Diet Quality, Microbial Lignan Metabolites, and Cardiometabolic Health among US Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Urinary Enterolignans
2.3. The Healthy Eating Index
2.4. Cardiometabolic Health
2.5. Demographic and Lifestyle Covariates
2.6. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Generalized Additive Model Exploration
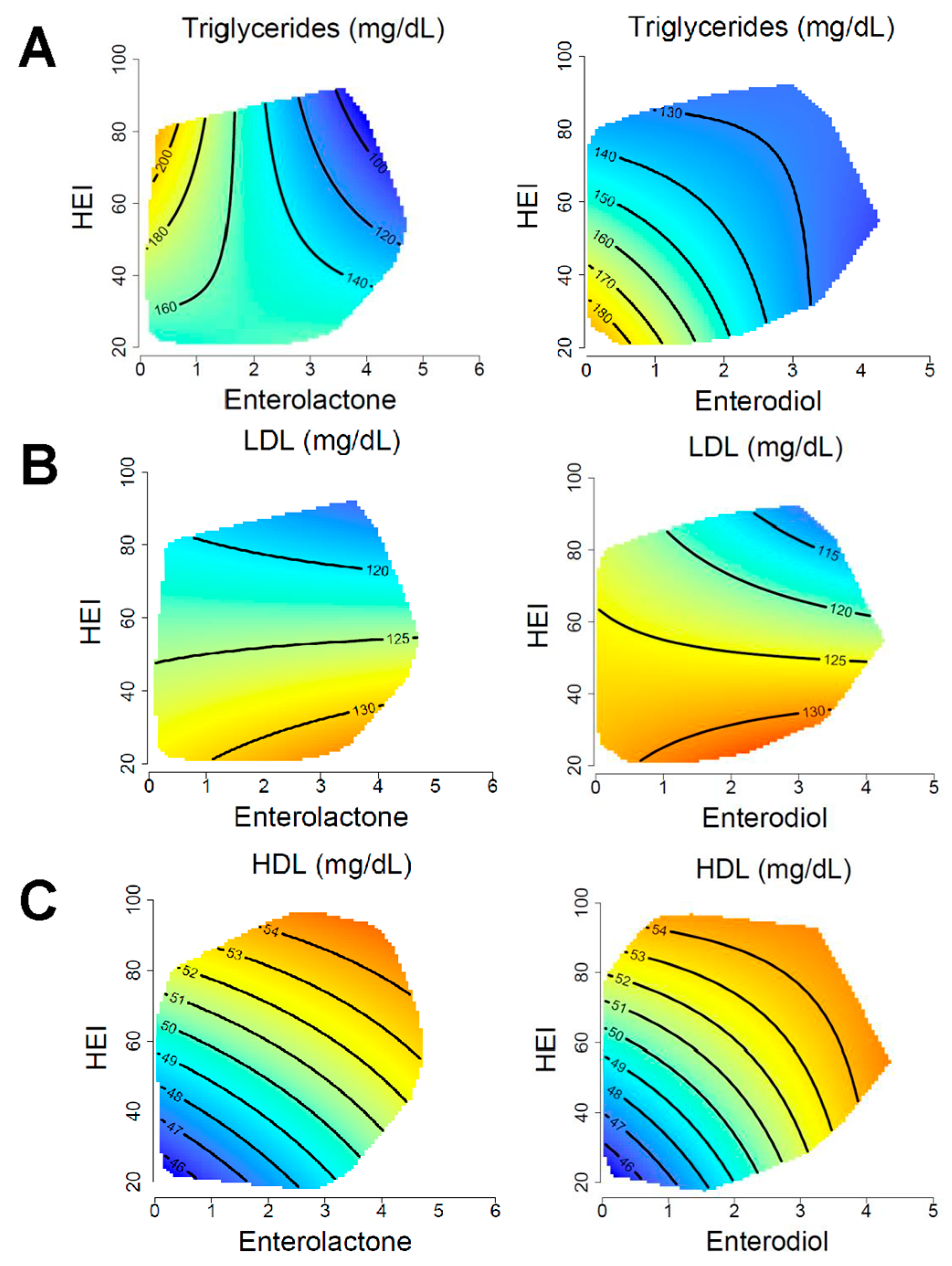
3.3. Blood Lipids
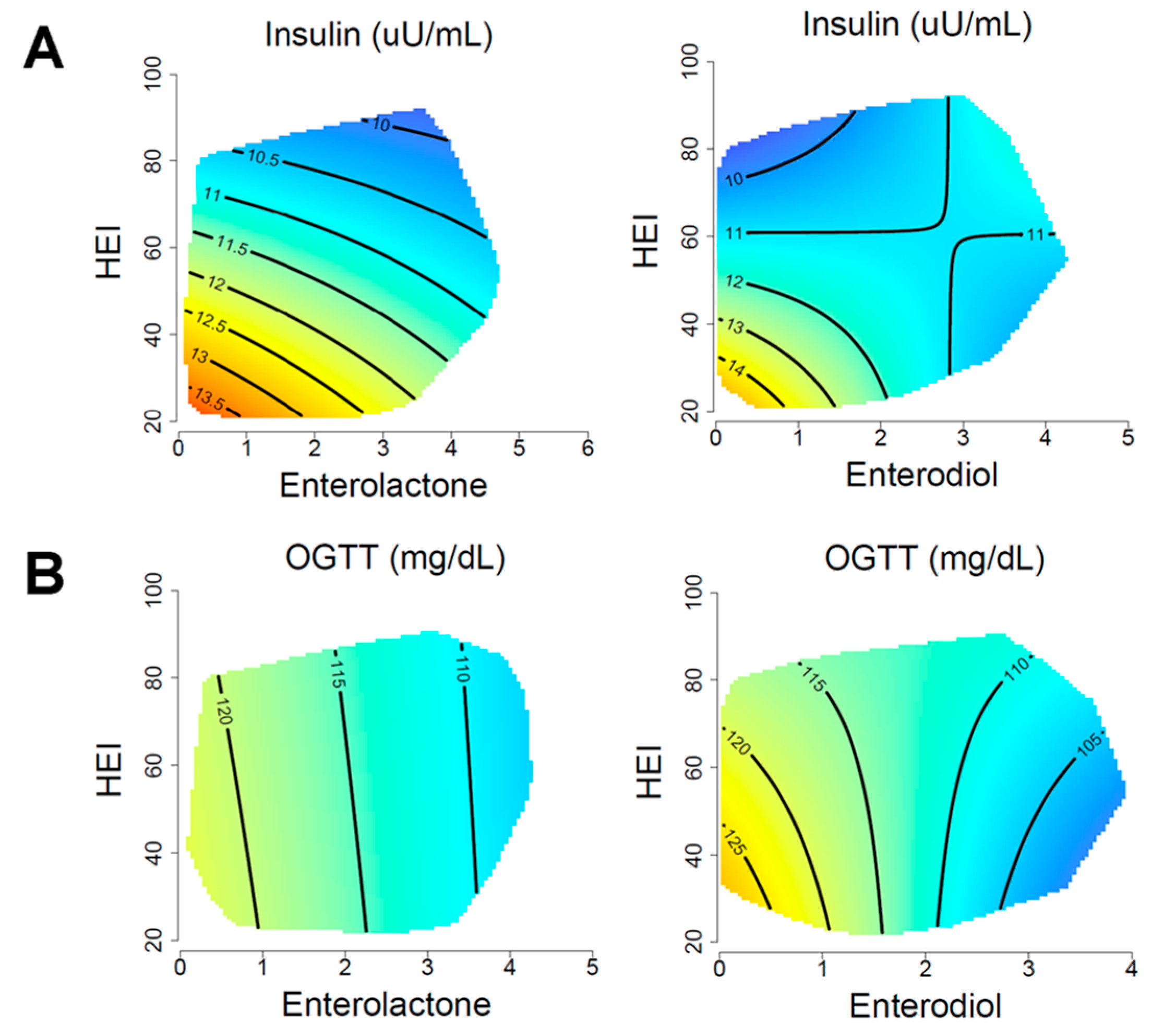
3.4. Glycemic Control
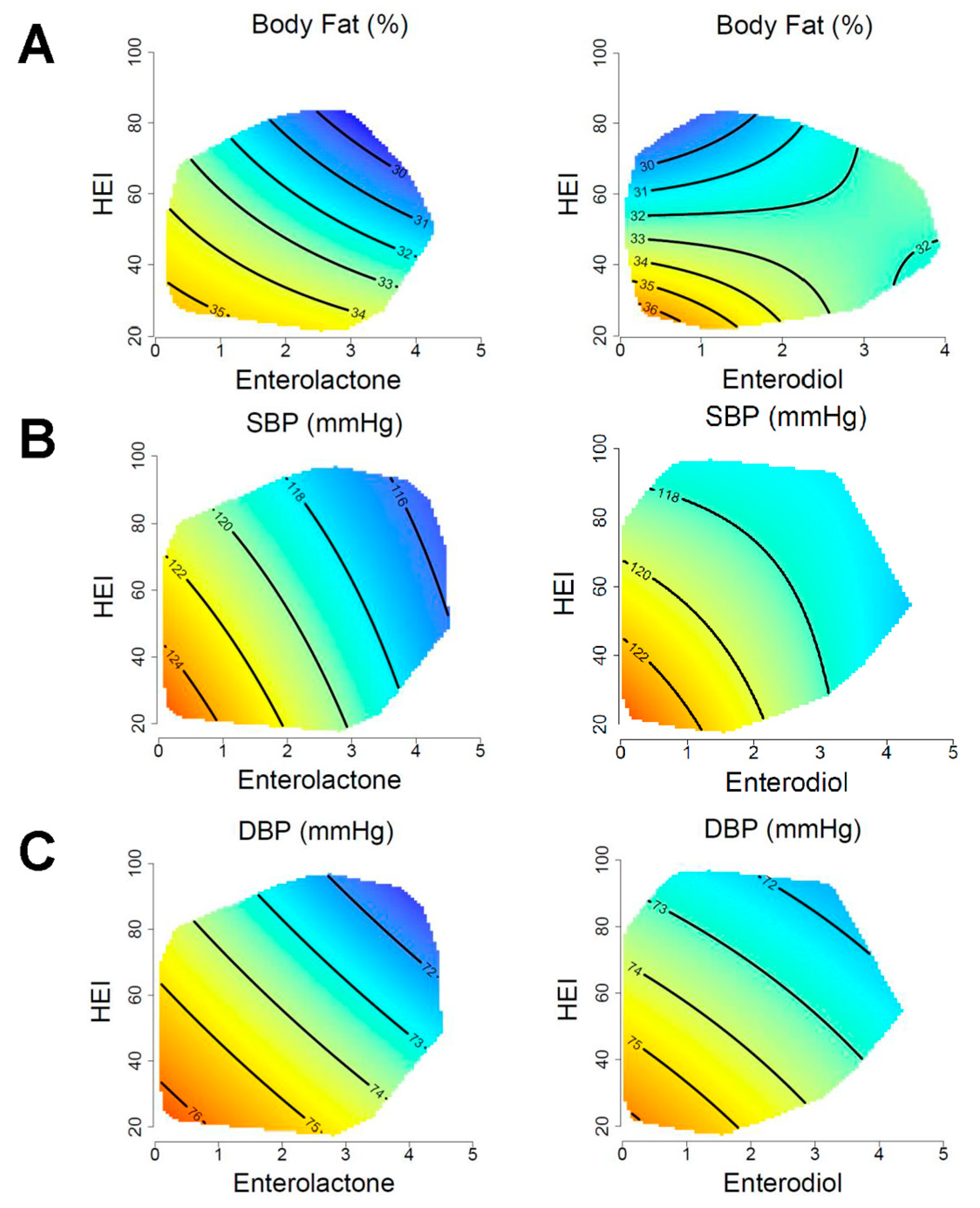
3.5. Adiposity and Blood Pressure
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- Reed, J.; Bain, S.; Kanamarlapudi, V. A Review of Current Trends with Type 2 Diabetes Epidemiology, Aetiology, Pathogenesis, Treatments and Future Perspectives. Diabetes Metab. Syndr. Obes. 2021, 14, 3567–3602. [Google Scholar] [CrossRef] [PubMed]
- [CDC], Centers for Disease Control and Prevention. Underlying Cause of Death 1999–2018; National Center for Health Statistics: Hyattsville, MD, USA, 2020.
- Mozaffarian, D.; Appel, L.J.; Horn, L.V. Components of a Cardioprotective Diet. Circulation 2011, 123, 2870–2891. [Google Scholar] [CrossRef] [PubMed]
- AlEssa, H.B.; Malik, V.S.; Yuan, C.; Willett, W.C.; Huang, T.; Hu, F.B.; Tobias, D.K. Dietary patterns and cardiometabolic and endocrine plasma biomarkers in US women. Am. J. Clin. Nutr. 2017, 105, 432–441. [Google Scholar] [CrossRef] [PubMed]
- McNaughton, S.A.; Dunstan, D.W.; Ball, K.; Shaw, J.; Crawford, D. Dietary quality is associated with diabetes and cardio-metabolic risk factors. J. Nutr. 2009, 139, 734–742. [Google Scholar] [CrossRef] [PubMed]
- Valdes, A.M.; Walter, J.; Segal, E.; Spector, T.D. Role of the gut microbiota in nutrition and health. BMJ 2018, 361, k2179. [Google Scholar] [CrossRef]
- Flint, H.J.; Scott, K.P.; Louis, P.; Duncan, S.H. The role of the gut microbiota in nutrition and health. Nat. Rev. Gastroenterol. Hepatol. 2012, 9, 577–589. [Google Scholar] [CrossRef]
- Ren, Z.; Pan, L.L.; Huang, Y.; Chen, H.; Liu, Y.; Liu, H.; Tu, X.; Liu, Y.; Li, B.; Dong, X.; et al. Gut microbiota-CRAMP axis shapes intestinal barrier function and immune responses in dietary gluten-induced enteropathy. EMBO Mol. Med. 2021, 13, e14059. [Google Scholar] [CrossRef]
- Purchiaroni, F.; Tortora, A.; Gabrielli, M.; Bertucci, F.; Gigante, G.; Ianiro, G.; Ojetti, V.; Scarpellini, E.; Gasbarrini, A. The role of intestinal microbiota and the immune system. Eur. Rev. Med. Pharmacol. Sci. 2013, 17, 323–333. [Google Scholar]
- Jumpertz, R.; Le, D.S.; Turnbaugh, P.J.; Trinidad, C.; Bogardus, C.; Gordon, J.I.; Krakoff, J. Energy-balance studies reveal associations between gut microbes, caloric load, and nutrient absorption in humans. Am. J. Clin. Nutr. 2011, 94, 58–65. [Google Scholar] [CrossRef]
- McLoughlin, R.F.; Berthon, B.S.; Jensen, M.E.; Baines, K.J.; Wood, L.G. Short-chain fatty acids, prebiotics, synbiotics, and systemic inflammation: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2017, 106, 930–945. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.D.; Nguyen, L.H.; Li, Y.; Yan, Y.; Ma, W.; Rinott, E.; Ivey, K.L.; Shai, I.; Willett, W.C.; Hu, F.B.; et al. The gut microbiome modulates the protective association between a Mediterranean diet and cardiometabolic disease risk. Nat. Med. 2021, 27, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.D.; Qi, Q.; Wang, Z.; Usyk, M.; Sotres-Alvarez, D.; Mattei, J.; Tamez, M.; Gellman, M.D.; Daviglus, M.; Hu, F.B.; et al. The Gut Microbiome Modifies the Association between a Mediterranean Diet and Diabetes in USA Hispanic/Latino Population. J. Clin. Endocrinol. Metab. 2022, 107, e924–e934. [Google Scholar] [CrossRef]
- Shivappa, N.; Wirth, M.D.; Murphy, E.A.; Hurley, T.G.; Hébert, J.R. Association between the Dietary Inflammatory Index (DII) and urinary enterolignans and C-reactive protein from the National Health and Nutrition Examination Survey-2003–2008. Eur. J. Nutr. 2019, 58, 797–805. [Google Scholar] [CrossRef]
- Liggins, J.; Grimwood, R.; Bingham, S.A. Extraction and quantification of lignan phytoestrogens in food and human samples. Anal. Biochem. 2000, 287, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Zinöcker, M.K.; Lindseth, I.A. The Western Diet–Microbiome-Host Interaction and Its Role in Metabolic Disease. Nutrients 2018, 10, 365. [Google Scholar] [CrossRef]
- Cuevas-Sierra, A.; Milagro, F.I.; Aranaz, P.; Martínez, J.A.; Riezu-Boj, J.I. Gut Microbiota Differences According to Ultra-Processed Food Consumption in a Spanish Population. Nutrients 2021, 13, 2710. [Google Scholar] [CrossRef]
- Senghor, B.; Sokhna, C.; Ruimy, R.; Lagier, J.-C. Gut microbiota diversity according to dietary habits and geographical provenance. Hum. Microbiome J. 2018, 7, 1–9. [Google Scholar] [CrossRef]
- Martínez Steele, E.; Monteiro, C.A. Association between Dietary Share of Ultra-Processed Foods and Urinary Concentrations of Phytoestrogens in the US. Nutrients 2017, 9, 209. [Google Scholar] [CrossRef]
- Simpson, S.J.; Le Couteur, D.G.; Raubenheimer, D.; Solon-Biet, S.M.; Cooney, G.J.; Cogger, V.C.; Fontana, L. Dietary protein, aging and nutritional geometry. Ageing Res. Rev. 2017, 39, 78–86. [Google Scholar] [CrossRef]
- Koemel, N.A.; Senior, A.M.; Dissanayake, H.U.; Ross, J.; McMullan, R.L.; Kong, Y.; Phang, M.; Hyett, J.; Raubenheimer, D.; Gordon, A. Maternal dietary fatty acid composition and newborn epigenetic aging—A geometric framework approach. Am. J. Clin. Nutr. 2022, 115, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Koemel, N.A.; Senior, A.M.; Celermajer, D.S.; Grech, A.; Gill, T.P.; Simpson, S.J.; Raubenheimer, D.; Skilton, M.R. Multi-Nutrient Analysis of Dietary Macronutrients with All-Cause, Cardiovascular, and Cancer Mortality: Data from NHANES 1999–2014. Nutrients 2023, 15, 345. [Google Scholar] [CrossRef]
- Adlercreutz, H. Lignans and human health. Crit. Rev. Clin. Lab. Sci. 2007, 44, 483–525. [Google Scholar] [CrossRef] [PubMed]
- Frankenfeld, C.L. Cardiometabolic Risk Factors Are Associated with High Urinary Enterolactone Concentration, Independent of Urinary Enterodiol Concentration and Dietary Fiber Intake in Adults. J. Nutr. 2014, 144, 1445–1453. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick, S.I.; Reedy, J.; Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Wilson, M.M.; Lerman, J.L.; Tooze, J.A. Applications of the Healthy Eating Index for Surveillance, Epidemiology, and Intervention Research: Considerations and Caveats. J. Acad. Nutr. Diet. 2018, 118, 1603–1621. [Google Scholar] [CrossRef]
- Hastie, T.; Tibshirani, R. Generalized Additive Models. Stat. Sci. 1986, 1, 297–310. [Google Scholar] [CrossRef]
- Willett, W.C.; Howe, G.R.; Kushi, L.H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 1997, 65, 1220S–1228S, Discussion 1229S–1231S. [Google Scholar] [CrossRef]
- Wood, S. mgcv: Mixed GAM Computation Vehicle with GCV/AIC/REML Smoothness Estimation; Engineering and Physical Sciences Research Council: Swindon, UK, 2012. [Google Scholar]
- Wood, S.N. Generalized Additive Models: An. Introduction with R; CRC Press: Boca Raton, FL, USA, 2017. [Google Scholar]
- Akaike, H.; Petrov, B.N.; Csaki, F. Second International Symposium on Information Theory; Akademia Kiado: Budapest, Hungary, 1973. [Google Scholar]
- Juul, F.; Vaidean, G.; Parekh, N. Ultra-processed foods and cardiovascular diseases: Potential mechanisms of action. Adv. Nutr. 2021, 12, 1673–1680. [Google Scholar] [CrossRef]
- Lichtenstein, A.H.; Appel, L.J.; Vadiveloo, M.; Hu, F.B.; Kris-Etherton, P.M.; Rebholz, C.M.; Sacks, F.M.; Thorndike, A.N.; Van Horn, L.; Wylie-Rosett, J. 2021 dietary guidance to improve cardiovascular health: A scientific statement from the American Heart Association. Circulation 2021, 144, e472–e487. [Google Scholar] [CrossRef]
- Shah, B.S.; Freeland-Graves, J.H.; Cahill, J.M.; Lu, H.; Graves, G.R. Diet quality as measured by the healthy eating index and the association with lipid profile in low-income women in early postpartum. J. Am. Diet. Assoc. 2010, 110, 274–279. [Google Scholar] [CrossRef]
- Pasdar, Y.; Hamzeh, B.; Moradi, S.; Mohammadi, E.; Cheshmeh, S.; Darbandi, M.; Faramani, R.S.; Najafi, F. Healthy eating index 2015 and major dietary patterns in relation to incident hypertension; a prospective cohort study. BMC Public Health 2022, 22, 734. [Google Scholar] [CrossRef] [PubMed]
- Morze, J.; Danielewicz, A.; Hoffmann, G.; Schwingshackl, L. Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: A Second Update of a Systematic Review and Meta-Analysis of Cohort Studies. J. Acad. Nutr. Diet. 2020, 120, 1998–2031.e1915. [Google Scholar] [CrossRef] [PubMed]
- Hansen, T.H.; Gøbel, R.J.; Hansen, T.; Pedersen, O. The gut microbiome in cardio-metabolic health. Genome Med. 2015, 7, 33. [Google Scholar] [CrossRef]
- Turnbaugh, P.J.; Ley, R.E.; Mahowald, M.A.; Magrini, V.; Mardis, E.R.; Gordon, J.I. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 2006, 444, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Nakaya, K.; Ikewaki, K. Microbiota and HDL metabolism. Curr. Opin. Lipidol. 2018, 29, 18–23. [Google Scholar] [CrossRef]
- Matey-Hernandez, M.L.; Williams, F.M.K.; Potter, T.; Valdes, A.M.; Spector, T.D.; Menni, C. Genetic and microbiome influence on lipid metabolism and dyslipidemia. Physiol. Genom. 2018, 50, 117–126. [Google Scholar] [CrossRef]
- Kazemian, N.; Mahmoudi, M.; Halperin, F.; Wu, J.C.; Pakpour, S. Gut microbiota and cardiovascular disease: Opportunities and challenges. Microbiome 2020, 8, 36. [Google Scholar] [CrossRef] [PubMed]
- Kitts, D.D.; Yuan, Y.V.; Wijewickreme, A.N.; Thompson, L.U. Antioxidant activity of the flaxseed lignan secoisolariciresinol diglycoside and its mammalian lignan metabolites enterodiol and enterolactone. Mol. Cell. Biochem. 1999, 202, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Owen, A.J.; Roach, P.D.; Abbey, M. Regulation of low-density lipoprotein receptor activity by estrogens and phytoestrogens in a HepG2 cell model. Ann. Nutr. Metab. 2004, 48, 269–275. [Google Scholar] [CrossRef]
- Hall, A.V.; Parbtani, A.; Clark, W.F.; Spanner, E.; Keeney, M.; Chin-Yee, I.; Philbrick, D.J.; Holub, B.J. Abrogation of MRL/lpr lupus nephritis by dietary flaxseed. Am. J. Kidney Dis. 1993, 22, 326–332. [Google Scholar] [CrossRef]
- Asnicar, F.; Berry, S.E.; Valdes, A.M.; Nguyen, L.H.; Piccinno, G.; Drew, D.A.; Leeming, E.; Gibson, R.; Le Roy, C.; Khatib, H.A.; et al. Microbiome connections with host metabolism and habitual diet from 1,098 deeply phenotyped individuals. Nat. Med. 2021, 27, 321–332. [Google Scholar] [CrossRef]
- Li, Y.; Wang, F.; Li, J.; Ivey, K.L.; Wilkinson, J.E.; Wang, D.D.; Li, R.; Liu, G.; Eliassen, H.A.; Chan, A.T.; et al. Dietary lignans, plasma enterolactone levels, and metabolic risk in men: Exploring the role of the gut microbiome. BMC Microbiol. 2022, 22, 82. [Google Scholar] [CrossRef]
- Makki, K.; Deehan, E.C.; Walter, J.; Backhed, F. The Impact of Dietary Fiber on Gut Microbiota in Host Health and Disease. Cell Host Microbe 2018, 23, 705–715. [Google Scholar] [CrossRef]
- Townsend, G.E., II.; Han, W.; Schwalm, N.D., III.; Raghavan, V.; Barry, N.A.; Goodman, A.L.; Groisman, E.A. Dietary sugar silences a colonization factor in a mammalian gut symbiont. Proc. Natl. Acad. Sci. USA 2019, 116, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Regitz-Zagrosek, V.; Kararigas, G. Mechanistic Pathways of Sex Differences in Cardiovascular Disease. Physiol. Rev. 2017, 97, 1–37. [Google Scholar] [CrossRef]
- Razavi, A.C.; Potts, K.S.; Kelly, T.N.; Bazzano, L.A. Sex, gut microbiome, and cardiovascular disease risk. Biol. Sex Differ. 2019, 10, 29. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Kararigas, G. Role of Biological Sex in the Cardiovascular-Gut Microbiome Axis. Front. Cardiovasc. Med. 2022, 8, 759735. [Google Scholar] [CrossRef]
- Korn, E.L.; Graubard, B.I. Epidemiologic studies utilizing surveys: Accounting for the sampling design. Am. J. Public Health 1991, 81, 1166–1173. [Google Scholar] [CrossRef] [PubMed]
| Participant Characteristics | Mean | SD |
|---|---|---|
| Age (years) | 43.6 | 16.5 |
| Female sex (%) | 50.4 | − |
| BMI (kg/m2) | 28.5 | 6.5 |
| Total Energy (kcal) | 2101 | 737 |
| Healthy Eating Index Score | 50.9 | 12.1 |
| Enterolactone μmol/L (log-transformed) | 2.54 | 0.75 |
| Enterodiol μmol/L (log-transformed) | 1.59 | 0.64 |
| Protein (TEI%) | 15.0 | 3.4 |
| Carbohydrate (TEI%) | 51.5 | 7.7 |
| Fat (TEI%) | 33.4 | 6.6 |
| Fiber (g) | 15.6 | 7.8 |
| Sugar (g) | 78.0 | 7.5 |
| Sodium (mg) | 2125 | 1256.4 |
| Race/Ethnicity | ||
| Hispanic (%) | 30.3 | − |
| Non-Hispanic White (%) | 46.6 | − |
| Non-Hispanic Black (%) | 19.0 | − |
| Other (%) | 4.1 | − |
| Family Income to Poverty Ratio | 2.54 | |
| Education Level | ||
| Less than high school (%) | 28.1 | − |
| High school graduate or GED (%) | 23.2 | − |
| Some College or More (%) | 48.7 | − |
| Nondrinker (%) | 24.6 | − |
| Nonsmoker (%) | 49.5 | − |
| Physical Activity (METs) | 1811 | 2363 |
| Lipid Profile | ||
| Triglycerides (mg/dL) | 135.3 | 113.3 |
| Total Cholesterol (mg/dL) | 200.3 | 40.7 |
| LDL Cholesterol (mg/dL) | 120.2 | 34.3 |
| HDL Cholesterol (mg/dL) | 52.2 | 15.7 |
| Glycemic Control | ||
| Glucose (mg/dL) | 99.2 | 21.6 |
| Insulin (uU/mL) | 12.1 | 9.7 |
| OGTT (mg/dL) | 114.8 | 50.9 |
| HbA1c (%) | 5.43 | 0.67 |
| Adiposity and Blood Pressure | ||
| Body Fat (%) | 31.9 | 10.71 |
| Systolic Blood Pressure (mmHg) | 121.3 | 17.6 |
| Diastolic Blood Pressure (mmHg) | 70.9 | 11.4 |
| Model 1 | Model 2 | Model 3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Metabolite | DE | AIC | p | DE | AIC | p | DE | AIC | p |
| Triglycerides | Enterodiol | 10.1% | 25,710.0 | <0.001 | 12.5% | 25,666.9 | 0.002 | 18.2% | 25,536.0 | 0.002 |
| Enterolactone | 10.8% | 25,684.1 | <0.001 | 13.6% | 25,624.2 | <0.001 | 19.1% | 25,489.3 | <0.001 | |
| Total Cholesterol | Enterodiol | 11.9% | 40,395.2 | 0.31 | 12.0% | 40,397.7 | 0.29 | 14.0% | 40,319.9 | 0.43 |
| Enterolactone | 12.0% | 40,394.7 | 0.27 | 14.0% | 40,319.9 | 0.43 | 14.0% | 40,318.2 | 0.31 | |
| LDL Cholesterol | Enterodiol | 10.5% | 21,114.5 | 0.007 | 10.5% | 21,118.0 | 0.006 | 13.3% | 21,068.4 | 0.01 |
| Enterolactone | 10.4% | 21,116.9 | 0.02 | 10.4% | 21,120.2 | 0.01 | 13.2% | 21,071.1 | 0.04 | |
| HDL Cholesterol | Enterodiol | 13.8% | 36,135.9 | <0.001 | 15.3% | 36,048.6 | <0.001 | 26.0% | 35,463.1 | <0.001 |
| Enterolactone | 13.9% | 36,130.5 | <0.001 | 15.3% | 36,057.7 | <0.001 | 25.9% | 35,466.2 | <0.001 | |
| Glucose | Enterodiol | 12.7% | 19,190.4 | 0.046 | 13.6% | 19,166.9 | 0.12 | 17.0% | 19,089.1 | 0.24 |
| Enterolactone | 12.4% | 19,201.6 | 0.13 | 13.4% | 19,175.7 | 0.25 | 16.8% | 19,097.3 | 0.47 | |
| Insulin | Enterodiol | 2.8% | 15,052.2 | <0.001 | 3.6% | 15,049.0 | <0.001 | 36.1% | 14,016.4 | 0.02 |
| Enterolactone | 3.8% | 15,030.0 | <0.001 | 4.6% | 15,029.6 | <0.001 | 36.3% | 14,014.4 | 0.002 | |
| OGTT | Enterodiol | 16.3% | 10,335.4 | 0.03 | 17.4% | 10,324.7 | 0.04 | 23.2% | 10,263.5 | 0.03 |
| Enterolactone | 16.2% | 10,342.1 | 0.046 | 17.2% | 10,331.1 | 0.07 | 22.9% | 10,272.9 | 0.08 | |
| HbA1c | Enterodiol | 10.3% | 4879.4 | 0.38 | 11.2% | 4851.0 | 0.51 | 15.9% | 4700.1 | 0.28 |
| Enterolactone | 10.5% | 4869.2 | 0.11 | 11.4% | 4841.9 | 0.19 | 15.6% | 4713.7 | 0.92 | |
| Body Fat (%) | Enterodiol | 43.9% | 7948.2 | 0.03 | 43.8% | 7950.7 | 0.02 | 44.6% | 7940.3 | 0.02 |
| Enterolactone | 44.0% | 7946.0 | 0.01 | 43.9% | 7948.3 | 0.007 | 44.7% | 7938.1 | 0.007 | |
| Systolic Blood Pressure | Enterodiol | 29.4% | 36,898.7 | <0.001 | 29.6% | 36,889.1 | <0.001 | 31.8% | 36,767.0 | <0.001 |
| Enterolactone | 29.9% | 36,867.8 | <0.001 | 30.1% | 36,859.8 | <0.001 | 32.1% | 36,745.7 | <0.001 | |
| Diastolic Blood Pressure | Enterodiol | 11.8% | 34,721.3 | <0.001 | 12.3% | 34,701.3 | <0.001 | 13.3% | 34,653.8 | 0.005 |
| Enterolactone | 11.8% | 34,718.8 | <0.001 | 12.3% | 34,701.2 | <0.001 | 13.3% | 34,655.6 | 0.007 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koemel, N.A.; Senior, A.M.; Benmarhnia, T.; Holmes, A.; Okada, M.; Oulhote, Y.; Parker, H.M.; Shah, S.; Simpson, S.J.; Raubenheimer, D.; et al. Diet Quality, Microbial Lignan Metabolites, and Cardiometabolic Health among US Adults. Nutrients 2023, 15, 1412. https://doi.org/10.3390/nu15061412
Koemel NA, Senior AM, Benmarhnia T, Holmes A, Okada M, Oulhote Y, Parker HM, Shah S, Simpson SJ, Raubenheimer D, et al. Diet Quality, Microbial Lignan Metabolites, and Cardiometabolic Health among US Adults. Nutrients. 2023; 15(6):1412. https://doi.org/10.3390/nu15061412
Chicago/Turabian StyleKoemel, Nicholas A., Alistair M. Senior, Tarik Benmarhnia, Andrew Holmes, Mirei Okada, Youssef Oulhote, Helen M. Parker, Sanam Shah, Stephen J. Simpson, David Raubenheimer, and et al. 2023. "Diet Quality, Microbial Lignan Metabolites, and Cardiometabolic Health among US Adults" Nutrients 15, no. 6: 1412. https://doi.org/10.3390/nu15061412
APA StyleKoemel, N. A., Senior, A. M., Benmarhnia, T., Holmes, A., Okada, M., Oulhote, Y., Parker, H. M., Shah, S., Simpson, S. J., Raubenheimer, D., Gill, T. P., Laouali, N., & Skilton, M. R. (2023). Diet Quality, Microbial Lignan Metabolites, and Cardiometabolic Health among US Adults. Nutrients, 15(6), 1412. https://doi.org/10.3390/nu15061412