Assessing Sodium Intake in Middle-Aged and Older Adults with Elevated Blood Pressure: Validation of Spot Urine Excretion and Dietary Survey-Derived Estimates
Abstract
1. Introduction
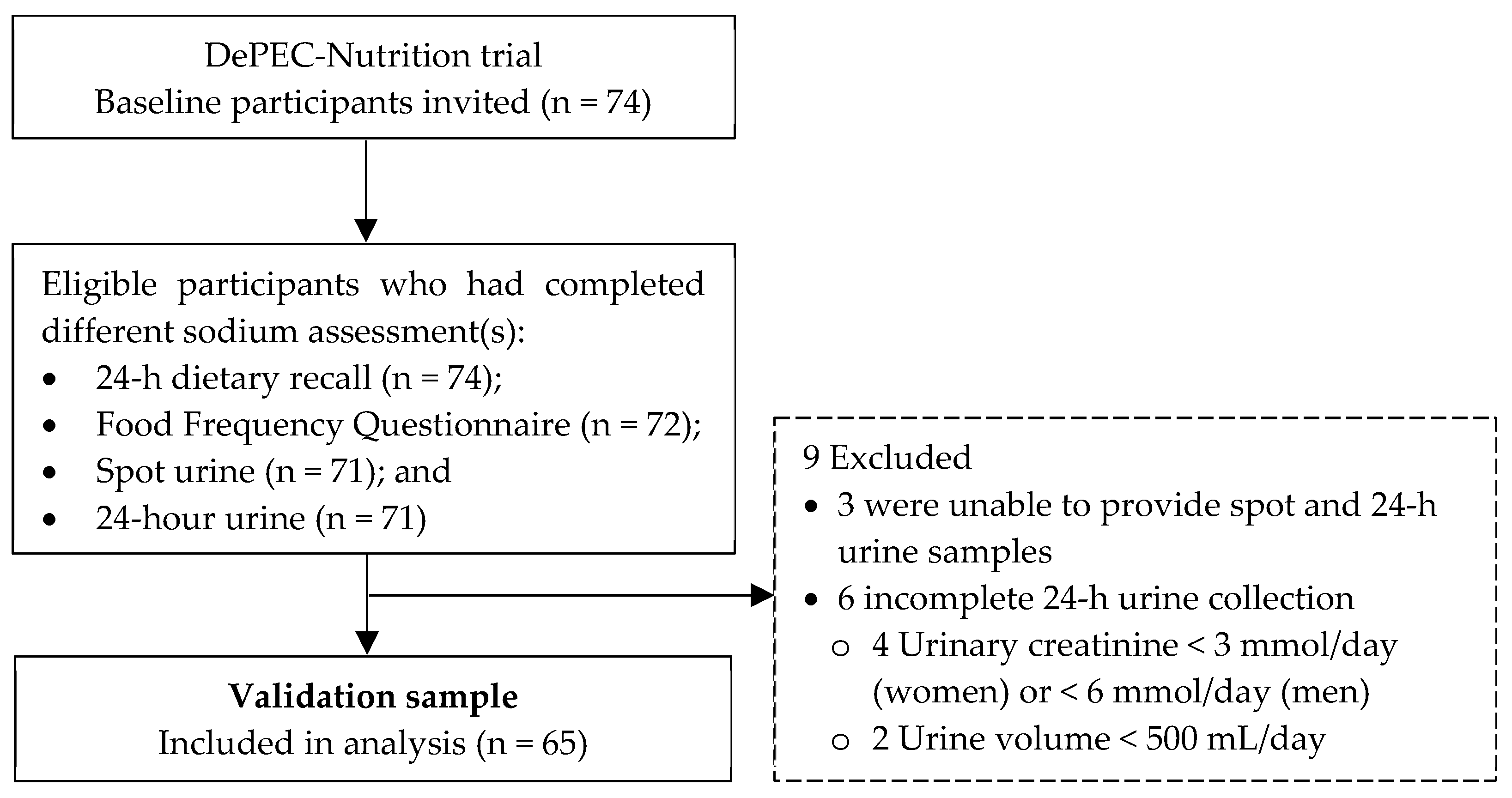
2. Materials and Methods
2.1. Study Design
2.2. Study Procedure
2.2.1. Assessment of Dietary Sodium Intake
2.2.2. Analysis of Dietary Sodium Intake
2.3. Development and Administration of 24DR Form
2.4. Development and Administration of FFQ
2.5. Statistical Analysis
3. Results
3.1. Sociodemographic, Anthropometry, and Clinical Characteristics
3.2. Biochemistry Data of 24-h Urine Collection and Salt Intake
3.3. Relative Validity of Alternative Methods for Estimating Dietary Sodium Intake
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Provido, S.M.; Abris, G.P.; Hong, S.; Yu, S.H.; Lee, C.B.; Lee, J.E. Association of Fried Food Intake with Prehypertension and Hypertension: The Filipino Women’s Diet and Health Study. Nutr. Res. Pract. 2020, 14, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. IHME 2020. Available online: https://vizhub.healthdata.org/gbd-results/ (accessed on 20 November 2023).
- World Health Organization. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis: World Health Day 2013. WHO. 2013. Available online: https://apps.who.int/iris/handle/10665/79059 (accessed on 20 November 2023).
- The World Health Organization. STEPwise Approach to Surveillance (STEPS); WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Lewington, S.; Clarke, R.; Qizilbash, N.; Peto, R.; Collins, R. Age-Specific Relevance of Usual Blood Pressure to Vascular Mortality: A Meta-Analysis of Individual Data for One Million Adults in 61 Prospective Studies. Lancet 2002, 360, 1903–1913. [Google Scholar]
- Campbell, N.R.C.; He, F.J.; Tan, M.; Cappuccio, F.P.; Neal, B.; Woodward, M.; Cogswell, M.E.; McLean, R.; Arcand, J.; MacGregor, G.A. The International Consortium for Quality Research on Dietary Sodium/Salt (TRUE) Position Statement on the Use of 24-Hour, Spot, and Short Duration (<24 Hours) Timed Urine Collections to Assess Dietary Sodium Intake. J. Clin. Hypertens. 2019, 21, 700–709. [Google Scholar]
- World Health Organization/Pan American Health Organization Regional Expert Group for Cardiovascular Disease Prevention through Population-Wide Dietary Salt Reduction. Protocol for Population Level Sodium Determination in 24-Hour Urine Samples; PAHO: Washington, DC, USA, 2010. [Google Scholar]
- Dennis, B.; Stamler, J.; Buzzard, M.; Conway, R.; Elliott, P.; Moag-Stahlberg, A.; Okayama, A.; Okuda, N.; Robertson, C.; Robinson, F.; et al. INTERMAP: The Dietary Data-Process and Quality Control. J. Hum. Hypertens. 2003, 17, 609–622. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Crino, M.; Wu, J.H.Y.; Woodward, M.; Barzi, F.; Land, M.A.; McLean, R.; Webster, J.; Enkhtungalag, B.; Neal, B. Mean Population Salt Intake Estimated from 24-Hour Urine Samples and Spot Urine Samples: A Systematic Review and Meta-Analysis. Int. J. Epidemiol. 2016, 45, 239–250. [Google Scholar] [CrossRef] [PubMed]
- Ji, C.; Sykes, L.; Paul, C.; Dary, O.; Legetic, B.; Campbell, N.R.C.; Cappuccio, F.P. Systematic Review of Studies Comparing 24-Hour and Spot Urine Collections for Estimating Population Salt Intake. Rev. Panam. Salud Publica 2012, 32, 307–315. [Google Scholar] [CrossRef]
- He, F.J.; Campbell, N.R.C.; Ma, Y.; MacGregor, G.A.; Cogswell, M.E.; Cook, N.R. Errors in Estimating Usual Sodium Intake by the Kawasaki Formula Alter Its Relationship with Mortality—Implications for Public Health. Int. J. Epidemiol. 2018, 47, 1784–1795. [Google Scholar] [CrossRef]
- Peng, Y.; Li, W.; Wang, Y.; Chen, H.; Bo, J.; Wang, X.; Su, X. Validation and Assessment of Three Methods to Estimate 24-Hour Urinary Sodium Excretion from Spot Urine Samples in Chinese Adults. PLoS ONE 2016, 11, e0149655. [Google Scholar]
- McLean, R.M.; Farmer, V.L.; Nettleton, A.; Cameron, C.M.; Cook, N.R.; Campbell, N.R.C. Twenty-Four-Hour Diet Recall and Diet Records Compared with 24-Hour Urinary Excretion to Predict an Individual’s Sodium Consumption: A Systematic Review. J. Clin. Hypertens. 2018, 20, 1360–1376. [Google Scholar] [CrossRef]
- McLean, R.M.; Farmer, V.L.; Nettleton, A.; Cameron, C.M.; Cook, N.R.; Campbell, N.R.C. Assessment of Dietary Sodium Intake Using a Food Frequency Questionnaire and 24-Hour Urinary Sodium Excretion: A Systematic Literature Review. J. Clin. Hypertens. 2017, 19, 1214–1230. [Google Scholar] [CrossRef]
- Zaki, N.A.M.; Ambak, R.; Othman, F.; Wong, N.I.; Man, C.S.; Morad, M.F.A.; He, F.J.; MacGregor, G.; Palaniveloo, L.; Baharudin, A. The Prevalence of Hypertension among Malaysian Adults and Its Associated Risk Factors: Data from Malaysian Community Salt Study (MyCoSS). J. Health Popul. Nutr. 2021, 40 (Suppl. S1), 8. [Google Scholar] [CrossRef] [PubMed]
- McGrattan, A.; Mohan, D.; Chua, P.W.; Donnelly, M.; Kee, F. Feasibility and Acceptability of a Dietary Intervention Study to Reduce Salt Intake and Increase High-Nitrate Vegetable Consumption among Middle-Aged and Older Malaysian Adults with Elevated Blood Pressure: A Study Protocol. BMJ Open 2020, 10, e035453. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.S.; McGrattan, A.; Soh, Y.C.; Threapleton, D.; Wang, Y.; O’Reilly, J. Feasibility and Acceptability of a Dietary Intervention to Reduce Salt Intake and Increase High-Nitrate Vegetable Consumption in Malaysian Middle-Aged and Older Adults with Elevated Blood Pressure: Findings from the DePEC-Nutrition Trial. Nutrients 2022, 14, 430. [Google Scholar] [CrossRef] [PubMed]
- Tee, E.S.; Mohd Ismail, N.; Mohd Nasir, A.; Khatijah, I. Nutrient Composition of Malaysian Foods, 4th ed.; Institute for Medical Research: Kuala Lumpur, Malaysia, 1997. [Google Scholar]
- Institute for Public Health (IPH). National Health and Morbidity Survey 2014: Malaysian Adult Nutrition Survey. Volume 1: Methodology and General Findings; IPH: Kuala Lumpur, Malaysia, 2014. [Google Scholar]
- Suzana, S.; Nik Shanita, S.; Zahara, A.M.; Norimah, A.K. Atlas of Food Exchanges & Portion Sizes, 3rd ed.; MDC Publishers: Kuala Lumpur, Malaysia, 2015. [Google Scholar]
- Shahar, S.; Shahril, M.R.; Abdullah, N.; Borhanuddin, B.; Kamaruddin, M.A.; Yusuf, N.A.M.; Dauni, A.; Rosli, H.; Zainuddin, N.S.; Jamal, R. Development and Relative Validity of a Semiquantitative Food Frequency Questionnaire to Estimate Dietary Intake among a Multi-Ethnic Population in the Malaysian Cohort Project. Nutrients 2021, 13, 1163. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.who.int/news-room/fact-sheets/detail/salt-reduction (accessed on 15 October 2023).
- Institute for Public Health (IPH). National Health and Morbidity Survey 2014: Malaysian Adult Nutrition Survey (MANS). Volume II—Survey Findings; MOH/S/IKU/45.15(RR); IPH: Kuala Lumpur, Malaysia, 2014. [Google Scholar]
- Ahmad, M.H.; Othman, F.; Baharudin, A.; Siew Man, C.; Yusuff, M.; Ambak, R.; Mohd Zaki, N.A.; Abdul Aziz, N.; Salleh, R. Sodium Intake in Malaysian Adults: Validation of Estimations by Dietary and Spot Urine Excretion. Int. J. Allied Health 2018, 2, 489–498. [Google Scholar]
- Institute for Public Health (IPH). Population-Based Salt Intake Survey to Support the National Salt Reduction Programme for Malaysia (Malaysian Community Salt Survey—MyCoSS); IPH: Kuala Lumpur, Malaysia, 2019. [Google Scholar]
- Rashidah, A.; Yeo, P.S.; Noor Ani, A.; Muhammad Fadhli, M.Y.; Tahir, A.; Feisul Idzwan, M.; Ahmad Ali, Z.; Suhaila, A.G.; Azli, B.; Viola, M.; et al. Sodium Intake among Normotensive Health Staff Assessed by 24-Hour Urinary Excretion: A Cross-Sectional Study. Malays. J. Nutr. 2014, 20, 317–326. [Google Scholar]
- National Coordinating Committee on Food & Nutrition, Ministry of Health Malaysia. Recommended Nutrient Intake (RNI) for Malaysia 2017: A Report of the Technical Working Group on Nutritional Guidelines; Ministry of Health Malaysia: Putrajaya, Malaysia, 2017. [Google Scholar]
- Tanaka, T.; Okamura, T.; Miura, K.; Kadowaki, T.; Ueshima, H.; Nakamura, Y.; Okayama, A. A Simple Method to Estimate Populational 24-Hour Urinary Sodium and Potassium Excretion Using a Casual Urine Specimen. J. Hum. Hypertens. 2002, 16, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Biltoft-Jensen, A.; Ygil, K.H.; Knudsen, L.; Matthiessen, J.; Fagt, S.; Trolle, E.; Nielsen, T.H.; Hansen, D.M.; Licht, C.L.; Martens, M.; et al. Validation of the 2 × 24 h Recall Method and a 7-d Web-Based Food Diary against Doubly Labelled Water in Danish Adults. Br. J. Nutr. 2023, 130, 1444–1457. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total (n = 65) | Men (n = 27) | Women (n = 38) | p-Value * |
|---|---|---|---|---|
| Age, years | 61.0 (11.0) | 61.0 (10.0) | 61.5 (13.0) | 0.627 |
| Ethnicity, n (%) | 0.647 | |||
| Malay | 43 (66.2) | 17 (63.0) | 26 (68.4) | |
| Chinese | 22 (33.8) | 10 (37.0) | 12 (31.6) | |
| Educational attainment, n (%) | 0.468 | |||
| No formal education | 6 (9.2) | 1 (3.7) | 5 (13.2) | |
| Primary | 22 (33.8) | 8 (29.6) | 14 (36.8) | |
| Secondary | 35 (53.8) | 17 (63.0) | 18 (47.4) | |
| Tertiary | 2 (3.1) | 1 (3.7) | 1 (2.6) | |
| Hypertension a status, n (%) | 0.474 | |||
| Prehypertensive | 25 (38.5) | 12 (44.4) | 13 (34.2) | |
| Hypertensive with medication | 17 (26.2) | 5 (18.5) | 12 (31.6) | |
| Hypertensive without medication | 23 (35.4) | 10 (37.0) | 13 (34.2) | |
| Blood pressure, mmHg | ||||
| Median systolic | 136.0 (24.0) | 139.0 (33.0) | 136.0 (20.0) | 0.754 |
| Median diastolic | 80.0 (13.0) | 79.0 (15.0) | 80.5 (11.0) | 0.917 |
| BMI b, kg/m2 | 26.5 (6.7) | 24.5 (6.2) | 27.4 (6.1) | 0.042 |
| Normal, n (%) | 11 (16.9) | 8 (29.6) | 3 (7.9) | 0.041 |
| Overweight, n (%) | 54 (83.1) | 19 (70.4) | 35 (92.1) | |
| Waist circumference, cm | 90.5 (12.9) | 91.5 (10.5) | 89.6 (13.6) | 0.543 |
| Central obesity c, n (%) | 50 (76.9) | 16 (59.3) | 34 (89.5) | 0.004 |
| Diabetes d, n (%) | 7 (10.8) | 2 (7.4) | 5 (13.2) | 0.690 |
| Current smoker, n (%) | 10 (15.4) | 9 (33.3) | 1 (2.6) | 0.001 |
| Alcohol user, n (%) | 5 (7.7) | 3 (11.1) | 2 (5.3) | 0.642 |
| MMSE e score | 26 (4) | 26 (4) | 26 (4) | 0.564 |
| Normal, n (%) | 62 (95.4) | 25 (92.6) | 37 (97.4) | 0.565 |
| Cognitive impaired, n (%) | 3 (4.6) | 2 (7.4) | 1 (2.6) | |
| Physical activity f | ||||
| MET-mins/week | 2320 (4560) | 3600 (5880) | 1820 (3120) | 0.543 |
| Low | 17 (26.2) | 6 (22.2) | 11 (28.9) | 0.319 |
| Moderate | 19 (29.2) | 6 (22.2) | 13 (34.2) | |
| High | 29 (44.6) | 15 (55.6) | 14 (36.8) |
| Variable | Total (n = 65) | Men (n = 27) | Women (n = 38) | p-Value * |
|---|---|---|---|---|
| Urinary biochemistry | ||||
| Volume, mL | 1386.2 (1257.8) | 1589.7 (1493.1) | 1269.6 (1079.2) | 0.543 |
| Duration of collection, h | 24.0 (1.0) | 24.0 (1.1) | 24.4 (1.6) | 0.045 |
| Sodium excretion, mg/day | 2615.5 (2182.4) | 2477.4 (1910.7) | 2659.3 (2410.4) | 0.917 |
| Creatinine concentration, mmol/day | 6.3 (5.6) | 10.2 (9.9) | 5.8 (3.0) | 0.034 |
| Dietary salt intake | ||||
| Salt intake a, g/day | 6.6 (5.5) | 6.3 (4.9) | 6.8 (6.1) | 0.917 |
| Met WHO’s recommendation of <5 g/day salt intake, n (%) | 20 (30.8) | 7 (25.9) | 13 (34.2) | 0.476 |
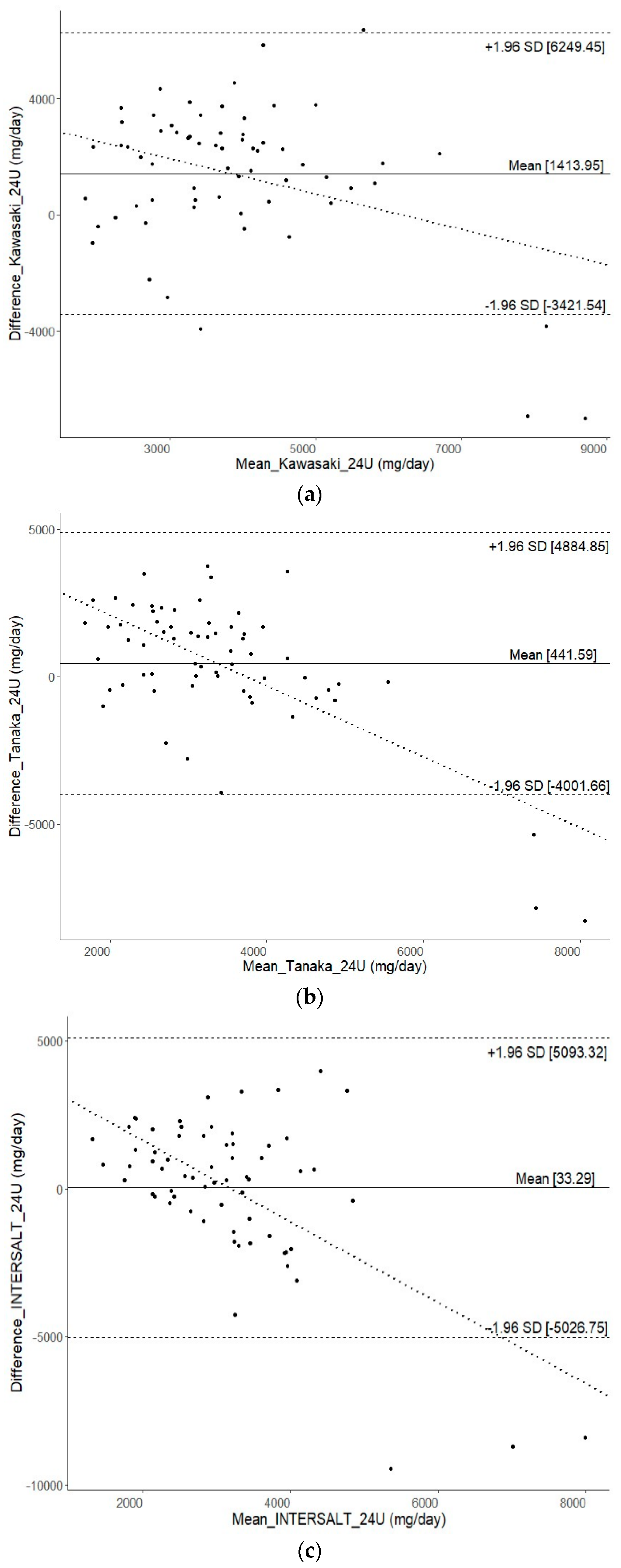
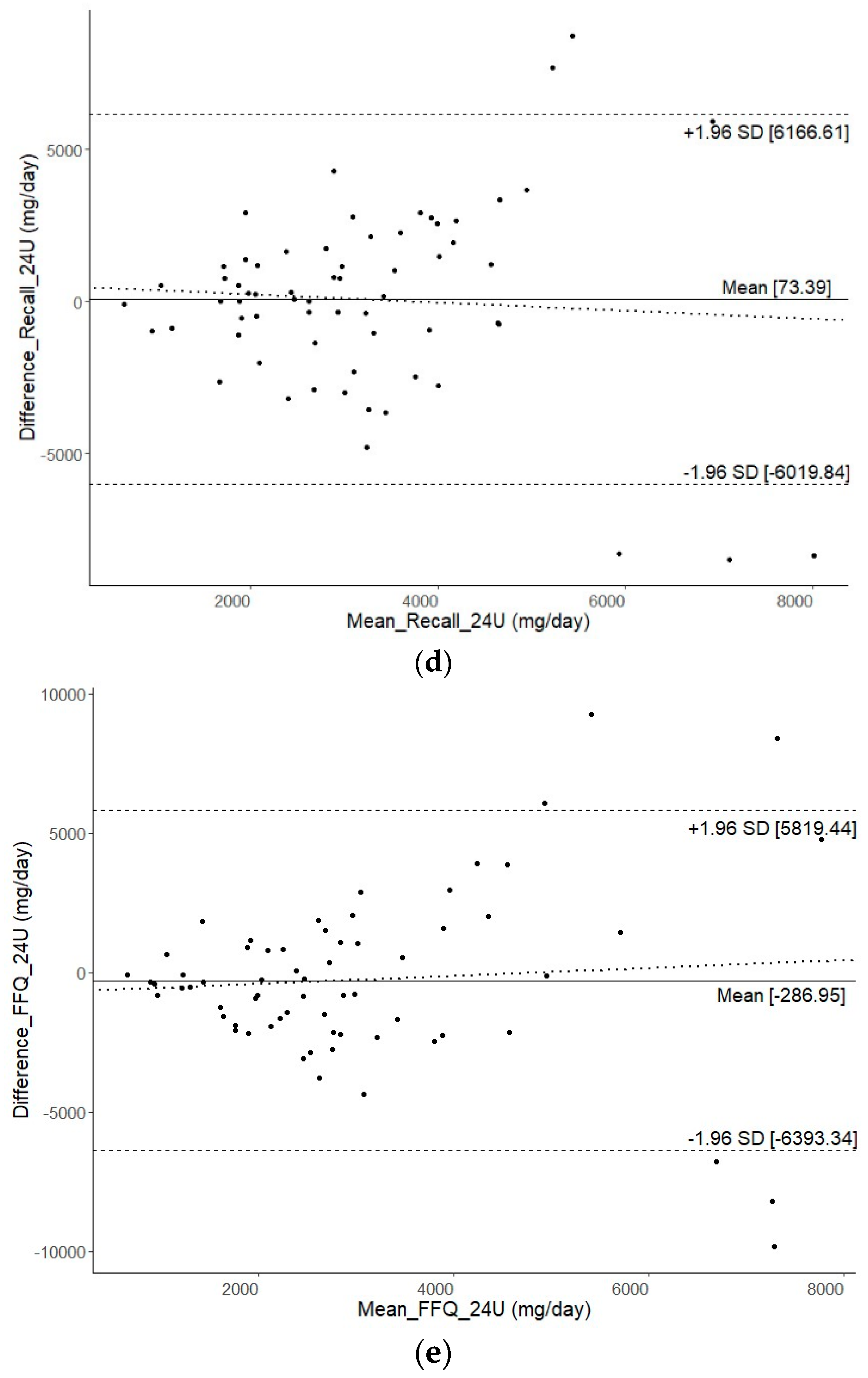
| Method | * Mean Difference (mg/Day) (95% CI) | SCC | ICC (95% CI) |
|---|---|---|---|
| 24-h urine (reference) | Reference | Reference | Reference |
| Spot urine (Kawasaki equation) | ** 1414.0 (802.6 to 2025.3) | 0.24 | 0.12 (−0.08 to 0.32) |
| Spot urine (Tanaka equation) | 441.6 (−120.1 to 1003.3) | 0.23 | 0.11 (−0.13 to 0.34) |
| Spot urine (INTERSALT equation) | 33.3 (−606.4 to 673.0) | −0.03 | −0.11 (−0.35 to 0.14) |
| 1-day 24-h dietary recall | 73.4 (−696.9 to 843.7) | 0.01 | −0.06 (−0.31 to 0.19) |
| Food Frequency Questionnaire | −287.0 (−1058.9 to 485.0) | 0.20 | 0.07 (−0.17 to 0.31) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soh, Y.C.; Fairley, A.; Alawad, M.; Lee, S.S.; Su, T.T.; Stephan, B.C.M.; Reidpath, D.; Robinson, L.; Yasin, S.; Siervo, M.; et al. Assessing Sodium Intake in Middle-Aged and Older Adults with Elevated Blood Pressure: Validation of Spot Urine Excretion and Dietary Survey-Derived Estimates. Nutrients 2024, 16, 1461. https://doi.org/10.3390/nu16101461
Soh YC, Fairley A, Alawad M, Lee SS, Su TT, Stephan BCM, Reidpath D, Robinson L, Yasin S, Siervo M, et al. Assessing Sodium Intake in Middle-Aged and Older Adults with Elevated Blood Pressure: Validation of Spot Urine Excretion and Dietary Survey-Derived Estimates. Nutrients. 2024; 16(10):1461. https://doi.org/10.3390/nu16101461
Chicago/Turabian StyleSoh, Yee Chang, Andrea Fairley, Mawada Alawad, Siew Siew Lee, Tin Tin Su, Blossom Christa Maree Stephan, Daniel Reidpath, Louise Robinson, Shajahan Yasin, Mario Siervo, and et al. 2024. "Assessing Sodium Intake in Middle-Aged and Older Adults with Elevated Blood Pressure: Validation of Spot Urine Excretion and Dietary Survey-Derived Estimates" Nutrients 16, no. 10: 1461. https://doi.org/10.3390/nu16101461
APA StyleSoh, Y. C., Fairley, A., Alawad, M., Lee, S. S., Su, T. T., Stephan, B. C. M., Reidpath, D., Robinson, L., Yasin, S., Siervo, M., & Mohan, D. (2024). Assessing Sodium Intake in Middle-Aged and Older Adults with Elevated Blood Pressure: Validation of Spot Urine Excretion and Dietary Survey-Derived Estimates. Nutrients, 16(10), 1461. https://doi.org/10.3390/nu16101461








