Maternal Dietary Deficiencies in Folic Acid and Choline Result in Larger Damage Volume, Reduced Neuro-Degeneration and -Inflammation and Changes in Choline Metabolites after Ischemic Stroke in Middle-Aged Offspring
Abstract
1. Introduction
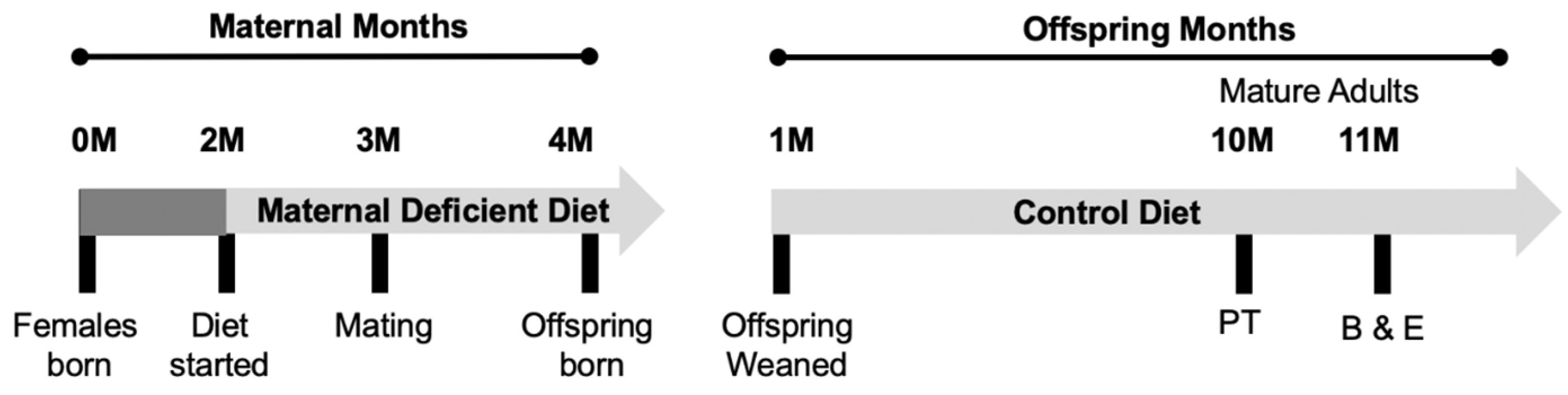
2. Materials and Methods
2.1. Dietary Composition
2.2. Photothrombosis Model
2.3. Behavioral Testing
2.3.1. Accelerating Rotarod
2.3.2. Forepaw Placement
2.3.3. Ladder Beam Walking
2.4. Brain Tissue Collection and Sectioning
2.5. Immunofluorescence Staining
2.6. Plasma One-Carbon Metabolite Measurements
2.7. Data Analysis and Statistics
3. Results
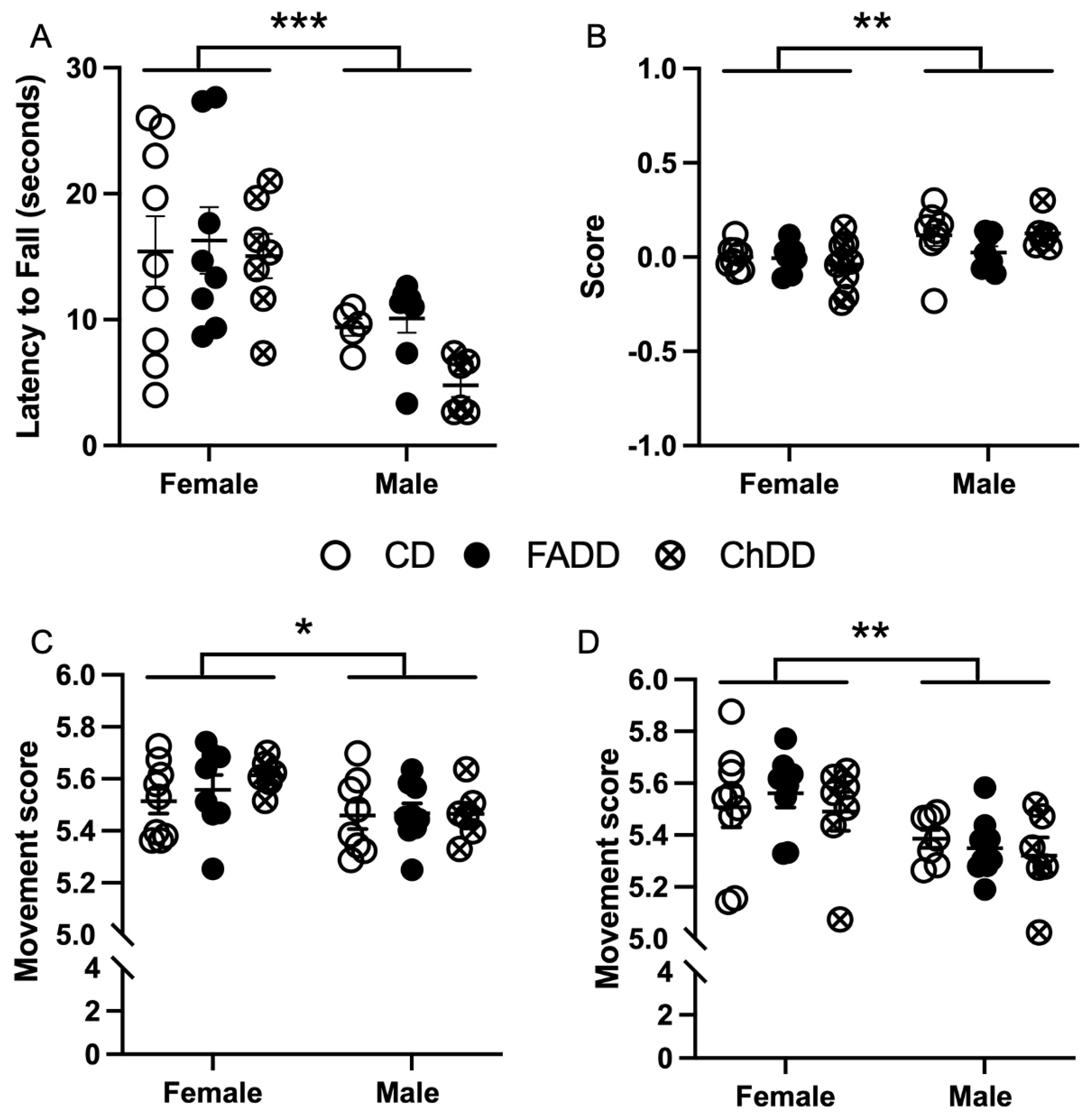
3.1. Accelerating Rotarod
3.2. Forepaw Placement
3.3. Ladder Beam
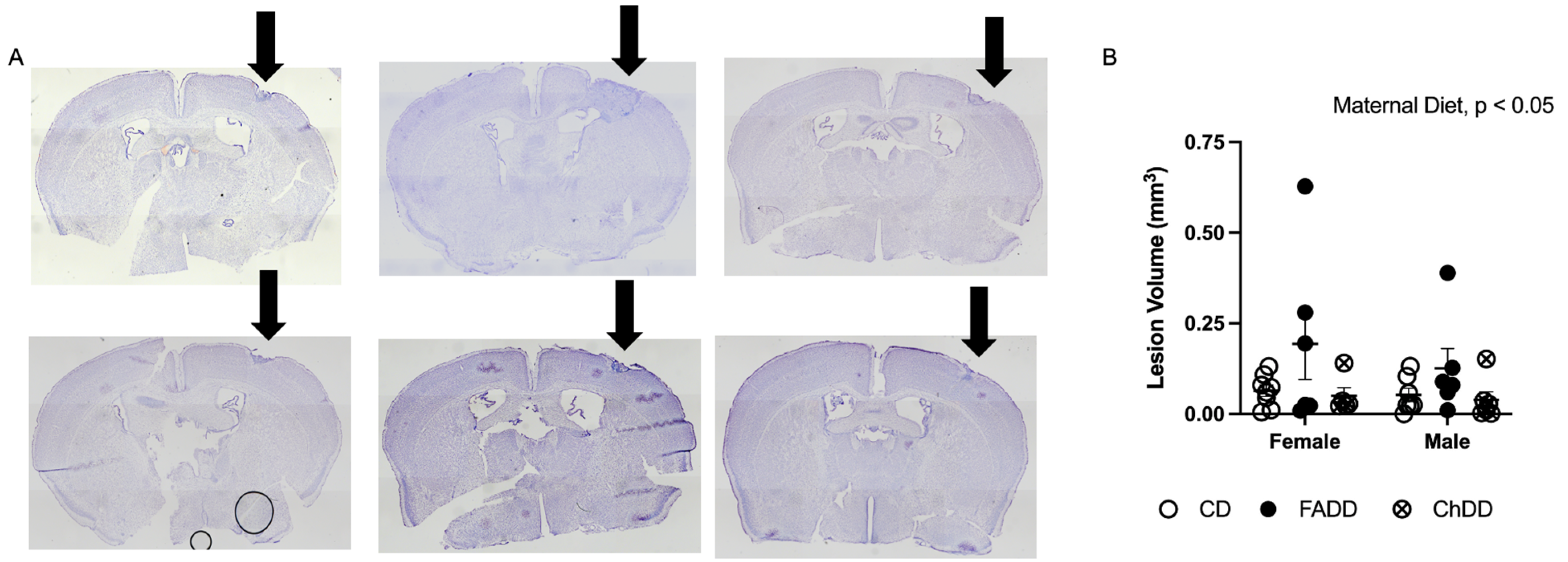
3.4. Ischemic Damage Volume Increased in Offspring as a Result of Maternal Dietary Deficiencies
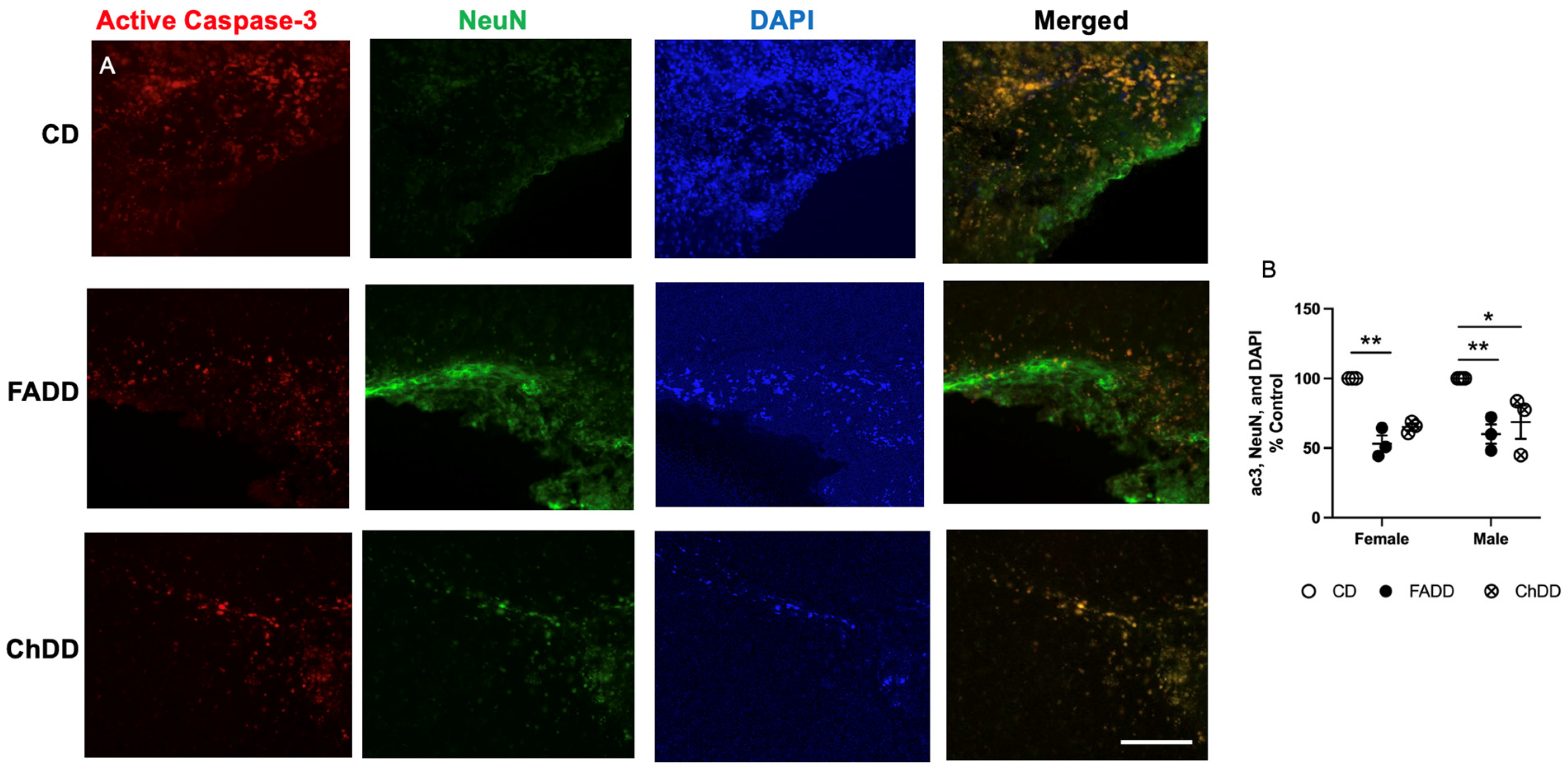
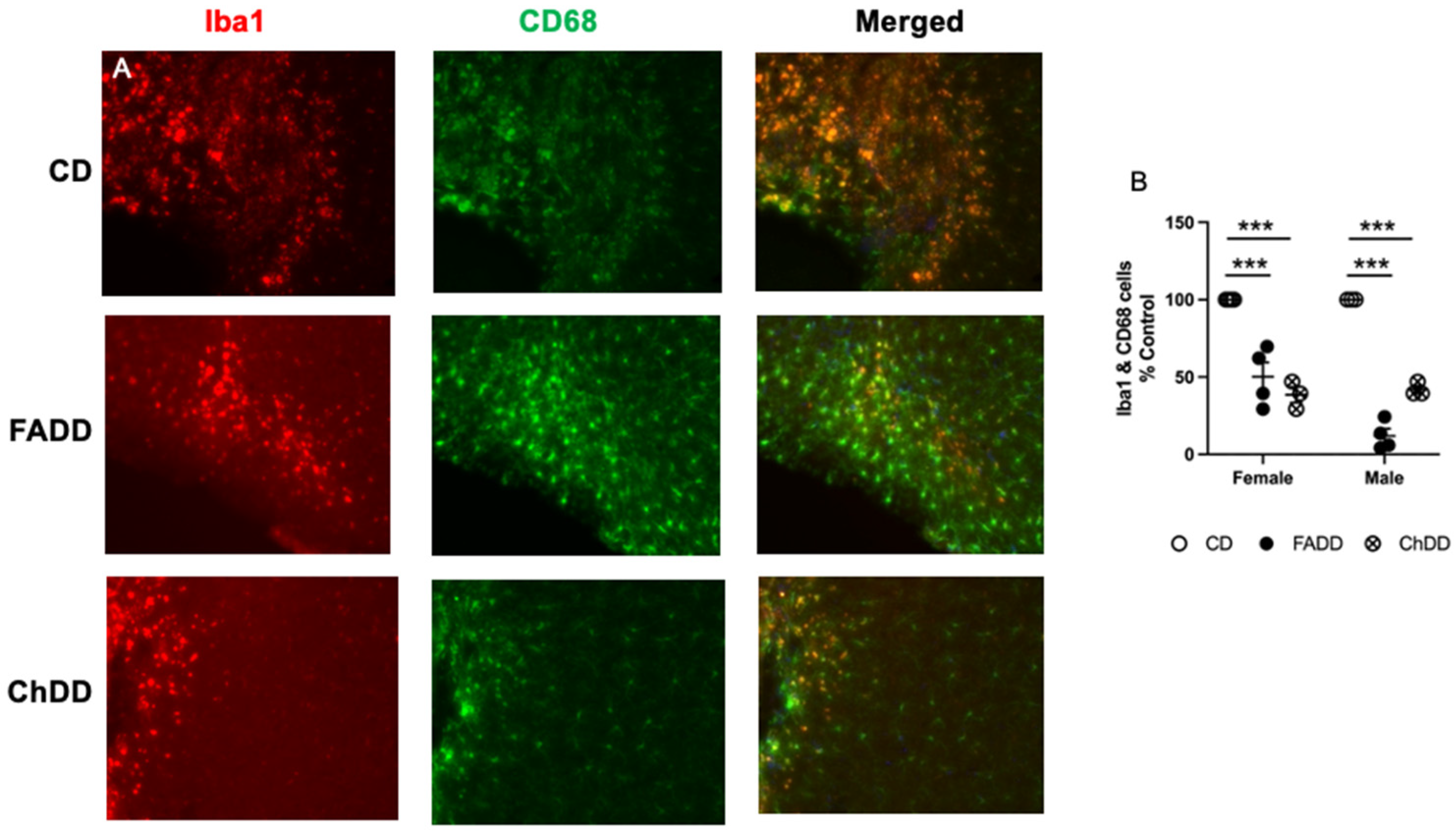
3.5. Decreased Neurodegeneration and Neuroinflammation in Male and Female Offspring from Deficient Mothers
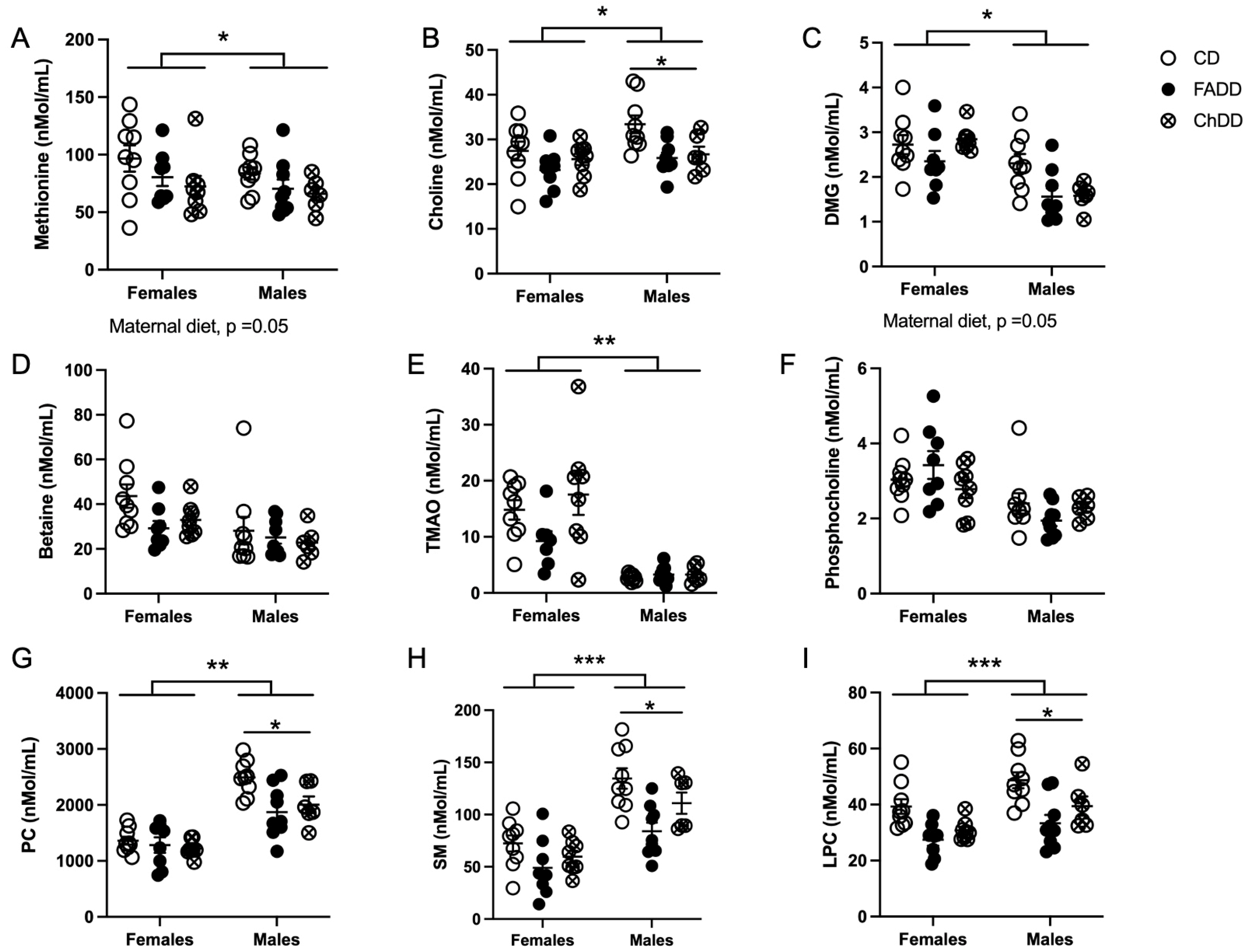
3.6. Plasma One-Carbon Metabolites
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Bejot, Y.; Daubail, B.; Jacquin, A.; Durier, J.; Osseby, G.-V.; Rouaud, O.; Giroud, M. Trends in the Incidence of Ischaemic Stroke in Young Adults between 1985 and 2011: The Dijon Stroke Registry. J. Neurol. Neurosurg. Psychiatry 2014, 85, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Cabral, N.L.; Freire, A.T.; Conforto, A.B.; Dos Santos, N.; Reis, F.I.; Nagel, V.; Guesser, V.V.; Safanelli, J.; Longo, A.L. Increase of Stroke Incidence in Young Adults in a Middle-Income Country: A 10-Year Population-Based Study. Stroke 2017, 48, 2925–2930. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Yang, L.; Yang, R.; Xu, W.; Chen, F.-P.; Li, N.; Zhang, J.-B. Ischemic Stroke in Young Adults of Northern China: Characteristics and Risk Factors for Recurrence. Eur. Neurol. 2017, 77, 115–122. [Google Scholar] [CrossRef]
- Rosengren, A.; Giang, K.W.; Lappas, G.; Jern, C.; Torén, K.; Björck, L. Twenty-Four-Year Trends in the Incidence of Ischemic Stroke in Sweden from 1987 to 2010. Stroke 2013, 44, 2388–2393. [Google Scholar] [CrossRef]
- Tang, M.; Yao, M.; Zhu, Y.; Peng, B.; Zhou, L.; Ni, J. Sex Differences of Ischemic Stroke in Young Adults—A Single-Center Chinese Cohort Study. J. Stroke Cerebrovasc. Dis. 2020, 29, 105087. [Google Scholar] [CrossRef] [PubMed]
- Tibæk, M.; Dehlendorff, C.; Jørgensen, H.S.; Forchhammer, H.B.; Johnsen, S.P.; Kammersgaard, L.P. Increasing Incidence of Hospitalization for Stroke and Transient Ischemic Attack in Young Adults: A Registry-Based Study. J. Am. Heart Assoc. 2016, 5, e003158. [Google Scholar] [CrossRef] [PubMed]
- Lecoffre, C.; de Peretti, C.; Gabet, A.; Grimaud, O.; Woimant, F.; Giroud, M.; Béjot, Y.; Olié, V. National Trends in Patients Hospitalized for Stroke and Stroke Mortality in France, 2008 to 2014. Stroke 2017, 48, 2939–2945. [Google Scholar] [CrossRef]
- Kissela, B.M.; Khoury, J.C.; Alwell, K.; Moomaw, C.J.; Woo, D.; Adeoye, O.; Flaherty, M.L.; Khatri, P.; Ferioli, S.; De Los Rios La Rosa, F.; et al. Age at Stroke: Temporal Trends in Stroke Incidence in a Large, Biracial Population. Neurology 2012, 79, 1781–1787. [Google Scholar] [CrossRef]
- Ramirez, L.; Kim-Tenser, M.A.; Sanossian, N.; Cen, S.; Wen, G.; He, S.; Mack, W.J.; Towfighi, A. Trends in Acute Ischemic Stroke Hospitalizations in the United States. J. Am. Heart Assoc. 2016, 5, e003233. [Google Scholar] [CrossRef]
- Kumar, A.; Aakriti; Gupta, V. A Review on Animal Models of Stroke: An Update. Brain Res. Bull. 2016, 122, 35–44. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; de Ferranti, S.; Després, J.-P.; Fullerton, H.J.; Howard, V.J.; et al. Heart Disease and Stroke Statistics—2015 Update. Circulation 2015, 131, e29–e322. [Google Scholar] [CrossRef] [PubMed]
- Sabbouh, T.; Torbey, M.T. Malnutrition in Stroke Patients: Risk Factors, Assessment, and Management. Neurocrit. Care 2018, 29, 374–384. [Google Scholar] [CrossRef]
- Ali, S.A.; Economides, D.L. Folic Acid Supplementation. Curr. Opin. Obstet. Gynecol. 2000, 12, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Bahous, R.H.; Jadavji, N.M.; Deng, L.; Cosín-Tomás, M.; Lu, J.; Malysheva, O.; Leung, K.-Y.; Ho, M.-K.; Pallàs, M.; Kaliman, P.; et al. High Dietary Folate in Pregnant Mice Leads to Pseudo-MTHFR Deficiency and Altered Methyl Metabolism, with Embryonic Growth Delay and Short-Term Memory Impairment in Offspring. Hum. Mol. Genet. 2017, 26, 888–900. [Google Scholar] [CrossRef] [PubMed]
- Zeisel, S.H.; Niculescu, M.D. Perinatal Choline Influences Brain Structure and Function. Nutr. Rev. 2006, 64, 197–203. [Google Scholar] [CrossRef]
- Locasale, J.W. Serine, Glycine and One-Carbon Units: Cancer Metabolism in Full Circle. Nat. Rev. Cancer 2013, 13, 572–583. [Google Scholar] [CrossRef]
- Mentch, S.J.; Locasale, J.W. One-Carbon Metabolism and Epigenetics: Understanding the Specificity. Ann. N. Y. Acad. Sci. 2016, 1363, 91–98. [Google Scholar] [CrossRef]
- Hankey, G.J. B Vitamins for Stroke Prevention. Stroke Vasc. Neurol. 2018, 3, 51–58. [Google Scholar] [CrossRef]
- Spence, J.D. B Vitamin Therapy for Homocysteine: Renal Function and Vitamin B12 Determine Cardiovascular Outcomes. Clin. Chem. Lab. Med. 2013, 51, 633–637. [Google Scholar] [CrossRef]
- Spence, J.D.; Yi, Q.; Hankey, G.J. B Vitamins in Stroke Prevention: Time to Reconsider. Lancet Neurol. 2017, 16, 750–760. [Google Scholar] [CrossRef]
- Li, Y.; Huang, T.; Zheng, Y.; Muka, T.; Troup, J.; Hu, F.B. Folic Acid Supplementation and the Risk of Cardiovascular Diseases: A Meta-Analysis of Randomized Controlled Trials. J. Am. Heart Assoc. 2016, 5, e003768. [Google Scholar] [CrossRef]
- Blusztajn, J.K.; Slack, B.E.; Mellott, T.J. Neuroprotective Actions of Dietary Choline. Nutrients 2017, 9, 815. [Google Scholar] [CrossRef] [PubMed]
- Virdi, S.; Jadavji, N.M. The Impact of Maternal Folates on Brain Development and Function after Birth. Metabolites 2022, 12, 876. [Google Scholar] [CrossRef] [PubMed]
- Jadavji, N.M.; Deng, L.; Malysheva, O.; Caudill, M.A.; Rozen, R. MTHFR Deficiency or Reduced Intake of Folate or Choline in Pregnant Mice Results in Impaired Short-Term Memory and Increased Apoptosis in the Hippocampus of Wild-Type Offspring. Neuroscience 2015, 300, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Jadavji, N.M.; Farr, T.; Khalil, A.; Boehm-Sturm, P.; Foddis, M.; Harms, C.; Füchtemeier, M.; Dirnagl, U. Elevated Levels of Plasma Homocysteine, Deficiencies in Dietary Folic Acid and Uracil-DNA Glycosylase Impair Learning in a Mouse Model of Vascular Cognitive Impairment. Behav. Brain Res. 2015, 283, 215–226. [Google Scholar] [CrossRef]
- Clementson, M.; Hurley, L.; Coonrod, S.; Bennett, C.; Marella, P.; Pascual, A.S.; Pull, K.; Wasek, B.; Bottiglieri, T.; Malysheva, O.; et al. Maternal Dietary Deficiencies in Folates or Choline during Pregnancy and Lactation Worsen Stroke Outcome in 3-Month-Old Male and Female Mouse Offspring. biorXiv 2022. [Google Scholar] [CrossRef]
- Jadavji, N.M.; Emmerson, J.T.; MacFarlane, A.J.; Willmore, W.G.; Smith, P.D. B-Vitamin and Choline Supplementation Increases Neuroplasticity and Recovery after Stroke. Neurobiol. Dis. 2017, 103, 89–100. [Google Scholar] [CrossRef]
- Farr, T.D.; Liu, L.; Colwell, K.L.; Whishaw, I.Q.; Metz, G.A. Bilateral Alteration in Stepping Pattern after Unilateral Motor Cortex Injury: A New Test Strategy for Analysis of Skilled Limb Movements in Neurological Mouse Models. J. Neurosci. Methods 2006, 153, 104–113. [Google Scholar] [CrossRef]
- Jensen, E.C. Quantitative Analysis of Histological Staining and Fluorescence Using Image. J. Anat. Rec. 2013, 296, 378–381. [Google Scholar] [CrossRef]
- Holm, P.; Ueland, P.M.; Kvalheim, G.; Lien, E.A. Determination of Choline, Betaine, and Dimethylglycine in Plasma by a High-Throughput Method Based on Normal-Phase Chromatography—Tandem Mass Spectrometry. Clin. Chem. 2003, 49, 286–294. [Google Scholar] [CrossRef]
- Koc, H.; Mar, M.H.; Ranasinghe, A.; Swenberg, J.A.; Zeisel, S.H. Quantitation of Choline and Its Metabolites in Tissues and Foods by Liquid Chromatography/Electrospray Ionization-Isotope Dilution Mass Spectrometry. Anal. Chem. 2002, 74, 4734–4740. [Google Scholar] [CrossRef] [PubMed]
- Taesuwan, S.; McDougall, M.Q.; Malysheva, O.V.; Bender, E.; Nevins, J.E.H.; Devapatla, S.; Vidavalur, R.; Caudill, M.A.; Klatt, K.C. Choline Metabolome Response to Prenatal Choline Supplementation across Pregnancy: A Randomized Controlled Trial. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2021, 35, e22063. [Google Scholar] [CrossRef] [PubMed]
- Jadavji, N.M.; Murray, L.K.; Emmerson, J.T.; Rudyk, C.A.; Hayley, S.; Smith, P.D. Paraquat Exposure Increases Oxidative Stress Within the Dorsal Striatum of Male Mice With a Genetic Deficiency in One-Carbon Metabolism. Toxicol. Sci. 2019, 169, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Tulchinsky, T.H. Micronutrient Deficiency Conditions: Global Health Issues. Public Health Rev. 2010, 32, 243–255. [Google Scholar] [CrossRef]
- Brann, D.W.; Dhandapani, K.; Wakade, C.; Mahesh, V.B.; Khan, M.M. Neurotrophic and Neuroprotective Actions of Estrogen: Basic Mechanisms and Clinical Implications. Steroids 2007, 72, 381. [Google Scholar] [CrossRef] [PubMed]
- Alkayed, N.J.; Harukuni, I.; Kimes, A.S.; London, E.D.; Traystman, R.J.; Hurn, P.D. Gender-Linked Brain Injury in Experimental Stroke. Stroke 1998, 29, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Park, E.-M.; Cho, S.; Frys, K.A.; Glickstein, S.B.; Zhou, P.; Anrather, J.; Ross, M.E.; Iadecola, C. Inducible Nitric Oxide Synthase Contributes to Gender Differences in Ischemic Brain Injury. J. Cereb. Blood Flow Metab. 2005, 26, 392–401. [Google Scholar] [CrossRef]
- Toung, T.J.K.; Traystman, R.J.; Hurn, P.D. Estrogen-Mediated Neuroprotection After Experimental Stroke in Male Rats. Stroke 1998, 29, 1666–1670. [Google Scholar] [CrossRef]
- Miller, N.R.; Jover, T.; Cohen, H.W.; Zukin, R.S.; Etgen, A.M. Estrogen Can Act via Estrogen Receptor α and β to Protect Hippocampal Neurons against Global Ischemia-Induced Cell Death. Endocrinology 2005, 146, 3070–3079. [Google Scholar] [CrossRef]
- Ferguson, S.A.; Berry, K.J.; Hansen, D.K.; Wall, K.S.; White, G.; Antony, A.C. Behavioral Effects of Prenatal Folate Deficiency in Mice. Birth Defects Res. Part—Clin. Mol. Teratol. 2005, 73, 249–252. [Google Scholar] [CrossRef]
- Labat-gest, V.; Tomasi, S. Photothrombotic Ischemia: A Minimally Invasive and Reproducible Photochemical Cortical Lesion Model for Mouse Stroke Studies. J. Vis. Exp. 2013, 76, e50370. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hurley, L.; Jauhal, J.; Ille, S.; Pull, K.; Malysheva, O.V.; Jadavji, N.M. Maternal Dietary Deficiencies in Folic Acid and Choline Result in Larger Damage Volume, Reduced Neuro-Degeneration and -Inflammation and Changes in Choline Metabolites after Ischemic Stroke in Middle-Aged Offspring. Nutrients 2023, 15, 1556. https://doi.org/10.3390/nu15071556
Hurley L, Jauhal J, Ille S, Pull K, Malysheva OV, Jadavji NM. Maternal Dietary Deficiencies in Folic Acid and Choline Result in Larger Damage Volume, Reduced Neuro-Degeneration and -Inflammation and Changes in Choline Metabolites after Ischemic Stroke in Middle-Aged Offspring. Nutrients. 2023; 15(7):1556. https://doi.org/10.3390/nu15071556
Chicago/Turabian StyleHurley, Lauren, Jesse Jauhal, Sharadyn Ille, Kasey Pull, Olga V. Malysheva, and Nafisa M. Jadavji. 2023. "Maternal Dietary Deficiencies in Folic Acid and Choline Result in Larger Damage Volume, Reduced Neuro-Degeneration and -Inflammation and Changes in Choline Metabolites after Ischemic Stroke in Middle-Aged Offspring" Nutrients 15, no. 7: 1556. https://doi.org/10.3390/nu15071556
APA StyleHurley, L., Jauhal, J., Ille, S., Pull, K., Malysheva, O. V., & Jadavji, N. M. (2023). Maternal Dietary Deficiencies in Folic Acid and Choline Result in Larger Damage Volume, Reduced Neuro-Degeneration and -Inflammation and Changes in Choline Metabolites after Ischemic Stroke in Middle-Aged Offspring. Nutrients, 15(7), 1556. https://doi.org/10.3390/nu15071556






