Individualized Supplementation of Immunoactive Micronutrients and Severity of Upper Respiratory Infection Symptoms—A Randomized Intervention Study
Abstract
1. Introduction
2. Materials and Methods
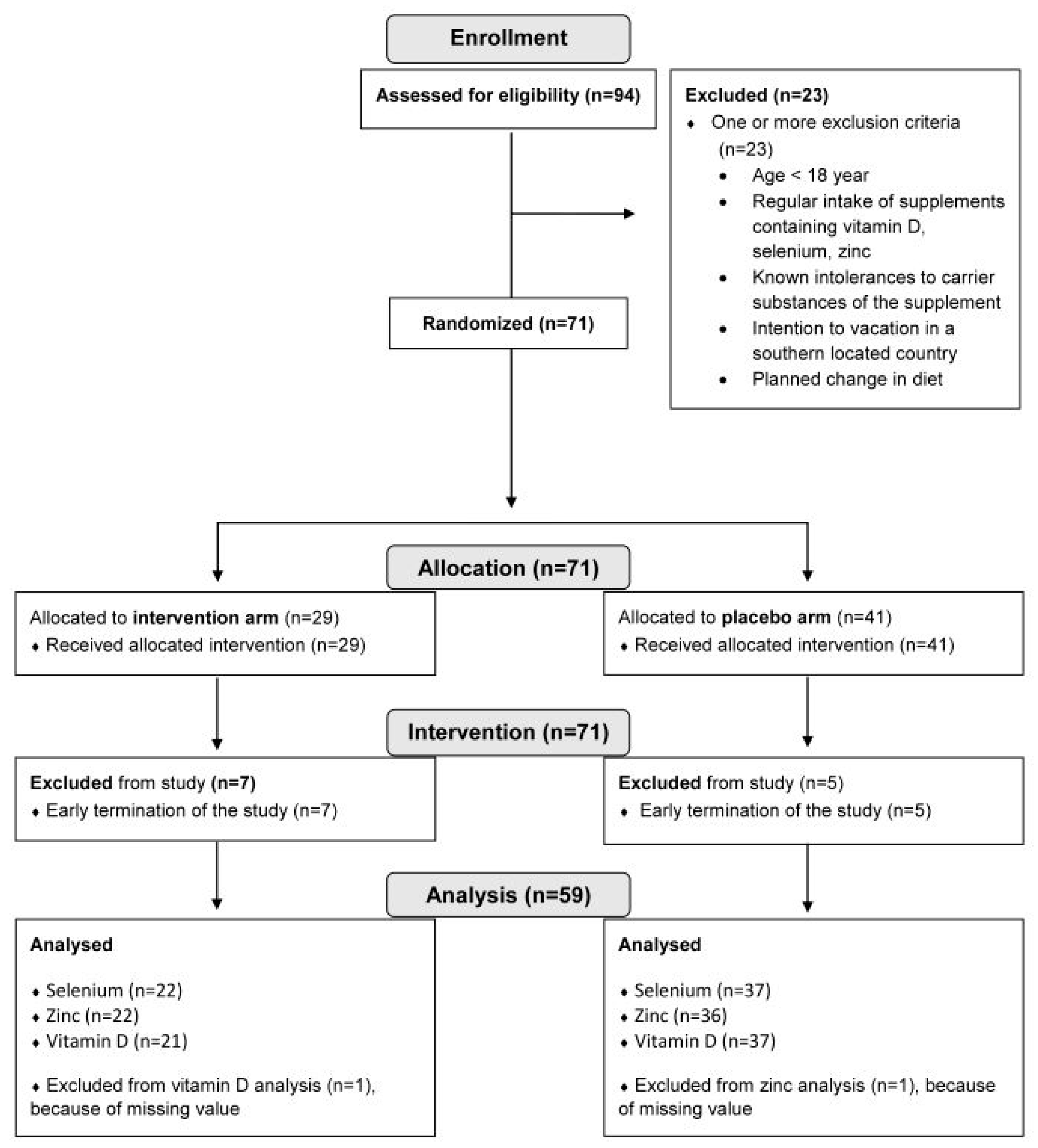
2.1. Study Participants
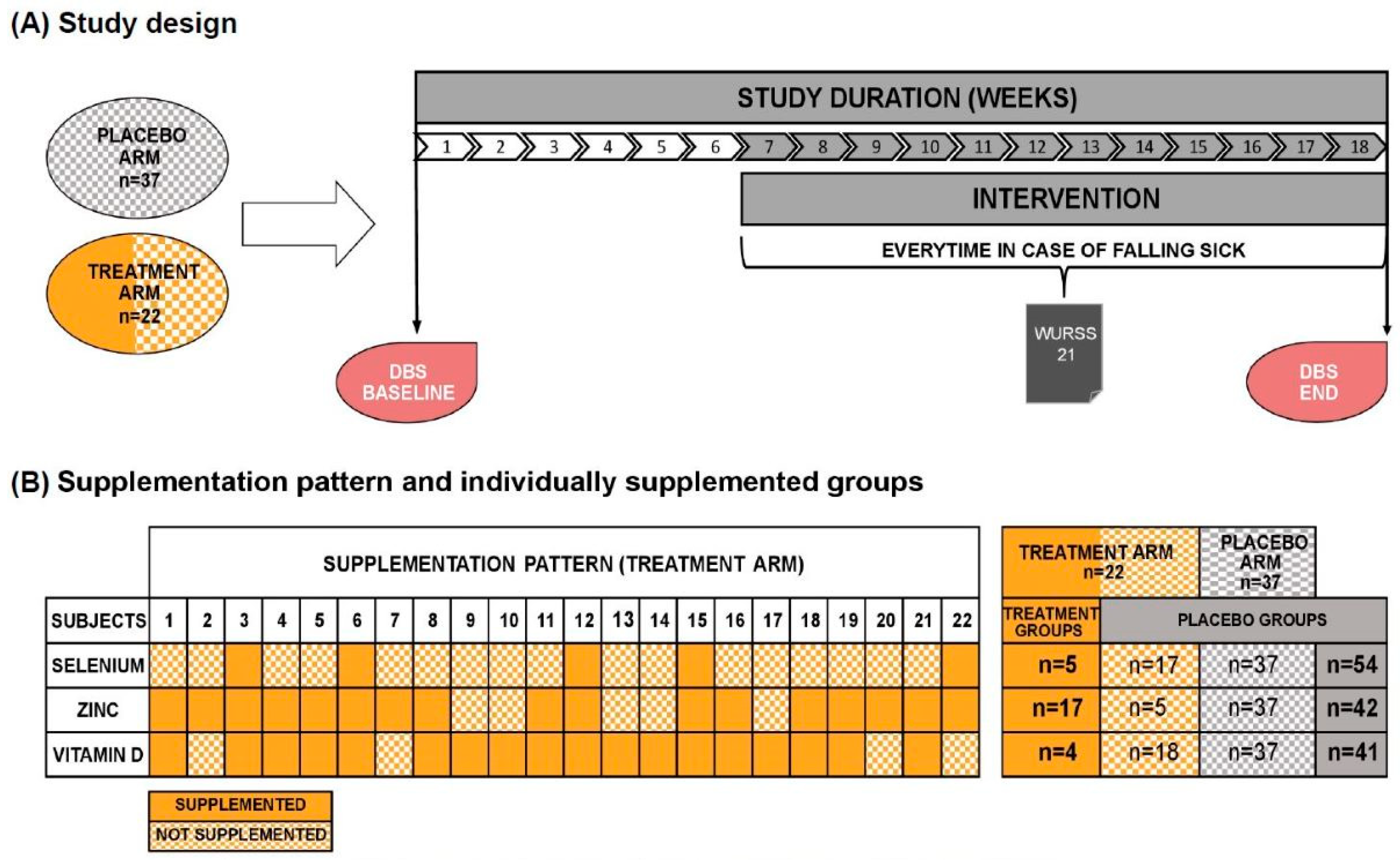
2.2. Study Design
2.3. Dried Blood Spot Analysis
2.4. Study Product
2.5. The Wisconsin Upper Respiratory Symptom Survey
2.6. Data Analysis and Statistics
3. Results
3.1. Participant Characteristics
3.2. Effect of Personalized Supplementation on the Micronutrient Status
3.3. Individual Supplementation with Micronutrients Does Not Reduce Frequency or Moderate Severity of URI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Albers, R.; Bourdet-Sicard, R.; Braun, D.; Calder, P.C.; Herz, U.; Lambert, C.; Lenoir-Wijnkoop, I.; Méheust, A.; Ouwehand, A.; Phothirath, P.; et al. Monitoring immune modulation by nutrition in the general population: Identifying and substantiating effects on human health. Br. J. Nutr. 2013, 110 (Suppl. S2), S1–S30. [Google Scholar] [CrossRef] [PubMed]
- Gombart, A.F.; Pierre, A.; Maggini, S. A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection. Nutrients 2020, 12, 236. [Google Scholar] [CrossRef]
- Pecora, F.; Persico, F.; Argentiero, A.; Neglia, C.; Esposito, S. The Role of Micronutrients in Support of the Immune Response against Viral Infections. Nutrients 2020, 12, 3198. [Google Scholar] [CrossRef] [PubMed]
- Galmés, S.; Serra, F.; Palou, A. Current State of Evidence: Influence of Nutritional and Nutrigenetic Factors on Immunity in the COVID-19 Pandemic Framework. Nutrients 2020, 12, 2738. [Google Scholar] [CrossRef] [PubMed]
- Vlieg-Boerstra, B.; de Jong, N.; Meyer, R.; Agostoni, C.; de Cosmi, V.; Grimshaw, K.; Milani, G.P.; Muraro, A.; Oude Elberink, H.; Pali-Schöll, I.; et al. Nutrient supplementation for prevention of viral respiratory tract infections in healthy subjects: A systematic review and meta-analysis. Allergy 2022, 77, 1373–1388. [Google Scholar] [CrossRef] [PubMed]
- Commission Regulation (EU) No 432/2012 of 16 May 2012 Establishing a List of Permitted Health Claims Made on Foods, Other than Those Referring to the Reduction of Disease Risk and to Children’s Development and Health: Regulation (EU) No 432/2012. Available online: https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2012:136:0001:0040:en:PDF (accessed on 1 May 2024).
- Laird, E.; Rhodes, J.; Kenny, R.A. Vitamin D and Inflammation: Potential Implications for Severity of COVID-19. Ir. Med. J. 2020, 113, 81. [Google Scholar]
- Girodon, F.; Galan, P.; Monget, A.L.; Boutron-Ruault, M.C.; Brunet-Lecomte, P.; Preziosi, P.; Arnaud, J.; Manuguerra, J.C.; Herchberg, S. Impact of trace elements and vitamin supplementation on immunity and infections in institutionalized elderly patients: A randomized controlled trial. MIN. VIT. AOX. geriatric network. Arch. Intern. Med. 1999, 159, 748–754. [Google Scholar] [CrossRef] [PubMed]
- Veverka, D.V.; Wilson, C.; Martinez, M.A.; Wenger, R.; Tamosuinas, A. Use of zinc supplements to reduce upper respiratory infections in United States Air Force Academy cadets. Complement. Ther. Clin. Pract. 2009, 15, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Ivory, K.; Prieto, E.; Spinks, C.; Armah, C.N.; Goldson, A.J.; Dainty, J.R.; Nicoletti, C. Selenium supplementation has beneficial and detrimental effects on immunity to influenza vaccine in older adults. Clin. Nutr. 2017, 36, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Broome, C.S.; McArdle, F.; Kyle, J.A.; Andrews, F.; Lowe, N.M.; Hart, C.A.; Arthur, J.R.; Jackson, M.J. An increase in selenium intake improves immune function and poliovirus handling in adults with marginal selenium status. Am. J. Clin. Nutr. 2004, 80, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Martineau, A.R.; Jolliffe, D.A.; Hooper, R.L.; Greenberg, L.; Aloia, J.F.; Bergman, P.; Dubnov-Raz, G.; Esposito, S.; Ganmaa, D.; Ginde, A.A.; et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ 2017, 356, i6583. [Google Scholar] [CrossRef]
- Hunter, J.; Arentz, S.; Goldenberg, J.; Yang, G.; Beardsley, J.; Myers, S.P.; Mertz, D.; Leeder, S. Zinc for the prevention or treatment of acute viral respiratory tract infections in adults: A rapid systematic review and meta-analysis of randomised controlled trials. BMJ Open 2021, 11, e047474. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, B.; El Abd, A.; Ducharme, F.M. Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis. Nutrients 2022, 14, 2134. [Google Scholar] [CrossRef] [PubMed]
- Denlinger, L.C.; King, T.S.; Cardet, J.C.; Craig, T.; Holguin, F.; Jackson, D.J.; Kraft, M.; Peters, S.P.; Ross, K.; Sumino, K.; et al. Vitamin D Supplementation and the Risk of Colds in Patients with Asthma. Am. J. Respir. Crit. Care Med. 2016, 193, 634–641. [Google Scholar] [CrossRef] [PubMed]
- Dubnov-Raz, G.; Rinat, B.; Hemilä, H.; Choleva, L.; Cohen, A.H.; Constantini, N.W. Vitamin D supplementation and upper respiratory tract infections in adolescent swimmers: A randomized controlled trial. Pediatr. Exerc. Sci. 2015, 27, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Vitamin D: Importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am. J. Clin. Nutr. 2004, 79, 362–371. [Google Scholar] [CrossRef]
- Gammoh, N.Z.; Rink, L. Zinc in Infection and Inflammation. Nutrients 2017, 9, 624. [Google Scholar] [CrossRef] [PubMed]
- Maares, M.; Haase, H. Zinc and immunity: An essential interrelation. Arch. Biochem. Biophys. 2016, 611, 58–65. [Google Scholar] [CrossRef]
- Shankar, A.H.; Prasad, A.S. Zinc and immune function: The biological basis of altered resistance to infection. Am. J. Clin. Nutr. 1998, 68, 447S–463S. [Google Scholar] [CrossRef]
- Filippini, T.; Fairweather-Tait, S.; Vinceti, M. Selenium and immune function: A systematic review and meta-analysis of experimental human studies. Am. J. Clin. Nutr. 2023, 117, 93–110. [Google Scholar] [CrossRef] [PubMed]
- Rayman, M.P. The importance of selenium to human health. Lancet 2000, 356, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Li-Ng, M.; Aloia, J.F.; Pollack, S.; Cunha, B.A.; Mikhail, M.; Yeh, J.; Berbari, N. A randomized controlled trial of vitamin D3 supplementation for the prevention of symptomatic upper respiratory tract infections. Epidemiol. Infect. 2009, 137, 1396–1404. [Google Scholar] [CrossRef] [PubMed]
- Murdoch, D.R.; Slow, S.; Chambers, S.T.; Jennings, L.C.; Stewart, A.W.; Priest, P.C.; Florkowski, C.M.; Livesey, J.H.; Camargo, C.A.; Scragg, R. Effect of vitamin D3 supplementation on upper respiratory tract infections in healthy adults: The VIDARIS randomized controlled trial. JAMA 2012, 308, 1333–1339. [Google Scholar] [CrossRef] [PubMed]
- Pae, M.; Wu, D. Nutritional modulation of age-related changes in the immune system and risk of infection. Nutr. Res. 2017, 41, 14–35. [Google Scholar] [CrossRef]
- Barrett, B.; Brown, R.; Mundt, M.; Safdar, N.; Dye, L.; Maberry, R.; Alt, J. The Wisconsin Upper Respiratory Symptom Survey is responsive, reliable, and valid. J. Clin. Epidemiol. 2005, 58, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Barrett, B.; Brown, R.L.; Mundt, M.P.; Thomas, G.R.; Barlow, S.K.; Highstrom, A.D.; Bahrainian, M. Validation of a short form Wisconsin Upper Respiratory Symptom Survey (WURSS-21). Health Qual. Life Outcomes 2009, 7, 76. [Google Scholar] [CrossRef] [PubMed]
- Bresson, J.-L.; Burlingame, B.; Dean, T.; Fairweather-Tait, S.; Heinonen, M.; Hirsch-Ernst, K.-I.; Mangelsdorf, I.; McArdle, H.; Naska, A.; Neuhäuser-Berthold, M.; et al. Scientific Opinion on Dietary Reference Values for vitamin D. EFSA J. 2016, 14, e04547. [Google Scholar] [CrossRef]
- Agostoni, C.; Canani, R.B.; Fairweather-Tait, S.; Heinonen, M.; Korhonen, H.; La Vieille, S.; Marchelli, R.; Martin, A.; Naska, A.; Neuhäuser-Berthold, M.; et al. Scientific Opinion on Dietary Reference Values for selenium. EFSA J. 2014, 12, 3846. [Google Scholar] [CrossRef]
- Agostoni, C.; Canani, R.B.; Fairweather-Tait, S.; Heinonen, M.; Korhonen, H.; La Vieille, S.; Marchelli, R.; Martin, A.; Naska, A.; Neuhäuser-Berthold, M.; et al. Scientific Opinion on Dietary Reference Values for zinc. EFSA J. 2014, 12, 3844. [Google Scholar] [CrossRef]
- Jolliffe, D.A.; Camargo, C.A.; Sluyter, J.D.; Aglipay, M.; Aloia, J.F.; Ganmaa, D.; Bergman, P.; Bischoff-Ferrari, H.A.; Borzutzky, A.; Damsgaard, C.T.; et al. Vitamin D supplementation to prevent acute respiratory infections: A systematic review and meta-analysis of aggregate data from randomised controlled trials. Lancet Diabetes Endocrinol. 2021, 9, 276–292. [Google Scholar] [CrossRef] [PubMed]
- BourBour, F.; Mirzaei Dahka, S.; Gholamalizadeh, M.; Akbari, M.E.; Shadnoush, M.; Haghighi, M.; Taghvaye-Masoumi, H.; Ashoori, N.; Doaei, S. Nutrients in prevention, treatment, and management of viral infections; special focus on Coronavirus. Arch. Physiol. Biochem. 2023, 129, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Jolliffe, D.A.; Griffiths, C.J.; Martineau, A.R. Vitamin D in the prevention of acute respiratory infection: Systematic review of clinical studies. J. Steroid Biochem. Mol. Biol. 2013, 136, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Pal, R.; Banerjee, M.; Bhadada, S.K.; Shetty, A.J.; Singh, B.; Vyas, A. Vitamin D supplementation and clinical outcomes in COVID-19: A systematic review and meta-analysis. J. Endocrinol. Investig. 2022, 45, 53–68. [Google Scholar] [CrossRef] [PubMed]

| Treatment Arm | Placebo Arm | Overall | |
|---|---|---|---|
| N 1 | 22 | 37 | 59 |
| Sex (f/m), n | 19/3 | 7/30 | 49/10 |
| Age 2, years | 26 ± 6 | 32 ± 13 | 30 ± 11 |
| BMI, kg/m2 | 22.5 ± 3.8 | 22.8 ± 2.9 | 22.7 ± 3.3 |
| Individually supplemented groups 3 | Treatment group | Placebo group(untreated treatment arm + placebo arm) | Overall |
| Selenium, n | 5 | 17 + 37 | 59 |
| Zinc, n | 17 | 5 + 37 | 59 |
| Vitamin D, n | 18 | 4 + 37 | 59 |
| Baseline 1 | End | Change (%) | |
|---|---|---|---|
| A: Selenium | [µg/mL] | [µg/mL] | |
| Placebo group (n = 54) | 0.171 ± 0.036 | 0.152 ± 0.046 | −6.03 ± 36.95 |
| Treatment group (n = 5) | 0.125 ± 0.009 | 0.147 ± 0.028 | 17.65 ± 16.32 |
| p-value 2 | 0.002 | 0.660 | 0.048 |
| B: Zinc | [µg/mL] | [µg/mL] | |
| Placebo group (n = 42) | 6.53 ± 1.86 | 6.05 ± 2.15 | −3.48 ± 36.75 |
| Treatment group (n = 17) | 5.34 ± 0.81 | 5.61 ± 1.16 | 6.90 ± 24.93 |
| p-value | 0.024 | 0.946 | 0.069 |
| C: Vitamin D | [nmol/L] | [nmol/L] | |
| Placebo group (n = 41) | 93.89 ± 38.16 | 93.89 ± 30.59 | 15.16 ± 58.17 |
| Treatment group (n = 17) | 70.46 ± 15.25 | 88.40 ± 27.61 | 31.45 ± 53.58 |
| p-value | 0.017 | 0.628 | 0.144 |
| Placebo | Treatment | |||||
|---|---|---|---|---|---|---|
| n of Falling Sick | WURSSmax 1 | n of Falling Sick | WURSSmax | p-Value 2 | ||
| Study Arms | 7 | 28.57 ± 11.84 | 9 | 43.11 ± 13.45 | 0.045 | |
| Individually supplemented groups | Selenium | 14 | 36.71 ± 14.64 | 2 | 37.00 ± 18.38 | ns |
| Zinc | 9 | 31.00 ± 12.70 | 7 | 44.14 ± 13.84 | ns | |
| Vitamin D | 8 | 33.37 ± 17.46 | 8 | 40.13 ± 10.72 | ns | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haas, M.; Brandl, B.; Schinhammer, L.; Skurk, T. Individualized Supplementation of Immunoactive Micronutrients and Severity of Upper Respiratory Infection Symptoms—A Randomized Intervention Study. Nutrients 2024, 16, 1400. https://doi.org/10.3390/nu16101400
Haas M, Brandl B, Schinhammer L, Skurk T. Individualized Supplementation of Immunoactive Micronutrients and Severity of Upper Respiratory Infection Symptoms—A Randomized Intervention Study. Nutrients. 2024; 16(10):1400. https://doi.org/10.3390/nu16101400
Chicago/Turabian StyleHaas, Melanie, Beate Brandl, Laura Schinhammer, and Thomas Skurk. 2024. "Individualized Supplementation of Immunoactive Micronutrients and Severity of Upper Respiratory Infection Symptoms—A Randomized Intervention Study" Nutrients 16, no. 10: 1400. https://doi.org/10.3390/nu16101400
APA StyleHaas, M., Brandl, B., Schinhammer, L., & Skurk, T. (2024). Individualized Supplementation of Immunoactive Micronutrients and Severity of Upper Respiratory Infection Symptoms—A Randomized Intervention Study. Nutrients, 16(10), 1400. https://doi.org/10.3390/nu16101400







