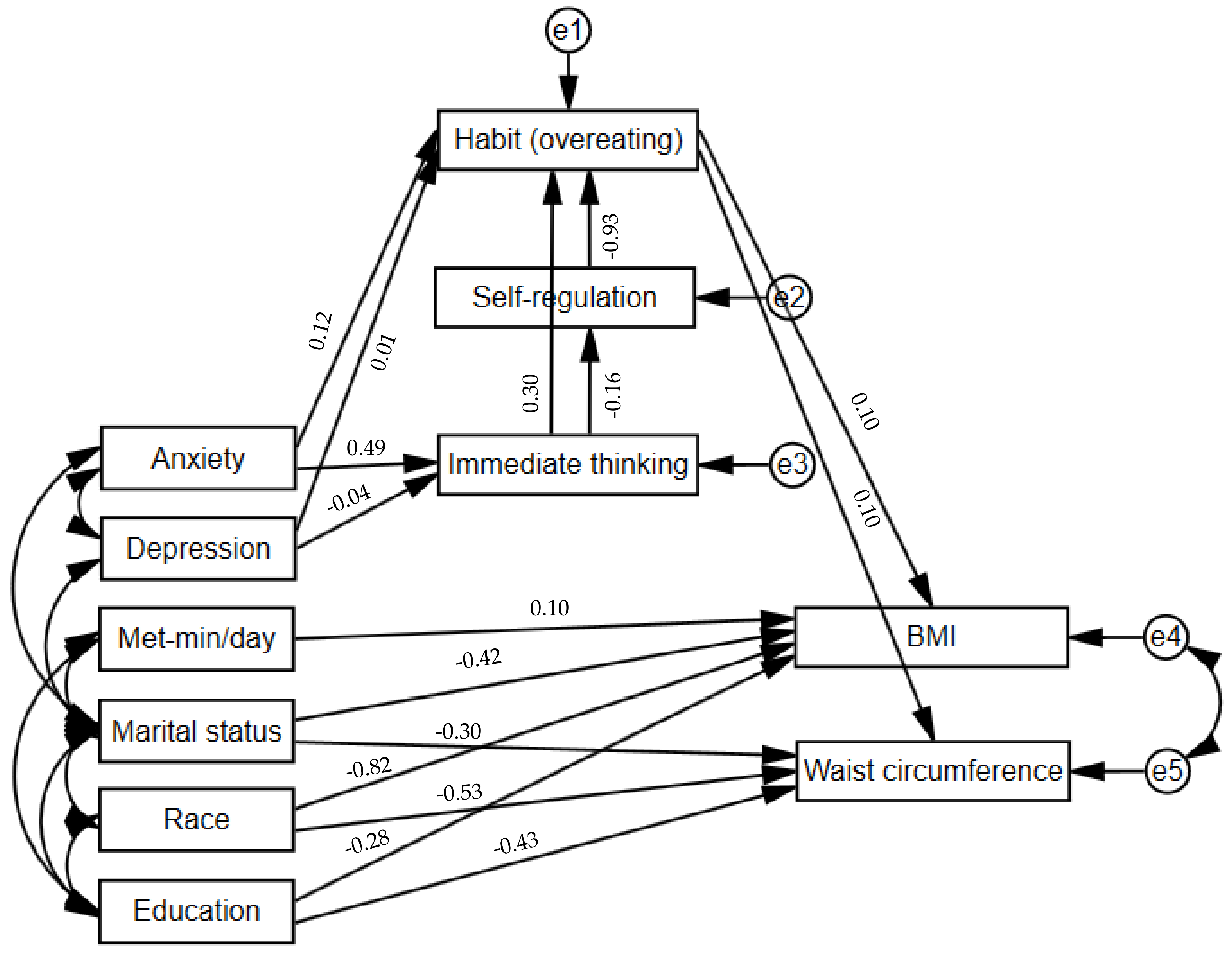
Socio-Demographic, Behavioral and Psychological Factors Associated with High BMI among Adults in a Southeast Asian Multi-Ethnic Society: A Structural Equation Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting and Participants
2.2. Data Collection and Variables Assessed
2.2.1. Sociodemographic and Anthropometric Profile
2.2.2. Intention to Change Eating Behaviors
2.2.3. Self-Regulation of Eating Behavior
2.2.4. Consideration of Future Consequences
2.2.5. Overeating Habit
2.2.6. Physical Activity
2.2.7. Depression and Anxiety
2.3. Data Analysis
3. Results
Post Hoc Subgroup Analysis
4. Discussion
Strengths and Limitations
5. Conclusions
6. Study Importance
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Clinical trial registration
Consent for publication
Abbreviations
| BMI | body mass index |
| HPA | hypothalamic–pituitary–adrenal |
| SES | socioeconomical status |
| TST | Temporal Self-Regulation Theory |
| NHG | National Healthcare Group |
| DSRB | Domain Specific Review Board |
| STROBE | STrengthening the Reporting of OBservational studies in Epidemiology |
| SREBQ | Self-regulation of Eating Behavior Questionnaire |
| CFCS | Consideration of future consequences scale |
| SRHI | Self-Report Habit Index |
| IPAQ-SF | International Physical Activity Questionnaire Short-Form |
| MET | Metabolic Equivalent Task |
| PHQ | Patient Health Questionnaire |
| GAD | Generalized Anxiety Disorder |
| SEM | Structural equation modeling |
| MLE | maximum likelihood estimation |
| CFI | comparative fit index |
| TLI | Tucker–Lewis Index |
| RMSEA | Root Mean Square Error of Approximation |
| CI | confidence interval |
References
- The GBD 2015 Obesity collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity and Overweight. 2016. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 2 January 2023).
- World Health Organization. WHO European Regional Obesity Report 2022; WHO: Geneva, Switzerland, 2022.
- Finegood, D.T.; Merth, T.D.; Rutter, H. Implications of the foresight obesity system map for solutions to childhood obesity. Obesity 2010, 18, S13. [Google Scholar] [CrossRef]
- Herle, M.; Smith, A.D.; Kininmonth, A.; Llewellyn, C. The role of eating behaviours in genetic susceptibility to obesity. Curr. Obes. Rep. 2020, 9, 512–521. [Google Scholar] [CrossRef] [PubMed]
- Pasquali, R. The hypothalamic–pituitary–adrenal axis and sex hormones in chronic stress and obesity: Pathophysiological and clinical aspects. Ann. N. Y. Acad. Sci. 2012, 1264, 20–35. [Google Scholar] [CrossRef] [PubMed]
- Pachucki, M.C.; Goodman, E. Social relationships and obesity: Benefits of incorporating a lifecourse perspective. Curr. Obes. Rep. 2015, 4, 217–223. [Google Scholar] [CrossRef]
- Devine, C.M.; Nelson, J.A.; Chin, N.; Dozier, A.; Fernandez, I.D. “Pizza is cheaper than salad”: Assessing workers’ views for an environmental food intervention. Obesity 2007, 15, 57S–68S. [Google Scholar] [CrossRef]
- Silva, A.A.M.; Vasconcelos, A.G.G.; Bettiol, H.; Barbieri, M.A. Socioeconomic status, birth weight, maternal smoking during pregnancy and adiposity in early adult life: An analysis using structural equation modeling. Cad. De Saúde Pública 2010, 26, 15–29. [Google Scholar] [CrossRef]
- Cockerham, W.C.; Hamby, B.W.; Oates, G.R. The social determinants of chronic disease. Am. J. Prev. Med. 2017, 52, S5–S12. [Google Scholar] [CrossRef]
- Daw, J.; Margolis, R.; Wright, L. Emerging adulthood, emergent health lifestyles: Sociodemographic determinants of trajectories of smoking, binge drinking, obesity, and sedentary behavior. J. Health Soc. Behav. 2017, 58, 181–197. [Google Scholar] [CrossRef]
- Singapore Department of Statistics, Key Household Income Trends, 2022. Available online: https://www.singstat.gov.sg/find-data/search-by-theme/households/household-income/visualising-data/key-household-income-trends (accessed on 2 March 2023).
- Ministry of Social and Family Development Singapore. ComCare Interim Assistance 2021. Available online: https://www.msf.gov.sg/Comcare/Pages/Urgent-Financial-Assistance.aspx (accessed on 2 March 2023).
- Impact, E. Global Food Security Index 2022. 2022. Available online: https://impact.economist.com/sustainability/project/food-security-index?gclid=Cj0KCQjw2cWgBhDYARIsALggUhqFpvkq5dw3Lfzde8_lfFAsVIuhoQkxWZT22OYMeNtLF2UjIqzoO14aAlSwEALw_wcB&gclsrc=aw.ds (accessed on 2 March 2023).
- Housing and Development Board, Singapore. HDB Ensures a Good Supply with Affordable Food Options [Press Release]. 2022. Available online: https://www.hdb.gov.sg/cs/infoweb/about-us/news-and-publications/letters-to-the-media/HDB-ensures-a-good-supply-with-affordable-food-options (accessed on 2 March 2023).
- Prioreschi, A.; Wrottesley, S.V.; Cohen, E.; Reddy, A.; Said-Mohamed, R.; Twine, R.; Tollman, S.M.; Kahn, K.; Dunger, D.B.; Norris, S.A. Examining the relationships between body image, eating attitudes, BMI, and physical activity in rural and urban South African young adult females using structural equation modeling. PLoS ONE 2017, 12, e0187508. [Google Scholar] [CrossRef]
- Pudrovska, T.; Anishkin, A. Early-life socioeconomic status and physical activity in later life: Evidence from structural equation models. J. Aging Health 2013, 25, 383–404. [Google Scholar] [CrossRef] [PubMed]
- Darbandi, M.; Najafi, F.; Pasdar, Y.; Rezaeian, S. Structural equation model analysis for the evaluation of factors associated with overweight and obesity in menopausal women in RaNCD cohort study. Menopause 2020, 27, 208–215. [Google Scholar] [CrossRef]
- Jalali-Farahani, S.; Amiri, P.; Karimi, M.; Gharibzadeh, S.; Mirmiran, P.; Azizi, F. Socio-behavioral factors associated with overweight and central obesity in Tehranian adults: A structural equation model. Int. J. Behav. Med. 2017, 24, 110–119. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Katzmarzyk, P.T.; Bryan, S.N.; Perez, C.E.; Ardern, C.I. Obesity, overweight and ethnicity. Health Rep. 2005, 16, 23. [Google Scholar] [PubMed]
- Kirby, J.B.; Liang, L.; Chen, H.-J.; Wang, Y. Race, place, and obesity: The complex relationships among community racial/ethnic composition, individual race/ethnicity, and obesity in the United States. Am. J. Public Health 2012, 102, 1572–1578. [Google Scholar] [CrossRef]
- Latner, J.D.; Stunkard, A.J.; Wilson, G.T. Stigmatized students: Age, sex, and ethnicity effects in the stigmatization of obesity. Obes. Res. 2005, 13, 1226–1231. [Google Scholar] [CrossRef]
- Ciria, L.F.; Watson, P.; Vadillo, M.A.; Luque, D. Is the habit system altered in individuals with obesity? A systematic review. Neurosci. Biobehav. Rev. 2021, 128, 621–632. [Google Scholar] [CrossRef]
- Soltis, K.E.; McDevitt-Murphy, M.E.; Murphy, J.G. Alcohol demand, future orientation, and craving mediate the relation between depressive and stress symptoms and alcohol problems. Alcohol. Clin. Exp. Res. 2017, 41, 1191–1200. [Google Scholar] [CrossRef]
- McKay, M.T.; Cole, J.C. The relationship between balanced and negative time perspectives, and symptoms of anxiety and depression. Psychiatry Res. 2020, 293, 113383. [Google Scholar] [CrossRef]
- Hall, P.A.; Fong, G.T. Temporal self-regulation theory: A model for individual health behavior. Health Psychol. Rev. 2007, 1, 6–52. [Google Scholar] [CrossRef]
- Moore, C.F.; Sabino, V.; Koob, G.F.; Cottone, P. Pathological overeating: Emerging evidence for a compulsivity construct. Neuropsychopharmacology 2017, 42, 1375–1389. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; WHO: Geneva, Switzerland, 2000.
- Orbell, S.; Hagger, M. Temporal framing and the decision to take part in type 2 diabetes screening: Effects of individual differences in consideration of future consequences on persuasion. Health Psychol. 2006, 25, 537. [Google Scholar] [CrossRef] [PubMed]
- Kliemann, N.; Beeken, R.J.; Wardle, J.; Johnson, F. Development and validation of the self-regulation of eating behaviour questionnaire for adults. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 87. [Google Scholar] [CrossRef]
- Chng, S.; Chew, H.S.J.; Joireman, J. When time is of the essence: Development and validation of brief consideration of future (and immediate) consequences scales. Personal. Individ. Differ. 2022, 186, 111362. [Google Scholar] [CrossRef]
- Joireman, J.; Shaffer, M.J.; Balliet, D.; Strathman, A. Promotion orientation explains why future-oriented people exercise and eat healthy: Evidence from the two-factor consideration of future consequences-14 scale. Personal. Soc. Social.Psychol. Bull. 2012, 38, 1272–1287. [Google Scholar] [CrossRef] [PubMed]
- Verplanken, B.; Orbell, S. Reflections on past behavior: A self-report index of habit strength 1. J. Appl. Soc. Psychol. 2003, 33, 1313–1330. [Google Scholar] [CrossRef]
- Gardner, B.; Abraham, C.; Lally, P.; de Bruijn, G.-J. Towards parsimony in habit measurement: Testing the convergent and predictive validity of an automaticity subscale of the Self-Report Habit Index. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 102. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Oja, P.; Sallis, J.F.; Yngve, A.; Ekelund, U.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sport. Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the international physical activity questionnaire short form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med. Care 2003, 41, 1284–1292. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef] [PubMed]
- IPAQ Research Committee. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)-Short and Long Forms. Available online: https://cir.nii.ac.jp/crid/1573950400545533440 (accessed on 2 March 2023).
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Structural equation modelling: Guidelines for determining model fit. Electron. J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar]
- Tzotzas, T.; Vlahavas, G.; Papadopoulou, S.K.; Kapantais, E.; Kaklamanou, D.; Hassapidou, M. Marital status and educational level associated to obesity in Greek adults: Data from the National Epidemiological Survey. BMC Public Health 2010, 10, 732. [Google Scholar] [CrossRef] [PubMed]
- Fu, C.E.; Ng, C.H.; Chew, N.W.; Heng, Z.E.Q.; Chin, Y.H.; Quek, J.; Lim, W.H.; Xiao, J.; Chan, K.E.; Tan, D.J.H.; et al. A poor perspective of self weight significantly increases adverse outcomes in non-alcoholic fatty liver disease (NAFLD). Front. Med. 2022, 9, 2946. [Google Scholar] [CrossRef]
- Averett, S.L.; Sikora, A.; Argys, L.M. For better or worse: Relationship status and body mass index. Econ. Hum. Biol. 2008, 6, 330–349. [Google Scholar] [CrossRef]
- Lee, Y.S.; Biddle, S.; Chan, M.F.; Cheng, A.; Cheong, M.; Chong, Y.S.; Wang, J.; van Dam, R.M.; Tham, K.W.; Teo, S.L.; et al. Health promotion board–ministry of health clinical practice guidelines: Obesity. Singap. Med. J. 2016, 57, 292. [Google Scholar] [CrossRef]
- Park, S.H.; Nicolaou, M.; Dickens, B.S.L.; Yang, Q.; Tan, K.W.; van Dam, R.M. Ethnicity, neighborhood and individual socioeconomic status, and obesity: The Singapore multiethnic cohort. Obesity 2020, 28, 2405–2413. [Google Scholar] [CrossRef]
- Caprio, S.; Daniels, S.R.; Drewnowski, A.; Kaufman, F.R.; Palinkas, L.A.; Rosenbloom, A.L.; Schwimmer, J.; Kirkman, M.S. Influence of race, ethnicity, and culture on childhood obesity: Implications for prevention and treatment. Obesity 2008, 16, 2566–2577. [Google Scholar] [CrossRef]
- Fesinmeyer, M.D.; North, K.E.; Ritchie, M.D.; Lim, U.; Franceschini, N.; Wilkens, L.R.; Peters, U.; Marchand, L.L.; Haiman, C.A.; Buyske, S.; et al. Genetic risk factors for, B.M.I and obesity in an ethnically diverse population: Results from the population architecture using genomics and epidemiology (PAGE) study. Obesity 2013, 21, 835–846. [Google Scholar] [CrossRef]
- Chew, N.; Chong, B.; Ng, C.H.; Kong, G.; Chin, Y.H.; Xiao, W.; Lee, M.; Dan, Y.Y.; Muthiah, M.D.; Foo, R. The genetic interactions between non-alcoholic fatty liver disease and cardiovascular diseases. Front. Genet. 2022, 13, 2145. [Google Scholar] [CrossRef] [PubMed]
- Loos, R.J.F.; Yeo, G.S.H. The genetics of obesity: From discovery to biology. Nat. Rev. Genet. 2022, 23, 120–133. [Google Scholar] [CrossRef] [PubMed]
- Salinas, Y.D.; Wang, L.; DeWan, A.T. Multiethnic genome-wide association study identifies ethnic-specific associations with body mass index in Hispanics and African Americans. BMC Genet. 2016, 17, 78. [Google Scholar] [CrossRef] [PubMed]
- Chew, H.S.J.; Gao, Y.; Shabbir, A.; Lim, S.L.; Geetha, K.; Kim, G.; Chong, C.S.; Lomanto, D.; So, B.Y.J. Personal motivation, self-regulation barriers and strategies for weight loss in people with overweight and obesity: A thematic framework analysis. Public Health Nutr. 2022, 25, 2426–2435. [Google Scholar] [CrossRef] [PubMed]
- Anand, V.V.; Zhe, E.L.C.; Chin, Y.H.; Lim, W.H.; Goh, R.S.J.; Lin, C.; Ng, C.H.; Kong, G.; Tay, P.W.L.; Devi, K.; et al. Barriers and facilitators to engagement with a weight management intervention in Asian patients with overweight or obesity: A Systematic Review. Endocr. Pract. 2022. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Chew, H.S.J.; Lopez, V. Global impact of COVID-19 on weight and weight-related behaviors in the adult population: A scoping review. Int. J. Environ. Res. Public Health 2021, 18, 1876. [Google Scholar] [CrossRef]
- Sumner, J.; Uijtdewilligen, L.; Chu, A.H.; Ng, S.H.; Barreira, T.V.; Sloan, R.A.; Van Dam, R.M.; Müller-Riemenschneider, F. Stepping volume and intensity patterns in a multi-ethnic urban Asian population. BMC Public Health 2018, 18, 1–8. [Google Scholar] [CrossRef]
- Cohen, A.K.; Rai, M.; Rehkopf, D.H.; Abrams, B. Educational attainment and obesity: A systematic review. Obes. Rev. 2013, 14, 989–1005. [Google Scholar] [CrossRef]
- Hsieh, T.H.; Lee, J.J.; Yu, E.W.; Hu, H.Y.; Lin, S.Y.; Ho, C.Y. Association between obesity and education level among the elderly in Taipei, Taiwan between 2013 and 2015: A cross-sectional study. Sci. Rep. 2020, 10, 20285. [Google Scholar] [CrossRef]
- Ogden, C.L.; Fakhouri, T.H.; Carroll, M.D.; Hales, C.M.; Fryar, C.D.; Li, X.; Freedman, D.S. Prevalence of obesity among adults, by household income and education—United States, 2011–2014. Morb. Mortal. Wkly. Rep. 2017, 66, 1369. [Google Scholar] [CrossRef]
- Sahranavard, S.; Miri, M.R.; Salehiniya, H. The relationship between self-regulation and educational performance in students. J. Educ. Health Promot. 2018, 7, 154. [Google Scholar]
- Chung, W.; Lim, S. Factors contributing to educational differences in obesity among women: Evidence from South Korea. BMC Public Health 2020, 20, 1136. [Google Scholar] [CrossRef] [PubMed]
- Lo, Y.T.; Chang, Y.H.; Lee, M.S.; Wahlqvist, M.L. Health and nutrition economics: Diet costs are associated with diet quality. Asia Pac. J. Clin. Nutr. 2009, 18, 598–604. [Google Scholar] [PubMed]
- McKay, D.L.; Houser, R.F.; Blumberg, J.B.; Goldberg, J.P. Nutrition information sources vary with education level in a population of older adults. J. Am. Diet. Assoc. 2006, 106, 1108–1111. [Google Scholar] [CrossRef] [PubMed]
- Adams, M.A.; Sallis, J.F.; Kerr, J.; Conway, T.L.; Saelens, B.E.; Frank, L.D.; Norman, G.J.; Cain, K.L. Neighborhood environment profiles related to physical activity and weight status: A latent profile analysis. Prev. Med. 2011, 52, 326–331. [Google Scholar] [CrossRef]
- Lash, D.N.; Smith, J.E.; Rinehart, J.K. Can the Theory of Planned Behavior predict dietary intention and future dieting in an ethnically diverse sample of overweight and obese veterans attending medical clinics? Appetite 2016, 99, 185–192. [Google Scholar] [CrossRef]
- Chew, H.S.J.; Li, J.; Chng, S. Improving adult eating behaviours by manipulating time perspective: A systematic review and meta-analysis. Psychol. Health 2023, 1–17. [Google Scholar] [CrossRef]
- Gianini, L.M.; White, M.A.; Masheb, R.M. Eating pathology, emotion regulation, and emotional overeating in obese adults with binge eating disorder. Eat. Behav. 2013, 14, 309–313. [Google Scholar] [CrossRef]
- Heatherton, T.F.; Wagner, D.D. Cognitive neuroscience of self-regulation failure. Trends Cogn. Sci. 2011, 15, 132–139. [Google Scholar] [CrossRef]
- Johnson, F.; Pratt, M.; Wardle, J. Dietary restraint and self-regulation in eating behavior. Int. J. Obes. 2012, 36, 665–674. [Google Scholar] [CrossRef]
- Chew, H.S.J.; Lau, S.T.; Lau, Y. Weight-loss interventions for improving emotional eating among adults with high body mass index: A systematic review with meta-analysis and meta-regression. Eur. Eat. Disord. Rev. 2022, 30, 304–327. [Google Scholar] [CrossRef] [PubMed]
- Robinson, O.J.; Vytal, K.; Cornwell, B.R.; Grillon, C. The impact of anxiety upon cognition: Perspectives from human threat of shock studies. Front. Hum. Neurosci. 2013, 7, 203. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, D.L.; White, K.S. The role of anxiety in binge eating behavior: A critical examination of theory and empirical literature. Health Psychol. Res. 2013, 1, 85–92. [Google Scholar] [CrossRef]
- Crisp, A.H.; Gelder, M.G.; Rix, S.; Meltzer, H.I.; Rowlands, O.J. Stigmatisation of people with mental illnesses. Br. J. Psychiatry 2000, 177, 4–7. [Google Scholar] [CrossRef]
- Pang, S.; Liu, J.; Mahesh, M.; Chua, B.Y.; Shahwan, S.; Lee, S.P.; Vaingankar, J.A.; Abdin, E.; Fung, D.S.S.; Chong, S.A.; et al. Stigma among Singaporean youth: A cross-sectional study on adolescent attitudes towards serious mental illness and social tolerance in a multiethnic population. BMJ Open 2017, 7, e016432. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, D.L.; White, K.S. The relation of anxiety, depression, and stress to binge eating behavior. J. Health Psychol. 2015, 20, 887–898. [Google Scholar] [CrossRef]
| Characteristics of Participants | Mean ± SD/Frequency (%) |
|---|---|
| * Age, years | 31.7 ± 10.1 (28.0; 24.0–27.0) |
| Young adults (21–35 years old) | 179 (71.6) |
| Middle aged adults (36–64 years old) | 71 (28.4) |
| Sex | |
| Males | 119 (47.6) |
| Females | 131 (52.4) |
| Marital status | |
| Single | 176 (70.4) |
| Married | 71 (28.4) |
| Divorced | 3 (1.2) |
| Race | |
| Chinese | 188 (75.2) |
| Indian | 29 (11.6) |
| Malay | 26 (10.4) |
| Others | 7 (2.8) |
| Religion | |
| Buddhism | 77 (30.7) |
| Christianity | 60 (24.0) |
| Hinduism | 18 (7.2) |
| Islam | 35 (14.0) |
| Freethinker | 46 (18.4) |
| Others | 14 (5.6) |
| Highest educational level | |
| Primary school | 2 (0.8) |
| Secondary school | 11 (4.4) |
| Pre-university | 77 (30.8) |
| University | 160 (63.7) |
| Per capita household income (SGD/month) | |
| <1000 | 23 (9.2) |
| 1000–3000 | 53 (21.2) |
| 3001–5000 | 60 (24.0) |
| 5001–10,000 | 85 (34.0) |
| >10,000 | 29 (11.6) |
| Residential region | |
| Central | 44 (17.6) |
| East | 20 (8.0) |
| North | 23 (9.2) |
| Northeast | 37 (14.8) |
| West | 81 (32.4) |
| Smoking | |
| No | 238 (95.2) |
| Yes | 12 (4.8) |
| Employment | |
| Part-time | 52 (20.8) |
| Full-time | 189 (75.6) |
| Retired | 9 (3.6) |
| * Body mass index, kg/m2, | 29.2 ± 7.2 (26.4; 24.3–31.3) |
| Overweight (23.0–24.9 kg/m2; moderate risk) | 84 (33.6) |
| Obese I (25.0–29.9 kg/m2; high risk) | 95 (38.0) |
| Obese II (≥30.0 kg/m2; very high risk) | 71 (28.4) |
| BMI Z-score | 0.003 ± 1 |
| * Waist circumference, cm | 93.4 ± 18.9 (89; 81.3–99.0) |
| High (male ≥ 90 cm; female ≥ 80 cm) | 171 (68.4) |
| Waist Circumference Z-score | 0.001 ± 1 |
| Characteristics of Participants | Mean ± SD/Frequency (%) |
|---|---|
| Intention to change eating behaviors | 5.7 ± 1.2 |
| SRHI (overeating) | 4.3 ± 1.5 |
| Behavioral frequency (overeating) | 4.4 ± 1.6 |
| Automaticity (overeating) | 4.3 ± 1.6 |
| Self-identify (overeating) | 4.0 ± 1.6 |
| SRHI (snacking) | 4.2 ± 1.4 |
| Behavioral frequency (snacking) | 4.5 ± 1.6 |
| Automaticity (snacking) | 4.0 ± 1.6 |
| Self-identify (snacking) | 4.1 ± 1.5 |
| CFCS-6 total | 4.4 ± 1.1 |
| CFCS-6 immediate | 4.3 ± 1.6 |
| CFCS-6 future | 5.0 ± 1.1 |
| SREBQ | 2.9 ± 0.5 |
| Low | 90 (35.9) |
| Moderate | 149 (59.6) |
| High | 11 (4.4) |
| GAD-2 | 1.79 ± 1.60 |
| Potentially at risk (≥3) | 61 (24.4) |
| PHQ-2 | 1.54 ± 1.59 |
| Potentially at risk (≥3) | 52 (20.8) |
| IPAQ-SF, MET-min/week | 2184.4 ± 2557.4 |
| Low | 88 (35.2) |
| Moderate | 65 (26.0) |
| High | 85 (34.0) |
| Identifies the following foods as tempting: | |
| Chocolate | 164 (65.6) |
| Crisps | 172 (68.8) |
| Cake | 167 (66.8) |
| Ice cream | 151 (60.4) |
| Fried foods | 149 (59.6) |
| Chips | 118 (47.2) |
| Bread/toast | 109 (43.6) |
| Pastries | 102 (40.8) |
| Pizza | 100 (40.0) |
| Biscuits | 60 (24.0) |
| Fizzy drinks | 59 (23.6) |
| Sweets | 46 (18.6) |
| Others | 41 (16.4) |
| Popcorn | 37 (14.8) |
| Nil | 8 (3.2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chew, H.S.J.; Loong, S.S.E.; Lim, S.L.; Tam, W.S.W.; Chew, N.W.S.; Chin, Y.H.; Chao, A.M.; Dimitriadis, G.K.; Gao, Y.; So, B.Y.J.; et al. Socio-Demographic, Behavioral and Psychological Factors Associated with High BMI among Adults in a Southeast Asian Multi-Ethnic Society: A Structural Equation Model. Nutrients 2023, 15, 1826. https://doi.org/10.3390/nu15081826
Chew HSJ, Loong SSE, Lim SL, Tam WSW, Chew NWS, Chin YH, Chao AM, Dimitriadis GK, Gao Y, So BYJ, et al. Socio-Demographic, Behavioral and Psychological Factors Associated with High BMI among Adults in a Southeast Asian Multi-Ethnic Society: A Structural Equation Model. Nutrients. 2023; 15(8):1826. https://doi.org/10.3390/nu15081826
Chicago/Turabian StyleChew, Han Shi Jocelyn, Shaun Seh Ern Loong, Su Lin Lim, Wai San Wilson Tam, Nicholas W. S. Chew, Yip Han Chin, Ariana M. Chao, Georgios K. Dimitriadis, Yujia Gao, Bok Yan Jimmy So, and et al. 2023. "Socio-Demographic, Behavioral and Psychological Factors Associated with High BMI among Adults in a Southeast Asian Multi-Ethnic Society: A Structural Equation Model" Nutrients 15, no. 8: 1826. https://doi.org/10.3390/nu15081826
APA StyleChew, H. S. J., Loong, S. S. E., Lim, S. L., Tam, W. S. W., Chew, N. W. S., Chin, Y. H., Chao, A. M., Dimitriadis, G. K., Gao, Y., So, B. Y. J., & Shabbir, A. (2023). Socio-Demographic, Behavioral and Psychological Factors Associated with High BMI among Adults in a Southeast Asian Multi-Ethnic Society: A Structural Equation Model. Nutrients, 15(8), 1826. https://doi.org/10.3390/nu15081826









