||
| BMI-for-age, z-score | 2233 | - | 0.59 ± 1.02 | 0.004 | 0.838 | |||
| <−2 (underweight) | 20 | 0.9 | −2.66 ± 0.62 | 187.6 | 71.1 | 250.1 | 0.957 | |
| >2 (overweight) | 163 | 7.1 | 2.82 ± 0.71 | 154.6 | 75.2 | 244.1 | ||
| Total annual household income (CNY) | 2272 | |||||||
| Low (≤149,000) | 592 | 25.9 | 156.5 | 88.0 | 268.3 | 0.132 | ||
| Medium (150,000–299,000) | 1171 | 51.3 | 147.5 | 70.8 | 263.9 | |||
| High (≥300,000) | 509 | 22.3 | 155.9 | 79.7 | 276.9 | |||
| Mothers | ||||||||
| Age (years) | 2282 | 30.5 ± 4.4 | ||||||
| <29 | 1033 | 45.3 | 152.6 | 76.5 | 268.2 | 0.784 | ||
| 30–34 | 797 | 34.9 | 149.9 | 74.2 | 260.5 | |||
| 35–39 | 382 | 16.7 | 156.0 | 78.4 | 279.6 | |||
| ≥40 | 70 | 3.1 | 149.8 | 59.6 | 272.8 | |||
| Maternal BMI (kg/m2) | 2254 | 22.2 ± 3.0 | −0.009 | 0.656 | ||||
| <18.5 | 180 | 7.9 | 161.0 | 98.7 | 255.1 | 0.322 | ||
| 18.5–24.9 | 1721 | 75.4 | 150.7 | 73.0 | 267.2 | |||
| 25–29.9 | 318 | 13.9 | 160.2 | 83.8 | 278.0 | |||
| ≥30 | 35 | 1.5 | 155.9 | 57.4 | 247.1 | |||
| Educational level | 2282 | - | - | |||||
| Junior high school or below (≤9 years) | 361 | 15.8 | 157.7 | 81.3 | 262.5 | 0.920 | ||
| High school or junior college (10–15 years) | 1035 | 45.4 | 152.9 | 74.3 | 274.4 | |||
| University or higher(≥16 years) | 886 | 38.8 | 149.7 | 75.2 | 265.8 | |||
| Birth parity | 2282 | |||||||
| Primiparous | 1398 | 61.3 | 152.3 | 73.3 | 265.8 | 0.908 | ||
| Multiparous | 884 | 38.7 | 152.0 | 80.3 | 273.4 | |||
| Smoking status | 2282 | |||||||
| No | 2260 | 99.0 | 151.9 | 75.3 | 267.2 | 0.227 | ||
| Yes | 22 | 1.0 | 177.7 | 110.4 | 296.7 | |||
| Alcohol intake during lactation | 2282 | |||||||
| Yes | 13 | 0.6 | 131.8 | 117.4 | 270.2 | 0.757 | ||
| No | 2269 | 99.4 | 152.4 | 75.5 | 267.5 | |||
| Maternal UIC (μg/L) | 2282 | - | 123.1 (62.3, 220.9) | 0.285 | <0.001 | |||
| UIC of lactating women | 588 | 25.8 | 121.3 (68.1, 206.4) | |||||
| UIC of weaning women | 1694 | 74.2 | 123.4 (58.4, 227.2) | |||||
| Feeding Behaviors | n | % | Children’s UIC (μg/L) | |||
|---|---|---|---|---|---|---|
| Median | P25th | P75th | p-Value | |||
| Feeding practice | 2282 | |||||
| +BM + FM + CF | 366 | 16.0 | 159.5 | 80.9 | 295.4 | 0.350 |
| +BM − FM + CF | 222 | 9.7 | 146.6 | 73.9 | 244.9 | |
| −BM + FM + CF | 1676 | 73.4 | 150.6 | 75.2 | 266.8 | |
| −BM − FM + CF | 18 | 0.8 | 182.6 | 52.1 | 340.5 | |
| Daily frequencies of breastfeeding | 2282 | |||||
| 0 times per day | 1694 | 74.2 | 150.9 | 75.2 | 267.0 | 0.650 |
| 1–3 times per day | 312 | 13.7 | 158.8 | 79.3 | 282.0 | |
| ≥4 times per day | 276 | 12.1 | 153.9 | 75.9 | 262.5 | |
| Duration of exclusive breastfeeding | 2279 | |||||
| 0–5 months | 1005 | 44.0 | 154.2 | 73.8 | 277.9 | 0.570 |
| 6 months | 614 | 26.9 | 150.6 | 79.6 | 270.5 | |
| ≥7 months | 660 | 28.9 | 150.4 | 76.9 | 253.5 | |
| Type of milk feeds first introduced | 2276 | |||||
| Breast milk | 1449 | 63.5 | 153.6 | 75.9 | 270.2 | 0.522 |
| Formula milk | 827 | 36.2 | 149.5 | 75.3 | 262.5 | |
| Daily consumption of formula milk in the last week | 2279 | |||||
| <500 mL per day | 1082 | 47.4 | 146.1 | 71.5 | 249.5 | 0.026 |
| ≥500 mL per day | 1195 | 52.5 | 156.2 | 79.7 | 277.9 | |
| Daily frequencies of regular complementary food | 2282 | |||||
| 1–3 times per day | 628 | 27.5 | 160.1 | 82.2 | 280.0 | 0.071 |
| ≥4 times per day | 1654 | 72.5 | 148.1 | 73.9 | 263.5 | |
| Addition of salt to the infants’ food | 2282 | |||||
| Iodized salt | 798 | 35.0 | 156.1 | 82.0 | 276.4 | 0.223 |
| Never or non-iodized salt | 1484 | 65.0 | 149.7 | 73.9 | 265.3 | |
| Condiments already introduced | 2282 | |||||
| Yes | 427 | 18.7 | 151.9 | 80.0 | 272.7 | 0.690 |
| No | 1855 | 81.3 | 152.1 | 75.2 | 267.0 | |
| Iodine-containing supplements used | 2282 | |||||
| No | 2238 | 98.1 | 151.9 | 75.2 | 268.2 | 0.402 |
| Yes | 44 | 1.9 | 176.1 | 106.7 | 262.6 | |
| Iodine-Rich Foods | n | At Least 1 Time per Day | 1–3 Times per Week | 1–3 Times per Month | Never/Rarely |
|---|---|---|---|---|---|
| Eggs | 2215 | 1064 (70.3) | 471 (20.6) | 61 (2.7) | 79 (3.5) |
| Infant formula | 2282 | 1890 (82.8) | 67 (2.9) | 49 (2.1) | 276 (12.1) |
| Fish | 2215 | 227 (9.9) | 1356 (59.4) | 454 (19.9) | 178 (7.8) |
| Livestock and poultry meat | 2215 | 780 (34.2) | 1046 (45.8) | 251 (11.0) | 138 (6.0) |
| Milk or other animal milk | 2282 | 397 (17.4) | 203 (8.9) | 167 (7.3) | 1515 (66.4) |
| Cheese | 2214 | 60 (2.6) | 109 (4.8) | 244 (10.7) | 1801 (78.9) |
| Laver | 2282 | 24 (1.1) | 228 (10.0) | 405 (17.7) | 1625 (71.2) |
| Seaweed | 2282 | 7 (0.3) | 83 (3.6) | 246 (10.8) | 1946 (85.3) |
| Dried small shrimp | 2282 | 32 (1.4) | 260 (11.4) | 423 (18.5) | 1567 (68.7) |
| Dried mussel | 2282 | 5 (0.2) | 24 (1.1) | 127 (5.6) | 2126 (93.2) |
| Variables | Coefficients (95%CI) | ||||
|---|---|---|---|---|---|
| 0.10 Quantile | 0.25 Quantile | 0.5 Quantile | 0.75 Quantile | 0.90 Quantile | |
| Maternal UIC | 0.094 (0.079, 0.108) *** | 0.133 (0.110, 0.155) *** | 0.251 (0.217, 0.284) *** | 0.385 (0.327, 0.442) *** | 0.491 (0.392, 0.591) *** |
| Maternal BMI | 0.124 (−0.856, 1.104) | −0.562 (−2.072, 0.948) | −0.283 (−2.582, 2.016) | −1.286 (−5.186, 2.613) | −6.004 (−12.781, 0.773) |
| Maternal age (years) | |||||
| <29 | 6.143 (−10.804, 23.091) | 6.997 (−19.104, 33.098) | −10.608 (−50.352, 29.135) | −5.590 (−72.998, 61.818) | 39.049 (−78.096, 156.194) |
| 30–34 | 8.997 (−8.095, 26.088) | 9.745 (−16.577, 36.067) | −2.033 (−42.113, 38.047) | −5.627 (−73.606, 62.352) | −3.414 (−121.552, 114.724) |
| 38–39 | 4.855 (−12.910, 22.620) | 12.285 (−15.074, 39.645) | −0.870 (−42.530, 40.790) | 30.279 (−40.380, 100.937) | 74.326 (−48.468, 197.121) |
| ≥40 | ref | ||||
| Maternal education level (years) | |||||
| Junior high school or below (≤9) | −5.702 (−14.949, 3.546) | −10.551 (−24.793, 3.691) | −6.871 (−28.558, 14.815) | −10.628 (−47.409, 26.154) | −11.576 (−75.497, 52.345) |
| High school or junior college (10–15) | −9.213 (−15.689, −2.738) ** | −8.720 (−18.692, 1.252) | 8.105 (−7.080, 23.289) | −0.110 (−25.864, 25.644) | −6.704 (−51.461, 38.052) |
| University or higher (≥16) | ref | ||||
| House Income (CNY) | |||||
| Low (≤149,000) | 3.687 (−5.117, 12.490) | 8.202 (−5.356, 21.760) | −1.678 (−22.323, 18.966) | 6.631 (−28.384, 41.654) | −33.497 (−94.347, 27.353) |
| Medium (150,000–299,000) | −5.785 (−13.131, 1.560) | −3.207 (−14.520, 8.106) | −7.906 (−25.132, 9.319) | −0.342 (−29.558, 28.874) | −11.577 (−62.350, 39.196) |
| High (≥300,000) | ref | ||||
| Children’s age (months) | −0.207 (−2.519, 2.104) | −1.502 (−5.062, 2.058) | −1.535 (−6.956, 3.886) | −11.998 (−21.193, −2.804) * | −20.642 (−36.620, −4.664) * |
| Children’s gender | |||||
| Male | −0.229 (−5.978, 5.521) | −0.157 (−9.011, 8.697) | −11.090 (−24.572, 2.392) | −5.195 (−28.062, 17.672) | −4.979 (−44.717, 34.760) |
| Female | ref | ||||
| Salt category | |||||
| Iodized salt | 6.295 (0.188, 12.402) * | 3.998 (−5.408, 13.403) | 7.200 (−7.121, 21.521) | 15.421 (−8.869, 39.710) | 20.222 (−21.990, 62.434) |
| Never or non-iodized salt | ref | ||||
| Iodine-containing supplement use | |||||
| No | −25.963 (−46.646,−5.279) * | −29.007 (−60.862, 2.848) | −23.532 (−72.037, 24.973) | −28.491 (−110.759, 53.777) | 47.466 (−95.504, 190.435) |
| Yes | ref | ||||
| Feeding practice | |||||
| +BM + FM + CF | 0.671(−11.188, 12.530) | 3.917 (−14.346, 22.181) | −8.158 (−35.968, 19.651) | −20.887 (−68.054, 26.280) | −86.285 (−168.254, −4.316) * |
| +BM − FM + CF | 3.854(−29.955, 37.663) | −14.831 (−66.900, 37.238) | 33.075 (−46.209, 112.359) | 48.191 (−86.280, 182.663) | −32.062 (−265.754, 201.631) |
| −BM + FM + CF | −3.124(−11.262, 5.014) | −4.045 (−16.579, 8.488) | −9.619 (−28.704, 9.466) | −16.419 (−48.788, 15.950) | −97.740 (−153.992, −41.488) ** |
| −BM − FM + CF | ref | ||||
| Daily consumption of formula milk in the last week | |||||
| <500 mL per day | −9.427(−15.828, −3.027) ** | −5.225 (−15.082, 4.632) | −6.899 (−21.908, 8.110) | −19.937 (−45.394, 5.519) | −8.775 (−53.015, 35.465) |
| ≥500 mL per day | ref | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, W.; Si, J.; Han, X.; Zheng, W.; Li, X.; Zhu, C.; Zang, J. Iodine Status of Infants and Toddlers under 2 Years of Age and Its Association with Feeding Behaviors and Maternal Iodine Status in Shanghai: A Quantile Regression Analysis. Nutrients 2024, 16, 1686. https://doi.org/10.3390/nu16111686
Zhou W, Si J, Han X, Zheng W, Li X, Zhu C, Zang J. Iodine Status of Infants and Toddlers under 2 Years of Age and Its Association with Feeding Behaviors and Maternal Iodine Status in Shanghai: A Quantile Regression Analysis. Nutrients. 2024; 16(11):1686. https://doi.org/10.3390/nu16111686
Chicago/Turabian StyleZhou, Wei, Jingyi Si, Xue Han, Weiwei Zheng, Xiangting Li, Changfeng Zhu, and Jiajie Zang. 2024. "Iodine Status of Infants and Toddlers under 2 Years of Age and Its Association with Feeding Behaviors and Maternal Iodine Status in Shanghai: A Quantile Regression Analysis" Nutrients 16, no. 11: 1686. https://doi.org/10.3390/nu16111686
APA StyleZhou, W., Si, J., Han, X., Zheng, W., Li, X., Zhu, C., & Zang, J. (2024). Iodine Status of Infants and Toddlers under 2 Years of Age and Its Association with Feeding Behaviors and Maternal Iodine Status in Shanghai: A Quantile Regression Analysis. Nutrients, 16(11), 1686. https://doi.org/10.3390/nu16111686






