Abstract
Background: Numerous observational studies have documented an association between the circadian rhythm and the composition of the gut microbiota. However, the bidirectional causal effect of the morning chronotype on the gut microbiota is unknown. Methods: A two-sample Mendelian randomization study was performed, using the summary statistics of the morning chronotype from the European Consortium and those of the gut microbiota from the largest available genome-wide association study meta-analysis, conducted by the MiBioGen consortium. The inverse variance-weighted (IVW), weighted mode, weighted median, MR-Egger regression, and simple mode methods were used to examine the causal association between the morning chronotype and the gut microbiota. A reverse Mendelian randomization analysis was conducted on the gut microbiota, which was identified as causally linked to the morning chronotype in the initial Mendelian randomization analysis. Cochran’s Q statistics were employed to assess the heterogeneity of the instrumental variables. Results: Inverse variance-weighted estimates suggested that the morning chronotype had a protective effect on Family Bacteroidaceae (β = −0.072; 95% CI: −0.143, −0.001; p = 0.047), Genus Parabacteroides (β = −0.112; 95% CI: −0.184, −0.039; p = 0.002), and Genus Bacteroides (β = −0.072; 95% CI: −0.143, −0.001; p = 0.047). In addition, the gut microbiota (Family Bacteroidaceae (OR = 0.925; 95% CI: 0.857, 0.999; p = 0.047), Genus Parabacteroides (OR = 0.915; 95% CI: 0.858, 0.975; p = 0.007), and Genus Bacteroides (OR = 0.925; 95% CI: 0.857, 0.999; p = 0.047)) demonstrated positive effects on the morning chronotype. No significant heterogeneity in the instrumental variables, or in horizontal pleiotropy, was found. Conclusion: This two-sample Mendelian randomization study found that Family Bacteroidaceae, Genus Parabacteroides, and Genus Bacteroides were causally associated with the morning chronotype. Further randomized controlled trials are needed to clarify the effects of the gut microbiota on the morning chronotype, as well as their specific protective mechanisms.
1. Introduction
The morning chronotype, characterized by a natural inclination to wake up and be active in the early hours of the day, is a fundamental aspect of human chronobiology [1]. It represents an individual’s preference for being more active and alert during specific times of the day, with morning chronotype individuals favoring the early hours [2]. This preference is governed by the circadian clock, a complex system that regulates the body’s internal processes over a 24 h cycle [3,4]. Morning chronotype individuals often experience a natural synchrony with the external environment, as their peak performance aligns with typical daytime activities [5,6]. Their unique chronotype predisposes them to various circadian-related traits and behaviors that can profoundly affect their overall health and well-being [7,8]. There is compelling evidence suggesting a connection between disruptions in the circadian rhythm and the onset of diseases, with a notable focus on metabolic and psychiatric disorders [9,10]. Recent research underscores the intricate and compelling connection between an individual’s mood and their chronotype, suggesting that our daily rhythms not only influence our sleep–wake patterns, but also play pivotal roles in shaping our emotional well-being and mental states [11,12,13].
The human gut microbiome is a crucial factor in both the maintenance of health and the emergence of diseases in humans [14]. At the same time, the gut microbiota, comprising trillions of microorganisms residing in the digestive system, has been recognized for its profound implications in various aspects of human health [15,16,17]. Recent studies have linked alterations in the composition of the gut microbiota with the onset and progression of several diseases [18,19]. Circadian rhythms manifest in nearly every organism, governing various aspects of biological and physiological processes. There exists a bidirectional circadian interaction between the host and its gut microbiota, and potential circadian orchestration of both the host and its gut microbiota in response to invading pathogens [20]. Disruptions to the circadian system can lead to alterations in the composition of microbiome communities, consequently impacting the host’s metabolism, energy regulation, and inflammatory pathways, and thus play a role in the development of metabolic syndrome. Previous research has shown that two SCFA-produced genera, Lachnospiraceae UCG004 and Odoribacter, promote extended sleep duration, while the order Selenomonadales and the class Negativicutes are associated with insomnia risk [21].
Mendelian randomization (MR) leverages genetic variants to create instrumental variables for assessing the causal link between exposure to and the outcome of a disease [22]. MR has been extensively utilized to investigate the causal links between the gut microbiota and various diseases, encompassing both metabolic and autoimmune conditions [23,24]. An association between the gut microbiota and the sleep phenotype was found in a recent Mendelian randomization study, but no inverse relationship was demonstrated [21]. Thus, understanding the relationship between the morning chronotype and the gut microbiota represents a burgeoning field of research that holds the significant potential to advance our knowledge of human biology and health. Our primary objective was to initiate an MR study through which to confirm the causal influence of the gut microbiota taxa on the morning chronotype, and examined the potential bidirectional nature of this causal effect.
2. Materials and Methods
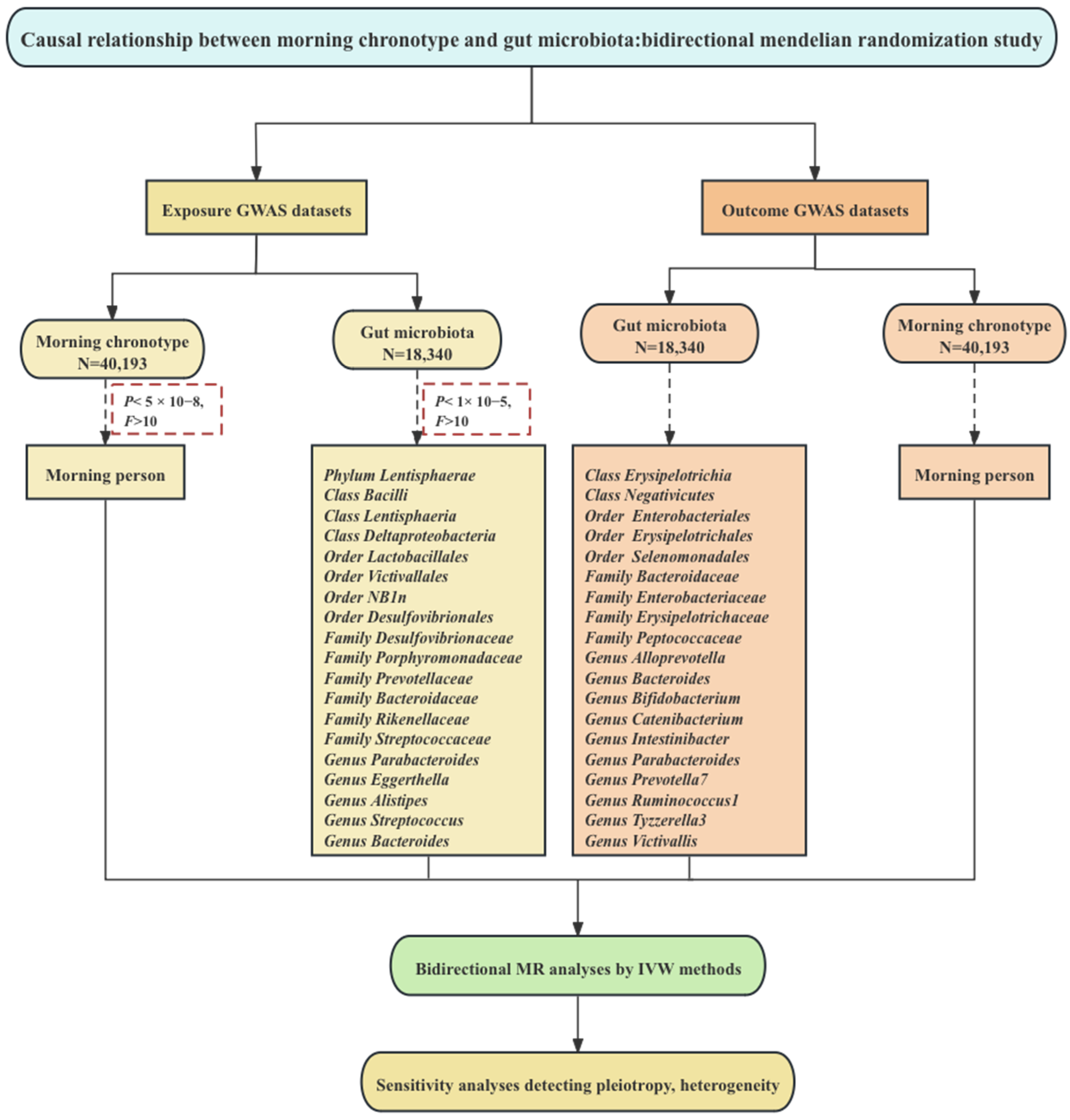
We obtained de-identified summary-level data from publicly accessible GWAS studies. The dataset focusing on the morning chronotype was derived from a collaboration within the European Consortium [25], which ensured a comprehensive representation of this particular trait. Simultaneously, the dataset encompassing information about the gut microbiota was obtained from a GWAS study conducted under the aegis of the international MiBioGen consortium initiative [26,27], reflecting a global perspective on this intricate field of research. It is important to emphasize that ethical and regulatory guidelines were rigorously upheld throughout this data collection endeavor. Each cohort contributing to the GWAS studies diligently obtained ethical approval and consent from their respective participants, reinforcing the ethical integrity of the research process. Our two-sample MR investigation was conducted following the framework illustrated in Figure 1.
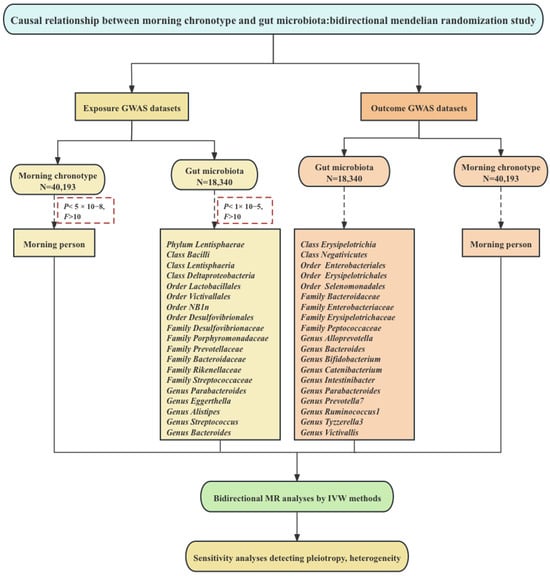
Figure 1.
Study design and framework. Note: Mendelian randomization necessitates the use of valid genetic instrumental variables that adhere to three essential assumptions. These include Assumption 1, which implies that genetic variants should predict exposure; Assumption 2, requiring that genetic variants remain independent of confounding factors; and Assumption 3, which asserts that genetic variants influence the outcome exclusively through exposure, rather than through alternative pathways.
2.1. The Morning Chronotype
To facilitate our analysis of genome-wide significant variants, we implemented a binary phenotype utilizing the same data field as that employed in the chronotype study. In this classification, we categorized participants based on their self-reported chronotype preferences [25]. Those who expressed a clear inclination towards being “Definitely an ‘evening’ person” or identified as “More of an ‘evening’ than ‘morning’ person” were grouped as controls. On the contrary, individuals who firmly characterized themselves as “Definitely a ‘morning’ person” or leaned towards “More of a ‘morning’ than ‘evening’ person” were classified as cases. Participants who provided responses such as “Do not know” or “Prefer not to answer” were considered as missing data, ensuring a comprehensive and robust analysis. This binary classification strategy encompassed a substantial cohort of 403,195 participants participating in the GWAS. Within this cohort, there were 252,287 cases and 150,908 controls, contributing to the depth and reliability of our investigation.
2.2. Gut Microbiota
Genetic instruments for gut microbiota were derived from a comprehensive association study encompassing 24 cohorts, consisting of 18,340 participants [26]. The studies with these cohorts were conducted in various countries, including the USA, Canada, Israel, Republic of Korea, Germany, Denmark, The Netherlands, Belgium, Sweden, Finland, and the UK. Out of the 24 cohorts, the majority focused on individuals of single ancestry, primarily those of European descent (16 cohorts, n = 13,266). Notably, 17 of the 24 cohorts (n = 13,804) had participants with mean ages ranging from 50 to 62 years. In the quantitative microbiome trait loci (mbQTL) mapping analysis for each cohort, only taxa that appeared in more than 10% of the samples were considered, resulting in a dataset comprising 211 taxa (131 genera, 35 families, 20 orders, 16 classes, and 9 phyla). Meanwhile, the binary trait loci mapping (mbBTL) analysis included taxa that appeared in a percentage range of 10% to 90% in the included samples. It is worth noting that all of the included cohorts incorporated adjustments for covariates related to sex and age in their calculations. The summary-level statistics from this association study are publicly accessible on the www.mibiogen.org website.
2.3. Genetic Instrument Selection
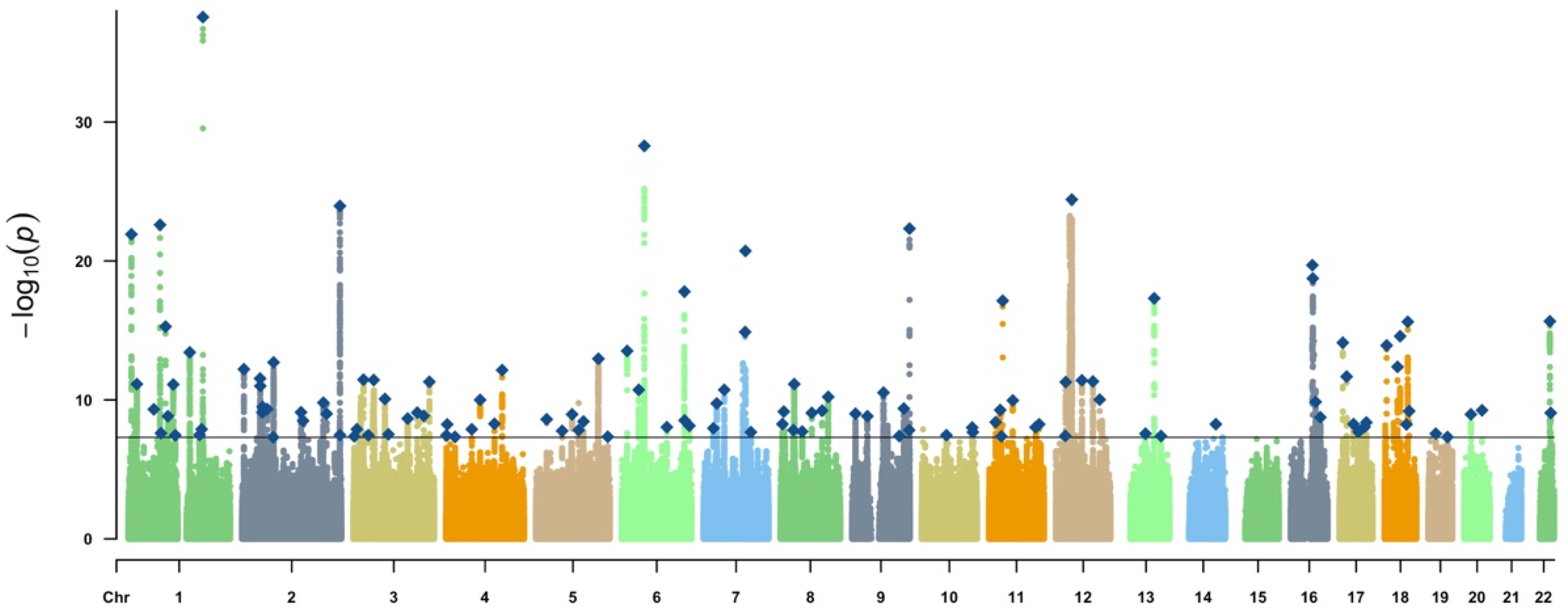
Single-nucleotide polymorphisms (SNPs) associated with the morning chronotype at the genome-wide significance level (p < 5 × 10−8) were extracted from the European ancestries of 403,195 individuals (Figure 2).

Figure 2.
Manhattan plot depicting the morning chronotype. Note: chr, chromosome; The solid gray line indicates the typical genome-wide significance threshold of p = 5 × 10−8 identified through permutation testing. Lead variants are annotated with a diamond.
In order to ensure the credibility and precision of our conclusions regarding the causal connection between the gut microbiome and the morning chronotype, a series of rigorous quality control measures were implemented to curate the most suitable instrumental variables (IVs) [28]. Initially, SNPs that exhibited significant relationships with the gut microbiome were chosen as IVs. Two distinct thresholds were applied in this selection process. The first threshold involved the identification of SNPs with statistical significance levels below the genome-wide threshold (p < 5 × 10−8) to serve as IVs. Unfortunately, this initial threshold yielded only a limited number of gut microbiota-related IVs. To explore a more comprehensive spectrum of potential causal associations between the morning chronotype and the gut microbiota, a second threshold was introduced. This threshold involved the selection of SNPs with significance levels smaller than the locus-wide threshold (p < 1.0 × 10–5) as the second set of IVs [23]. Following this, we utilized the PLINK method to perform SNP clumping, following stringent linkage disequilibrium (LD) criteria, with an R2 < 0.001 threshold and genomic windows exceeding 10,000 kb, to guarantee the independence of our genetic instrumental variables. For situations in which SNPs displayed LD, we retained the one with the most significant p-value.
2.4. Statistical Analysis
Five popular MR methods were used for features containing multiple IVs: inverse variance-weighted (IVW) test [29], weighted mode [30], weighted median [31], the MR-Egger regression [32], and simple mode methods [33]. The IVW method is noted to exhibit slightly greater power than the others in specific circumstances [31]. As a consequence, for results involving multiple instrumental variables, the primary approach relied on the IVW method, while the other four methods were employed to provide supplementary insights.
To assess the robustness of the results, several sensitivity analyses were performed. A leave-one-out analysis was conducted to ascertain whether a single SNP was responsible for driving the causal signal. This approach involves a comparison of the variance explained by the instrumental variables for both the exposure and the outcome. We conducted a heterogeneity test using Cochran’s Q statistics and the two-sample MR package across the instrumental variables. Significant Q statistics with a p-value < 0.05 may suggest the existence of heterogeneity [34,35]. Additionally, we computed F statistics to assess the presence of weak instrument bias [36]. The strength of each IV was assessed by calculating its F-statistic using the formula , where R2 represents the proportion of variance in the exposure explained by the genetic variants, and N represents sample size [37]. Any F-value below 10 was considered indicative of a weak instrument, which was subsequently excluded from the analysis.
In our quest to investigate the potential causal influence of the gut microbiota on the identified morning chronotype, we carried out a reverse MR analysis. In this reverse MR analysis, we considered the gut microbiota as the exposure and the identified morning chronotype as the outcome, utilizing SNPs associated with gut microbiota as IVs. To assess the directionality of causality, we employed the MR Steiger directionality test [38]. The MR analyses were performed in the R version 4.0.2 computing environment, using the latest TwoSampleMR (https://github.com/MRCIEU/TwoSampleMR, accessed on date (20 September 2023)) packages.
3. Results
3.1. Genetic Instruments of Exposure and Outcome
Following the initial SNP selection, in which a stringent significance threshold of p < 5 × 10–8 was applied, we performed pairwise LD clumping and aligned coding alleles between the exposure and outcome summary statistics. This process enabled us to identify instrumental variables (IVs) that met the three core Mendelian randomization (MR) assumptions. In our study on the morning chronotype, we analyzed data from 403,195 participants, among whom 62.6% (252,287 individuals) self-identified as morning people. Ultimately, 122 SNPs were employed as IVs for assessing the morning chronotype, and find detailed information about these IVs can be found in Table S1. In a similar vein, for our investigation on the gut microbiota, we conducted SNP selection with a significance threshold of p < 1 × 10–5, followed by pairwise LD clumping and coding allele alignment, to identify valid IVs satisfying the three fundamental MR assumptions. This phase of the study comprised 18,340 individuals drawn from 24 different cohorts, with the majority (13,266) having European ancestry. In accordance with our IV selection criteria, we utilized a total of 235 SNPs as instrumental variables for the analysis of the gut microbiota, and you can refer to Table S2 for comprehensive details on the selected instrumental variables.
3.2. MR of the Morning Chronotype and the Gut Microbiota
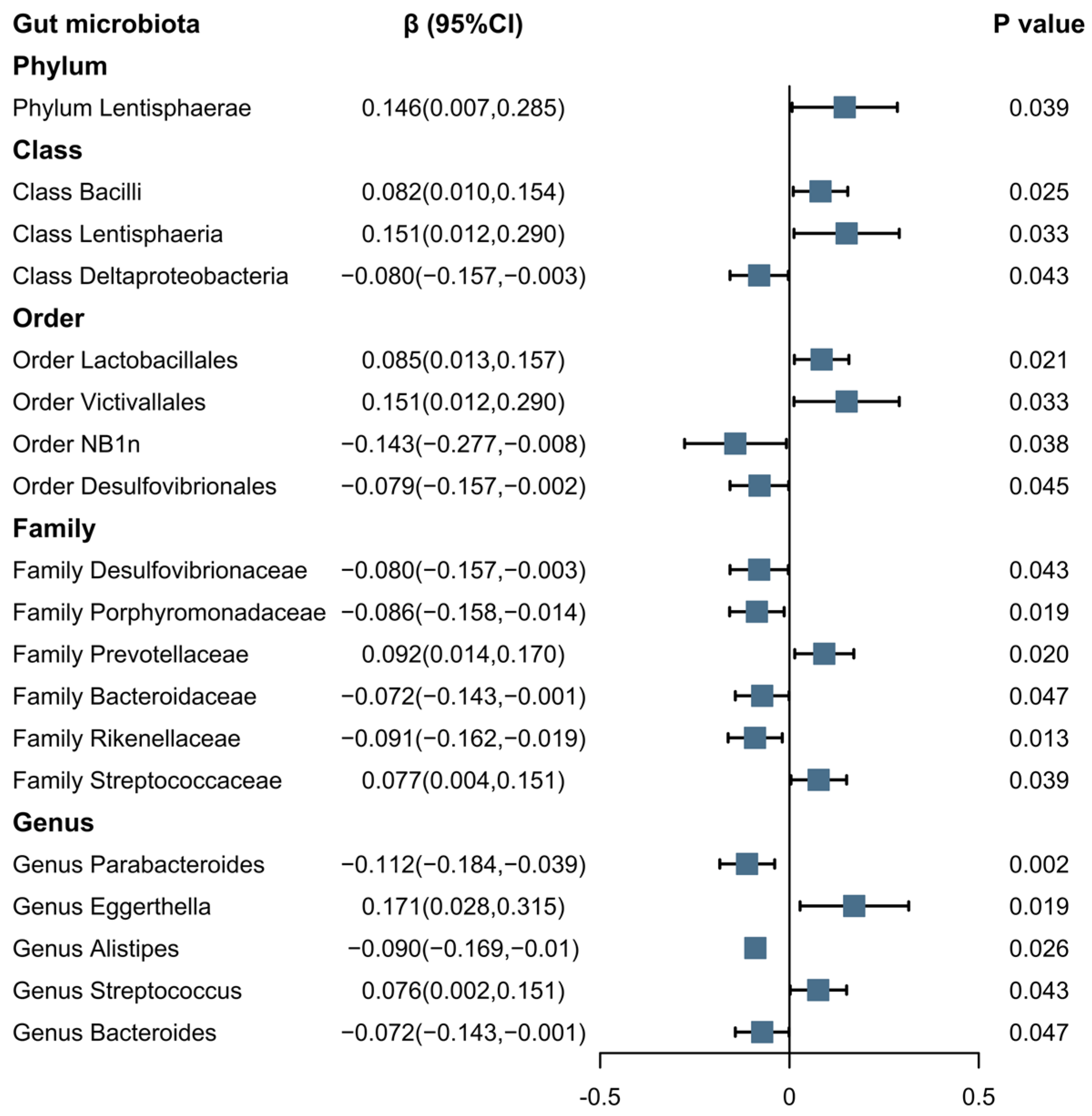
The results, as displayed in Figure 3, indicate a positive association between the morning chronotype and several microbial taxonomic categories—Phylum Lentisphaerae (β = 0.146; 95% CI: 0.007, 0.285; p = 0.039); Class Bacilli (β = 0.082; 95% CI: 0.010, 0.154; p = 0.025); Class Lentisphaeria (β = 0.151; 95% CI: 0.012, 0.290; p = 0.033); Order Lactobacillales (β = 0.085; 95% CI: 0.013, 0.157; p = 0.021); Order Victivallales (β = 0.151; 95% CI: 0.012, 0.290; p = 0.033); Family Prevotellaceae (β = 0.092; 95% CI: 0.014, 0.17; p = 0.020); Family Streptococcaceae (β = 0.077; 95% CI: 0.004, 0.151; p = 0.039); Genus Eggerthella (β = 0.171; 95% CI: 0.028, 0.315; p = 0.019); and Genus Streptococcus (β = 0.076; 95% CI: 0.002, 0.151; p = 0.043)—using the IVW method. Conversely, a negative association was observed between the morning chronotype and the following microbial taxonomic categories using the IVW method: Class Deltaproteobacteria (β = −0.080; 95% CI: −0.157, −0.003; p = 0.043); Order Desulfovibrionales (β = −0.143; 95% CI: −0.277, −0.008; p = 0.038); Family Desulfovibrionaceae (β = −0.079; 95% CI: −0.157, −0.002; p = 0.045); Family Porphyromonadaceae (β = −0.08; 95% CI: −0.157, −0.003; p = 0.043); Family Prevotellaceae (β = −0.086; 95% CI: −0.158, −0.014; p = 0.019); Family Bacteroidaceae (β = −0.072; 95% CI: −0.143, −0.001; p = 0.047); Family Rikenellaceae (β = −0.091; 95% CI: −0.162, −0.019; p = 0.013); Genus Parabacteroides (β = −0.112; 95% CI: −0.184, −0.039; p = 0.002); Genus Alistipes (β = −0.090; 95% CI: −0.169, −0.010; p = 0.026); and Genus Bacteroides (β = −0.072; 95% CI: −0.143, −0.001; p = 0.047).

Figure 3.
The association between the morning chronotype and the gut microbiota using IVW methods. Note: Blue solid squares represent OR values.
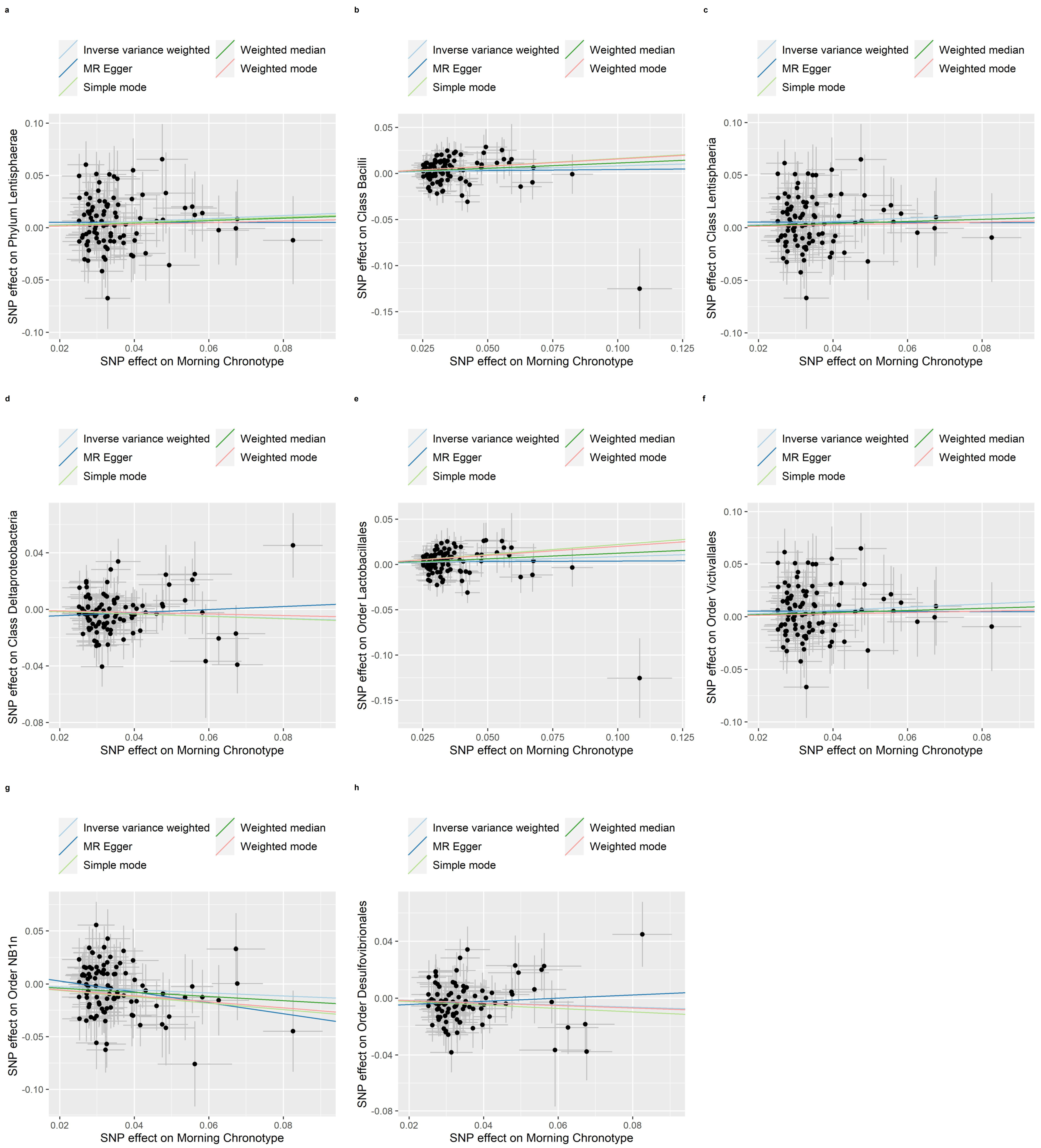
The weighted median, MR-Egger regression, weighted mode and simple mode methods that provided evidence of the relationship between the morning chronotype and the gut microbiota are shown in Table S3. In addition, Figure 4, Figure 5 and Figure 6 show scatter plots of the SNP-outcome associations against the SNP-exposure associations. Figures S1–S19 showcase Mendelian randomization plots that elucidated the connection between the gut microbiota and the morning chronotype. Our rigorous analysis, employing advanced statistical methods, provides a robust confirmation of the accuracy and directionality of the causal effects. The MR Steiger directionality test, as presented in Table S4, affirms that the causal effects align with our expectations, bolstering the validity of our findings. Furthermore, our investigation into horizontal pleiotropy, conducted through MR-Egger regression analyses, yielded no substantial evidence of its presence across all analyses, as demonstrated in Table S5. Additionally, our study identified evidence for heterogeneity among the causal effects, as indicated with Cochran’s Q statistic. This statistical evidence, with a significance level of p for Cochran’s Q < 0.05, implies that there are variations in the estimated causal effects. This finding, detailed in Table S6, adds depth to our understanding of the complexity and diversity of the causal relationships under investigation. In summary, our comprehensive analysis employs a range of methods to ensure the reliability and validity of our results, providing a solid foundation for the conclusions drawn from our study.

Figure 4.
Scatter plots in which the SNP-gut microbiota (phyla, classes, and orders) associations are plotted against the SNP-morning chronotype associations. (a) Phylum Lentisphaerae; (b) Class Bacilli; (c) Class Lentisphaeria; (d) Class Deltaproteobacteria; (e) Order Lactobacillales; (f) Order Victivallales; (g) Order NB1n; (h) Order Desulfovibrionales. Note: black dots represent effects; grey lines represent confidence interval.
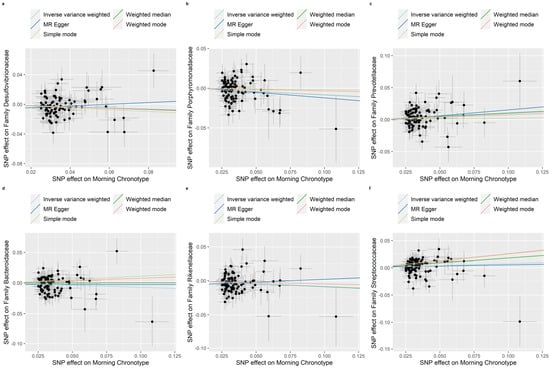
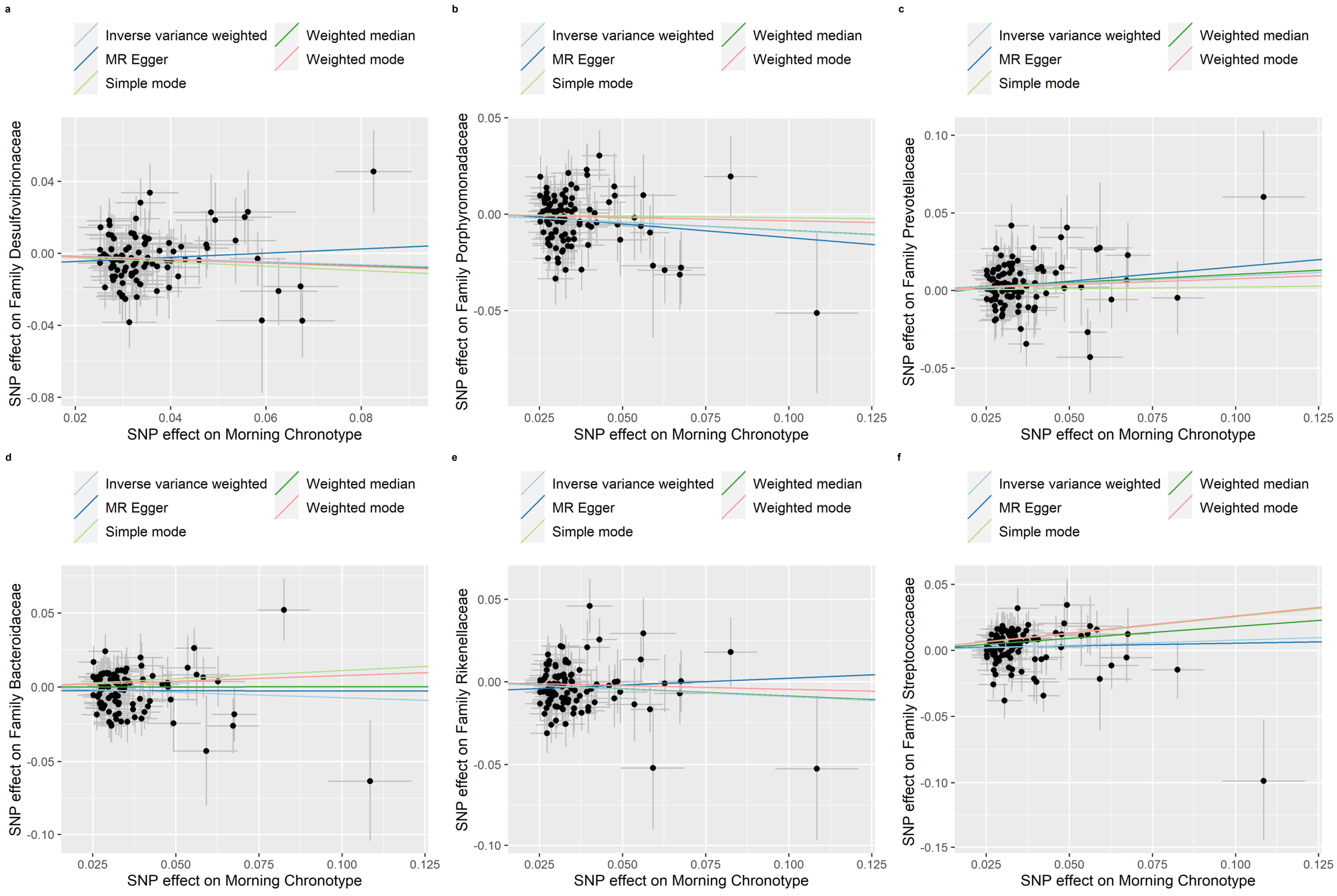
Figure 5.
Scatter plots in which the SNP-gut microbiota (families) associations are plotted against the SNP-morning chronotype associations. (a) Family Desulfovibrionaceae; (b) Family Porphyromonadaceae; (c) Family Prevotellaceae; (d) Family Bacteroidaceae; (e) Family Rikenellaceae; (f) Family Streptococcaceae. Note: black dots represent effects; grey lines represent confidence interval.

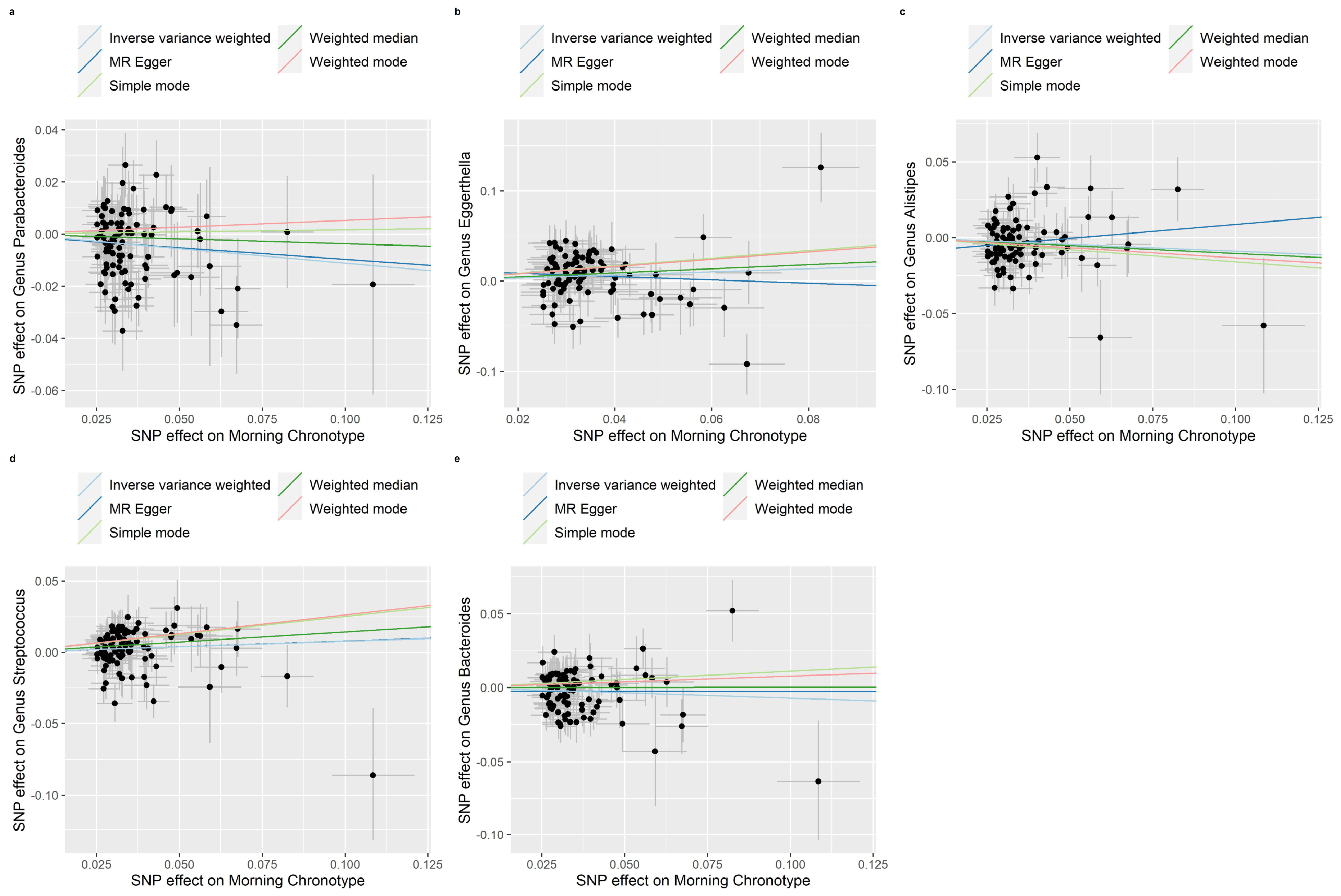
Figure 6.
Scatter plots in which the SNP-gut microbiota (genera) associations are plotted against the SNP-morning chronotype associations. (a) Genus Parabacteroides; (b) Genus Eggerthella; (c) Genus Alistipes; (d) Genus Streptococcus; (e) Genus Bacteroides. Note: black dots represent effects; grey lines represent confidence interval.
3.3. Reverse MR of the Gut Microbiota and the Morning Chronotype
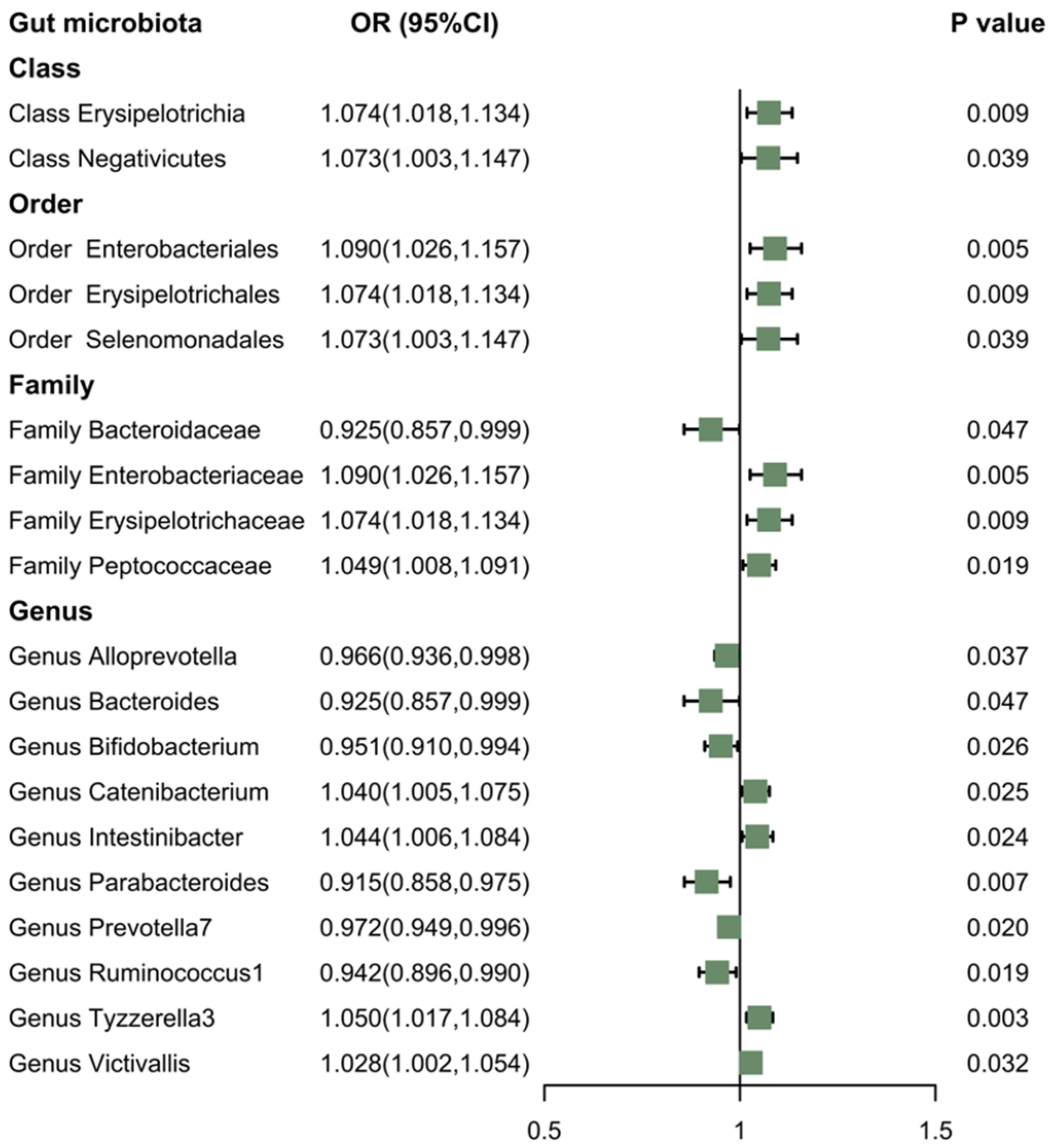
According to the results of reverse MR analysis, there was a suggestive association between the gut microbiota and the morning chronotype (Figure 7). Specifically, the IVW method provided evidence that certain gut microbiota—Class Erysipelotrichia (OR: 1.074; 95% CI: 1.018, 1.134; p = 0.009); Class Negativicutes (OR: 1.073; 95% CI: 1.003, 1.47; p = 0.039); Order Enterobacteriales (OR: 1.090; 95% CI: 1.026, 1.157; p = 0.005); Order Erysipelotrichales (OR: 1.074; 95% CI: 1.018, 1.134; p = 0.009); Order Selenomonadales (OR: 1.073; 95% CI: 1.003, 1.147; p = 0.039); Family Enterobacteriaceae (OR: 1.090; 95% CI: 1.026, 1.157; p = 0.005); Family Erysipelotrichaceae (OR: 1.074; 95% CI: 1.018, 1.134; p = 0.009); Family Peptococcaceae (OR: 1.049; 95% CI: 1.008, 1.091; p = 0.019); Genus Catenibacterium (OR: 1.040; 95% CI: 1.005, 1.075; p = 0.025); Genus Intestinibacter (OR: 1.044; 95% CI: 1.006, 1.084; p = 0.024); Genus Tyzzerella3 (OR: 1.050; 95% CI: 1.017, 1.084; p = 0.003); and Genus Victivallis (OR: 1.028; 95% CI: 1.002, 1.054; p = 0.032)—were positively associated with the morning chronotype. However, Family Bacteroidaceae (OR: 0.925; 95% CI: 0.857, 0.999; p = 0.047); Genus Alloprevotella (OR: 0.966; 95% CI: 0.936, 0.998; p = 0.037); Genus Bacteroides (OR: 0.925; 95% CI: 0.857, 0.999; p = 0.047); Genus Bifidobacterium (OR: 0.951; 95% CI: 0.910, 0.994; p = 0.026); Genus Parabacteroides (OR: 0.915; 95% CI: 0.858, 0.975; p = 0.007); Genus Prevotella7 (OR: 0.972; 95% CI: 0.949, 0.996; p = 0.020); and Genus Ruminococcus1 (OR: 0.942; 95% CI: 0.896, 0.990; p = 0.019) were found to be negatively associated with the morning chronotype.

Figure 7.
The association between the gut microbiota and the morning chronotype using IVW methods. Note: Green solid squares represent OR values.
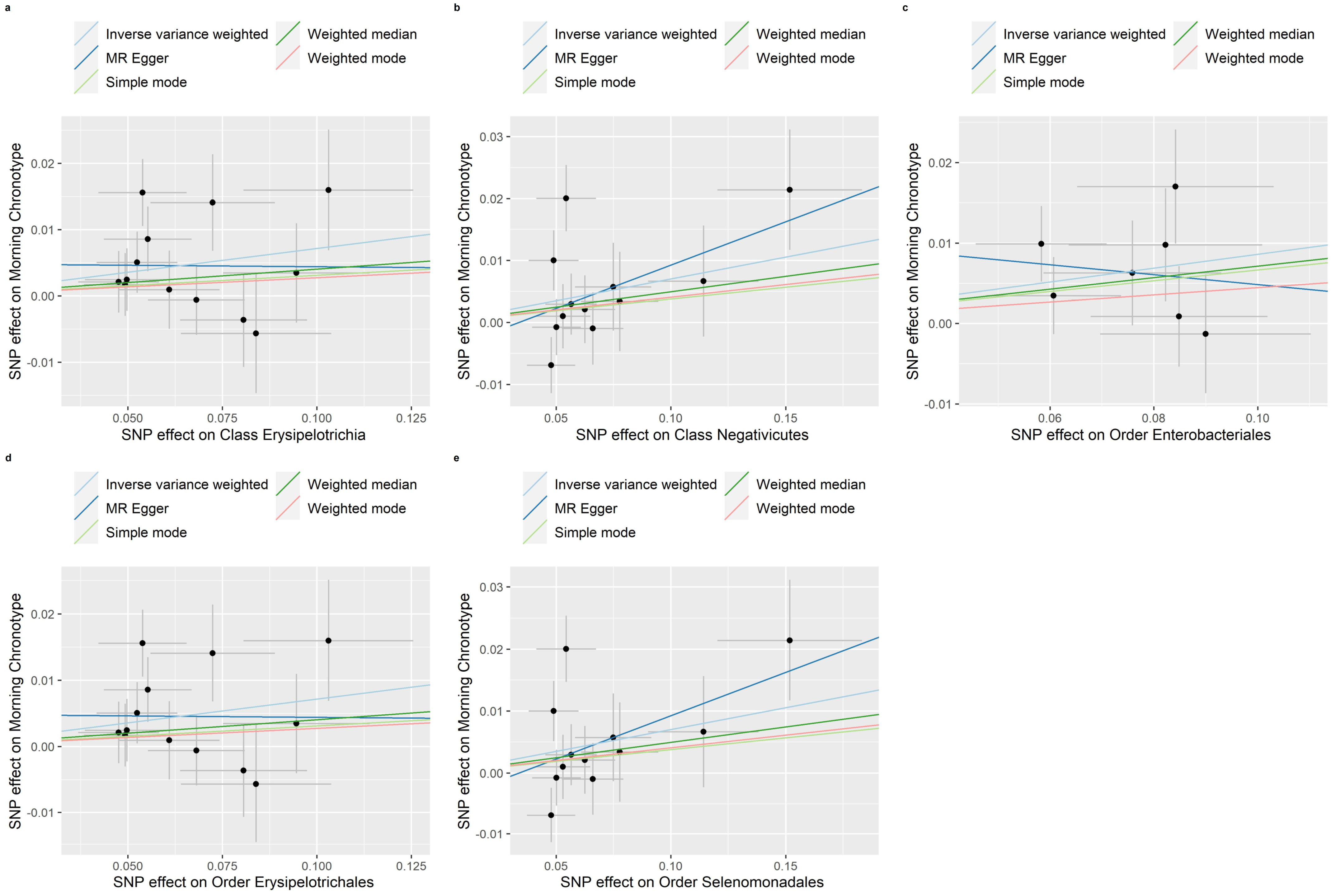
Evidence of a connection between the gut microbiota and the morning chronotype was demonstrated through the weighted median, MR-Egger regression, weighted mode, and simple mode methods in this study (Table S7). In addition, Figure 8, Figure 9 and Figure 10 show scatter plots of the SNP-outcome associations against the SNP-exposure associations. Figures S20–S38 showcase Mendelian randomization plots that elucidated the connection between the gut microbiota and the morning chronotype. The MR Steiger directionality test validated the correctness of the causal effect directions (Table S8). Across all analyses in the MR-Egger regression, there was no substantial evidence of horizontal pleiotropy (Table S9). Additionally, we did observe evidence of heterogeneity among the causal effects, as indicated with Cochran’s Q statistic (i.e., p for Cochran’s Q < 0.05) in the IVW model (Table S10). To address potential outlier SNPs, we conducted the MR-PRESSO test and found no outlier SNPs.

Figure 8.
Scatter plots in which the SNP-morning chronotype associations are plotted against the SNP-gut microbiota (classes and orders) associations. (a) Class Erysipelotrichia; (b) Class Negativicutes; (c) Order Enterobacteriales; (d) Order Erysipelotrichales; (e) Order Selenomonadales. Note: black dots represent effects; grey lines represent confidence interval.

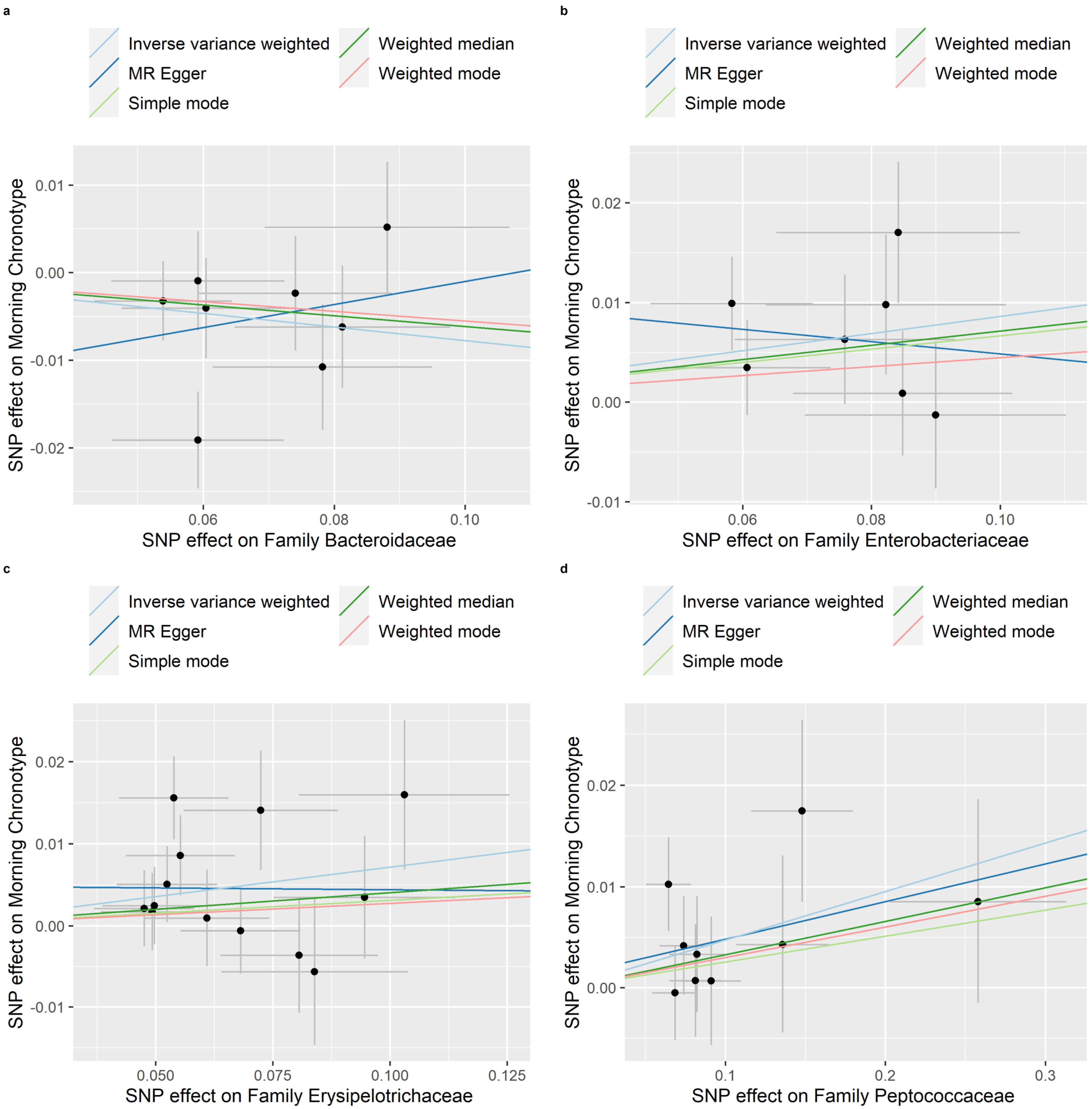
Figure 9.
Scatter plots in which the SNP-morning chronotype associations are plotted against the SNP-gut microbiota (families) associations. (a) Family Bacteroidaceae; (b) Family Enterobacteriaceae; (c) Family Erysipelotrichaceae; (d) Family Peptococcaceae. Note: black dots represent effects; grey lines represent confidence interval.

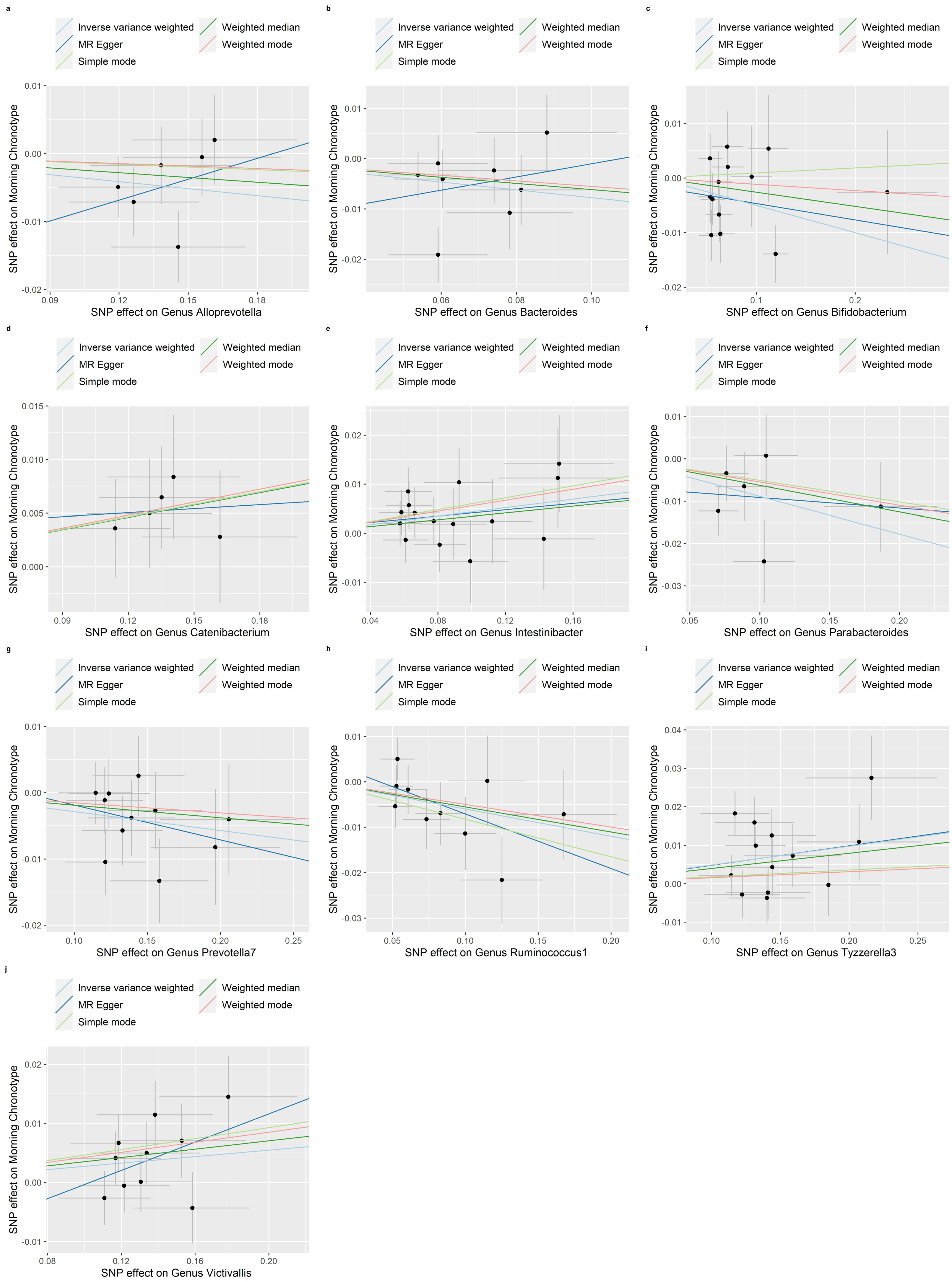
Figure 10.
Scatter plots in which the SNP-morning chronotype associations are plotted against the SNP-gut microbiota (genera) associations. (a) Genus Alloprevotella; (b) Genus Bacteroides; (c) Genus Bifidobacterium; (d) Genus Catenibacterium; (e) Genus Intestinibacter; (f) Genus Parabacteroides; (g) Genus Prevotella7; (h) Genus Ruminococcus1; (i) Genus Tyzzerella3; (j) Genus Victivallis. Note: black dots represent effects; grey lines represent confidence interval.
4. Discussion
In this study, we employed summary statistics of the morning chronotype and summary statistics of the gut microbiota, sourced from the MiBioGen consortium’s largest GWAS meta-analysis. Our approach involved conducting a two-sample MR analysis to investigate the potential causal relationship between the morning chronotype and the gut microbiota. Our analysis revealed causal associations between the morning chronotype and certain microbial taxa, including those of Family Bacteroidaceae, Genus Parabacteroides, and Genus Bacteroides. To gain a more comprehensive understanding of the effects of the morning chronotype on the gut microbiota and its underlying mechanisms, additional randomized controlled trials (RCTs) are warranted.
In recent years, there has been a growing focus on the potential contributions of the gut microbiota to human well-being [39]. In our study, we found that Family Bacteroidaceae, Genus Parabacteroides, and Genus Bacteroides were casually associated with the morning chronotype. Importantly, individuals with a morning chronotype have the capacity to decrease the population of their gut microbiota. There are studies consistent with the results of this study [40,41]. Some studies have found that a strong correlation was observed between Bacteroidaceae and hematopoietic damage markers, suggesting that an increased abundance of Bacteroidaceae could potentially contribute to the hematopoietic toxicity induced by benzene [42]. In contrast, Bacteroidaceae establish multi-organ connections between sites of intestinal inflammation and distal bone marrow, promoting the proliferation and differentiation of myeloid cells specialized in intestinal tissue repair [41].
Within the intricate community of the gut microbiota, particular attention has been directed toward the bacterial genus Parabacteroides. Our study suggests that being a morning person may be associated with a reduction in the abundance of Parabacteroides. However, a previous study found that the abundance of Parabacteroides was inversely associated with obesity, especially in the female and middle-aged populations [43]. A possible reason for this is that Parabacteroides modulate the host metabolism by increasing the production of the secondary bile acids and succinate [44]. There is currently no clear explanation for the association between Parabacteroides and being a morning person. Further research is needed to unravel the intricate interactions and underlying mechanisms that might elucidate this intriguing relationship and shed light on the biological and genetic factors influencing one’s chronotype.
The maintenance of intestinal barrier function depends on the balance of pathogenic bacteria and probiotics [45]. In recent research, it has come to light that various Bacteroides species play pivotal roles in promoting gut homeostasis through the secretion of immunomodulatory factors [46,47]. These beneficial microorganisms have been found to actively contribute to the delicate balance within the gastrointestinal system by releasing compounds that help regulate the immune response and maintain a harmonious environment in the gut [48]. Nevertheless, it is important to note that certain Bacteroides species can exhibit a dual nature, with both beneficial and potentially harmful roles, depending on their specific locations within the host [49]. Current studies on the human gut microbiome have indicated the significant involvement of microbiota in the initiation of different forms of cancer in humans, and recent research has suggested that microbiota play pivotal roles in the genesis of various types of cancer [50,51,52]. Our research has revealed a compelling link between being a morning person and a decrease in Bacteroides abundance, and future investigations may offer a more nuanced understanding of these connections and their potential implications for health. Potential factors include the fact that a microbiome imbalance can lead to a greater susceptibility to cancer, as pathogens are capable of exerting detrimental effects on the host’s physiology, metabolism, and immune system, consequently promoting the growth of tumors [53].
This study boasts several strengths, including the utilization of MR analysis to establish the causal link between the gut microbiota and the morning chronotype. Genetic variants associated with gut microbiota were derived from the most extensive GWAS meta-analysis available, ensuring the robustness of the instruments in the MR analysis. To address potential issues, like horizontal pleiotropy, the study employed tests such as MR-PRESSO and the MR-Egger regression intercept term. However, it is crucial to acknowledge certain limitations while interpreting the results. The reliance on summary statistics instead of raw data precluded the possibility of conducting subgroup analyses, marking a constraint in the study’s scope. Since the lowest taxonomic level in the exposure dataset was genus, this restriction prevented us from further exploring the causal association between the gut microbiota and the morning chronotype at the species level. However, this taxonomic restriction underscores the need for more detailed information at the species level to better understand the nuanced relationship between the composition of the gut microbiota and the expression of morning chronotype traits. Subsequent studies should contemplate employing metagenomic sequencing techniques on cohorts with distinctly assigned chronotypes to investigate the correlation between the morning chronotype and the gut microbiota [54].
5. Conclusions
In summary, our comprehensive analysis identified a causal association between being a morning person and having specific microbial taxa in the gut, such as Family Bacteroidaceae, Genus Parabacteroides, and Genus Bacteroides. This noteworthy discovery underscores the intricate interplay between the morning chronotype and the composition of the gut microbiota, serving as a poignant reminder that our health is a complex tapestry, intricately woven from the diverse threads of lifestyle, genetics, and environmental factors. Furthermore, the association we studied should also increase the necessity for rigorous randomized controlled trials through which to better understand the impact of the morning chronotype on the gut microbiota and its mechanisms.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu16010046/s1, Figure S1. Mendelian randomization plots for the relationship of the morning chronotype with Phylum Lentisphaerae; Figure S2. Mendelian randomization plots for the relationship of the morning chronotype with Class Bacilli; Figure S3. Mendelian randomization plots for the relationship of the morning chronotype with Class Lentisphaeria; Figure S4. Mendelian randomization plots for the relationship of the morning chronotype with Class Deltaproteobacteria; Figure S5. Mendelian randomization plots for the relationship of the morning chronotype with Order Lactobacillales; Figure S6. Mendelian randomization plots for the relationship of the morning chronotype with Order Victivallales; Figure S7. Mendelian randomization plots for the relationship of the morning chronotype with Order NB1n; Figure S8. Mendelian randomization plots for the relationship of the morning chronotype with Order Desulfovibrionales; Figure S9. Mendelian randomization plots for the relationship of the morning chronotype with Family Desulfovibrionaceae; Figure S10. Mendelian randomization plots for the relationship of the morning chronotype with Family Porphyromonadaceae; Figure S11. Mendelian randomization plots for the relationship of the morning chronotype with Family Prevotellaceae; Figure S12. Mendelian randomization plots for the relationship of the morning chronotype with Family Bacteroidaceae; Figure S13. Mendelian randomization plots for the relationship of the morning chronotype with Family Rikenellaceae; Figure S14. Mendelian randomization plots for the relationship of the morning chronotype with Family Streptococcaceae; Figure S15. Mendelian randomization plots for the relationship of the morning chronotype with Genus Parabacteroides; Figure S16. Mendelian randomization plots for the relationship of the morning chronotype with Genus Eggerthella; Figure S17. Mendelian randomization plots for the relationship of the morning chronotype with Genus Alistipes; Figure S18. Mendelian randomization plots for the relationship of the morning chronotype with Genus Streptococcus; Figure S19. Mendelian randomization plots for the relationship of the morning chronotype with Genus Bacteroides; Figure S20. Mendelian randomization plots for the relationship of Class Erysipelotrichia with the morning chronotype; Figure S21. Mendelian randomization plots for the relationship of Class Negativicutes with the morning chronotype; Figure S22. Mendelian randomization plots for the relationship of Family Bacteroidaceae with the morning chronotype; Figure S23. Mendelian randomization plots for the relationship of Family Enterobacteriaceae with the morning chronotype; Figure S24. Mendelian randomization plots for the relationship of Family Erysipelotrichaceae with the morning chronotype; Figure S25. Mendelian randomization plots for the relationship of Family Peptococcaceae with the morning chronotype; Figure S26. Mendelian randomization plots for the relationship of Genus Alloprevotella with the morning chronotype; Figure S27. Mendelian randomization plots for the relationship of Genus Bacteroides with the morning chronotype; Figure S28. Mendelian randomization plots for the relationship of Genus Bifidobacterium with the morning chronotype; Figure S29. Mendelian randomization plots for the relationship of Genus Catenibacterium with the morning chronotype; Figure S30. Mendelian randomization plots for the relationship of Genus Intestinibacter with the morning chronotype; Figure S31. Mendelian randomization plots for the relationship of Genus Parabacteroides with the morning chronotype; Figure S32. Mendelian randomization plots for the relationship of Genus Prevotella7 with the morning chronotype; Figure S33. Mendelian randomization plots for the relationship of Genus Ruminococcus1 with the morning chronotype; Figure S34. Mendelian randomization plots for the relationship of Genus Tyzzerella3 with the morning chronotype; Figure S35. Mendelian randomization plots for the relationship of Genus Victivallis with the morning chronotype; Figure S36. Mendelian randomization plots for the relationship of Order Enterobacteriales with the morning chronotype; Figure S37. Mendelian randomization plots for the relationship of Order Erysipelotrichales with the morning chronotype; Figure S38. Mendelian randomization plots for the relationship of Order Selenomonadales with the morning chronotype; Table S1: Summary information on diurnal preference SNPs used as genetic instruments for the Mendelian randomization analyses; Table S2: Summary information on the gut microbiota SNPs used as genetic instruments for the Mendelian randomization analyses; Table S3: The association between morning diurnal preference and the gut microbiota using MR methods; Table S4: Results of MR Steiger directionality test for morning diurnal preference on the gut microbiota; Table S5: Inspected the horizontal pleiotropy through its intercept and provides estimates after correcting for the pleiotropic effects in the MR- Egger regression; Table S6: Verified the heterogeneity between the causal estimates of each SNPs in the IVW and MR- Egger methods; Table S7: The association between the gut microbiota and morning diurnal preference using MR methods; Table S8: Results of MR Steiger directionality test for morning diurnal preference on the gut microbiota; Table S9: Inspected the horizontal pleiotropy through its intercept and provides estimates after correcting for the pleiotropic effects in the MR- Egger regression; Table S10: Verified the heterogeneity between the causal estimates of each SNPs in the IVW and MR- Egger method.
Author Contributions
M.C. and Z.W. contributed equally to this work. Conceptualization, M.C. and Z.W.; data curation, D.S.T., Z.Y., Z.X., D.Z., D.W. and Y.Z.; formal analysis, M.C.; funding acquisition, Z.W. and X.W.; resources, D.S.T., Z.Y., Z.X., D.Z., D.W. and Y.Z.; software, M.C. and Z.W.; supervision, X.W., Y.Q. and Y.J.; validation, M.C.; visualization, Y.Q.; writing—original draft, M.C. and Z.W.; writing—review and editing, X.W. and Y.J. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Natural Science Foundation No. 82204067 (X.W.) and No. 82304166 (Z.W.).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets analyzed during the current study are available from the European Consortium [25], and the MiBioGen repository, https://mibiogen.gcc.rug.nl/ (accessed on date (25 September 2023)) [26].
Acknowledgments
We express our gratitude to the participants, as well as to the international European Consortium and the MiBioGen consortium initiative, for their valuable contributions in openly sharing the genetic data.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Dunlap, J.C.; Loros, J.J. Yes, circadian rhythms actually do affect almost everything. Cell Res. 2016, 26, 759–760. [Google Scholar] [CrossRef] [PubMed]
- Horne, J.A.; Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar] [PubMed]
- Pan, X.; Mota, S.; Zhang, B. Circadian Clock Regulation on Lipid Metabolism and Metabolic Diseases. Adv. Exp. Med. Biol. 2020, 1276, 53–66. [Google Scholar] [CrossRef] [PubMed]
- Cox, K.H.; Takahashi, J.S. Circadian clock genes and the transcriptional architecture of the clock mechanism. J. Mol. Endocrinol. 2019, 63, R93–R102. [Google Scholar] [CrossRef] [PubMed]
- Montaruli, A.; Castelli, L.; Mulè, A.; Scurati, R.; Esposito, F.; Galasso, L.; Roveda, E. Biological Rhythm and Chronotype: New Perspectives in Health. Biomolecules 2021, 11, 487. [Google Scholar] [CrossRef] [PubMed]
- Bauducco, S.; Richardson, C.; Gradisar, M. Chronotype, circadian rhythms and mood. Curr. Opin. Psychol. 2020, 34, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Mason, A.M.; Titova, O.E.; Vithayathil, M.; Kar, S.; Chen, J.; Li, X.; Burgess, S.; Larsson, S.C. Morning chronotype and digestive tract cancers: Mendelian randomization study. Int. J. Cancer 2023, 152, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Summa, K.C.; Voigt, R.M.; Forsyth, C.B.; Shaikh, M.; Cavanaugh, K.; Tang, Y.; Vitaterna, M.H.; Song, S.; Turek, F.W.; Keshavarzian, A. Disruption of the Circadian Clock in Mice Increases Intestinal Permeability and Promotes Alcohol-Induced Hepatic Pathology and Inflammation. PLoS ONE 2013, 8, e67102. [Google Scholar] [CrossRef]
- Takahashi, J.S.; Hong, H.K.; Ko, C.H.; McDearmon, E.L. The genetics of mammalian circadian order and disorder: Implications for physiology and disease. Nat. Rev. Genet. 2008, 9, 764–775. [Google Scholar] [CrossRef]
- Schmid, S.M.; Hallschmid, M.; Schultes, B. The metabolic burden of sleep loss. Lancet Diabetes Endocrinol. 2015, 3, 52–62. [Google Scholar] [CrossRef]
- Baglioni, C.; Battagliese, G.; Feige, B.; Spiegelhalder, K.; Nissen, C.; Voderholzer, U.; Lombardo, C.; Riemann, D. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 2011, 135, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Lovato, N.; Gradisar, M. A meta-analysis and model of the relationship between sleep and depression in adolescents: Recommendations for future research and clinical practice. Sleep Med. Rev. 2014, 18, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Taylor, B.J.; Hasler, B.P. Chronotype and Mental Health: Recent Advances. Curr. Psychiatry Rep. 2018, 20, 59. [Google Scholar] [CrossRef] [PubMed]
- Jayasudha, R.; Das, T.; Kalyana Chakravarthy, S.; Sai Prashanthi, G.; Bhargava, A.; Tyagi, M.; Rani, P.K.; Pappuru, R.R.; Shivaji, S. Gut mycobiomes are altered in people with type 2 Diabetes Mellitus and Diabetic Retinopathy. PLoS ONE 2020, 15, e0243077. [Google Scholar] [CrossRef] [PubMed]
- Adak, A.; Khan, M.R. An insight into gut microbiota and its functionalities. Cell. Mol. Life Sci. 2019, 76, 473–493. [Google Scholar] [CrossRef]
- Milani, C.; Duranti, S.; Bottacini, F.; Casey, E.; Turroni, F.; Mahony, J.; Belzer, C.; Delgado Palacio, S.; Arboleya Montes, S.; Mancabelli, L.; et al. The First Microbial Colonizers of the Human Gut: Composition, Activities, and Health Implications of the Infant Gut Microbiota. Microbiol. Mol. Biol. Rev. 2017, 81, e00036-17. [Google Scholar] [CrossRef]
- Zmora, N.; Suez, J.; Elinav, E. You are what you eat: Diet, health and the gut microbiota. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 35–56. [Google Scholar] [CrossRef]
- Park, E.M.; Chelvanambi, M.; Bhutiani, N.; Kroemer, G.; Zitvogel, L.; Wargo, J.A. Targeting the gut and tumor microbiota in cancer. Nat. Med. 2022, 28, 690–703. [Google Scholar] [CrossRef]
- Meng, C.; Bai, C.; Brown, T.D.; Hood, L.E.; Tian, Q. Human Gut Microbiota and Gastrointestinal Cancer. Genom. Proteom. Bioinform. 2018, 16, 33–49. [Google Scholar] [CrossRef] [PubMed]
- Xia, Y.; Ding, X.; Wang, S.; Ren, W. Circadian orchestration of host and gut microbiota in infection. Biol. Rev. Camb. Philos. Soc. 2023, 98, 115–131. [Google Scholar] [CrossRef]
- Yue, M.; Jin, C.; Jiang, X.; Xue, X.; Wu, N.; Li, Z.; Zhang, L. Causal Effects of Gut Microbiota on Sleep-Related Phenotypes: A Two-Sample Mendelian Randomization Study. Clocks Sleep 2023, 5, 566–580. [Google Scholar] [CrossRef] [PubMed]
- Greenland, S. An introduction to instrumental variables for epidemiologists. Int. J. Epidemiol. 2000, 29, 722–729. [Google Scholar] [CrossRef] [PubMed]
- Sanna, S.; van Zuydam, N.R.; Mahajan, A.; Kurilshikov, A.; Vich Vila, A.; Võsa, U.; Mujagic, Z.; Masclee, A.A.M.; Jonkers, D.; Oosting, M.; et al. Causal relationships among the gut microbiome, short-chain fatty acids and metabolic diseases. Nat. Genet. 2019, 51, 600–605. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Ni, J.J.; Han, B.X.; Yan, S.S.; Wei, X.T.; Feng, G.J.; Zhang, H.; Zhang, L.; Li, B.; Pei, Y.F. Causal Relationship Between Gut Microbiota and Autoimmune Diseases: A Two-Sample Mendelian Randomization Study. Front. Immunol. 2021, 12, 746998. [Google Scholar] [CrossRef]
- Jones, S.E.; Lane, J.M.; Wood, A.R.; van Hees, V.T.; Tyrrell, J.; Beaumont, R.N.; Jeffries, A.R.; Dashti, H.S.; Hillsdon, M.; Ruth, K.S.; et al. Genome-wide association analyses of chronotype in 697,828 individuals provides insights into circadian rhythms. Nat. Commun. 2019, 10, 343. [Google Scholar] [CrossRef]
- Kurilshikov, A.; Medina-Gomez, C.; Bacigalupe, R.; Radjabzadeh, D.; Wang, J.; Demirkan, A.; Le Roy, C.I.; Raygoza Garay, J.A.; Finnicum, C.T.; Liu, X.; et al. Large-scale association analyses identify host factors influencing human gut microbiome composition. Nat. Genet. 2021, 53, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Kurilshikov, A.; Radjabzadeh, D.; Turpin, W.; Croitoru, K.; Bonder, M.J.; Jackson, M.A.; Medina-Gomez, C.; Frost, F.; Homuth, G.; et al. Meta-analysis of human genome-microbiome association studies: The MiBioGen consortium initiative. Microbiome 2018, 6, 101. [Google Scholar] [CrossRef]
- Long, Y.; Tang, L.; Zhou, Y.; Zhao, S.; Zhu, H. Causal relationship between gut microbiota and cancers: A two-sample Mendelian randomisation study. BMC Med. 2023, 21, 66. [Google Scholar] [CrossRef]
- Burgess, S.; Butterworth, A.; Thompson, S.G. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet. Epidemiol. 2013, 37, 658–665. [Google Scholar] [CrossRef]
- Hartwig, F.P.; Davey Smith, G.; Bowden, J. Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int. J. Epidemiol. 2017, 46, 1985–1998. [Google Scholar] [CrossRef]
- Bowden, J.; Davey Smith, G.; Haycock, P.C.; Burgess, S. Consistent Estimation in Mendelian Randomization with Some Invalid Instruments Using a Weighted Median Estimator. Genet. Epidemiol. 2016, 40, 304–314. [Google Scholar] [CrossRef]
- Bowden, J.; Davey Smith, G.; Burgess, S. Mendelian randomization with invalid instruments: Effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 2015, 44, 512–525. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Zhang, S.; Tian, Y.; Si, H.; Zeng, Y.; Wu, Y.; Liu, Y.; Li, M.; Sun, K.; Wu, L.; et al. Genetic Causal Association between Iron Status and Osteoarthritis: A Two-Sample Mendelian Randomization. Nutrients 2022, 14, 3683. [Google Scholar] [CrossRef] [PubMed]
- Greco, M.F.; Minelli, C.; Sheehan, N.A.; Thompson, J.R. Detecting pleiotropy in Mendelian randomisation studies with summary data and a continuous outcome. Stat. Med. 2015, 34, 2926–2940. [Google Scholar] [CrossRef] [PubMed]
- Bowden, J.; Del Greco, M.F.; Minelli, C.; Zhao, Q.; Lawlor, D.A.; Sheehan, N.A.; Thompson, J.; Davey Smith, G. Improving the accuracy of two-sample summary-data Mendelian randomization: Moving beyond the NOME assumption. Int. J. Epidemiol. 2019, 48, 728–742. [Google Scholar] [CrossRef]
- Burgess, S.; Thompson, S.G. Bias in causal estimates from Mendelian randomization studies with weak instruments. Stat. Med. 2011, 30, 1312–1323. [Google Scholar] [CrossRef] [PubMed]
- Staiger, D.; Stock, J.H. Instrumental variables regression with weak instruments. Econometrica 1997, 65, 557–586. [Google Scholar] [CrossRef]
- Hemani, G.; Tilling, K.; Davey Smith, G. Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genet. 2017, 13, e1007081. [Google Scholar] [CrossRef]
- Clemente, J.C.; Ursell, L.K.; Parfrey, L.W.; Knight, R. The impact of the gut microbiota on human health: An integrative view. Cell 2012, 148, 1258–1270. [Google Scholar] [CrossRef]
- Khosravi, A.; Yáñez, A.; Price, J.G.; Chow, A.; Merad, M.; Goodridge, H.S.; Mazmanian, S.K. Gut microbiota promote hematopoiesis to control bacterial infection. Cell Host Microbe 2014, 15, 374–381. [Google Scholar] [CrossRef]
- Sezaki, M.; Hayashi, Y.; Nakato, G.; Wang, Y.; Nakata, S.; Biswas, S.; Morishima, T.; Fakruddin, M.; Moon, J.; Ahn, S.; et al. Hematopoietic stem and progenitor cells integrate microbial signals to promote post-inflammation gut tissue repair. EMBO J. 2022, 41, e110712. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Kang, H.; Zhang, W.; Wang, J.; Liu, Z.; Jing, J.; Han, L.; Gao, A. Probiotics ameliorate benzene-induced systemic inflammation and hematopoietic toxicity by inhibiting Bacteroidaceae-mediated ferroptosis. Sci. Total Environ. 2023, 899, 165678. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Zhang, X.; Fu, J.; Duan, Z.; Qiu, W.; Cai, Y.; Ma, W.; Zhou, H.; Chen, Y.; Zheng, J.; et al. Sex- and Age-Dependent Associations between Parabacteroides and Obesity: Evidence from Two Population Cohort. Microorganisms 2023, 11, 2087. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Liao, M.; Zhou, N.; Bao, L.; Ma, K.; Zheng, Z.; Wang, Y.; Liu, C.; Wang, W.; Wang, J.; et al. Parabacteroides distasonis Alleviates Obesity and Metabolic Dysfunctions via Production of Succinate and Secondary Bile Acids. Cell Rep. 2019, 26, 222–235.e225. [Google Scholar] [CrossRef] [PubMed]
- Ohland, C.L.; MacNaughton, W.K. Probiotic bacteria and intestinal epithelial barrier function. Am. J. Physiol.-Gastrointest. Liver Physiol. 2010, 298, G807–G819. [Google Scholar] [CrossRef] [PubMed]
- Hiippala, K.; Jouhten, H.; Ronkainen, A.; Hartikainen, A.; Kainulainen, V.; Jalanka, J.; Satokari, R. The Potential of Gut Commensals in Reinforcing Intestinal Barrier Function and Alleviating Inflammation. Nutrients 2018, 10, 988. [Google Scholar] [CrossRef] [PubMed]
- Brown, E.M.; Ke, X.; Hitchcock, D.; Jeanfavre, S.; Avila-Pacheco, J.; Nakata, T.; Arthur, T.D.; Fornelos, N.; Heim, C.; Franzosa, E.A.; et al. Bacteroides-Derived Sphingolipids Are Critical for Maintaining Intestinal Homeostasis and Symbiosis. Cell Host Microbe 2019, 25, 668–680.e667. [Google Scholar] [CrossRef]
- Sichetti, M.; De Marco, S.; Pagiotti, R.; Traina, G.; Pietrella, D. Anti-inflammatory effect of multistrain probiotic formulation (L. rhamnosus, B. lactis, and B. longum). Nutrition 2018, 53, 95–102. [Google Scholar] [CrossRef]
- Zafar, H.; Saier, M.H., Jr. Gut Bacteroides species in health and disease. Gut Microbes 2021, 13, 1848158. [Google Scholar] [CrossRef]
- Zitvogel, L.; Galluzzi, L.; Viaud, S.; Vétizou, M.; Daillère, R.; Merad, M.; Kroemer, G. Cancer and the gut microbiota: An unexpected link. Sci. Transl. Med. 2015, 7, 271ps1. [Google Scholar] [CrossRef]
- Gopalakrishnan, V.; Helmink, B.A.; Spencer, C.N.; Reuben, A.; Wargo, J.A. The Influence of the Gut Microbiome on Cancer, Immunity, and Cancer Immunotherapy. Cancer Cell 2018, 33, 570–580. [Google Scholar] [CrossRef] [PubMed]
- Baffy, G. Gut Microbiota and Cancer of the Host: Colliding Interests. Adv. Exp. Med. Biol. 2020, 1219, 93–107. [Google Scholar] [CrossRef] [PubMed]
- Tong, Y.; Gao, H.; Qi, Q.; Liu, X.; Li, J.; Gao, J.; Li, P.; Wang, Y.; Du, L.; Wang, C. High fat diet, gut microbiome and gastrointestinal cancer. Theranostics 2021, 11, 5889–5910. [Google Scholar] [CrossRef]
- Carasso, S.; Fishman, B.; Lask, L.S.; Shochat, T.; Geva-Zatorsky, N.; Tauber, E. Metagenomic analysis reveals the signature of gut microbiota associated with human chronotypes. FASEB J. 2021, 35, e22011. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).