Clinical and Imaging Outcomes after Vitamin D Supplementation in Patients with Multiple Sclerosis: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria and Data Items
2.2. Information Sources and Search Strategy
2.3. Selection and Data Collection Process
2.4. Study Risk of Bias Assessment
3. Results
3.1. Study Selection
3.2. Relapses
3.3. Disability
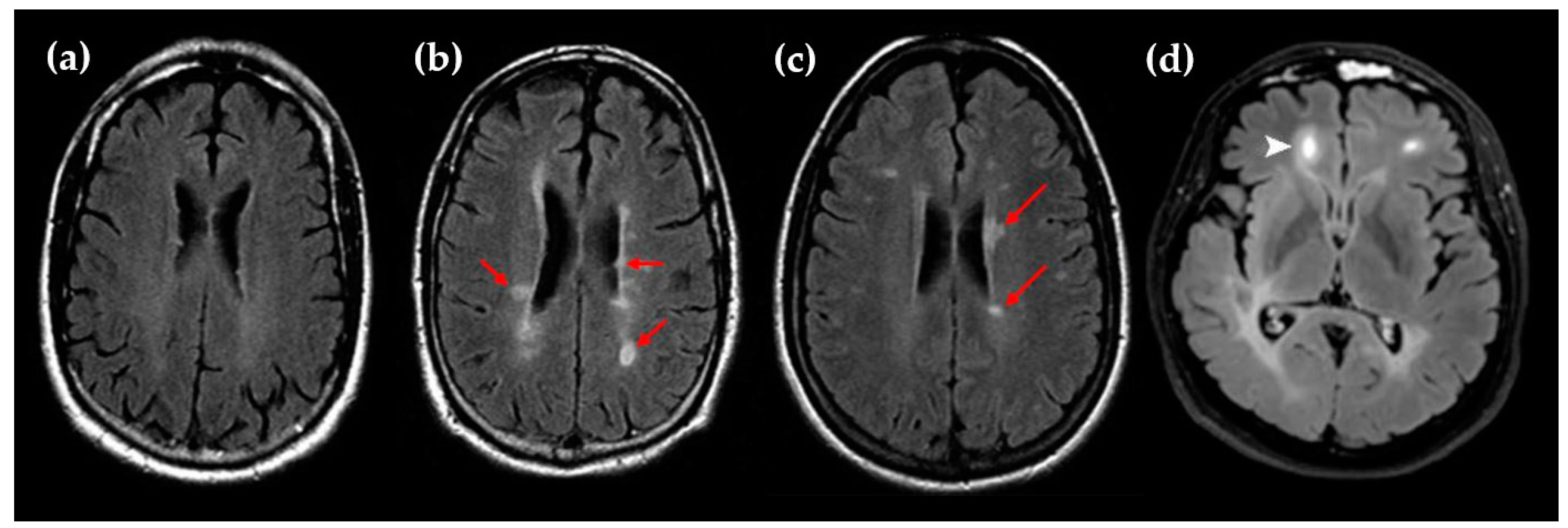
3.4. MRI Lesions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Walton, C.; King, R.; Rechtman, L.; Kaye, W.; Leray, E.; Marrie, R.A.; Robertson, N.; La Rocca, N.; Uitdehaag, B.; van der Mei, I.; et al. Rising Prevalence of Multiple Sclerosis Worldwide: Insights from the Atlas of MS, Third Edition. Mult. Scler. 2020, 26, 1816–1821. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freedman, M.S.; et al. Diagnosis of Multiple Sclerosis: 2017 Revisions of the McDonald Criteria. Lancet Neurol. 2018, 17, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Wattjes, M.P.; Ciccarelli, O.; Reich, D.S.; Banwell, B.; de Stefano, N.; Enzinger, C.; Fazekas, F.; Filippi, M.; Frederiksen, J.; Gasperini, C.; et al. 2021 MAGNIMS-CMSC-NAIMS Consensus Recommendations on the Use of MRI in Patients with Multiple Sclerosis. Lancet Neurol. 2021, 20, 653–670. [Google Scholar] [CrossRef] [PubMed]
- Dastagir, A.; Healy, B.C.; Chua, A.S.; Chitnis, T.; Weiner, H.L.; Bakshi, R.; Tauhid, S. Brain and Spinal Cord MRI Lesions in Primary Progressive vs. Relapsing-Remitting Multiple Sclerosis. eNeurologicalSci 2018, 12, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Lopaisankrit, T.; Thammaroj, J. Brain and Spinal Cord MRI Findings in Thai Multiple Sclerosis Patients. J. Imaging 2023, 9, 27. [Google Scholar] [CrossRef]
- Simpson, S.; Wang, W.; Otahal, P.; Blizzard, L.; van der Mei, I.A.F.; Taylor, B.V. Latitude Continues to Be Significantly Associated with the Prevalence of Multiple Sclerosis: An Updated Meta-Analysis. J. Neurol. Neurosurg. Psychiatry 2019, 90, 1193–1200. [Google Scholar] [CrossRef]
- Hedström, A.K.; Olsson, T.; Kockum, I.; Hillert, J.; Alfredsson, L. Low Sun Exposure Increases Multiple Sclerosis Risk Both Directly and Indirectly. J. Neurol. 2020, 267, 1045–1052. [Google Scholar] [CrossRef]
- Vandebergh, M.; Degryse, N.; Dubois, B.; Goris, A. Environmental Risk Factors in Multiple Sclerosis: Bridging Mendelian Randomization and Observational Studies. J. Neurol. 2022, 269, 4565–4574. [Google Scholar] [CrossRef]
- Behrens, J.R.; Rasche, L.; Gieß, R.M.; Pfuhl, C.; Wakonig, K.; Freitag, E.; Deuschle, K.; Bellmann-Strobl, J.; Paul, F.; Ruprecht, K.; et al. Low 25-Hydroxyvitamin D, but Not the Bioavailable Fraction of 25-Hydroxyvitamin D, Is a Risk Factor for Multiple Sclerosis. Eur. J. Neurol. 2016, 23, 62–67. [Google Scholar] [CrossRef]
- Munger, K.L.; Levin, L.I.; Hollis, B.W.; Howard, N.S.; Ascherio, A. Serum 25-Hydroxyvitamin D Levels and Risk of Multiple Sclerosis. JAMA 2006, 296, 2832–2838. [Google Scholar] [CrossRef]
- Ascherio, A.; Munger, K.L.; White, R.; Köchert, K.; Simon, K.C.; Polman, C.H.; Freedman, M.S.; Hartung, H.-P.; Miller, D.H.; Montalbán, X.; et al. Vitamin D as an Early Predictor of Multiple Sclerosis Activity and Progression. JAMA Neurol. 2014, 71, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Cantorna, M.T.; Snyder, L.; Lin, Y.-D.; Yang, L. Vitamin D and 1,25(OH)2D Regulation of T Cells. Nutrients 2015, 7, 3011–3021. [Google Scholar] [CrossRef] [PubMed]
- Haindl, M.T.; Hochmeister, S. Vitamin D in Multiple Sclerosis—Lessons From Animal Studies. Front. Neurol. 2021, 12, 757795. [Google Scholar] [CrossRef]
- Haghmorad, D.; Yazdanpanah, E.; Jadid Tavaf, M.; Zargarani, S.; Soltanmohammadi, A.; Mahmoudi, M.B.; Mahmoudi, M. Prevention and Treatment of Experimental Autoimmune Encephalomyelitis Induced Mice with 1, 25-Dihydroxyvitamin D3. Neurol. Res. 2019, 41, 943–957. [Google Scholar] [CrossRef] [PubMed]
- Lemire, J.M.; Archer, D.C. 1,25-Dihydroxyvitamin D3 Prevents the in Vivo Induction of Murine Experimental Autoimmune Encephalomyelitis. J. Clin. Investig. 1991, 87, 1103–1107. [Google Scholar] [CrossRef] [PubMed]
- Cantorna, M.T.; Hayes, C.E.; DeLuca, H.F. 1,25-Dihydroxyvitamin D3 Reversibly Blocks the Progression of Relapsing Encephalomyelitis, a Model of Multiple Sclerosis. Proc. Natl. Acad. Sci. USA 1996, 93, 7861–7864. [Google Scholar] [CrossRef]
- Chang, J.-H.; Cha, H.-R.; Lee, D.-S.; Seo, K.Y.; Kweon, M.-N. 1,25-Dihydroxyvitamin D3 Inhibits the Differentiation and Migration of TH17 Cells to Protect against Experimental Autoimmune Encephalomyelitis. PLoS ONE 2010, 5, e12925. [Google Scholar] [CrossRef]
- Mayne, C.G.; Spanier, J.A.; Relland, L.M.; Williams, C.B.; Hayes, C.E. 1,25-Dihydroxyvitamin D3 Acts Directly on the T Lymphocyte Vitamin D Receptor to Inhibit Experimental Autoimmune Encephalomyelitis. Eur. J. Immunol. 2011, 41, 822–832. [Google Scholar] [CrossRef]
- Zhen, C.; Feng, X.; Li, Z.; Wang, Y.; Li, B.; Li, L.; Quan, M.; Wang, G.; Guo, L. Suppression of Murine Experimental Autoimmune Encephalomyelitis Development by 1,25-Dihydroxyvitamin D3 with Autophagy Modulation. J. Neuroimmunol. 2015, 280, 1–7. [Google Scholar] [CrossRef]
- Chang, S.H.; Chung, Y.; Dong, C. Vitamin D Suppresses Th17 Cytokine Production by Inducing C/EBP Homologous Protein (CHOP) Expression. J. Biol. Chem. 2010, 285, 38751–38755. [Google Scholar] [CrossRef]
- Hupperts, R.; Smolders, J.; Vieth, R.; Holmøy, T.; Marhardt, K.; Schluep, M.; Killestein, J.; Barkhof, F.; Beelke, M.; Grimaldi, L.M.E.; et al. Randomized Trial of Daily High-Dose Vitamin D3 in Patients with RRMS Receiving Subcutaneous Interferon β-1a. Neurology 2019, 93, e1906–e1916. [Google Scholar] [CrossRef] [PubMed]
- Dörr, J.; Bäcker-Koduah, P.; Wernecke, K.-D.; Becker, E.; Hoffmann, F.; Faiss, J.; Brockmeier, B.; Hoffmann, O.; Anvari, K.; Wuerfel, J.; et al. High-Dose Vitamin D Supplementation in Multiple Sclerosis—Results from the Randomized EVIDIMS (Efficacy of Vitamin D Supplementation in Multiple Sclerosis) Trial. Mult. Scler. J. Exp. Transl. Clin. 2020, 6, 2055217320903474. [Google Scholar] [CrossRef] [PubMed]
- Camu, W.; Lehert, P.; Pierrot-Deseilligny, C.; Hautecoeur, P.; Besserve, A.; Deleglise, A.-S.J.; Payet, M.; Thouvenot, E.; Souberbielle, J.C. Cholecalciferol in Relapsing-Remitting MS: A Randomized Clinical Trial (CHOLINE). Neurol. Neuroimmunol. Neuroinflamm. 2019, 6, e597. [Google Scholar] [CrossRef] [PubMed]
- Hahn, J.; Cook, N.R.; Alexander, E.K.; Friedman, S.; Walter, J.; Bubes, V.; Kotler, G.; Lee, I.-M.; Manson, J.E.; Costenbader, K.H. Vitamin D and Marine Omega 3 Fatty Acid Supplementation and Incident Autoimmune Disease: VITAL Randomized Controlled Trial. BMJ 2022, 376, e066452. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.-Y.; Zhang, W.-G.; Chen, J.J.; Zhang, Z.-L.; Han, S.-F.; Qin, L.-Q. Vitamin D Intake and Risk of Type 1 Diabetes: A Meta-Analysis of Observational Studies. Nutrients 2013, 5, 3551–3562. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- O’Connell, K.; Sulaimani, J.; Basdeo, S.A.; Kinsella, K.; Jordan, S.; Kenny, O.; Kelly, S.B.; Murphy, D.; Heffernan, E.; Killeen, R.P.; et al. Effects of Vitamin D3 in Clinically Isolated Syndrome and Healthy Control Participants: A Double-Blind Randomised Controlled Trial. Mult. Scler. J. Exp. Transl. Clin. 2017, 3, 2055217317727296. [Google Scholar] [CrossRef]
- Laursen, J.H.; Søndergaard, H.B.; Sørensen, P.S.; Sellebjerg, F.; Oturai, A.B. Vitamin D Supplementation Reduces Relapse Rate in Relapsing-Remitting Multiple Sclerosis Patients Treated with Natalizumab. Mult. Scler. Relat. Disord. 2016, 10, 169–173. [Google Scholar] [CrossRef]
- Soilu-Hänninen, M.; Åivo, J.; Lindström, B.-M.; Elovaara, I.; Sumelahti, M.-L.; Färkkilä, M.; Tienari, P.; Atula, S.; Sarasoja, T.; Herrala, L.; et al. A Randomised, Double Blind, Placebo Controlled Trial with Vitamin D3 as an Add on Treatment to Interferon β-1b in Patients with Multiple Sclerosis. J. Neurol. Neurosurg. Psychiatry 2012, 83, 565–571. [Google Scholar] [CrossRef]
- Kampman, M.T.; Steffensen, L.H.; Mellgren, S.I.; Jørgensen, L. Effect of Vitamin D3 Supplementation on Relapses, Disease Progression, and Measures of Function in Persons with Multiple Sclerosis: Exploratory Outcomes from a Double-Blind Randomised Controlled Trial. Mult. Scler. 2012, 18, 1144–1151. [Google Scholar] [CrossRef]
- Kotb, M.A.; Kamal, A.M.; Aldossary, N.M.; Bedewi, M.A. Effect of Vitamin D Replacement on Depression in Multiple Sclerosis Patients. Mult. Scler. Relat. Disord. 2019, 29, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Darwish, H.; Haddad, R.; Osman, S.; Ghassan, S.; Yamout, B.; Tamim, H.; Khoury, S. Effect of Vitamin D Replacement on Cognition in Multiple Sclerosis Patients. Sci. Rep. 2017, 7, 45926. [Google Scholar] [CrossRef] [PubMed]
- Achiron, A.; Givon, U.; Magalashvili, D.; Dolev, M.; Liraz Zaltzman, S.; Kalron, A.; Stern, Y.; Mazor, Z.; Ladkani, D.; Barak, Y. Effect of Alfacalcidol on Multiple Sclerosis-Related Fatigue: A Randomized, Double-Blind Placebo-Controlled Study. Mult. Scler. 2015, 21, 767–775. [Google Scholar] [CrossRef] [PubMed]
- Golan, D.; Halhal, B.; Glass-Marmor, L.; Staun-Ram, E.; Rozenberg, O.; Lavi, I.; Dishon, S.; Barak, M.; Ish-Shalom, S.; Miller, A. Vitamin D Supplementation for Patients with Multiple Sclerosis Treated with Interferon-Beta: A Randomized Controlled Trial Assessing the Effect on Flu-like Symptoms and Immunomodulatory Properties. BMC Neurol. 2013, 13, 60. [Google Scholar] [CrossRef]
- Farsani, Z.S.; Behmanesh, M.; Sahraian, M.A. Interleukin-10 but Not Transforming Growth Factor-Β1 Gene Expression Is up-Regulated by Vitamin D Treatment in Multiple Sclerosis Patients. J. Neurol. Sci. 2015, 350, 18–23. [Google Scholar] [CrossRef]
- Etemadifar, M.; Janghorbani, M. Efficacy of High-Dose Vitamin D3 Supplementation in Vitamin D Deficient Pregnant Women with Multiple Sclerosis: Preliminary Findings of a Randomized-Controlled Trial. Iran J. Neurol. 2015, 14, 67–73. [Google Scholar]
- Shaygannejad, V.; Janghorbani, M.; Ashtari, F.; Dehghan, H. Effects of Adjunct Low-Dose Vitamin d on Relapsing-Remitting Multiple Sclerosis Progression: Preliminary Findings of a Randomized Placebo-Controlled Trial. Mult. Scler. Int. 2012, 2012, 452541. [Google Scholar] [CrossRef]
- Mosayebi, G.; Ghazavi, A.; Ghasami, K.; Jand, Y.; Kokhaei, P. Therapeutic Effect of Vitamin D3 in Multiple Sclerosis Patients. Immunol. Investig. 2011, 40, 627–639. [Google Scholar] [CrossRef]
- Sotirchos, E.S.; Bhargava, P.; Eckstein, C.; Van Haren, K.; Baynes, M.; Ntranos, A.; Gocke, A.; Steinman, L.; Mowry, E.M.; Calabresi, P.A. Safety and Immunologic Effects of High- vs. Low-Dose Cholecalciferol in Multiple Sclerosis. Neurology 2016, 86, 382–390. [Google Scholar] [CrossRef]
- Burton, J.M.; Kimball, S.; Vieth, R.; Bar-Or, A.; Dosch, H.-M.; Cheung, R.; Gagne, D.; D’Souza, C.; Ursell, M.; O’Connor, P. A Phase I/II Dose-Escalation Trial of Vitamin D3 and Calcium in Multiple Sclerosis. Neurology 2010, 74, 1852–1859. [Google Scholar] [CrossRef]
- Wingerchuk, D.M.; Lesaux, J.; Rice, G.P.A.; Kremenchutzky, M.; Ebers, G.C. A Pilot Study of Oral Calcitriol (1,25-Dihydroxyvitamin D3) for Relapsing-Remitting Multiple Sclerosis. J. Neurol. Neurosurg. Psychiatry 2005, 76, 1294–1296. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.S.; Liu, Y.; Gray, O.M.; Baker, J.E.; Kolbe, S.C.; Ditchfield, M.R.; Egan, G.F.; Mitchell, P.J.; Harrison, L.C.; Butzkueven, H.; et al. A Randomized Trial of High-Dose Vitamin D2 in Relapsing-Remitting Multiple Sclerosis. Neurology 2011, 77, 1611–1618. [Google Scholar] [CrossRef] [PubMed]
- Rolf, L.; Muris, A.-H.; Bol, Y.; Damoiseaux, J.; Smolders, J.; Hupperts, R. Vitamin D3 Supplementation in Multiple Sclerosis: Symptoms and Biomarkers of Depression. J. Neurol. Sci. 2017, 378, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Naghavi Gargari, B.; Behmanesh, M.; Shirvani Farsani, Z.; Pahlevan Kakhki, M.; Azimi, A.R. Vitamin D Supplementation Up-Regulates IL-6 and IL-17A Gene Expression in Multiple Sclerosis Patients. Int. Immunopharmacol. 2015, 28, 414–419. [Google Scholar] [CrossRef]
- Golan, D.; Staun-Ram, E.; Glass-Marmor, L.; Lavi, I.; Rozenberg, O.; Dishon, S.; Barak, M.; Ish-Shalom, S.; Miller, A. The Influence of Vitamin D Supplementation on Melatonin Status in Patients with Multiple Sclerosis. Brain Behav. Immun. 2013, 32, 180–185. [Google Scholar] [CrossRef]
- Hänninen, K.; Jääskeläinen, O.; Herukka, S.-K.; Soilu-Hänninen, M. Vitamin D Supplementation and Serum Neurofilament Light Chain in Interferon-Beta-1b-Treated MS Patients. Brain Behav. 2020, 10, e01772. [Google Scholar] [CrossRef]
- Kimball, S.M.; Ursell, M.R.; O’Connor, P.; Vieth, R. Safety of Vitamin D3 in Adults with Multiple Sclerosis. Am. J. Clin. Nutr. 2007, 86, 645–651. [Google Scholar] [CrossRef]
- Smolders, J.; Hupperts, R.; Barkhof, F.; Grimaldi, L.M.E.; Holmoy, T.; Killestein, J.; Rieckmann, P.; Schluep, M.; Vieth, R.; Hostalek, U.; et al. Efficacy of Vitamin D3 as Add-on Therapy in Patients with Relapsing–Remitting Multiple Sclerosis Receiving Subcutaneous Interferon Beta-1a: A Phase II, Multicenter, Double-Blind, Randomized, Placebo-Controlled Trial. J. Neurol. Sci. 2011, 311, 44–49. [Google Scholar] [CrossRef]
- Jelinek, G.A.; Marck, C.H.; Weiland, T.J.; Pereira, N.; van der Meer, D.M.; Hadgkiss, E.J. Latitude, Sun Exposure and Vitamin D Supplementation: Associations with Quality of Life and Disease Outcomes in a Large International Cohort of People with Multiple Sclerosis. BMC Neurol. 2015, 15, 132. [Google Scholar] [CrossRef]
- Hanaei, S.; Sahraian, M.A.; Mohammadifar, M.; Ramagopalan, S.V.; Ghajarzadeh, M. Effect of Vitamin D Supplements on Relapse Rate and Expanded Disability Status Scale (EDSS) in Multiple Sclerosis (MS): A Systematic Review and Meta-Analysis. Int. J. Prev. Med. 2021, 12, 42. [Google Scholar] [CrossRef]
- Jagannath, V.A.; Filippini, G.; Di Pietrantonj, C.; Asokan, G.V.; Robak, E.W.; Whamond, L.; Robinson, S.A. Vitamin D for the Management of Multiple Sclerosis. Cochrane Database Syst. Rev. 2018, 9, CD008422. [Google Scholar] [CrossRef] [PubMed]
- Xie, F.; Huang, T.; Lou, D.; Fu, R.; Ni, C.; Hong, J.; Ruan, L. Effect of Vitamin D Supplementation on the Incidence and Prognosis of Depression: An Updated Meta-Analysis Based on Randomized Controlled Trials. Front. Public Health 2022, 10, 903547. [Google Scholar] [CrossRef] [PubMed]
- Głąbska, D.; Kołota, A.; Lachowicz, K.; Skolmowska, D.; Stachoń, M.; Guzek, D. Vitamin D Supplementation and Mental Health in Multiple Sclerosis Patients: A Systematic Review. Nutrients 2021, 13, 4207. [Google Scholar] [CrossRef] [PubMed]

| PICOS Parameter | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Adult patients with MS, CIS, or radiologically isolated syndrome (RIS) as defined in the different versions of the McDonald criteria. All subgroups of MS patients [(relapsing remitting multiple sclerosis (RRMS), primary progressive, secondary progressive (SPMS), or progressive relapsing], regardless of gender, disease duration, degree of disability and MRI lesions, and baseline vitamin D levels. | |
| Intervention | Any form of vitamin D [vitamin D2 or vitamin D3, 25(OH)D3, 1α(OH)D3 or 1,25(OH)2D3] with or without associated supplementation in calcium. Any duration, dose, dosing frequency of supplementation. Any administration route. | Supplementation with multiple nutrients (other than calcium). Records were also excluded if data on vitamin D dosing were retrospectively obtained. |
| Comparison | With a comparison group (placebo, usual care or low-dose use of vitamin D) or without a comparison group (uncontrolled trials). | |
| Outcomes | Primary outcomes were the changes after vitamin D supplementation in
| Records were also excluded if MS patients retrospectively self-reported data on outcomes. |
| Study design | Articles/records published in English and in peer-reviewed journals or in recognized databases of trial registration. | Articles not published in English, methodological articles, reviews, meta-analyses, comments, letters to the editor, studies conducted in animals, case reports. |
| Refs. | First Author, Year Trial Registration Number | Country | Study Design | Study Group | Time |
|---|---|---|---|---|---|
| [22] | Dörr et al., 2020 NCT01440062 | Germany | Randomized, double-blind low-dose controlled | Interferon (IFN)-β1b RRMS/CIS | Not provided |
| [21,43] | Hupperts et al., 2019 Rolf et al., 2017 NCT01285401 | 11 European countries | Randomized, double-blind, placebo-controlled | IFN-β1a- treated RRMS | February 2011 to May 2015 |
| [23] | Camu et al., 2019 NCT01198132 | France | Randomized, double-blind, placebo-controlled | RRMS | January 2010 to June 2013 |
| [31] | Kotb et al., 2019 | Saudi Arabia | Uncontrolled | RRMS | 2013–2018 |
| [32] | Darwish et al., 2017 NCT01952483 | Lebanon | Uncontrolled | RRMS/CIS | Not provided |
| [27] | O’Connell et al., 2017 NCT01728922 | Ireland | Randomized, double-blind, placebo-controlled | CIS | November 2012 to June 2015 |
| [28] | Laursen et al., 2016 | Denmark | Uncontrolled | Natalizumab-treated RRMS | 2009–2010 |
| [39] | Sotirchos et al., 2016 NCT01024777 | USA | Randomized, double-blind, low-dose-controlled | RRMS | April 2010 to January 2013 |
| [35,44] | Farsani et al., 2015 Naghavi Gargari et al., 2015 IRCT2014011216181N1 | Iran | Uncontrolled | RRMS | November 2012 to October 2013 |
| [36] | Etemadifar et al., 2015 | Iran | Randomized, open-label, routine care-controlled | Pregnant women with MS | July 2011 to December 2012 |
| [33] | Achiron et al., 2015 | Israel | Randomized, double-blind, placebo-controlled | MS | Not provided |
| [34,45] | Golan et al., 2013a and 2013b NCT01005095 | Israel | Randomized, double-blind, low-dose-controlled | RRMS | November 2010 to April 2012 |
| [29,46] | Soilu-Hänninen et al., 2012 Hänninen et al., 2020 NCT01339676 | Finland | Randomized, double-blind, placebo-controlled | IFN-treated RRMS | March 2008 to August 2011 |
| [30] | Kampman et al., 2012 NCT00785473 | Norway | Randomized, double-blind, placebo-controlled | MS | November 2008 to September 2011 |
| [37] | Shaygannejad et al., 2012 IRCT201104166202N1 | Iran | Randomized, double-blind, placebo-controlled | RRMS | October 2007 to October 2008 |
| [42] | Stein et al., 2011 ACTRN12606000359538 | Australia | Randomized, double-blind, low-dose-controlled | RRMS | December 2006 to May 2009 |
| [38] | Mosayebi et al., 2011 | Iran | Randomized, double-blind, placebo-controlled | IFN-treated MS | October 2009 to April 2011 |
| [40,47] | Kimball et al., 2007 Burton et al., 2010 NCT00644904 | Canada | Randomized, open-label, controlled | RRMS | December 2003 to January 2005 |
| [41] | Wingerchuk et al., 2005 | USA | Uncontrolled | RRMS | March 1999 to March 2001 |
| Refs. | First Author, Year Trial Name | Number of CIS/MS Participants | Age at Baseline | Inclusion and Exclusion Criteria |
|---|---|---|---|---|
| [22] | Dörr et al., 2020 EVIDIMS trial | 53 | 41 ± 2.1 | Inclusion: patients with CIS or RRMS; age 18–65 years (y); EDSS score 0–6; no relapse in the last 30 days; IFN-β1b treatment >3 months. Exclusion: pregnancy; history of sarcoidosis; hepatopathy or renal dysfunction; nephrolithiasis; pseudo-hypoparathyroidism; vitamin D supplementation with more than 500 IU/d in the last 6 months; hypercalcemia or urine calcium/creatinine ratio > 1; concomitant medication with hydrochlorothiazide, digitoxin, digoxin, barbiturates, phenytoin; incompatibility with MRI. |
| [21,43] | Hupperts et al., 2019 Rolf et al., 2017 SOLAR trial | 229 | 34 ± 8.0 | Inclusion: RRMS; age 18–55 y; adequate renal and hepatic function; early-stage MS on brain or spinal MRI; first clinical event in the last 5 years; EDSS score lower than 4.0; active disease with either one relapse or MRI new lesion within the last 18 months; no or low vitamin D supplementation (lower than 1000 IU/d). Exclusion: lactation or pregnancy; other disease than MS that could explain symptoms; relapse in the last 30 days before inclusion; use of corticosteroids within 30 days before inclusion; complete transverse myelitis or bilateral optic neuritis; abnormalities of vitamin D metabolism other than low dietary intake or decreased sun exposure; urinary calcium higher than 1.0 mmol/mmol of creatinine or hypercalcemia (11 mg/dL); hepatic impairment (alanine or aspartate aminotransferase higher than three times the upper limit of normal (ULN); bilirubin higher than 1.5 times ULN if associated with any elevation of alanine aminotransferase or alkaline phosphatase; or alkaline phosphatase higher than 2.5 times ULN); drugs other than corticosteroids that affect vitamin D metabolism; vitamin D supplementation higher than 400 IU/d; conditions with susceptibility to hypercalcemia (e.g., treatment with digitalis or hydrochlorothiazide, arrhythmia or heart disease, nephrolithiasis). |
| [23] | Camu et al., 2019 CHOLINE trial | 129 | 38 ± 9.3 | Inclusion: patients with RRMS; age 18–65 y; serum 25(OH)D < 75 nM; treatment with IFN-β1a for 4 ± 2 months prior to randomization; EDSS 0–5; ≥1 relapse during the previous 2 y; stable disease over the last 30 days. Exclusion: medications affecting vitamin D metabolism other than corticosteroids; previous or ongoing hypercalcemia; estimated glomerular filtration rate (eGFR) lower than 60 mL/min. |
| [31] | Kotb et al., 2019 | 35 | 27 ± 4 | Inclusion: patients with RRMS; age ≥18 y; no exacerbations; regular treatment with IFN; no new MRI lesions. Exclusion: glucocorticoid treatment within 4 weeks prior to recruitment; disease-modifying drugs (DMD) other than IFN; vitamin D >1000 UI/d; use of glucocorticoid or relapse in the last 30 days; severe depression; pregnancy; serum creatinine >1.5 mg/dL; hypersensitivity to vitamin D; history of hyperparathyroidism, tuberculosis, nephrolithiasis, or sarcoidosis. |
| [32] | Darwish et al., 2017 | 88 | 34 ± 11 | Inclusion: patients with RIS, CIS, RRMS, SPMS; age ≥16 y; 25(OH)D <250 nM. Exclusion: not reported. |
| [27] | O’Connell et al., 2017 | 67 | 37 ± 8.7 (group 10,000 UI/d) 33 ± 4.6 (group 5000 UI/d) | Inclusion: patients with CIS; age 18–55 y; symptom onset in the last 3 months; more than one asymptomatic T2 lesions on brain MRI; no treatment with corticosteroids in the last month; no other DMD. Exclusion: disease other than MS that could explain symptoms; exacerbation in the last six weeks; treatment with any immunomodulating therapy in the last three months; steroids in the last month or any previous treatment with other immunosuppressant or mitoxantrone; no hypercalcemia, renal impairment, intolerance to vitamin D, parathyroid dysfunction, sarcoidosis; pregnancy or lack of contraception; prior or current treatment with thiazide diuretics or vitamin D supplementation (≥1000 IU/d). |
| [28] | Laursen et al., 2016 | 134 | 41 (23–63) | Inclusion: RRMS patients with natalizumab treatment for at least 1 year prior to enrolment. Exclusion: pregnancy; development of SPMS, cancer, anti-natalizumab antibodies. |
| [39] | Sotirchos et al., 2016 | 40 | 41 ± 8.1 | Inclusion: RRMS; age 18–55 y; serum 25(OH)D 50–125 nM. Exclusion: vitamin D supplementation >1000 IU; change of immunomodulatory therapy within the past 3 months; systemic glucocorticoid therapy or relapse in the last month; pregnancy; serum creatinine higher than 1.5 mg/dL; vitamin D intolerance; history of hyperparathyroidism, sarcoidosis, tuberculosis, or nephrolithiasis. |
| [35,44] | Farsani et al., 2015 Naghavi Gargari et al., 2015 | 32 | 31 ± 7.1 | Inclusion: RRMS; remission period; serum 25(OH)D <50 nM; EDSS score 0–5. Exclusion: treatment with steroid or immunosuppressive drugs. |
| [36] | Etemadifar et al., 2015 | 15 | 27 ± 2.4 | Inclusion: pregnant women with MS; age 20–40 y; stable neurological functioning for at least 1 month prior to study entry; EDSS score ≤ 6; serum 25(OH)D level < 50 nM. Exclusion: substantial disorders in psychiatric, hematologic, cardiac, endocrinological, renal, hepatic or metabolic functions; vitamin D3 supplement; any condition predisposing to hypercalcemia; nephrolithiasis; renal insufficiency. |
| [33] | Achiron et al., 2015 | 158 | 41 ± 9.8 | Inclusion: fatigue severity scale score ≥ 40; age 18–55 years; EDSS score > 5.5. Exclusion: relapse within 30 days before the study; serum calcium level > 10.5 mg/dL; history of hypersensitivity or intolerance to 1α(OH)D3 or related substances; a life-threatening and/or unstable clinical condition and/or alcohol or drug abuse. |
| [34,45] | Golan et al., 2013a and 2013b | 45 | 43 ± 12 | Inclusion: age ≥ 18 y; patients who continued to suffer from flu-like symptoms after 4 months of treatment with IFN-β; 25(OH)D blood levels lower than 75 nM; EDSS score lower than 7. Exclusion: intestinal malabsorption, cirrhosis, nephrotic syndrome, hyperthyroidism, eGFR less than 40 mL/min, rickets, hypoparathyroidism, hypercalcemia at baseline, known malignancy, granulomatous disorders and lymphomas; treatment with orlistat, anticonvulsants, rifampin, isoniazide, ketoconazole, leucovorin, 5FU, hydrochlorothiazide; arrhythmia; heart disease; nephrolithiasis; pregnancy. |
| [29,46] | Soilu-Hänninen et al., 2012 Hänninen et al., 2020 Finnish Vitamin D Study | 66 | 39 (range 22–53) | Inclusion: RRMS with IFN-β1b for at least 1 month; age 18–55 y; EDSS score ≤ 5.5; use of a contraceptive method. Exclusion: calcemia > 2.6 mM; serum 25(OH)D > 85 nM; primary hyperparathyroidism; pregnancy or lack of contraception; alcohol or drug abuse; immunomodulatory treatment other than IFN-β1b; intolerance to cholecalciferol or peanuts; treatment with digitalis, vitamin D3 analogs or vitamin D, calcitonin; any condition predisposing to hypercalcemia, sarcoidosis, nephrolithiasis or renal impairment; significant hypertension (higher than 180/110 mmHg); hyper- or hypothyroidism in the last year; a history of nephrolithiasis in the last 5 years; cardiac insufficiency or dysrhythmia; unstable ischemic heart disease; depression. |
| [30] | Kampman et al., 2012 | 68 | 40 ± 8 | Inclusion: RRMS; age 18–50 y; EDSS score ≤ 4.5. Exclusion: inability to walk more than 500 m; history of conditions affecting bone; lactation or pregnancy in the last 6 months; use of bone-active drugs other than intravenous methylprednisolone for the treatment of relapse; nephrolithiasis in the last 5 years; menopause; unwillingness to use appropriate contraception. |
| [37] | Shaygannejad et al. 2012 | 50 | 39 ± 8.4 | Inclusion: RRMS; age 15–60 y; EDSS score ≤ 6; stable neurological condition for more than 4 weeks prior to study; circulating 25(OH)D level higher than 100 nM. Exclusion: substantial disorders in psychiatric, neurological, cardiac, endocrinological, hematologic, hepatic, renal, or metabolic systems; treatment with digitalis, vitamin D supplementation; any condition predisposing to hypercalcemia, renal insufficiency nephrolithiasis; pregnancy. |
| [42] | Stein et al., 2011 | 23 | 34 [inter-quartile range (IQR) 30–49] | Inclusion: RRMS; age > 18 y; relapse in the last 2 years despite immunomodulatory treatment. Exclusion: primary or SPMS; pregnancy; clinical relapse or use of systemic glucocorticoid within the prior month; EDSS higher than 5; current DMD other than IFN or glatiramer acetate; elevated calcemia; creatinine higher than 0.2 mM; elevated serum uric acid; eGFR < 60 mL/min; |
| [38] | Mosayebi et al., 2011 | 59 | 34 ± 9 | Inclusion: MS; age 18–60 y; at least one relapse in the 12 months; more than three lesions on spinal or brain MRI; baseline EDSS score lower than 4.0. Exclusion: patients with CIS or progressive MS; clinical relapses during the study; use of digitalis; vitamin D supplementation; drug abuse; any condition pre-disposing to hypercalcemia; nephrolithiasis or renal impairment; pregnancy or lack of contraception; refusal to restrict dietary calcium. |
| [40,47] | Kimball et al., 2007 Burton et al., 2010 | 49 | 41 (range 22–54) | Inclusion: MS; age 18–55 y; EDSS score lower than 7.0. Exclusion: use of steroids within 30 days; relapse within 60 days; chemotherapy within 12 months; pregnancy/inadequate contraception; vitamin D intake higher than 4000 IU daily; serum 25(OH)D level > 150 nM; lymphoma or granulomatous disease; cardiac arrhythmia; kidney impairment; altered calcium metabolism. |
| [41] | Wingerchuk et al., 2005 | 15 | 36 (range 22–44) | Inclusion: RRMS; age 18–65 y; EDSS score 0–5.0; at least one clinical exacerbation in the previous year; contraindication to or patient’s desire against treatment with IFN-β and glatiramer acetate. Exclusion: progressive MS; use of glatiramer acetate, IFN-β, corticosteroid or immunosuppressive treatment within the previous two months; use of vitamin D supplementation or digitalis; any condition predisposing to hypercalcemia; nephrolithiasis or renal insufficiency; pregnancy or lack of contraception method; and refusal to restrict dietary calcium. |
| Refs. | First Author, Year | Number of Included Participants | Intervention | Duration (Months) | Effect on 25(OH)D Blood Levels |
|---|---|---|---|---|---|
| [22] | Dörr et al., 2020 | 53 | Oral vitamin D3 20,400 vs. 400 IU daily | 18 | From 48 (range 18–133) to 155 (130–200) nM |
| [21,43] | Hupperts et al., 2019 Rolf et al., 2017 | 229 | Oral vitamin D3 6670 IU daily for 1 month, followed by 14,007 IU daily for 11 months | 12 | From 50 (IQR 35–75) to 220 (160–250) nM |
| [23] | Camu et al., 2019 | 129 | Oral vitamin D3 100,000 IU every 2 weeks | 24 | From 49 ± 18 to 157 nM |
| [31] | Kotb et al., 2019 | 35 | Oral vitamin D3 10,000 IU daily | 12 | From 23 ± 9.8 to 86 ± 7.3 nM |
| [32] | Darwish et al., 2017 | 88 | Oral vitamin D3 10,000 IU daily | 3 | From 40 ± 16 to 123 ± 37 nM |
| [27] | O’Connell et al., 2017 | 67 | Oral vitamin D3 5000 or 10,000 IU daily | 6 | From 53 to 129 or 168 nM |
| [28] | Laursen et al., 2016 | 134 | Oral vitamin D3 2000 or 3000 or 4000 IU daily | 6 | From 34 to 33 (24–41) nM |
| [39] | Sotirchos et al., 2016 | 40 | Oral vitamin D3 10,000 vs. 400 IU daily | 6 | From 68 ± 22 to 155 nM |
| [35,44] | Farsani et al., 2015 | 32 | Oral vitamin D 50,000 IU weekly | 2 | From 31 ± 15 to 107 ± 43 nM |
| [36] | Etemadifar et al., 2015 | 15 | Oral vitamin D3. 50,000 weekly from 12 to 16 weeks of gestation | 5–6 | From 38 ± 7 to 84 ± 38 nM |
| [33] | Achiron et al., 2015 | 158 | Oral 1α(OH)D3 1 µg daily | 6 | Not provided |
| [34,45] | Golan et al., 2013a and 2013b | 45 | Oral vitamin D3. 75,000 IU every 3 weeks vs. 800 IU daily | 12 | From 48 ± 14 to 68 ± 11 or 123 ± 32 nM |
| [29,46] | Soilu-Hänninen et al., 2012; Hänninen et al., 2020 | 66 | Oral vitamin D3 20,000 IU weekly | 12 | From 54 (range 19–82) to 110 (67–163) nM |
| [30] | Kampman et al., 2012 | 68 | Oral vitamin D3 20,000 IU each week + 500 mg Ca if calcium intake < 500 mg daily | 24 | From 56 ± 29 to 121 nM |
| [37] | Shaygannejad et al., 2012 | 50 | Oral 1,25(OH)2D3 0.50 µg daily | 12 | Not provided |
| [42] | Stein et al., 2011 | 23 | Oral vitamin D2 7000 vs. 1000 IU daily | 6 | From 59 (IQR 47–61) to 120 (89–170)/ 69 (49–110) nM |
| [38] | Mosayebi et al., 2011 | 59 | Intra-muscular vitamin D3 300,000 IU monthly | 6 | From 25 to 140 nM |
| [40,47] | Kimball et al., 2007 Burton et al., 2010 | 49 | Oral vitamin D3 Escalating doses up to 40,000 IU daily for 7 months followed by 10,000 IU daily for 3 months, followed by 2 months without vitamin D + 1.2 g calcium throughout the study | 12 | From 73 (range 38–146) to 413 nM |
| [41] | Wingerchuk et al., 2005 | 15 | Oral 1,25(OH)2D3. Escalating doses from 0.5 to 2.5 µg daily | 11 | Not provided |
| Refs. | First Author, Year | Number Treated/Control Patients | Effects on Relapses |
|---|---|---|---|
| [22] | Dörr et al., 2020 | 28/25 | No difference in the cumulative number of relapses between the high-dose (n = 5) and low-dose (n = 7) vitamin D3 groups (p = 0.6) |
| [21] | Hupperts et al., 2019 | 98/88 | No difference in ARR between the vitamin D3-treated (0.28 ± 0.59) and placebo (0.41 ± 0.83) groups (p = 0.17). No difference in the proportion of patients who were free of relapses (78.8% vs. 75.0%, p = 0.47). |
| [23] | Camu et al., 2019 | 63/66 (post-hoc: 45/45) | Decreased rate ratio of relapses between the vitamin D3 and placebo groups (0.395, p = 0.01). A total of 19 relapses in the vitamin D3 group compared to 25 relapses in the placebo group. No difference in the time to first relapse [hazard ratio 0.801, 95% confidence interval (CI) 0.403–1.454, p = 0.43). |
| [27] | O’Connell et al., 2017 | 48/19 | ARR of 0.2 (n = 1 relapse reported in the vitamin D3 group receiving 5000 UI/day). No statistical analysis in comparison with the placebo group. |
| [28] | Laursen et al., 2016 | 43/0 | Each nM increase in 25(OH)D was independently associated with a −0.014 (95% CI −0.026 to −0.003) decrease in ARR (p = 0.02) in the vitamin D3-supplemented MS patients with baseline levels of 25(OH)D < 50 nM. |
| [39] | Sotirchos et al., 2016 | 19/21 | One relapse in each treatment arm (high dose vs. low dose of vitamin D3) during the study. No comparative statistical analysis. |
| [36] | Etemadifar et al., 2015 | 6/9 | Decrease in the mean number of relapses in the vitamin D3-treated and untreated groups, without statistical difference (−0.4, 95% CI −0.9–0.2, p < 0.06). |
| [33] | Achiron et al., 2015 | 80/78 | A reduction in the number of relapses (10.5% vs. 33%, p = 0.006) and an increase in the proportion of relapse-free patients (90% vs. 67%, p = 0.007) in the 1α(OH)D3-treated group. |
| [34] | Golan et al., 2013 | 24/21 | No significant change in ARR between the onset and the end of follow-up in the low-dose and high-dose vitamin D3-treated groups. |
| [29,46] | Soilu-Hänninen et al., 2012 Hänninen et al., 2020 | 34/32 | Decrease in ARR in the vitamin D3-supplemented (−47%) and placebo (−45%) groups, without statistical difference between groups. No significant difference in the time to first relapse between groups (hazard ratio 1.12, 95% CI 0.41 to 3.1). |
| [30] | Kampman et al., 2012 | 35/36 | No difference in the ARR between groups (ARR difference 0.06, 95% CI −0.08 to 0.20). |
| [37] | Shaygannejad et al., 2012 | 25/25 | 66% and 68% of patients remained relapse-free in the 1,25(OH)2D3 and placebo groups, respectively (odds-ratio 1.06, 95% CI 0.71–1.58). Significant decrease in ARR in the supplemented (−69%) and placebo (−62%) groups. |
| [42] | Stein et al., 2011 | 11/12 | Relapses occurred in four (36.5%) patients in the high-dose vitamin D2 group vs. none in the low-dose vitamin D2 (p = 0.04). |
| [40,47] | Kimball et al., 2007 Burton et al., 2010 | 25/24 | Decrease in ARR in the vitamin D3-supplemented (−41%) and control (−17%) groups, without statistical difference between groups (p = 0.09). No difference in the proportion of patients who were free of relapses (84% vs. 63%, p = 0.09). |
| [41] | Wingerchuk et al., 2005 | 15/0 | Relapses occurred in four (27%) patients supplemented with 1,25(OH)2D3. |
| Refs. | First Author, Year | Number Treated/ Control Patients | Baseline EDSS Treated/ Control | Effects on the EDSS Score |
|---|---|---|---|---|
| [22] | Dörr et al., 2020 | 21/17 | 2.0 ± 3.5 (range) /2.0 (5.5) | No difference in the EDSS score at the end of follow-up between the high-dose and low-dose vitamin D3 groups [2.0 (range 3.5) vs. 2.0 (5.5), p = 0.26] and in the change from baseline [0 (4) vs. 0 (2.5)], p = 0.64. |
| [21] | Hupperts et al., 2019 | 98/88 | Not provided | Similar proportion of patients who were free from EDSS progression at week 48 between the high-dose vitamin D3 and placebo groups (70.8% vs. 75.9%, p = 0.39). |
| [23] | Camu et al., 2019 | 63/66 (post hoc: 45/45) | 1.7 ± 1.4/ 1.2 ± 1.2 | Lower progression of the EDSS score in the vitamin D3 group (−0.06 ± 0.78) than in the placebo group (0.32 ± 0.87, 95% CI −0.614 to −0.043; p = 0.03). Mean decrease of EDSS of −0.003 per 1 nM increase of 25(OH)D concentration (95% CI −0.006 to −0.001; p = 0.006). |
| [31] | Kotb et al., 2019 | 35/0 | 2.2 ± 0.5 | Higher mean EDSS at end of the follow-up (2.6 ± 0.5) compared to baseline (p = 0.02). |
| [27] | O’Connell et al., 2017 | 48/19 | 0.9 ± 1.0/ 0.9 ± 1.2/ 0.4 ± 0.5 | No significant difference in the EDSS score between groups at any time point. No quantitative data provided. |
| [35] | Farsani et al., 2015 | 32/0 | 2.1 ± 1.1 | Decrease in the mean EDSS score after vitamin D treatment to 1.89 ± 1.08 (p = 0.0036). No correlation between the EDSS score and 25(OH)D levels. |
| [36] | Etemadifar et al., 2015 | 6/9 | 1.2 ± 0.3/ 1.3 ± 0.4 | Lower mean EDSS score in the vitamin D3-supplemented group compared to the routine care group at month 6 after delivery (1.1 ± 0.2 vs. 1.7 ± 0.6, p < 0.05). |
| [33] | Achiron et al., 2015 | 80/78 | 2.5 ± 1.6/ 2.8 ± 1.6 | No significant change in the EDSS score in patients treated with 1,25(OH)2D3 or the placebo (0.06 vs. 0.31, p = 0.10). |
| [34,45] | Golan et al., 2013a et 2013b | 15/15 | 2.9 ± 2.0/ 3.6 ± 2.2 | No significant change in the EDSS score in each group. EDSS at the end of vitamin D3 treatment: 3.8 ± 2 vs. 3.4 ± 2.4 (no statistical analysis). |
| [29,46] | Soilu-Hänninen et al., 2012 Hänninen et al., 2020 | 32/30 | 2.0 ± 0.2/ 1.5 ± 1.2 | Slight decrease in the mean EDSS score in the vitamin D3 group (to 1.8 ± 0.2). Similar EDSS score in the placebo group during the study (to 1.6 ± 1.3, p = 0.071). |
| [30] | Kampman et al., 2012 | 35/36 | Not provided | No significant difference between groups in the absolute difference in EDSS (−0.01, 95% CI −0.35 to 0.35, p = 0.97). |
| [37] | Shaygannejad et al., 2012 | 25/25 | 1.6 ± 0.7/ 1.7 ± 1.2 | No significant difference in the EDSS score at the end of treatment between the 1,25(OH)2D3 and placebo groups (1.63 ± 0.70 vs. 1.94 ± 1.41). Lower progression in the EDSS score during the study in the 1,25(OH)2D3 group than in the placebo group (difference 0.21, p < 0.05). |
| [42] | Stein et al., 2011 | 11/12 | 2.5 (IQR 2–4)/ 2.0 (1.0–3.0) | Higher EDSS score at the end of the follow-up in the high-dose vitamin D2 group: 3 (IQR 2–4) vs. 2 (1–2) in the low-dose group (p = 0.04). |
| [38] | Mosayebi et al., 2011 | 26/33 | 2.1 ± 1.2/ 2.5 ± 1.1 | No significant difference in the EDSS score between the vitamin D3-treated and control groups (EDSS scores after treatment: 2.31 ± 1.3 and 2.67 ± 1.25, respectively). |
| [40,47] | Kimball et al., 2007 Burton et al., 2010 | 25/24 | 1.5 ± 1.6/ 1.2 ± 1.6 | No significant difference in the change in the EDSS score during the trial between the vitamin D3 and placebo groups (−0.23 vs. 0.30, p > 0.05). Lower proportion of patients who completed the trial with a higher EDSS score in the vitamin D3 group than in the placebo group (8 vs. 38%, p = 0.02). |
| [41] | Wingerchuk et al., 2005 | 15/0 | 1.9 (range 0–4.0) | Mean EDSS at the end of the study: 2.2. Median EDSS change = 0 (range −1.0 to 2.0). 27% of patients worsened ≥1 EDSS point. |
| Refs. | First Author, Year | No Treated/Control Patients | Effects on MRI Lesions |
|---|---|---|---|
| [22] | Dörr et al., 2020 EVIDIMS trial | 21/17 | Lower number of T2-weighted lesions at month 18 in the high-dose vitamin D3 group compared to the low-dose vitamin D3 group [53.4 ± 7.3 (SE) vs. 84.1 ± 13.5], but the change from baseline did not differ between the two groups (1.3 ± 0.1 vs. 2.1 ± 1.4, p = 0.15). The change from baseline in the T2 lesion volume did not differ between the two groups (0.1 ± 0.1 vs. 0.2 ± 0.3 mL, p = 0.98). The cumulative number of new Gd lesions was 2 and 14 in the high-dose and low-dose groups (p = 0.09). |
| [21] | Hupperts et al., 2019 SOLAR trial | 98/88 | 32% reduction in the number of new Gd-enhancing or new/enlarging T2 lesions in the vitamin D3 group compared to the placebo at week 48 (incidence rate ratio 0.68, p = 0.005). No difference between treatments in the proportion of patients free from new T1 hypointense lesions at week 48 (79 vs. 64%, p = 0.30). Higher difference in the change in the total volume of T2 lesions (p = 0.035). |
| [23] | Camu et al., 2019 CHOLINE trial | 44/41 | Significant reduction in the volume of hypointense T1-weighted lesions (−312 mm3, 95% CI −596 to −29, p = 0.03) and new T1 lesions (rate ratio 0.494, 95% CI 0.267–0.913, p = 0.03) in vitamin D3-treated patients compared to the placebo. No difference in the number of Gd-enhancing T1 and new T2 lesions. |
| [27] | O’Connell et al., 2017 | 19/7 | No difference in the number of new T2 lesions or new Gd-enhancing lesions between groups at month 6. The number of CIS patients with new disease activity based on MRI was 50% (10,000 IU/day of vitamin D3), 56% (5000 IU/day of vitamin D3), and 43% (placebo). |
| [29] | Soilu-Hänninen et al., 2012 Finnish Vitamin D Study | 32/30 | Lower number of Gd-enhancing T1 lesions in the vitamin D3-treated group compared to the placebo at month 12 (0.1 ± 0.2 vs. 0.7 ± 3.5, p = 0.004). No difference in the number of new/enlarging T2 lesions (0.5 ± 1.0 vs. 1.1 ± 2.2, p = 0.29) and in the change in the total volume of T2 lesions (83 ± 128 vs. 287 ± 283 mm3, p = 0.105). |
| [42] | Stein et al., 2011 | 11/12 | No difference in the cumulative number of Gd-enhancing lesions in the high-dose vitamin D2-treated group compared to the low-dose vitamin D2 group (14 ± 0.2 vs. 0.7 ± 3.5, p = 0.004), in the number of patients with new lesions and in the change in the total volume of T2 lesions [−330 (IQR −950 to −30) vs. −95 (−310 to −25) mm3, p = 0.6). |
| [38] | Mosayebi et al., 2011 | 26/33 | No difference in the number of Gd-enhancing lesions between the MS patients taking 300,000 IU monthly of vitamin D3 or the placebo (from 1.5 ± 1 to 1.9 ± 0.7 and 1.6 ± 0.8 to 2.0 ± 1.0, respectively). |
| [47] | Kimball et al., 2007 | 12/0 | Reduction in the mean number of Gd-enhancing lesions after vitamin D3 supplementation (from 1.75 ± 1.42 to 0.83 ± 0.72, p = 0.03). |
| [41] | Wingerchuk et al., 2005 | 15/0 | New T2-weighted lesions were found in 43% of patients at week 24 and in 29% at week 48. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Langlois, J.; Denimal, D. Clinical and Imaging Outcomes after Vitamin D Supplementation in Patients with Multiple Sclerosis: A Systematic Review. Nutrients 2023, 15, 1945. https://doi.org/10.3390/nu15081945
Langlois J, Denimal D. Clinical and Imaging Outcomes after Vitamin D Supplementation in Patients with Multiple Sclerosis: A Systematic Review. Nutrients. 2023; 15(8):1945. https://doi.org/10.3390/nu15081945
Chicago/Turabian StyleLanglois, Julie, and Damien Denimal. 2023. "Clinical and Imaging Outcomes after Vitamin D Supplementation in Patients with Multiple Sclerosis: A Systematic Review" Nutrients 15, no. 8: 1945. https://doi.org/10.3390/nu15081945
APA StyleLanglois, J., & Denimal, D. (2023). Clinical and Imaging Outcomes after Vitamin D Supplementation in Patients with Multiple Sclerosis: A Systematic Review. Nutrients, 15(8), 1945. https://doi.org/10.3390/nu15081945






