High Serum Phosphate Is Associated with Cardiovascular Mortality and Subclinical Coronary Atherosclerosis: Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
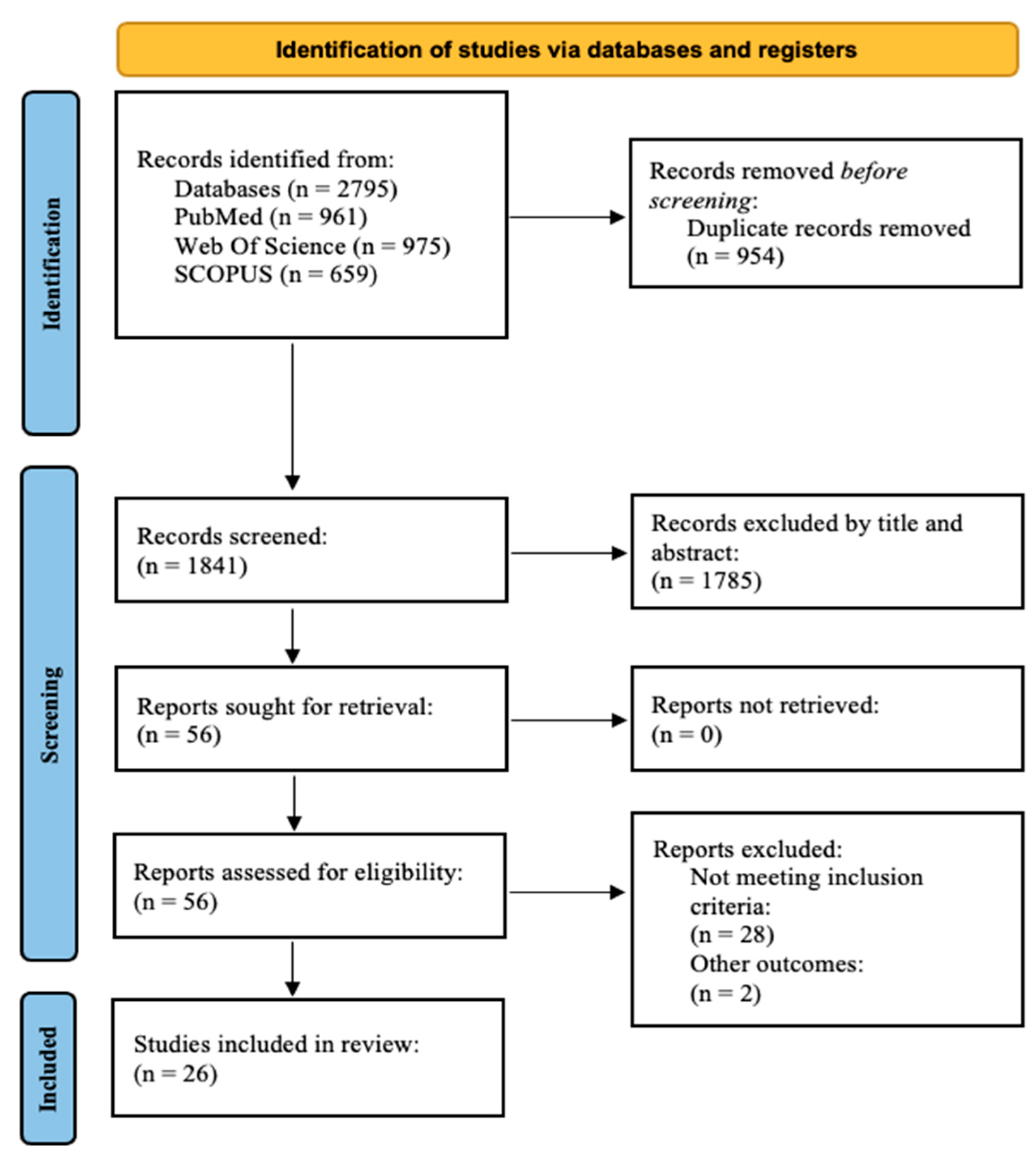
2.1. Search Strategy and Selection Criteria
2.2. Study Selection
2.3. Data Extraction and Risk of Bias Assessment
2.4. Statistical Analysis
3. Results
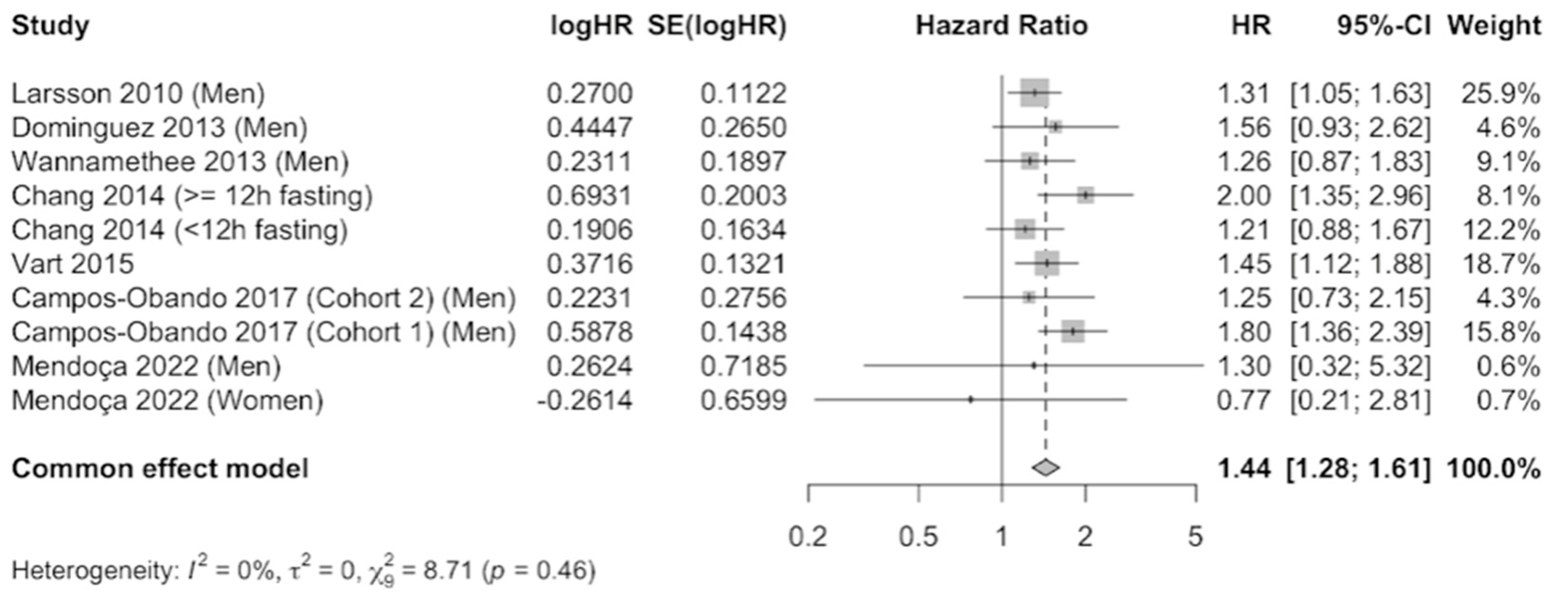
3.1. Cardiovascular Mortality
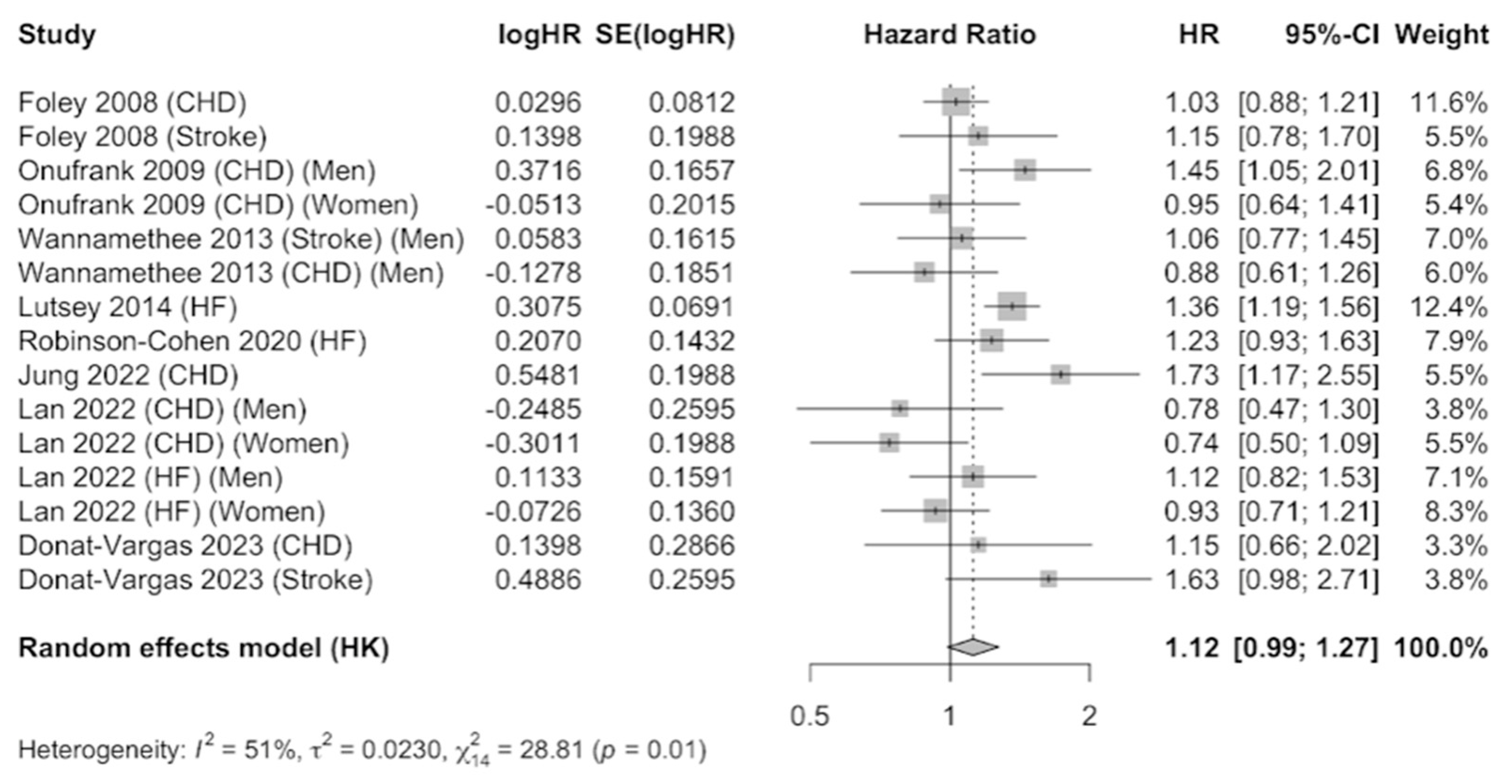
3.2. Cardiovascular Diseases
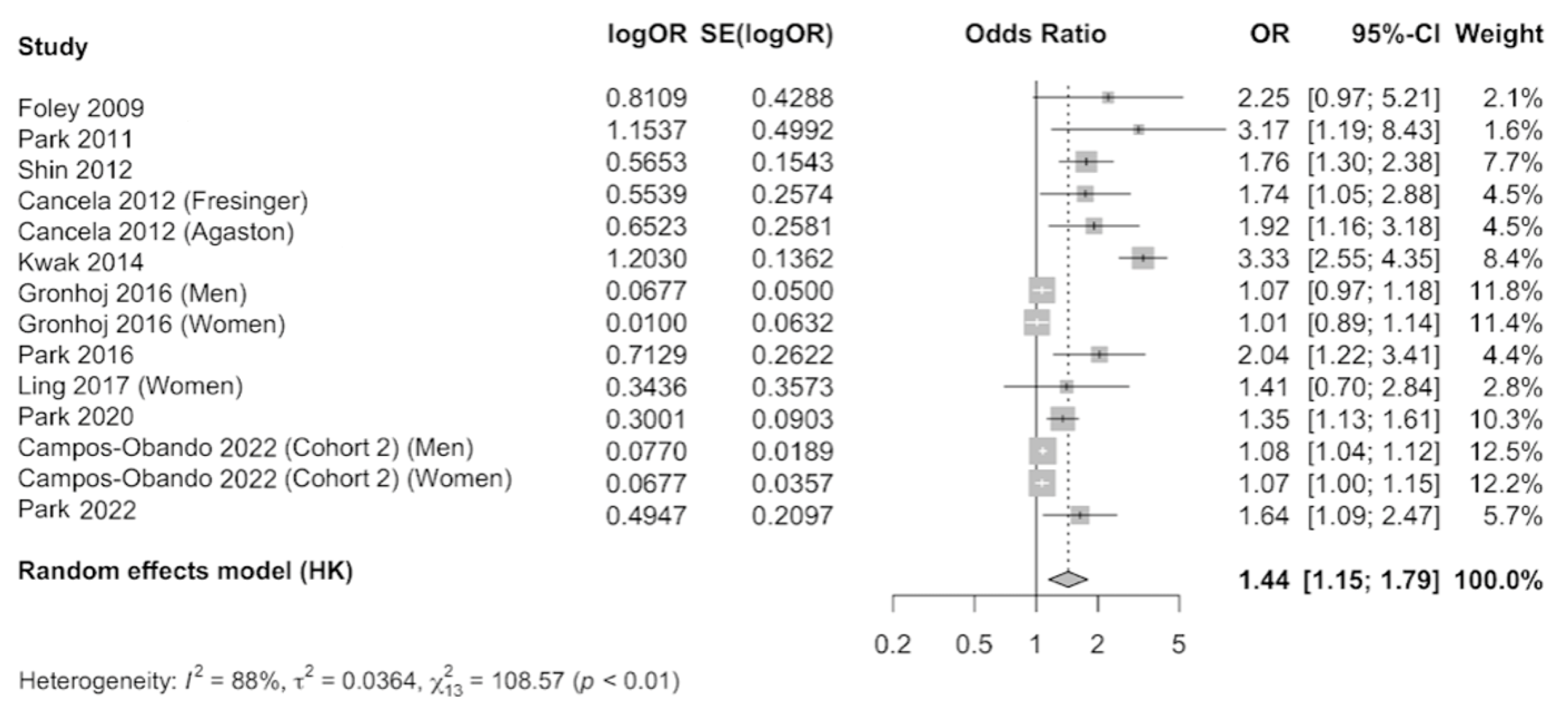
3.3. Subclinical Coronary Atherosclerosis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Grønhøj, M.H.; Gerke, O.; Mickley, H.; Hald, F.; Lambrechtsen, J.; Sand, N.P.R.; Rasmussen, L.M.; Olsen, M.H.; Diederichsen, A. Associations between Calcium-Phosphate Metabolism and Coronary Artery Calcification; a Cross Sectional Study of a Middle-Aged General Population. Atherosclerosis 2016, 251, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Xia, C.; Vonder, M.; Sidorenkov, G.; Den Dekker, M.; Oudkerk, M.; Van Bolhuis, J.N.; Pelgrim, G.J.; Rook, M.; De Bock, G.H.; Van Der Harst, P.; et al. Cardiovascular Risk Factors and Coronary Calcification in a Middle-Aged Dutch Population: The ImaLife Study. J. Thorac. Imaging 2021, 36, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Vliegenthart, R.; Oudkerk, M.; Hofman, A.; Oei, H.H.S.; Van Dijck, W.; Van Rooij, F.J.A.; Witteman, J.C.M. Coronary Calcification Improves Cardiovascular Risk Prediction in the Elderly. Circulation 2005, 112, 572–577. [Google Scholar] [CrossRef] [PubMed]
- Gregory, R.; Gregory, M.; Catherine, J.; Giovanni, A.; Enrico, A.; Larry, B.; Noël, B.; Andrea, B. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2020 Update a Report from the American Heart Association. Circulation 2020, 141, E139–E596. [Google Scholar] [CrossRef] [PubMed]
- Vikulova, D.N.; Grubisic, M.; Zhao, Y.; Lynch, K.; Humphries, K.H.; Pimstone, S.N.; Brunham, L.R. Premature Atherosclerotic Cardiovascular Disease: Trends in Incidence, Risk Factors, and Sex-Related Differences, 2000 to 2016. J. Am. Heart Assoc. 2019, 8, e012178. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.W.F.; D’agostino, R.B.; Levy, D.; Belanger, A.M.; Silbershatz, H.; Kannel, W.B. Prediction of Coronary Heart Disease Using Risk Factor Categories. Circulation 1998, 97, 1837–1847. [Google Scholar] [CrossRef] [PubMed]
- Conroy, R.M.; Pyörälä, K.; Fitzgerald, A.P.; Sans, S.; Menotti, A.; De Backer, G.; De Bacquer, D.; Ducimetière, P.; Jousilahti, P.; Keil, U.; et al. Estimation of Ten-Year Risk of Fatal Cardiovascular Disease in Europe: The SCORE Project. Eur. Heart J. 2003, 24, 987–1003. [Google Scholar] [CrossRef]
- Sheridan, K.; Logomarsino, J.V. Effects of Serum Phosphorus on Vascular Calcification in a Healthy, Adult Population: A Systematic Review. J. Vasc. Nurs. 2017, 35, 157–169. [Google Scholar] [CrossRef]
- Zhou, C.; Shi, Z.; Ouyang, N.; Ruan, X. Hyperphosphatemia and Cardiovascular Disease. Front. Cell. Dev. Biol. 2021, 9, 644363. [Google Scholar] [CrossRef]
- Villa-Bellosta, R. Vascular Calcification: Key Roles of Phosphate and Pyrophosphate. Int. J. Mol. Sci. 2021, 22, 13536. [Google Scholar] [CrossRef]
- Chonchol, M.; Dale, R.; Schrier, R.W.; Estacio, R. Serum Phosphorus and Cardiovascular Mortality in Type 2 Diabetes. Am. J. Med. 2009, 122, 380–386. [Google Scholar] [CrossRef]
- Volk, C.; Schmidt, B.; Brandsch, C.; Kurze, T.; Schlegelmilch, U.; Grosse, I.; Ulrich, C.; Girndt, M.; Stangl, G.I. Acute Effects of an Inorganic Phosphorus Additive on Mineral Metabolism and Cardiometabolic Risk Factors in Healthy Subjects. J. Clin. Endocrinol. Metab. 2022, 107, E852–E864. [Google Scholar] [CrossRef]
- Ling, Y.; Wang, Z.; Wu, B.; Gao, X. Association of Bone Metabolism Markers with Coronary Atherosclerosis and Coronary Artery Disease in Postmenopausal Women. J. Bone Miner. Metab. 2017, 36, 352–363. [Google Scholar] [CrossRef]
- Younes, M.; Aquilina, G.; Castle, L.; Engel, K.H.; Fowler, P.; Frutos Fernandez, M.J.; Fürst, P.; Gürtler, R.; Husøy, T.; Mennes, W.; et al. Re-Evaluation of Phosphoric Acid–Phosphates–Di-, Tri- and Polyphosphates (E 338–341, E 343, E 450–452) as Food Additives and the Safety of Proposed Extension of Use. EFSA J. 2019, 17, e05674. [Google Scholar] [CrossRef]
- Ritz, E.; Hahn, K.; Ketteler, M.; Kuhlmann, M.K.; Mann, J. Phosphate Additives in Food—A Health Risk. Dtsch. Arztebl. Int. 2012, 109, 49–55. [Google Scholar] [CrossRef]
- Calvo, M.S.; Uribarri, J. Contributions to Total Phosphorus Intake: All Sources Considered. Semin. Dial. 2013, 26, 54–61. [Google Scholar] [CrossRef]
- McCarty, M.F.; DiNicolantonio, J.J. Bioavailable Dietary Phosphate, a Mediator of Cardiovascular Disease, May Be Decreased with Plant-Based Diets, Phosphate Binders, Niacin, and Avoidance of Phosphate Additives. Nutrition 2014, 30, 739–747. [Google Scholar] [CrossRef]
- Cupisti, A.; Kalantar-Zadeh, K. Management of Natural and Added Dietary Phosphorus Burden in Kidney Disease. Semin. Nephrol. 2013, 33, 180–190. [Google Scholar] [CrossRef]
- Chang, A.R.; Anderson, C. Dietary Phosphorus Intake and the Kidney. Annu. Rev. Nutr. 2017, 37, 321–346. [Google Scholar] [CrossRef]
- Standing Committee on the Scientific Evaluation of Dietary Reference Intakes; Institute of Medicine (US). Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride; National Academies Press: Washington, DC, USA, 1997; ISBN 0-309-06350-7. [Google Scholar]
- Campos-Obando, N.; Lahousse, L.; Brusselle, G.; Stricker, B.H.; Hofman, A.; Franco, O.H.; Uitterlinden, A.G.; Zillikens, M.C. Serum Phosphate Levels Are Related to All-Cause, Cardiovascular and COPD Mortality in Men. Eur. J. Epidemiol. 2018, 33, 859–871. [Google Scholar] [CrossRef] [PubMed]
- Palmer, S.C.; ChB, M.; Hayen, A.; Macaskill, P.; Pellegrini, F.; Craig, J.C.; Elder, G.J.; Strippoli, M.G.F.; Renal Group, C.; Craig, A. Serum Levels of Phosphorus, Parathyroid Hormone, and Calcium and Risks of Death and Cardiovascular Disease in Individuals with Chronic Kidney Disease A Systematic Review and Meta-Analysis. JAMA 2011, 305, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Bai, W.; Li, J.; Liu, J. Serum Phosphorus, Cardiovascular and All-Cause Mortality in the General Population: A Meta-Analysis. Clin. Chim. Acta 2016, 461, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Park, K.S.; Lee, H.; Jeon, Y.-J.; Park, S.; Ann, S.H.; Kim, Y.-G.; Lee, Y.; Park, J.; Choi, S.H.; Park, G.-M. Serum Phosphorus and Subclinical Coronary Atherosclerosis in Asymptomatic Subjects without Kidney Dysfunction. Clin. Nephrol. 2022, 98, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Campos-Obando, N.; Bosman, A.; Kavousi, M.; Medina-Gomez, C.; van der Eerden, B.C.J.; Bos, D.; Franco, O.H.; Uitterlinden, A.G.; Zillikens, M.C. Genetic Evidence for a Causal Role of Serum Phosphate in Coronary Artery Calcification: The Rotterdam Study. J. Am. Heart Assoc. 2022, 11, e023024. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-Analysis of Observational Studies in Epidemiology: A Proposal for Reporting. Meta-Analysis of Observational Studies in Epidemiology (MOOSE) Group. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- Joanna Briggs Institute Critical-Appraisal-Tools—Critical Appraisal Tools|JBI. Available online: https://jbi.global/critical-appraisal-tools (accessed on 12 April 2023).
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in Meta-Analysis Detected by a Simple, Graphical Test. Br. Med. J. 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Abramowitz, M.; Muntner, P.; Coco, M.; Southern, W.; Lotwin, I.; Hostetter, T.H.; Melamed, M.L. Serum Alkaline Phosphatase and Phosphate and Risk of Mortality and Hospitalization. Clin. J. Am. Soc. Nephrol. 2010, 5, 1064–1071. [Google Scholar] [CrossRef]
- McGovern, A.P.; de Lusignan, S.; van Vlymen, J.; Liyanage, H.; Tomson, C.R.; Gallagher, H.; Rafiq, M.; Jones, S. Serum Phosphate as a Risk Factor for Cardiovascular Events in People with and without Chronic Kidney Disease: A Large Community Based Cohort Study. PLoS ONE 2013, 8, e74996. [Google Scholar] [CrossRef]
- Dominguez, J.R.; Kestenbaum, B.; Chonchol, M.; Block, G.; Laughlin, G.A.; Lewis, C.E.; Katz, R.; Barrett-Connor, E.; Cummings, S.; Orwoll, E.S.; et al. Relationships between Serum and Urine Phosphorus with All-Cause and Cardiovascular Mortality: The Osteoporotic Fractures in Men (MrOS) Study. Am. J. Kidney Dis. 2013, 61, 555–563. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.R.; Grams, M.E. Serum Phosphorus and Mortality in the Third National Health and Nutrition Examination Survey (NHANES III): Effect Modification by Fasting. Am. J. Kidney Dis. 2014, 64, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Larsson, T.E.; Olauson, H.; Hagström, E.; Ingelsson, E.; Ärnlöv, J.; Lind, L.; Sundström, J. Conjoint Effects of Serum Calcium and Phosphate on Risk of Total, Cardiovascular, and Noncardiovascular Mortality in the Community. Arterioscler. Thromb. Vasc. Biol. 2010, 30, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Vart, P.; Nigatu, Y.T.; Jaglan, A.; van Zon, S.K.R.; Shafique, K. Joint Effect of Hypertension and Elevated Serum Phosphorus on the Risk of Mortality in National Health and Nutrition Examination Survey-III. J. Am. Heart Assoc. 2015, 4, e001706. [Google Scholar] [CrossRef]
- Mendonça, L.; Gonçalves, F.; Sampaio, S.; Castro-Chaves, P.; Pereira, L. Association between Serum Phosphorus and Mortality in NHANES 2003–2006: The Effect of Gender and Renal Function. J. Nephrol. 2022, 35, 165–178. [Google Scholar] [CrossRef]
- Wannamethee, S.G.; Sattar, N.; Papcosta, O.; Lennon, L.; Whincup, P.H. Alkaline Phosphatase, Serum Phosphate, and Incident Cardiovascular Disease and Total Mortality in Older Men. Arterioscler. Thromb. Vasc. Bio. 2013, 33, 1070–1076. [Google Scholar] [CrossRef]
- Lan, Q.; Zhang, Y.; Lin, F.; Meng, Q.; Buys, N.; Fan, H.; Sun, J. Sex-Specific Associations Between Serum Phosphate Concentration and Cardiometabolic Disease. Diabetes Metab. Syndr. Obes. 2022, 15, 813–826. [Google Scholar] [CrossRef]
- Jung, D.H.; Park, B.; Lee, Y.J. Longitudinal Effects of Serum Calcium and Phosphate Levels and Their Ratio on Incident Ischemic Heart Disease among Korean Adults. Biomolecules 2022, 12, 103. [Google Scholar] [CrossRef]
- Robinson-Cohen, C.; Shlipak, M.; Sarnak, M.; Katz, R.; Peralta, C.; Young, B.; Hoofnagle, A.N.; Szklo, M.; Ix, J.H.; Psaty, B.M.; et al. Impact of Race on the Association of Mineral Metabolism with Heart Failure: The Multi-Ethnic Study of Atherosclerosis. J. Clin. Endocrinol. Metab. 2020, 105, E1144–E1151. [Google Scholar] [CrossRef]
- Foley, R.N.; Collins, A.J.; Ishani, A.; Kalra, P.A. Calcium-Phosphate Levels and Cardiovascular Disease in Community-Dwelling Adults: The Atherosclerosis Risk in Communities (ARIC) Study. Am. Heart J. 2008, 156, 556–563. [Google Scholar] [CrossRef]
- Lutsey, P.L.; Alonso, A.; Michos, E.D.; Loehr, L.R.; Astor, B.C.; Coresh, J.; Folsom, A.R. Serum Magnesium, Phosphorus, and Calcium Are Associated with Risk of Incident Heart Failure: The Atherosclerosis Risk in Communities (ARIC) Study. Am. J. Clin. Nutr. 2014, 100, 756–764. [Google Scholar] [CrossRef]
- Donat-Vargas, C.; Guallar-Castillon, P.; Nyström, J.; Larsson, S.C.; Kippler, M.; Vahter, M.; Faxén-Irving, G.; Michaelsson, K.; Wolk, A.; Stenvinkel, P.; et al. Urinary Phosphate Is Associated with Cardiovascular Disease Incidence. J. Intern. Med. 2023, 294, 358–369. [Google Scholar] [CrossRef]
- Onufrak, S.J.; Bellasi, A.; Cardarelli, F.; Vaccarino, V.; Muntner, P.; Shaw, L.J.; Raggi, P. Investigation of Gender Heterogeneity in the Associations of Serum Phosphorus with Incident Coronary Artery Disease and All-Cause Mortality. Am. J. Epidemiol. 2009, 169, 67–77. [Google Scholar] [CrossRef]
- Cancela, A.L.; Santos, R.D.; Titan, S.M.; Goldenstein, P.T.; Rochitte, C.E.; Lemos, P.A.; dos Reis, L.M.; Graciolli, F.G.; Jorgetti, V.; Moysés, R.M. Phosphorus Is Associated with Coronary Artery Disease in Patients with Preserved Renal Function. PLoS ONE 2012, 7, e36883. [Google Scholar] [CrossRef]
- Park, K.S.; Park, J.; Choi, S.H.; Ann, S.H.; Singh, G.B.; Shin, E.S.; Lee, J.S.; Chung, H.C. Serum Phosphorus Concentration and Coronary Artery Calcification in Subjects without Renal Dysfunction. PLoS ONE 2016, 11, e0151007. [Google Scholar] [CrossRef]
- Park, K.S.; Chang, J.W.; Kim, T.Y.; Kim, H.W.; Lee, E.K.; Kim, H.S.; Yang, W.S.; Kim, S.B.; Park, S.K.; Lee, S.K.; et al. Lower Concentrations of Serum Phosphorus within the Normal Range Could Be Associated with Less Calcification of the Coronary Artery in Koreans with Normal Renal Function. Am. J. Clin. Nutr. 2011, 94, 1465–1470. [Google Scholar] [CrossRef]
- Shin, S.; Kim, K.J.; Chang, H.J.; Cho, I.; Kim, Y.J.; Choi, B.W.; Rhee, Y.; Lim, S.K.; Yang, W.I.; Shim, C.Y.; et al. Impact of Serum Calcium and Phosphate on Coronary Atherosclerosis Detected by Cardiac Computed Tomography. Eur. Heart J. 2012, 33, 2873–2881. [Google Scholar] [CrossRef]
- Foley, R.N.; Collins, A.J.; Herzog, C.A.; Ishani, A.; Kalra, P.A. Serum Phosphorus Levels Associate with Coronary Atherosclerosis in Young Adults. J. Am. Soc. Nephrol. 2009, 20, 397–404. [Google Scholar] [CrossRef]
- Park, K.S.; Lee, Y.; Park, G.M.; Park, J.H.; Kim, Y.G.; Yang, D.H.; Kang, J.W.; Lim, T.H.; Kim, H.K.; Choe, J.; et al. Association between Serum Phosphorus and Subclinical Coronary Atherosclerosis in Asymptomatic Korean Individuals without Kidney Dysfunction. Am. J. Clin. Nutr. 2020, 112, 66–73. [Google Scholar] [CrossRef]
- Kwak, S.M.; Kim, J.S.; Choi, Y.; Chang, Y.; Kwon, M.J.; Jung, J.G.; Jeong, C.; Ahn, J.; Kim, H.S.; Shin, H.; et al. Dietary Intake of Calcium and Phosphorus and Serum Concentration in Relation to the Risk of Coronary Artery Calcification in Asymptomatic Adults. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 1763–1769. [Google Scholar] [CrossRef]
- Bringhurst, F.; Demay, M.; Krane, S.; Kronenberg, H. Bone and Mineral Metabolism in Health and Disease. In Harrison’s Principles of Internal Medicine, 20th ed.; Kasper, D., Fauci, A., Hauser, S., Longo, D., Jameson, J., Lozcalzo, J., Eds.; McGraw-Hill Education: New York, NY, USA, 2018; Available online: https://accessmedicine.mhmedical.com/content.aspx?bookid=2129§ionid=192530305 (accessed on 10 April 2023).
- Chang, A.R.; Lazo, M.; Appel, L.J.; Gutiérrez, O.M.; Grams, M.E. High Dietary Phosphorus Intake Is Associated with All-Cause Mortality: Results from NHANES III1-3. Am. J. Clin. Nutr. 2014, 99, 320–327. [Google Scholar] [CrossRef]
- Mertens, E.; Colizzi, C.; Peñalvo, J.L. Ultra-Processed Food Consumption in Adults across Europe. Eur. J. Nutr. 2022, 61, 1521–1539. [Google Scholar] [CrossRef]
- Huybrechts, I.; Rauber, F.; Nicolas, G.; Casagrande, C.; Kliemann, N.; Wedekind, R.; Biessy, C.; Scalbert, A.; Touvier, M.; Aleksandrova, K.; et al. Characterization of the Degree of Food Processing in the European Prospective Investigation into Cancer and Nutrition: Application of the Nova Classification and Validation Using Selected Biomarkers of Food Processing. Front. Nutr. 2022, 9, 1035580. [Google Scholar] [CrossRef]
- Gutiérrez, O.M. Sodium- and Phosphorus-Based Food Additives: Persistent but Surmountable Hurdles in the Management of Nutrition in Chronic Kidney Disease. Adv. Chronic Kidney Dis. 2013, 20, 150–156. [Google Scholar] [CrossRef]
- Ferraro, S.; Benedetti, S.; Mannarino, S.; Marcovina, S.; Biganzoli, E.M.; Zuccotti, G. Prediction of atherosclerotic cardiovascular risk in early childhood. Clin. Chim. Acta 2024, 552, 117684. [Google Scholar] [CrossRef]
- Kestenbaum, B. Phosphate Metabolism in the Setting of Chronic Kidney Disease: Significance and Recommendations for Treatment. Semin. Dial. 2007, 20, 286–294. [Google Scholar] [CrossRef]
- Sun, Q.; Bertrand, K.A.; Franke, A.A.; Rosner, B.; Curhan, G.C.; Willett, W.C. Reproducibility of Urinary Biomarkers in Multiple 24-h Urine Samples. Am. J. Clin. Nutr. 2017, 105, 159–168. [Google Scholar] [CrossRef]
- Karp, H.J.; Vaihia, K.P.; Kärkkäinen, M.U.M.; Niemistö, M.J.; Lamberg-Allardt, C.J.E. Acute Effects of Different Phosphorus Sources on Calcium and Bone Metabolism in Young Women: A Whole-Foods Approach. Calcif. Tissue Int. 2007, 80, 251–258. [Google Scholar] [CrossRef]
- Laflamme, D.; Backus, R.; Brown, S.; Butterwick, R.; Czarnecki-Maulden, G.; Elliott, J.; Fascetti, A.; Polzin, D. A Review of Phosphorus Homeostasis and the Impact of Different Types and Amounts of Dietary Phosphate on Metabolism and Renal Health in Cats. J. Vet. Intern. Med. 2020, 34, 2187–2196. [Google Scholar] [CrossRef] [PubMed]
- Shuto, E.; Taketani, Y.; Tanaka, R.; Harada, N.; Isshiki, M.; Sato, M.; Nashiki, K.; Amo, K.; Yamamoto, H.; Higashi, Y.; et al. Dietary Phosphorus Acutely Impairs Endothelial Function. J. Am. Soc. Nephrol. 2009, 20, 1504–1512. [Google Scholar] [CrossRef] [PubMed]
- Jono, S.; Mckee, M.D.; Murry, C.E.; Shioi, A.; Nishizawa, Y.; Mori, K.; Morii, H.; Giachelli, C.M. Phosphate regulation of vascular smooth muscle cell calcification. Circ. Res. 2000, 87, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Christou, G.A. Not Only the Status of Body Weight and Metabolic Health Matters for Cardiovascular Events, but Also the Temporal Changes. Eur. J. Prev. Cardiol. 2021, 28, E25–E27. [Google Scholar] [CrossRef] [PubMed]
| PubMed | ((“Phosphates/blood” [Mesh] OR “Phosphorus/blood” [Mesh]) AND (“Cardiovascular Mortality” OR “Cardiovascular Diseases” [Mesh] OR “Stroke” [Mesh] OR “Atherosclerosis” [Mesh] OR “Coronary Artery Disease” [Mesh] OR “Carotid Artery Diseases” [Mesh] OR “Coronary Disease” [Mesh] OR “Femoral Artery Diseases”)) AND ((English [Filter] OR Spanish [Filter]) AND (Humans [Filter])). |
| SCOPUS | TITLE-ABS-KEY (“Serum Phosphate” OR “Serum Phosphorus” OR “Plasma Phosphate” OR “Plasma Phosphorus”) AND TITLE-ABS-KEY (“Cardiovascular Mortality” OR “Cardiovascular Disease” OR “Stroke” OR “Atherosclerosis” OR “Coronary Artery Disease” OR “Carotid Artery Disease” OR “Coronary Disease” OR “Femoral Artery Disease”) AND LANGUAGE (English) OR LANGUAGE (Spanish) AND (LIMIT-TO (SRCTYPE, “j”)) AND (LIMIT-TO (DOCTYPE, “ar”) OR LIMIT-TO (DOCTYPE, “re”)) AND (LIMIT-TO (LANGUAGE, “English”) OR LIMIT TO (LANGUAGE, “Spanish”)). |
| Web Of Science | (“Serum Phosphate” OR “Serum Phosphorus” OR “Plasma Phosphate” OR “Plasma Phosphorus” (Topic)) AND (“Cardiovascular Mortality” OR “Cardiovascular Disease” OR “Stroke” OR “Atherosclerosis” OR “Coronary Artery Disease” OR “ Carotid Artery Disease” OR “Coronary Disease” OR “Femoral Artery Disease” (Topic)) AND (English OR Spanish (Language)) AND (Article OR Review Article (Document Types)). |
| Author (Year) | Country (Sample) | Sample Size | Men (%) | Age | Follow-Up | Nº of Cases | Results | Adjustment for Confounders | Quality Score (JBI Checklist) |
|---|---|---|---|---|---|---|---|---|---|
| Mendoça et al. (2022) [38] | U.S.A. (NHANES 2003–2006) | 5698 | 44% | 18 y | 81 months | N/A (n total = 141) | HR (95% CI) (T2 vs. T3) Men: 1.30 (0.32– 5.35) Women: 0.77 (0.21– 2.79) | Age, sex, poverty–income ratio, education, BMI, eGRF rate, albumin–creatinine ratio, non–HDL cholesterol, C-reactive protein, albumin, protein intake, HTA, diabetes, history of MI, history of stroke and smoking status, PTH, 25-hydroxyvitamin D, serum Ca, dietary Ca, and dietary phosphorus. | 9/11 (JBI: 9, 10) Included |
| Campos- Obando et al. (2017) [22] | The Netherlands (Rotterdam Study Cohort I and II (RS I and II) | 2710 RS-I: 1577 RS-II: 1133 | 100% | ≥55 y | RS-I: 22 y RS-II: 12 y | RS-I: 266 RS-II: 77 | HR (95% CI) per 1 mg/dL increase in P levels. RS-I: 1.80 (1.35–2.39) RS-II: 1.25 (0.73– 2.15) | Age, BMI, and smoking. | 9/11 (JBI: 9, 10) Included |
| Vart et al. (2015) [37] | U.S.A. (NHANES 1988–1994) | 15,833 | N/A | 18 y | 14.3 y | 1691 | HR (95% CI) (<4.2 vs. 4.2 mg/dL) 1.45 (1.12–1.88) | Age, gender, race, and eGRF rate. | 10/11 (JBI: 10) Included |
| Chang et al. (2014) [35] | U.S.A. (NHANES 1988–1994) | 12,984 <12 h fasting: 6312 12 h fasting: 6633 | <12 h fasting: 47.5% ≥12 h fasting: 48.2% | 20 y | 14.3 y | N/A | HR (95% CI) (Q4 vs. Q1) <12 h fasting: 1.21 (0.88–1.67) ≥12 h fasting: 2.00 (1.36–2.96) | Examination session (morning vs. afternoon/evening), age, sex, race, ethnicity, poverty–income ratio, body mass index, systolic blood pressure, diabetes, smoking status, physical activity, non-HDL cholesterol level, log albumin–creatinine ratio, eGRF rate, and vitamin D status. | 10/11 (JBI: 10) Included |
| Dominguez et al. (2013) [34] | U.S.A. Osteoporotic Fractures in Men (MrOS) Study | 670 | 100% | 65 y | 9.3 y | N/A | HR (95% CI) (Q4 vs. Q1) 1.56 (0.93–2.62) | Age and race, eGRF rate, microalbuminuria (yes/no), prevalent CVD, diabetes, systolic blood pressure, blood pressure medication use, tobacco use (current, former, never), BMI, total cholesterol level, HDL cholesterol level, and lipid medication use. | 11/11 Included |
| Wannamethee et al. (2013) [39] | England (British Regional Heart Study) | 1693 | 100% | 60–79 y | 11 y | 166 | HR (95% CI) (Q4 vs. Q1) 1.26 (0.87–1.83) | Age, cigarette smoking, alcohol intake, physical activity, social class, BMI, use of antihypertensive drugs, diabetes function, systolic blood pressure, eGRF rate, C-reactive protein, and von Willebrand factor. | 10/11 (JBI: 10 Included |
| Larsson et al. (2010) [36] | Sweden (Rotterdam Study) | 2176 | 100% | 50 y | 29.8 y | 466 | HR (95% CI) (Q4 vs. Q1) 1.31 (1.06–1.63) | Age, albumin, eGRF rate, diabetes, use of antihypertensive medication, systolic and diastolic blood pressures, total cholesterol, triglycerides, BMI, and smoking. | 9/11 (JBI: 1, 10) Included |
| Author (Year) | Country (Sample) | Study Design | Sample Size | Men (%) | Age | Follow-Up | Outcome | Nº of Cases | Results | Adjustment for Confounders | Quality Score (JBI Checklist) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Donat-Vargas et al. (2023) [45] | Sweden (Swedish Mammography Cohort 1987–1990) | Cohort study | 1625 | 0% | 56–85 y | 9.4 y | CHD | 75 | HR (95% CI) (T1 vs. T3) 1.15 (0.66–2.03) | Age, BMI, education, family history of MI < 60 years, history of diabetes, history of HTA, smoking, walking/cycling >20 min/day, leisure time inactivity >5 h/day, adherence to Mediterranean diet, alcohol consumption, vitamin D supplement use, eGRF rate, urinary sodium (mmol/mmol creatinine), plasma Ca (mmol/L), use of diuretics (ATC-codes C03), and plasma P (mmol/L). | 11/11 Included |
| Donat-Vargas et al. (2023) [45] | Sweden (Swedish Mammography Cohort 1987–1990) | Cohort study | 1625 | 0% | 56–85 y | 9.4 y | STROKE | 101 | HR (95% CI) (T1 vs. T3) 1.63 (0.98–2.71) | Age, BMI, education, family history of MI < 60 years, history of diabetes, history of HTA, smoking, walking/cycling >20 min/day, leisure time inactivity >5 h/day, adherence to Mediterranean diet, alcohol consumption, vitamin D supplement use, eGRF rate, urinary sodium (mmol/mmol creatinine), plasma Ca (mmol/L), use of diuretics (ATC-codes C03), and plasma P (mmol/L). | 11/11 Included |
| Jung et al. (2022) [41] | South Korea (Health Risk Assessment study, and Health Insurance Review and Assessment Service) | Cohort study | 15,259 | 52.3% | 30–85 y | 50 months | CHD | 315 | HR (95% CI) (Q1 vs. Q4) 1.73 (1.18–2.55) | Age, sex, BMI, smoking status, alcohol intake, physical activity, mean arterial blood pressure, C-reactive protein level, chronic kidney disease, serum Ca, serum potassium, and eGRF rate. | 10/11 (JBI: 9) Included |
| Lan et al. (2022) [40] | China (Gaohang community) | Cohort study | 3948 | 44.2% | 60–79 y | 4 y | CHD | 371 | HR (95% CI) (Q1 vs. Q4) Men: 0.78 (0.47–1.30) Women: 0.74 (0.50–1.09) | Systolic blood pressure, total Ca, bicarbonate, fasting glucose, HbA1c, and smoking habits in males; age, systolic blood pressure, waist circumference, BMI, total Ca, bicarbonate, total cholesterol, education, and kidney disease history in females. | 11/11 Included |
| Lan et al. (2022) [40] | China (Gaohang community) | Cohort study | 3948 | 44.1% | 60–79 y | 4 y | HEART FAILURE | 811 | HR (95% CI) (Q1 vs. Q4) Men: 1.12 (0.81–1.53) Women: 0.93 (0.71–1.21) | Systolic blood pressure, total Ca, bicarbonate, fasting glucose, HbA1c and smoking habits in males; age, systolic blood pressure, waist circumference, BMI, total Ca, bicarbonate, total cholesterol, education, and kidney disease history in females. | 11/11 Included |
| Robinson- Cohen et al. (2020) [42] | U.S.A. (MESA 2000–2002) | Cohort study | 6413 | 46.8% | 45–84 y | 14.9 y | HEART FAILURE | 333 | HR (95% CI) (≤4 vs. >4 mg/dL) 1.13 (0.92–1.63) | Age, sex, gross family income in the past 12 months, educational attainment, in analyses including all participants, ethnicity, BMI, systolic blood pressure, use of antihypertensive medication, low-density total cholesterol, diabetes status, smoking status, and eGRF rate. | 10/11 (JBI: 10 Included |
| Lutsey et al. (2014) [44] | U.S.A. (ARIC 1987–1989) | Cohort study | 14,709 | 45.5% | 45–84 y | 21.8 y | HEART FAILURE | 2250 | HR (95% CI) (Q1 vs. Q5) 1.36 (1.18–1.56) | Age, sex, race, center, education, physical activity, smoking status, BMI, prevalent diabetes, systolic blood pressure, HTA medication use, lipid-lowering medication use, prevalent CHD, eGRF rate, LDL cholesterol, HDL cholesterol, triglycerides, and incident CHD as a time-varying covariate. | 10/11 (JBI: 10) Included |
| Wannamethee et al. (2013) [39] | England (British Regional Heart Study 1978–1980) | Cohort study | 1693 | 100% | 60–79 y | 11 y | CHD | 313 | HR (95% CI) (Q1 vs. Q4) 0.88 (0.61–1.13) | Age, cigarette smoking, alcohol intake, physical activity, social class, BMI, use of antihypertensive drugs, diabetes function, systolic blood pressure, eGRF rate, C-reactive protein, and von Willebrand factor. | 10/11 (JBI: 10) Included |
| Wannamethee et al. (2013) [39] | England (British Regional Heart Study 1978–1980) | Cohort study | 1693 | 100% | 60–79 y | 11 y | STROKE | 228 | HR (95% CI) (Q1 vs. Q4) 1.06 (0.78–1.26) | Age, cigarette smoking, alcohol intake, physical activity, social class, BMI, use of antihypertensive drugs, diabetes function, systolic blood pressure, eGRF rate, C-reactive protein, and von Willebrand factor. | 10/11 (JBI: 10) Included |
| Onufrak et al. (2009) [46] | U.S.A. (ARIC 1987–1989) | Cohort study | 13,998 | 46.8% | 45–84 y | 13 y | CHD | 922 | HR (95% CI) (Q2 vs. Q5) Men:1.45 (1.04–2.01) Women: 0.95 (0.63–1.41) | Age, black race, current smoking, diabetes mellitus, HTA, total cholesterol, HDL cholesterol, eGRF rate, current use of estrogen replacement therapy, and menopausal status. | 10/11 (JBI: 10) Included |
| Foley et al. (2008) [43] | U.S.A. (ARIC 1987–1989) | Cohort study | 13,616 | 44.8% | 30–75 y | 12.6 y | CHD | 1666 | HR (95% CI) (Q1 vs. Q5) 1.03 (0.88–1.21) | Age, sex, current smoking cigarette smoking years, BMI, HDL cholesterol, LDL cholesterol, triglycerides, serum albumin, eGRF rate, caloric intake, and phosphorus intake. | 10/11 (JBI: 10) Included |
| Author (Year) | Country (Sample) | Sample Size | Men (%) | Age | Diagnostic and Measurement | Nº of Cases | Results | Adjustment for Confounders | Quality Score (JBI Checklist) |
|---|---|---|---|---|---|---|---|---|---|
| Campos-Obando et al. (2022) [26] | The Netherlands (Rotterdam Study Cohort I, II, III and IV (RS I, II, III and IV)) | 1889 | 44% | 18 y | Coronary computed tomography. Agatston score CACs > 100–300 | Men: 600/878 Women: 418/1011 | PR (95% CI) (Q1 vs. Q5) Men: 1.08 (1.04–1.12) Women: 1.07 (1.00–1.15) | Age, BMI, blood pleasure, smoking, prevalent CVD, prevalent diabetes mellitus, prevalent serum levels of 25-hydroxyvitamin D, total Ca, C-reactive protein, total cholesterol to HDL cholesterol ratio, and glucose. | 8/8 Included |
| Park et al. (2022) [25] | South Korea (Ulsan University Hospital 2014–2020) | 1636 | 43.5% | ≥55 y | Coronary computed tomography Any atherosclerosis plaque. | 297 | OR (95% CI) (T1 vs. T3) 1.64 (1.09–2.48) | Age, sex, systolic blood pressure, diastolic blood pressure, BMI, fasting blood glucose, HbA1C, LDL cholesterol, HDL cholesterol, triglycerides, creatine, and Ca. | 8/8 Included |
| Park et al. (2020) [52] | South Korea (Health Screening and Promotion Center in the Asan Medical Center 2007–2011) | 6329 | 72.9% | 18 y | Coronary computed tomography Any atherosclerosis plaque. | 2634 | OR (95% CI) (Q1 vs. Q4) 1.35 (1.13–1.61) | Age, sex, obesity, current smoking, HTA, diabetes mellitus, hyperlipidemia, family history of coronary artery disease, high-sensitivity C-reactive protein 2 mg/dL, and corrected Ca concentration. | 8/8 Included |
| Ling et al. (2017) [14] | China (Cardiology Department of Zhongshan Hospital in Shanghai 2015–2016) | 227 | 0% | 20 y | Coronary computed tomography Gensi score Gensi score > 0 | 111 | OR (95% CI) (≤3.59 vs. >3.59 mg/dL) 1.41 (0.70–2.84) | Age, BMI, smoking, HTA, diabetes, LDL cholesterol, HDL cholesterol, triglycerides, eGRF rate, statin use, and high-sensitivity C-reactive protein. | 8/8 Included |
| Grønhøj et al. (2016) [1] | Denmark (Danrisk Study 2009–2010) | 1046 | 47% | 65 y | Coronary computed tomography. Agatston score CACs divided in 4 categories: 0, 1–99, 100–399, 400 | 1-99 AU: 335 (M 196/W 139) 100-399 AU: 98 (M 66/W 32) 400 AU: 54 (M 41/W13) | OR (95% CI) per 0.31 mg/dL increase in P levels. Men: 1.07 (0.97–1.18) Women: 1.01 (0.90–1.14) | Creatine, age, gender, smoking, HTA, hypercholesterolemia, and family history of CVDs. | 8/8 Included |
| Park et al. (2016) [48] | South Korea (Ulsan University Hospital 2009–2013) | 2509 | 63.2% | 60–79 y | Coronary computed tomography Agatston score CACs > 100 | 307 | OR (95% CI) (Q4 vs. Q1) 2.04 (1.22–3.41) | Age, sex, diabetes, BMI, systolic blood pressure, corrected serum Ca, albumin, HbA1c, LDL cholesterol, and HDL cholesterol. | 8/8 Included |
| Kwak et al. (2014) [53] | South Korea (Kangbuk Samsung Health Study) | 23,652 | 83.5% | 49.8 7.3 y | Coronary computed tomography Agatston score CACs 100 | 437 | OR (95% CI) (Q4 vs. Q1) 3.33 (2.55–4.35) | Age, sex, smoking status, alcohol intake, physical activity, BMI, educational level, family history of CVDs, medication for dyslipidemia, diabetes mellitus, HTA, eGRF rate, albumin, ferritin, total calorie intake, Ca intake, phosphorus intake, and Ca supplements. | 8/8 Included |
| Shin et al. (2012) [50] | South Korea (Severance Hospital 2004–2009) | 7553 | 57% | 30 y | Coronary computed tomography Agatston score CACs > 100 | 8% | OR (95% CI) (Q4 vs. Q1) 1.76 (1.29–2.38) | Age, male gender, BMI, HTA, diabetes, smoking, dyslipidemia, and proteinuria. | 8/8 Included |
| Cancela et al. (2012) [47] | Brasil (Heart Institute of Hospital das Clínicas 2008–2009) | 290 | 57.5% | 18 y | Coronary computed tomography Agatston score CACs > 10 | 169 | OR (95% CI) (T3 vs. T1) 1.92 (1.56–3.19) | Age, gender, diabetes, HTA, FGF23 level, and PTH concentration. | 8/8 Included |
| Cancela et al. (2012) [47] | Brasil (Heart Institute of Hospital das Clínicas 2008–2009) | 286 | N/A | 18 y | Coronary computed tomography. Fresinger score Fresinger score > 4 | 137 | OR (95% CI) (T3 vs. T1) 1.74 (1.06–2.88) | Gender, race, age, HTA, diabetes, logPTH, and logFGF23. | 8/8 Included |
| Park et al. (2011) [49] | South Korea (Asan Medical Center 2007–2009) | 402 | 64% | 18 y | Coronary computed tomography Agatston score CACs > 100 | 75 | OR (95% CI) (Q4 vs. Q1) 3.17 (1.19–8.41) | Age, sex, BMI, diabetes, HTA, systolic and diastolic blood pressures, family history of CVDs, corrected serum Ca, Ca-phosphorus product, serum glucose, total, HDL cholesterol, and triglycerides. | 8/8 Included |
| Foley et al. (2009) [51] | U.S.A. (CARDIA 1985–1986) | 3015 | 44.6% | 18–30 y | Coronary computed tomography Agatston score CACs 100 vs. <100 | 1.6% | OR (95% CI) (Q4 vs. Q1) 2.25 (0.97–5.21) | Age, gender, race, education, BMI cigarette, HTA, diabetes, exercise, glucose, family history of MI, LDL cholesterol, HDL cholesterol, triglycerides, systolic and diastolic blood pressures, phosphorus intake, Ca intake, fat intake, alcohol intake, protein intake, carbohydrate intake, and medications. | 8/8 Included |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torrijo-Belanche, C.; Moreno-Franco, B.; Muñoz-Cabrejas, A.; Calvo-Galiano, N.; Casasnovas, J.A.; Sayón-Orea, C.; Guallar-Castillón, P. High Serum Phosphate Is Associated with Cardiovascular Mortality and Subclinical Coronary Atherosclerosis: Systematic Review and Meta-Analysis. Nutrients 2024, 16, 1599. https://doi.org/10.3390/nu16111599
Torrijo-Belanche C, Moreno-Franco B, Muñoz-Cabrejas A, Calvo-Galiano N, Casasnovas JA, Sayón-Orea C, Guallar-Castillón P. High Serum Phosphate Is Associated with Cardiovascular Mortality and Subclinical Coronary Atherosclerosis: Systematic Review and Meta-Analysis. Nutrients. 2024; 16(11):1599. https://doi.org/10.3390/nu16111599
Chicago/Turabian StyleTorrijo-Belanche, Carolina, Belén Moreno-Franco, Ainara Muñoz-Cabrejas, Naiara Calvo-Galiano, José Antonio Casasnovas, Carmen Sayón-Orea, and Pilar Guallar-Castillón. 2024. "High Serum Phosphate Is Associated with Cardiovascular Mortality and Subclinical Coronary Atherosclerosis: Systematic Review and Meta-Analysis" Nutrients 16, no. 11: 1599. https://doi.org/10.3390/nu16111599
APA StyleTorrijo-Belanche, C., Moreno-Franco, B., Muñoz-Cabrejas, A., Calvo-Galiano, N., Casasnovas, J. A., Sayón-Orea, C., & Guallar-Castillón, P. (2024). High Serum Phosphate Is Associated with Cardiovascular Mortality and Subclinical Coronary Atherosclerosis: Systematic Review and Meta-Analysis. Nutrients, 16(11), 1599. https://doi.org/10.3390/nu16111599







