Abstract
Malnutrition is common in older adults, and its risk is greater in those living with dementia. Relative to cognitively healthy peers, the prevalence of malnutrition is also increased in individuals with early stages of cognitive disorders owing to pathophysiological, cognitive, and psychosocial changes related to cognitive impairment. Malnutrition is associated with adverse health outcomes, including faster cognitive and functional decline. Here, we provide an overview of the prevention, assessment, and management of malnutrition in older adults, with a special focus on the aspects that are important to consider in individuals with early stages of cognitive disorders. Strategies to prevent malnutrition include systematic screening for malnourishment using validated tools to detect those at risk. If the screening reveals an increased risk of malnutrition, a detailed assessment including the individual’s nutritional, medical, and functional status as well as dietary intake should be performed. The management of malnutrition in the early stages of cognitive disorders should be based on the findings of a comprehensive assessment and be personalized according to the individual’s specific characteristics. In the article, we also provide an overview of the evidence on vitamin supplements and specific dietary patterns to prevent cognitive decline or attenuate its progression.
1. Introduction
The European Society of Clinical Nutrition and Metabolism (ESPEN) has defined malnutrition as “a state resulting from a lack of intake or uptake of nutrition that leads to altered body composition (decreased fat-free mass) and body cell mass, leading to diminished physical and mental function and impaired clinical outcome from disease” [1]. Approximately 20% of European adults aged ≥ 65 years are malnourished or at risk of malnutrition, but the prevalence of this condition varies greatly across communities and healthcare settings [2]. Malnutrition at an advanced age is associated with reduced quality of life, increased morbidity, hospitalizations, institutionalization, and mortality, as well as higher health care costs [3]. This highlights the importance of its prevention, early detection, and treatment.
Older adults are vulnerable to malnutrition due to multiple factors. Biological aging causes physiological changes in body functions that diminish the reserve capacities of organ systems and predispose to the development of malnutrition, especially in stressful situations [3]. Aging is also associated with a greater susceptibility to acute and chronic diseases [4]. Any acute or chronic disease has the potential to result in or aggravate malnutrition, as it frequently reduces appetite and food intake, impacts nutrient absorption and metabolism, and alters energy expenditure [3,5]. Therefore, malnutrition is especially prevalent in older adults with acute or chronic diseases, frailty, and functional decline [6].
Cognitive disorders and dementia are examples of chronic diseases associated with an increased risk of malnutrition [7]. Neurocognitive disorders are acquired conditions that involve deficits in neurocognitive functioning, including, for instance, memory, language skills, attention, executive functions, processing speed, and visual spatial skills. Cognitive impairment that is severe enough to interfere with an individual’s performance in everyday life is referred to as dementia. According to the International Classification of Diseases 11 (ICD-11), dementia is a clinical syndrome “characterized by the presence of marked impairment in two or more cognitive domains relative to that expected given the individual’s age and general premorbid level of cognitive functioning, which represents a decline from the individual’s previous level of functioning” [8]. The prevalence of malnutrition increases with the severity of dementia [7]. However, the risk of malnutrition is already greater in individuals with early dementia compared with cognitively healthy older adults [9].
Considerable evidence exists on the management of malnutrition in the advanced stages of dementia, but there is a scarcity of information on the subject in the early phases of cognitive disorders. The causes and most efficient treatment strategies of malnutrition in individuals with early stages of dementia are different from those with more advanced diseases. This narrative review aimed to clarify the current knowledge on the prevention and management of malnutrition in older adults with early stages of cognitive disorders. First, we focus on the analysis of mechanisms underlying malnutrition in older adults in general and in those with early-stage dementia. Then, we discuss the current knowledge on the prevention and treatment of malnutrition in this patient population. Finally, we review the evidence on the effects of vitamin supplements and specific dietary patterns on preventing cognitive decline.
2. Mechanisms of Malnutrition in Old Age
Age-related changes in the regulation of appetite have a central role in the so-called “anorexia of aging”, defined as the loss of appetite and/or decreased food intake in late life [10]. Several mechanisms are responsible for and mutually interconnected in the decline of appetite with aging, such as olfactory dysfunction, decreased hunger, increased satiety, chronic low-level inflammation, and alterations in gastric motility [10]. The sense of smell and taste deteriorates with aging. Olfactory dysfunction affects up to 60% of individuals over 65 years [11]. Physiological age-related changes in olfactory and gustatory function include a decreased number of taste buds and atrophy of the remaining ones [10], impaired ability to regenerate olfactory neurons [12], reduced saliva secretion, and a decreased release of odor molecules from foods due to impaired chewing [12]. Diseases, medications, smoking, and environmental exposures may worsen these changes [10,11,13]. This may contribute to a reduced nutrient intake and have an influence on food choices, usually resulting in a less varied diet [10].
Aging also influences the levels of several hunger and satiety hormones, such as ghrelin, leptin, insulin, cholecystokinin (CCK), and peptide YY, which contribute to the anorexia of aging [10]. Ghrelin is a hunger-stimulating hormone released during fasting by the gastrointestinal mucosa in the stomach [14]. Its sensitivity decreases because of a concomitant increase in the satiety hormones insulin and leptin [15]. Insulin acts directly as a satiety hormone and indirectly as an enhancer of the anorexigenic stimulus of leptin in the hypothalamus [16,17]. The levels of leptin, produced by the adipose tissue, and insulin, produced by the pancreas, rise in the blood as a long-term signal of adiposity [16]. Blood levels of leptin and insulin correlate with adiposity levels in the adipose tissue’s central system for energy storage and potentiate the central satiety sensation. CCK is a satiety hormone released in response to the delivery of nutrients in the proximal small intestine [18]. Higher circulating levels of leptin and CCK and an increased fasting and post-prandial plasma insulin concentration have been found in older adults compared with younger individuals [17,19,20,21,22,23]. High CCK levels are correlated with greater satiety after meals, thereby contributing to the anorexia of aging [21]. Studies have also shown an increase in circulating concentrations of peptide YY in the late postprandial phase in older adults [24]. Peptide YY, a hormone produced after meals by specialized enteroendocrine cells (L-cells) mainly located in the distal gastrointestinal tract, induces satiety over the short term [25]. Long- and short-term signals of satiety interact so that insulin inhibits ghrelin and leptin reinforces the CCK signal, and vice versa [26]. This process is accompanied by an increase in fasting and postprandial plasma insulin concentrations that, in turn, hinder the orexigenic stimulus of ghrelin in the hypothalamus [17].
Chronic low-grade inflammation, a hallmark of the aging process [27], may modify the response of the hypothalamus to peripheral stimuli [10]. Circulating levels of interleukin (IL)-1, IL-6, and tumor necrosis factor alpha (TNF-α) are generally higher in older adults compared with younger individuals, independent of specific diseases or multimorbidity [28]. TNF-α and IL-1 stimulate leptin mRNA expression, thereby increasing its circulating levels [29]. Inflammation is also associated with delayed gastric emptying and clampdown of small intestinal motility [25] as well as skeletal muscle loss [30,31,32]. Indeed, inflammatory biomolecules interact with prostaglandin and corticotrophin-releasing factor to inhibit gastric emptying [31]. Individuals with chronic obstructive pulmonary disease suffer from both the consequences of energy wasting (due to respiratory inefficiency) and anorexia, caused by inflammatory mediators. Similarly, cancer and heart failure cause cachexia by increasing energy requirements and anorexia. In these conditions, high concentrations of cytokines such as IL-6 and TNF-α have a strong anorexigenic effect [33].
In addition to these mechanisms, abnormalities in gastrointestinal function are involved in the anorexia of aging [10]. Altered gastric motility may cause early satiation, which is correlated with reduced fundus compliance. Due to age-related changes, the fundus of the stomach in older adults produces less nitric oxide (NO) [16]. NO is a ubiquitous gaseous molecule that is thought to be the main inhibitory neurotransmitter responsible for gastrointestinal relaxation in response to gastric filling [34]. A lack of NO diminishes gastric compliance and leads to rapid antral filling, giving a sensation of satiety [25]. In addition, delayed gastric emptying may decrease appetite and food intake by enhancing and prolonging antral distension as well as modifying small intestine satiety signals [10]. Moreover, chronic gastritis and some drugs (e.g., proton-pomp inhibitors) may cause hypochlorhydria, which further delays gastric emptying [35].
3. Risk Factors for Malnutrition in Early Cognitive Disorders
Cognitive, psychological, social, pathophysiological, and medication-related factors increase the risk of malnutrition in individuals with early cognitive disorders.
3.1. Cognitive, Psychological, and Social Factors
Mild dementia is characterized by a moderate memory loss interfering with everyday life, moderate difficulties in time and space orientation and problem handling, difficulties in community affairs, a mild impairment of daily functioning, and a need for prompting [36]. Executive function impairment, which influences an individual’s ability to plan, organize, and complete tasks, and attention deficits are common early symptoms of cognitive disorders [37,38]. Thus, adults with early dementia often face challenges and difficulties in the acquisition of food products and food preparation, as well as maintaining their previous food intake [39,40,41,42,43]. Indeed, difficulties in daily functioning are associated with poorer nutritional status in community-dwelling individuals with newly diagnosed Alzheimer’s disease (AD) [44]. In addition, difficulties in maintaining attention while eating are associated with poor appetite in those with mild cognitive impairment (MCI) [45].
Changes in appetite, depression, and apathy, which are frequent behavioral and psychiatric symptoms of dementia (BPSD) in the early disease stages, may increase the risk of malnutrition [46,47,48]. The prevalence of depression in individuals with mild dementia is about 38%, and the prevalence of apathy is greater than 50% [49]. Depression is associated with an increased risk of malnutrition, as a decrease in appetite is one of the core clinical features of depression [50]. In addition, apathy has been associated with malnutrition in older women with MCI and early-stage AD [51].
Social support has a key role in the everyday lives of individuals with mild dementia. However, social support is frequently inadequate for these people. This may be caused by a lack of social relationships but also by the fact that those suffering from early dementia often refuse to accept help from other people, even if there are clear deficiencies in their self-care abilities [43]. This is because anosognosia, an inability to recognize cognitive, behavioral, and functional impairment caused by a dementing illness, is a common symptom of mild dementia [52]. A lack of support may contribute to the development of malnutrition.
3.2. Pathophysiological Factors
Pathophysiological changes associated with the early stages of dementia, such as olfactory and gustatory dysfunction, increase the risk of malnutrition. As mentioned earlier, olfactory and gustatory functions decline with age, but their deterioration is accelerated in the preclinical stages of dementia [53,54,55,56]. The basis of olfactory dysfunction in the setting of cognitive disorders is not well established, but it is suggested that cortical atrophy and gray matter abnormalities in the brain related to cognitive aging and cognitive disorders may play a role [57]. Unexpectedly, many studies did not find an association between olfactory dysfunction and malnutrition in older adults [12,58,59,60]. Notwithstanding, Kim et al. [61] showed that older adults with a high smell threshold had a lower intake of calories, protein, fat, carbohydrates, and minerals than those with a lower threshold.
Involuntary weight loss is common in individuals with mild dementia and even in preclinical disease stages [62,63,64,65]. The mechanisms behind weight loss are only partially understood. While weight loss indicates a negative energy balance, it is unclear if this is due to a decreased food intake and/or an increased energy expenditure. A systematic review included seven articles that compared energy and protein intake between individuals with AD and cognitively healthy controls [66]. The results indicated no differences in food intake, but the heterogeneity of findings was high, and study methodologies were considered to be of poor or moderate quality. Most studies considered patients with moderate or severe dementia, and only one study included individuals with mild dementia [67]. The latter found that the intake of nutrients and energy was significantly lower in individuals with mild dementia than in cognitively healthy older adults [67]. In contrast, Doorduijn et al. [68] did not find differences in food intake, but they showed that resting energy expenditure was increased in individuals with MCI and early AD compared with controls. A recent systematic review by Porter et al. [69] included six studies that compared total energy expenditure in people with and without dementia. The results showed that there were no significant differences in total energy expenditure between these groups. However, the included studies included dementia patients as a single group and did not account for disease severity. Hence, additional studies are needed to clarify the reasons for involuntary weight loss in individuals with preclinical and early dementia stages.
3.3. Medication-Related Factors
One of the pathophysiological mechanisms of AD is a decrease in neurotransmitter acetylcholine (ACh) levels in the brain. The cerebral availability of ACh can be increased pharmacologically by blocking the activity of the acetylcholinesterase enzyme (AChE), which is responsible for the degradation of ACh. AChE inhibitors, namely donepezil, galantamine, and rivastigmine, are the front-line pharmacotherapies in the treatment of cognitive and behavioral symptoms in mild and moderate AD [70]. Because AChE inhibitors increase cholinergic activity not only in the brain but also in the gastrointestinal system, common side effects, particularly at the beginning of treatment, include nausea, vomiting, and diarrhea. Soysal et al. [71] conducted a systematic review and meta-analysis exploring the influence of therapy with AChE inhibitors on weight change. The meta-analysis of nine randomized controlled trials (RCTs) showed a twofold increased risk of weight loss in participants on AChE inhibitors compared with those taking placebo. In addition, a significant cumulative incidence of weight loss was observed in longitudinal and open-label studies in patients taking AChE inhibitors. Thus, the use of AchE inhibitors may increase the risk of malnutrition.
4. Consequences of Malnutrition
4.1. Adverse Health Outcomes of Energy-Protein Malnutrition
Energy-protein malnutrition causes alterations in body composition and function that, in turn, increase the risk of complications and predispose to serious adverse health outcomes (Figure 1) [3]. Sarcopenia is a common condition in older adults that is associated with malnutrition [72] and cognitive impairment [73]. Together, these geriatric syndromes cause a vicious circle that worsens the severity and outcomes of each of them [39].
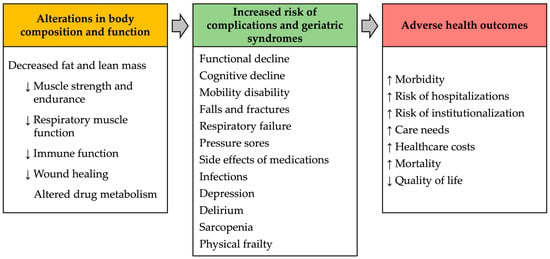
Figure 1.
Consequences of malnutrition in older adults.
In cross-sectional studies, malnutrition has been associated with cognitive impairment and dementia [74,75], as well as with BPSD in individuals with mild dementia [51]. Longitudinal studies in patients with dementia examined the associations between malnutrition and rates of cognitive and/or functional decline. Borda et al. [76] followed 202 patients diagnosed with mild dementia for five years. Their results showed that malnutrition at baseline and over the follow-up was a significant predictor of functional decline but not of cognitive decline. In contrast, in the Cache County Dementia Progression Study [77], which followed 292 patients with dementia for six years, malnutrition predicted faster rates of cognitive decline. Kishino et al. [78] showed that a poor nutritional status was associated with worsening of BPSD, especially verbal aggressiveness and emotional disinhibition, over a 2.5-year follow-up in women with MCI and AD.
4.2. Micronutrient Deficiencies
4.2.1. B-Complex Vitamins
B-complex vitamins are a group of eight water-soluble vitamins that have essential and closely interrelated roles in cellular metabolism [79,80]. They act as co-enzymes in various enzymatic reactions and have critical roles in the biosynthesis of RNA and DNA. In particular, B vitamins have essential roles in cellular energy production within mitochondria, where they act as co-enzymes in the citric acid cycle and the electron transport chain, as well as in the metabolism of glucose, fatty acids, and amino acids. B vitamins are also essential for the synthesis of several neurochemicals, signaling molecules, and other substrates in the folate and methionine cycles [79]. Hence, normal brain function is dependent on the continuous supply of B-complex vitamins [79]. Most of them are not stored in the body and, therefore, require regular intake to avoid deficiency. The exception is vitamin B12, which is stored in the liver, kidney, and other body tissues [80,81]. For this reason, vitamin B12 deficiency is usually manifested only after a few years of insufficient intake. However, if the reason for its deficiency is malabsorption, the symptoms and consequences of vitamin B12 deficiency become apparent more rapidly [81].
There are several reasons that contribute to susceptibility to B vitamin deficiencies in old age. First, the intake of foods that are sources of B vitamins tends to decrease with aging [82]. This may lead to an inadequate vitamin intake and, therefore, contribute to the development of vitamin deficiency. Second, the prevalence of chronic diseases that alter the absorption of B vitamins is increased in older adults. An example of this is atrophic gastritis, which causes malabsorption of vitamin B12, leading to its deficiency if not adequately supplemented. The main causes of atrophic gastritis include chronic Helicobacter pylori infection, autoimmune gastritis, and the long-term use of medications that lower the acidity of the stomach, like proton pump inhibitors and H2-receptor antagonists [83]. Third, many medications that are commonly used by older adults have an influence on the absorption or metabolism of B vitamins [80,84]. Examples of these are proton-pump inhibitors, H2-receptor antagonists, and metformin that cause malabsorption of vitamin B12 [85].
Vitamins B1 and B12 are the most studied B-complex vitamins in the context of cognitive disorders, and their deficiencies are clearly associated with cognitive impairment and dementia [86,87]. However, any B vitamin deficiency has been shown to disrupt normal brain function and cause cognitive and/or neuropsychiatric symptoms (Table 1).

Table 1.
B complex vitamins, risk factors for their deficiencies, and cognitive and neuropsychiatric symptoms of their deficiencies in adults.
4.2.2. Vitamin D
The main reasons for vitamin D deficiency, commonly defined as serum/plasma 25-hydroxyvitamin D levels below 25–30 nmol/L [93], include a lack of exposure to sufficient UVB light and poor nutritional intake [94]. It should be noted that few foods naturally contain vitamin D. These include oily fish (salmon, mackerel, and herring), mushrooms exposed to sunlight or sundried, cod liver oil, and meat such as pork and beef [95,96,97]. As for sunlight, exposure to the sun above and below approximately 33° latitude in the winter does not result in any significant production of vitamin D [98,99]. There are also other factors involved in vitamin D deficiency. Single nucleotide polymorphisms in genes related to vitamin D metabolism are known to affect the level of 25-hydroxyvitamin D and the response to supplementation [100]. Inflammation has also been shown to reduce 25-hydroxyvitamin D [93], and some studies found increased vitamin clearance in association with conditions such as hyperparathyroidism [101] and low calcium intake [102].
Vitamin D deficiency has been associated with cognitive decline in cross-sectional and longitudinal studies. Systematic reviews and meta-analyses by Chai et al. [103], Goodwill and Szoeke [104], van der Schaft et al. [105], Sommer et al. [106], and Shen and Ji [107] confirmed significant associations between vitamin D deficiency and dementia and showed that the risk of dementia increased with the severity of vitamin D deficiency.
5. Prevention and Management of Malnutrition
In the following paragraphs, we describe strategies for malnutrition prevention and treatment in older adults, with a special focus on the aspects that are important to consider in individuals with early stages of cognitive disorders.
5.1. Screening and Assessment of Malnutrition
Routine screening for malnutrition is imperative for its prevention and the recognition of individuals who are either at risk of malnutrition or already malnourished (Figure 2) [108].
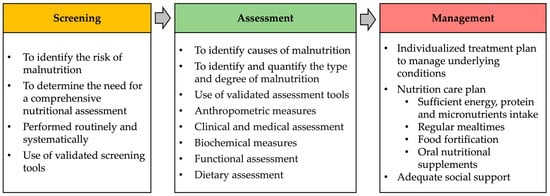
Figure 2.
Screening, assessment, and management of malnutrition in older adults.
Even though malnutrition is widespread in older adults with dementia and is associated with poor outcomes, it easily remains undetected unless systematically screened. Therefore, ESPEN recommends that every person with dementia be routinely screened for malnutrition using validated tools [39]. The consensus statements of most clinical nutrition societies (including ESPEN) recommend that the diagnosis of malnutrition in older adults is based on a two-step process (screening and assessment) and Global Leadership Initiative on Malnutrition (GLIM) criteria [109]. GLIM criteria comprise three phenotypic criteria (low body mass index (BMI), involuntary weight loss > 5% in the last six months, and reduced muscle mass) and two etiological criteria (reduced food intake or assimilation of nutrients and inflammation or disease burden). In order to diagnose malnutrition, at least one phenotypic criterion and one etiological criterion should be present. The severity of malnutrition is based on phenotypic criteria.
The Mini Nutrition Assessment–Short Form (MNA–SF) is a frequently used screening tool in older adults and is suitable for those with dementia [110]. In the latter case, to reduce misjudgment, it is recommended that the patient’s answers be confirmed by relatives or caregivers. The MNA–SF includes items about food intake, weight loss, mobility, acute conditions, neuropsychological problems, and BMI. The resulting score differentiates individuals as having normal nutritional status, being at risk of malnutrition, or being malnourished. Given the high prevalence of weight loss in patients with early stages of dementia, regular monitoring of weight is another useful method for the early detection of malnutrition risk.
If the screening reveals an increased risk of malnutrition or malnourishment, it is necessary to perform a comprehensive assessment of the patient’s nutritional, medical, and functional status to identify underlying causes of malnutrition and quantify its type and degree [108] (Figure 2). It is also necessary to perform a dietary assessment to obtain information on the patient’s usual food and beverage intake. Validated nutrition assessment tools are recommended to be used to support assessment. The most commonly used is the MNA (complete form), which comprehensively evaluates the nutritional status and causes of malnutrition [111].
There are usually many simultaneous underlying causes of malnutrition. Common treatable causes include mastication and swallowing problems, side effects of medications, depression, loneliness, pain, anxiety, restricted mobility, constipation, difficulties in food preparation or acquisition, and social problems (lack of support, family conflict) [112,113]. In the medical evaluation, it is also imperative to rule out micronutrient deficiencies that may be a cause of or at least take part in the process of cognitive impairment.
5.2. Management of Malnutrition
5.2.1. Individualized Management of Malnutrition
The management of malnutrition is based on the findings of the assessment. It includes the treatment or management of identified underlying causes of malnutrition and the implementation of nutritional strategies to improve energy, protein, and micronutrient intake (Figure 2).
5.2.2. Strategies to Ensure Adequate Food Intake
Nutritional strategies to improve food intake include guidance on regular mealtimes and avoidance of long fasting periods during the day and night, food fortification, oral nutritional supplements (ONS), and appealing and appetizing foods according to personal preferences. Dietary restrictions are not recommended, as they may increase the risk of malnutrition. Food fortification is useful to support adequate dietary intake. Several systematic literature reviews evaluated the effects of dietary enrichment with conventional foods and showed an increase in protein and energy intake using food fortification [114,115,116].
ONS are products that contain a combination of macro- and micronutrients designed to improve dietary intake when diet alone is insufficient to reach nutritional goals [117]. ONS are used in addition to a balanced diet. Studies have shown positive effects of ONS on body weight and BMI in individuals with dementia [118,119].
Nutrition-related problems such as eating behavior disorders associated with dementia pose a heavy burden on caregivers, who may become stressed, depressed, and socially isolated. Caregiver stress, in turn, is associated with malnutrition of older adults being cared for [120], and it may also aggravate nutritional problems in individuals with dementia. Nutritional education programs designed for caregivers, including information on weight loss, nutritional needs, and interaction during mealtimes, may reduce the stress of the caregiver. Furthermore, as male caregivers often have poor knowledge of cooking and other household activity skills, they could benefit from specific training considering these skills [121]. Scientific evidence has shown a positive effect of caregiver education on the nutritional status of older adults with dementia [122,123]. In addition, modifying environmental factors (like sounds and lightning) to ensure a pleasant environment while eating may improve the nutritional status of individuals with dementia [124,125]. It is also demonstrated that eating in company stimulates dietary intake [124,126,127]. Mealtime interventions with a focus on the social elements of eating and drinking have been shown to increase energy intake in older adults [128].
Appetite stimulants (orexigenic drugs) are an available method to support food intake in patients with a loss of appetite. However, there is a lack of studies on their use in individuals with dementia. Because these drugs have various side effects, they are not generally recommended in this setting [129,130].
5.2.3. Prevention of Dehydration
The central nervous system consists of 80% water, stored in astrocytes [131]. Aging causes alterations in water homeostasis through several mechanisms (e.g., renal function alterations, regulation of thirst, vasopressin secretion changes, alterations of body composition) that increase the risk of dehydration and hyperosmolality [132]. Chronic hypovolemia, due to long-lasting hypohydration, may reduce brain volume and disrupt normal neural pathways, thus predisposing older adults to cognitive decline [131,133]. Lauriola et al. [134] showed that hypovolemia was more prevalent in individuals with cognitive impairment and dementia compared with cognitively healthy older adults. Dehydration was also associated with lower MNA scores. The PREDIMED-Plus study included 1957 individuals with metabolic syndrome [135]. More than half of the participants were physiologically dehydrated. Lower hydration status was associated with a greater decline in global cognitive function over a 2-year follow-up. The Berlin Aging Study showed that chronic dehydration was associated with a steeper decline in cognitive functioning over time in older adults [136]. These results highlight the importance of preventing, recognizing, and treating fluid balance disorders at an advanced age.
5.2.4. Replacement Therapy for Vitamin Deficiency and Cognition
Considering the essential roles of vitamins B and D in the physiological functions of the body, replacement therapy for their deficiencies is beneficial for the general health of patients. There is also evidence that, if replacement therapy for vitamin B deficiency is started before irreversible damage to the central nervous system has occurred, cognitive functions may be restored [137,138,139,140,141] (Table 2). However, if dementia has already developed, cognitive impairment is most probably irreversible. The findings on the effects of replacement therapy for vitamin D deficiency on cognition are mixed; some studies found a significant beneficial effect on cognitive functions [142,143,144,145], while others did not confirm these findings [146,147,148] (Table 2).

Table 2.
Original studies on the effects of vitamin B or D replacement therapy on cognitive functions.
6. Evidence on Nutritional Strategies Aimed at Preventing Cognitive Decline
6.1. Vitamin Supplements
Systematic reviews and meta-analyses have summarized the evidence on RCTs that have examined the effects of vitamin B or D supplements on improving cognitive functions or preventing cognitive decline in older individuals without vitamin deficiencies (Table 3) [149,150,151,152,153,154,155,156,157,158,159,160,161]. These studies show that there are no beneficial effects of vitamin B or D supplements on cognitive functions, and they are therefore not recommended to improve cognition or to prevent cognitive decline in either cognitively healthy older adults or in those with dementia.

Table 3.
Systematic reviews and/or meta-analyses of the effects of B or D vitamin supplements on improving cognition function or preventing cognitive decline.
6.2. Healthy Dietary Patterns for Neuroprotection
There is an increasing interest in healthy dietary patterns and specific diets that may prevent cognitive decline [162,163]. A meta-analysis of observational studies by Liu et al. [164] and a systematic review by van de Rest et al. [165] found that adherence to high-quality diets or healthy dietary patterns was associated with a lower risk of cognitive impairment compared with participants on low diet quality or an unhealthy dietary pattern.
The Mediterranean diet (MeDi) is an extensively studied dietary pattern with cardiovascular health benefits yielded by a high consumption of fruits, vegetables, legumes, whole grains, and olive oil, moderate consumption of fish, and a low consumption of red meat and foods containing saturated fats [166]. The PREDIMED trial enrolled 447 participants without cognitive impairment (233 women; mean age, 66.9 years) and compared the effects of three different dietary patterns on cognitive functions: MeDi supplemented with extra virgin olive oil (1 l/week), MeDi supplemented with mixed nuts (30 g/die), and a control diet [167]. The adoption of MeDi enriched with olive oil or nuts for 4 years was associated with better cognitive functions compared with the control group. A meta-analysis by Coelho-Junior et al. [168] found that high MeDi adherence was associated with better global cognition and a reduced risk of decline in global cognitive function, but no benefit was observed for the prevention of cognitive impairment or dementia. Similar findings were reported in a systematic review by Limongi et al. [169]. A systematic review by Petersson and Philippou [170] concluded that adherence to a MeDi was associated with better cognitive performance in cross-sectional studies, but the causal relationship remained unclear. A systematic review by Lourida et al. [171] showed that higher MeDi adherence was associated with better cognitive function, lower rates of cognitive decline, and a reduced risk of AD. Singh et al. [172] included only prospective studies in their meta-analysis and concluded that a higher adherence to a MeDi was associated with a reduced risk of developing cognitive impairment and of progressing from MCI to AD. However, a systematic review by Radd-Vagenas et al. [173], including only RCTs, did not find beneficial effects of MeDi on cognition. More longitudinal studies with long-term follow-up are needed to evaluate the effectiveness of MeDi in the prevention of dementia.
The Dietary Approaches to Stop Hypertension (DASH) diet [173] and the MeDi–DASH Diet Intervention for Neurological Delay (MIND) [174] are dietary patterns based on MeDi that have been further developed to achieve health benefits. The DASH diet is designed to prevent and treat hypertension and is based on a high consumption of plant-based foods and a low intake of total fat, saturated fatty acids, cholesterol, and sodium [173]. The MIND dietary pattern has been developed to prevent dementia, and it is a combination of the MeDi and DASH diets, enriched by foods with neuroprotective properties like berries and green leafy vegetables [174]. van den Brink et al. [174] compared the effects of MeDi, DASH, and MIND diets on cognitive functions in middle-aged and older adults. The authors concluded that all these dietary patterns were associated with a lower risk of cognitive decline compared with control groups, with the strongest associations reported for the MIND diet. Similarly, a systematic review by Solfrizzi et al. [175] found that higher MeDi adherence was associated with better cognitive functions and that the DASH and MIND diets were associated with slower rates of cognitive decline and a reduction in AD rates compared with control diets. More studies are needed to certify the benefits of the MIND and DASH diets for the prevention of dementia.
7. Conclusions
Individuals with early stages of cognitive disorders are susceptible to energy-protein malnutrition and micronutrient deficiencies owing to factors related to biological aging and special features of cognitive disorders that influence food intake and energy expenditure. To avoid the adverse health outcomes of malnutrition, prevention strategies should be systematically implemented in the care of individuals with early dementia. These include routine screening for malnutrition, regular monitoring of body weight, and the provision of adequate support in everyday life. If malnutrition or a condition of risk is detected, a comprehensive assessment of the individual’s situation should be undertaken, and a personalized plan for the management of malnutrition and the treatment of underlying causes should be developed. Micronutrient deficiencies should be promptly identified and treated. There is evidence that early treatment of B and D vitamin deficiency may restore cognitive decline due to vitamin deficiency. However, if dementia has already developed, the changes in cognitive function are most likely irreversible. In contrast, strong evidence exists against the use of vitamin B and D supplements for the prevention of cognitive decline in individuals without deficiency. Instead, adherence to healthy dietary patterns may have predictive effects on cognitive decline. For example, MeDi is associated with better cognitive performance in cross-sectional studies. Some longitudinal studies have indicated that healthy diets may prevent cognitive decline and diminish dementia rates, but more longitudinal studies with longer follow-up and clinically meaningful outcome measures are needed to confirm these findings.
Author Contributions
Conceptualization, E.M.; writing—original draft preparation, E.D., H.K. and I.L.; writing—review and editing, H.K. and E.M.; visualization, H.K.; supervision, E.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the Finnish Medical Foundation (grant no. 6554), the Juho Vainio Foundation (N/A), the Italian Ministry of Health (Ricerca Corrente 2024), intramural research grants from Università Cattolica del Sacro Cuore (D1.2020, D1.2022, and D1.2023), and the nonprofit research foundation “Centro Studi Achille e Linda Lorenzon” (N/A). The authors also acknowledge co-funding from Next Generation EU in the context of the National Recovery and Resilience Plan, Investment PE8—Project Age-It: “Ageing Well in an Ageing Society”. This resource was co-financed by the Next Generation EU (DM 1557, 11.10.2022). The views and opinions expressed are only those of the authors and do not necessarily reflect those of the European Union or the European Commission. Neither the European Union nor the European Commission can be held responsible for them.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study, in the collection, analysis, or interpretation of data, in the writing of the manuscript, or in the decision to publish the results.
References
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef] [PubMed]
- Leij-Halfwerk, S.; Verwijs, M.H.; van Houdt, S.; Borkent, J.W.; Guaitoli, P.R.; Pelgrim, T.; Heymans, M.W.; Power, L.; Visser, M.; Corish, C.A.; et al. Prevalence of protein-energy malnutrition risk in european older adults in community, residential and hospital settings, according to 22 malnutrition screening tools validated for use in adults ≥65 years: A systematic review and meta-analysis. Maturitas 2019, 126, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Dent, E.; Wright, O.R.L.; Woo, J.; Hoogendijk, E.O. Malnutrition in older adults. Lancet 2023, 401, 951–966. [Google Scholar] [CrossRef] [PubMed]
- Marengoni, A.; Angleman, S.; Melis, R.; Mangialasche, F.; Karp, A.; Garmen, A.; Meinow, B.; Fratiglioni, L. Aging with multimorbidity: A systematic review of the literature. Ageing Res. Rev. 2011, 10, 430–439. [Google Scholar] [CrossRef] [PubMed]
- Campbell, I.T. Limitations of nutrient intake. The effect of stressors: Trauma, sepsis and multiple organ failure. Eur. J. Clin. Nutr. 1999, 53 (Suppl. S1), S143–S147. [Google Scholar] [CrossRef]
- Ligthart-Melis, G.C.; Luiking, Y.C.; Kakourou, A.; Cederholm, T.; Maier, A.B.; de van der Schueren, M.A.E. Frailty, sarcopenia, and malnutrition frequently (co-)occur in hospitalized older adults: A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2020, 21, 1216–1228. [Google Scholar] [CrossRef] [PubMed]
- Arifin, H.; Chen, R.; Banda, K.J.; Kustanti, C.Y.; Chang, C.Y.; Lin, H.C.; Liu, D.; Lee, T.Y.; Chou, K.R. Meta-analysis and moderator analysis of the prevalence of malnutrition and malnutrition risk among older adults with dementia. Int. J. Nurs. Stud. 2024, 150, 104648. [Google Scholar] [CrossRef]
- World Health Organization, Geneva. International Classification of Diseases Eleventh Revision (ICD-11). Available online: https://icd.who.int/en (accessed on 10 May 2024).
- Cavalli, A.; Lelli, D.; Pedone, C.; Boccardi, V.; Mecocci, P.; Incalzi, R.A. Attention, praxis, and reasoning are associated with risk of undernutrition in older people with cognitive impairment. J. Alzheimers Dis. 2022, 89, 1017–1024. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Calvani, R.; Tosato, M.; Martone, A.M.; Ortolani, E.; Savera, G.; Sisto, A.; Marzetti, E. Anorexia of aging: Risk factors, consequences, and potential treatments. Nutrients 2016, 8, 69. [Google Scholar] [CrossRef]
- Landis, B.N.; Konnerth, C.G.; Hummel, T. A study on the frequency of olfactory dysfunction. Laryngoscope 2004, 114, 1764–1769. [Google Scholar] [CrossRef]
- Smoliner, C.; Fischedick, A.; Sieber, C.C.; Wirth, R. Olfactory function and malnutrition in geriatric patients. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 1582–1588. [Google Scholar] [CrossRef]
- Doty, R.L. Influence of Age and Age-related diseases on olfactory function. Ann. N. Y. Acad. Sci. 1989, 561, 76–86. [Google Scholar] [CrossRef] [PubMed]
- van der Lely, A.J.; Tschop, M.; Heiman, M.L.; Ghigo, E. Biological, physiological, pathophysiological, and pharmacological aspects of ghrelin. Endocr. Rev. 2004, 25, 426–457. [Google Scholar] [CrossRef]
- Gutzwiller, J.-P.; Göke, B.; Drewe, J.; Hildebrand, P.; Ketterer, S.; Handschin, D.; Winterhalder, R.; Conen, D.; Beglinger, C. Glucagon-like peptide-1: A potent regulator of food intake in humans. Gut 1999, 44, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Di Francesco, V.; Fantin, F.; Omizzolo, F.; Residori, L.; Bissoli, L.; Bosello, O.; Zamboni, M. The anorexia of aging. Dig. Dis. 2007, 25, 129–137. [Google Scholar] [CrossRef]
- Di Francesco, V.; Zamboni, M.; Zoico, E.; Mazzali, G.; Dioli, A.; Omizzolo, F.; Bissoli, L.; Fantin, F.; Rizzotti, P.; Solerte, S.B.; et al. Unbalanced serum leptin and ghrelin dynamics prolong postprandial satiety and inhibit hunger in healthy elderly: Another reason for the “anorexia of aging”. Am. J. Clin. Nutr. 2006, 83, 1149–1152. [Google Scholar] [CrossRef] [PubMed]
- Strader, A.D.; Woods, S.C. Gastrointestinal hormones and food intake. Gastroenterology 2005, 128, 175–191. [Google Scholar] [CrossRef]
- Zamboni, M.; Zoico, E.; Fantin, F.; Panourgia, M.P.; Di Francesco, V.; Tosoni, P.; Solerte, B.; Vettor, R.; Bosello, O. Relation between leptin and the metabolic syndrome in elderly women. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, 396–400. [Google Scholar] [CrossRef]
- Vincenzo, D.F.; Mauro, Z.; Andrea, D.; Elena, Z.; Gloria, M.; Francesca, O.; Luisa, B.; Sebastiano, B.S.; Luigi, B.; Ottavio, B. Delayed postprandial gastric emptying and impaired gallbladder contraction together with elevated cholecystokinin and peptide YY serum levels sustain satiety and inhibit hunger in healthy elderly persons. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 1581–1585. [Google Scholar] [CrossRef]
- MacIntosh, C.G.; Andrews, J.M.; Jones, K.L.; Wishart, J.M.; Morris, H.A.; Jansen, J.B.; Morley, J.E.; Horowitz, M.; Chapman, I.M. Effects of age on concentrations of plasma cholecystokinin, glucagon-like peptide 1, and peptide YY and their relation to appetite and pyloric motility. Am. J. Clin. Nutr. 1999, 69, 999–1006. [Google Scholar] [CrossRef]
- MacIntosh, C.G.; Morley, J.E.; Wishart, J.; Morris, H.; Jansen, J.B.M.J.; Horowitz, M.; Chapman, I.M. Effect of exogenous cholecystokinin (CCK)-8 on food intake and plasma CCK, leptin, and insulin concentrations in older and young adults: Evidence for increased CCK activity as a cause of the anorexia of aging. J. Clin. Endocrinol. Metab. 2001, 86, 5830–5837. [Google Scholar] [CrossRef]
- Sturm, K.; MacIntosh, C.G.; Parker, B.A.; Wishart, J.; Horowitz, M.; Chapman, I.M. Appetite, food intake, and plasma concentrations of cholecystokinin, ghrelin, and other gastrointestinal hormones in undernourished older women and well-nourished young and older women. J. Clin. Endocrinol. Metab. 2003, 88, 3747–3755. [Google Scholar] [CrossRef]
- Cummings, D.E.; Overduin, J. Gastrointestinal regulation of food intake. J. Clin. Investig. 2007, 117, 13–23. [Google Scholar] [CrossRef]
- Chapman, I.M.; MacIntosh, C.G.; Morley, J.E.; Horowitz, M. The anorexia of ageing. Biogerontology 2002, 3, 67–71. [Google Scholar] [CrossRef]
- Morton, G.J.; Cummings, D.E.; Baskin, D.G.; Barsh, G.S.; Schwartz, M.W. Central nervous system control of food intake and body weight. Nature 2006, 443, 289–295. [Google Scholar] [CrossRef]
- Baechle, J.J.; Chen, N.; Makhijani, P.; Winer, S.; Furman, D.; Winer, D.A. Chronic inflammation and the hallmarks of aging. Mol. Metab. 2023, 74, 101755. [Google Scholar] [CrossRef]
- Franceschi, C.; Campisi, J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69 (Suppl. S1), S4–S9. [Google Scholar] [CrossRef]
- La Cava, A. Leptin in inflammation and autoimmunity. Cytokine 2017, 98, 51–58. [Google Scholar] [CrossRef]
- Morley, J.E.; Thomas, D.R. Anorexia and aging: Pathophysiology. Nutrition 1999, 15, 499–503. [Google Scholar] [CrossRef]
- Yeh, S.-S.; Blackwood, K.; Schuster, M.W. The cytokine basis of cachexia and its treatment: Are they ready for prime time? J. Am. Med. Dir. Assoc. 2008, 9, 219–236. [Google Scholar] [CrossRef]
- Laviano, A.; Meguid, M.M.; Inui, A.; Muscaritoli, M.; Rossi-Fanelli, F. Therapy insight: Cancer anorexia-cachexia syndrome--when all you can eat is yourself. Nat. Clin. Pract. Oncol. 2005, 2, 158–165. [Google Scholar] [CrossRef]
- Yeh, S.S.; Schuster, M.W. Geriatric cachexia: The role of cytokines. Am. J. Clin. Nutr. 1999, 70, 183–197. [Google Scholar] [CrossRef]
- Idrizaj, E.; Traini, C.; Vannucchi, M.G.; Baccari, M.C. Nitric oxide: From gastric motility to gastric dysmotility. Int. J. Mol. Sci. 2021, 22, 9990. [Google Scholar] [CrossRef]
- Edinoff, A.N.; Wu, N.W.; Parker, K.; Dudossat, E.; Linquest, L.; Flanagan, C.J.; Dharani, A.; Patel, H.; Willett, O.; Cornett, E.M.; et al. Proton pump inhibitors, kidney damage, and mortality: An updated narrative review. Adv. Ther. 2023, 40, 2693–2709. [Google Scholar] [CrossRef]
- Huang, H.; Tseng, Y.; Chen, Y.; Chen, P.; Chiu, H. Diagnostic accuracy of the clinical dementia rating scale for detecting mild cognitive impairment and dementia: A bivariate meta-analysis. Int. J. Geriatr. Psychiatry 2021, 36, 239–251. [Google Scholar] [CrossRef]
- Silveri, M.C.; Reali, G.; Jenner, C.; Puopolo, M. Attention and memory in the preclinical stage of dementia. J. Geriatr. Psych. Neur. 2007, 20, 67–75. [Google Scholar] [CrossRef]
- Grober, E.; Hall, C.B.; Lipton, R.B.; Zonderman, A.B.; Resnick, S.M.; Kawas, C. Memory impairment, executive dysfunction, and intellectual decline in preclinical Alzheimer’s disease. J. Int. Neuropsychol. Soc. 2008, 14, 266–278. [Google Scholar] [CrossRef]
- Volkert, D.; Chourdakis, M.; Faxen-Irving, G.; Frühwald, T.; Landi, F.; Suominen, M.H.; Vandewoude, M.; Wirth, R.; Schneider, S.M. ESPEN guidelines on nutrition in dementia. Clin. Nutr. 2015, 34, 1052–1073. [Google Scholar] [CrossRef]
- Razani, J.; Casas, R.; Wong, J.T.; Lu, P.; Alessi, C.; Josephson, K. Relationship between executive functioning and activities of daily living in patients with relatively mild dementia. Appl. Neuropsychol. 2007, 14, 208–214. [Google Scholar] [CrossRef]
- Marshall, G.A.; Rentz, D.M.; Frey, M.T.; Locascio, J.J.; Johnson, K.A.; Sperling, R.A. Executive function and instrumental activities of daily living in MCI and AD. Alzheimers Dement. 2011, 7, 300–308. [Google Scholar] [CrossRef]
- Holm, B.; Söderhamn, O. Factors associated with nutritional status in a group of people in an early stage of dementia. Clin. Nutr. 2003, 22, 385–389. [Google Scholar] [CrossRef]
- Johansson, M.M.; Marcusson, J.; Wressle, E. Cognitive impairment and its consequences in everyday life: Experiences of people with mild cognitive impairment or mild dementia and their relatives. Int. Psychogeriatr. 2015, 27, 949–958. [Google Scholar] [CrossRef]
- Droogsma, E.; Van Asselt, D.Z.B.; Scholzel-Dorenbos, C.J.M.; Van Steijn, J.H.M.; Van Walderveen, P.E.; Van Der Hooft, C.S. Nutritional status of community-dwelling elderly with newly diagnosed Alzheimer’s disease: Prevalence of malnutrition and the relation of various factors to nutritional status. J. Nutr. Health Aging 2013, 17, 606–610. [Google Scholar] [CrossRef]
- Suma, S.; Watanabe, Y.; Hirano, H.; Kimura, A.; Edahiro, A.; Awata, S.; Yamashita, Y.; Matsushita, K.; Arai, H.; Sakurai, T. Factors affecting the appetites of persons with Alzheimer’s disease and mild cognitive impairment: Factors related to appetite and dementia. Geriatr. Gerontol. Int. 2018, 18, 1236–1243. [Google Scholar] [CrossRef]
- Di Iulio, F.; Palmer, K.; Blundo, C.; Casini, A.R.; Gianni, W.; Caltagirone, C.; Spalletta, G. Occurrence of neuropsychiatric symptoms and psychiatric disorders in mild Alzheimer’s disease and mild cognitive impairment subtypes. Int. Psychogeriatr. 2010, 22, 629–640. [Google Scholar] [CrossRef]
- Köhler, C.A.; Magalhães, T.F.; Oliveira, J.M.M.P.; Alves, G.S.; Knöchel, C.; Oertel-Knöchel, V.; Pantel, J.; Carvalho, A.F. Neuropsychiatric disturbances in mild cognitive impairment (MCI): A Systematic review of population-based studies. Curr. Alzheimer Res. 2016, 13, 1066–1082. [Google Scholar] [CrossRef]
- Kai, K.; Hashimoto, M.; Amano, K.; Tanaka, H.; Fukuhara, R.; Ikeda, M. Relationship between eating disturbance and dementia severity in patients with Alzheimer’s disease. PLoS ONE 2015, 10, e0133666. [Google Scholar] [CrossRef]
- Leung, D.K.Y.; Chan, W.C.; Spector, A.; Wong, G.H.Y. Prevalence of depression, anxiety, and apathy symptoms across dementia stages: A systematic review and meta-analysis. Int. J. Geriatr. Psychiatry 2021, 36, 1330–1344. [Google Scholar] [CrossRef]
- Simmons, W.K.; Burrows, K.; Avery, J.A.; Kerr, K.L.; Bodurka, J.; Savage, C.R.; Drevets, W.C. Depression-related increases and decreases in appetite: Dissociable patterns of aberrant activity in reward and interoceptive neurocircuitry. Am. J. Psychiatry 2016, 173, 418–428. [Google Scholar] [CrossRef]
- Kimura, A.; Sugimoto, T.; Kitamori, K.; Saji, N.; Niida, S.; Toba, K.; Sakurai, T. Malnutrition is associated with behavioral and psychiatric symptoms of dementia in older women with mild cognitive impairment and early-stage Alzheimer’s disease. Nutrients 2019, 11, 1951. [Google Scholar] [CrossRef]
- Zamboni, G.; Wilcock, G. Lack of awareness of symptoms in people with dementia: The structural and functional basis. Int. J. Geriatr. Psychiatry 2011, 26, 783–792. [Google Scholar] [CrossRef] [PubMed]
- Pacyna, R.R.; Han, S.D.; Wroblewski, K.E.; McClintock, M.K.; Pinto, J.M. Rapid olfactory decline during aging predicts dementia and GMV loss in AD brain regions. Alzheimers Dement. 2023, 19, 1479–1490. [Google Scholar] [CrossRef]
- Bathini, P.; Brai, E.; Auber, L.A. Olfactory dysfunction in the pathophysiological continuum of dementia. Ageing Res. Rev. 2019, 55, 100956. [Google Scholar] [CrossRef]
- Yap, A.C.; Mahendran, R.; Kua, E.H.; Zhou, W.; Wang, D.Y. Olfactory dysfunction is associated with mild cognitive impairment in community-dwelling older adults. Front. Aging Neurosci. 2022, 14, 930686. [Google Scholar] [CrossRef] [PubMed]
- Steinbach, S.; Hundt, W.; Vaitl, A.; Heinrich, P.; Förster, S.; Bürger, K.; Zahnert, T. Taste in mild cognitive impairment and Alzheimer’s disease. J. Neurol. 2010, 257, 238–246. [Google Scholar] [CrossRef]
- Yoo, H.S.; Jeon, S.; Chung, S.J.; Yun, M.; Lee, P.H.; Sohn, Y.H.; Evans, A.C.; Ye, B.S. Olfactory dysfunction in Alzheimer’s disease-and Lewy body-related cognitive impairment. Alzheimers Dement. 2018, 14, 1243–1252. [Google Scholar] [CrossRef] [PubMed]
- Jin, S.-Y.; Jeong, H.S.; Lee, J.W.; Kwon, K.R.; Rha, K.-S.; Kim, Y.M. Effects of nutritional status and cognitive ability on olfactory function in geriatric patients. Auris Nasus Larynx 2016, 43, 56–61. [Google Scholar] [CrossRef]
- Gunzer, W. Changes of olfactory performance during the process of aging—Psychophysical testing and its relevance in the fight against malnutrition. J. Nutr. Health Aging 2017, 21, 1010–1015. [Google Scholar] [CrossRef]
- Toussaint, N.; de Roon, M.; van Campen, J.P.C.M.; Kremer, S.; Boesveldt, S. Loss of olfactory function and nutritional status in vital older adults and geriatric patients. Chem. Senses 2015, 40, 197–203. [Google Scholar] [CrossRef]
- Kim, W.Y.; Hur, M.; Cho, M.S.; Lee, H.S. Effect of olfactory function on nutritional status of Korean elderly women. Nutr. Res. 2003, 23, 723–734. [Google Scholar] [CrossRef]
- Gao, S.; Nguyen, J.T.; Hendrie, H.C.; Unverzagt, F.W.; Hake, A.; Smith-Gamble, V.; Hall, K. accelerated weight loss and incident dementia in an elderly African-American cohort. J. Am. Geriatr. Soc. 2011, 59, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Ogunniyi, A.; Gao, S.; Unverzagt, F.W.; Baiyewu, O.; Gureje, O.; Nguyen, J.T.; Smith-Gamble, V.; Murrell, J.R.; Hake, A.M.; Hall, K.S.; et al. Weight loss and incident dementia in elderly Yoruba Nigerians: A 10-year follow-up study. Int. Psychogeriatr. 2011, 23, 387–394. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.K.; Wilkins, C.H.; Morris, J.C. Accelerated weight loss may precede diagnosis in Alzheimer disease. Arch. Neurol. 2006, 63, 1312–1317. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Fu, W.; Cao, S.; Jiang, H.; Guo, Y.; Xv, H.; Liu, J.; Gan, Y.; Lu, Z. Weight loss and the risk of dementia: A meta-analysis of cohort studies. Curr. Alzheimer Res. 2021, 18, 125–135. [Google Scholar] [CrossRef] [PubMed]
- Doorduijn, A.S.; van de Rest, O.; van der Flier, W.M.; Visser, M.; de van der Schueren, M.A.E. Energy and protein intake of Alzheimer’s disease patients compared to cognitively normal controls: Systematic review. J. Am. Med. Dir. Assoc. 2019, 20, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Shatenstein, B.; Kergoat, M.-J.; Reid, I. Poor nutrient intakes during 1-year follow-up with community-dwelling older adults with early-stage Alzheimer dementia compared to cognitively intact matched controls. J. Am. Diet. Assoc. 2007, 107, 2091–2099. [Google Scholar] [CrossRef] [PubMed]
- Doorduijn, A.S.; De Van Der Schueren, M.A.E.; Van De Rest, O.; De Leeuw, F.A.; Hendriksen, H.M.A.; Teunissen, C.E.; Scheltens, P.; Van Der Flier, W.M.; Visser, M. Energy Intake and expenditure in patients with Alzheimer’s disease and mild cognitive impairment: The NUDAD project. Alzheimers Res. Ther. 2020, 12, 116. [Google Scholar] [CrossRef] [PubMed]
- Porter, J.; Thompson, H.; Tjahyo, A.S. Understanding total energy expenditure in people with dementia: A systematic review with directions for future research. Australas. J. Ageing 2021, 40, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Vecchio, I.; Sorrentino, L.; Paoletti, A.; Marra, R.; Arbitrio, M. The state of the art on acetylcholinesterase inhibitors in the treatment of Alzheimer’s disease. J. Cent. Nerv. Syst. Dis. 2021, 13, 11795735211029113. [Google Scholar] [CrossRef]
- Soysal, P.; Isik, A.T.; Stubbs, B.; Solmi, M.; Volpe, M.; Luchini, C.; D’Onofrio, G.; Pilotto, A.; Manzato, E.; Sergi, G.; et al. Acetylcholinesterase inhibitors are associated with weight loss in older people with dementia: A systematic review and meta-analysis. J. Neurol. Neurosurg. Psychiatry 2016, 87, 1368–1374. [Google Scholar] [CrossRef]
- Beaudart, C.; Sanchez-Rodriguez, D.; Locquet, M.; Reginster, J.Y.; Lengelé, L.; Bruyère, O. Malnutrition as a strong predictor of the onset of sarcopenia. Nutrients 2019, 11, 2883. [Google Scholar] [CrossRef]
- Chang, K.-V.; Hsu, T.-H.; Wu, W.-T.; Huang, K.-C.; Han, D.-S. Association between sarcopenia and cognitive impairment: A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2016, 17, 1164.e7–1164.e15. [Google Scholar] [CrossRef] [PubMed]
- Feng, L.; Chu, Z.; Quan, X.; Zhang, Y.; Yuan, W.; Yao, Y.; Zhao, Y.; Fu, S. Malnutrition is positively associated with cognitive decline in centenarians and oldest-old adults: A cross-sectional study. EClinicalMedicine 2022, 47, 101336. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.W.; Kim, Y.; Choi, Y.H.; Lee, J.M.; Yoon, B.; Park, K.W.; Kim, S.E.; Kim, H.J.; Yoon, S.J.; Jeong, J.H.; et al. Association of nutritional status with cognitive stage in the elderly Korean population: The Korean Brain Aging Study for the Early Diagnosis and Prediction of Alzheimer’s Disease. J. Clin. Neurol. 2019, 15, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Borda, M.G.; Ayala Copete, A.M.; Tovar-Rios, D.A.; Jaramillo-Jimenez, A.; Giil, L.M.; Soennesyn, H.; Gómez-Arteaga, C.; Venegas-Sanabria, L.C.; Kristiansen, I.; Chavarro-Carvajal, D.A.; et al. Association of malnutrition with functional and cognitive trajectories in people living with dementia: A five-year follow-up study. J. Alzheimers Dis. 2021, 79, 1713–1722. [Google Scholar] [CrossRef] [PubMed]
- Sanders, C.; Behrens, S.; Schwartz, S.; Wengreen, H.; Corcoran, C.D.; Lyketsos, C.G.; Tschanz, J.T. Nutritional status is associated with faster cognitive decline and worse functional impairment in the progression of dementia. J. Alzheimers Dis. 2016, 52, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Kishino, Y.; Sugimoto, T.; Kimura, A.; Kuroda, Y.; Uchida, K.; Matsumoto, N.; Saji, N.; Niida, S.; Sakurai, T. Longitudinal association between nutritional status and BPSD in older women with mild cognitive impairment and early-stage Alzheimer’s disease. Clin. Nutr. 2022, 41, 1906–1912. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, D.O. B Vitamins and the brain: Mechanisms, dose and efficacy—A review. Nutrients 2016, 8, 68. [Google Scholar] [CrossRef] [PubMed]
- Hanna, M.; Jaqua, E.; Nguyen, V.; Clay, J. B Vitamins: Functions and uses in medicine. Perm. J. 2022, 26, 89–97. [Google Scholar] [CrossRef]
- Temova Rakuša, Ž.; Roškar, R.; Hickey, N.; Geremia, S. Vitamin B12 in foods, food supplements, and medicines—A review of its role and properties with a focus on its stability. Molecules 2022, 28, 240. [Google Scholar] [CrossRef]
- Gillies, N.; Cameron-Smith, D.; Pundir, S.; Wall, C.R.; Milan, A.M. Exploring trajectories in dietary adequacy of the B vitamins folate, riboflavin, vitamins B6 and B12, with advancing older age: A systematic review. Br. J. Nutr. 2021, 126, 449–459. [Google Scholar] [CrossRef] [PubMed]
- Russell, R.M. Factors in aging that effect the bioavailability of nutrients. J. Nutr. 2001, 131, 1359S–1361S. [Google Scholar] [CrossRef]
- Basu, T.K.; Donaldson, D. Intestinal absorption in health and disease: Micronutrients. Best Pract. Res. Clin. Gastroenterol. 2003, 17, 957–979. [Google Scholar] [CrossRef]
- Porter, K.M.; Ward, M.; Hughes, C.F.; O’Kane, M.; Hoey, L.; McCann, A.; Molloy, A.M.; Cunningham, C.; Casey, M.C.; Tracey, F.; et al. Hyperglycemia and metformin use are associated with B vitamin deficiency and cognitive dysfunction in older adults. J. Clin. Endocr. Metab. 2019, 104, 4837–4847. [Google Scholar] [CrossRef] [PubMed]
- Gibson, G.E.; Hirsch, J.A.; Fonzetti, P.; Jordan, B.D.; Cirio, R.T.; Elder, J. Vitamin B1 (thiamine) and dementia. Ann. N. Y. Acad. Sci. 2016, 1367, 21–30. [Google Scholar] [CrossRef]
- Briani, C.; Torre, C.D.; Citton, V.; Manara, R.; Pompanin, S.; Binotto, G.; Adami, F. Cobalamin deficiency: Clinical picture and radiological findings. Nutrients 2013, 5, 4521. [Google Scholar] [CrossRef]
- Pacei, F.; Tesone, A.; Laudi, N.; Laudi, E.; Cretti, A.; Pnini, S.; Varesco, F.; Colombo, C. The relevance of thiamine evaluation in a practical setting. Nutrients 2020, 12, 2810. [Google Scholar] [CrossRef]
- Mosegaard, S.; Dipace, G.; Bross, P.; Carlsen, J.; Gregersen, N.; Olsen, R.K.J. Riboflavin deficiency—Implications for general human health and inborn errors of metabolism. Int. J. Mol. Sci. 2020, 21, 3847. [Google Scholar] [CrossRef] [PubMed]
- Porter, K.; Hoey, L.; Hughes, C.F.; Ward, M.; McNulty, H. Causes, consequences and public health implications of low B-vitamin status in ageing. Nutrients 2016, 8, 725. [Google Scholar] [CrossRef]
- Gasperi, V.; Sibilano, M.; Savini, I.; Catani, M.V. Niacin in the central nervous system: An update of biological aspects and clinical applications. Int. J. Mol. Sci. 2019, 20, 974. [Google Scholar] [CrossRef]
- Xu, J.; Patassini, S.; Begley, P.; Church, S.; Waldvogel, H.J.; Faull, R.L.M.; Unwin, R.D.; Cooper, G.J.S. Cerebral deficiency of vitamin B5 (d-pantothenic acid; pantothenate) as a potentially-reversible cause of neurodegeneration and dementia in sporadic Alzheimer’s disease. Biochem. Biophys. Res. Commun. 2020, 527, 676–681. [Google Scholar] [CrossRef] [PubMed]
- Roth, D.E.; Abrams, S.A.; Aloia, J.; Bergeron, G.; Bourassa, M.W.; Brown, K.H.; Calvo, M.S.; Cashman, K.D.; Combs, G.; De-Regil, L.M.; et al. Global prevalence and disease burden of vitamin D deficiency: A roadmap for action in low- and middle-income countries. Ann. N. Y. Acad. Sci. 2018, 1430, 44–79. [Google Scholar] [CrossRef] [PubMed]
- Bouillon, R.; Antonio, L.; Olarte, O.R. Calcifediol (25OH vitamin D3) deficiency: A risk factor from early to old age. Nutrients 2022, 14, 1168. [Google Scholar] [CrossRef] [PubMed]
- Hossein-nezhad, A.; Holick, M.F. Vitamin D for health: A global perspective. Mayo Clin. Proc. 2013, 88, 720–755. [Google Scholar] [CrossRef] [PubMed]
- Heaney, R.P.; Armas, L.A.G.; French, C. All-source basal vitamin D inputs are greater than previously thought and cutaneous inputs are smaller. J. Nutr. 2013, 143, 571–575. [Google Scholar] [CrossRef] [PubMed]
- Crowe, F.L.; Steur, M.; Allen, N.E.; Appleby, P.N.; Travis, R.C.; Key, T.J. Plasma concentrations of 25-hydroxyvitamin D in meat eaters, fish eaters, vegetarians and vegans: Results from the EPIC-Oxford study. Public Health Nutr. 2011, 14, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Wacker, M.; Holick, M.F. Sunlight and vitamin D: A global perspective for health. Dermatoendocrinol. 2013, 5, 51–108. [Google Scholar] [CrossRef]
- Holick, M.F. Biological effects of sunlight, ultraviolet radiation, visible light, infrared radiation and vitamin D for health. Anticancer Res. 2016, 36, 1345–1356. [Google Scholar]
- Wang, T.J.; Zhang, F.; Richards, J.B.; Kestenbaum, B.; van Meurs, J.B.; Berry, D.; Kiel, D.P.; Streeten, E.A.; Ohlsson, C.; Koller, D.L.; et al. Common genetic determinants of vitamin D insufficiency: A genome-wide association study. Lancet 2010, 376, 180–188. [Google Scholar] [CrossRef]
- Clements, M.R.; Johnson, L.; Fraser, D.R. A New mechanism for induced vitamin D deficiency in calcium deprivation. Nature 1987, 325, 62–65. [Google Scholar] [CrossRef]
- Steingrimsdottir, L.; Gunnarsson, O.; Indridason, O.S.; Franzson, L.; Sigurdsson, G. Relationship between serum parathyroid hormone levels, vitamin D sufficiency, and calcium intake. JAMA 2005, 294, 2336–2341. [Google Scholar] [CrossRef] [PubMed]
- Chai, B.; Gao, F.; Wu, R.; Dong, T.; Gu, C.; Lin, Q.; Zhang, Y. Vitamin D deficiency as a risk factor for dementia and Alzheimer’s disease: An updated meta-analysis. BMC Neurol. 2019, 19, 284. [Google Scholar] [CrossRef]
- Goodwill, A.M.; Szoeke, C. A systematic review and meta-analysis of the effect of low vitamin D on cognition. J. Am. Geriatr. Soc. 2017, 65, 2161–2168. [Google Scholar] [CrossRef] [PubMed]
- van der Schaft, J.; Koek, H.L.; Dijkstra, E.; Verhaar, H.J.J.; van der Schouw, Y.T.; Emmelot-Vonk, M.H. The association between vitamin D and cognition: A systematic review. Ageing Res. Rev. 2013, 12, 1013–1023. [Google Scholar] [CrossRef]
- Sommer, I.; Griebler, U.; Kien, C.; Auer, S.; Klerings, I.; Hammer, R.; Holzer, P.; Gartlehner, G. Vitamin D deficiency as a risk factor for dementia: A systematic review and meta-analysis. BMC Geriatr. 2017, 17, 16. [Google Scholar] [CrossRef]
- Shen, L.; Ji, H.F. Vitamin D deficiency is associated with increased risk of Alzheimer’s disease and dementia: Evidence from meta-analysis. Nutr. J. 2015, 14, 76. [Google Scholar] [CrossRef]
- Serón-Arbeloa, C.; Labarta-Monzón, L.; Puzo-Foncillas, J.; Mallor-Bonet, T.; Lafita-López, A.; Bueno-Vidales, N.; Montoro-Huguet, M. Malnutrition screening and assessment. Nutrients 2022, 14, 2392. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the Global Clinical Nutrition Community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef]
- Kaiser, M.J.; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.; Charlton, K.E.; Maggio, M.; et al. Validation of the Mini Nutritional Assessment Short-Form (MNA®-SF): A practical tool for identification of nutritional status. J. Nutr. Health Aging 2009, 13, 782–788. [Google Scholar] [CrossRef]
- Guigoz, Y.; Vellas, B.; Garry, P.J. Assessing the nutritional status of the elderly: The Mini Nutritional Assessment as part of the geriatric evaluation. Nutr. Rev. 1996, 54, S59–S65. [Google Scholar] [CrossRef]
- Alibhai, S.M.H.; Greenwood, C.; Payette, H. An approach to the management of unintentional weight loss in elderly people. Can. Med. Assoc. J. 2005, 172, 773–780. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E. Undernutrition in Older Adults. Fam Pract 2012, 29, i89–i93. [Google Scholar] [CrossRef] [PubMed]
- Morilla-Herrera, J.C.; Martín-Santos, F.J.; Caro-Bautista, J.; Saucedo-Figueredo, C.; García-Mayor, S.; Morales-Asencio, J.M. Effectiveness of food-based fortification in older people. A systematic review and meta-analysis. J. Nutr. Health Aging 2016, 20, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Trabal, J.; Farran-Codina, A. Effects of dietary enrichment with conventional foods on energy and protein intake in older adults: A systematic review. Nutr. Rev. 2015, 73, 624–633. [Google Scholar] [CrossRef]
- Lam, I.T.Y.; Keller, H.H.; Pfisterer, K.; Duizer, L.; Stark, K.; Duncan, A.M. Micronutrient food fortification for residential care: A scoping review of current interventions. J. Am. Med. Dir. Assoc. 2016, 17, 588–595. [Google Scholar] [CrossRef] [PubMed]
- Lochs, H.; Dejong, C.; Hammarqvist, F.; Hebuterne, X.; Leon-Sanz, M.; Schütz, T.; van Gemert, W.; van Gossum, A.; Valentini, L.; Lübke, H.; et al. ESPEN guidelines on enteral nutrition: Gastroenterology. Clin. Nutr. 2006, 25, 260–274. [Google Scholar] [CrossRef] [PubMed]
- Allen, V.J.; Methven, L.; Gosney, M.A. Use of nutritional complete supplements in older adults with dementia: Systematic review and meta-analysis of clinical outcomes. Clin. Nutr. 2013, 32, 950–957. [Google Scholar] [CrossRef]
- Lauque, S.; Arnaud-Battandier, F.; Gillette, S.; Plaze, J.-M.; Andrieu, S.; Cantet, C.; Vellas, B. Improvement of weight and fat-free mass with oral nutritional supplementation in patients with Alzheimer’s disease at risk of malnutrition: A prospective randomized study. J. Am. Geriatr. Soc. 2004, 52, 1702–1707. [Google Scholar] [CrossRef] [PubMed]
- Tana, C.; Lauretani, F.; Ticinesi, A.; Gionti, L.; Nouvenne, A.; Prati, B.; Meschi, T.; Maggio, M. Impact of nutritional status on caregiver burden of elderly outpatients. A cross-sectional study. Nutrients 2019, 11, 281. [Google Scholar] [CrossRef]
- Fjellström, C.; Starkenberg, Å.; Wesslén, A.; Licentiate, M.S.; Tysén Bäckström, A.-C.; Faxén-Irving, G. To be a good food provider: An exploratory study among spouses of persons with Alzheimer’s disease. Am. J. Alzheimers Dis. 2010, 25, 521–526. [Google Scholar] [CrossRef]
- Bunn, D.K.; Abdelhamid, A.; Copley, M.; Cowap, V.; Dickinson, A.; Howe, A.; Killett, A.; Poland, F.; Potter, J.F.; Richardson, K.; et al. Effectiveness of interventions to indirectly support food and drink intake in people with dementia: Eating and Drinking Well in dementiA (EDWINA) systematic review. BMC Geriatr. 2016, 16, 89. [Google Scholar] [CrossRef] [PubMed]
- Young, K.; Bunn, F.; Trivedi, D.; Dickinson, A. Nutritional education for community dwelling older people: A systematic review of randomised controlled trials. Int. J. Nurs. Stud. 2011, 48, 751–780. [Google Scholar] [CrossRef] [PubMed]
- Stroebele, N.; De Castro, J.M. Effect of ambience on food intake and food choice. Nutrition 2004, 20, 821–838. [Google Scholar] [CrossRef] [PubMed]
- Nieuwenhuizen, W.F.; Weenen, H.; Rigby, P.; Hetherington, M.M. Older adults and patients in need of nutritional support: Review of current treatment options and factors influencing nutritional intake. Clin. Nutr. 2010, 29, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Nijs, K.A.N.D.; de Graaf, C.; Kok, F.J.; van Staveren, W.A. Effect of family style mealtimes on quality of life, physical performance, and body weight of nursing home residents: Cluster randomised controlled trial. BMJ 2006, 332, 1180–1183. [Google Scholar] [CrossRef]
- e Castro, J.M.; Brewer, E.M. The amount eaten in meals by humans is a power function of the number of people present. Physiol. Behav. 1992, 51, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Locher, J.L.; Robinson, C.O.; Roth, D.L.; Ritchie, C.S.; Burgio, K.L. The effect of the presence of others on caloric intake in homebound older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 1475–1478. [Google Scholar] [CrossRef] [PubMed]
- Volicer, L.; Stelly, M.; Morris, J.; McLaughlin, J.; Volicer, B.J. Effects of dronabinol on anorexia and disturbed behavior in patients with Alzheimer’s disease. Int. J. Geriatr. Psych. 1997, 12, 913–919. [Google Scholar] [CrossRef]
- Thomas, D.R. Guidelines for the use of orexigenic drugs in long-term care. Nutr. Clin. Pract. 2006, 21, 82–87. [Google Scholar] [CrossRef]
- Duning, T.; Kloska, S.; Steinsträter, O.; Kugel, H.; Heindel, W.; Knecht, S. Dehydration confounds the assessment of brain atrophy. Neurology 2005, 64, 548–550. [Google Scholar] [CrossRef]
- Cowen, L.E.; Hodak, S.P.; Verbalis, J.G. Age-associated abnormalities of water homeostasis. Endocrinol. Metab. Clin. N. Am. 2013, 42, 349–370. [Google Scholar] [CrossRef]
- Schliess, F.; Häussinger, D. Cell volume and insulin signaling. In International Review of Cytology; Elsevier Science & Technology: Cambridge, MA, USA, 2003; Volume 225, pp. 187–228. ISBN 0074-7696. [Google Scholar]
- Lauriola, M.; Mangiacotti, A.; D’Onofrio, G.; Cascavilla, L.; Paris, F.; Paroni, G.; Seripa, D.; Greco, A.; Sancarlo, D. Neurocognitive disorders and dehydration in older patients: Clinical experience supports the hydromolecular hypothesis of dementia. Nutrients 2018, 10, 562. [Google Scholar] [CrossRef] [PubMed]
- Nishi, S.K.; Babio, N.; Paz-Graniel, I.; Serra-Majem, L.; Vioque, J.; Fitó, M.; Corella, D.; Pintó, X.; Bueno-Cavanillas, A.; Tur, J.A.; et al. Water intake, hydration status and 2-year changes in cognitive performance: A prospective cohort study. BMC Med. 2023, 21, 82. [Google Scholar] [CrossRef] [PubMed]
- Mantantzis, K.; Drewelies, J.; Duezel, S.; Steinhagen-Thiessen, E.; Demuth, I.; Wagner, G.G.; Lindenberger, U.; Gerstorf, D. Dehydration predicts longitudinal decline in cognitive functioning and well-being among older adults. Psychol. Aging 2020, 35, 517–528. [Google Scholar] [CrossRef]
- Eastley, R.; Wilcock, G.K.; Bucks, R.S. Vitamin B12 deficiency in dementia and cognitive impairment: The effects of treatment on neuropsychological function. Int. J. Geriatr. Psychiatry 2000, 15, 226–233. [Google Scholar] [CrossRef]
- Ueno, A.; Hamano, T.; Enomoto, S.; Shirafuji, N.; Nagata, M.; Kimura, H.; Ikawa, M.; Yamamura, O.; Yamanaka, D.; Ito, T.; et al. Influences of vitamin B 12 supplementation on cognition and homocysteine in patients with vitamin B 12 deficiency and cognitive impairment. Nutrients 2022, 14, 1494. [Google Scholar] [CrossRef]
- Kwok, T.; Lee, J.; Ma, R.C.; Wong, S.Y.; Kung, K.; Lam, A.; Ho, C.S.; Lee, V.; Harrison, J.; Lam, L. A Randomized placebo controlled trial of vitamin B12 supplementation to prevent cognitive decline in older diabetic people with borderline low serum vitamin B12. Clin. Nutr. 2017, 36, 1509–1515. [Google Scholar] [CrossRef] [PubMed]
- Eussen, S.J.; de Groot, L.C.; Joosten, L.W.; Bloo, R.J.; Clarke, R.; Ueland, P.M.; Schneede, J.; Blom, H.J.; Hoefnagels, W.H.; Staveren, W.A. van Effect of oral vitamin B-12 with or without folic acid on cognitive function in older people with mild vitamin B-12 deficiency: A randomized, placebo-controlled trial. Am. J. Clin. Nutr. 2006, 84, 361–370. [Google Scholar] [CrossRef]
- Fioravanti, M.; Ferrario, E.; Massaia, M.; Cappa, G.; Rivolta, G.; Grossi, E.; Buckley, A.E. Low Folate levels in the cognitive decline of elderly patients and the efficacy of folate as a treatment for improving memory deficits. Arch. Gerontol. Geriatr. 1998, 26, 1–13. [Google Scholar] [CrossRef]
- Beauchet, O.; Launay, C.P.; Galery, K.; Vilcocq, C.; Dontot-Payen, F.; Rousseau, B.; Benoit, V.; Allali, G. Effects of vitamin D and calcium fortified yogurts on gait, cognitive performances, and serum 25-hydroxyvitamin D concentrations in older community-dwelling females: Results from the GAit, MEmory, DiEtary and vitamin D (GAME-D2) randomized controlled trial. Nutrients 2019, 11, 2880. [Google Scholar] [CrossRef]
- Hu, J.; Jia, J.; Zhang, Y.; Miao, R.; Huo, X.; Ma, F. Effects of vitamin D3 supplementation on cognition and blood lipids: A 12-month randomised, double-blind, placebo-controlled trial. J. Neurol. Neurosurg. Psychiatry 2018, 89, 1341–1347. [Google Scholar] [CrossRef] [PubMed]
- Jia, J.; Hu, J.; Huo, X.; Miao, R.; Zhang, Y.; Ma, F. Effects of vitamin D supplementation on cognitive function and blood Aβ-related biomarkers in older adults with Alzheimer’s disease: A randomised, double-blind, placebo-controlled trial. J. Neurol. Neurosurg. Psychiatry 2019, 90, 1347–1352. [Google Scholar] [CrossRef] [PubMed]
- Castle, M.; Fiedler, N.; Pop, L.C.; Schneider, S.J.; Schlussel, Y.; Sukumar, D.; Hao, L.; Shapses, S.A. Three doses of vitamin D and cognitive outcomes in older women: A double-blind randomized controlled trial. J. Gerontol. A Biol. Sci. Med. Sci. 2020, 75, 835–842. [Google Scholar] [CrossRef] [PubMed]
- Jorde, R.; Kubiak, J.; Svartberg, J.; Fuskevåg, O.M.; Figenschau, Y.; Martinaityte, I.; Grimnes, G. Vitamin D supplementation has no effect on cognitive performance after four months in mid-aged and older subjects. J. Neurol. Sci. 2019, 396, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Han, J.H.; Ginde, A.A.; Brown, S.M.; Baughman, A.; Collar, E.M.; Ely, E.W.; Gong, M.N.; Hope, A.A.; Hou, P.C.; Hough, C.L.; et al. Effect of early high-dose vitamin D3 repletion on cognitive outcomes in critically ill adults. Chest 2021, 160, 909–918. [Google Scholar] [CrossRef] [PubMed]
- Owusu, J.E.; Islam, S.; Katumuluwa, S.S.; Stolberg, A.R.; Usera, G.L.; Anwarullah, A.A.; Shieh, A.; Dhaliwal, R.; Ragolia, L.; Mikhail, M.B.; et al. Cognition and vitamin D in older African-American women—Physical performance and osteoporosis prevention with vitamin D in older African Americans trial and dementia. J. Am. Geriatr. Soc. 2019, 67, 81–86. [Google Scholar] [CrossRef]
- Balk, E.M.; Raman, G.; Tatsioni, A.; Chung, M.; Lau, J.; Rosenberg, I.H. Vitamin B6, B12, and folic acid supplementation and cognitive function: A systematic review of randomized trials. Arch. Intern. Med. 2007, 167, 21–30. [Google Scholar] [CrossRef]
- Ford, A.H.; Almeida, O.P. Effect of vitamin B supplementation on cognitive function in the elderly: A systematic review and meta-analysis. Drugs Aging 2019, 36, 419–434. [Google Scholar] [CrossRef]
- McCleery, J.; Abraham, R.P.; Denton, D.A.; Rutjes, A.W.S.; Chong, L.-Y.; Al-Assaf, A.S.; Griffith, D.J.; Rafeeq, S.; Yaman, H.; Malik, M.A.; et al. Vitamin and mineral supplementation for preventing dementia or delaying cognitive decline in people with mild cognitive impairment. Cochrane Database Syst. Rev. 2018, 11, CD011905. [Google Scholar] [CrossRef]
- Rutjes, A.W.; Denton, D.A.; Di Nisio, M.; Chong, L.; Abraham, R.P.; Al-Assaf, A.S.; Anderson, J.L.; Malik, M.A.; Vernooij, R.W.; Martínez, G.; et al. Vitamin and mineral supplementation for maintaining cognitive function in cognitively healthy people in mid and late life. Cochrane Database Syst. Rev. 2018, 2019, CD011906. [Google Scholar] [CrossRef]
- Behrens, A.; Graessel, E.; Pendergrass, A.; Donath, C. Vitamin B-can it prevent cognitive decline? A systematic review and meta-analysis. Syst. Rev. 2020, 9, 111. [Google Scholar] [CrossRef] [PubMed]
- Malouf, R.; Grimley Evans, J.; Malouf, R. Vitamin B6 for cognition. Cochrane Database Syst. Rev. 2003, 2010, CD004393. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Guo, Y.; Men, J.; Fu, H.; Xu, T. The preventive efficacy of vitamin B supplements on the cognitive decline of elderly adults: A systematic review and meta-analysis. BMC Geriatr. 2021, 21, 367. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Liang, F.; Zhang, L.; Liu, J.; Dou, H. Vitamin D supplement for prevention of Alzheimer’s disease: A systematic review and meta-analysis. Am. J. Ther. 2021, 28, E638–E648. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.Y.; Cheng, Y.C.; Chiu, C.C.; Liu, H.C.; Huang, M.C.; Tu, Y.K.; Kuo, P.H. Effects of Vitamin D Supplementation on cognitive outcomes: A systematic review and meta-analysis. Neuropsychol. Rev. 2023; online ahead of print. [Google Scholar] [CrossRef]
- da Silva, A.B.J.; Barros, W.M.A.; da Silva, M.L.; Silva, J.M.L.; Souza, A.P.d.S.; da Silva, K.G.; de Sousa Fernandes, M.S.; Carneiro, A.C.B.d.F.; Souza, V.d.O.N.; Lagranha, C.J. Impact of vitamin D on cognitive functions in healthy individuals: A systematic review in randomized controlled clinical trials. Front. Psychol. 2022, 13, 987203. [Google Scholar] [CrossRef] [PubMed]
- Wald, D.S.; Kasturiratne, A.; Simmonds, M. Effect of folic acid, with or without other B vitamins, on cognitive decline: Meta-analysis of randomized trials. Am. J. Med. 2010, 123, 522–527.e2. [Google Scholar] [CrossRef] [PubMed]
- Beauchet, O.; Cooper-Brown, L.A.; Allali, G. Vitamin D Supplementation and cognition in adults: A systematic review of randomized controlled trials. CNS Drugs 2021, 35, 1249–1264. [Google Scholar] [CrossRef] [PubMed]
- Markun, S.; Gravestock, I.; Jäger, L.; Rosemann, T.; Pichierri, G.; Burgstaller, J.M. Effects of vitamin B12 supplementation on cognitive function, depressive symptoms, and fatigue: A systematic review, meta-analysis, and meta-regression. Nutrients 2021, 13, 923. [Google Scholar] [CrossRef]
- Grodstein, F. Gaps and novel approaches in nutrition epidemiology for dementia prevention. Alzheimers Dement. 2021, 17, e049652. [Google Scholar] [CrossRef]
- Yassine, H.N.; Samieri, C.; Livingston, G.; Glass, K.; Wagner, M.; Tangney, C.; Plassman, B.L.; Ikram, M.A.; Voigt, R.M.; Gu, Y.; et al. Nutrition state of science and dementia prevention: Recommendations of the nutrition for dementia prevention working group. Lancet Healthy Longev. 2022, 3, e501–e512. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.H.; Gao, X.; Na, M.; Kris-Etherton, P.M.; Mitchell, D.C.; Jensen, G.L. Dietary pattern, diet quality, and dementia: A systematic review and meta-analysis of prospective cohort studies. J. Alzheimers Dis. 2020, 78, 151–168. [Google Scholar] [CrossRef] [PubMed]
- van de Rest, O.; Berendsen, A.A.; Haveman-Nies, A.; de Groot, L.C. Dietary patterns, cognitive decline, and dementia: A systematic review. Adv. Nutr. 2015, 6, 154–168. [Google Scholar] [CrossRef] [PubMed]
- Rosato, V.; Temple, N.J.; La Vecchia, C.; Castellan, G.; Tavani, A.; Guercio, V. Mediterranean diet and cardiovascular disease: A systematic review and meta-analysis of observational studies. Eur. J. Nutr. 2019, 58, 173–191. [Google Scholar] [CrossRef] [PubMed]
- Valls-Pedret, C.; Sala-Vila, A.; Serra-Mir, M.; Corella, D.; de la Torre, R.; Martínez-González, M.Á.; Martínez-Lapiscina, E.H.; Fitó, M.; Pérez-Heras, A.; Salas-Salvadó, J.; et al. Mediterranean diet and age-related cognitive decline: A randomized clinical trial. JAMA Intern. Med. 2015, 175, 1094–1103. [Google Scholar] [CrossRef] [PubMed]
- Coelho-Júnior, H.J.; Trichopoulou, A.; Panza, F. Cross-sectional and longitudinal associations between adherence to Mediterranean diet with physical performance and cognitive function in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2021, 70, 101395. [Google Scholar] [CrossRef] [PubMed]
- Limongi, F.; Siviero, P.; Bozanic, A.; Noale, M.; Veronese, N.; Maggi, S. The effect of adherence to the Mediterranean diet on late-life cognitive disorders: A systematic review. J. Am. Med. Dir. Assoc. 2020, 21, 1402–1409. [Google Scholar] [CrossRef] [PubMed]
- Petersson, S.D.; Philippou, E. Mediterranean diet, cognitive function, and dementia: A systematic review of the evidence. Adv. Nutr. 2016, 7, 889–904. [Google Scholar] [CrossRef]
- Lourida, I.; Soni, M.; Thompson-Coon, J.; Purandare, N.; Lang, I.A.; Ukoumunne, O.C.; Llewellyn, D.J. Mediterranean diet, cognitive function, and dementia: A systematic review. Epidemiology 2013, 24, 479–489. [Google Scholar] [CrossRef]
- Singh, B.; Parsaik, A.K.; Mielke, M.M.; Erwin, P.J.; Knopman, D.S.; Petersen, R.C.; Roberts, R.O. Association of Mediterranean diet with mild cognitive impairment and Alzheimer’s disease: A systematic review and meta-analysis. J. Alzheimers Dis. 2014, 39, 271–282. [Google Scholar] [CrossRef]
- Radd-Vagenas, S.; Duffy, S.L.; Naismith, S.L.; Brew, B.J.; Flood, V.M.; Fiatarone Singh, M.A. Effect of the Mediterranean diet on cognition and brain morphology and function: A systematic review of randomized controlled trials. Am. J. Clin. Nutr. 2018, 107, 389–404. [Google Scholar] [CrossRef] [PubMed]
- van den Brink, A.C.; Brouwer-Brolsma, E.M.; Berendsen, A.A.M.; van de Rest, O. The Mediterranean, Dietary Approaches to Stop Hypertension (DASH), and Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diets are associated with less cognitive decline and a lower risk of Alzheimer’s disease—A review. Adv. Nutr. 2019, 10, 1040–1065. [Google Scholar] [CrossRef] [PubMed]
- Solfrizzi, V.; Custodero, C.; Lozupone, M.; Imbimbo, B.P.; Valiani, V.; Agosti, P.; Schilardi, A.; D’Introno, A.; La Montagna, M.; Calvani, M.; et al. Relationships of dietary patterns, foods, and micro- and macronutrients with Alzheimer’s disease and late-life cognitive disorders: A systematic review. J. Alzheimers Dis. 2017, 59, 815–849. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).