Carbohydrate Intake and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Prospective Studies
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analysis
3. Results
3.1. Literature Search
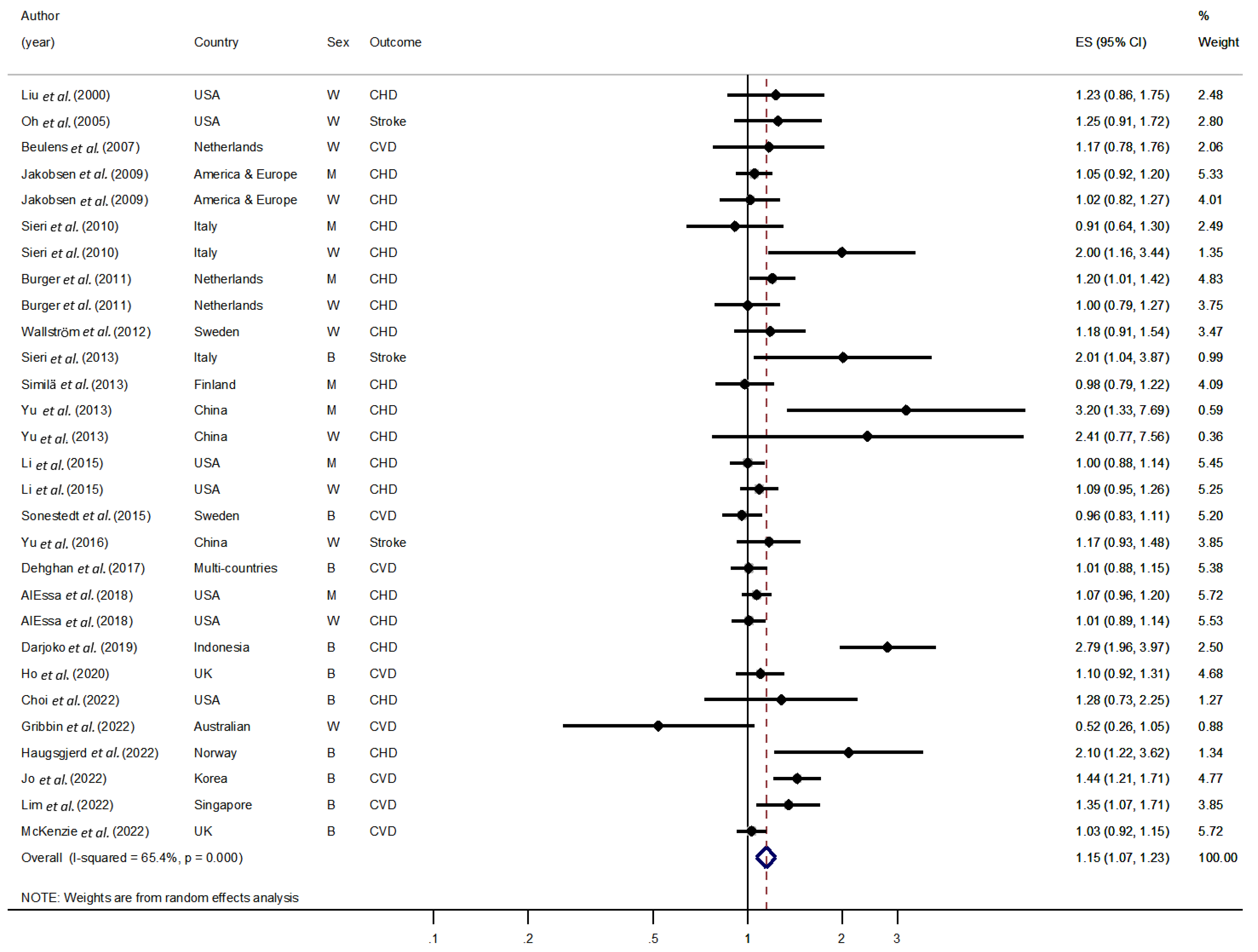
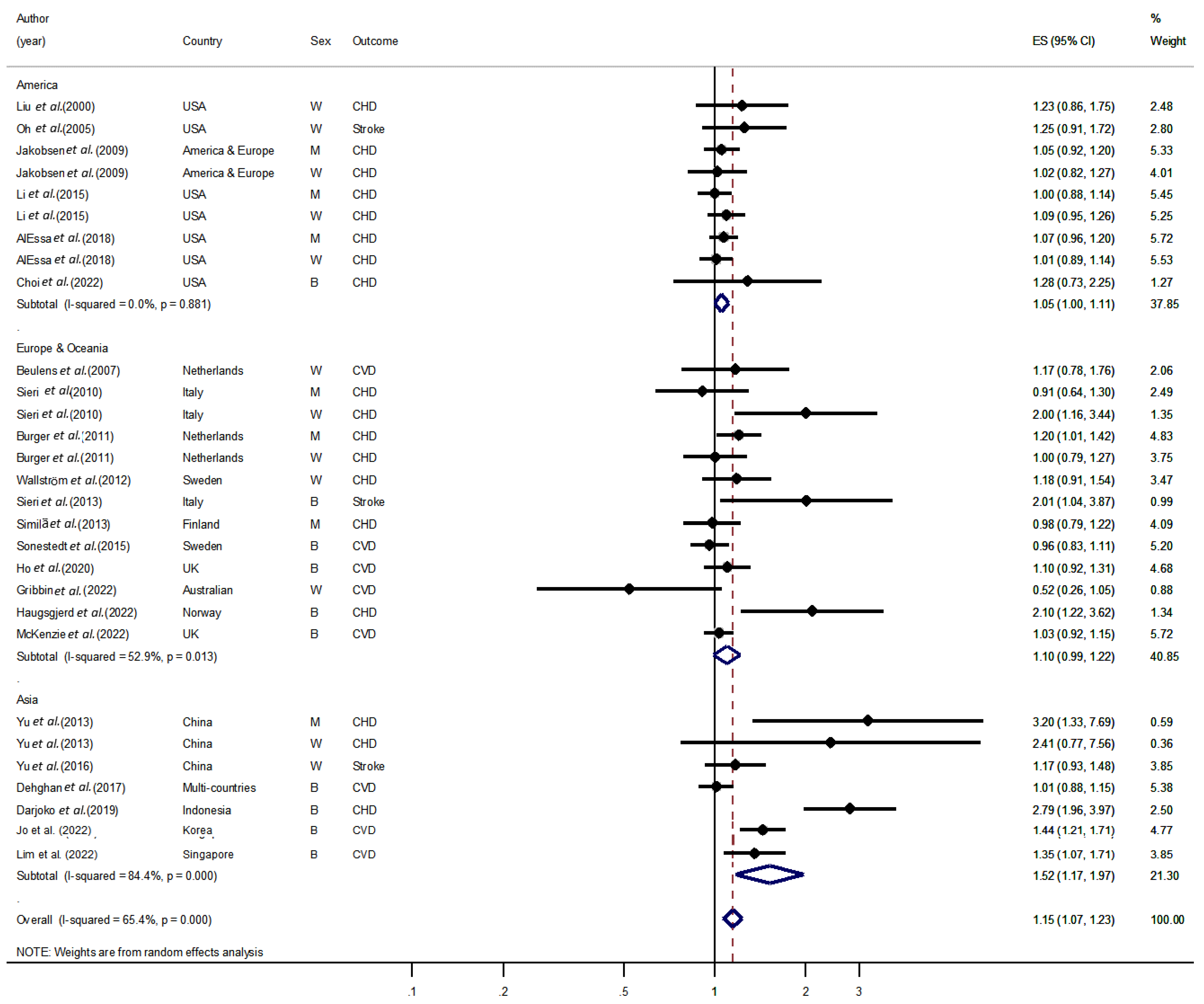
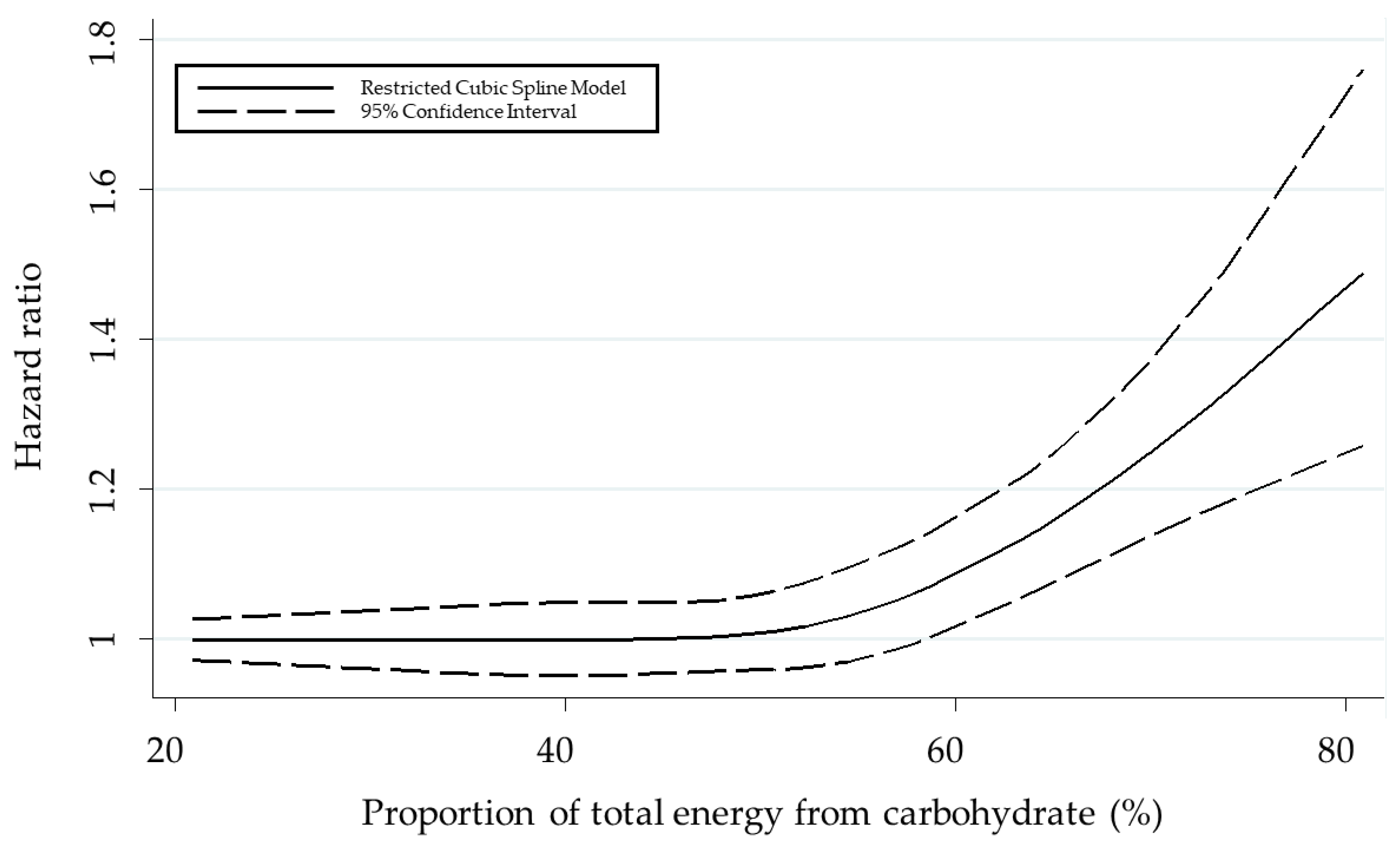
3.2. Pooled Results on the Association between Carbohydrate Intake and CVD
3.3. Influence Analysis and Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 9 September 2022).
- World Health Organization. Prevention of Cardiovascular Disease Guidelines for Assessment and Management of Cardiovascular Risk. Available online: https://apps.who.int/iris/handle/10665/43685 (accessed on 1 November 2022).
- Cena, H.; Calder, P.C. Defining a healthy diet: Evidence for the role of contemporary dietary patterns in health and disease. Nutrients 2020, 12, 334. [Google Scholar] [CrossRef] [PubMed]
- Azzam, A. Is the world converging to a ‘Western diet’? Public Health Nutr. 2021, 24, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Schmidhuber, J.; Sur, P.; Fay, K.; Huntley, B.; Salama, J.; Lee, A.; Cornaby, L.; Horino, M.; Murray, C.; Afshin, A. The Global Nutrient Database: Availability of macronutrients and micronutrients in 195 countries from 1980 to 2013. Lancet Planet. Health 2018, 2, e353–e368. [Google Scholar] [CrossRef]
- Dehghan, M.; Mente, A.; Zhang, X.; Swaminathan, S.; Li, W.; Mohan, V.; Iqbal, R.; Kumar, R.; Wentzel-Viljoen, E.; Rosengren, A. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): A prospective cohort study. Lancet 2017, 390, 2050–2062. [Google Scholar] [CrossRef] [PubMed]
- Ha, K.; Kim, K.; Chun, O.K.; Joung, H.; Song, Y. Differential association of dietary carbohydrate intake with metabolic syndrome in the US and Korean adults: Data from the 2007–2012 NHANES and KNHANES. Eur. J. Clin. Nutr. 2018, 72, 848–860. [Google Scholar] [CrossRef]
- Parks, E.J. Effect of dietary carbohydrate on triglyceride metabolism in humans. J. Nutr. 2001, 131, 2772S–2774S. [Google Scholar] [CrossRef] [PubMed]
- Esan, O.; Wierzbicki, A.S. Triglycerides and cardiovascular disease. Curr. Opin. Cardiol. 2021, 36, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Poznyak, A.V.; Kashirskikh, D.A.; Sukhorukov, V.N.; Kalmykov, V.; Omelchenko, A.V.; Orekhov, A.N. Cholesterol Transport Dysfunction and Its Involvement in Atherogenesis. Int. J. Mol. Sci. 2022, 23, 1332. [Google Scholar] [CrossRef]
- Mohammadifard, N.; Mansourian, M.; Firouzi, S.; Taheri, M.; Haghighatdoost, F. Longitudinal association of dietary carbohydrate and the risk cardiovascular disease: A dose-response meta-analysis. Crit. Rev. Food Sci. Nutr. 2021, 62, 6277–6292. [Google Scholar] [CrossRef]
- Darjoko, S.T.; Wahyuningsih, T.; Sudikno, S. High carbohydrate intake increases risk of coronary heart disease in adults: A prospective cohort study. Universa Med. 2019, 38, 90–99. [Google Scholar] [CrossRef]
- Jo, U.; Park, K. Carbohydrate-Based Diet May Increase the Risk of Cardiovascular Disease: A Pooled Analysis of Two Prospective Cohort Studies; Poster Session Presented at the Annual Meeting of the Korean Society of Food Science and Nutrition: Jeju Island, Republic of Korea, 2022. [Google Scholar]
- Lim, C.G.; Tai, E.S.; van Dam, R.M. Replacing dietary carbohydrates and refined grains with different alternatives and risk of cardiovascular diseases in a multi-ethnic Asian population. Am. J. Clin. Nutr. 2022, 115, 854–863. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.; Gallaher, D.D.; Svendsen, K.; Meyer, K.A.; Steffen, L.M.; Schreiner, P.J.; Shikany, J.M.; Rana, J.S.; Duprez, D.A.; Jacobs, D.R., Jr. Simple Nutrient-Based Rules vs. a Nutritionally Rich Plant-Centered Diet in Prediction of Future Coronary Heart Disease and Stroke: Prospective Observational Study in the US. Nutrients 2022, 14, 469. [Google Scholar] [CrossRef] [PubMed]
- Gribbin, S.; Enticott, J.; Hodge, A.M.; Moran, L.; Thong, E.; Joham, A.; Zaman, S. Association of carbohydrate and saturated fat intake with cardiovascular disease and mortality in Australian women. Heart 2022, 108, 932–939. [Google Scholar] [CrossRef]
- Haugsgjerd, T.R.; Egeland, G.M.; Nygård, O.K.; Igland, J.; Sulo, G.; Lysne, V.; Vinknes, K.J.; Bjornevik, K.; Tell, G.S. Intake of carbohydrates and SFA and risk of CHD in middle-age adults: The Hordaland Health Study (HUSK). Public Health Nutr. 2022, 25, 634–648. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, B.L.; Harris, K.; Peters, S.A.; Webster, J.; Woodward, M. The association of energy and macronutrient intake with all-cause mortality, cardiovascular disease and dementia: Findings from 120,963 women and men in the UK Biobank. Br. J. Nutr. 2022, 127, 1858–1867. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. Newcastle-Ottawa Quality Assessment Scale Cohort Studies; University of Ottawa: Ottawa, ON, Canada, 2014. [Google Scholar]
- Lee, J. Meta-analysis. J. Korean Endocr. Soc. 2008, 23, 361–378. [Google Scholar] [CrossRef]
- Liu, Q.; Cook, N.R.; Bergström, A.; Hsieh, C.-C. A two-stage hierarchical regression model for meta-analysis of epidemiologic nonlinear dose–response data. Comput. Stat. Data Anal. 2009, 53, 4157–4167. [Google Scholar] [CrossRef]
- Orsini, N.; Bellocco, R.; Greenland, S. Generalized least squares for trend estimation of summarized dose–response data. Stata J. 2006, 6, 40–57. [Google Scholar] [CrossRef]
- Liu, S.; Willett, W.C.; Stampfer, M.J.; Hu, F.B.; Franz, M.; Sampson, L.; Hennekens, C.H.; Manson, J.E. A prospective study of dietary glycemic load, carbohydrate intake, and risk of coronary heart disease in US women. Am. J. Clin. Nutr. 2000, 71, 1455–1461. [Google Scholar] [CrossRef]
- Oh, K.; Hu, F.B.; Cho, E.; Rexrode, K.M.; Stampfer, M.J.; Manson, J.E.; Liu, S.; Willett, W.C. Carbohydrate intake, glycemic index, glycemic load, and dietary fiber in relation to risk of stroke in women. Am. J. Epidemiol. 2005, 161, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Beulens, J.W.; de Bruijne, L.M.; Stolk, R.P.; Peeters, P.H.; Bots, M.L.; Grobbee, D.E.; van der Schouw, Y.T. High dietary glycemic load and glycemic index increase risk of cardiovascular disease among middle-aged women: A population-based follow-up study. J. Am. Coll. Cardiol. 2007, 50, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Jakobsen, M.U.; O’Reilly, E.J.; Heitmann, B.L.; Pereira, M.A.; Bälter, K.; Fraser, G.E.; Goldbourt, U.; Hallmans, G.; Knekt, P.; Liu, S. Major types of dietary fat and risk of coronary heart disease: A pooled analysis of 11 cohort studies. Am. J. Clin. Nutr. 2009, 89, 1425–1432. [Google Scholar] [CrossRef] [PubMed]
- Sieri, S.; Krogh, V.; Berrino, F.; Evangelista, A.; Agnoli, C.; Brighenti, F.; Pellegrini, N.; Palli, D.; Masala, G.; Sacerdote, C. Dietary glycemic load and index and risk of coronary heart disease in a large italian cohort: The EPICOR study. Arch. Intern. Med. 2010, 170, 640–647. [Google Scholar] [CrossRef] [PubMed]
- Burger, K.N.; Beulens, J.W.; Boer, J.M.; Spijkerman, A.M.; van der A, D.L. Dietary glycemic load and glycemic index and risk of coronary heart disease and stroke in Dutch men and women: The EPIC-MORGEN study. PLoS ONE 2011, 6, e25955. [Google Scholar] [CrossRef]
- Wallström, P.; Sonestedt, E.; Hlebowicz, J.; Ericson, U.; Drake, I.; Persson, M.; Gullberg, B.; Hedblad, B.; Wirfält, E. Dietary fiber and saturated fat intake associations with cardiovascular disease differ by sex in the Malmö Diet and Cancer Cohort: A prospective study. PLoS ONE 2012, 7, e31637. [Google Scholar] [CrossRef]
- Sieri, S.; Brighenti, F.; Agnoli, C.; Grioni, S.; Masala, G.; Bendinelli, B.; Sacerdote, C.; Ricceri, F.; Tumino, R.; Giurdanella, M.C. Dietary glycemic load and glycemic index and risk of cerebrovascular disease in the EPICOR cohort. PLoS ONE 2013, 8, e62625. [Google Scholar] [CrossRef]
- Similä, M.E.; Kontto, J.P.; Männistö, S.; Valsta, L.M.; Virtamo, J. Glycaemic index, carbohydrate substitution for fat and risk of CHD in men. Br. J. Nutr. 2013, 110, 1704–1711. [Google Scholar] [CrossRef]
- Yu, D.; Shu, X.-O.; Li, H.; Xiang, Y.-B.; Yang, G.; Gao, Y.-T.; Zheng, W.; Zhang, X. Dietary carbohydrates, refined grains, glycemic load, and risk of coronary heart disease in Chinese adults. Am. J. Epidemiol. 2013, 178, 1542–1549. [Google Scholar] [CrossRef]
- Li, Y.; Hruby, A.; Bernstein, A.M.; Ley, S.H.; Wang, D.D.; Chiuve, S.E.; Sampson, L.; Rexrode, K.M.; Rimm, E.B.; Willett, W.C. Saturated fats compared with unsaturated fats and sources of carbohydrates in relation to risk of coronary heart disease: A prospective cohort study. J. Am. Coll. Cardiol. 2015, 66, 1538–1548. [Google Scholar] [CrossRef]
- Sonestedt, E.; Hellstrand, S.; Schulz, C.-A.; Wallström, P.; Drake, I.; Ericson, U.; Gullberg, B.; Hedblad, B.; Orho-Melander, M. The association between carbohydrate-rich foods and risk of cardiovascular disease is not modified by genetic susceptibility to dyslipidemia as determined by 80 validated variants. PLoS ONE 2015, 10, e0126104. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.; Zhang, X.; Shu, X.-O.; Cai, H.; Li, H.; Ding, D.; Hong, Z.; Xiang, Y.-B.; Gao, Y.-T.; Zheng, W. Dietary glycemic index, glycemic load, and refined carbohydrates are associated with risk of stroke: A prospective cohort study in urban Chinese women. Am. J. Clin. Nutr. 2016, 104, 1345–1351. [Google Scholar] [CrossRef] [PubMed]
- AlEssa, H.B.; Cohen, R.; Malik, V.S.; Adebamowo, S.N.; Rimm, E.B.; Manson, J.E.; Willett, W.C.; Hu, F.B. Carbohydrate quality and quantity and risk of coronary heart disease among US women and men. Am. J. Clin. Nutr. 2018, 107, 257–267. [Google Scholar] [CrossRef]
- Ho, F.K.; Gray, S.R.; Welsh, P.; Petermann-Rocha, F.; Foster, H.; Waddell, H.; Anderson, J.; Lyall, D.; Sattar, N.; Gill, J.M. Associations of fat and carbohydrate intake with cardiovascular disease and mortality: Prospective cohort study of UK Biobank participants. BMJ 2020, 368, m688. [Google Scholar] [CrossRef]
- Shan, Z.; Rehm, C.D.; Rogers, G.; Ruan, M.; Wang, D.D.; Hu, F.B.; Mozaffarian, D.; Zhang, F.F.; Bhupathiraju, S.N. Trends in dietary carbohydrate, protein, and fat intake and diet quality among US adults, 1999–2016. JAMA 2019, 322, 1178–1187. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Zhang, Z.; Liu, M.; Zhang, Y.; Li, H.; He, P.; Li, Q.; Liu, C.; Qin, X. Dietary carbohydrate intake and new-onset diabetes: A nationwide cohort study in China. Metabolism 2021, 123, 154865. [Google Scholar] [CrossRef]
- Saito, A.; Imai, S.; Htun, N.C.; Okada, E.; Yoshita, K.; Yoshiike, N.; Takimoto, H. The trends in total energy, macronutrients and sodium intake among Japanese: Findings from the 1995–2016 National Health and Nutrition Survey. Br. J. Nutr. 2018, 120, 424–434. [Google Scholar] [CrossRef]
- Kwon, Y.-J.; Lee, H.S.; Park, J.-Y.; Lee, J.-W. Associating intake proportion of carbohydrate, fat, and protein with all-cause mortality in Korean adults. Nutrients 2020, 12, 3208. [Google Scholar] [CrossRef]
- Tan, V.; Lee, Y.; Venkataraman, K.; Khoo, E.; Tai, E.; Chong, Y.; Gluckman, P.; Leow, M.; Khoo, C. Ethnic differences in insulin sensitivity and beta-cell function among Asian men. Nutr. Diabetes 2015, 5, e173. [Google Scholar] [CrossRef]
- Chan, J.C.; Malik, V.; Jia, W.; Kadowaki, T.; Yajnik, C.S.; Yoon, K.-H.; Hu, F.B. Diabetes in Asia: Epidemiology, risk factors, and pathophysiology. JAMA 2009, 301, 2129–2140. [Google Scholar] [CrossRef]
- Rhee, E.-J.; Kim, H.C.; Kim, J.H.; Lee, E.Y.; Kim, B.J.; Kim, E.M.; Song, Y.; Lim, J.H.; Kim, H.J.; Choi, S. 2018 Guidelines for the management of dyslipidemia in Korea. J. Lipid Atheroscler. 2019, 8, 78–131. [Google Scholar] [CrossRef] [PubMed]
- Parks, E.J.; Hellerstein, M.K. Carbohydrate-induced hypertriacylglycerolemia: Historical perspective and review of biological mechanisms. Am. J. Clin. Nutr. 2000, 71, 412–433. [Google Scholar] [CrossRef] [PubMed]
- Ameer, F.; Scandiuzzi, L.; Hasnain, S.; Kalbacher, H.; Zaidi, N. De novo lipogenesis in health and disease. Metabolism 2014, 63, 895–902. [Google Scholar] [CrossRef] [PubMed]
- Yanai, H.; Katsuyama, H.; Hamasaki, H.; Abe, S.; Tada, N.; Sako, A. Effects of carbohydrate and dietary fiber intake, glycemic index and glycemic load on HDL metabolism in Asian populations. J. Clin. Med. Res. 2014, 6, 321. [Google Scholar] [CrossRef]
- Ma, Y.; Li, Y.; Chiriboga, D.E.; Olendzki, B.C.; Hebert, J.R.; Li, W.; Leung, K.; Hafner, A.R.; Ockene, I.S. Association between carbohydrate intake and serum lipids. J. Am. Coll. Nutr. 2006, 25, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Kopin, L.; Lowenstein, C.J. Dyslipidemia. Ann. Intern. Med. 2017, 167, ITC81–ITC96. [Google Scholar] [CrossRef]
- Mikkelsen, K.; Apostolopoulos, V. B vitamins and ageing. Biochem. Cell Biol. Ageing Part I Biomed. Sci. 2018, 90, 451–470. [Google Scholar]
- Soh, S.M.; Chung, S.-J.; Yoon, J. Dietary and health characteristics of Korean adults according to the level of energy intake from carbohydrate: Analysis of the 7th (2016–2017) Korea National Health and Nutrition Examination Survey Data. Nutrients 2020, 12, 429. [Google Scholar] [CrossRef] [PubMed]
- Wu, G. Dietary protein intake and human health. Food Funct. 2016, 7, 1251–1265. [Google Scholar] [CrossRef]
- Miller, G.D.; Jarvis, J.K.; McBean, L.D. The importance of meeting calcium needs with foods. J. Am. Coll. Nutr. 2001, 20, 168S–185S. [Google Scholar] [CrossRef]
| Population | Adults |
|---|---|
| Exposure | Carbohydrate intake |
| Comparator | Highest vs. lowest categories of exposure |
| Reference range vs. every range of exposure | |
| Outcomes | Cardiovascular disease |
| Study design | Cohort study |
| PICOS, participant, intervention (exposure), comparison, outcome, and study design | |
| Author (Year) | Country | Age (Year) | N | Sex | Study Name | Follow-Up Year | Dietary Assessment Method | Outcomes | HR/RR (95% CI) | Adjustment | Study Quality Score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Liu et al. (2000) [24] | USA | 38–63 | 75,521 | W | NHS | 10 | FFQ | CHD | 1.23 (0.86–1.75) | Residual energy-adjusted carbohydrate, age, BMI, cigarette smoking, alcohol intake, parental family history of myocardial infarction before the age of 60 y, self-reported history of hypertension or history of high cholesterol, menopausal status, aspirin use, use of multiple vitamin or vitamin E supplement, physical activity, protein intake, intake of saturated, polyunsaturated, trans fats, dietary fiber, vitamin E, folate, and total energy intake | 7 |
| Oh et al. (2005) [25] | USA | 30–55 | 78,779 | W | NHS | 18 | FFQ | Stoke | 1.25 (0.91–1.73) | Age, BMI, smoking, alcohol intake, parental history of MI, history of hypertension, hypercholesterolemia, diabetes, menopausal status, postmenopausal hormone use, aspirin use, multivitamin use, vitamin E supplement use, physical activity, energy, cereal fiber, saturated fat, MUFA, PUFA, trans fat, and omega-3 fatty acids | 7 |
| Beulens et al. (2007) [26] | Netherlands | 49–70 | 15,714 | W | EPIC | 9 | FFQ | CVD | 1.17 (0.78–1.77) | Age, hypertension, cholesterolemia, smoking, BMI, mean systolic blood pressure, total physical activity, menopausal status, hormone replacement therapy use, oral contraceptives use, alcohol intake, total energy intake, energy-adjusted intake of vitamin E, protein, dietary fiber, folate, saturated fat, MUFA, and PUFA | 6 |
| Jakobsen et al. (2009) [27] | American and Europe | 47–61 | 344,696 | M W | AHS, ARIC, ATBC, FMC, GPS, HPFS, IIHD, IWHS, NHS, VIP, WHS | 4–10 | FFQ or DH | CHD | 1.05 (0.92–1.21) 1.02 (0.82–1.28) | Intakes MUFA, PUFA, trans fat, protein, glycemic carbohydrate, energy, smoking, BMI, physical activity, education, alcohol intake and history of hypertension | 5 |
| Sieri et al. (2010) [28] | Italy | M: 35–64 W: 35–74 | 47,749 | M W | EPICOR | 7.9 | FFQ | CHD | 0.91 (0.64–1.30) 2.00 (1.16–3.43) | Non-alcohol energy intake, hypertension, smoking, education, categories of alcohol intake, BMI, fiber intake, and physical activity | 7 |
| Burger et al. (2011) [29] | Netherlands | 21–64 | 19,608 | M W | EPIC-MORGEN | 11.9 | FFQ | CHD | 1.20 (1.02–1.43) 1.00 (0.79–1.28) | Age, smoking packyears, education, BMI, physical activity, hypertension, oral contraceptive use, total energy, energy-adjusted nutrients (alcohol, vitamin C, dietary fiber, saturated fat, monounsaturated fat), plasma total cholesterol, and HDL-C | 6 |
| Wallström et al. (2012) [30] | Sweden | 44–73 | 20,674 | W | MDCS | 13.5 (mean) | FFQ & 7-days DH | CHD | 1.18 (0.91–1.54) | Age, method version, total energy intake, season, BMI class, smoking category, education, alcohol category, systolic blood pressure, antihypertensive treatment, antihyperlipidemic treatment, leisure time physical activity, and quintiles of energy-adjusted dietary fiber | 7 |
| Sieri et al. (2013) [31] | Italy | 35–75 | 44,099 | B | EPIC | 10.9 | FFQ | Stoke | 2.01 (1.04–3.86) | Sex, age, education, smoking, BMI, alcohol, non-alcohol, energy intake, cereal fiber intake, saturated fat, monounsaturated fat, polyunsaturated fat, and physical activity | 7 |
| Similä et al. (2013) [32] | Finland | 50–69 | 21,955 | M | ATBC | 19 | FFQ | CHD | 0.98 (0.79–1.22) | Age, intervention group, smoking, BMI, physical activity, serum total and HDL-C, blood pressure, and intakes of energy, alcohol, total fat, protein, magnesium, and potassium | 6 |
| Yu et al. (2013) [33] | China | M: 40–74 W: 40–70 | 117,366 | M W | SWHS & SMHS | 5.4 (mean) | FFQ | CHD | 3.20 (1.33–7.68) 2.41 (0.77–7.57) | Age, educational level, income, smoking status, alcohol consumption, physical activity level, waist-to-hip ratio, history of hypertension, dietary intakes of total energy, saturated fat, and protein | 7 |
| Li et al. (2015) [34] | USA | M: 40–75 W: 30–55 | 127,536 | M W | NHS & HPFS | M: >24 W: >30 | FFQ | CHD | 1.00 (0.88–1.14) 1.09 (0.94–1.25) | Total energy intake, the energy contribution from protein, cholesterol intake, alcohol intake, smoking status, BMI, physical activity, use of vitamins, aspirin, family history of MI, diabetes, presence of baseline hypercholesterolemia and hypertension, and percentage of energy from carbohydrates from whole grains, from refined starches/sugars and from other foods simultaneously | 7 |
| Sonestedt et al. (2015) [35] | Sweden | 44–74 | 26,445 | B | MDCS | 14 | DH | CVD | 0.96 (0.83–1.11) | Age, sex, season, diet method version, energy intake, BMI, smoking, alcohol consumption, leisure-time physical activity, and education | 7 |
| Yu et al. (2016) [36] | China | 40–70 | 64,328 | W | SWHS | 10 (mean) | FFQ | Stoke | 1.17 (0.92–1.47) | Age, education, cigarette smoking, BMI, family history of stroke, history of hypertension, history of dyslipidemia, total energy intake, saturated fat intake, and a partial diet quality score | 7 |
| Dehghan et al. (2017) [6] | Multicenteris | 35–70 | 135,335 | B | PURE study | 7.4 | FFQ | CVD | 1.01 (0.88–1.15) | Age, sex, education, waist-to-hip ratio, smoking, physical activity, diabetes, urban or rural location, and energy intake | 6 |
| AlEssa et al. (2018) [37] | USA | M: 40–75 W: 30–55 | 117,885 | M W | NHS & HPFS | M: 26 F: 28 | FFQ | CHD | 1.07 (0.96–1.20) 1.01 (0.89–1.14) | Age, BMI, family history of CHD, smoking status, alcohol intake, physical activity level, multivitamin use, aspirin use, vitamin E use, race, total energy, polyunsaturated fat–to–saturated fat ratio and trans fat | 7 |
| Darjoko et al. (2019) [12] | Indonesia | Over 25 | 4840 | B | CS-RFNCD | 6 | FFQ & food recall questionnaire | CHD | 2.79 (1.96–3.97) | - | 5 |
| Ho et al. (2020) [38] | UK | 37–73 | 195,658 | B | UK Biobank | 10.6 | 24 h RC | CVD | 1.10 (0.91–1.30) | Age, sex, deprivation index, ethnicity, smoking status, height, BMI, systolic blood pressure, baseline diabetes, mental health disorders, total physical activity, daily alcohol intake, and total energy intake | 7 |
| Choi et al. (2022) [15] | USA | 18–30 | 4701 | B | CARDIA | 32 (median) | Interviewer-administered DH | CHD | 1.28 (0.72–2.22) | Age at baseline, sex, race, total energy intake, maximal educational attainment, parental history of CVD, pack-years of smoking, physical activity level, use of lipid-lowering medications, and BMI | 6 |
| Gribbin et al. (2022) [16] | Australia | 52.5 ± 1.5 | 9899 | W | ALSWH | 15 | FFQ | CVD | 0.52 (0.26–1.06) | Age, menopausal status, country of birth, area of residence, occupation, education, household income, marital status, smoking status, physical activity levels, BMI, polycystic ovary syndrome, gestational diabetes mellitus, hypertension, diabetes mellitus, % saturated fat intake, % PUFA, % MUFA, % cholesterol, % alcohol, fiber, glycemic index, and glycemic load | 6 |
| Haugsgjerd et al. (2022) [17] | Norway | 46–49 | 2995 | B | HUSK | 10.8 (mean) | FFQ | CHD | 2.10 (1.22–3.63) | Age, sex, energy intake, physical activity, and smoking | 7 |
| Jo et al. (2022) [13] | Korea | over 40 | 173,696 | B | KoGES | KARE: 9.59 HEXA: 4.25 | FFQ | CVD | 1.44 (1.21–1.71) | Age, sex, household income, smoking status, alcohol consumption status, physical activity level, and obesity status | 6 |
| Lim et al. (2022) [14] | Singapore | 21–65 | 12,408 | B | Singapore MEC | 10.1 (mean) | FFQ | CVD | 1.35 (1.07–1.71) | Age, sex, ethnicity, total energy intake, moderate-to-vigorous physical activity, smoking, alcohol consumption, educational level, history of diabetes, hypertension, dyslipidemia, family history of heart disease, menopausal status, BMI, intake of fiber and cholesterol for carbohydrate, and mutually adjusted for intake of all other nutrients except for carbohydrate for the remaining nutrients | 7 |
| McKenzie et al. (2022) [18] | UK | 40–69 | 120,963 | B | UK biobank | 11.1 (mean) | Two or more 24 h RC | CVD | 1.03 (0.92–1.15) | Age, smoking, sex, height, weight, mean alcohol intake, physical activity, systolic blood pressure, Townsend score, diabetes, lipid-lowering medication, and antihypertensive medication | 7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jo, U.; Park, K. Carbohydrate Intake and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Prospective Studies. Nutrients 2023, 15, 1740. https://doi.org/10.3390/nu15071740
Jo U, Park K. Carbohydrate Intake and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Prospective Studies. Nutrients. 2023; 15(7):1740. https://doi.org/10.3390/nu15071740
Chicago/Turabian StyleJo, Unhui, and Kyong Park. 2023. "Carbohydrate Intake and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Prospective Studies" Nutrients 15, no. 7: 1740. https://doi.org/10.3390/nu15071740
APA StyleJo, U., & Park, K. (2023). Carbohydrate Intake and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Prospective Studies. Nutrients, 15(7), 1740. https://doi.org/10.3390/nu15071740







