Adherence to the Mediterranean Diet in Women and Reproductive Health across the Lifespan: A Narrative Review
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Study Selection and Data Extraction
2.4. Quality Assessment
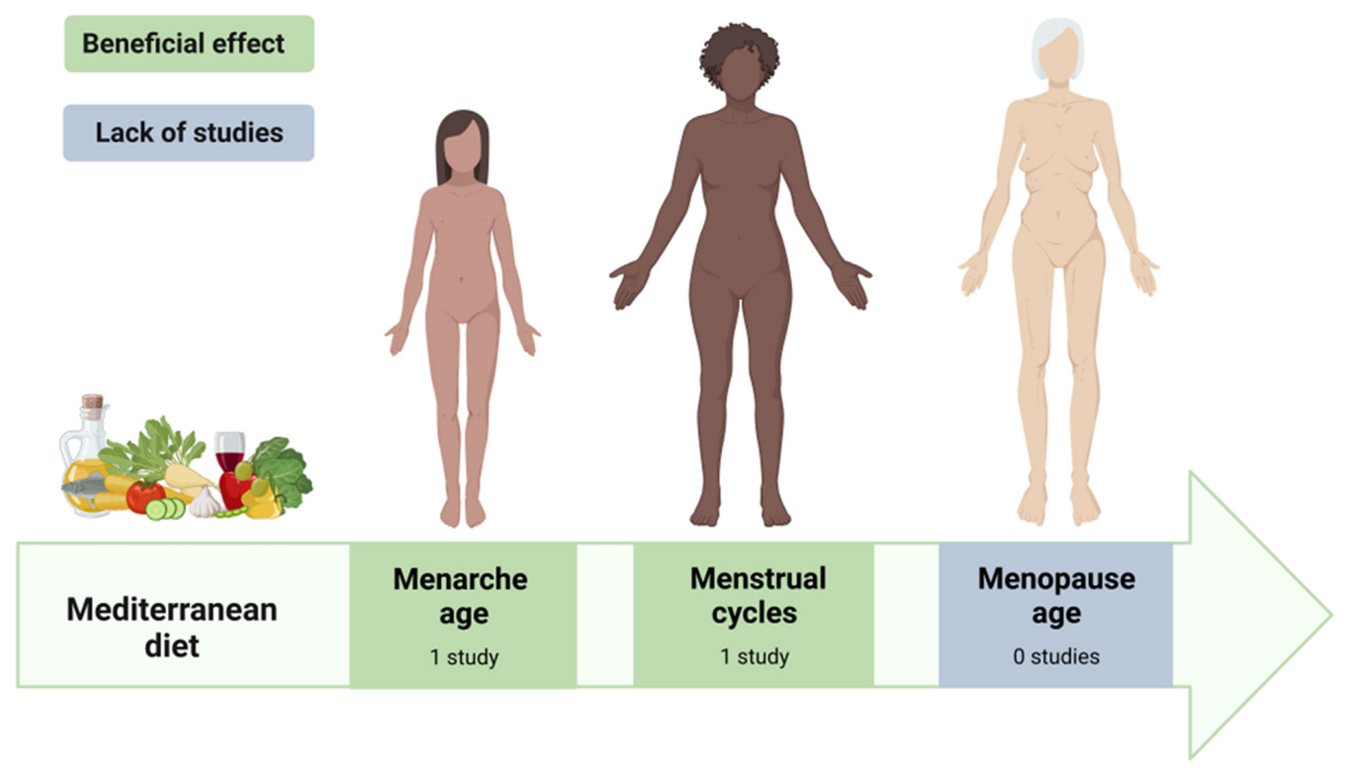
3. Reproductive Health
3.1. Menarche
3.1.1. Observational Studies
3.1.2. Possible Mechanism
3.2. Menstrual Cycle
Observational Studies
3.3. Menopause
3.3.1. Age of Onset of Menopause
| Authors (Country) | Type of Study | Number and Age of Participants | Assessment of Mediterranean Diet | Effect | Quality Assessment a |
|---|---|---|---|---|---|
| AGE OF MENARCHE | |||||
| Szamreta et al. [18] (USA) | Longitudinal cohort study | n = 202 10.0 ± 0.58 years | Adapted MD score | No association | Low |
| MENSTRUAL CYCLE | |||||
| Onieva-Zafra et al. [30] (Spain) | Cross- sectional | n = 311 21.2 ± 2.6 years | KIDMED questionnaire | Women with low adherence had longer menstrual cycles. No association with regularity, amount of flow, duration of menses, or menstrual pain. | Medium |
| AGE OF ONSET OF MENOPAUSE | |||||
| No study was conducted | |||||
3.3.2. The European Menopause and Andropause Society (EMAS) Position Statement
3.3.3. Symptoms and Health Problems Related to Perimenopausal Age
4. Reproductive Health Dysfunction
4.1. Premenstrual Syndrome
4.1.1. Observational Studies
4.1.2. Possible Mechanism
4.2. Dysmenorrhea
Observational Studies
4.3. Sexual Dysfunction
4.3.1. Experimental and Observational Studies
4.3.2. Possible Mechanism
4.4. Endometriosis
4.4.1. Experimental Studies
4.4.2. Possible Mechanism
4.5. Polycystic Ovary Syndrome
4.5.1. Randomized Controlled Trials
4.5.2. Case-Control Studies
4.5.3. Cross-Sectional Studies
4.5.4. Possible Mechanism
4.6. Infertility
4.6.1. Observational Studies
4.6.2. Possible Mechanism
| Authors (Country) | Type of Study | Number and Age of Participants | Assessment of Mediterranean Diet | Effect | Quality Assessment a |
|---|---|---|---|---|---|
| PREMENSTRUAL SYNDROME | |||||
| Kwon et al. [48] (South Korea) | Cross-sectional | Non-PMS: n = 91 33 (26–37) years PMS: n = 171 31 (26–37) years | Mediterranean Diet Adherence Screener | Low adherence to MD was associated with increased risk of PMS. | Medium |
| DYSMENORRHEA | |||||
| Onieva-Zafra et al. [30] (Spain) | Cross-sectional | n = 311 21.2 ± 2.6 years | KIDMED questionnaire | No association. | Medium |
| SEXUAL DYSFUNCTION | |||||
| Esposito et al. [76] (Italy) | Randomized controlled trial study Women with metabolic syndrome and FSD Intervention: MD for 2 years | MD n = 21 42.3 ± 4.5 years CD n = 28 41.5 ± 3.9 years | Evaluated by the nutritionist for 24 months (consultations every month) | Improved FSFI and reduced CRP levels in the intervention group. No single sexual domain (desire, arousal, lubrication, orgasm, satisfaction, pain) was significantly ameliorated. | Major limitations |
| Maiorino et al. [77] (Italy) | Randomized clinical trial study Women with type 2 diabetes and FSD Intervention: MD for 8.1 years | MD n = 54 50.9 ± 9.2 years LFD n = 55 51.2 ± 9.3 years | MD score | Less deterioration in the sexual health of the intervention group. | Major limitations |
| Giugliano et al. [78] (Italy) | Cross-sectional study Women with type 2 diabetes and FSD | n = 595 57.9 ± 6.7 years | MD score | Women with the highest MD score had lowest prevalence of sexual dysfunction. | Medium |
| ENDOMETRIOSIS | |||||
| Ott et al. [83] (Austria) | Experimental study Women with endometriosis Intervention: MD for 5 months | n = 68 35.3 ± 11.2 years | Self-reported by each patient | Significant relief of general pain and an improvement in the general condition. | Major limitations |
| POLYCYSTIC OVARY SYNDROME | |||||
| Cincione et al. [87] (Italy) | Randomized controlled trial Overweight and/or obese women with PCOS Intervention: hypocaloric MD vs. KD for 45 days | MD n = 71 33.6 ± 4.9 years KD n = 73 33.4 ± 5.7 years | Evaluated by the nutritionist through counseling every 2 weeks and reinforced by phone calls every 2–3 days | Both interventions were effective. The improvement in the anthropometric, metabolic, and endocrine parameters was significantly higher in the KD compared to the MD group. | Major limitations |
| Mei et al. [88] (China) | Randomized controlled trial Overweight women with PCOS Intervention: MD/LC vs. LF for 12 weeks | MD/LC n = 30 28.0 ± 5.3 years LF n = 29 28.1 ± 7.1 years | Evaluated and monitored by the nutritionist | Both dietary models were effective. MED/LC effectiveness was higher than the LF. | Major limitations |
| Wang et al. [89] (China) | Case-control study Cases: PCOS patients Controls: healthy women | PCOS n = 202 30.2 ± 3.4 years Controls n = 325 31.8 ± 3.8 years | MD pattern | Protective association with PCOS. | Medium |
| Cutillas-Tolin et al. [90] (Spain) | Case-control study Cases: PCOS patients Controls: healthy women | PCOS n = 121 Controls n = 155 29.1 ± 5.7 years | Relative MD score Adapted MD score | No associations. | High |
| Moran et al. [85] (Australia) | Population cross-sectional study Women with and without self-declared PCOS | PCOS n = 414 33.5 ± 0.1 years Non-PCOS n = 7155 33.7 ± 0.1 years | MD pattern | Protective association MD with PCOS. | High |
| Barrea et al. [91] (Italy) | Cross-sectional study Women with and without diagnosed PCOS | PCOS n = 112 24.2 ± 5.5 years Non-PCOS n = 112 24.1 ± 5.1 years | PREDIMED questionnaire | PCOS vs. non-PCOS group had a lower adherence to the MD. | High |
| Barrea et al. [92] (Italy) | Cross-sectional study Treatment-naïve women with PCOS and obesity | PCOS MHO n = 54 23.8 ± 3.7 years PCOS MUO n = 40 24.5 ± 3.7 years | PREDIMED questionnaire | MUO vs. MHO patients had a lower adherence to the MD. | High |
| INFERTILITY | |||||
| Sun et al. [106] (China) | Prospective cohort study Infertile women before IVF treatment | LMD n = 362 31.85 ± 3.68 years HMD n = 228 31.67 ± 3.80 years | MD score | Higher number of available embryos; positively correlated with the number of fertilized oocytes and embryo yielded. | High |
| Karayiannis et al. [107] (Greece) | Prospective cohort study Women before first IVF treatment | T1 n = 79 35 (32–37) years T2 n = 79 36 (32–39) years T3 n = 86 36 (34–38) years | MD score | Higher rates of clinical pregnancy and live birth. | High |
| Gaskins et al. [108] (United States) | Prospective cohort study Women with at least one cycle of ART | n = 357 35.3 ± 4.0 years | MD score | Higher probability of live birth. | Medium |
| Ricci et al. [109] (Italy) | Prospective cohort study Women before IVF treatment | n = 474 36.6 ± 3.6 years | MD score | Protective effect of intermediate adherence to MD on oocyte number and clinical pregnancy in women > 35 years. | Medium |
| Gaskins et al. [110] (United States) | Prospective cohort study Women with no history of pregnancy loss and who reported at least one pregnancy | Total n = 11,072 Q1 n = 2356 30.0 (28.0–33.0) years Q4 n = 2677 32.0 (30.0–35.0) years | Adapted MD score | No effect on the risk of pregnancy loss. | High |
| Vujkovic et al. [111] (Netherlands) | Cross-sectional study Women undergoing IVF treatment | LMD n = 54 35.2 (23.2–43.7) years IMD n = 54 33.9 (23.7–40.6) years HMD n = 53 37.2 (29.3–42.1) years | MD pattern | Significantly increased probability of pregnancy. | High |
5. Beneficial Effects of MD on Women’s Reproductive Health: Impact of Single Components or Synergistic Effect?
6. Implications for Future Research
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Women’s Health. Available online: https://www.who.int/health-topics/women-s-health (accessed on 23 March 2023).
- O’Neil, A.; Russell, J.D.; Thompson, K.; Martinson, M.L.; Peters, S.A.E. The Impact of Socioeconomic Position (SEP) on Women’s Health over the Lifetime. Maturitas 2020, 140, 1–7. [Google Scholar] [CrossRef]
- Rieder, J.K.; Darabos, K.; Weierich, M.R. Estradiol and Women’s Health: Considering the Role of Estradiol as a Marker in Behavioral Medicine. Int. J. Behav. Med. 2020, 27, 294–304. [Google Scholar] [CrossRef]
- Daan, N.M.P.; Fauser, B.C.J.M. Menopause Prediction and Potential Implications. Maturitas 2015, 82, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Widmer, R.J.; Flammer, A.J.; Lerman, L.O.; Lerman, A. The Mediterranean Diet, Its Components, and Cardiovascular Disease. Am. J. Med. 2015, 128, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Cancer and Mediterranean Diet: A Review. Available online: https://pubmed.ncbi.nlm.nih.gov/31480794/ (accessed on 13 March 2023).
- Esposito, K.; Maiorino, M.I.; Bellastella, G.; Chiodini, P.; Panagiotakos, D.; Giugliano, D. A Journey into a Mediterranean Diet and Type 2 Diabetes: A Systematic Review with Meta-Analyses. BMJ Open 2015, 5, e008222. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. 2000. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 1 March 2023).
- Critical Appraisal Skills Programme CASP (Randomised Controlled Trial) Checklist. Available online: https://casp-uk.net/images/checklist/documents/CASP-Randomised-Controlled-Trial-Checklist/CASP-RCT-Checklist-PDF-Fillable-Form.pdf (accessed on 23 March 2023).
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomised Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Thiyagarajan, D.K.; Basit, H.; Jeanmonod, R. Physiology, Menstrual Cycle; StatPearls Publishing: St. Petersburg, FL, USA, 2021. [Google Scholar]
- Karapanou, O.; Papadimitriou, A. Determinants of Menarche. Reprod. Biol. Endocrinol. 2010, 8, 115. [Google Scholar] [CrossRef] [PubMed]
- Rivas Paz, M.; Torres Mendoza, B.M.; Torres Castillo, N. Age of the Onset of Menarche and Its Complications: A Literature Review. Int. J. Gynecol. Obstet. 2023, 1–12. [Google Scholar] [CrossRef]
- Jung, H.; Sung, Y.-A.; Hong, Y.S.; Song, D.K.; Hong, S.-H.; Lee, H. Relationship between Age at Menarche and Metabolic Diseases in Korean Postmenopausal Women: The Korea National Health and Nutrition Examination Survey 2016–2018. PLoS ONE 2023, 18, e0280929. [Google Scholar] [CrossRef]
- Jeong, S.-M.; Yoo, J.E.; Jeon, K.H.; Han, K.; Lee, H.; Lee, D.-Y.; Shin, D.W. Associations of Reproductive Factors with Incidence of Myocardial Infarction and Ischemic Stroke in Postmenopausal Women: A Cohort Study. BMC Med. 2023, 21, 64. [Google Scholar] [CrossRef]
- Fuhrman, B.J.; Moore, S.C.; Byrne, C.; Makhoul, I.; Kitahara, C.M.; Berrington de González, A.; Linet, M.S.; Weiderpass, E.; Adami, H.-O.; Freedman, N.D.; et al. Association of the Age at Menarche with Site-Specific Cancer Risks in Pooled Data from Nine Cohorts. Cancer Res. 2021, 81, 2246–2255. [Google Scholar] [CrossRef]
- Zhang, Q.; Greenbaum, J.; Zhang, W.-D.; Sun, C.-Q.; Deng, H.-W. Age at Menarche and Osteoporosis: A Mendelian Randomization Study. Bone 2018, 117, 91–97. [Google Scholar] [CrossRef]
- Szamreta, E.A.; Qin, B.; Rivera-Núñez, Z.; Parekh, N.; Barrett, E.S.; Ferrante, J.; Lin, Y.; Bandera, E.V. Greater Adherence to a Mediterranean-like Diet Is Associated with Later Breast Development and Menarche in Peripubertal Girls. Public Health Nutr. 2020, 23, 1020–1030. [Google Scholar] [CrossRef] [PubMed]
- Soriguer, F.J.; Gonzalez-Romero, S.; Esteva, I.; García-arnés, J.A.; Tinahones, F.; de Adana, M.S.R.; Olveira, G.; Mancha, I.; Vazques, F. Does the Intake of Nuts and Seeds Alter the Appearance of Menarche? Acta Obstet. Gynecol. Scand. 1995, 74, 455–461. [Google Scholar] [CrossRef]
- Ramezani Tehrani, F.; Moslehi, N.; Asghari, G.; Gholami, R.; Mirmiran, P.; Azizi, F. Intake of Dairy Products, Calcium, Magnesium, and Phosphorus in Childhood and Age at Menarche in the Tehran Lipid and Glucose Study. PLoS ONE 2013, 8, e57696. [Google Scholar] [CrossRef] [PubMed]
- Jansen, E.C.; Marín, C.; Mora-Plazas, M.; Villamor, E. Higher Childhood Red Meat Intake Frequency Is Associated with Earlier Age at Menarche. J. Nutr. 2015, 146, 792–798. [Google Scholar] [CrossRef] [PubMed]
- Moslehi, N.; Asghari, G.; Mirmiran, P.; Azizi, F. Longitudinal Association of Dietary Sources of Animal and Plant Protein throughout Childhood with Menarche. BMC Pediatr. 2021, 21, 206. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Gu, Q.; Cui, X.; Zhu, Z.; Zang, J.; Wang, Z.; Wu, F.; Shen, X. Higher Poultry Consumption Was Associated with an Earlier Age at Menarche. Acta Paediatr. 2021, 110, 889–895. [Google Scholar] [CrossRef]
- Wiley, A.S. Milk Intake and Total Dairy Consumption: Associations with Early Menarche in NHANES 1999–2004. PLoS ONE 2011, 6, e14685. [Google Scholar] [CrossRef]
- Berrino, F.; Bellati, C.; Secreto, G.; Camerini, E.; Pala, V.; Panico, S.; Allegro, G.; Kaaks, R. Reducing Bioavailable Sex Hormones through a Comprehensive Change in Diet: The Diet and Androgens (DIANA) Randomized Trial. Cancer Epidemiol. Biomark. Prev. 2001, 10, 25–33. [Google Scholar]
- Carruba, G.; Granata, O.M.; Pala, V.; Campisi, I.; Agostara, B.; Cusimano, R.; Ravazzolo, B.; Traina, A. A Traditional Mediterranean Diet Decreases Endogenous Estrogens in Healthy Postmenopausal Women. Nutr. Cancer 2006, 56, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Tosti, V.; Bertozzi, B.; Fontana, L. Health Benefits of the Mediterranean Diet: Metabolic and Molecular Mechanisms. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Bailey, M.A.; Holscher, H.D. Microbiome-Mediated Effects of the Mediterranean Diet on Inflammation. Adv. Nutr. 2018, 9, 193–206. [Google Scholar] [CrossRef]
- Bae, J.; Park, S.; Kwon, J.-W. Factors Associated with Menstrual Cycle Irregularity and Menopause. BMC Women’s Health 2018, 18, 36. [Google Scholar] [CrossRef]
- Onieva-Zafra, M.D.; Fernández-Martínez, E.; Abreu-Sánchez, A.; Iglesias-López, M.T.; García-Padilla, F.M.; Pedregal-González, M.; Parra-Fernández, M.L. Relationship between Diet, Menstrual Pain and Other Menstrual Characteristics among Spanish Students. Nutrients 2020, 12, 1759. [Google Scholar] [CrossRef] [PubMed]
- Santoro, N.; Roeca, C.; Peters, B.A.; Neal-Perry, G. The Menopause Transition: Signs, Symptoms, and Management Options. J. Clin. Endocrinol. Metab. 2021, 106, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Gold, E.B. The Timing of the Age at Which Natural Menopause Occurs. Obstet. Gynecol. Clin. N. Am. 2011, 38, 425–440. [Google Scholar] [CrossRef]
- Sapre, S.; Thakur, R. Lifestyle and Dietary Factors Determine Age at Natural Menopause. J. Midlife Health 2014, 5, 3–5. [Google Scholar] [CrossRef]
- Ceylan, B.; Özerdoğan, N. Factors Affecting Age of Onset of Menopause and Determination of Quality of Life in Menopause. Turk. J. Obs. Gynecol. 2015, 12, 43–49. [Google Scholar] [CrossRef]
- Grisotto, G.; Farago, J.S.; Taneri, P.E.; Wehrli, F.; Roa-Díaz, Z.M.; Minder, B.; Glisic, M.; Gonzalez-Jaramillo, V.; Voortman, T.; Marques-Vidal, P.; et al. Dietary Factors and Onset of Natural Menopause: A Systematic Review and Meta-Analysis. Maturitas 2022, 159, 15–32. [Google Scholar] [CrossRef]
- Nagata, C.; Takatsuka, N.; Kawakami, N.; Shimizu, H. Association of Diet with the Onset of Menopause in Japanese Women. Am. J. Epidemiol. 2000, 152, 863–867. [Google Scholar] [CrossRef] [PubMed]
- Nagel, G.; Altenburg, H.-P.; Nieters, A.; Boffetta, P.; Linseisen, J. Reproductive and Dietary Determinants of the Age at Menopause in EPIC-Heidelberg. Maturitas 2005, 52, 337–347. [Google Scholar] [CrossRef] [PubMed]
- Dorjgochoo, T.; Kallianpur, A.; Gao, Y.-T.; Cai, H.; Yang, G.; Li, H.; Zheng, W.; Shu, X.O. Dietary and Lifestyle Predictors of Age at Natural Menopause and Reproductive Span in the Shanghai Women’s Health Study. Menopause 2008, 15, 924–933. [Google Scholar] [CrossRef] [PubMed]
- Cano, A.; Marshall, S.; Zolfaroli, I.; Bitzer, J.; Ceausu, I.; Chedraui, P.; Durmusoglu, F.; Erkkola, R.; Goulis, D.G.; Hirschberg, A.L.; et al. The Mediterranean Diet and Menopausal Health: An EMAS Position Statement. Maturitas 2020, 139, 90–97. [Google Scholar] [CrossRef]
- Herber-Gast, G.-C.M.; Mishra, G.D. Fruit, Mediterranean-Style, and High-Fat and -Sugar Diets Are Associated with the Risk of Night Sweats and Hot Flushes in Midlife: Results from a Prospective Cohort Study. Am. J. Clin. Nutr. 2013, 97, 1092–1099. [Google Scholar] [CrossRef]
- Flor-Alemany, M.; Marín-Jiménez, N.; Coll-Risco, I.; Aranda, P.; Aparicio, V.A. Influence of Dietary Habits and Mediterranean Diet Adherence on Menopausal Symptoms. The FLAMENCO Project. Menopause 2020, 27, 1015–1021. [Google Scholar] [CrossRef]
- Sayón-Orea, C.; Santiago, S.; Cuervo, M.; Martínez-González, M.A.; Garcia, A.; Martínez, J.A. Adherence to Mediterranean Dietary Pattern and Menopausal Symptoms in Relation to Overweight/Obesity in Spanish Perimenopausal and Postmenopausal Women. Menopause 2015, 22, 750–757. [Google Scholar] [CrossRef]
- Ruiz-Cabello, P.; Coll-Risco, I.; Acosta-Manzano, P.; Borges-Cosic, M.; Gallo-Vallejo, F.J.; Aranda, P.; López-Jurado, M.; Aparicio, V.A. Influence of the Degree of Adherence to the Mediterranean Diet on the Cardiometabolic Risk in Peri and Menopausal Women. The Flamenco Project. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 217–224. [Google Scholar] [CrossRef]
- Walsh, S.; Ismaili, E.; Naheed, B.; O’Brien, S. Diagnosis, Pathophysiology and Management of Premenstrual Syndrome. Obstet. Gynaecol. 2015, 17, 99–104. [Google Scholar] [CrossRef]
- World Health Organization International Classification of Diseases, 11th Revision (ICD-11). Available online: https://icd.who.int/en (accessed on 23 March 2023).
- Ryu, A.; Kim, T.-H. Premenstrual Syndrome: A Mini Review. Maturitas 2015, 82, 436–440. [Google Scholar] [CrossRef]
- Appleton, S.M. Premenstrual Syndrome: Evidence-Based Evaluation and Treatment. Clin. Obstet. Gynecol. 2018, 61, 52. [Google Scholar] [CrossRef]
- Kwon, Y.-J.; Sung, D.-I.; Lee, J.-W. Association among Premenstrual Syndrome, Dietary Patterns, and Adherence to Mediterranean Diet. Nutrients 2022, 14, 2460. [Google Scholar] [CrossRef]
- Andrade, V.; Jorge, R.; García-Conesa, M.-T.; Philippou, E.; Massaro, M.; Chervenkov, M.; Ivanova, T.; Maksimova, V.; Smilkov, K.; Ackova, D.G.; et al. Mediterranean Diet Adherence and Subjective Well-Being in a Sample of Portuguese Adults. Nutrients 2020, 12, 3837. [Google Scholar] [CrossRef] [PubMed]
- Kaluza, J.; Lozynska, K.; Rudzinska, J.; Granda, D.; Sicinska, E.; Szmidt, M.K. Mediterranean-Style Diet and Other Determinants of Well-Being in Omnivorous, Vegetarian, and Vegan Women. Nutrients 2023, 15, 725. [Google Scholar] [CrossRef]
- Lo Moro, G.; Corezzi, M.; Bert, F.; Buda, A.; Gualano, M.R.; Siliquini, R. Mental Health and Adherence to Mediterranean Diet among University Students: An Italian Cross-Sectional Study. J. Am. Coll. Health 2021, 1–11. [Google Scholar] [CrossRef] [PubMed]
- López-Olivares, M.; Mohatar-Barba, M.; Fernández-Gómez, E.; Enrique-Mirón, C. Mediterranean Diet and the Emotional Well-Being of Students of the Campus of Melilla (University of Granada). Nutrients 2020, 12, 1826. [Google Scholar] [CrossRef]
- Western Dietary Pattern Is Related to Premenstrual Syndrome: A Case–Control Study|British Journal of Nutrition|Cambridge Core. Available online: https://www.cambridge.org/core/journals/british-journal-of-nutrition/article/western-dietary-pattern-is-related-to-premenstrual-syndrome-a-casecontrol-study/F2C1436021136BDA3A9CC0968C351E46 (accessed on 13 March 2023).
- Bazyar, H.; Zare Javid, A.; Dasi, E.; Sadeghian, M. Major Dietary Patterns in Relation to Obesity and Quality of Sleep among Female University Students. Clin. Nutr. ESPEN 2020, 39, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Babakhani, K.; Sotoudeh, G.; Siassi, F.; Qorbani, M. Comparison of Vegetable Intake in Nurses with and without Premenstrual Syndrome: A Case-Control Study. Shiraz E-Med. J. 2020, 21, e91319. [Google Scholar] [CrossRef]
- Hashim, M.S.; Obaideen, A.A.; Jahrami, H.A.; Radwan, H.; Hamad, H.J.; Owais, A.A.; Alardah, L.G.; Qiblawi, S.; Al-Yateem, N.; Faris, M.A.-I.E. Premenstrual Syndrome Is Associated with Dietary and Lifestyle Behaviors among University Students: A Cross-Sectional Study from Sharjah, UAE. Nutrients 2019, 11, 1939. [Google Scholar] [CrossRef] [PubMed]
- Takeda, T.; Imoto, Y.; Nagasawa, H.; Takeshita, A.; Shiina, M. Fish Consumption and Premenstrual Syndrome and Dysphoric Disorder in Japanese Collegiate Athletes. J. Pediatr. Adolesc. Gynecol. 2016, 29, 386–389. [Google Scholar] [CrossRef]
- Mohammadi, M.M.; Dehghan Nayeri, N.; Mashhadi, M.; Varaei, S. Effect of Omega-3 Fatty Acids on Premenstrual Syndrome: A Systematic Review and Meta-Analysis. J. Obs. Gynaecol. Res. 2022, 48, 1293–1305. [Google Scholar] [CrossRef]
- Iacovides, S.; Avidon, I.; Baker, F.C. What We Know about Primary Dysmenorrhea Today: A Critical Review. Hum. Reprod. Update 2015, 21, 762–778. [Google Scholar] [CrossRef]
- Ferries-Rowe, E.; Corey, E.; Archer, J.S. Primary Dysmenorrhea: Diagnosis and Therapy. Obs. Gynecol. 2020, 136, 1047–1058. [Google Scholar] [CrossRef]
- Bajalan, Z.; Alimoradi, Z.; Moafi, F. Nutrition as a Potential Factor of Primary Dysmenorrhea: A Systematic Review of Observational Studies. Gynecol. Obstet. Investig. 2019, 84, 209–224. [Google Scholar] [CrossRef]
- Barcikowska, Z.; Wójcik-Bilkiewicz, K.; Sobierajska-Rek, A.; Grzybowska, M.E.; Wąż, P.; Zorena, K. Dysmenorrhea and Associated Factors among Polish Women: A Cross-Sectional Study. Pain Res. Manag. 2020, 2020, 6161536. [Google Scholar] [CrossRef]
- Tavallaee, M.; Joffres, M.R.; Corber, S.J.; Bayanzadeh, M.; Rad, M.M. The Prevalence of Menstrual Pain and Associated Risk Factors among Iranian Women. J. Obstet. Gynaecol. Res. 2011, 37, 442–451. [Google Scholar] [CrossRef]
- Zeru, A.B.; Muluneh, M.A. Thyme Tea and Primary Dysmenorrhea among Young Female Students. Adolesc. Health Med. Ther. 2020, 11, 147–155. [Google Scholar] [CrossRef]
- World Health Organization. Defining Sexual Health: Report of a Technical Consultation on Sexual Health, 28–31 January 2002; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Laumann, E.O.; Paik, A.; Rosen, R.C. Sexual Dysfunction in the United States: Prevalence and Predictors. J. Am. Med. Assoc. 1999, 281, 537–544. [Google Scholar] [CrossRef]
- Laumann, E.O.; Nicolosi, A.; Glasser, D.B.; Paik, A.; Gingell, C.; Moreira, E.; Wang, T.; GSSAB Investigators’ Group. Sexual Problems among Women and Men Aged 40–80 y: Prevalence and Correlates Identified in the Global Study of Sexual Attitudes and Behaviors. Int. J. Impot. Res. 2005, 17, 39–57. [Google Scholar] [CrossRef]
- Brotto, L.; Atallah, S.; Johnson-Agbakwu, C.; Rosenbaum, T.; Abdo, C.; Byers, E.S.; Graham, C.; Nobre, P.; Wylie, K. Psychological and Interpersonal Dimensions of Sexual Function and Dysfunction. J. Sex. Med. 2016, 13, 538–571. [Google Scholar] [CrossRef]
- Towe, M.; La, J.; El-Khatib, F.; Roberts, N.; Yafi, F.A.; Rubin, R. Diet and Female Sexual Health. Sex. Med. Rev. 2020, 8, 256–264. [Google Scholar] [CrossRef]
- Rosen, C.; Brown, J.; Heiman, S.; Leib, R. The Female Sexual Function Index (FSFI): A Multidimensional Self-Report Instrument for the Assessment of Female Sexual Function. J. Sex. Marital. Ther. 2000, 26, 191–208. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Giugliano, D. Obesity, the Metabolic Syndrome, and Sexual Dysfunction. Int. J. Impot. Res. 2005, 17, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Doumas, M.; Tsiodras, S.; Tsakiris, A.; Douma, S.; Chounta, A.; Papadopoulos, A.; Kanellakopoulou, K.; Giamarellou, H. Female Sexual Dysfunction in Essential Hypertension: A Common Problem Being Uncovered. J. Hypertens. 2006, 24, 2387–2392. [Google Scholar] [CrossRef] [PubMed]
- Salonia, A.; Lanzi, R.; Scavini, M.; Pontillo, M.; Gatti, E.; Petrella, G.; Licata, G.; Nappi, R.E.; Bosi, E.; Briganti, A.; et al. Sexual Function and Endocrine Profile in Fertile Women with Type 1 Diabetes. Diabetes Care 2006, 29, 312–316. [Google Scholar] [CrossRef]
- Schulster, M.L.; Liang, S.E.; Najari, B.B. Metabolic Syndrome and Sexual Dysfunction. Curr. Opin. Urol. 2017, 27, 435–440. [Google Scholar] [CrossRef]
- Esposito, K.; Ciotola, M.; Marfella, R.; Di Tommaso, D.; Cobellis, L.; Giugliano, D. The Metabolic Syndrome: A Cause of Sexual Dysfunction in Women. Int. J. Impot. Res. 2005, 17, 224–226. [Google Scholar] [CrossRef]
- Esposito, K.; Ciotola, M.; Giugliano, F.; Schisano, B.; Autorino, R.; Iuliano, S.; Vietri, M.T.; Cioffi, M.; De Sio, M.; Giugliano, D. Mediterranean Diet Improves Sexual Function in Women with the Metabolic Syndrome. Int. J. Impot. Res. 2007, 19, 486–491. [Google Scholar] [CrossRef] [PubMed]
- Maiorino, M.I.; Bellastella, G.; Caputo, M.; Castaldo, F.; Improta, M.R.; Giugliano, D.; Esposito, K. Effects of Mediterranean Diet on Sexual Function in People with Newly Diagnosed Type 2 Diabetes: The MÈDITA Trial. J. Diabetes Its Complicat. 2016, 30, 1519–1524. [Google Scholar] [CrossRef]
- Giugliano, F.; Maiorino, M.I.; Di Palo, C.; Autorino, R.; De Sio, M.; Giugliano, D.; Esposito, K. Adherence to Mediterranean Diet and Sexual Function in Women with Type 2 Diabetes. J. Sex. Med. 2010, 7, 1883–1890. [Google Scholar] [CrossRef]
- Clark, J.S.; Dyer, K.A.; Davis, C.R.; Shivappa, N.; Hébert, J.R.; Woodman, R.; Hodgson, J.M.; Murphy, K.J. Adherence to a Mediterranean Diet for 6 Months Improves the Dietary Inflammatory Index in a Western Population: Results from the MedLey Study. Nutrients 2023, 15, 366. [Google Scholar] [CrossRef]
- Zondervan, K.T.; Becker, C.M.; Missmer, S.A. Endometriosis. N. Engl. J. Med. 2020, 382, 1244–1256. [Google Scholar] [CrossRef]
- Smolarz, B.; Szyłło, K.; Romanowicz, H. Endometriosis: Epidemiology, Classification, Pathogenesis, Treatment and Genetics (Review of Literature). IJMS 2021, 22, 10554. [Google Scholar] [CrossRef]
- Afrin, S.; AlAshqar, A.; El Sabeh, M.; Miyashita-Ishiwata, M.; Reschke, L.; Brennan, J.T.; Fader, A.; Borahay, M.A. Diet and Nutrition in Gynecological Disorders: A Focus on Clinical Studies. Nutrients 2021, 13, 1747. [Google Scholar] [CrossRef]
- Ott, J.; Nouri, K.; Hrebacka, D.; Gutschelhofer, S.; Huber, J.C.; Wenzl, R. Endometriosis and Nutrition-Recommending a Mediterranean Diet Decreases Endometriosis-Associated Pain: An Experimental Observational Study. J. Aging Res. Clin. Pract. 2012, 1, 162–166. [Google Scholar]
- Lizneva, D.; Suturina, L.; Walker, W.; Brakta, S.; Gavrilova-Jordan, L.; Azziz, R. Criteria, Prevalence, and Phenotypes of Polycystic Ovary Syndrome. Fertil. Steril. 2016, 106, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Moran, L.; Grieger, J.; Mishra, G.; Teede, H. The Association of a Mediterranean-Style Diet Pattern with Polycystic Ovary Syndrome Status in a Community Cohort Study. Nutrients 2015, 7, 8553–8564. [Google Scholar] [CrossRef] [PubMed]
- Teede, H.J.; Joham, A.E.; Paul, E.; Moran, L.J.; Loxton, D.; Jolley, D.; Lombard, C. Longitudinal Weight Gain in Women Identified with Polycystic Ovary Syndrome: Results of an Observational Study in Young Women: Weight Gain and BMI in PCOS. Obesity 2013, 21, 1526–1532. [Google Scholar] [CrossRef]
- Cincione, I.R.; Graziadio, C.; Marino, F.; Vetrani, C.; Losavio, F.; Savastano, S.; Colao, A.; Laudisio, D. Short-Time Effects of Ketogenic Diet or Modestly Hypocaloric Mediterranean Diet on Overweight and Obese Women with Polycystic Ovary Syndrome. J. Endocrinol. Investig. 2022, 46, 769–777. [Google Scholar] [CrossRef] [PubMed]
- Mei, S.; Ding, J.; Wang, K.; Ni, Z.; Yu, J. Mediterranean Diet Combined with a Low-Carbohydrate Dietary Pattern in the Treatment of Overweight Polycystic Ovary Syndrome Patients. Front. Nutr. 2022, 9, 876620. [Google Scholar] [CrossRef]
- Wang, Q.; Sun, Y.; Xu, Q.; Liu, W.; Wang, P.; Yao, J.; Zhao, A.; Chen, Y.; Wang, W. Higher Dietary Inflammation Potential and Certain Dietary Patterns Are Associated with Polycystic Ovary Syndrome Risk in China: A Case-Control Study. Nutr. Res. 2022, 100, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Cutillas-Tolín, A.; Arense-Gonzalo, J.J.; Mendiola, J.; Adoamnei, E.; Navarro-Lafuente, F.; Sánchez-Ferrer, M.L.; Prieto-Sánchez, M.T.; Carmona-Barnosi, A.; Vioque, J.; Torres-Cantero, A.M. Are Dietary Indices Associated with Polycystic Ovary Syndrome and Its Phenotypes? A Preliminary Study. Nutrients 2021, 13, 313. [Google Scholar] [CrossRef] [PubMed]
- Barrea, L.; Arnone, A.; Annunziata, G.; Muscogiuri, G.; Laudisio, D.; Salzano, C.; Pugliese, G.; Colao, A.; Savastano, S. Adherence to the Mediterranean Diet, Dietary Patterns and Body Composition in Women with Polycystic Ovary Syndrome (PCOS). Nutrients 2019, 11, 2278. [Google Scholar] [CrossRef]
- Barrea, L.; Muscogiuri, G.; Pugliese, G.; de Alteriis, G.; Colao, A.; Savastano, S. Metabolically Healthy Obesity (MHO) vs. Metabolically Unhealthy Obesity (MUO) Phenotypes in PCOS: Association with Endocrine-Metabolic Profile, Adherence to the Mediterranean Diet, and Body Composition. Nutrients 2021, 13, 3925. [Google Scholar] [CrossRef]
- Che, X.; Chen, Z.; Liu, M.; Mo, Z. Dietary Interventions: A Promising Treatment for Polycystic Ovary Syndrome. Ann. Nutr. Metab. 2021, 77, 313–323. [Google Scholar] [CrossRef]
- Çıtar Dazıroğlu, M.E.; Acar Tek, N. The Effect on Inflammation of Adherence to the Mediterranean Diet in Polycystic Ovary Syndrome. Curr. Nutr. Rep. 2023, 12, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Mulgund, A.; Hamada, A.; Chyatte, M.R. A Unique View on Male Infertility around the Globe. Reprod. Biol. Endocrinol. 2015, 13, 37. [Google Scholar] [CrossRef]
- GBD 2015 Risk Factors Collaborators. Global, Regional, and National Comparative Risk Assessment of 79 Behavioural, Environmental and Occupational, and Metabolic Risks or Clusters of Risks, 1990–2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. [Google Scholar] [CrossRef]
- Grammatikos, A.; Johnston, S.; Rice, C.M.; Gompels, M. A Family with a Novel CTLA4 Haploinsufficiency Mutation and Neurological Symptoms. J. Clin. Immunol. 2021, 41, 1411–1416. [Google Scholar] [CrossRef]
- Muffone, A.R.M.C.; de Oliveira Lübke, P.D.P.; Rabito, E.I. Mediterranean Diet and Infertility: A Systematic Review with Meta-Analysis of Cohort Studies. Nutr. Rev. 2022, nuac087. [Google Scholar] [CrossRef]
- Rossi, B.V.; Abusief, M.; Missmer, S.A. Modifiable Risk Factors and Infertility: What Are the Connections? Am. J. Lifestyle Med. 2016, 10, 220–231. [Google Scholar] [CrossRef]
- Silvestris, E.; de Pergola, G.; Rosania, R.; Loverro, G. Obesity as Disruptor of the Female Fertility. Reprod. Biol. Endocrinol. 2018, 16, 22. [Google Scholar] [CrossRef]
- Cohen, N.J.; Yao, M.; Midya, V.; India-Aldana, S.; Mouzica, T.; Andra, S.S.; Narasimhan, S.; Meher, A.K.; Arora, M.; Chan, J.K.Y.; et al. Exposure to Perfluoroalkyl Substances and Women’s Fertility Outcomes in a Singaporean Population-Based Preconception Cohort. Sci. Total Environ. 2023, 873, 162267. [Google Scholar] [CrossRef]
- Al-Gubory, K.H.; Fowler, P.A.; Garrel, C. The Roles of Cellular Reactive Oxygen Species, Oxidative Stress and Antioxidants in Pregnancy Outcomes. Int. J. Biochem. Cell. Biol. 2010, 42, 1634–1650. [Google Scholar] [CrossRef]
- Zabaleta, M.E. Mediterranean Diet: Woman Fertility and Pregnancy. Mediterr. J. Nutr. Metab. 2020, 13, 101–111. [Google Scholar] [CrossRef]
- Ly, C.; Yockell-Lelièvre, J.; Ferraro, Z.M.; Arnason, J.T.; Ferrier, J.; Gruslin, A. The Effects of Dietary Polyphenols on Reproductive Health and Early Development. Hum. Reprod. Update 2015, 21, 228–248. [Google Scholar] [CrossRef] [PubMed]
- Madej, D.; Granda, D.; Sicinska, E.; Kaluza, J. Influence of Fruit and Vegetable Consumption on Antioxidant Status and Semen Quality: A Cross-Sectional Study in Adult Men. Front. Nutr. 2021, 8, 753843. [Google Scholar] [CrossRef]
- Sun, H.; Lin, Y.; Lin, D.; Zou, C.; Zou, X.; Fu, L.; Meng, F.; Qian, W. Mediterranean Diet Improves Embryo Yield in IVF: A Prospective Cohort Study. Reprod. Biol. Endocrinol. 2019, 17, 73. [Google Scholar] [CrossRef] [PubMed]
- Karayiannis, D.; Kontogianni, M.D.; Mendorou, C.; Mastrominas, M.; Yiannakouris, N. Adherence to the Mediterranean Diet and IVF Success Rate among Non-Obese Women Attempting Fertility. Hum. Reprod. 2018, 33, 494–502. [Google Scholar] [CrossRef]
- Gaskins, A.J.; Nassan, F.L.; Chiu, Y.-H.; Arvizu, M.; Williams, P.L.; Keller, M.G.; Souter, I.; Hauser, R.; Chavarro, J.E. Dietary Patterns and Outcomes of Assisted Reproduction. Am. J. Obstet. Gynecol. 2019, 220, 567.e1–567.e18. [Google Scholar] [CrossRef]
- Ricci, E.; Bravi, F.; Noli, S.; Somigliana, E.; Cipriani, S.; Castiglioni, M.; Chiaffarino, F.; Vignali, M.; Gallotti, B.; Parazzini, F. Mediterranean Diet and Outcomes of Assisted Reproduction: An Italian Cohort Study. Am. J. Obstet. Gynecol. 2019, 221, 627.e1–627.e14. [Google Scholar] [CrossRef] [PubMed]
- Gaskins, A.J.; Rich-Edwards, J.W.; Hauser, R.; Williams, P.L.; Gillman, M.W.; Penzias, A.; Missmer, S.A.; Chavarro, J.E. Prepregnancy Dietary Patterns and Risk of Pregnancy Loss. Am. J. Clin. Nutr. 2014, 100, 1166–1172. [Google Scholar] [CrossRef] [PubMed]
- Vujkovic, M.; de Vries, J.H.; Lindemans, J.; Macklon, N.S.; van der Spek, P.J.; Steegers, E.A.P.; Steegers-Theunissen, R.P.M. The Preconception Mediterranean Dietary Pattern in Couples Undergoing In Vitro Fertilization/Intracytoplasmic Sperm Injection Treatment Increases the Chance of Pregnancy. Fertil. Steril. 2010, 94, 2096–2101. [Google Scholar] [CrossRef] [PubMed]
- Saura-Calixto, F. Dietary Fiber as a Carrier of Dietary Antioxidants: An Essential Physiological Function. J. Agric. Food Chem. 2011, 59, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Ghamari, K.; Kashani, L.; Jafarinia, M.; Tadayon Najafabadi, B.; Shokraee, K.; Esalatmanesh, S.; Akhondzadeh, S. Vitamin E and Ginseng Supplementation to Enhance Female Sexual Function: A Randomized, Double-Blind, Placebo-Controlled, Clinical Trial. Women Health 2020, 60, 1164–1173. [Google Scholar] [CrossRef] [PubMed]
- Szmidt, M.K.; Granda, D.; Sicinska, E.; Kaluza, J. Primary Dysmenorrhea in Relation to Oxidative Stress and Antioxidant Status: A Systematic Review of Case-Control Studies. Antioxidants 2020, 9, 994. [Google Scholar] [CrossRef]
- Amini, L.; Chekini, R.; Nateghi, M.R.; Haghani, H.; Jamialahmadi, T.; Sathyapalan, T.; Sahebkar, A. The Effect of Combined Vitamin C and Vitamin e Supplementation on Oxidative Stress Markers in Women with Endometriosis: A Randomized, Triple-Blind Placebo-Controlled Clinical Trial. Pain Res. Manag. 2021, 2021, 1–6. [Google Scholar] [CrossRef]
- Alikamali, M.; Mohammad-Alizadeh-Charandabi, S.; Maghalian, M.; Mirghafourvand, M. The Effects of Vitamin E on the Intensity of Primary Dysmenorrhea: A Systematic Review and Meta-Analysis. Clin. Nutr. ESPEN 2022, 52, 50–59. [Google Scholar] [CrossRef]
- Gaskins, A.J.; Mumford, S.L.; Rovner, A.J.; Zhang, C.; Chen, L.; Wactawski-Wende, J.; Perkins, N.J.; Schisterman, E.F. BioCycle Study Group Whole Grains Are Associated with Serum Concentrations of High Sensitivity C-Reactive Protein among Premenopausal Women. J. Nutr. 2010, 140, 1669–1676. [Google Scholar] [CrossRef]
- Liang, Z.; Di, N.; Li, L.; Yang, D. Gut Microbiota Alterations Reveal Potential Gut-Brain Axis Changes in Polycystic Ovary Syndrome. J. Endocrinol. Investig. 2021, 44, 1727–1737. [Google Scholar] [CrossRef] [PubMed]
- Rudnicka, E.; Suchta, K.; Grymowicz, M.; Calik-Ksepka, A.; Smolarczyk, K.; Duszewska, A.M.; Smolarczyk, R.; Meczekalski, B. Chronic Low Grade Inflammation in Pathogenesis of PCOS. Int. J. Mol. Sci. 2021, 22, 3789. [Google Scholar] [CrossRef] [PubMed]
- Granda, D.; Szmidt, M.K.; Kaluza, J. Is Premenstrual Syndrome Associated with Inflammation, Oxidative Stress and Antioxidant Status? A Systematic Review of Case–Control and Cross-Sectional Studies. Antioxidants 2021, 10, 604. [Google Scholar] [CrossRef]
- Wang, X.; Xu, T.; Liu, R.; Wu, G.; Gu, L.; Zhang, Y.; Zhang, F.; Fu, H.; Ling, Y.; Wei, X.; et al. High-Fiber Diet or Combined with Acarbose Alleviates Heterogeneous Phenotypes of Polycystic Ovary Syndrome by Regulating Gut Microbiota. Front. Endocrinol. 2022, 12, 806331. [Google Scholar] [CrossRef]
- De Cosmi, V.; Cipriani, S.; Parazzini, F.; Ricci, E.; Esposito, G.; Noli, S.; Somigliana, E.; Agostoni, C. Fatty Acids Intake and Outcomes of Assisted Reproduction in Women Referring to an Italian Fertility Service: Cross-Sectional Analysis of a Prospective Cohort Study. J. Hum. Nutr. Diet. 2022, 35, 833–844. [Google Scholar] [CrossRef] [PubMed]
- Szczuko, M.; Kikut, J.; Szczuko, U.; Szydłowska, I.; Nawrocka-Rutkowska, J.; Ziętek, M.; Verbanac, D.; Saso, L. Nutrition Strategy and Life Style in Polycystic Ovary Syndrome—Narrative Review. Nutrients 2021, 13, 2452. [Google Scholar] [CrossRef]
- Corella, D.; Coltell, O.; Macian, F.; Ordovás, J.M. Advances in Understanding the Molecular Basis of the Mediterranean Diet Effect. Annu. Rev. Food Sci. Technol. 2018, 9, 227–249. [Google Scholar] [CrossRef] [PubMed]
- Divella, R.; Daniele, A.; Savino, E.; Paradiso, A. Anticancer Effects of Nutraceuticals in the Mediterranean Diet: An Epigenetic Diet Model. Cancer Genom. Proteom. 2020, 17, 335–350. [Google Scholar] [CrossRef] [PubMed]
- Bakrim, S.; Aboulaghras, S.; Aanniz, T.; Benali, T.; El Omari, N.; El-Shazly, M.; Lee, L.-H.; Mustafa, S.K.; Sahib, N.; Rebezov, M.; et al. Effects of Mediterranean Diets and Nutrigenomics on Cardiovascular Health. Crit. Rev. Food Sci. Nutr. 2023, 1–20. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szmidt, M.K.; Granda, D.; Madej, D.; Sicinska, E.; Kaluza, J. Adherence to the Mediterranean Diet in Women and Reproductive Health across the Lifespan: A Narrative Review. Nutrients 2023, 15, 2131. https://doi.org/10.3390/nu15092131
Szmidt MK, Granda D, Madej D, Sicinska E, Kaluza J. Adherence to the Mediterranean Diet in Women and Reproductive Health across the Lifespan: A Narrative Review. Nutrients. 2023; 15(9):2131. https://doi.org/10.3390/nu15092131
Chicago/Turabian StyleSzmidt, Maria Karolina, Dominika Granda, Dawid Madej, Ewa Sicinska, and Joanna Kaluza. 2023. "Adherence to the Mediterranean Diet in Women and Reproductive Health across the Lifespan: A Narrative Review" Nutrients 15, no. 9: 2131. https://doi.org/10.3390/nu15092131
APA StyleSzmidt, M. K., Granda, D., Madej, D., Sicinska, E., & Kaluza, J. (2023). Adherence to the Mediterranean Diet in Women and Reproductive Health across the Lifespan: A Narrative Review. Nutrients, 15(9), 2131. https://doi.org/10.3390/nu15092131









