The Nutritional Quality of Food Provision at UK Government-Funded Holiday Clubs: A Cross-Sectional Analysis of Energy and Nutrient Content
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Overview
2.2. Assessment against School Food Standards
2.3. Estimation of Nutrient Profile
2.4. Development of the Meal Quality Index
2.5. Statistical Analysis
3. Results
3.1. School Foods Standards Adherence
3.2. Menu Characteristics and Quality Scoring
3.3. Hot and Cold Menu Variants
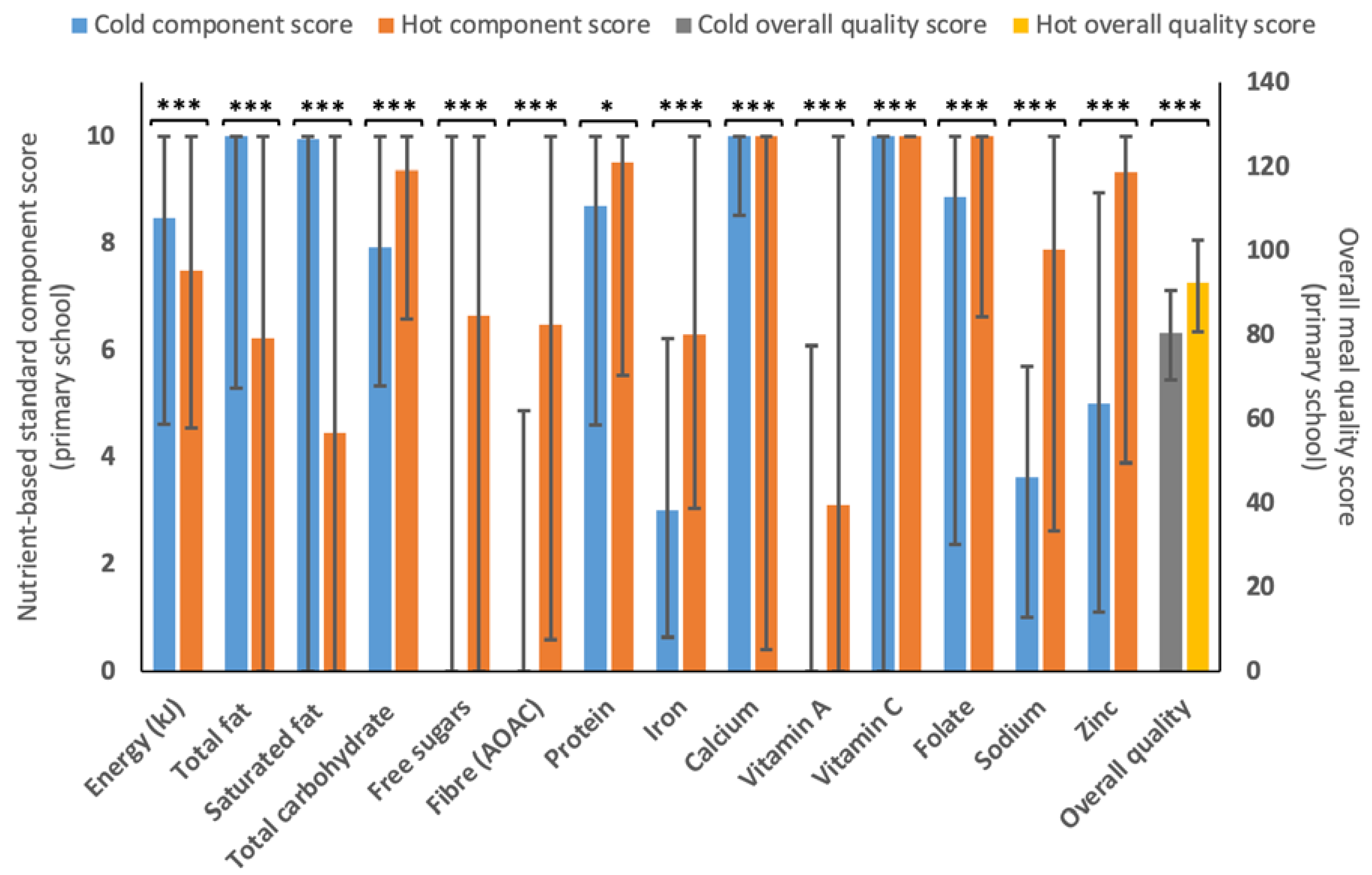
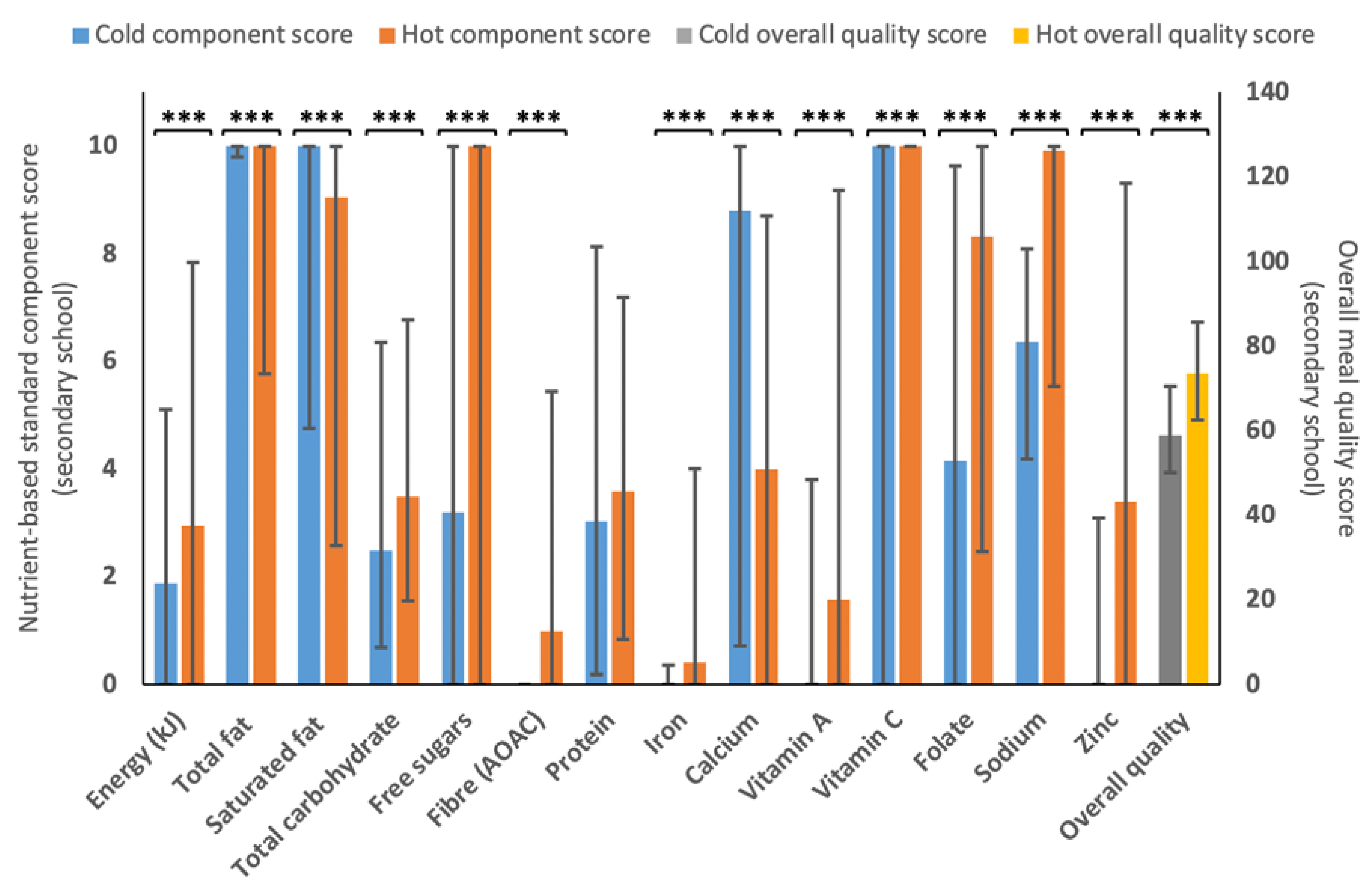
3.4. Vegetarian and Non-Vegetarian Menu Variants
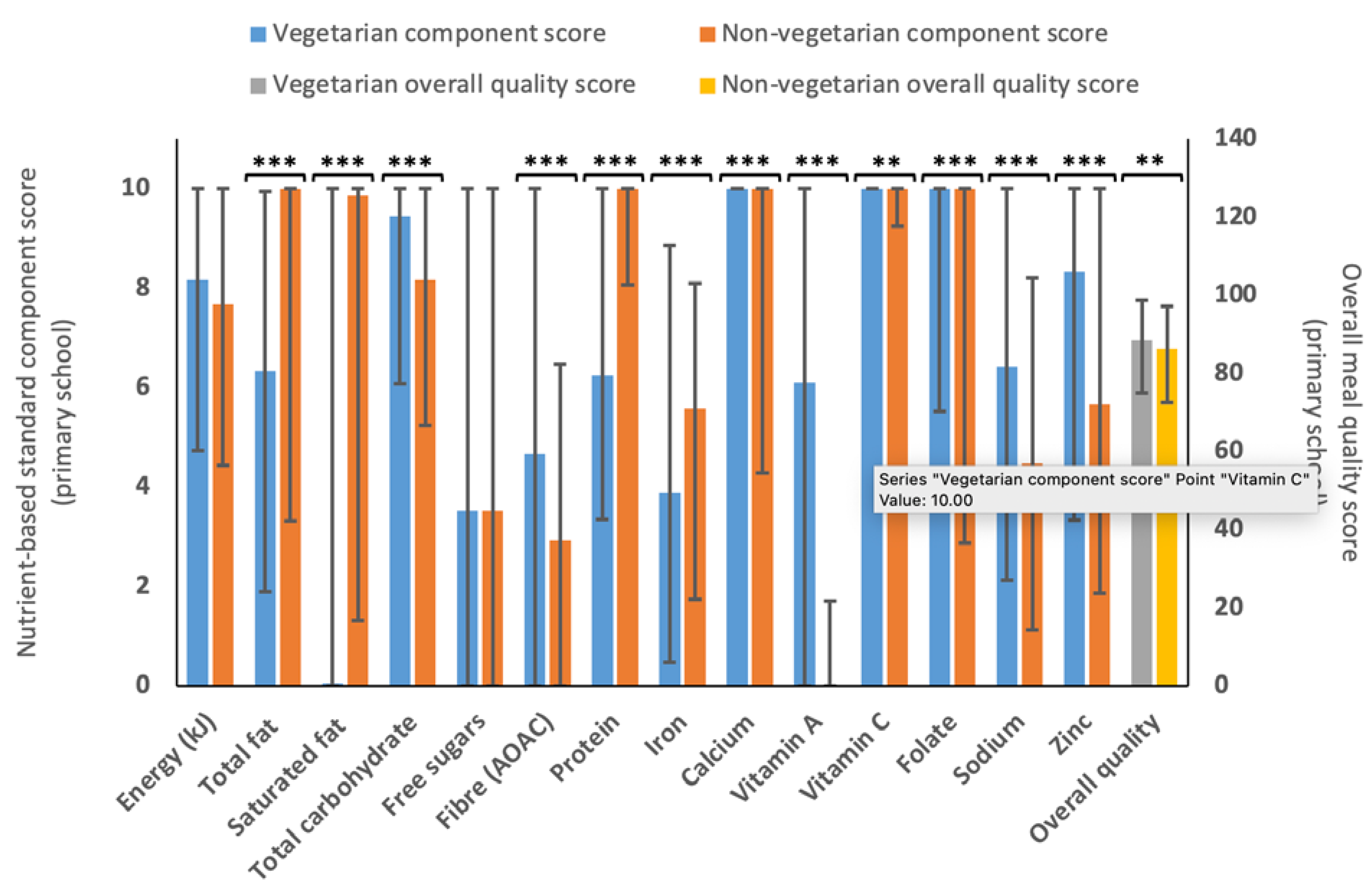
4. Discussion
4.1. Adherence to School Food Standards
4.2. Overall Meal Quality and Nutrient Content
4.3. Nutritional Quality of Hot and Cold Menu Variants
4.4. Nutritional Quality of Vegetarian and Non-Vegetarian Menu Variants
4.5. Strengths and Limitations
4.6. Future Work and Impact of Findings
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pereira, A.L.; Handa, S.; Holmqvist, G. Prevalence and Correlates of Food Insecurity among Children across the Globe; UNICEF: New York, NY, USA, 2017; Available online: https://www.unicef-irc.org/publications/pdf/IWP_2017_09.pdf (accessed on 5 April 2023).
- Francis-Devine, B.; Danechi, S.; Tyler, G. House of Commons Library: Briefing Paper 9209, 30 April 2021: Food poverty: Households, Food Banks and Free School Meals. 2021. Available online: https://researchbriefings.files.parliament.uk/documents/CBP-9209/CBP-9209.pdf (accessed on 5 April 2023).
- Office for Health Improvement & Disparities. Childhood Obesity: Applying All Our Health; Public Health England: London, UK, 2022. Available online: https://www.gov.uk/government/publications/childhood-obesity-applying-all-our-health/childhood-obesity-applying-all-our-health (accessed on 5 April 2023).
- Orr, J.; Freer, J.; Morris, J.K.; Hancock, C.; Walton, R.; Dunkel, L.; Storr, H.L.; Prendergast, A.J. Regional differences in short stature in England between 2006 and 2019: A cross-sectional analysis from the National Child Measurement Programme. PLoS Med. 2021, 18, e1003760. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 2015, 4, 187. [Google Scholar]
- Vilcins, D.; Sly, P.D.; Jagals, P. Environmental risk factors associated with child stunting: A systematic review of the literature. Ann. Glob. Health 2018, 84, 551. [Google Scholar] [CrossRef] [PubMed]
- Beverley, B.; David, C.; Kerry, S.J.; Polly, P.; Caireen, R.; Toni, S.; Gillian, S. National Diet and Nutrition Survey Rolling programme Years 9 to 11 (2016/2017 to 2018/2019)-a Survey Carried Out on Behalf of Public Health England and the Food Standards Agency. 2020. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/943114/NDNS_UK_Y9-11_report.pdf (accessed on 5 April 2023).
- World Health Organization. Malnutrition. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 5 March 2023).
- Quek, Y.H.; Tam, W.W.; Zhang, M.W.; Ho, R.C. Exploring the association between childhood and adolescent obesity and depression: A meta-analysis. Obes. Rev. 2017, 18, 742–754. [Google Scholar] [CrossRef] [PubMed]
- Haapala, E.A.; Eloranta, A.-M.; Venäläinen, T.; Schwab, U.; Lindi, V.; Lakka, T.A. Associations of diet quality with cognition in children–the Physical Activity and Nutrition in Children Study. Br. J. Nutr. 2015, 114, 1080–1087. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.; Khandpur, N.; Neri, D.; Touvier, M.; Huybrechts, I.; Millett, C.; Vamos, E.P. Association between childhood consumption of ultraprocessed food and adiposity trajectories in the Avon Longitudinal Study of parents and children birth cohort. JAMA Pediatr. 2021, 175, e211573. [Google Scholar] [CrossRef]
- Grey, K.; Gonzales, G.B.; Abera, M.; Lelijveld, N.; Thompson, D.; Berhane, M.; Abdissa, A.; Girma, T.; Kerac, M. Severe malnutrition or famine exposure in childhood and cardiometabolic non-communicable disease later in life: A systematic review. BMJ Glob. Health 2021, 6, e003161. [Google Scholar] [CrossRef]
- Department for Education. National School Breakfast Club. 2022. Available online: https://www.gov.uk/guidance/national-school-breakfast-club-programme (accessed on 5 March 2023).
- Department for Education. Free School Meals: Guidance for Schools and Local Authorities. 2022. Available online: https://www.gov.uk/government/publications/free-school-meals-guidance-for-schools-and-local-authorities (accessed on 5 March 2023).
- Forsey, A. Hungry Holidays: A Report on Hunger amongst Children during School Holidays; Feeding Britain: Glasgow, UK, 2017. [Google Scholar]
- Long, R.; Danechi, S. School Meals and Nutritional Standards (England). Available online: https://commonslibrary.parliament.uk/research-briefings/sn04195/ (accessed on 5 March 2023).
- Department for Education. Holiday Activities and Food Programme 2022. Available online: https://www.gov.uk/government/publications/holiday-activities-and-food-programme/holiday-activities-and-food-programme-2021 (accessed on 5 March 2023).
- Cox, C.; Campbell-Jack, D.; Blades, R. Evaluation of the 2021 Holiday Activities and Food Programme: Research Report: March 2022. 2022. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1065868/Evaluation_of_the_2021_holiday_activities_and_food_programme.pdf (accessed on 5 April 2023).
- Department for Education. School Food Standards Practical Guide. 2022. Available online: https://www.gov.uk/government/publications/school-food-standards-resources-for-schools/school-food-standards-practical-guide (accessed on 5 March 2023).
- Crilley, E.; Brownlee, I.; Defeyter, M.A. The diet of children attending a holiday programme in the UK: Adherence to UK food-based dietary guidelines and school food standards. Int. J. Environ. Res. Public Health 2021, 19, 55. [Google Scholar] [CrossRef]
- Mann, E.; Widdison, C.; Defeyter, M.A. Implementing holiday provision programmes: A qualitative investigation of the experiences of senior stakeholders. Open J. Soc. Sci. 2020, 8, 286. [Google Scholar] [CrossRef]
- Defeyter, M.; Stretesky, P.; Sattar, Z.; Crilley, E. Evaluation of ‘a Day Out, Not a Handout’holiday Provision Programme; Northumbria University Newcastle: Newcastle upon Tyne, UK, 2018. [Google Scholar]
- Morgan, K.; McConnon, L.; Van Godwin, J.; Hawkins, J.; Bond, A.; Fletcher, A. Use of the school setting during the summer holidays: Mixed-methods evaluation of food and fun clubs in wales. J. Sch. Health 2019, 89, 829–838. [Google Scholar] [CrossRef]
- Shinwell, J.; Finlay, E.; Allen, C.; Defeyter, G. An Evaluation of Children in Northern Ireland’s Summer 2019 Holiday Provision. 2020. Available online: http://www.ci-ni.org.uk/wp-content/uploads/Evaluation-of-CiNIs-Summer-2019-Holiday-Projects-1.pdf (accessed on 5 April 2023).
- Public Health England. The Eatwell Guide. Available online: https://www.gov.uk/government/publications/the-eatwell-guide (accessed on 5 March 2023).
- Gil, Á.; de Victoria, E.M.; Olza, J. Indicators for the evaluation of diet quality. Nutr. Hosp. 2015, 31, 128–144. [Google Scholar] [PubMed]
- Gorgulho, B.M.; Pot, G.K.; Sarti, F.M.; Marchioni, D. Indices for the assessment of nutritional quality of meals: A systematic review. Br. J. Nutr. 2016, 115, 2017–2024. [Google Scholar] [CrossRef] [PubMed]
- Sabinsky, M.S.; Toft, U.; Andersen, K.K.; Tetens, I. Development and validation of a Meal Index of dietary Quality (Meal IQ) to assess the dietary quality of school lunches. Public Health Nutr. 2012, 15, 2091–2099. [Google Scholar] [CrossRef] [PubMed]
- Patterson, E.; Quetel, A.-K.; Lilja, K.; Simma, M.; Olsson, L.; Elinder, L.S. Design, testing and validation of an innovative web-based instrument to evaluate school meal quality. Public Health Nutr. 2013, 16, 1028–1036. [Google Scholar] [CrossRef]
- Forner, F.; Volkhardt, I.; Meier, T.; Christen, O.; Stangl, G.I. The nutriRECIPE-Index–development and validation of a nutrient-weighted index for the evaluation of recipes. BMC Nutr. 2021, 7, 74. [Google Scholar] [CrossRef]
- Verger, E.O.; Eussen, S.; Holmes, B.A. Evaluation of a nutrient-based diet quality index in UK young children and investigation into the diet quality of consumers of formula and infant foods. Public Health Nutr. 2016, 19, 1785–1794. [Google Scholar] [CrossRef]
- Verger, E.O.; Mariotti, F.; Holmes, B.A.; Paineau, D.; Huneau, J.-F. Evaluation of a diet quality index based on the probability of adequate nutrient intake (PANDiet) using national French and US dietary surveys. PLoS ONE 2012, 7, e42155. [Google Scholar] [CrossRef]
- Leitzmann, C. Vegetarian nutrition: Past, present, future. Am. J. Clin. Nutr. 2014, 100, 496S–502S. [Google Scholar] [CrossRef]
- Defeyter, G.; Stretesky, P.; Pepper, G.; Shinwell, J. BRING IT ON BRUM 2021; Northumbria University: Newcastle upon Tyne, UK, 2022. [Google Scholar]
- Public Health England. Composition of Foods Integrated Dataset (CoFID). Available online: https://www.gov.uk/government/publications/composition-of-foods-integrated-dataset-cofid#:~:text=The%20'Composition%20of%20Foods%20Integrated,recipes%20within%20the%20pork%20section (accessed on 5 March 2023).
- Department for Education. Portion Sizes and Food Groups. 2023. Available online: https://www.gov.uk/government/publications/school-food-standards-resources-for-schools/portion-sizes-and-food-groups (accessed on 5 March 2023).
- Davies, O.H.; Suleiman, S.; Nicholas, J.; Bradbury, J.; Msebele, S.; Prior, G.; Hall, L.; Wreford, S.; Jarvis, L.; McGee, A. Food portion weights in primary and secondary school lunches in England. J. Hum. Nutr. Diet. 2008, 21, 46–62. [Google Scholar] [CrossRef]
- Agnoli, C.; Baroni, L.; Bertini, I.; Ciappellano, S.; Fabbri, A.; Papa, M.; Pellegrini, N.; Sbarbati, R.; Scarino, M.; Siani, V. Position paper on vegetarian diets from the working group of the Italian Society of Human Nutrition. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 1037–1052. [Google Scholar] [CrossRef]
- Melina, V.; Craig, W.; Levin, S. Position of the Academy of Nutrition and Dietetics: Vegetarian diets. J. Acad. Nutr. Diet. 2016, 116, 1970–1980. [Google Scholar] [CrossRef] [PubMed]
- Louie, J.C.Y.; Moshtaghian, H.; Boylan, S.; Flood, V.M.; Rangan, A.; Barclay, A.; Brand-Miller, J.; Gill, T. A systematic methodology to estimate added sugar content of foods. Eur. J. Clin. Nutr. 2015, 69, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Swan, G.E.; Powell, N.A.; Knowles, B.L.; Bush, M.T.; Levy, L.B. A definition of free sugars for the UK. Public Health Nutr. 2018, 21, 1636–1638. [Google Scholar] [CrossRef]
- Public Health England. Appendix AA Calculation of Free Sugars and AOAC Fibre in the NDNS RP. Available online: https://s3.eu-west-2.amazonaws.com/fsa-catalogue2/NDNS+Y1-9_Appendix+AA_Calculation+of+free+sugars+and+AOAC+fibre_FINAL.pdf (accessed on 5 March 2023).
- Scottish Government. Healthy Eating in Schools: Guidance 2020. Available online: https://www.gov.scot/publications/healthy-eating-schools-guidance-2020/ (accessed on 5 March 2023).
- Scientific Advisory Committee on Nutrition. Salt and Health; The Stationery Office: London, UK, 2003. [Google Scholar]
- Scientific Advisory Committee on Nutrition. Dietary Reference Values for Energy; The Stationery Office: London, UK, 2012. [Google Scholar]
- Scientific Advisory Committee on Nutrition. Carbohydrates and Health Report. Public Health England 2015. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/445503/SACN_Carbohydrates_and_Health.pdf (accessed on 5 April 2023).
- Brownlee, I.A.; Low, J.; Duriraju, N.; Chun, M.; Ong, J.X.Y.; Tay, M.E.; Hendrie, G.A.; Santos-Merx, L. Evaluation of the proximity of Singaporean children’s dietary habits to food-based dietary guidelines. Nutrients 2019, 11, 2615. [Google Scholar] [CrossRef] [PubMed]
- Savarino, G.; Corsello, A.; Corsello, G. Macronutrient balance and micronutrient amounts through growth and development. Ital. J. Pediatr. 2021, 47, 1–14. [Google Scholar] [CrossRef]
- Crawley, H. Nutrient-Based Standards for School Food: A Summary of the Standards and Recommendations of the Caroline Walker Trust and the National Heart Forum; National Heart Forum/Caroline Walker Trust: London, UK, 2005. [Google Scholar]
- Das, J.K.; Salam, R.A.; Thornburg, K.L.; Prentice, A.M.; Campisi, S.; Lassi, Z.S.; Koletzko, B.; Bhutta, Z.A. Nutrition in adolescents: Physiology, metabolism, and nutritional needs. Ann. N. Y. Acad. Sci. 2017, 1393, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. Dietary Reference Values. A Guide; HMSO: London, UK, 1991. [Google Scholar]
- Pike, V.; Zlotkin, S. Excess micronutrient intake: Defining toxic effects and upper limits in vulnerable populations. Ann. N. Y. Acad. Sci. 2019, 1446, 21–43. [Google Scholar] [CrossRef] [PubMed]
- Tay, M.E.; Foster, E.; Stevenson, L.; Brownlee, I. The Adherence of Singaporean Students in Different Educational Institutions to National Food-Based Dietary Guidelines. Nutrients 2020, 12, 2995. [Google Scholar] [CrossRef]
- Wilcox, M.D.; Chater, P.I.; Stanforth, K.J.; Williams, R.; Brownlee, I.A.; Pearson, J.P. A Pilot Pre and Post 4 Week Intervention Evaluating the Effect of a Proprietary, Powdered, Plant Based Food on Micronutrient Status, Dietary Intake, and Markers of Health in a Healthy Adult Population. Front. Nutr. 2022, 9, 1545. [Google Scholar] [CrossRef]
- Osowski, C.P.; Lindroos, A.K.; Barbieri, H.E.; Becker, W. The contribution of school meals to energy and nutrient intake of Swedish children in relation to dietary guidelines. Food Nutr. Res. 2015, 59, 27563. [Google Scholar] [CrossRef]
- Secretary of State for Education. The Requirements for School Food (England) Regulations 2014. 2014. Available online: https://www.legislation.gov.uk/uksi/2014/1603/made (accessed on 5 April 2023).
- Food Standards Agency. School Food Standards Compliance Pilot Underway in 18 Local Authorities across England. Available online: https://www.food.gov.uk/news-alerts/news/school-food-standards-compliance-pilot-underway-in-18-local-authorities-across-england (accessed on 12 March 2023).
- Edwards, C.A.; Xie, C.; Garcia, A.L. Dietary fibre and health in children and adolescents. Proc. Nutr. Soc. 2015, 74, 292–302. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.; Toumpakari, Z.; Papadaki, A. Social gradients and physical activity trends in an obesogenic dietary pattern: Cross-sectional analysis of the UK National Diet and Nutrition Survey 2008–2014. Nutrients 2018, 10, 388. [Google Scholar] [CrossRef] [PubMed]
- Donker, A.E.; van der Staaij, H.; Swinkels, D.W. The critical roles of iron during the journey from fetus to adolescent: Developmental aspects of iron homeostasis. Blood Rev. 2021, 50, 100866. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Wessling-Resnick, M. Iron and mechanisms of emotional behavior. J. Nutr. Biochem. 2014, 25, 1101–1107. [Google Scholar] [CrossRef]
- Jáuregui-Lobera, I. Iron deficiency and cognitive functions. Neuropsychiatr. Dis. Treat. 2014, 10, 2087–2095. [Google Scholar] [CrossRef]
- Abdelhamid, A.S.; Martin, N.; Bridges, C.; Brainard, J.S.; Wang, X.; Brown, T.J.; Hanson, S.; Jimoh, O.F.; Ajabnoor, S.M.; Deane, K.H. Polyunsaturated fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2018, 2018, CD012345. [Google Scholar]
- Schwingshackl, L.; Hoffmann, G. Monounsaturated fatty acids, olive oil and health status: A systematic review and meta-analysis of cohort studies. Lipids Health Dis. 2014, 13, 1–15. [Google Scholar] [CrossRef]
- Te Morenga, L.; Montez, J.M. Health effects of saturated and trans-fatty acid intake in children and adolescents: Systematic review and meta-analysis. PLoS ONE 2017, 12, e0186672. [Google Scholar] [CrossRef]
- Hooper, L.; Martin, N.; Jimoh, O.F.; Kirk, C.; Foster, E.; Abdelhamid, A.S. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst. Rev. 2020, 5, CD011737. [Google Scholar] [CrossRef]
- Evans, C.E.; Cleghorn, C.L.; Greenwood, D.C.; Cade, J.E. A comparison of British school meals and packed lunches from 1990 to 2007: Meta-analysis by lunch type. Br. J. Nutr. 2010, 104, 474–487. [Google Scholar] [CrossRef]
- Evans, C.E.; Mandl, V.; Christian, M.S.; Cade, J.E. Impact of school lunch type on nutritional quality of English children’s diets. Public Health Nutr. 2016, 19, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.E.L.; Melia, K.E.; Rippin, H.L.; Hancock, N.; Cade, J. A repeated cross-sectional survey assessing changes in diet and nutrient quality of English primary school children’s packed lunches between 2006 and 2016. BMJ Open 2020, 10, e029688. [Google Scholar] [CrossRef] [PubMed]
- Haney, E.; Parnham, J.C.; Chang, K.; Laverty, A.A.; Von Hinke, S.; Pearson-Stuttard, J.; White, M.; Millett, C.; Vamos, E.P. Dietary quality of school meals and packed lunches: A national study of primary and secondary schoolchildren in the UK. Public Health Nutr. 2023, 26, 425–436. [Google Scholar] [CrossRef] [PubMed]
- Pearce, J.; Harper, C.; Haroun, D.; Wood, L.; Nelson, M. Key differences between school lunches and packed lunches in primary schools in England in 2009. Public Health Nutr. 2011, 14, 1507–1510. [Google Scholar] [CrossRef]
- Pearce, J.; Wood, L.; Nelson, M. Lunchtime food and nutrient intakes of secondary-school pupils; a comparison of school lunches and packed lunches following the introduction of mandatory food-based standards for school lunch. Public Health Nutr. 2013, 16, 1126–1131. [Google Scholar] [CrossRef]
- Rogers, I.; Ness, A.; Hebditch, K.; Jones, L.; Emmett, P. Quality of food eaten in English primary schools: School dinners vs packed lunches. Eur. J. Clin. Nutr. 2007, 61, 856–864. [Google Scholar] [CrossRef]
- Spence, S.; Delve, J.; Stamp, E.; Matthews, J.N.; White, M.; Adamson, A.J. The impact of food and nutrient-based standards on primary school children’s lunch and total dietary intake: A natural experimental evaluation of government policy in England. PLoS ONE 2013, 8, e78298. [Google Scholar] [CrossRef]
- Stevens, L.; Nelson, M. The contribution of school meals and packed lunch to food consumption and nutrient intakes in UK primary school children from a low income population. J. Hum. Nutr. Diet. 2011, 24, 223–232. [Google Scholar] [CrossRef]
- Evans, C.E.; Greenwood, D.C.; Thomas, J.; Cade, J. A cross-sectional survey of children’s packed lunches in the UK: Food-and nutrient-based results. J. Epidemiol. Community Health 2010, 64, 977–983. [Google Scholar] [CrossRef]
- Jefferson, A.; Cowbrough, K. School Lunch Box Survey 2004; Food Standards Agency: London, UK, 2004.
- Fidler Mis, N.; Braegger, C.; Bronsky, J.; Campoy, C.; Domellöf, M.; Embleton, N.D.; Hojsak, I.; Hulst, J.; Indrio, F.; Lapillonne, A. Sugar in infants, children and adolescents: A position paper of the European society for paediatric gastroenterology, hepatology and nutrition committee on nutrition. J. Pediatr. Gastroenterol. Nutr. 2017, 65, 681–696. [Google Scholar] [CrossRef]
- Magriplis, E.; Michas, G.; Petridi, E.; Chrousos, G.P.; Roma, E.; Benetou, V.; Cholopoulos, N.; Micha, R.; Panagiotakos, D.; Zampelas, A. Dietary sugar intake and its association with obesity in children and adolescents. Children 2021, 8, 676. [Google Scholar] [CrossRef] [PubMed]
- Brady, T.M.; Horst, G.; Appel, L.J.; Khoury, P.R.; Urbina, E.M. Dietary sodium intake and sodium load is associated with arterial stiffness in children and young adults. J. Hypertens. 2022, 40, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Leyvraz, M.; Chatelan, A.; da Costa, B.R.; Taffe, P.; Paradis, G.; Bovet, P.; Bochud, M.; Chiolero, A. Sodium intake and blood pressure in children and adolescents: A systematic review and meta-analysis of experimental and observational studies. Int. J. Epidemiol. 2018, 47, 1796–1810. [Google Scholar] [CrossRef] [PubMed]
- Kaess, B.M.; Rong, J.; Larson, M.G.; Hamburg, N.M.; Vita, J.A.; Levy, D.; Benjamin, E.J.; Vasan, R.S.; Mitchell, G.F. Aortic stiffness, blood pressure progression, and incident hypertension. JAMA 2012, 308, 875–881. [Google Scholar] [CrossRef]
- Cheng, Y.L.; Hu, H.; Song, J.; MacGregor, G.A.; He, F.J. Socioeconomic status and dietary sodium intake in children from 2008 to 2019 in the UK. J. Hypertens. 2022, 40, 1499–1503. [Google Scholar] [CrossRef]
- Clarys, P.; Deliens, T.; Huybrechts, I.; Deriemaeker, P.; Vanaelst, B.; De Keyzer, W.; Hebbelinck, M.; Mullie, P. Comparison of nutritional quality of the vegan, vegetarian, semi-vegetarian, pesco-vegetarian and omnivorous diet. Nutrients 2014, 6, 1318–1332. [Google Scholar] [CrossRef]
- Dahmani, J.; Nicklaus, S.; Marty, L. Nutritional quality and greenhouse gas emissions of vegetarian and non-vegetarian school meals: A case study in France (Dijon). Proc. Nutr. Soc. 2022, 81, E60. [Google Scholar] [CrossRef]
- Poinsot, R.; Vieux, F.; Dubois, C.; Perignon, M.; Méjean, C.; Darmon, N. Nutritional quality of vegetarian and non-vegetarian dishes at school: Are nutrient profiling systems sufficiently informative? Nutrients 2020, 12, 2256. [Google Scholar] [CrossRef]
- Vieux, F.; Dubois, C.; Duchêne, C.; Darmon, N. Nutritional quality of school meals in France: Impact of guidelines and the role of protein dishes. Nutrients 2018, 10, 205. [Google Scholar] [CrossRef]
- Adams, E.L.; Raynor, H.A.; Thornton, L.M.; Mazzeo, S.E.; Bean, M.K. Nutrient intake during school lunch in title I elementary schools with universal free meals. Health Educ. Behav. 2022, 49, 118–127. [Google Scholar] [CrossRef]
- De Keyzer, W.; Van Caneghem, S.; Heath, A.-L.M.; Vanaelst, B.; Verschraegen, M.; De Henauw, S.; Huybrechts, I. Nutritional quality and acceptability of a weekly vegetarian lunch in primary-school canteens in Ghent, Belgium: ‘Thursday Veggie Day’. Public Health Nutr. 2012, 15, 2326–2330. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Singh, J.P.; Shevkani, K.; Singh, N.; Kaur, A. Bioactive constituents in pulses and their health benefits. J. Food Sci. Technol. 2017, 54, 858–870. [Google Scholar] [CrossRef] [PubMed]
- Craddock, J.C.; Genoni, A.; Strutt, E.F.; Goldman, D.M. Limitations with the Digestible Indispensable Amino Acid Score (DIAAS) with special attention to plant-based diets: A review. Curr. Nutr. Rep. 2021, 10, 93–98. [Google Scholar] [CrossRef]
- Seves, S.M.; Verkaik-Kloosterman, J.; Biesbroek, S.; Temme, E.H. Are more environmentally sustainable diets with less meat and dairy nutritionally adequate? Public Health Nutr. 2017, 20, 2050–2062. [Google Scholar] [CrossRef] [PubMed]
- Farsi, D.N.; Uthumange, D.; Munoz, J.M.; Commane, D.M. The nutritional impact of replacing dietary meat with meat alternatives in the UK: A modelling analysis using nationally representative data. Br. J. Nutr. 2022, 127, 1731–1741. [Google Scholar] [CrossRef]
- Hotz, C.; Gibson, R.S. Traditional food-processing and preparation practices to enhance the bioavailability of micronutrients in plant-based diets. J. Nutr. 2007, 137, 1097–1100. [Google Scholar] [CrossRef]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A. Food in the Anthropocene: The EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Alkerwi, A.A. Diet quality concept. Nutrition 2014, 30, 613–618. [Google Scholar] [CrossRef]
- Parnham, J.C.; Chang, K.; Rauber, F.; Levy, R.B.; Millett, C.; Laverty, A.A.; von Hinke, S.; Vamos, E.P. The ultra-processed food content of school meals and packed lunches in the United Kingdom. Nutrients 2022, 14, 2961. [Google Scholar] [CrossRef]
- Department for Environment, Food and Rural Affairs. Government Food Strategy. 2022. Available online: https://www.gov.uk/government/publications/government-food-strategy/government-food-strategy#:~:text=To%20address%20near%20term%20need,food%20businesses%20across%20the%20UK (accessed on 5 April 2023).

| Component | Minimum (0) Scoring Criteria | Maximum (10) Scoring Criteria | ||
|---|---|---|---|---|
| Primary (5–11 years) | Secondary (11–18 years) | Primary (5–11 years) | Secondary (11–18 years) | |
| Energy (kJ) | ≤1082.5 kJ or ≥3247.5 kJ b | ≤1557 kJ or ≥4671 kJ b | 2165 kJ (±325 kJ) a | 3114 kJ (±467 kJ) a |
| Fat | 20.1 g a | 29 g a | ≤10 g b | ≤14.5 g b |
| Saturated fat | 6.3 g a | 9.1 g a | ≤3.15 g b | ≤4.5 g b |
| Total CHO | ≤34.5 g b | ≤49.6 g b | ≥69.1 g a | ≥99.3 g a |
| Free sugars | 10.4 g a | 14.9 g a | ≤5.2 g b | ≤7.4 g b |
| Fibre | ≤3 g b | ≤4.5 g b | ≥6 g a | ≥9 g a |
| Protein | ≤9.7 g b | ≤13.9 g b | ≥19.4 g a | ≥27.9 g a |
| Iron | ≤1.6 mg d | ≤2.4 mg c | ≥3 mg a | ≥4.4 mg a |
| Calcium | ≤97.5 mg c | ≤144 mg c | ≥165 mg a | ≥300 mg a |
| Vitamin A | ≤75 µg c | ≤80 µg c | ≥150 µg a | ≥187 µg a |
| Vitamin C | ≤2.4 mg c | ≤3 mg c | ≥9 mg/d a | ≥11 mg a |
| Folate | ≤22.5 µg c | ≤30 µg c | ≥45 µg a | ≥60 µg a |
| Sodium (mg) | 686 mg a | 824 mg a | ≤343 mg b | ≤412 mg b |
| Zinc | ≤1.2 mg c | ≤1.65 mg c | ≥2.1 mg a | ≥2.8 mg a |
| School Food Standard | % Adherence (n/Total Assessable) | % Unassessable (of 167) |
|---|---|---|
| A1. ≥ 1 portions of starchy foods per day | 95.2 (159/167) | 0 (0) |
| A2. ≥ 3 different starchy foods each week * | 79.8 (99/124) | 25.7 (43 |
| A3. ≥ 1 wholegrain varieties each week | 22.8 (23/101) | 39.5 (66) |
| A4. Starchy food cooked in fat/oil ≤ 2 days each week | 87.7 (107/122) | 26.9 (45) |
| A5. Bread (with no added fat or oil) must be available every day | 43.3 (61/141) | 15.6 (26) |
| 1. ≥ 1 portion of vegetables or salad as an accompaniment every day | 50.3 (84/167) | 0.0 (0) |
| B2. ≥ 1 portions of fruit every day | 72.5 (121/167) | 0.0 (0) |
| B3. Dessert containing ≥ 50% fruit 2+ times per week | 75.2 (88/117) | 29.9 (50) |
| B4. ≥ 3 different fruits and ≥ 3 different vegetables each week | 64.5 (71/110) | 34.1 (57) |
| C1. A portion of food from this group every day | 53.3 (88/165) | 1.2 (2) |
| C2. Lower fat milk must be available for drinking at least once a day during school (HAF holiday club) hours | 14.8 (9/61) | 63.5 (106) |
| D1. A portion of food from this group every day | 64.0 (103/161) | 3.6 (6) |
| D2. A portion of meat or poultry on ≥ 3 days each week? * | 60.6 (43/71) | 57.5 (96) |
| D3. Oily fish ≥ 1 every three weeks | 34.0 (17/40) | 70.1 (117) |
| D4. For vegetarians, a portion of non-dairy protein on ≥ 3 days each week * | 61.9 (39/63) | 62.3 (104) |
| D5. A meat or poultry product (manufactured or homemade, and meeting the legal requirements) ≤ 1 week * | 71.0 (49/69) | 58.7 (98) |
| E1. ≤ 2 portions of food that have been deep-fried or coated per week | 96.0 (119/124) | 25.7 (43) |
| E2. ≤ 2 portions of food which include pastry each week? * | 96.0 (120/125) | 25.1 (42) |
| E3. No snacks, except nuts, seeds, vegetables and fruit with no added salt, sugar or fat | 72.7 (117/161) | 3.6 (6) |
| E4. No confectionery, chocolate or chocolate coated products | 64.6 (104/161) | 3.6 (6) |
| E5. Desserts, cakes and biscuits are allowed at lunchtime. They must not contain any confectionery | 57.1 (80/140) | 16.2 (27) |
| E6. Salt must not be available to add to food after it has been cooked ** | 100.0 (17/17) | 89.8 (150) |
| E7. Any condiments must be limited to sachets or portions of no more than 10 g or one teaspoonful * | 0 (0/167) | 100 (167) |
| F1. One of the permitted drink options ** | 93.7 (59/63) | 62.3 (104) |
| Nutrient-Based Standard | Primary School-Age (5–11) n (%) | Secondary School-Age (11–18) n (%) |
|---|---|---|
| Energy (kJ) | 948 (34.4) | 241 (8.7) |
| Total fat | 2303 (83.5) | 2627 (95.2) |
| Saturated fat | 1776 (64.4) | 2357 (85.4) |
| Total carbohydrate | 1186 (43.0) | 161 (5.8) |
| Free sugars | 1562 (56.6) | 1799 (65.2) |
| Fibre (AOAC) | 584 (21.2) | 133 (4.8) |
| Protein | 1284 (46.5) | 280 (10.2) |
| Iron | 535 (19.4) | 145 (5.3) |
| Calcium | 1762 (63.9) | 889 (32.2) |
| Vitamin A | 639 (23.2) | 377 (13.7) |
| Vitamin C | 2098 (76.0) | 2031 (73.6) |
| Folate | 1529 (55.4) | 881 (31.9) |
| Sodium | 2325 (84.3) | 2587 (93.8) |
| Zinc | 971 (35.2) | 362 (13.1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vitale, M.; Crossland, S.; Shinwell, J.; Stretesky, P.B.; Defeyter, M.A.; Brownlee, I.A. The Nutritional Quality of Food Provision at UK Government-Funded Holiday Clubs: A Cross-Sectional Analysis of Energy and Nutrient Content. Nutrients 2023, 15, 1937. https://doi.org/10.3390/nu15081937
Vitale M, Crossland S, Shinwell J, Stretesky PB, Defeyter MA, Brownlee IA. The Nutritional Quality of Food Provision at UK Government-Funded Holiday Clubs: A Cross-Sectional Analysis of Energy and Nutrient Content. Nutrients. 2023; 15(8):1937. https://doi.org/10.3390/nu15081937
Chicago/Turabian StyleVitale, Martina, Shannon Crossland, Jackie Shinwell, Paul B. Stretesky, Margaret Anne Defeyter, and Iain Andrew Brownlee. 2023. "The Nutritional Quality of Food Provision at UK Government-Funded Holiday Clubs: A Cross-Sectional Analysis of Energy and Nutrient Content" Nutrients 15, no. 8: 1937. https://doi.org/10.3390/nu15081937
APA StyleVitale, M., Crossland, S., Shinwell, J., Stretesky, P. B., Defeyter, M. A., & Brownlee, I. A. (2023). The Nutritional Quality of Food Provision at UK Government-Funded Holiday Clubs: A Cross-Sectional Analysis of Energy and Nutrient Content. Nutrients, 15(8), 1937. https://doi.org/10.3390/nu15081937







