Sex-Specific Dietary Patterns and Social Behaviour in Low-Risk Individuals
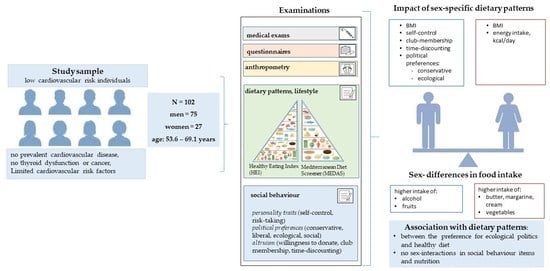
Abstract
1. Introduction
1.1. Dietary Patterns and Cardiovascular Disease
1.2. Relation between Social Behaviour, Dietary Pattern and Cardiovascular Health
1.3. The Role of Sex-Specific Dietary Patterns for Social Behaviour and Health
1.4. Aim of the Study
2. Materials and Methods
2.1. Design, Setting and Participants
2.1.1. AHRI Study
2.1.2. HCHS Study
2.2. Variables, Measurements and Processes
2.3. Data Handling
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Study Participants
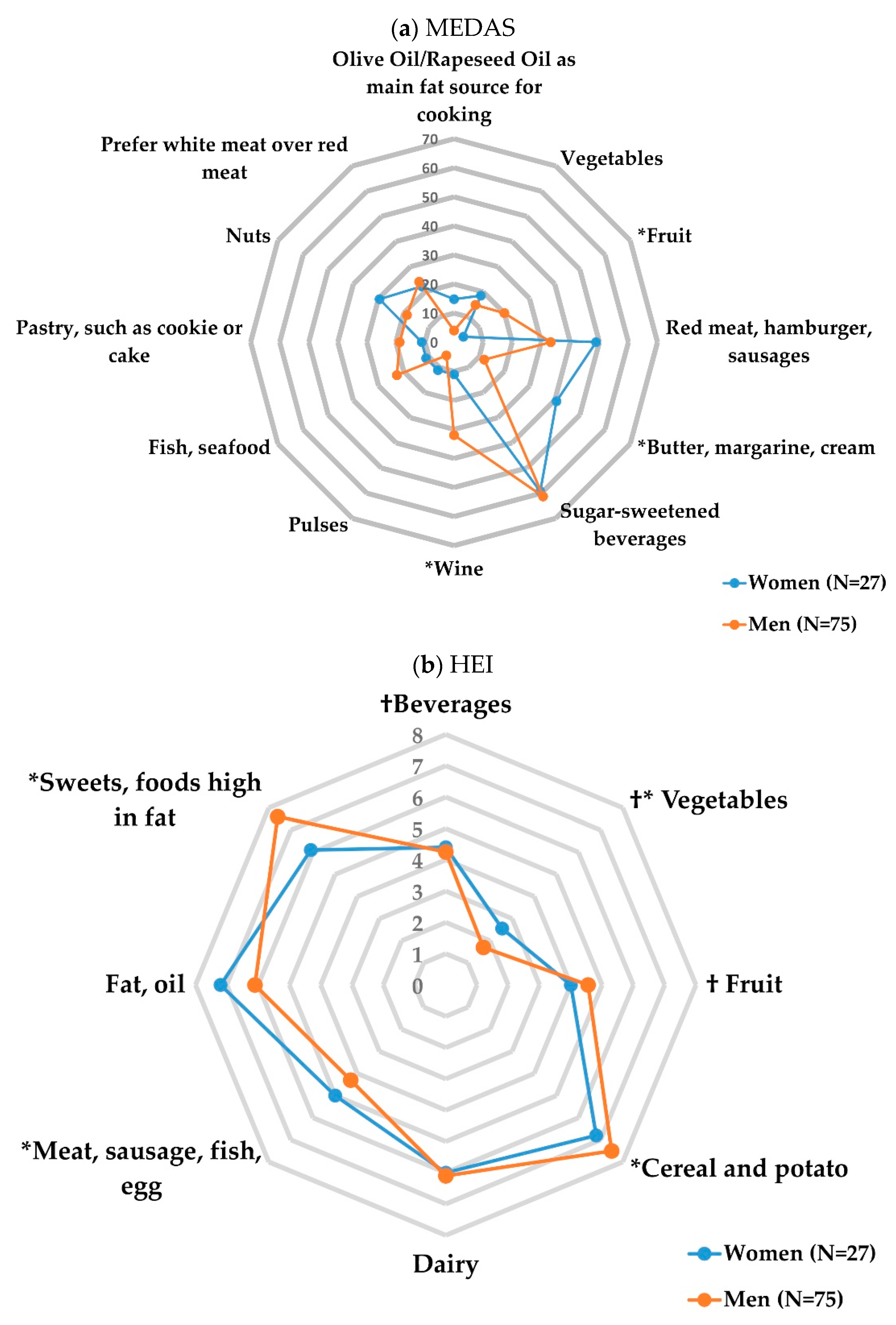
3.2. Sex-Specific Dietary Patterns
3.3. Correlation Analysis
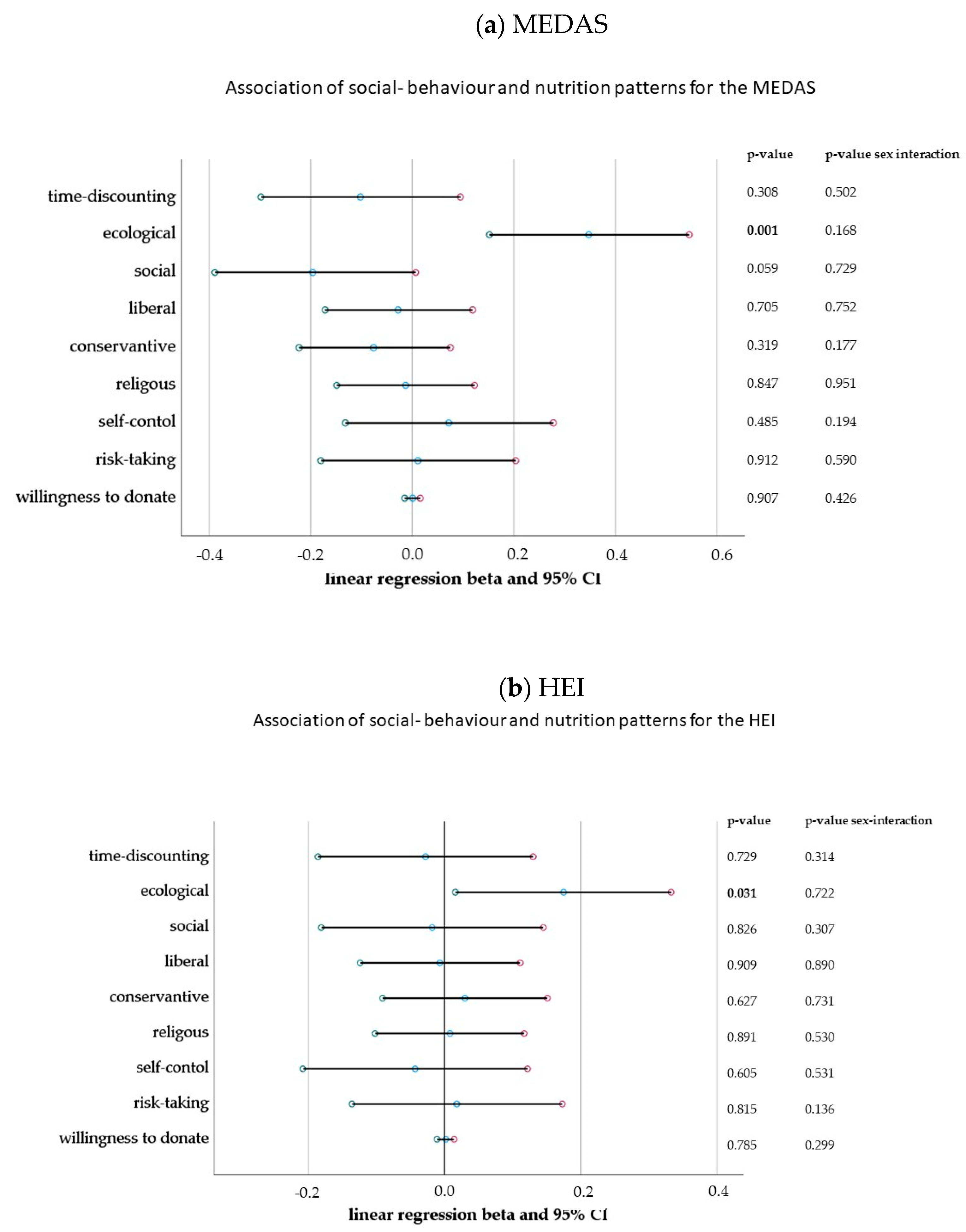
3.4. Association of Social Behaviour and Nutrition Patterns and the Effect of Moderation by Sex
4. Discussion
4.1. Main Findings and Implications for Future Investigations
4.2. Dietary Patterns and Sex
4.3. Social Behaviour, Personality Traits and Political Preferences
4.4. Recommendations for Primary Prevention
- ■
- The association of ecological preferences and healthy dietary patterns inform preventive agendas to focus on different behavioural strategies to promote environmentally sustainable food consumption in high-income countries.
- ■
- Health aspects are not the only determinants of food choices. People may have various food-related goals, such as to save money or maintain a sustainable lifestyle, which are often more salient and compete with the importance of health considerations.
- ■
- Social characteristics such as self-control and ecological preferences could support the ability to reflect on the influence of environmental factors such as marketing and peers. To educate individuals about this, behavioural insights that could support healthy dietary patterns could be integrated into behavioural primary prevention strategies.
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vaduganathan, M.; Mensah, G.A.; Turco, J.V.; Fuster, V.; Roth, G.A. The Global Burden of Cardiovascular Diseases and Risk. J. Am. Coll. Cardiol. 2022, 80, 2361–2371. [Google Scholar] [CrossRef] [PubMed]
- Zampelas, A.; Magriplis, E. Dietary patterns and risk of cardiovascular diseases: A review of the evidence. Proc. Nutr. Soc. 2020, 79, 68–75. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Bogensberger, B.; Hoffmann, G. Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: An Updated Systematic Review and Meta-Analysis of Cohort Studies. J. Acad. Nutr. Diet. 2018, 118, 74–100. [Google Scholar] [CrossRef] [PubMed]
- Eleftheriou, D.; Benetou, V.; Trichopoulou, A.; La Vecchia, C.; Bamia, C. Mediterranean diet and its components in relation to all-cause mortality: Meta-analysis. Br. J. Nutr. 2018, 120, 1081–1097. [Google Scholar] [CrossRef]
- Kastorini, C.-M.; Milionis, H.J.; Esposito, K.; Giugliano, D.; Goudevenos, J.A.; Panagiotakos, D.B. The effect of Mediterranean diet on metabolic syndrome and its components: A meta-analysis of 50 studies and 534,906 individuals. J. Am. Coll. Cardiol. 2011, 57, 1299–1313. [Google Scholar] [CrossRef]
- Lunn, T.E.; Nowson, C.A.; Worsley, A.; Torres, S.J. Does personality affect dietary intake? Nutrition 2014, 30, 403–409. [Google Scholar] [CrossRef]
- Conner, T.S.; Thompson, L.M.; Knight, R.L.; Flett, J.A.M.; Richardson, A.C.; Brookie, K.L. The Role of Personality Traits in Young Adult Fruit and Vegetable Consumption. Front. Psychol. 2017, 8, 119. [Google Scholar] [CrossRef] [PubMed]
- Plante, C.N.; Rosenfeld, D.L.; Plante, M.; Reysen, S. The role of social identity motivation in dietary attitudes and behaviors among vegetarians. Appetite 2019, 141, 104307. [Google Scholar] [CrossRef] [PubMed]
- Levy, D.E.; Pachucki, M.C.; O’Malley, A.J.; Porneala, B.; Yaqubi, A.; Thorndike, A.N. Social connections and the healthfulness of food choices in an employee population. Nat. Hum. Behav. 2021, 5, 1349–1357. [Google Scholar] [CrossRef]
- Higgs, S. Social norms and their influence on eating behaviours. Appetite 2015, 86, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Conklin, A.I.; Forouhi, N.G.; Surtees, P.; Khaw, K.T.; Wareham, N.J.; Monsivais, P. Social relationships and healthful dietary behaviour: Evidence from over-50s in the EPIC cohort, UK. Soc. Sci. Med. 2014, 100, 167–175. [Google Scholar] [CrossRef]
- Provencher, V.; Bégin, C.; Gagnon-Girouard, M.P.; Tremblay, A.; Boivin, S.; Lemieux, S. Personality traits in overweight and obese women: Associations with BMI and eating behaviors. Eat. Behav. 2008, 9, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Molloy, G.J.; O’Carroll, R.E.; Ferguson, E. Conscientiousness and Medication Adherence: A Meta-analysis. Ann. Behav. Med. 2013, 47, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Hakulinen, C.; Jokela, M. Chapter 3—Personality as Determinant of Smoking, Alcohol Consumption, Physical Activity, and Diet Preferences. In Personality and Disease; Johansen, C., Ed.; Academic Press: San Diego, CA, USA, 2018; pp. 33–48. [Google Scholar] [CrossRef]
- Jokela, M.; Batty, G.D.; Nyberg, S.T.; Virtanen, M.; Nabi, H.; Singh-Manoux, A.; Kivimäki, M. Personality and All-Cause Mortality: Individual-Participant Meta-Analysis of 3,947 Deaths in 76,150 Adults. Am. J. Epidemiol. 2013, 178, 667–675. [Google Scholar] [CrossRef]
- Essien, U.R.; Kornej, J.; Johnson, A.E.; Schulson, L.B.; Benjamin, E.J.; Magnani, J.W. Social determinants of atrial fibrillation. Nat. Rev. Cardiol. 2021, 18, 763–773. [Google Scholar] [CrossRef]
- Shepherd, R. Social determinants of food choice. Proc. Nutr. Soc. 1999, 58, 807–812. [Google Scholar] [CrossRef]
- Lappalainen, R.; Kearney, J.; Gibney, M. A pan EU survey of consumer attitudes to food, nutrition and health: An overview. Food Qual. Prefer. 1998, 9, 467–478. [Google Scholar] [CrossRef] [PubMed]
- Jagodzinski, A.; Johansen, C.; Koch-Gromus, U.; Aarabi, G.; Adam, G.; Anders, S.; Augustin, M.; der Kellen, R.B.; Beikler, T.; Behrendt, C.A.; et al. Rationale and Design of the Hamburg City Health Study. Eur. J. Epidemiol. 2020, 35, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Neumann, F.A.; Jagemann, B.; Makarova, N.; Börschel, C.S.; Aarabi, G.; Gutmann, F.; Schnabel, R.B.; Zyriax, B.-C. Mediterranean Diet and Atrial Fibrillation: Lessons Learned from the AFHRI Case–Control Study. Nutrients 2022, 14, 3615. [Google Scholar] [CrossRef]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- von Rusten, A.; Illner, A.-K.; Boeing, H.; Flothkotter, M. Begutachtetes Original-Die Bewertung der Lebensmittelaufnahme mittels eines’ Healthy Eating Index’(HEI-EPIC). Ernahr.-Umsch. 2009, 56, 450. [Google Scholar]
- Sterne, J.A.C.; White, I.R.; Carlin, J.B.; Spratt, M.; Royston, P.; Kenward, M.G.; Wood, A.M.; Carpenter, J.R. Multiple imputation for missing data in epidemiological and clinical research: Potential and pitfalls. BMJ 2009, 338, b2393. [Google Scholar] [CrossRef] [PubMed]
- Baranzini, D. SPSS Single Dataframe Aggregating SPSS Multiply Imputed Split Files. 2018. Available online: https://www.researchgate.net/profile/Daniele_Baranzini/publication/328887514_SPSS_Single_dataframe_aggregating_SPSS_Multiply_Imputed_split_files/data/5be9a1cf299bf1124fce0d62/The-Bar-Procedure.docx (accessed on 22 January 2023).
- Northstone, K. Dietary patterns: The importance of sex differences. Br. J. Nutr. 2012, 108, 393–394. [Google Scholar] [CrossRef] [PubMed]
- Bennett, E.; Peters, S.A.; Woodward, M. Sex differences in macronutrient intake and adherence to dietary recommendations: Findings from the UK Biobank. BMJ Open 2018, 8, e020017. [Google Scholar] [CrossRef]
- Modlinska, K.; Adamczyk, D.; Maison, D.; Pisula, W. Gender differences in attitudes to vegans/vegetarians and their food preferences, and their implications for promoting sustainable dietary patterns—A systematic review. Sustainability 2020, 12, 6292. [Google Scholar] [CrossRef]
- Tande, D.L.; Magel, R.; Strand, B.N. Healthy Eating Index and abdominal obesity. Public Health Nutr. 2010, 13, 208–214. [Google Scholar] [CrossRef]
- Wang, C.; Xu, Y. Mechanisms for sex differences in energy homeostasis. J. Mol. Endocrinol. 2019, 62, R129. [Google Scholar] [CrossRef] [PubMed]
- Vahid, F.; Jalili, M.; Rahmani, W.; Nasiri, Z.; Bohn, T. A Higher Healthy Eating Index Is Associated with Decreased Markers of Inflammation and Lower Odds for Being Overweight/Obese Based on a Case-Control Study. Nutrients 2022, 14, 5127. [Google Scholar] [CrossRef] [PubMed]
- Colpani, V.; Baena, C.P.; Jaspers, L.; Van Dijk, G.M.; Farajzadegan, Z.; Dhana, K.; Tielemans, M.J.; Voortman, T.; Freak-Poli, R.; Veloso, G.G. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: A systematic review and meta-analysis. Eur. J. Epidemiol. 2018, 33, 831–845. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Alcohol and Health 2018; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Prättälä, R.; Paalanen, L.; Grinberga, D.; Helasoja, V.; Kasmel, A.; Petkeviciene, J. Gender differences in the consumption of meat, fruit and vegetables are similar in Finland and the Baltic countries. Eur. J. Public Health 2007, 17, 520–525. [Google Scholar] [CrossRef] [PubMed]
- Martín-María, N.; Lara, E.; Cabello, M.; Olaya, B.; Haro, J.M.; Miret, M.; Ayuso-Mateos, J.L. To be happy and behave in a healthier way. A longitudinal study about gender differences in the older population. Psychol. Health 2023, 38, 307–323. [Google Scholar] [CrossRef] [PubMed]
- Engel, S.; Tholstrup, T. Butter increased total and LDL cholesterol compared with olive oil but resulted in higher HDL cholesterol compared with a habitual diet. Am. J. Clin. Nutr. 2015, 102, 309–315. [Google Scholar] [CrossRef]
- Wang, X.; Magkos, F.; Mittendorfer, B. Sex Differences in Lipid and Lipoprotein Metabolism: It’s Not Just about Sex Hormones. J. Clin. Endocrinol. Metab. 2011, 96, 885–893. [Google Scholar] [CrossRef]
- Peters, S.A.E.; Muntner, P.; Woodward, M. Sex Differences in the Prevalence of, and Trends in, Cardiovascular Risk Factors, Treatment, and Control in the United States, 2001 to 2016. Circulation 2019, 139, 1025–1035. [Google Scholar] [CrossRef]
- Soriano-Maldonado, C.; Lopez-Pineda, A.; Orozco-Beltran, D.; Quesada, J.A.; Alfonso-Sanchez, J.L.; Pallarés-Carratalá, V.; Navarro-Perez, J.; Gil-Guillen, V.F.; Martin-Moreno, J.M.; Carratala-Munuera, C. Gender Differences in the Diagnosis of Dyslipidemia: ESCARVAL-GENERO. Int. J. Environ. Res. Public Health 2021, 18, 2419. [Google Scholar] [CrossRef] [PubMed]
- Turrini, A.; D’Addezio, L.; Maccati, F.; Davy, B.M.; Arber, S.; Davidson, K.; Grunert, K.; Schuhmacher, B.; Pfau, C.; Kozłowska, K.; et al. The Informal Networks in Food Procurement by Older People—A Cross European Comparison. Ageing Int. 2010, 35, 253–275. [Google Scholar] [CrossRef]
- Alshehri, M.; Kruse-Diehr, A.J.; McDaniel, J.T.; Partridge, J.; Null, D.B. Impact of social support on the dietary behaviors of international college students in the United States. J. Am. Coll. Health 2021, 1–9. [Google Scholar] [CrossRef]
- Ellis, A.; Jung, S.E.; Palmer, F.; Shahan, M. Individual and interpersonal factors affecting dietary intake of community-dwelling older adults during the COVID-19 pandemic. Public Health Nutr. 2022, 25, 1667–1677. [Google Scholar] [CrossRef] [PubMed]
- Junger, M.; van Kampen, M. Cognitive ability and self-control in relation to dietary habits, physical activity and bodyweight in adolescents. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 22. [Google Scholar] [CrossRef]
- Stutts, L.A.; Blomquist, K.K. A longitudinal study of weight and shape concerns and disordered eating groups by gender and their relationship to self-control. Eat. Weight Disord.–Stud. Anorex. Bulim. Obes. 2021, 26, 227–237. [Google Scholar] [CrossRef]
- Szabo, K.; Piko, B.F.; Fitzpatrick, K.M. Adolescents’ attitudes towards healthy eating: The role of self-control, motives and self-risk perception. Appetite 2019, 143, 104416. [Google Scholar] [CrossRef]
- Van Dooren, C.; Marinussen, M.; Blonk, H.; Aiking, H.; Vellinga, P. Exploring dietary guidelines based on ecological and nutritional values: A comparison of six dietary patterns. Food Policy 2014, 44, 36–46. [Google Scholar] [CrossRef]
- Baca-Motes, K.; Edwards, A.M.; Waalen, J.; Edmonds, S.; Mehta, R.R.; Ariniello, L.; Ebner, G.S.; Talantov, D.; Fastenau, J.M.; Carter, C.T. Digital recruitment and enrollment in a remote nationwide trial of screening for undiagnosed atrial fibrillation: Lessons from the randomized, controlled mSToPS trial. Contemp. Clin. Trials Commun. 2019, 14, 100318. [Google Scholar] [CrossRef] [PubMed]
- Schreier, H.M.; Schonert-Reichl, K.A.; Chen, E. Effect of volunteering on risk factors for cardiovascular disease in adolescents: A randomized controlled trial. JAMA Pediatr. 2013, 167, 327–332. [Google Scholar] [CrossRef]
- Weissberger, G.H.; Samek, A.; Mosqueda, L.; Nguyen, A.L.; Lim, A.C.; Fenton, L.; Han, S.D. Increased Financial Altruism is Associated with Alzheimer’s Disease Neurocognitive Profile in Older Adults. J. Alzheimer’s Dis. 2022, 88, 995–1005. [Google Scholar] [CrossRef]
- Shim, E.; Chapman, G.B.; Townsend, J.P.; Galvani, A.P. The influence of altruism on influenza vaccination decisions. J. R. Soc. Interface 2012, 9, 2234–2243. [Google Scholar] [CrossRef] [PubMed]
- Cavazza, N.; Guidetti, M.; Butera, F. Ingredients of gender-based stereotypes about food. Indirect influence of food type, portion size and presentation on gendered intentions to eat. Appetite 2015, 91, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Çınar, Ç.; Wesseldijk, L.W.; Karinen, A.K.; Jern, P.; Tybur, J.M. Sex differences in the genetic and environmental underpinnings of meat and plant preferences. Food Qual. Prefer. 2022, 98, 104421. [Google Scholar] [CrossRef]
- Obara-Gołębiowska, M.; Michałek-Kwiecień, J. Personality traits, dieting self-efficacy and health behaviors in emerging adult women: Implications for health promotion and education. Health Promot. Perspect. 2020, 10, 230. [Google Scholar] [CrossRef]
| Variables | Total (N = 102) | Women (n = 27) | Men (n = 75) | Standardised Test Statistic | p-Value |
|---|---|---|---|---|---|
| Sociodemographic and clinical data | |||||
| Age, years | 62.4 (53.6, 69.1) | 62.4 (56.6, 70.3) | 63.5 (53.3, 69.0) | −0.0618 c | 0.536 |
| Income categories | |||||
| Low (<EUR 2500) | 16 (15.5%) | 7 (25.9%) | 9 (12.0%) | 10.268 b | 0.008 |
| Middle (EUR 2500 < EUR 5000) | 56 (54.9%) | 18 (66.7%) | 38(50.7%) | ||
| High (>EUR 5000) | 30 (29.4%) | 2 (7.4%) | 28 (37.3%) | ||
| Body mass index, kg/m2 | 25.5 (23.1, 27.8) | 25.0 (23.1, 27.3) | 25.4 (23.1, 27.8) | 0.155 c | 0.876 |
| Body mass index categories | |||||
| Underweight | 1 (1.0%) | - | 1 (1.4%) | 0.985 b | 0.875 |
| Normal weight | 48 (47.1%) | 14 (51.9%) | 33 (44.6%) | ||
| Overweight | 46 (45.1%) | 11 (40.7%) | 36 (47.3%) | ||
| Obesity | 7 (7.9%) | 2 (7.4%) | 5 (6.8%) | ||
| Prevalent diseases | |||||
| Type 2 diabetes mellitus | 2 (2.0%) | - | 2 (2.7%) | 1.421 a | 0.153 |
| Arterial hypertension | 22 (21.6%) | 8 (29.6%) | 14 (18.7%) | 1.410 a | 0.235 |
| atrial fibrillation | 52 (51%) | 14 (51.0%) | 38 (50.7%) | 0.011 a | 0.916 |
| Dyslipidaemia | 21 (20.6%) | 10 (37.0%) | 11 (14.7%) | 6.077 a | 0.014 |
| Lifestyle factors | |||||
| MEDAS, points | 3 (1, 4) | 3 (1, 5) | 2 (2, 4) | −0.320 c | 0.749 |
| Healthy Eating Index, points | 54.9 (47.3, 60.3) | 55.6 (48.6, 61,8) | 54.8 (67.2, 59.3) | −0.804 c | 0.421 |
| Healthy Eating Index, categories | |||||
| Poor (≤40 pts.) | 10 (9.8%) | 1 (13.7%) | 9 (12.0%) | 1.355 | 0.556 |
| Improvable (>40–64 pts.) | 77 (75.5%) | 22 (80.4%) | 55 (73.3%) | ||
| Good (>64 pts.) | 15 (14.7) | 4 (5.9%) | 11 (14.7%) | ||
| Diet change past 12 months | |||||
| No | 82 (80.4%) | 22 (78.4%) | 60 (80.0%) | 0.028 a | 0.868 |
| Yes, partially | 20 (19.6%) | 5 (18.5%) | 15 (20.0%) | ||
| Energy intake, kcal/day | 2187 (1904, 2504) | 2138 (1224, 2418) | 2253 (1974, 2583) | 3.243 | 0.001 |
| Physical activity, MET-h/day (in Log10) | 3.3 (3.1, 3.6) | 3.5 (3.1, 3.8) | 3.3 (3.1, 3.5) | 1.737 c | 0.082 |
| Alcohol consumption | 82 (80.4) | 18 (66.7%) | 63 (84.0%) | 4.249 a | 0.039 |
| Smoking | |||||
| Current | 62 (60.8%) | 6 (22.2%) | 10 (13.3%) | 2.018 b | 0.379 |
| Former | 9 (33.3%) | 41 (54.7%) | |||
| Social behaviour | |||||
| Personality traits | |||||
| Risk taking | 6 (5.7) | 6 (5.6) | 6 (5.8) | 10.563 b | 0.250 |
| Self-control | 9 (8.10) | 8 (7.8) | 9 (8.10) | 12.425 b | 0.139 |
| Religiousness | 4 (1.6) | 4 (1.5) | 4 (1.7) | 10.468 b | 0.276 |
| Political preferences | |||||
| Conservative | 5 (2.7) | 4 (1.5) | 6 (4.8) | 17.628 b | 0.032 |
| Liberal | 6 (2.7) | 5 (2.6) | 6 (4.8) | 14.993 b | 0.088 |
| Social | 8 (6.9) | 8 (7.9) | 8 (6.9) | 6.444 b | 0.826 |
| Ecological | 8 (7.9) | 8 (7.9) | 8 (6.9) | 6.670 b | 0.783 |
| Altruism | |||||
| Willingness to donate in EUR (EUR 0 to 50) | EUR 20 ± 22 | 25 (20.50) | 20 (20.50) | −0.580 c | 0.562 |
| Low willingness to donate (EUR 0–25) | 61 (59.8%) | 16 (59.3%) | 45 (60.0%) | 0.005 a | 0.946 |
| High willingness to donation (EUR 25–50) | 41 (41.2%) | 11 (40.7%) | 30 (40.0%) | ||
| Club membership | |||||
| No | 37 (36.3%) | 17 (63.3%) | 20 (26.7%) | 10.655 b | 0.004 |
| Yes, passive | 12 (11.8%) | 2 (7.4%) | 10 (13.3%) | ||
| Yes, active | 53 (52.0%) | 8 (29.6) | 45 (60.0%) | ||
| Time discounting | 4 (2.6) | 3 (2.4) | 4 (3.5) | 3.175 b | 0.957 |
| Independent Variables | MEDAS | HEI | ||||||
|---|---|---|---|---|---|---|---|---|
| Women | Men | Women | Men | |||||
| R | p-Value | R | p-Value | R | p-Value | R | p-Value | |
| Sociodemographic and clinical data | ||||||||
| Age, years | −0.042 | 0.836 | 0.104 | 0.375 | 0.037 | 0.854 | 0.301 | 0.009 |
| Income | 0.078 | 0.698 | −0.009 | 0.942 | 0.014 | 0.889 | −0.069 | 0.555 |
| Body mass index, kg/m2 | −0.077 | 0.702 | −0.432 | 0.001 | −0.391 | 0.044 | −0.406 | 0.001 |
| Lifestyle factors | ||||||||
| MEDAS, points | - | - | - | - | 0.307 | 0.119 | 0.352 | 0.002 |
| Healthy Eating Index, points | 0.307 | 0.119 | −0.352 | 0.002 | - | - | - | - |
| Diet change past year | 0.257 | 0.196 | 0.184 | 0.114 | −0.037 | 0.856 | 0.050 | 0.670 |
| Energy intake, kcal/day | 0.003 | 0.986 | −0.010 | 0.932 | 0.446 | 0.020 | 0.165 | 0.158 |
| Physical activity, MET-h/day | 0.233 | 0.242 | 0.089 | 0.448 | −0.255 | 0.199 | −0.065 | 0.577 |
| Social behaviour | ||||||||
| Altruism | ||||||||
| Willingness to donate | 0.112 | 0.577 | −0.032 | 0.783 | 0.252 | 0.206 | −0.007 | 0.955 |
| Club membership | 0.359 | 0.066 | 0.038 | 0.745 | 0.192 | 0.337 | −0.228 | 0.049 |
| Time discounting | −0.290 | 0.142 | −0.218 | 0.060 | 0.191 | 0.341 | −0.250 | 0.030 |
| Personality traits | ||||||||
| Risk taking | −0.221 | 0.268 | 0.103 | 0.379 | 0.188 | 0.348 | 0.014 | 0.905 |
| Self-control | 0.026 | 0.898 | 0.293 | 0.011 | 0.093 | 0.646 | 0.153 | 0.326 |
| Religiousness | −0.025 | 0.900 | 0.029 | 0.804 | 0.140 | 0.487 | 0.075 | 0.521 |
| Political preferences | ||||||||
| Conservative | 0.026 | 0.899 | −0.230 | 0.047 | 0.146 | 0.486 | 0.45 | 0.700 |
| Liberal | 0.035 | 0.862 | 0.029 | 0.802 | 0.074 | 0.714 | 0.145 | 0.214 |
| Social | 0.110 | 0.584 | 0.165 | 0.158 | 0.173 | 0.387 | 0.097 | 0.407 |
| Ecological | 0.155 | 0.441 | 0.479 | 0.001 | 0.048 | 0.812 | 0.244 | 0.053 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Engler, D.; Schnabel, R.B.; Neumann, F.A.; Zyriax, B.-C.; Makarova, N. Sex-Specific Dietary Patterns and Social Behaviour in Low-Risk Individuals. Nutrients 2023, 15, 1832. https://doi.org/10.3390/nu15081832
Engler D, Schnabel RB, Neumann FA, Zyriax B-C, Makarova N. Sex-Specific Dietary Patterns and Social Behaviour in Low-Risk Individuals. Nutrients. 2023; 15(8):1832. https://doi.org/10.3390/nu15081832
Chicago/Turabian StyleEngler, Daniel, Renate B. Schnabel, Felix Alexander Neumann, Birgit-Christiane Zyriax, and Nataliya Makarova. 2023. "Sex-Specific Dietary Patterns and Social Behaviour in Low-Risk Individuals" Nutrients 15, no. 8: 1832. https://doi.org/10.3390/nu15081832
APA StyleEngler, D., Schnabel, R. B., Neumann, F. A., Zyriax, B.-C., & Makarova, N. (2023). Sex-Specific Dietary Patterns and Social Behaviour in Low-Risk Individuals. Nutrients, 15(8), 1832. https://doi.org/10.3390/nu15081832