Longitudinal Associations of Dietary Fructose, Sodium, and Potassium and Psychological Stress with Vascular Aging Index and Incident Cardiovascular Disease in the CARDIA Cohort
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Study Measures and Outcomes
2.3. Statistical Analysis
3. Results
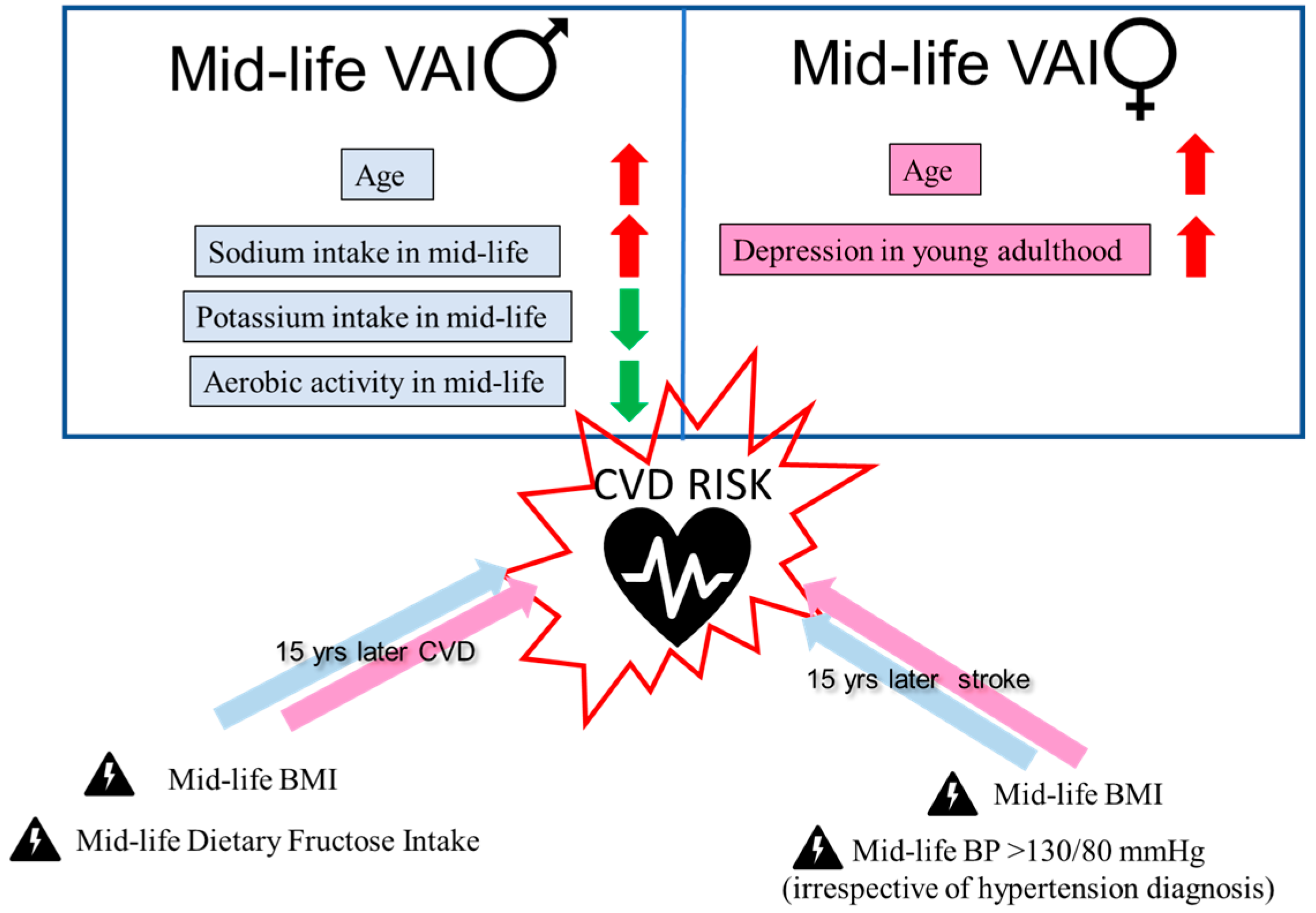
3.1. Association of Demographic, Dietary, and Stress Predictors with VAI
3.2. Predictors of CVDs, Stroke, and Death in the CARDIA Cohort
3.2.1. Primary Outcome: CVDs
3.2.2. Secondary Outcome: Stroke
3.2.3. Tertiary Outcome: Death
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| aPWV | aortic pulse-wave velocity |
| CARDIA | Coronary Artery Risk Development in Young Adults Study |
| cfPWV | carotid-femoral pulse wave velocity |
| cIMT | carotid intima–media thickness |
| CVDs | cardiovascular diseases |
| HFCS | high fructose corn syrup |
| NO | nitric oxide |
| obsHBP | observed high blood pressure (BP > 130/80 mmHg) |
| VAI | vascular aging index |
References
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation 2022, 145, e153–e639. [Google Scholar] [CrossRef] [PubMed]
- de Rezende Mikael, L.; de Paiva, A.M.G.; Gomes, M.M.; Sousa, A.L.L.; Jardim, P.C.B.V.; de Oliveira Vitorino, P.V.; Euzébio, M.B.; de Moura Sousa, W.; Barroso, W.K.S. Vascular Aging and Arterial Stiffness. Arq. Bras. Cardiol. 2017, 109, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Q.; Hu, M.-J.; Cui, Y.-J.; Liang, L.; Zhou, M.-M.; Yang, Y.-W.; Huang, F. Carotid-Femoral Pulse Wave Velocity in the Prediction of Cardiovascular Events and Mortality: An Updated Systematic Review and Meta-Analysis. Angiology 2018, 69, 617–629. [Google Scholar] [CrossRef] [PubMed]
- Nilsson Wadström, B.; Fatehali, A.-A.H.; Engström, G.; Nilsson, P.M. A Vascular Aging Index as Independent Predictor of Cardiovascular Events and Total Mortality in an Elderly Urban Population. Angiology 2019, 70, 929–937. [Google Scholar] [CrossRef] [PubMed]
- Ungvari, Z.; Tarantini, S.; Donato, A.J.; Galvan, V.; Csiszar, A. Mechanisms of Vascular Aging. Circ. Res. 2018, 123, 849–867. [Google Scholar] [CrossRef]
- Harvey, A.; Montezano, A.C.; Lopes, R.A.; Rios, F.; Touyz, R.M. Vascular Fibrosis in Aging and Hypertension: Molecular Mechanisms and Clinical Implications. Can. J. Cardiol. 2016, 32, 659–668. [Google Scholar] [CrossRef]
- LaRocca, T.J.; Martens, C.R.; Seals, D.R. Nutrition and other lifestyle influences on arterial aging. Ageing Res. Rev. 2017, 39, 106–119. [Google Scholar] [CrossRef]
- Merz, A.A.; Cheng, S. Sex differences in cardiovascular ageing. Heart 2016, 102, 825–831. [Google Scholar] [CrossRef]
- Sara, J.D.S.; Toya, T.; Ahmad, A.; Clark, M.M.; Gilliam, W.P.; Lerman, L.O.; Lerman, A. Mental Stress and Its Effects on Vascular Health. Mayo Clin. Proc. 2022, 97, 951–990. [Google Scholar] [CrossRef]
- Vespa, J.; Armstrong, D.M.; Medina, L. Demographic Turning Points for the United States: Population Projections for 2020 to 2060; US Department of Commerce, Economics and Statistics Administration: Washington, DC, USA, 2018. [Google Scholar]
- Sabbatini, A.R.; Kararigas, G. Menopause-Related Estrogen Decrease and the Pathogenesis of HFpEF: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2020, 75, 1074–1082. [Google Scholar] [CrossRef]
- Stanhewicz, A.E.; Wenner, M.M.; Stachenfeld, N.S. Sex differences in endothelial function important to vascular health and overall cardiovascular disease risk across the lifespan. Am. J. Physiol. Heart Circ. Physiol. 2018, 315, H1569–H1588. [Google Scholar] [CrossRef] [PubMed]
- Moreau, K.L. Modulatory influence of sex hormones on vascular aging. Am. J. Physiol. Heart Circ. Physiol. 2019, 316, H522–H526. [Google Scholar] [CrossRef]
- Ji, H.; Kwan, A.C.; Chen, M.T.; Ouyang, D.; Ebinger, J.E.; Bell, S.P.; Niiranen, T.J.; Bello, N.A.; Cheng, S. Sex Differences in Myocardial and Vascular Aging. Circ. Res. 2022, 130, 566–577. [Google Scholar] [CrossRef]
- Kuehner, C. Why is depression more common among women than among men? Lancet Psychiatry 2017, 4, 146–158. [Google Scholar] [CrossRef] [PubMed]
- Hankin, B.L.; Mermelstein, R.; Roesch, L. Sex differences in adolescent depression: Stress exposure and reactivity models. Child Dev. 2007, 78, 279–295. [Google Scholar] [CrossRef] [PubMed]
- Plaisier, I.; de Bruijn, J.; Smit, J.; de Graaf, R.; Have, M.T.; Beekman, A.; van Dyck, R.; Penninx, B. Work and family roles and the association with depressive and anxiety disorders: Differences between men and women. J. Affect. Disord. 2008, 105, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Connelly, P.J.; Azizi, Z.; Alipour, P.; Delles, C.; Pilote, L.; Raparelli, V. The Importance of Gender to Understand Sex Differences in Cardiovascular Disease. Can. J. Cardiol. 2021, 37, 699–710. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Allen, N.B.; Anderson, C.A.; Black, T.; Brewer, L.C.; Foraker, R.E.; Grandner, M.A.; Lavretsky, H.; Perak, A.M.; Sharma, G.; et al. Life’s Essential 8: Updating and Enhancing the American Heart Association’s Construct of Cardiovascular Health: A Presidential Advisory From the American Heart Association. Circulation 2022, 146, e18–e43. [Google Scholar] [CrossRef]
- Rossman, M.J.; LaRocca, T.J.; Martens, C.R.; Seals, D.R. Healthy lifestyle-based approaches for successful vascular aging. J. Appl. Physiol. 2018, 125, 1888–1900. [Google Scholar] [CrossRef]
- Nowak, K.L.; Rossman, M.J.; Chonchol, M.; Seals, D.R. Strategies for Achieving Healthy Vascular Aging. Hypertension 2018, 71, 389–402. [Google Scholar] [CrossRef]
- D’Elia, L.; Galletti, F.; La Fata, E.; Sabino, P.; Strazzullo, P. Effect of dietary sodium restriction on arterial stiffness: Systematic review and meta-analysis of the randomized controlled trials. J. Hypertens. 2018, 36, 734–743. [Google Scholar] [CrossRef] [PubMed]
- Ezekowitz, J.A.; Colin-Ramirez, E.; Ross, H.; Escobedo, J.; Macdonald, P.; Troughton, R.; Saldarriaga, C.; Alemayehu, W.; McAlister, F.A.; Arcand, J.; et al. Reduction of dietary sodium to less than 100 mmol in heart failure (SODIUM-HF): An international, open-label, randomised, controlled trial. Lancet 2022, 399, 1391–1400. [Google Scholar] [CrossRef] [PubMed]
- McDonough, A.A.; Veiras, L.C.; Guevara, C.A.; Ralph, D.L. Cardiovascular benefits associated with higher dietary K(+) vs. lower dietary Na(+): Evidence from population and mechanistic studies. Am. J. Physiol. Endocrinol. Metab. 2017, 312, E348–E356. [Google Scholar] [CrossRef] [PubMed]
- Houston, M.C. The importance of potassium in managing hypertension. Curr. Hypertens. Rep. 2011, 13, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.W.; Dumke, K.A.; Goran, M.I. Fructose content in popular beverages made with and without high-fructose corn syrup. Nutrition 2014, 30, 928–935. [Google Scholar] [CrossRef] [PubMed]
- Ventura, E.E.; Davis, J.N.; Goran, M.I. Sugar content of popular sweetened beverages based on objective laboratory analysis: Focus on fructose content. Obesity 2011, 19, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Tappy, L.; Le, K.A. Metabolic effects of fructose and the worldwide increase in obesity. Physiol. Rev. 2010, 90, 23–46. [Google Scholar] [CrossRef]
- Komnenov, D.; Levanovich, P.E.; Perecki, N.; Chung, C.S.; Rossi, N.F. Aortic Stiffness and Diastolic Dysfunction in Sprague Dawley Rats Consuming Short-Term Fructose Plus High Salt Diet. Integr. Blood Press. Control. 2020, 13, 111–124. [Google Scholar] [CrossRef]
- Komnenov, D.; Rossi, N.F. Fructose-induced salt-sensitive blood pressure differentially affects sympathetically mediated aortic stiffness in male and female Sprague-Dawley rats. Physiol. Rep. 2023, 11, e15687. [Google Scholar] [CrossRef]
- Komnenov, D.; Levanovich, P.E.; Rossi, N.F. Hypertension Associated with Fructose and High Salt: Renal and Sympathetic Mechanisms. Nutrients 2019, 11, 569. [Google Scholar] [CrossRef]
- Soncrant, T.; Komnenov, D.; Beierwaltes, W.H.; Chen, H.; Wu, M.; Rossi, N.F. Bilateral renal cryodenervation decreases arterial pressure and improves insulin sensitivity in fructose-fed Sprague-Dawley rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2018, 315, R529–R538. [Google Scholar] [CrossRef] [PubMed]
- Levanovich, P.E.; Chung, C.S.; Komnenov, D.; Rossi, N.F. Fructose plus High-Salt Diet in Early Life Results in Salt-Sensitive Cardiovascular Changes in Mature Male Sprague Dawley Rats. Nutrients 2021, 13, 3129. [Google Scholar] [CrossRef] [PubMed]
- Levanovich, P.E.; Daugherty, A.M.; Komnenov, D.; Rossi, N.F. Dietary fructose and high salt in young male Sprague Dawley rats induces salt-sensitive changes in renal function in later life. Physiol. Rep. 2022, 10, e15456. [Google Scholar] [CrossRef] [PubMed]
- Jayalath, V.H.; de Souza, R.J.; Ha, V.; Mirrahimi, A.; Blanco-Mejia, S.; Di Buono, M.; Jenkins, A.L.; Leiter, L.A.; Wolever, T.M.; Beyene, J.; et al. Sugar-sweetened beverage consumption and incident hypertension: A systematic review and meta-analysis of prospective cohorts. Am. J. Clin. Nutr. 2015, 102, 914–921. [Google Scholar] [CrossRef]
- Gao, J.-W.; Hao, Q.-Y.; Zhang, H.-F.; Li, X.-Z.; Yuan, Z.-M.; Guo, Y.; Wang, J.-F.; Zhang, S.-L.; Liu, P.-M. Low-Carbohydrate Diet Score and Coronary Artery Calcium Progression: Results from the CARDIA Study. Arter. Thromb. Vasc. Biol. 2021, 41, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Duffey, K.J.; Gordon-Larsen, P.; Steffen, L.M.; Jacobs, D.R., Jr.; Popkin, B.M. Drinking caloric beverages increases the risk of adverse cardiometabolic outcomes in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am. J. Clin. Nutr. 2010, 92, 954–959. [Google Scholar] [CrossRef] [PubMed]
- Friedman, G.D.; Cutter, G.R.; Donahue, R.P.; Hughes, G.H.; Hulley, S.B.; Jacobs, D.R., Jr.; Liu, K.; Savage, P.J. CARDIA: Study design, recruitment, and some characteristics of the examined subjects. J. Clin. Epidemiol. 1988, 41, 1105–1116. [Google Scholar] [CrossRef]
- Jacobs, D.R., Jr.; Yatsuya, H.; Hearst, M.O.; Thyagarajan, B.; Kalhan, R.; Rosenberg, S.; Smith, L.J.; Barr, R.G.; Duprez, D.A. Rate of decline of forced vital capacity predicts future arterial hypertension: The Coronary Artery Risk Development in Young Adults Study. Hypertension 2012, 59, 219–225. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M. The 2017 American College of Cardiology/American Heart Association clinical practice guideline for high blood pressure in adults. JAMA Cardiol. 2018, 3, 352–353. [Google Scholar] [CrossRef]
- McDonald, A.; Van Horn, L.; Slattery, M.; Hilner, J.; Bragg, C.; Caan, B.; Jr, D.J.; Liu, K.; Hubert, H.; Gernhofer, N.; et al. The CARDIA dietary history: Development, implementation, and evaluation. J. Am. Diet. Assoc. 1991, 91, 1104–1112. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Jacobs, D.R.; Hahn, L.P.; Haskell, W.L.; Pirie, P.; Sidney, S. Validity and reliability of short physical activity history: CARDIA and the Minnesota Heart Health Program. J. Cardiopulm. Rehabil. Prev. 1989, 9, 448–459. [Google Scholar] [CrossRef]
- Baker, S.E.; Limberg, J.K.; Ranadive, S.M.; Joyner, M.J. Neurovascular control of blood pressure is influenced by aging, sex, and sex hormones. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2016, 311, R1271–R1275. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Zhu, Y.; Malik, V.; Li, X.; Peng, X.; Zhang, F.F.; Shan, Z.; Liu, L. Intake of Sugar-Sweetened and Low-Calorie Sweetened Beverages and Risk of Cardiovascular Disease: A Meta-Analysis and Systematic Review. Adv. Nutr. 2021, 12, 89–101. [Google Scholar] [CrossRef] [PubMed]
- Stanhope, K.L.; Schwarz, J.M.; Keim, N.L.; Griffen, S.C.; Bremer, A.A.; Graham, J.L.; Hatcher, B.; Cox, C.L.; Dyachenko, A.; Zhang, W.; et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J. Clin. Invest. 2009, 119, 1322–1334. [Google Scholar] [CrossRef] [PubMed]
- Siasos, G.; Tsigkou, V.; Coskun, A.U.; Oikonomou, E.; Zaromitidou, M.; Lerman, L.O.; Lerman, A.; Stone, P.H. The Role of Shear Stress in Coronary Artery Disease. Curr. Top. Med. Chem. 2023, 23, 2132–2157. [Google Scholar] [CrossRef]
- Pigeyre, M.; Yazdi, F.T.; Kaur, Y.; Meyre, D. Recent progress in genetics, epigenetics and metagenomics unveils the pathophysiology of human obesity. Clin. Sci. 2016, 130, 943–986. [Google Scholar] [CrossRef]
- Redinger, R.N. The pathophysiology of obesity and its clinical manifestations. Gastroenterol. Hepatol. 2007, 3, 856. [Google Scholar]
- Conner, M.; Norman, P. Health behaviour: Current issues and challenges. Psychol. Health 2017, 32, 895–906. [Google Scholar] [CrossRef]
| Male (n = 1159) | Female (n = 1497) | p Value | |
|---|---|---|---|
| Continuous variables, Mean (SD) | |||
| Age at baseline | 26 ± 3 | 26 ± 3 | 0.685 |
| BMI at baseline | 23.5 ± 4.6 | 23.4 ± 4.9 | 0.906 |
| % calories from sucrose at baseline | 6.11 ± 4.82 | 6.28 ± 6.14 | 0.337 |
| CES-D baseline | 1.42 ± 0.64 | 1.61 ± 0.80 | <0.001 |
| % calories from fructose at year 20 | 4.38 ± 3.05 | 4.52 ± 3.65 | 0.061 |
| % calories from sucrose at year 20 | 7.07 ± 3.66 | 7.63 ± 4.11 | 0.002 |
| Sodium (mg) at year 20 | 3679 ± 2153 | 2694 ± 1454 | <0.001 |
| Potassium (mg) at year 20 | 3318 ± 1621 | 2754 ± 1344 | <0.001 |
| CES-D scores at year 20 | 8.26 ± 6.87 | 9.35 ± 8.23 | 0.021 |
| Right carotid PWV (cm/s) at year 20 | 55.60 ± 15.92 | 58.90 ± 17.65 | <0.001 |
| Left carotid PWV (cm/s) at year 20 | 52.50 ± 15.65 | 56.80 ± 17.20 | <0.001 |
| cIMT (mm) at year 20 | 0.62 ± 0.19 | 0.57 ± 0.16 | <0.001 |
| Vascular Aging Index at year 20 | 15.00 ± 2.74 | 14.39 ± 2.33 | <0.001 |
| Categorical variables, Numbers (%) | |||
| HBP observed at baseline | 228 ± 8.6 | 111 ± 4.2 | <0.001 |
| HBP observed at year 20 | 75 ± 6.4 | 97 ± 6.5 | 0.993 |
| Baseline High Cholesterol | 24 ± 2.1 | 29 ± 1.9 | 0.669 |
| Baseline Heart Problems | 48 ± 4.1 | 102 ± 6.8 | 0.007 |
| Baseline Diabetes | 3 ± 0.2 | 9 ± 0.6 | 0.216 |
| Baseline Kidney Problems | 20 ± 1.7 | 77 ± 5.2 | <0.001 |
| On CVD Medications at Baseline | 1 ± 0.08 | 4 ± 0.2 | 0.31 |
| Run at least 1 h/month in the past 12 months | 122 (10.5) | 83 (5.5) | <0.001 |
| Bike at least 1 h/month in the past 12 months | 460 (17.4) | 394 (14.9) | <0.001 |
| Racket sport at least 1 h/month in the past 12 months | 514 (19.4) | 465 (17.6) | <0.001 |
| Male | Female | |||||
|---|---|---|---|---|---|---|
| b-Weight | B-Weight | p Value | b-Weight | B-Weight | p Value | |
| Predictors measured at baseline | ||||||
| Age | 0.130 | 0.163 | <0.001 | 0.100 | 0.154 | <0.001 |
| Depression scores | 0.067 | 0.016 | 0.598 | 0.186 | 0.063 | 0.015 |
| Dietary sodium | 0.000 | 0.037 | 0.212 | 0.000 | 0.004 | 0.884 |
| % calories from sucrose | 0.016 | 0.027 | 0.363 | 0.004 | 0.012 | 0.661 |
| BMI | 0.019 | 0.032 | 0.274 | 0.005 | 0.011 | 0.678 |
| obsHBP | 0.345 | 0.050 | 0.094 | −0.039 | −0.004 | 0.866 |
| Predictors measured at year 20 of follow-up | ||||||
| Age | 0.137 | 0.171 | <0.001 | 0.079 | 0.127 | <0.001 |
| CES-D score | −0.008 | −0.021 | 0.514 | 0.009 | 0.033 | 0.236 |
| % calories from fructose | −0.028 | −0.031 | 0.349 | 0.026 | 0.042 | 0.157 |
| Dietary sodium | 0.000 | 0.145 | 0.003 | 0.000 | 0.023 | 0.575 |
| Dietary potassium | 0.000 | −0.160 | <0.001 | 0.000 | −0.059 | 0.150 |
| obsHBP | 0.110 | 0.010 | 0.757 | 0.101 | 0.011 | 0.694 |
| Aerobic activity (run/bike/racquet sports) | −0.763 | −0.085 | 0.007 | −0.400 | −0.042 | 0.137 |
| Model 1 | p-Value | Model 2 | p-Value | Model 3 | p-Value | |
|---|---|---|---|---|---|---|
| Primary Outcome: any CVDs (fatal or non-fatal) | ||||||
| BMI | 1.065 [1.039–1.092] | <0.001 | 1.065 [1.039–1.092] | <0.001 | 1.067 [1.041–1.094] | <0.001 |
| obsHBP baseline | 1.321 [0.878–1.988] | 0.182 | 1.323 [0.879–1.992] | 0.179 | 1.287 [0.855–1.938] | 0.227 |
| obsHBP Y20 | 1.037 [0.577–1.862] | 0.904 | 1.039 [0.578–1.866] | 0.898 | 1.025 [0.571–1.839] | 0.934 |
| % cal fructose Y20 | 1.051 [1.009–1.094] | 0.016 | 1.049 [1.006–1.093] | 0.024 | 1.049 [1.007–1.093] | 0.022 |
| % cal sucrose Y20 | 0.981 [0.942–1.022] | 0.369 | 0.981 [0.942–1.022] | 0.358 | 0.980 [0.941–1.021] | 0.339 |
| CES-D Y20 | 1.004 [0.983–1.025] | 0.698 | 1.004 [0.984–1.026] | 0.677 | 1.003 [0.982–1.024] | 0.779 |
| VAI | 0.999 [0.941–1.060] | 0.968 | 1.000 [0.942–1.062] | 0.998 | 0.999 [0.941–1.061] | 0.985 |
| Secondary Outcome: stroke (fatal or non-fatal) | ||||||
| BMI | 1.069 [1.025–1.115] | 0.002 | 1.068 [1.024–1.115] | 0.002 | 1.069 [1.024–1.116] | 0.002 |
| obsHBP baseline | 2.010 [1.078–3.747] | 0.028 | 2.020 [1.083–3.771] | 0.027 | 1.984 [1.061–3.711] | 0.032 |
| obsHBP Y20 | 0.382 [0.090–1.610] | 0.190 | 0.389 [0.092–1.645] | 0.199 | 0.385 [0.091–1.627] | 0.194 |
| % cal fructose Y20 | 1.046 [0.975–1.121] | 0.210 | 1.032 [0.959–1.111] | 0.399 | 1.033 [0.960–1.112] | 0.380 |
| % cal sucrose Y20 | 0.947 [0.877–1.021] | 0.156 | 0.946 [0.877–1.020] | 0.147 | 0.944 [0.875–1.018] | 0.133 |
| CES-D Y20 | 0.996 [0.960–1.033] | 0.832 | 0.998 [0.962–1.035] | 0.897 | 0.996 [0.960–1.034] | 0.845 |
| VAI | 0.857 [0.857–1.068] | 0.433 | 0.9664 [0.863–1.078] | 0.521 | 0.964 [0.861–1.079] | 0.526 |
| Tertiary Outcome: death | ||||||
| BMI | 1.036 [1.011–1.060] | 0.004 | 1.036 [1.011–1.061] | 0.004 | 1.035 [1.011–1.060] | 0.004 |
| obsHBP baseline | 1.042 [0.707–1.538] | 0.834 | 1.041 [0.705–1.536] | 0.841 | 1.047 [0.709–1.547] | 0.818 |
| obsHBP Y20 | 0.797 [0.450–1.411] | 0.436 | 0.793 [0.447–1.404] | 0.425 | 0.794 [0.448–1.406] | 0.429 |
| % cal fructose Y20 | 1.017 [0.978–1.057] | 0.406 | 1.019 [0.980–1.060] | 0.345 | 1.019 [0.980–1.060] | 0.344 |
| % cal sucrose Y20 | 0.985 [0.951–1.021] | 0.411 | 0.986 [0.952–1.021] | 0.432 | 0.986 [0.952–1.022] | 0.441 |
| CES-D Y20 | 0.997 [0.979–1.016] | 0.750 | 0.997 [0.978–1.015] | 0.718 | 0.997 [0.978–1.015] | 0.718 |
| VAI | 0.980 [0.928–1.035] | 0.466 | 0.978 [0.926–1.033] | 0.433 | 0.978 [0.926–1.034] | 0.436 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osborne, M.; Bernard, A.; Falkowski, E.; Peterson, D.; Vavilikolanu, A.; Komnenov, D. Longitudinal Associations of Dietary Fructose, Sodium, and Potassium and Psychological Stress with Vascular Aging Index and Incident Cardiovascular Disease in the CARDIA Cohort. Nutrients 2024, 16, 127. https://doi.org/10.3390/nu16010127
Osborne M, Bernard A, Falkowski E, Peterson D, Vavilikolanu A, Komnenov D. Longitudinal Associations of Dietary Fructose, Sodium, and Potassium and Psychological Stress with Vascular Aging Index and Incident Cardiovascular Disease in the CARDIA Cohort. Nutrients. 2024; 16(1):127. https://doi.org/10.3390/nu16010127
Chicago/Turabian StyleOsborne, Meaghan, Alexa Bernard, Emily Falkowski, Deni Peterson, Anusha Vavilikolanu, and Dragana Komnenov. 2024. "Longitudinal Associations of Dietary Fructose, Sodium, and Potassium and Psychological Stress with Vascular Aging Index and Incident Cardiovascular Disease in the CARDIA Cohort" Nutrients 16, no. 1: 127. https://doi.org/10.3390/nu16010127
APA StyleOsborne, M., Bernard, A., Falkowski, E., Peterson, D., Vavilikolanu, A., & Komnenov, D. (2024). Longitudinal Associations of Dietary Fructose, Sodium, and Potassium and Psychological Stress with Vascular Aging Index and Incident Cardiovascular Disease in the CARDIA Cohort. Nutrients, 16(1), 127. https://doi.org/10.3390/nu16010127






