The Effects of Different Modalities of an Acute Energy Deficit on Sleep and Next Morning Appetitive and Compensatory Behavior in Healthy Young Adults: The EDIES Protocol
Abstract
1. Introduction
1.1. Background and Rationale
1.2. Aims
2. Materials and Methods
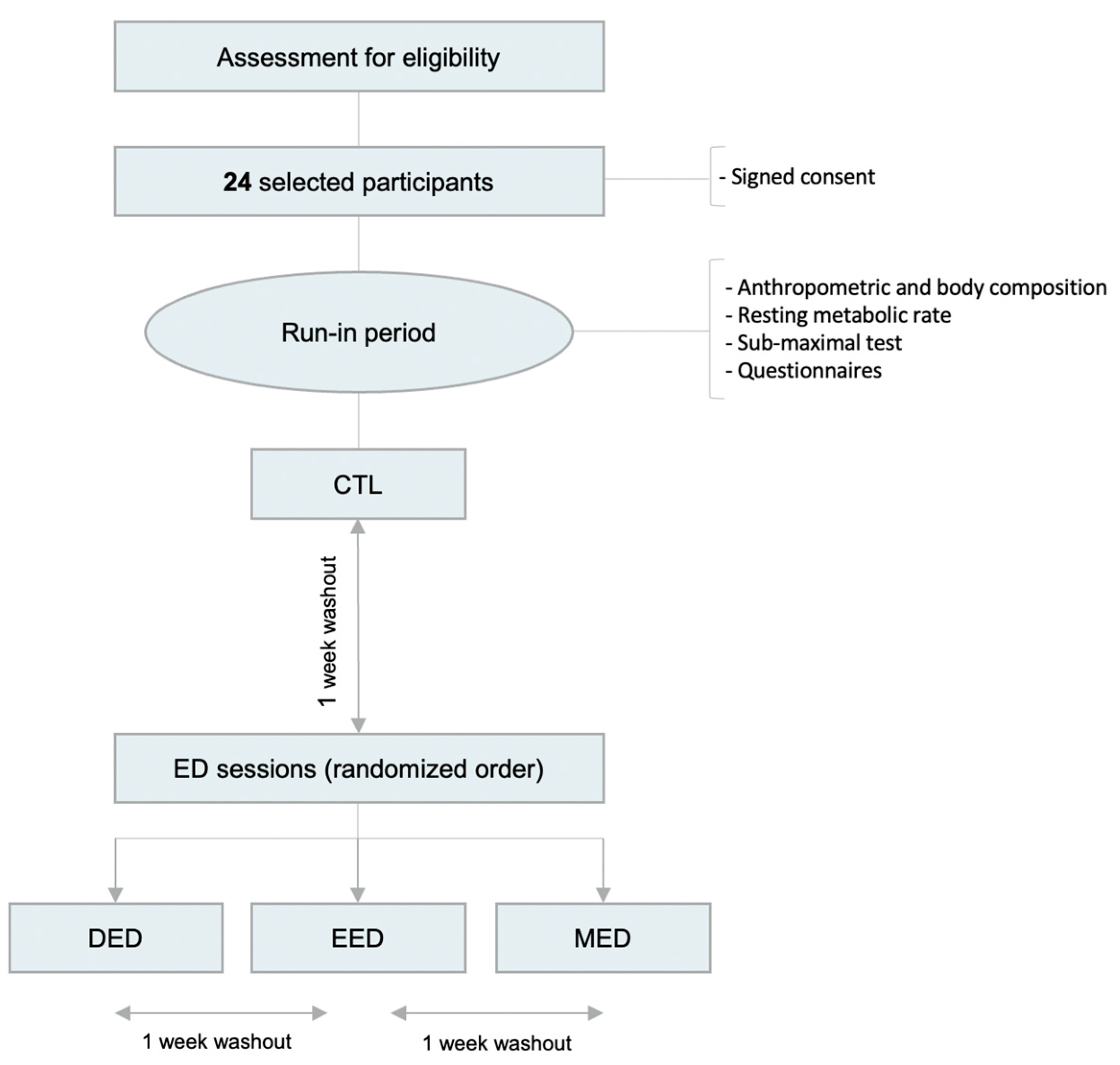
2.1. Study Setting and Design
2.2. Participants
2.2.1. Sample Size
2.2.2. Recruitment
2.2.3. Eligibility Criteria
2.3. Randomization
2.3.1. Sequence Generation
2.3.2. Concealment and Blinding
2.4. Run-In Period and Baseline Assessments
2.4.1. Run-In Period Overview
2.4.2. Baseline Assessments
- Anthropometric and body composition: Body mass will be measured using a digital weight scale (UM-076, TANITA, Tokyo, Japan). Height will be assessed using a portable stadiometer with the participants barefooted (HR001, TANITA, Tokyo, Japan). The skinfold thickness will be measured in duplicate by the same investigator on the right side of the body at the biceps, triceps, subscapular, and supra-iliac sites using a Harpenden caliper (Baty International, Burgess Hill, UK). Relative fat mass will be then calculated using Siri equations amended by Weststrate and Deurenberg (1989) [26].
- The resting metabolic rate (RMR) and submaximal test: The resting metabolic rate will be measured in the morning, under a fasted state, by indirect calorimetry using a mobile spiroergometric system (METAMAX 3B-R2, CORTEX Biophysik GmbH, Leipzig, Germany). Before each test, the equipment will be calibrated according to the manufacturer’s recommendations. The participants will be placed in a supine position in a thermoneutral environment (22–25 °C room temperature) for 45 min before starting the measurements. After reaching a steady state, the O2 consumption and CO2 production, normalized for temperature, barometric pressure, and humidity, will be recorded and averaged at one-minute intervals for 20–45 min and averaged over the entire measurement period. The resting energy expenditure (in kcal/day) and the respiratory quotient (CO2/O2 ratio) will be calculated thereafter. The resting metabolic rate assessment will be followed by a submaximal test in order to estimate the peak oxygen consumption (VO2 peak) and therefore calibrate the energy deficit sessions’ exercise. The exercise will be performed on an adjustable cycle ergometer (Wattbike Ltd., Nottingham, UK). After a warm-up period (2 min), performed at 45 W, the output will be increased by 15 W every 5 min (allowing to ensure a stable state for each step) until the participants reach 60% of the age-predicted maximum heart rate amended by Tanaka et al. (2001) [27]. The heart rate (HR) will be continuously recorded using a heart rate sensor (Polar H10, Polar Electro, Kempele, Finland). The energy expenditure (EE) will be estimated for each step by multiplying the O2 consumption (VO2) by the energy equivalent (kcal/L O2) for each participant. The five steps will allow for the establishment of the HR–VO2 relationship for each participant, which will be used to calibrate the exercise intensity required for an expenditure of 125 and 250 kcal.
- Questionnaires: The to-be-completed questionnaires will include (1) the International Physical Activity Questionnaire (IPAQ) to estimate the physical activity level [28]; (2) the Morningness-Eveningness Questionnaire (MEQ) to determine the participants’ chronotype (i.e., evening, intermediate, or morning typology) [29]; (3) the Pittsburg Sleep Quality Index (PSQI) to assess the quality of sleep over the last month [30]; (4) the Dutch Eating Behavior Questionnaire (DEBQ) with scales for restrained, emotional and external eating behaviors [31]; and (5) the Multidimensional Fatigue Inventory (MFI) to assess fatigue traits [32].
2.5. Experimental Sessions
2.5.1. Control Session
2.5.2. Energy Deficit Sessions
- DED session: 500 kcal dietary deficit (−250 kcal on breakfast and −250 kcal on lunch);
- EED session: 500 kcal deficit, induced by two exercise bouts (−250 kcal after breakfast and −250 kcal after lunch);
- MED session: 250 kcal dietary deficit (−125 kcal at breakfast and −125 kcal at lunch) and a 250 kcal deficit induced by exercise (−125 kcal after breakfast and −125 kcal after lunch).
2.6. Assessement of Energy Balance
2.7. Outcomes
2.7.1. Primary Outcome: Sleep Efficiency
2.7.2. Experimental Secondary Outcomes
- Other sleep outcomes: Beyond SE, the Sleep Profiler-PSG2 provides other sleep variables, such as the following: total sleep time (TST); sleep onset latency (SOL); wake after sleep onset (WASO); the number of awakenings lasting more than 30 s; the arousal index and staging (time spent in non-rapid (NREM; Stage-1, Stage-2, and Stage-3) and rapid eye movement (REM)), according to the American Academy of Sleep Medicine recommendations [43].
- Mood: The Profile of Mood States will be used to assess the participant’s mood before the night of each experimental session [36]. All participants will be asked to rate “How are you feeling right now?” using 24 mood descriptors (e.g., nervous, unhappy, etc.). For each descriptor, the participants have to answer using a 5-point Likert scale, from 0 (not at all) to 4 (extremely). This questionnaire is divided into six subscales (fatigue, confusion, vigor, depression, tension, and anger), each containing four mood descriptors.
- Ad libitum energy intake: A standardized buffet breakfast will be organized on day1 of each session [44]. Consumed food items will be weighed and recorded by the investigators. Subsequently, the computerized nutrient analysis software (Bilnut 4.0 SCDA, Nutrisoft) and Ciqual tables (2020 version) will calculate the energy intake and the part of energy derived from each class of macronutrients.
- Food liking and wanting: LFPQ will be used to assess the individual’s food preferences [37]. It comprises two sub-tasks that require interactions from the participant. The first task (explicit task) involves an explicit assessment of food pictures using the 100-unit VAS. Single food images are randomly displayed to the participant on a screen computer, who is required to rate it according to “How pleasant would it be to taste some of this food now?” (explicit liking) and “How much do you want some of this food now?” (explicit wanting). The second task (implicit or forced choice task) requires a quick choice to be made between paired combinations of food pictures from different categories. During this task, a series of food image pairs are presented to the participant with the instruction, “Which food do you most want to eat now?”.
- Appetite sensations: Sensations of hunger, appetite, and a desire to eat will be measured using a VAS (150 mm) throughout all sessions (i.e., 9 measures on day 0, and 8 measures on day 1). These VASs were previously validated by Flint et al. (2000) [35].
- Sleepiness: The subjective level of sleepiness will be measured using the KSS [33]. The participant has to rate his subjective sensation of sleepiness in the last 10 min using a 9-point scale, ranging from 1 (extremely alert) to 9 (extremely sleepy).
- Fatigue: The French-validated version of the ROF scale will be used to assess the state of fatigue [34]. This is an 11-point scale, from 0 (not fatigued at all) to 10 (total fatigue and exhaustion), with accompanying descriptors and schematic components, which allow for tracking perceived fatigue across different ranges of daily life, physical activity, and recovery contexts.
2.7.3. Baseline Secondary Outcomes
- Subjective sleep quality: The PSQI questionnaire will be used to assess sleep quality [30]. It comprises 19 self-reported questions and measures seven components (i.e., overall sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of medication for sleep, and daytime dysfunction due to sleepiness). The sum of scores from the seven components provides a global score from 0 (better) to 21 (worse). A global score of ≤5 is associated with good sleep quality; in reverse, a global score of ≥5 is associated with poor sleep quality.
- Eating behaviors: Eating behaviors will be measured using the DEBQ, a 33-item questionnaire assessing three distinct eating behaviors: emotional eating (13 items), external eating (10 items), and restrained eating (10 items) [31]. For each item, the participants have to answer using a 5-point Likert scale, from 1 (never) to 5 (very often), with higher scores indicating greater endorsement of the eating behavior.
- Chronotype: The MEQ will be used to define each participant’s chronotype [29]. The participants have to score 19 items using a 5-point Likert scale. The sum of the item scores ranges from 16 to 86. Scores of 41 and below indicate “evening types”, scores of 59 and above indicate “morning types”, and scores between 42–58 indicate “intermediate types”.
- Subjective physical activity. The short form (7 questions) of IPAQ will be used to assess the participant’s physical activity level [28]. The participants will be asked to report the time spent being physically active in the last 7 days using four different dimensions (i.e., vigorous physical activity, moderate physical activity, time to walk, and time spent sitting). Data collected with this questionnaire allow the classification of participants into three categories: inactive, minimally active, health-enhancing physical activity and/or to obtain a continuous measure reported as MET-minutes for each dimension (walking MET-min/week, moderate MET-min/week, and vigorous MET-min/week).
- Fatigue trait. The fatigue trait will be measured using the MFI questionnaire [32], which includes 20 items addressing different dimensions of fatigue, divided into 5 categories: general fatigue, physical fatigue, mental fatigue, reduced activities, and reduced motivation. The questionnaire includes positively and negatively worded items that are rated using a 5-point Likert scale. The dimension subscores (4–20) and global scores (20–100) can be calculated, with a high score indicating a high degree of fatigue.
2.8. Strategies to Improve Study Adherence and Compliance
2.9. Data Management and Confidentiality
2.10. Statistical Methods
2.10.1. Statistical Analysis for Sleep Outcomes
2.10.2. Statistical Analysis for Secondary Outcomes
2.10.3. Plan to Handle Missing Data
2.10.4. Methods for Additional Statistical Analyses
2.10.5. Plan to Give Access to Full Protocol, Data, and Statistical Code
3. Discussion and Future Perspectives
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Aragon, A.A.; Schoenfeld, B.J.; Wildman, R.; Kleiner, S.; VanDusseldorp, T.; Taylor, L.; Earnest, C.P.; Arciero, P.J.; Wilborn, C.; Kalman, D.S. International Society of Sports Nutrition Position Stand: Diets and Body Composition. J. Int. Soc. Sports Nutr. 2017, 14, 16. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D. What Is the Required Energy Deficit per Unit Weight Loss? Int. J. Obes. 2008, 32, 573–576. [Google Scholar] [CrossRef] [PubMed]
- Strasser, B.; Spreitzer, A.; Haber, P. Fat Loss Depends on Energy Deficit Only, Independently of the Method for Weight Loss. Ann. Nutr. Metab. 2007, 51, 428–432. [Google Scholar] [CrossRef] [PubMed]
- Thivel, D.; Metz, L.; Julian, V.; Isacco, L.; Verney, J.; Ennequin, G.; Charlot, K.; Beaulieu, K.; Finlayson, G.; King, J.A. Diet-but Not Exercise-Induced Iso-Energetic Deficit Induces Compensatory Appetitive Responses. Eur. J. Clin. Nutr. 2021, 75, 1425–1432. [Google Scholar] [CrossRef]
- O’Connor, K.L.; Scisco, J.L.; Smith, T.J.; Young, A.J.; Montain, S.J.; Price, L.L.; Lieberman, H.R.; Karl, J.P. Altered Appetite-Mediating Hormone Concentrations Precede Compensatory Overeating after Severe, Short-Term Energy Deprivation in Healthy Adults. J. Nutr. 2016, 146, 209–217. [Google Scholar] [CrossRef]
- Thivel, D.; Finlayson, G.; Miguet, M.; Pereira, B.; Duclos, M.; Boirie, Y.; Doucet, E.; Blundell, J.E.; Metz, L. Energy Depletion by 24-h Fast Leads to Compensatory Appetite Responses Compared with Matched Energy Depletion by Exercise in Healthy Young Males. Br. J. Nutr. 2018, 120, 583–592. [Google Scholar] [CrossRef]
- Ross, K.M.; Graham Thomas, J.; Wing, R.R. Successful Weight Loss Maintenance Associated with Morning Chronotype and Better Sleep Quality. J. Behav. Med. 2016, 39, 465–471. [Google Scholar] [CrossRef]
- Thomson, C.A.; Morrow, K.L.; Flatt, S.W.; Wertheim, B.C.; Perfect, M.M.; Ravia, J.J.; Sherwood, N.E.; Karanja, N.; Rock, C.L. Relationship between Sleep Quality and Quantity and Weight Loss in Women Participating in a Weight-loss Intervention Trial. Obesity 2012, 20, 1419–1425. [Google Scholar] [CrossRef]
- Chaput, J.-P.; McHill, A.W.; Cox, R.C.; Broussard, J.L.; Dutil, C.; da Costa, B.G.; Sampasa-Kanyinga, H.; Wright, K.P., Jr. The Role of Insufficient Sleep and Circadian Misalignment in Obesity. Nat. Rev. Endocrinol. 2023, 19, 82–97. [Google Scholar] [CrossRef]
- St-Onge, M.-P. The Role of Sleep Duration in the Regulation of Energy Balance: Effects on Energy Intakes and Expenditure. J. Clin. Sleep Med. 2013, 9, 73–80. [Google Scholar] [CrossRef]
- Nedeltcheva, A.V.; Kilkus, J.M.; Imperial, J.; Schoeller, D.A.; Penev, P.D. Insufficient Sleep Undermines Dietary Efforts to Reduce Adiposity. Ann. Intern. Med. 2010, 153, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Stich, F.M.; Huwiler, S.; D’Hulst, G.; Lustenberger, C. The Potential Role of Sleep in Promoting a Healthy Body Composition: Underlying Mechanisms Determining Muscle, Fat, and Bone Mass and Their Association with Sleep. Neuroendocrinology 2022, 112, 673–701. [Google Scholar] [CrossRef] [PubMed]
- Alvarenga, T.A.F.; Andersen, M.L.; Papale, L.A.; Antunes, I.B.; Tufik, S. Influence of Long-Term Food Restriction on Sleep Pattern in Male Rats. Brain Res. 2005, 1057, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Dewasmes, G.; Duchamp, C.; Minaire, Y. Sleep Changes in Fasting Rats. Physiol. Behav. 1989, 46, 179–184. [Google Scholar] [CrossRef]
- Michalsen, A.; Schlegel, F.; Rodenbeck, A.; Lüdtke, R.; Huether, G.; Teschler, H.; Dobos, G.J. Effects of Short-Term Modified Fasting on Sleep Patterns and Daytime Vigilance in Non-Obese Subjects: Results of a Pilot Study. Ann. Nutr. Metab. 2003, 47, 194–200. [Google Scholar] [CrossRef]
- Peuhkuri, K.; Sihvola, N.; Korpela, R. Dietary Factors and Fluctuating Levels of Melatonin. Food Nutr. Res. 2012, 56, 17252. [Google Scholar] [CrossRef]
- Röjdmark, S.; Wetterberg, L. Short-term Fasting Inhibits the Nocturnal Melatonin Secretion in Healthy Man. Clin. Endocrinol. 1989, 30, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Zhdanova, I.V.; Lynch, H.J.; Wurtman, R.J. Melatonin: A Sleep-Promoting Hormone. Sleep 1997, 20, 899–907. [Google Scholar]
- Zisapel, N. Sleep and Sleep Disturbances: Biological Basis and Clinical Implications. Cell. Mol. Life Sci. 2007, 64, 1174–1186. [Google Scholar] [CrossRef]
- Karklin, A.; Driver, H.S.; Buffenstein, R. Restricted Energy Intake Affects Nocturnal Body Temperature and Sleep Patterns. Am. J. Clin. Nutr. 1994, 59, 346–349. [Google Scholar] [CrossRef]
- Fagerberg, P. Negative Consequences of Low Energy Availability in Natural Male Bodybuilding: A Review. Int. J. Sport Nutr. Exerc. Metab. 2018, 28, 385–402. [Google Scholar] [CrossRef] [PubMed]
- Pardue, A.; Trexler, E.T.; Sprod, L.K. Case Study: Unfavorable but Transient Physiological Changes during Contest Preparation in a Drug-Free Male Bodybuilder. Int. J. Sport Nutr. Exerc. Metab. 2017, 27, 550–559. [Google Scholar] [CrossRef] [PubMed]
- Kredlow, M.A.; Capozzoli, M.C.; Hearon, B.A.; Calkins, A.W.; Otto, M.W. The Effects of Physical Activity on Sleep: A Meta-Analytic Review. J. Behav. Med. 2015, 38, 427–449. [Google Scholar] [CrossRef] [PubMed]
- Driver, H.S.; Taylor, S.R. Exercise and Sleep. Sleep Med. Rev. 2000, 4, 387–402. [Google Scholar] [CrossRef]
- Netzer, N.C.; Stoohs, R.A.; Netzer, C.M.; Clark, K.; Strohl, K.P. Using the Berlin Questionnaire to Identify Patients at Risk for the Sleep Apnea Syndrome. Ann. Intern. Med. 1999, 131, 485–491. [Google Scholar] [CrossRef]
- Weststrate, J.A.; Deurenberg, P. Body Composition in Children: Proposal for a Method for Calculating Body Fat Percentage from Total Body Density or Skinfold-Thickness Measurements. Am. J. Clin. Nutr. 1989, 50, 1104–1115. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-Predicted Maximal Heart Rate Revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef]
- Taillard, J.; Philip, P.; Chastang, J.-F.; Bioulac, B. Validation of Horne and Ostberg Morningness-Eveningness Questionnaire in a Middle-Aged Population of French Workers. J. Biol. Rhythm. 2004, 19, 76–86. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Van Strien, T.; Frijters, J.E.; Bergers, G.P.; Defares, P.B. The Dutch Eating Behavior Questionnaire (DEBQ) for Assessment of Restrained, Emotional, and External Eating Behavior. Int. J. Eat. Disord. 1986, 5, 295–315. [Google Scholar] [CrossRef]
- Gentile, S.; Delarozière, J.C.; Favre, F.; Sambuc, R.; San Marco, J.L. Validation of the French ‘Multidimensional Fatigue Inventory’(MFI 20). Eur. J. Cancer Care 2003, 12, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Åkerstedt, T.; Anund, A.; Axelsson, J.; Kecklund, G. Subjective Sleepiness Is a Sensitive Indicator of Insufficient Sleep and Impaired Waking Function. J. Sleep Res. 2014, 23, 242–254. [Google Scholar] [CrossRef]
- Brownstein, C.G.; Rimaud, D.; Singh, B.; Fruleux-Santos, L.-A.; Sorg, M.; Micklewright, D.; Millet, G.Y. French Translation and Validation of the Rating-of-Fatigue Scale. Sports Med. Open 2021, 7, 25. [Google Scholar] [CrossRef] [PubMed]
- Flint, A.; Raben, A.; Blundell, J.E.; Astrup, A. Reproducibility, Power and Validity of Visual Analogue Scales in Assessment of Appetite Sensations in Single Test Meal Studies. Int. J. Obes. 2000, 24, 38. [Google Scholar] [CrossRef] [PubMed]
- Cayrou, S.; Dickès, P.; Dolbeault, S. Version Française Du Profile of Mood States (POMS-f). J. Thérapie Comport. Cogn. 2003, 13, 83–88. [Google Scholar]
- Finlayson, G.; King, N.; Blundell, J.E. Liking vs. Wanting Food: Importance for Human Appetite Control and Weight Regulation. Neurosci. Biobehav. Rev. 2007, 31, 987–1002. [Google Scholar] [CrossRef]
- Leenaars, C.H.; Zant, J.C.; Aussems, A.; Faatz, V.; Snackers, D.; Kalsbeek, A. The Leeds Food Preference Questionnaire after Mild Sleep Restriction—A Small Feasibility Study. Physiol. Behav. 2016, 154, 28–33. [Google Scholar] [CrossRef]
- Crouter, S.E.; Churilla, J.R.; Bassett, D.R. Accuracy of the Actiheart for the Assessment of Energy Expenditure in Adults. Eur. J. Clin. Nutr. 2008, 62, 704–711. [Google Scholar] [CrossRef]
- Westbrook, P.R.; Levendowski, D.J.; Zavora, T.; Davis, G.; Popovic, D.; Berka, C.; Mitrovic, M.; Veljkovic, B. System for the Assessment of Sleep Quality in Adults and Children. U.S. Patent 8,355,769, 15 January 2014. [Google Scholar]
- Levendowski, D.J.; Popovic, D.; Berka, C.; Westbrook, P.R. Retrospective Cross-Validation of Automated Sleep Staging Using Electroocular Recording in Patients with and without Sleep Disordered Breathing. Int. Arch. Med. 2012, 5, 21. [Google Scholar] [CrossRef]
- Popovic, D.; Khoo, M.; Westbrook, P. Automatic Scoring of Sleep Stages and Cortical Arousals Using Two Electrodes on the Forehead: Validation in Healthy Adults. J. Sleep Res. 2014, 23, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Berry, R.B.; Brooks, R.; Gamaldo, C.; Harding, S.M.; Lloyd, R.M.; Quan, S.F.; Troester, M.T.; Vaughn, B.V. AASM Scoring Manual Updates for 2017 (Version 2.4). J. Clin. Sleep Med. 2017, 13, 665–666. [Google Scholar] [CrossRef] [PubMed]
- Gregersen, N.T.; Flint, A.; Bitz, C.; Blundell, J.E.; Raben, A.; Astrup, A. Reproducibility and Power of Ad Libitum Energy Intake Assessed by Repeated Single Meals. Am. J. Clin. Nutr. 2008, 87, 1277–1281. [Google Scholar] [CrossRef]
- Jakobsen, J.C.; Gluud, C.; Wetterslev, J.; Winkel, P. When and How Should Multiple Imputation Be Used for Handling Missing Data in Randomised Clinical Trials–a Practical Guide with Flowcharts. BMC Med. Res. Methodol. 2017, 17, 162. [Google Scholar] [CrossRef] [PubMed]
- Northeast, R.C.; Vyazovskiy, V.V.; Bechtold, D.A. Eat, Sleep, Repeat: The Role of the Circadian System in Balancing Sleep–Wake Control with Metabolic Need. Curr. Opin. Physiol. 2020, 15, 183–191. [Google Scholar] [CrossRef]
- Chaput, J.-P. Sleep Patterns, Diet Quality and Energy Balance. Physiol. Behav. 2014, 134, 86–91. [Google Scholar] [CrossRef]
- Zuraikat, F.M.; Wood, R.A.; Barragán, R.; St-Onge, M.-P. Sleep and Diet: Mounting Evidence of a Cyclical Relationship. Annu. Rev. Nutr. 2021, 41, 309–332. [Google Scholar] [CrossRef]
- VanItallie, T.B. Sleep and Energy Balance: Interactive Homeostatic Systems. Metabolism 2006, 55, S30–S35. [Google Scholar] [CrossRef]
- Saidi, O.; Rochette, E.; Bovet, M.; Merlin, E.; Duché, P. Acute Intense Exercise Improves Sleep and Decreases next Morning Consumption of Energy-Dense Food in Adolescent Girls with Obesity and Evening Chronotype. Pediatr. Obes. 2020, 15, e12613. [Google Scholar] [CrossRef]
- Baker, F.C.; Lee, K.A. Menstrual Cycle Effects on Sleep. Sleep Med. Clin. 2022, 17, 283–294. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saidi, O.; Chatain, C.; Del Sordo, G.C.; Demaria, R.; Lequin, L.; Rochette, E.; Larribaut, J.; Gruet, M.; Duché, P. The Effects of Different Modalities of an Acute Energy Deficit on Sleep and Next Morning Appetitive and Compensatory Behavior in Healthy Young Adults: The EDIES Protocol. Nutrients 2023, 15, 1962. https://doi.org/10.3390/nu15081962
Saidi O, Chatain C, Del Sordo GC, Demaria R, Lequin L, Rochette E, Larribaut J, Gruet M, Duché P. The Effects of Different Modalities of an Acute Energy Deficit on Sleep and Next Morning Appetitive and Compensatory Behavior in Healthy Young Adults: The EDIES Protocol. Nutrients. 2023; 15(8):1962. https://doi.org/10.3390/nu15081962
Chicago/Turabian StyleSaidi, Oussama, Cyril Chatain, Giovanna C. Del Sordo, Rémi Demaria, Ludivine Lequin, Emmanuelle Rochette, Julie Larribaut, Mathieu Gruet, and Pascale Duché. 2023. "The Effects of Different Modalities of an Acute Energy Deficit on Sleep and Next Morning Appetitive and Compensatory Behavior in Healthy Young Adults: The EDIES Protocol" Nutrients 15, no. 8: 1962. https://doi.org/10.3390/nu15081962
APA StyleSaidi, O., Chatain, C., Del Sordo, G. C., Demaria, R., Lequin, L., Rochette, E., Larribaut, J., Gruet, M., & Duché, P. (2023). The Effects of Different Modalities of an Acute Energy Deficit on Sleep and Next Morning Appetitive and Compensatory Behavior in Healthy Young Adults: The EDIES Protocol. Nutrients, 15(8), 1962. https://doi.org/10.3390/nu15081962





