HMC Ameliorates Hyperglycemia via Acting PI3K/AKT Pathway and Improving FOXO1 Pathway in ob/ob Mice
Abstract
1. Introduction
2. Materials and Methods
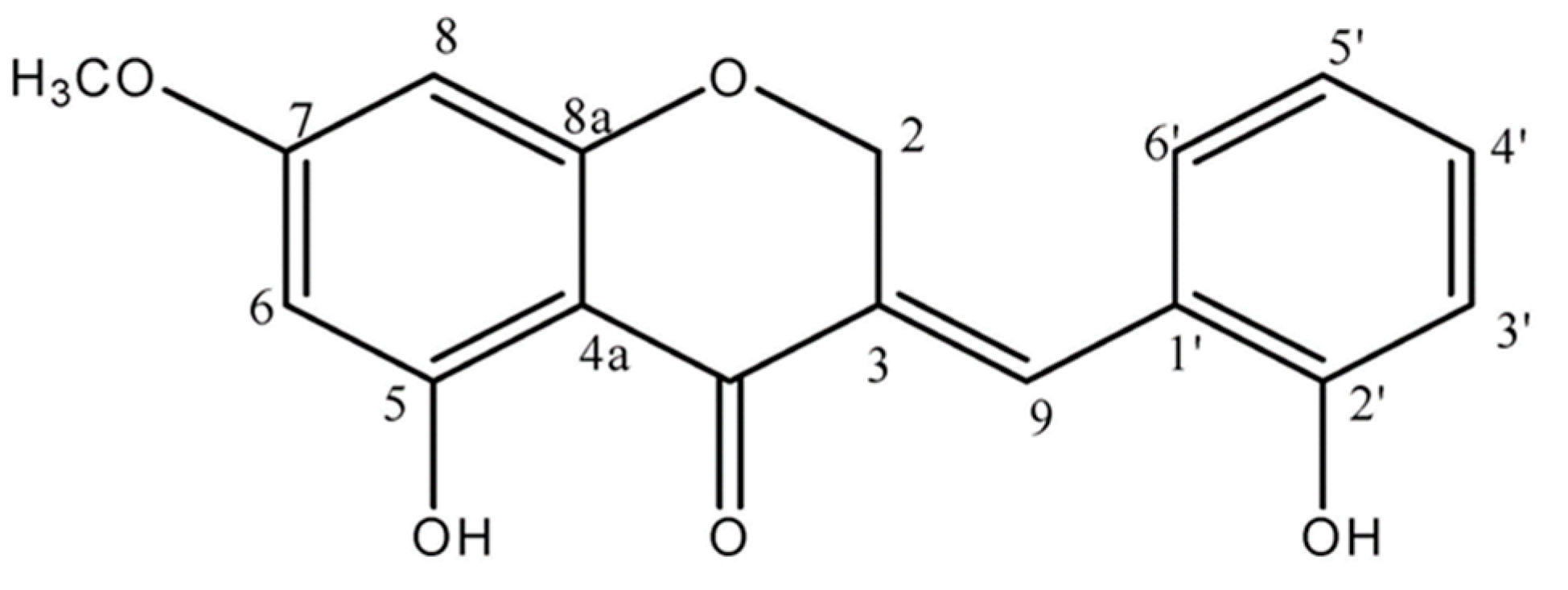
2.1. Preparation of Material
2.2. Animals
2.3. Plasma and Tissue Collection
2.4. Western Blot Analysis
2.5. Isolation of PMs from Skeletal Muscle
2.6. Blood Glucose and Glycosylated Hemoglobin
2.7. Plasma Insulin Level
2.8. HOMA-IR
2.9. Statistical Analyses
3. Results
3.1. Body Weight and Intake
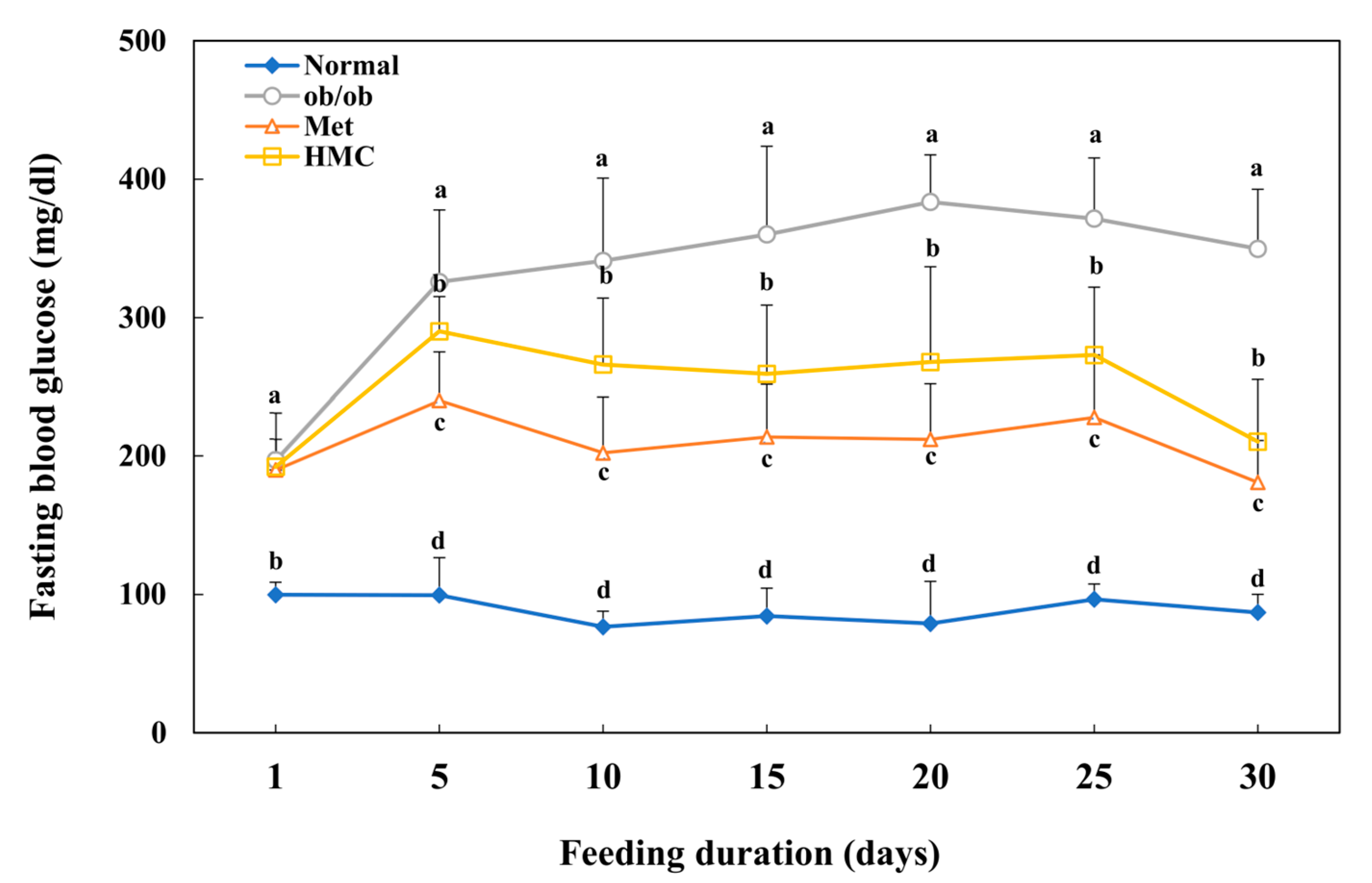
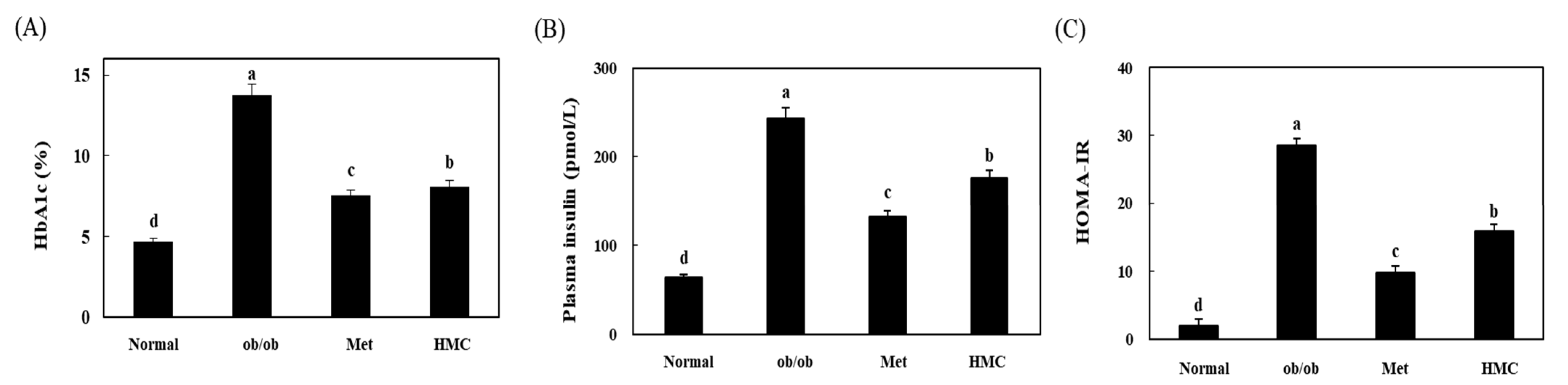
3.2. Blood Glucose and HbAlc Levels
3.3. Insulin Levels
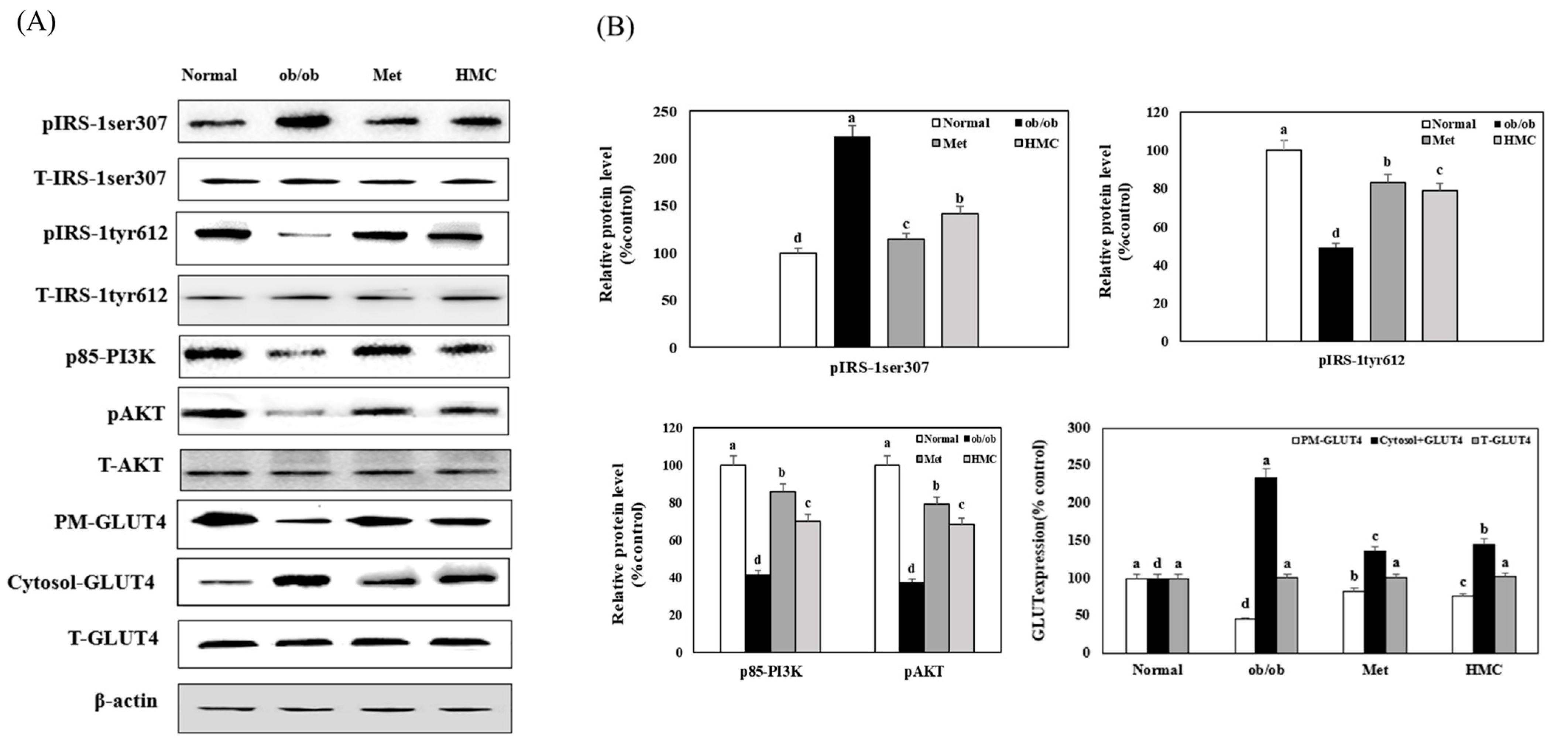
3.4. Expression of IRS-1, PI3K, AKT and PM-GLUT4
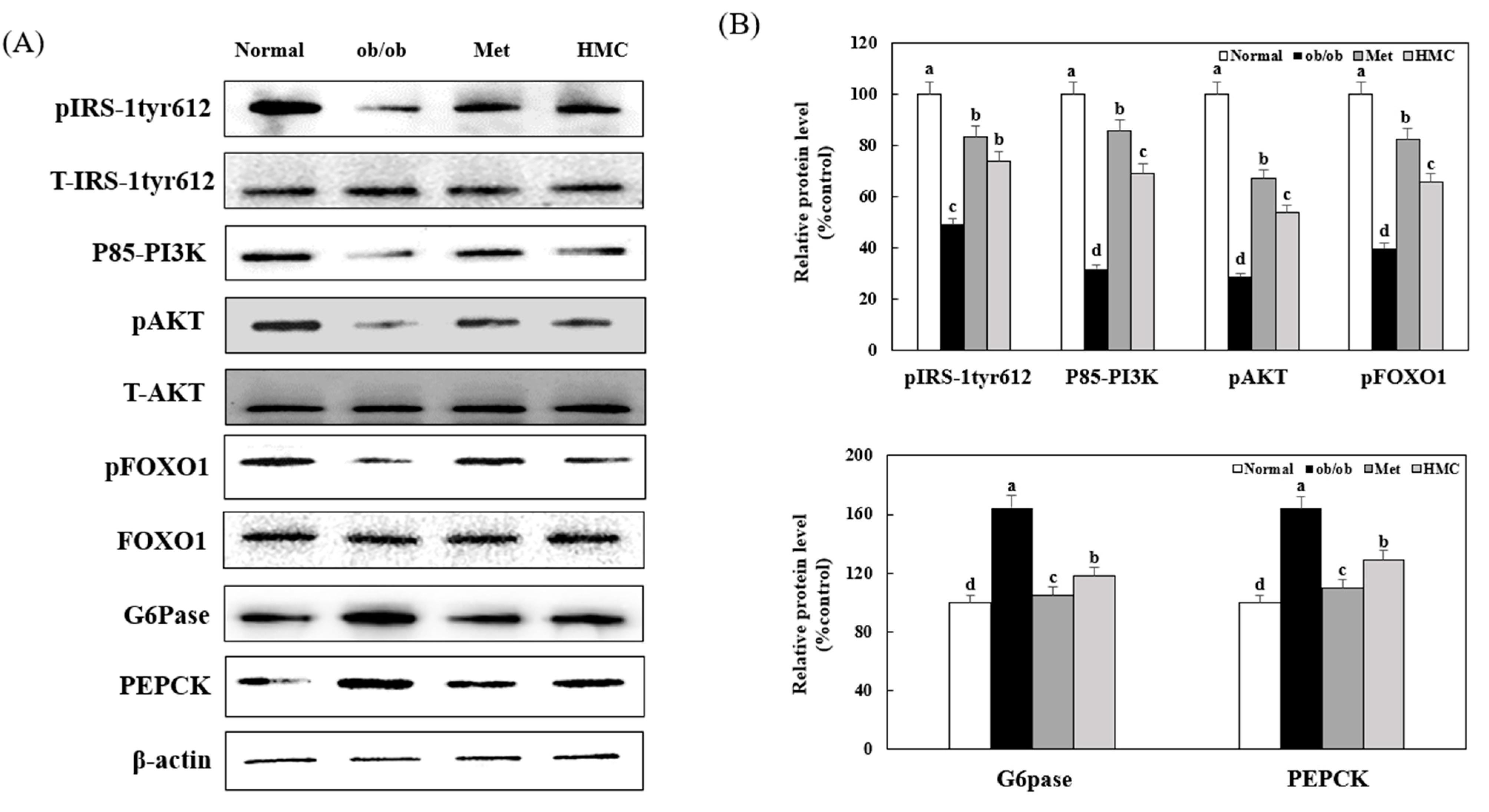
3.5. Expression of AKT, FOXO1, G6pase, and PEPCK
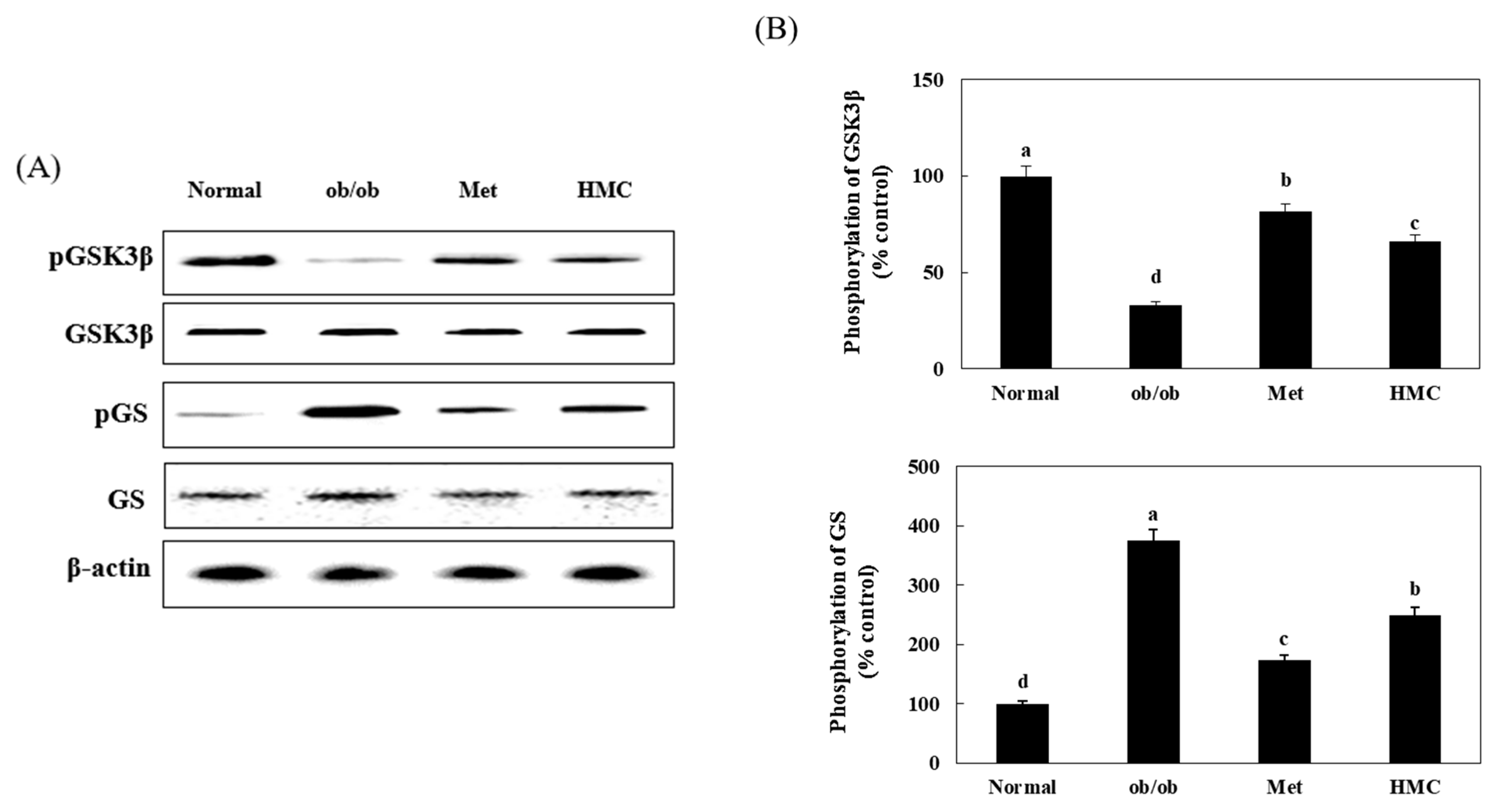
3.6. Expression of GSK3β and GS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cheong, S.H.; Furuhashi, K.; Ito, K.; Nagaoka, M.; Yonezawa, T.; Miura, Y.; Yagasaki, K. Antihyperglycemic effect of equol, a daidzein derivative, in cultured L6 myocytes and ob/ob mice. Mol. Nutr. Food Res. 2014, 58, 267–277. [Google Scholar] [CrossRef]
- Fadini, G.P.; Miorin, M.; Facco, M.; Bonamico, S.; Baesso, I.; Grego, F.; Menegolo, M.; de Kreutzenberg, S.V.; Tiengo, A.; Agostini, C.; et al. Circu-lating endothelial progenitor cells are reduced in peripheralvascular complications of type 2 diabetes mellitus. J. Am. Coll. Cardiol. 2005, 45, 1449–1457. [Google Scholar] [CrossRef] [PubMed]
- He, L.; Sabet, A.; Djedjos, S.; Miller, R.; Sun, X.; Hussain, M.A.; Radovick, S.; Wondisford, F.E. Metformin andinsulin suppress hepatic gluconeogenesis through phospho-rylation of CREB binding protein. Cell 2009, 137, 635–646. [Google Scholar] [CrossRef] [PubMed]
- Kurosaki, E.; Nakano, R.; Momose, K.; Shimaya, A.; Suzuki, T.; Shibasaki, M.; Shikama, H. Hy-poglycemic agent YM440 suppresses hepatic glucose outputvia gluconeogenesis by reducing glucose-6-phosphatase ac-tivity in obese Zucker rats. Eur. J. Pharmacol. 2003, 468, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Dohm, G.L.; Tapscott, E.B.; Pories, W.J.; Dabbs, D.J.; Flickinger, E.G.; Meelheim, D.; Fushiki, T.; Atkinson, S.M.; Elton, C.W.; Caro, J.F. An in vitro human muscle preparation suitable for metabolicstudies. Decreased insulin stimulation of glucose transportin muscle from morbidly obese and diabetic subjects. J. Clin. Investig. 1988, 82, 486–494. [Google Scholar] [CrossRef] [PubMed]
- DeFronzo, R.A.; Bonadonna, R.C.; Ferrannini, E. Pathogen-esis of NIDDM. A balanced overview. Diabetes Care 1992, 15, 318–368. [Google Scholar] [CrossRef]
- Xie, Y.; Shi, X.; Sheng, K.; Han, G.; Li, W.; Zhao, Q.; Jiang, B.; Feng, J.; Li, J.; Gu, Y. PI3K/Akt signaling transduction pathway, erythropoiesis and glycolysis in hypoxia. Mol. Med. Rep. 2018, 19, 783–791. [Google Scholar] [CrossRef]
- Zhu, Y.; Zhang, H.; Wei, Y.; Cai, M.; Gu, R.; Wang, Y.; Ma, Y.; Chen, L. Pea-derived peptides, VLP, LLP, VA, and LL, improve insulin resistance in HepG2 cells via activating IRS-1/PI3K/AKT and blocking ROS-mediated p38MAPK signaling. J. Food Biochem. 2020, 44, 13454. [Google Scholar] [CrossRef]
- Yan, F.; Dai, G.; Zheng, X. Mulberry anthocyanin extract ameliorates insulin resistance by regulating PI3K/AKT pathway in HepG2 cells and db/db mice. J. Nutr. Biochem. 2016, 36, 68–80. [Google Scholar] [CrossRef]
- Cui, X.; Qian, D.-W.; Jiang, S.; Shang, E.-X.; Zhu, Z.-H.; Duan, J.-A. Scutellariae Radix and Coptidis Rhizoma Improve Glucose and Lipid Metabolism in T2DM Rats via Regulation of the Metabolic Profiling and MAPK/PI3K/Akt Signaling Pathway. Int. J. Mol. Sci. 2018, 19, 3634. [Google Scholar] [CrossRef]
- Guo, S. Molecular basis of insulin resistance: The role of IRS and Foxo1 in the control of diabetes mellitus and its complications. Drug Discov. Today Dis. Mech. 2013, 10, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Guo, S. Insulin signaling, resistance, and the metabolic syndrome: Insights from mouse models into disease mechanisms. J. Endocrinol. 2014, 220, T1–T23. [Google Scholar] [CrossRef] [PubMed]
- Cordero-Herrera, I.; Martin, M.A.; Goya, L.; Ramos, S. Cocoa flavonoids attenuate high glucose-induced insulin signalling blockade and modulate glucose uptake and production in human HepG2 cells. Food Chem. Toxicol. 2014, 64, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Barthel, A.; Schmoll, D. Novel concepts in insulin regulation of hepatic gluconeogenesis. Am. J. Physiol. Endocrinol. Metab. 2003, 285, 685–692. [Google Scholar] [CrossRef]
- Matsumoto, M.; Pocai, A.; Rossetti, L.; Depinho, R.A.; Accili, D. Impaired Regulation of Hepatic Glucose Production in Mice Lacking the Forkhead Transcription Factor Foxo1 in Liver. Cell Metab. 2007, 6, 208–216. [Google Scholar] [CrossRef]
- Tsuzuki, K.; Itoh, Y.; Inoue, Y.; Hayashi, H. TRB1 negatively regulates gluconeogenesis by suppressingthe transcriptional activity of FOXO1. FEBS Lett. 2019, 593, 369–380. [Google Scholar] [CrossRef]
- MacAulay, K.; Doble, B.W.; Patel, S.; Hansotia, T.; Sinclair, E.M.; Drucker, D.J.; Nagy, A.; Woodgett, J.R. Glycogen synthase kinase 3alpha-specific regulation of murine hepatic glycogen metabolism. Cell Metab. 2007, 6, 329–337. [Google Scholar] [CrossRef]
- Sajan, M.P.; Ivey, R.A.; Lee, M.C.; Farese, R.V. Hepatic insulin resistance in ob/ob mice involves increases in ceramide, aPKC activity, and selective impairment of Akt-dependent FoxO1 phosphorylation. J. Lipid Res. 2015, 56, 70–80. [Google Scholar] [CrossRef]
- Park, M.-H.; Kang, J.-H.; Kim, H.-J.; Han, J.-S. Gelidium amansii ethanol extract suppresses fat accumulation by down-regulating adipogenic transcription factors in ob/ob mice model. Food Sci. Biotechnol. 2017, 26, 207–212. [Google Scholar] [CrossRef]
- Park, J.E.; Seo, Y.; Han, J.S. HM-Chromanone Isolated from Portulaca Oleracea L. Protects INS-1 Pancreatic β Cells against Glucotoxicity-Induced Apoptosis. Nutrients 2019, 11, 404. [Google Scholar]
- Park, J.E.; Park, J.Y.; Seo, Y.; Han, J.S. A new chromanone isolated from Portulaca oleracea L. increases glucose uptake by stimulating GLUT4 translocation to the plasma membrane in 3T3-L1 adipocytes. Int. J. Biol. Macromol. 2018, 123, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Park, J.E.; Seo, Y.; Han, J.S. HM-chromanone, a component of Portulaca oleracea L., stimulates glucose uptake and glycogen synthesis in skeletal muscle cell. Phytomedicine 2021, 83, 153473. [Google Scholar] [CrossRef] [PubMed]
- Je, J.Y.; Park, J.E.; Seo, Y.; Han, J.S. HM-chromanone inhibits adipogenesis by regulating adipogenic transcription factors and AMPK in 3T3-L1 adipocytes. Eur. J. Pharmacol. 2021, 892, 173689. [Google Scholar] [CrossRef]
- Harjai, K.J.; Stone, G.W.; Boura, J.; Mattos, L.; Chandra, H.; Cox, D.; Grines, L.; O’Neill, W.; Grines, C. Primary Angioplasty in Myocardial Infarction Investigators. Comparison of outcomes of diabetic and nondiabetic patients undergoing primary angioplasty for acute myocardial infarction. Am. J. Cardiol. 2003, 91, 1041–1045. [Google Scholar] [CrossRef]
- Pawar, K.; Thompkinson, D.K. Multiple functional ingredient approach in formulating dietary supplement for management of diabetes: A review. Crit. Rev. Food Sci. Nutr. 2014, 54, 957–973. [Google Scholar] [CrossRef]
- Lee, S.M.; Bustamante, S.; Flores, C.; Bezerra, J.; Goda, T.; Koldovský, O. Chronic effects of an alpha-glucosidase inhibitor (Bay o 1248) on intestinal disaccharidase activity in normal and diabetic mice. J. Pharmacol. Exp. Ther. 1987, 240, 132–137. [Google Scholar]
- Bailey, C.J. Insulin resistance and antidiabetic drugs. Biochem. Pharmacol. 1999, 58, 1511–1520. [Google Scholar] [CrossRef]
- Abd Elmeged, L.S.M.; Alghamdi, A.A.A. The effect of consuming different proportions of hummer fish on biochemical and histopathological changes of hyperglycemic rats. Saudi J. Biol. Sci. 2022, 29, 140–147. [Google Scholar] [CrossRef]
- Kianbakht, S.; Abasi, B.; Dabaghian, F.H. Anti-hyperglycemic effect of Vaccinium arctostaphylos in type 2 diabetic patients: A randomized controlled trial. Forsch. Komplementmed. 2013, 20, 17–22. [Google Scholar] [CrossRef]
- Carter, S.; Clifton, P.M.; Keogh, J.B. Effect of Intermittent Compared with Continuous Energy Restricted Diet on Glycemic Control in Patients with Type 2 Diabetes: A Randomized Noninferiority Trial. JAMA Netw. Open 2018, 1, e180756. [Google Scholar] [CrossRef]
- Cui, A.; Fan, H.; Zhang, Y.; Zhang, Y.; Niu, D.; Liu, S.; Liu, Q.; Ma, W.; Shen, Z.; Shen, L.; et al. Dexamethasone-induced Krüppel-like factor 9 expression promotes hepatic gluconeogenesis and hyperglycemia. J. Clin. Investig. 2019, 129, 2266–2278. [Google Scholar] [CrossRef]
- Wang, H.; Fowler, M.I.; Messenger, D.J.; Terry, L.A.; Gu, X.; Zhou, L.; Liu, R.; Su, J.; Shi, S.; Ordaz-Ortiz, J.J.; et al. Homoisoflavonoids Are Potent Glucose Transporter 2 (GLUT2) Inhibitors: A Potential Mechanism for the Glucose-Lowering. J. Agric. Food Chem. 2018, 66, 3137–3145. [Google Scholar] [CrossRef]
- Nitin, S. HbA1c and factors other than diabetes mellitus affecting it. Nitin S. Singapore Med. J. 2010, 51, 616. [Google Scholar]
- Guo, W.; Zhou, Q.; Jia, Y.; Xu, J. Increased Levels of Glycated Hemoglobin A1c and Iron Deficiency Anemia: A Review. Med. Sci. Monit. 2019, 25, 8371–8378. [Google Scholar] [CrossRef]
- Yazdanpanah, S.; Rabiee, M.; Tahriri, M.; Abdolrahim, M.; Rajab, A.; Jazayeri, H.E.; Tayebi, L. Evaluation of glycated albumin (GA) and GA/HbA1c ratio for diagnosis of diabetes and glycemic control: A comprehensive review. Crit. Rev. Clin. Lab. Sci. 2017, 54, 219–232. [Google Scholar] [CrossRef]
- Edelman, D.; Olsen, M.K.; Dudley, T.K.; Harris, A.C.; Oddone, E.Z. Utility of hemoglobin A1c in predicting diabetes risk. J. Gen. Intern Med. 2004, 19, 1175–1180. [Google Scholar] [CrossRef]
- Angelidi, A.M.; Filippaios, A.; Mantzoros, C.S. Severe insulin resistance syndromes. J. Clin. Investig. 2021, 131, e142245. [Google Scholar] [CrossRef]
- Turner, M.C.; Martin, N.R.W.; Player, D.J.; Ferguson, R.A.; Wheeler, P.; Green, C.J.; Akam, E.C.; Lewis, M.P. Characterising hyperinsulinemia-induced insulin resistance in human skeletal muscle cells. J. Mol. Endocrinol. 2020, 64, 125–132. [Google Scholar] [CrossRef]
- Schrezenmeir, J. Hyperinsulinemia, hyperproinsulinemia and insulin resistance in the metabolic syndrome. Experientia 1996, 52, 426–432. [Google Scholar] [CrossRef]
- Grote, C.W.; Groover, A.L.; Ryals, J.M.; Geiger, P.C.; Feldman, E.L.; Wright, D.E. Peripheral nervous system insulin resistance in ob/ob mice. Acta Neuropathol. Commun. 2013, 1, 15. [Google Scholar] [CrossRef]
- Yang, Q.; Vijayakumar, A.; Kahn, B.B. Metabolites as regulators of insulin sensitivity and metabolism. Nat. Rev. Mol. Cell Biol. 2018, 19, 654–672. [Google Scholar] [CrossRef]
- He, L.; Zhang, F.-J.; Li, H.-Y.; Li, L.; Song, L.-G.; Mao, Y.; Li, J.; Liu, H.-M.; Li, F.-L.; Xu, L.-Y.; et al. Anti-diabetic Role of Adropin in Streptozotocin Induced Diabetic Rats via Alteration of PI3K/Akt and Insulin Signaling Pathway. J. Oleo Sci. 2021, 70, 657–664. [Google Scholar] [CrossRef]
- Kim, J.K. Inflammation and insulin resistance: An old story with new ideas. Korean Diabetes J. 2010, 34, 137–145. [Google Scholar] [CrossRef]
- Shaw, L.M. The insulin receptor substrate (IRS) proteins: At the intersection of metabolism and cancer. Cell Cycle 2011, 10, 1750–1756. [Google Scholar] [CrossRef]
- Liu, Q.; Li, X.; Li, C.; Zheng, Y.; Peng, G. 1-Deoxynojirimycin Alleviates Insulin Resistance via Activation of Insulin Signaling PI3K/AKT Pathway in Skeletal Muscle of db/db Mice. Molecules 2015, 20, 21700–21714. [Google Scholar] [CrossRef]
- Choi, S.B.; Park, S. A steroidal glycoside from Polygonatum odoratum (Mill.) Druce. improves insulin resistance but does not alter insulin secretion in 90% pancreatectomized rats. Biosci. Biotechnol. Biochem. 2002, 66, 2036–2043. [Google Scholar] [CrossRef]
- Khil, L.-Y.; Han, S.-S.; Kim, S.-G.; Chang, T.-S.; Jeon, S.-D.; So, D.-S.; Moon, C.-K. Effects of Brazilin on GLUT4 Recruitment in Isolated Rat Epididymal Adipocytes. Biochem. Pharmacol. 1999, 58, 1705–1712. [Google Scholar] [CrossRef]
- Sivalingam, S.; Kandhasamy, S.; Chandrasekaran, S.; Vijayan, K.; Jacob, J.P.; Perumal, A.; Vijayakumar, S. A flavone derivative from Andrographis echioides leaf extract positively alters the molecular targets of insulin signaling pathway. S. Afr. J. Bot. 2022, 146, 760–770. [Google Scholar] [CrossRef]
- Benchoula, K.; Arya, A.; Parhar, I.S.; Hwa, W.E. FoxO1 signaling as a therapeutic target for type 2 diabetes and obesity. Eur. J. Pharmacol. 2021, 891, 173758. [Google Scholar] [CrossRef]
- Alikhani, M.; Alikhani, Z.; Graves, D.T. FOXO1 Functions as a Master Switch That Regulates Gene Expression Necessary for Tumor Necrosis Factor-induced Fibroblast Apoptosis. J. Biol. Chem. 2005, 280, 12096–12102. [Google Scholar] [CrossRef]
- He, L.; Li, Y.; Zeng, N.; Stiles, B.L. Regulation of basal expression of hepatic PEPCK and G6Pase by AKT2. Biochem. J. 2020, 477, 1021–1031. [Google Scholar] [CrossRef]
- Kaidanovich-Beilin, O.; Eldar-Finkelman, H. Long-Term Treatment with Novel Glycogen Synthase Kinase-3 Inhibitor Improves Glucose Homeostasis in ob/ob Mice: Molecular Characterization in Liver and Muscle Oksana Kaidanovich-Beilin and Hagit Eldar-Finkelman. J. Pharmacol. Exp. Ther. 2006, 316, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Oza, M.J.; Kulkarni, Y.A. Formononetin Treatment in Type 2 Diabetic Rats Reduces Insulin Resistance and Hyperglycemia. Front. Pharmacol. 2018, 9, 7739. [Google Scholar] [CrossRef] [PubMed]
- Tay, K.C.; Tan, L.T.; Chan, C.K.; Hong, S.L.; Chan, K.G.; Yap, W.H.; Pusparajah, P.; Lee, L.H.; Goh, B.H. Formononetin: A Review of Its Anticancer Potentials and Mechanisms. Front. Pharmacol. 2019, 10, 820. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhang, N.; Yang, F.; Qi, J.; Song, X.C.; Hu, Z.F.; Zhu, D.N. Homoisoflavonoids from the fibrous roots of Polygonatum odoratum with glucose uptake-stimulatory activity in 3T3-L1 adipocytes. J. Nat. Prod. 2010, 73, 548–552. [Google Scholar] [CrossRef]
- Proença, C.; Oliveira, A.; Freitas, M.; Ribeiro, D.; Sousa, J.L.C.; Ramos, M.J.; Silva, A.M.S.; Fernandes, P.A.; Fernandes, E. Structural Specificity of Flavonoids in the Inhibition of Human Fructose 1,6-Bisphosphatase. J. Nat. Prod. 2020, 83, 1541–1552. [Google Scholar] [CrossRef]
| Body Weight | Normal | ob/ob | Met | HMC |
|---|---|---|---|---|
| Initial weight (g) | 20.39 ± 1.19 b | 34.25 ± 1.74 a | 34.07 ± 1.80 a | 34.13 ± 0.85 a |
| Final weight (g) | 23.84 ± 1.69 c | 39.45 ± 4.28 a | 38.82 ± 4.63 a | 36.42 ± 3.13 b |
| Weight gain (g) | 3.45 ± 0.99 c | 5.20 ± 1.05 a | 4.75 ± 0.85 b | 2.29 ± 0.56 d |
| Average food intake (g/day) | 4.24 ± 0.33 c | 6.25 ± 0.66 a | 5.86 ± 0.46 b | 5.92 ± 0.62 b |
| Average water intake (mL/day) | 8.39 ± 2.23 c | 20.11 ± 3.02 a | 13.90 ± 2.92 b | 15.45 ± 2.91 b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoo, J.; Park, J.E.; Han, J.S. HMC Ameliorates Hyperglycemia via Acting PI3K/AKT Pathway and Improving FOXO1 Pathway in ob/ob Mice. Nutrients 2023, 15, 2023. https://doi.org/10.3390/nu15092023
Yoo J, Park JE, Han JS. HMC Ameliorates Hyperglycemia via Acting PI3K/AKT Pathway and Improving FOXO1 Pathway in ob/ob Mice. Nutrients. 2023; 15(9):2023. https://doi.org/10.3390/nu15092023
Chicago/Turabian StyleYoo, Jeong, Jae Eun Park, and Ji Sook Han. 2023. "HMC Ameliorates Hyperglycemia via Acting PI3K/AKT Pathway and Improving FOXO1 Pathway in ob/ob Mice" Nutrients 15, no. 9: 2023. https://doi.org/10.3390/nu15092023
APA StyleYoo, J., Park, J. E., & Han, J. S. (2023). HMC Ameliorates Hyperglycemia via Acting PI3K/AKT Pathway and Improving FOXO1 Pathway in ob/ob Mice. Nutrients, 15(9), 2023. https://doi.org/10.3390/nu15092023







