Cross-Sectional Association of Dietary Patterns and Supplement Intake with Presence and Gray-Scale Median of Carotid Plaques—A Comparison between Women and Men in the Population-Based Hamburg City Health Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Study Design
2.2. Ultrasound Images
2.3. Gray-Scale Median
2.4. Questionnaires and Dietary Scores
2.5. Statistical Analysis
3. Results
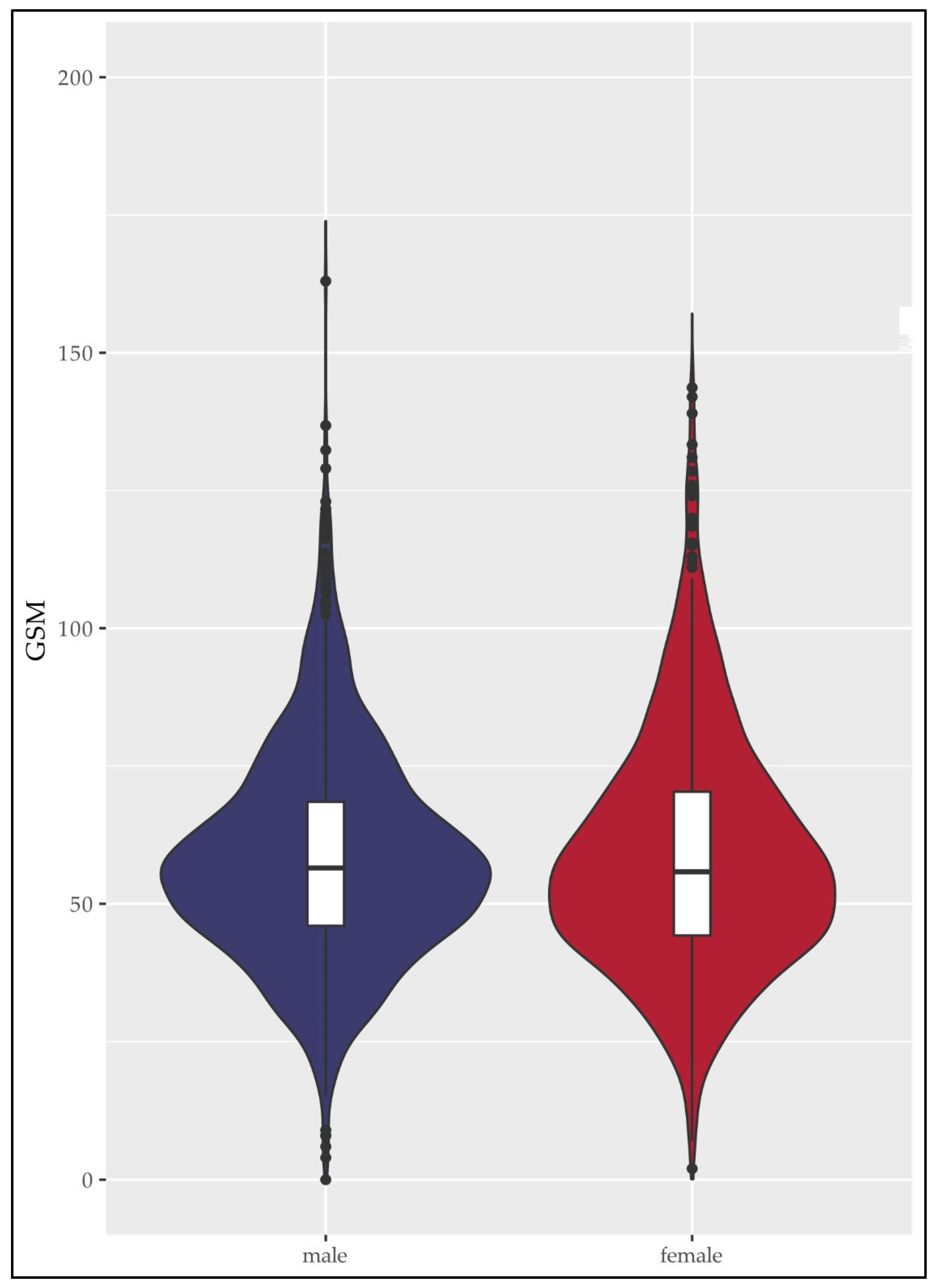
3.1. Baseline Characteristics of GSM-Sub-Cohort
3.2. Linear Regression of Nutrition Parameters and Examined Supplements with GSM in Women and Men
3.3. Results of Logistic Regression Regarding the Presence of Carotid Plaques
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kim, M.J.; Jung, S.K. Nutraceuticals for prevention of atherosclerosis: Targeting monocyte infiltration to the vascular endothelium. J. Food Biochem. 2020, 44, e13200. [Google Scholar] [CrossRef] [PubMed]
- Torres, N.; Guevara-Cruz, M.; Velázquez-Villegas, L.A.; Tovar, A.R. Nutrition and Atherosclerosis. Arch. Med. Res. 2015, 46, 408–426. [Google Scholar] [CrossRef] [PubMed]
- Badimon, L.; Vilahur, G. Thrombosis formation on atherosclerotic lesions and plaque rupture. J. Intern. Med. 2014, 276, 618–632. [Google Scholar] [CrossRef] [PubMed]
- Penson, P.E.; Banach, M. The Role of Nutraceuticals in the Optimization of Lipid-Lowering Therapy in High-Risk Patients with Dyslipidaemia. Curr. Atheroscler. Rep. 2020, 22, 67. [Google Scholar] [CrossRef] [PubMed]
- Scheen, A.J. From atherosclerosis to atherothrombosis: From a silent chronic pathology to an acute critical event. Rev. Med. Liege 2018, 73, 224–228. [Google Scholar]
- Saba, L.; Sanagala, S.S.; Gupta, S.K.; Koppula, V.K.; Johri, A.M.; Sharma, A.M.; Kolluri, R.; Bhatt, D.L.; Nicolaides, A.; Suri, J.S. Ultrasound-based internal carotid artery plaque characterization using deep learning paradigm on a supercomputer: A cardiovascular disease/stroke risk assessment system. Int. J. Cardiovasc. Imaging 2021, 37, 1511–1528. [Google Scholar] [CrossRef]
- Baud, J.M.; Stanciu, D.; Yeung, J.; Maurizot, A.; Chabay, S.; de Malherbe, M.; Chadenat, M.L.; Bachelet, D.; Pico, F. Contrast enhanced ultrasound of carotid plaque in acute ischemic stroke (CUSCAS study). Rev. Neurol. 2021, 177, 115–123. [Google Scholar] [CrossRef]
- Flaherty, M.L.; Kissela, B.; Khoury, J.C.; Alwell, K.; Moomaw, C.J.; Woo, D.; Khatri, P.; Ferioli, S.; Adeoye, O.; Broderick, J.P.; et al. Carotid artery stenosis as a cause of stroke. Neuroepidemiology 2013, 40, 36–41. [Google Scholar] [CrossRef]
- Gong, H.Y.; Shi, X.K.; Zhu, H.Q.; Chen, X.Z.; Zhu, J.; Zhao, B.W. Evaluation of carotid atherosclerosis and related risk factors using ultrasonic B-Flow technology in elderly patients. J. Int. Med. Res. 2020, 48, 300060520961224. [Google Scholar] [CrossRef]
- Spanos, K.; Tzorbatzoglou, I.; Lazari, P.; Maras, D.; Giannoukas, A.D. Carotid artery plaque echomorphology and its association with histopathologic characteristics. J. Vasc. Surg. 2018, 68, 1772–1780. [Google Scholar] [CrossRef]
- Karim, R.; Xu, W.; Kono, N.; Li, Y.; Yan, M.; Stanczyk, F.Z.; Hodis, H.N.; Mack, W.J. Comparison of Cardiovascular Disease Risk Factors Between 2 Subclinical Atherosclerosis Measures in Healthy Postmenopausal Women: Carotid Artery Wall Thickness and Echogenicity: Carotid Artery Wall Thickness and Echogenicity. J. Ultrasound Med. 2022, 42, 35–44. [Google Scholar] [CrossRef]
- Lorenz, M.W.; Markus, H.S.; Bots, M.L.; Rosvall, M.; Sitzer, M. Prediction of clinical cardiovascular events with carotid intima-media thickness: A systematic review and meta-analysis. Circulation 2007, 115, 459–467. [Google Scholar] [CrossRef]
- Willeit, P.; Tschiderer, L.; Allara, E.; Reuber, K.; Seekircher, L.; Gao, L.; Liao, X.; Lonn, E.; Gerstein, H.C.; Yusuf, S.; et al. Carotid Intima-Media Thickness Progression as Surrogate Marker for Cardiovascular Risk: Meta-Analysis of 119 Clinical Trials Involving 100,667 Patients. Circulation 2020, 142, 621–642. [Google Scholar] [CrossRef] [PubMed]
- Della-Morte, D.; Dong, C.; Crisby, M.; Gardener, H.; Cabral, D.; Elkind, M.S.V.; Gutierrez, J.; Sacco, R.L.; Rundek, T. Association of Carotid Plaque Morphology and Glycemic and Lipid Parameters in the Northern Manhattan Study. Front. Cardiovasc. Med. 2022, 9, 793755. [Google Scholar] [CrossRef] [PubMed]
- Naylor, R.; Rantner, B.; Ancetti, S.; de Borst, G.J.; De Carlo, M.; Halliday, A.; Kakkos, S.K.; Markus, H.S.; McCabe, D.J.H.; Sillesen, H.; et al. European Society for Vascular Surgery (ESVS) 2023 Clinical Practice Guidelines on the Management of Atherosclerotic Carotid and Vertebral Artery Disease. Eur. J. Vasc. Endovasc. Surg. 2022, 65., 7–111. [Google Scholar] [CrossRef]
- Kadoglou, N.P.E.; Moulakakis, K.G.; Mantas, G.; Kakisis, J.D.; Mylonas, S.N.; Valsami, G.; Liapis, C.D. The Association of Arterial Stiffness With Significant Carotid Atherosclerosis and Carotid Plaque Vulnerability. Angiology 2022, 73, 668–674. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Kwong, D.L.; Wu, V.W.; Yip, S.P.; Law, H.K.; Lee, S.W.; Ying, M.T. Computer-assisted ultrasound assessment of plaque characteristics in radiation-induced and non-radiation-induced carotid atherosclerosis. Quant. Imaging Med. Surg. 2021, 11, 2292–2306. [Google Scholar] [CrossRef] [PubMed]
- Doonan, R.J.; Gorgui, J.; Veinot, J.P.; Lai, C.; Kyriacou, E.; Corriveau, M.M.; Steinmetz, O.K.; Daskalopoulou, S.S. Plaque echodensity and textural features are associated with histologic carotid plaque instability. J. Vasc. Surg. 2016, 64, 671–677.e678. [Google Scholar] [CrossRef]
- Grogan, J.K.; Shaalan, W.E.; Cheng, H.; Gewertz, B.; Desai, T.; Schwarze, G.; Glagov, S.; Lozanski, L.; Griffin, A.; Castilla, M.; et al. B-mode ultrasonographic characterization of carotid atherosclerotic plaques in symptomatic and asymptomatic patients. J. Vasc. Surg. 2005, 42, 435–441. [Google Scholar] [CrossRef]
- Mitchell, C.C.; Stein, J.H.; Cook, T.D.; Salamat, S.; Wang, X.; Varghese, T.; Jackson, D.C.; Sandoval Garcia, C.; Wilbrand, S.M.; Dempsey, R.J. Histopathologic Validation of Grayscale Carotid Plaque Characteristics Related to Plaque Vulnerability. Ultrasound Med. Biol. 2017, 43, 129–137. [Google Scholar] [CrossRef]
- Salem, M.K.; Bown, M.J.; Sayers, R.D.; West, K.; Moore, D.; Nicolaides, A.; Robinson, T.G.; Naylor, A.R. Identification of patients with a histologically unstable carotid plaque using ultrasonic plaque image analysis. Eur. J. Vasc. Endovasc. Surg. 2014, 48, 118–125. [Google Scholar] [CrossRef]
- Sztajzel, R.; Momjian, S.; Momjian-Mayor, I.; Murith, N.; Djebaili, K.; Boissard, G.; Comelli, M.; Pizolatto, G. Stratified gray-scale median analysis and color mapping of the carotid plaque: Correlation with endarterectomy specimen histology of 28 patients. Stroke 2005, 36, 741–745. [Google Scholar] [CrossRef]
- Ariyoshi, K.; Okuya, S.; Kunitsugu, I.; Matsunaga, K.; Nagao, Y.; Nomiyama, R.; Takeda, K.; Tanizawa, Y. Ultrasound analysis of gray-scale median value of carotid plaques is a useful reference index for cerebro-cardiovascular events in patients with type 2 diabetes. J. Diabetes Investig. 2015, 6, 91–97. [Google Scholar] [CrossRef] [PubMed]
- el-Barghouty, N.; Nicolaides, A.; Bahal, V.; Geroulakos, G.; Androulakis, A. The identification of the high risk carotid plaque. Eur. J. Vasc. Endovasc. Surg. 1996, 11, 470–478. [Google Scholar] [CrossRef] [PubMed]
- Nicolaides, A.N.; Kakkos, S.K.; Kyriacou, E.; Griffin, M.; Sabetai, M.; Thomas, D.J.; Tegos, T.; Geroulakos, G.; Labropoulos, N.; Doré, C.J.; et al. Asymptomatic internal carotid artery stenosis and cerebrovascular risk stratification. J. Vasc. Surg. 2010, 52, 1481–1485.e5. [Google Scholar] [CrossRef] [PubMed]
- Andersson, J.; Sundstrom, J.; Gustavsson, T.; Hulthe, J.; Elmgren, A.; Zilmer, K.; Zilmer, M.; Lind, L. Echogenecity of the carotid intima-media complex is related to cardiovascular risk factors, dyslipidemia, oxidative stress and inflammation: The Prospective Investigation of the Vasculature in Uppsala Seniors (PIVUS) study. Atherosclerosis 2009, 204, 612–618. [Google Scholar] [CrossRef]
- Jung, M.; Parrinello, C.M.; Xue, X.; Mack, W.J.; Anastos, K.; Lazar, J.M.; Selzer, R.H.; Shircore, A.M.; Plankey, M.; Tien, P.; et al. Echolucency of the carotid artery intima-media complex and intima-media thickness have different cardiovascular risk factor relationships: The Women’s Interagency HIV Study. J. Am. Heart Assoc. 2015, 4, e001405. [Google Scholar] [CrossRef]
- Spence, J.D. Technology Insight: Ultrasound measurement of carotid plaque--patient management, genetic research, and therapy evaluation. Nat. Clin. Pract. Neurol. 2006, 2, 611–619. [Google Scholar] [CrossRef]
- Gepner, A.D.; Young, R.; Delaney, J.A.; Budoff, M.J.; Polak, J.F.; Blaha, M.J.; Post, W.S.; Michos, E.D.; Kaufman, J.; Stein, J.H. Comparison of Carotid Plaque Score and Coronary Artery Calcium Score for Predicting Cardiovascular Disease Events: The Multi-Ethnic Study of Atherosclerosis. J. Am. Heart Assoc. 2017, 6, e005179. [Google Scholar] [CrossRef]
- Hollander, M.; Bots, M.L.; Del Sol, A.I.; Koudstaal, P.J.; Witteman, J.C.; Grobbee, D.E.; Hofman, A.; Breteler, M.M. Carotid plaques increase the risk of stroke and subtypes of cerebral infarction in asymptomatic elderly: The Rotterdam study. Circulation 2002, 105, 2872–2877. [Google Scholar] [CrossRef]
- Vilanova, M.B.; Franch-Nadal, J.; Falguera, M.; Marsal, J.R.; Canivell, S.; Rubinat, E.; Miró, N.; Molló, À.; Mata-Cases, M.; Gratacòs, M.; et al. Prediabetes Is Independently Associated with Subclinical Carotid Atherosclerosis: An Observational Study in a Non-Urban Mediterranean Population. J. Clin. Med. 2020, 9, 2139. [Google Scholar] [CrossRef]
- Wang, C.; Fang, X.; Wu, X.; Hua, Y.; Zhang, Z.; Gu, X.; Tang, Z.; Guan, S.; Liu, H.; Liu, B.; et al. Metabolic syndrome and risks of carotid atherosclerosis and cardiovascular events in community-based older adults in China. Asia Pac. J. Clin. Nutr. 2019, 28, 870–878. [Google Scholar] [CrossRef] [PubMed]
- Munjral, S.; Ahluwalia, P.; Jamthikar, A.D.; Puvvula, A.; Saba, L.; Faa, G.; Singh, I.M.; Chadha, P.S.; Turk, M.; Johri, A.M.; et al. Nutrition, atherosclerosis, arterial imaging, cardiovascular risk stratification, and manifestations in COVID-19 framework: A narrative review. Front. Biosci. 2021, 26, 1312–1339. [Google Scholar] [CrossRef]
- McClintock, T.R.; Parvez, F.; Wu, F.; Islam, T.; Ahmed, A.; Rani Paul, R.; Shaheen, I.; Sarwar, G.; Rundek, T.; Demmer, R.T.; et al. Major dietary patterns and carotid intima-media thickness in Bangladesh. Public. Health Nutr. 2016, 19, 218–229. [Google Scholar] [CrossRef]
- Maddock, J.; Ziauddeen, N.; Ambrosini, G.L.; Wong, A.; Hardy, R.; Ray, S. Adherence to a Dietary Approaches to Stop Hypertension (DASH)-type diet over the life course and associated vascular function: A study based on the MRC 1946 British birth cohort. Br. J. Nutr. 2018, 119, 581–589. [Google Scholar] [CrossRef]
- GómezSánchez, M.; Gómez Sánchez, L.; Patino-Alonso, M.C.; Alonso-Domínguez, R.; Sánchez-Aguadero, N.; Lugones-Sánchez, C.; Rodríguez Sánchez, E.; García Ortiz, L.; Gómez-Marcos, M.A. Adherence to the Mediterranean Diet in Spanish Population and Its Relationship with Early Vascular Aging according to Sex and Age: EVA Study. Nutrients 2020, 12, 1025. [Google Scholar] [CrossRef] [PubMed]
- Koutsonida, M.; Kanellopoulou, A.; Markozannes, G.; Gousia, S.; Doumas, M.T.; Sigounas, D.E.; Tzovaras, V.T.; Vakalis, K.; Tzoulaki, I.; Evangelou, E.; et al. Adherence to Mediterranean Diet and Cognitive Abilities in the Greek Cohort of Epirus Health Study. Nutrients 2021, 13, 3363. [Google Scholar] [CrossRef]
- Gardener, H.; Wright, C.B.; Cabral, D.; Scarmeas, N.; Gu, Y.; Cheung, K.; Elkind, M.S.; Sacco, R.L.; Rundek, T. Mediterranean diet and carotid atherosclerosis in the Northern Manhattan Study. Atherosclerosis 2014, 234, 303–310. [Google Scholar] [CrossRef]
- Jimenez-Torres, J.; Alcala-Diaz, J.F.; Torres-Pena, J.D.; Gutierrez-Mariscal, F.M.; Leon-Acuna, A.; Gomez-Luna, P.; Fernandez-Gandara, C.; Quintana-Navarro, G.M.; Fernandez-Garcia, J.C.; Perez-Martinez, P.; et al. Mediterranean Diet Reduces Atherosclerosis Progression in Coronary Heart Disease: An Analysis of the CORDIOPREV Randomized Controlled Trial. Stroke 2021, 52, 3440–3449. [Google Scholar] [CrossRef]
- Martinez-Gonzalez, M.A.; Salas-Salvado, J.; Estruch, R.; Corella, D.; Fito, M.; Ros, E.; Predimed, I. Benefits of the Mediterranean Diet: Insights From the PREDIMED Study. Prog. Cardiovasc. Dis. 2015, 58, 50–60. [Google Scholar] [CrossRef]
- Mateo-Gallego, R.; Uzhova, I.; Moreno-Franco, B.; Leon-Latre, M.; Casasnovas, J.A.; Laclaustra, M.; Penalvo, J.L.; Civeira, F. Adherence to a Mediterranean diet is associated with the presence and extension of atherosclerotic plaques in middle-aged asymptomatic adults: The Aragon Workers’ Health Study. J. Clin. Lipidol. 2017, 11, 1372–1382. [Google Scholar] [CrossRef] [PubMed]
- Penalvo, J.L.; Fernandez-Friera, L.; Lopez-Melgar, B.; Uzhova, I.; Oliva, B.; Fernandez-Alvira, J.M.; Laclaustra, M.; Pocock, S.; Mocoroa, A.; Mendiguren, J.M.; et al. Association Between a Social-Business Eating Pattern and Early Asymptomatic Atherosclerosis. J. Am. Coll. Cardiol. 2016, 68, 805–814. [Google Scholar] [CrossRef]
- Petersen, K.S.; Clifton, P.M.; Keogh, J.B. The association between carotid intima media thickness and individual dietary components and patterns. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Sala-Vila, A.; Romero-Mamani, E.S.; Gilabert, R.; Nunez, I.; de la Torre, R.; Corella, D.; Ruiz-Gutierrez, V.; Lopez-Sabater, M.C.; Pinto, X.; Rekondo, J.; et al. Changes in ultrasound-assessed carotid intima-media thickness and plaque with a Mediterranean diet: A substudy of the PREDIMED trial. Arter. Thromb. Vasc. Biol. 2014, 34, 439–445. [Google Scholar] [CrossRef]
- Bhat, S.; Mocciaro, G.; Ray, S. The association of dietary patterns and carotid intima-media thickness: A synthesis of current evidence. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 1273–1287. [Google Scholar] [CrossRef]
- Fung, T.T.; Chiuve, S.E.; McCullough, M.L.; Rexrode, K.M.; Logroscino, G.; Hu, F.B. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch. Intern. Med. 2008, 168, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Levitan, E.B.; Wolk, A.; Mittleman, M.A. Consistency with the DASH diet and incidence of heart failure. Arch. Intern. Med. 2009, 169, 851–857. [Google Scholar] [CrossRef]
- Rautiainen, S.; Manson, J.E.; Lichtenstein, A.H.; Sesso, H.D. Dietary supplements and disease prevention—A global overview. Nat. Rev. Endocrinol. 2016, 12, 407–420. [Google Scholar] [CrossRef]
- Rontogianni, M.O.; Kanellopoulou, A.; Markozannes, G.; Bouras, E.; Derdemezis, C.; Doumas, M.T.; Sigounas, D.E.; Tzovaras, V.T.; Vakalis, K.; Panagiotakos, D.B.; et al. Prevalence and Determinants of Sex-Specific Dietary Supplement Use in a Greek Cohort. Nutrients 2021, 13, 2857. [Google Scholar] [CrossRef]
- Chen, F.; Du, M.; Blumberg, J.B.; Ho Chui, K.K.; Ruan, M.; Rogers, G.; Shan, Z.; Zeng, L.; Zhang, F.F. Association Among Dietary Supplement Use, Nutrient Intake, and Mortality Among U.S. Adults: A Cohort Study. Ann. Intern. Med. 2019, 170, 604–613. [Google Scholar] [CrossRef]
- Li, K.; Kaaks, R.; Linseisen, J.; Rohrmann, S. Vitamin/mineral supplementation and cancer, cardiovascular, and all-cause mortality in a German prospective cohort (EPIC-Heidelberg). Eur. J. Nutr. 2012, 51, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Marques-Vidal, P.; Pécoud, A.; Hayoz, D.; Paccaud, F.; Mooser, V.; Waeber, G.; Vollenweider, P. Prevalence and characteristics of vitamin or dietary supplement users in Lausanne, Switzerland: The CoLaus study. Eur. J. Clin. Nutr. 2009, 63, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Rock, C.L. Multivitamin-multimineral supplements: Who uses them? Am. J. Clin. Nutr. 2007, 85, 277s–279s. [Google Scholar] [CrossRef] [PubMed]
- Schwarzpaul, S.; Strassburg, A.; Luhrmann, P.M.; Neuhauser-Berthold, M. Intake of vitamin and mineral supplements in an elderly german population. Ann. Nutr. Metab. 2006, 50, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Dickinson, A.; Blatman, J.; El-Dash, N.; Franco, J.C. Consumer usage and reasons for using dietary supplements: Report of a series of surveys. J. Am. Coll. Nutr. 2014, 33, 176–182. [Google Scholar] [CrossRef]
- Jenkins, D.J.A.; Spence, J.D.; Giovannucci, E.L.; Kim, Y.I.; Josse, R.G.; Vieth, R.; Sahye-Pudaruth, S.; Paquette, M.; Patel, D.; Blanco Mejia, S.; et al. Supplemental Vitamins and Minerals for Cardiovascular Disease Prevention and Treatment: JACC Focus Seminar. J. Am. Coll. Cardiol. 2021, 77, 423–436. [Google Scholar] [CrossRef]
- Li, Y.; Huang, T.; Zheng, Y.; Muka, T.; Troup, J.; Hu, F.B. Folic Acid Supplementation and the Risk of Cardiovascular Diseases: A Meta-Analysis of Randomized Controlled Trials. J. Am. Heart Assoc. 2016, 5, e003768. [Google Scholar] [CrossRef]
- Khan, S.U.; Khan, M.U.; Riaz, H.; Valavoor, S.; Zhao, D.; Vaughan, L.; Okunrintemi, V.; Riaz, I.B.; Khan, M.S.; Kaluski, E.; et al. Effects of Nutritional Supplements and Dietary Interventions on Cardiovascular Outcomes: An Umbrella Review and Evidence Map. Ann. Intern. Med. 2019, 171, 190–198. [Google Scholar] [CrossRef]
- Tian, T.; Yang, K.Q.; Cui, J.G.; Zhou, L.L.; Zhou, X.L. Folic Acid Supplementation for Stroke Prevention in Patients with Cardiovascular Disease. Am. J. Med. Sci. 2017, 354, 379–387. [Google Scholar] [CrossRef]
- Jagodzinski, A.; Johansen, C.; Koch-Gromus, U.; Aarabi, G.; Adam, G.; Anders, S.; Augustin, M.; der Kellen, R.B.; Beikler, T.; Behrendt, C.A.; et al. Rationale and Design of the Hamburg City Health Study. Eur. J. Epidemiol. 2020, 35, 169–181. [Google Scholar] [CrossRef]
- Mathiesen, E.B.; Bonaa, K.H.; Joakimsen, O. Echolucent plaques are associated with high risk of ischemic cerebrovascular events in carotid stenosis: The tromso study. Circulation 2001, 103, 2171–2175. [Google Scholar] [CrossRef] [PubMed]
- Odhner, I. JS Paint [software]. Available online: https://github.com/1j01/jspaint (accessed on 15 March 2023).
- Petroudi, S. Segmentation of the common carotid intima-media complex in ultrasound images using active contours. IEEE Trans. Biomed. Eng. 2012, 59, 3060–3069. [Google Scholar] [CrossRef] [PubMed]
- Nothlings, U.; Hoffmann, K.; Bergmann, M.M.; Boeing, H. Fitting portion sizes in a self-administered food frequency questionnaire. J. Nutr. 2007, 137, 2781–2786. [Google Scholar] [CrossRef] [PubMed]
- Hebestreit, K.; Yahiaoui-Doktor, M.; Engel, C.; Vetter, W.; Siniatchkin, M.; Erickson, N.; Halle, M.; Kiechle, M.; Bischoff, S.C. Validation of the German version of the Mediterranean Diet Adherence Screener (MEDAS) questionnaire. BMC Cancer 2017, 17, 341. [Google Scholar] [CrossRef] [PubMed]
- Folsom, A.R.; Parker, E.D.; Harnack, L.J. Degree of concordance with DASH diet guidelines and incidence of hypertension and fatal cardiovascular disease. Am. J. Hypertens. 2007, 20, 225–232. [Google Scholar] [CrossRef]
- van Buuren, S.; Groothuis-Oudshoorn, C. MICE: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- Li, K.; Kaaks, R.; Linseisen, J.; Rohrmann, S. Consistency of vitamin and/or mineral supplement use and demographic, lifestyle and health-status predictors: Findings from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Heidelberg cohort. Br. J. Nutr. 2010, 104, 1058–1064. [Google Scholar] [CrossRef]
- Oliván-Blázquez, B.; Aguilar-Latorre, A.; Motrico, E.; Gómez-Gómez, I.; Zabaleta-Del-Olmo, E.; Couso-Viana, S.; Clavería, A.; Maderuelo-Fernandez, J.A.; Recio-Rodríguez, J.I.; Moreno-Peral, P.; et al. The Relationship between Adherence to the Mediterranean Diet, Intake of Specific Foods and Depression in an Adult Population (45–75 Years) in Primary Health Care. A Cross-Sectional Descriptive Study. Nutrients 2021, 13, 2724. [Google Scholar] [CrossRef]
- Catalan, M.; Herreras, Z.; Pinyol, M.; Sala-Vila, A.; Amor, A.J.; de Groot, E.; Gilabert, R.; Ros, E.; Ortega, E. Prevalence by sex of preclinical carotid atherosclerosis in newly diagnosed type 2 diabetes. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 742–748. [Google Scholar] [CrossRef]
- de Kreutzenberg, S.V.; Coracina, A.; Volpi, A.; Fadini, G.P.; Frigo, A.C.; Guarneri, G.; Tiengo, A.; Avogaro, A. Microangiopathy is independently associated with presence, severity and composition of carotid atherosclerosis in type 2 diabetes. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Harari, F.; Barregard, L.; Östling, G.; Sallsten, G.; Hedblad, B.; Forsgard, N.; Borné, Y.; Fagerberg, B.; Engström, G. Blood Lead Levels and Risk of Atherosclerosis in the Carotid Artery: Results from a Swedish Cohort. Environ. Health Perspect. 2019, 127, 127002. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Engström, G.; Berglund, G.; Janzon, L.; Hedblad, B. Incidence of ischemic stroke in relation to asymptomatic carotid artery atherosclerosis in subjects with normal blood pressure. A prospective cohort study. Cereb. Dis. 2008, 26, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Rundek, T.; Arif, H.; Boden-Albala, B.; Elkind, M.S.; Paik, M.C.; Sacco, R.L. Carotid plaque, a subclinical precursor of vascular events: The Northern Manhattan Study. Neurology 2008, 70, 1200–1207. [Google Scholar] [CrossRef]
- Višković, K.; Rutherford, G.W.; Sudario, G.; Stemberger, L.; Brnić, Z.; Begovac, J. Ultrasound measurements of carotid intima-media thickness and plaque in HIV-infected patients on the Mediterranean diet. Croat. Med. J. 2013, 54, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Terschuren, C.; Damerau, L.; Petersen, E.L.; Harth, V.; Augustin, M.; Zyriax, B.C. Association of Dietary Pattern, Lifestyle and Chronotype with Metabolic Syndrome in Elderly-Lessons from the Population-Based Hamburg City Health Study. Int. J. Environ. Res. Public. Health 2021, 19, 377. [Google Scholar] [CrossRef]
- Spahl, L. Automatische Dichtebestimmung von Plaques in der Arteria carotis. In Projektpraktikumsbericht im Rahmen des Studienganges Medizinische Informatik der Universität zu Lübeck durchgeführt; Universitätsklinikum Hamburg-Eppendorf: Hamburg, Germany, 2019. [Google Scholar]

| Overall | Men | Women | p-Value | |
|---|---|---|---|---|
| n (%) | 2163 (100) | 1242 (57, 4) | 921 (42, 6) | |
| Age in years (median [IQR]) | 68 (62, 73) | 68 (62, 73) | 68 (62, 72) | 0.44 |
| SES index (median [IQR]) | 12.30 (9.97, 16.00) | 13.30 (10.30, 16.70) | 11.40 (9.40, 14.20) | <0.001 |
| NA | 1307 (60.4) | 653 (52.6) | 654 (71) | |
| BMI (kg/m2) (%) | <0.001 | |||
| NA | 130 (6.0) | 67 (5.4) | 63 (6.8) | |
| Normal weight (BMI 18.5–24.9 kg/m2) | 677 (31.3) | 322 (25.9) | 355 (38.5) | |
| Obesity (BMI ≥ 30 kg/m2) | 459 (21.2) | 272 (21.9) | 187 (20.3) | |
| Overweight (BMI 25–29.9 kg/m2) | 883 (40.8) | 576 (46.4) | 307 (33.3) | |
| Underweight (BMI < 18.5 kg/m2) | 14 (0.6) | 5 (0.4) | 9 (1.0) | |
| Smoking status (%) | 486 (22.5) | 282 (22.7) | 204 (22.1) | 0.697 |
| NA | 11 (0.5) | 5 (0.4) | 6 (0.7) | |
| Not performing any sports (%) | 646 (29.9) | 397 (32.0) | 249 (27.0) | 0.047 |
| NA | 180 (8.3) | 100 (8.1) | 80 (8.7) | |
| Total energy intake, kcal (median [IQR]) | 2009.48 (1613.75, 2564.23) | 2311.52 (1853.48, 2837.52) | 1729.92 (1419.01, 2101.23) | <0.001 |
| NA | 242 (11.2) | 141 (11.4) | 101 (11) | |
| MEDAS score (%) | <0.001 | |||
| NA | 244 (11.3) | 142 (11.4) | 102 (11.1) | |
| 0–3 points | 576 (26.6) | 453 (36.5) | 123 (13.4) | |
| 4 points | 439 (20.3) | 272 (21.9) | 167 (18.1) | |
| 5 points | 356 (16.5) | 175 (14.1) | 181 (19.7) | |
| 6+ points | 548 (25.3) | 200 (16.1) | 348 (37.8) | |
| DASH score (%) | <0.001 | |||
| NA | 244 (11.3) | 142 (11.4) | 102 (11.1) | |
| 0–3.5 points | 489 (22.6) | 395 (31.8) | 94 (10.2) | |
| 3.6–4.5 points | 643 (29.7) | 377 (30.4) | 266 (28.9) | |
| 4.6–5.0 points | 325 (15.0) | 152 (12.2) | 173 (18.8) | |
| 5.1+ points | 462 (21.4) | 176 (14.2) | 286 (31.1) | |
| Any supplement intake (%) | 755 (34.9) | 352 (28.3) | 403 (43.8) | <0.001 |
| NA | 177 (8.2) | 100 (8.1) | 77 (8.4) | |
| Multivitamins (%) | 167 (7.7) | 96 (7.7) | 71 (7.7) | 1 |
| Multiminerals (%) | 180 (8.3) | 78 (6.3) | 102 (11.1) | <0.001 |
| Calcium (%) | 127 (5.9) | 68 (5.5) | 59 (6.4) | 0.413 |
| Magnesium (%) | 382 (17.7) | 179 (14.4) | 203 (22.0) | <0.001 |
| Vitamin B (%) | 110 (5.1) | 45 (3.6) | 65 (7.1) | <0.001 |
| Folate (%) | 76 (3.5) | 30 (2.4) | 46 (5.0) | 0.002 |
| Hyperlipidemia (%) | 744 (34.4) | 498 (40.1) | 246 (26.7) | <0.001 |
| NA | 100 (4.6) | 53 (4.3) | 47 (5.1) | |
| Arterial hypertension (%) | 1644 (76.0) | 974 (78.4) | 670 (72.7) | <0.001 |
| NA | 62 (2.9) | 44 (3.5) | 18 (2.0) | |
| Diabetes mellitus (%) | 256 (11.8) | 171 (13.8) | 85 (9.2) | 0.002 |
| NA | 118 (5.5) | 59 (4.8) | 59 (6.4) | |
| Prior MI (%) | 119 (5.5) | 103 (8.3) | 16 (1.7) | <0.001 |
| NA | 17 (0.8) | 10 (0.8) | 7 (0.8) | |
| Heart failure (%) | 174 (8.0) | 115 (9.3) | 59 (6.4) | 0.014 |
| NA | 20 (0.9) | 15 (1.2) | 5 (0.5) | |
| Atrial fibrillation (%) | 183 (8.5) | 120 (9.7) | 63 (6.8) | 0.014 |
| NA | 199 (9.2) | 101 (8.1) | 98 (10.6) | |
| Prior stroke (%) | 100 (4.6) | 65 (5.2) | 35 (3.8) | 0.121 |
| NA | 17 (0.8) | 7 (0.6) | 10 (1.1) | |
| PAD (ABI < 0.9) (%) | 255 (11.8) | 140 (11.3) | 115 (12.5) | 0.308 |
| NA | 1140 (52.7) | 645 (51.9) | 495 (53.7) | |
| GFR (median [IQR]) | 87.20 (78.40, 93.20) | 88.90 (81.20, 94.60) | 84.80 (76.30, 90.30) | <0.001 |
| NA | 211 (9.8) | 105 (8.5) | 106 (11.5) | |
| Lipid-lowering drugs (%) | 617 (28.5) | 413 (33.3) | 204 (22.1) | <0.001 |
| NA | 60 (2.8) | 39 (3.1) | 21 (2.3) | |
| Antihypertensives (%) | 1000 (46.2) | 598 (48.1) | 402 (43.6) | 0.035 |
| NA | 60 (2.8) | 39 (3.1) | 21 (2.3) | |
| Antidiabetics (%) | 171 (7.9) | 119 (9.6) | 52 (5.6) | 0.001 |
| NA | 60 (2.8) | 39 (3.1) | 21 (2.3) | |
| Antiplatelets (%) | 600 (27.7) | 409 (32.9) | 191 (20.7) | <0.001 |
| NA | 60 (2.8) | 39 (3.1) | 21 (2.3) |
| Model Parameters | Men | Women | ||
|---|---|---|---|---|
| GSM [95% CI] 1 | p-Value | GSM [95% CI] 1 | p-Value | |
| MEDAS 4 points 2 | −0.14 (−3.06, 2.79) | 0.927 | −2.82 (−7.78, 2.15) | 0.267 |
| MEDAS 5 points 2 | −1.10 (−4.45, 2.25) | 0.521 | −2.02 (−6.78, 2.74) | 0.406 |
| MEDAS 6+ points 2 | −1.53 (−4.71, 1.66) | 0.347 | −1.88 (−6.19, 2.43) | 0.393 |
| DASH 3.6–4.5 points 3 | −1.27 (−4.09, 1.55) | 0.378 | −1.69 (−6.57, 3.19) | 0.497 |
| DASH 4.6–5.0 points 3 | −0.95 (−4.66, 2.75) | 0.614 | −3.76 (−9.06, 1.53) | 0.164 |
| DASH 5.1+ points 3 | −1.45 (−4.86, 1.96) | 0.406 | −0.33 (−5.22, 4.57) | 0.896 |
| Any supplement intake 4 | −0.69 (−4.12, 2.74) | 0.693 | −1.06 (−4.78, 2.67) | 0.578 |
| Multivitamins 4 | −2.67 (−7.94, 2.61) | 0.322 | −2.03 (−8.53, 4.47) | 0.540 |
| Multiminerals 4 | 1.52 (−4.11, 7.15) | 0.597 | −0.87 (−6.53, 4.79) | 0.763 |
| Calcium 4 | −0.14 (−5.57, 5.29) | 0.960 | 2.57 (−3.61, 8.76) | 0.415 |
| Magnesium 4 | −0.01 (−4.20, 4.18) | 0.995 | −0.19 (−4.43, 4.05) | 0.930 |
| Vitamin B 4 | −2.19 (−8.59, 4.21) | 0.502 | 3.93 (−1.93, 9.79) | 0.189 |
| Folate 4 | 9.12 (1.37, 16.86) | 0.021 | −2.50 (−9.31, 4.31) | 0.472 |
| Characteristics | OR (95% CI) | p-Value |
|---|---|---|
| High MEDAS vs. medium MEDAS | 1.07 (0.92, 1.24) | 0.367 |
| Low MEDAS vs. medium MEDAS | 0.86 (0.75, 1.00) | 0.052 |
| High DASH vs. medium DASH | 1.18 (1.02, 1.36) | 0.027 |
| Low DASH vs. medium DASH | 0.95 (0.82, 1.10) | 0.469 |
| Supplement intake yes vs. no | 0.96 (0.85, 1.08) | 0.490 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Assies, J.M.; Sältz, M.D.; Peters, F.; Behrendt, C.-A.; Jagodzinski, A.; Petersen, E.L.; Schäfer, I.; Twerenbold, R.; Blankenberg, S.; Rimmele, D.L.; et al. Cross-Sectional Association of Dietary Patterns and Supplement Intake with Presence and Gray-Scale Median of Carotid Plaques—A Comparison between Women and Men in the Population-Based Hamburg City Health Study. Nutrients 2023, 15, 1468. https://doi.org/10.3390/nu15061468
Assies JM, Sältz MD, Peters F, Behrendt C-A, Jagodzinski A, Petersen EL, Schäfer I, Twerenbold R, Blankenberg S, Rimmele DL, et al. Cross-Sectional Association of Dietary Patterns and Supplement Intake with Presence and Gray-Scale Median of Carotid Plaques—A Comparison between Women and Men in the Population-Based Hamburg City Health Study. Nutrients. 2023; 15(6):1468. https://doi.org/10.3390/nu15061468
Chicago/Turabian StyleAssies, Julia Maria, Martje Dorothea Sältz, Frederik Peters, Christian-Alexander Behrendt, Annika Jagodzinski, Elina Larissa Petersen, Ines Schäfer, Raphael Twerenbold, Stefan Blankenberg, David Leander Rimmele, and et al. 2023. "Cross-Sectional Association of Dietary Patterns and Supplement Intake with Presence and Gray-Scale Median of Carotid Plaques—A Comparison between Women and Men in the Population-Based Hamburg City Health Study" Nutrients 15, no. 6: 1468. https://doi.org/10.3390/nu15061468
APA StyleAssies, J. M., Sältz, M. D., Peters, F., Behrendt, C.-A., Jagodzinski, A., Petersen, E. L., Schäfer, I., Twerenbold, R., Blankenberg, S., Rimmele, D. L., Thomalla, G., Makarova, N., & Zyriax, B.-C. (2023). Cross-Sectional Association of Dietary Patterns and Supplement Intake with Presence and Gray-Scale Median of Carotid Plaques—A Comparison between Women and Men in the Population-Based Hamburg City Health Study. Nutrients, 15(6), 1468. https://doi.org/10.3390/nu15061468










