Abstract
Food insecurity refers to the uncertain availability of or limited access to nutritious food. Poor diets prevalent among food insecure populations may incite an inflammatory state and subsequently negatively affect skeletal muscle metabolism. To examine the inflammatory mechanistic potential of the association between food insecurity and the risk of low muscle strength, we analyzed cross-sectional data from 8624 adults aged ≥20 years from the Korean National Health and Nutrition Examination Survey 2014–2015. Household food security status was assessed using an 18-item food security survey module. The inflammatory potential of diets was estimated by the dietary inflammation index (DII). Low muscle strength was ascertained using hand grip strength. In the multivariable-adjusted model, greater food insecurity was significantly associated with a higher DII score and risk of low muscle strength. The multivariable-adjusted mean difference (95% confidence interval) on the DII, comparing the “moderate-to-severe” food insecurity group with the “food secure” group, was 0.43 (0.06–0.80) (P-trend: <0.001) and the odds ratio (95% confidence intervals) of low muscle strength for the same comparison groups was 2.06 (1.07–3.96) (P-trend: 0.005). Our results suggest that individuals with greater food insecurity may be susceptible to diets with greater inflammatory potential, which may contribute to a loss of muscle strength.
1. Introduction
Skeletal muscle is an integral body tissue that plays a pivotal role in physical strength, physical performance, and metabolic regulation [1]. Muscle strength is an indicator of muscle function and is increasingly seen as a robust predictor of a range of health outcomes [2,3,4,5]. For instance, hand grip strength (HGS), a simple and reliable measurement of muscle strength [6,7], has been inversely associated with the risk of physical disability, respiratory disease, cancers, cardiovascular diseases, and all-cause and cardiovascular mortality [2,8]. The onset of loss of muscle mass and muscle strength begins in the early 30s and accelerates with aging, being observed to disproportionally affect individuals of low socioeconomic status [9,10].
Food insecurity refers to a lack of consistent access to sufficient, safe, and nutritious food for an active, healthy life and is associated with poor nutritional status [11] and unfavorable health outcomes, including obesity, metabolic syndrome, and diabetes [12]. According to the United Nations, nearly 2.3 billion people, accounting for 29.3% of the global population, were reported to be moderately or severely food insecure in 2021, which is an increase of 350 million since the onset of the COVID-19 pandemic [13]. Diet is well known to be important for preserving healthy muscle [14,15], and individuals at risk of food insecurity are thus more likely to be susceptible to muscle deterioration. Indeed, the positive association of food insecurity with the risk of low muscle strength has been reported in two previous cross-sectional studies [16,17], but evidence is still limited [16,17] and the underlying mechanisms of the associations have not been elucidated.
Nevertheless, substantial evidence suggests that food insecurity may affect muscle strength by altering the inflammatory state of the body. Diet is thought to modulate systemic inflammation, whose association with inflammatory biomarkers is well-documented in the literature [18], and inflammation is increasingly recognized as having a negative effect on muscle maintenance, altering cellular protein metabolisms to favor proteolysis over synthesis [19,20,21,22]. Previously reported associations of a pro-inflammatory diet [23,24,25] or inflammatory markers [22,26,27] with the risk of low muscle strength further support this speculation. However, there is a paucity of evidence that the poor diets prevalent among food insecure groups indeed incite diets with high inflammatory potential [28,29].
Therefore, we hypothesized that the greater possibility of inflammation via poor diets associated with food insecurity may have a significant implication for muscle strength. To examine our hypothesis, we investigated (1) the association between food insecurity levels and the dietary inflammatory index (DII), a well-known composite measure for estimating the inflammatory capacity of the entire diet [18], and (2) the association between food insecurity and the risk of low muscle strength in the Korea Health and Nutrition Survey (KNHANES), a nationally representative cross-sectional survey of Koreans [30]. In a secondary analysis, we also explored whether the association of low muscle strength with levels of food insecurity varies according to population characteristics.
2. Materials and Methods
2.1. Study Population
This study used data from the 6th KNHANES (2104–2015). In brief, the KNHANES is an ongoing national survey that has been conducted by the Korea Centers for Disease Control (KCDC) since 1998 [30]. As a nationwide survey, the KNHANES enrolls nationally representative non-institutional civilians following a multi-level clustered probabilistic sampling design. The KNHANES consists of a household screening survey, health interview, health examination, and nutritional survey and collects details of several variables pertaining to the demographic, social, health, and nutritional status of the participants. All surveys are conducted with the consent of the participants. The institutional review boards of the KCDC have approved all KNHANES protocols. The present study was exempt from review by the institutional review board of Ewha Womans University because it used de-identified and publicly available data (IRB no. 202209-0020-01).
Of the 14,930 individuals who participated in the KNHANES (2014–2015), we excluded those who: (1) were under 19 years of age (N = 3178), (2) were pregnant (N = 658), (3) provided no response to the food security survey (N = 1043), (4) had no measurements for HGS (N = 971), and (5) had implausible energy intake (≤500 kcal, ≥5000 kcal [31]) (N = 456) (Figure 1). Consequently, the final sample size analyzed in our study was 8624 adults.
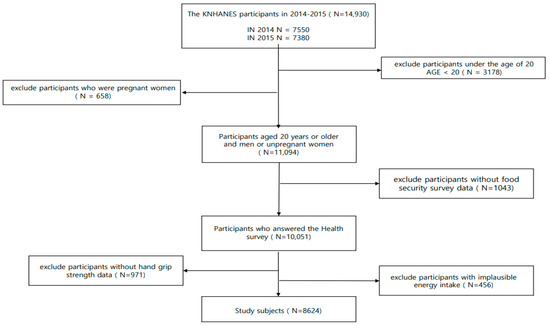
Figure 1.
Flow diagram of the study population selection.
2.2. Assessment of Food Insecurity
The primary exposure of interest was the household food security level. Household food insecurity was measured using the revised 18-item US Household Food Security Survey Module (USHFSSM) [32], the use of which has previously been validated in the Korean population [33]. In brief, the USHFSSM asks questions related to household- and individual-level experiences or behaviors relating to food purchasing, food availability, and diet over the previous 12 months. Of the 18 questions, eight pertain to children’s experiences and thus were omitted if no child was present in the household. The overall level of food insecurity was quantified by scoring the responses to the USHFSSM. Applying the USDA standard coding procedure of giving a point to affirmative responses indicative of insufficient resources for food, 0 or 1 points were allocated to each question [32]. For example, 1 point was given to those who answered “yes” to questions with two responses (“yes” or “no”) or those who answered “frequently” or “occasionally” to questions with three responses (“frequently”, “occasionally”, or “never”). The points from all 18 questions were summed to create a food insecurity score within the range of 0–18 for households with children and 0–10 for households without children. Higher scores indicate greater food insecurity levels. The reliability coefficient α of the USHFSSM is ≥0.89 for households both with and without children, which suggests a high level of confidence [31].
The USDA guidelines define food insecurity levels into four categories: “food secure” (score of 0–2 for households with/without children), “food insecure without hunger” (3–7 for households with children; 3–5 for households without children), “moderately food insecure with hunger” (8–12 for households with children; 6–8 for households without children), and “severely food insecure with hunger” (13–18 for households with children; 9–10 for households without children) [32]. However, the number of individuals within the “moderately food insecure with hunger” and “severely food insecure with hunger” categories was small in our study. Thus, we combined the latter two USDA categories and analyzed our study population by re-defining the food insecurity level into three groups, as follows [34]: “food secure” (USDA food secure group), “mildly food insecure” (USDA food insecure without hunger group), and “moderate-to-severe food insecurity” (USDA moderately and severely food insecure with hunger groups).
2.3. Measurement of Dietary Inflammatory Potential
The inflammatory potential of diets was assessed using the DII, which was developed by Shivappa et al. [18]; the details of its development [18] and validation [35,36] have been given previously. In brief, the DII is a composite score of 45 food parameters, including micronutrients, macronutrients, and individual food items, weighted by their dietary inflammatory effects. Each food parameter’s inflammatory effect was quantified as a score on the basis of its associations with inflammatory markers obtained from nearly 2000 articles [18]. To calculate the DII, the present study used DII food parameter intake data obtained from 24 h recall. The following 23 of the 45 DII food parameters in the original DII scoring algorithm were available and used for the DII calculation: energy, vitamin A, vitamin C, carbohydrates, proteins, total fat, saturated fatty acids, single unsaturated fatty acids, polyunsaturated fatty acids, omega-3 fatty acids, omega-6 fatty acids, cholesterol, dietary fiber, iron, carotene, thiamine, riboflavin, niacin, garlic, onions, ginger, pepper, and tea (black tea, green tea). For each DII food parameter, the actual intake was first standardized to a z-score using the world standard mean and deviation derived from the world composite database from 11 nations [18]. The z-score was then converted into a percentile and centered on zero by doubling the value and subtracting 1. The centered percentile intake value was multiplied by the respective inflammatory effect score to create a food-parameter-specific DII score. Finally, the DII score for each food parameter was summed across all the available food parameters to create an overall DII. A higher DII score suggests a higher pro-inflammatory potential for the diet.
2.4. Ascertainment of Low Muscle Strength
Muscle strength was estimated by measuring HGS, a well-known and reliable measure of muscle strength [6,7], using a digital grip strength dynamometer (Model T.K.K.5401, Takei Co., Ltd., Ishioka, Japan). The HGS testing was performed according to the standardized manual recommended by the Centers for Disease Control and Prevention, and the dynamometer was calibrated and checked by trained staffs to ensure the accuracy of the data [37]. HGS was assessed in a standing position with the arm and wrist in the anatomical position, and participants were asked not to wield the grip dynamometer or hold their breath during testing [38]. HGS was measured three times on each hand with a 1 min interval between each trial, alternating the left and right hands. To determine low muscle strength, the maximally measured HGS value out of the three measurements of the dominant hand was used, and low muscle strength was defined as <28 kg for men and <18 kg for women, using the recently revised diagnostic criteria recommended by the Asian Working Group for Sarcopenia [39,40].
2.5. Assessment of Covariates
The KNHANES collected data on sociodemographics (age, sex, marital status, area of residence, education, income), behavioral factors (body mass index (BMI), smoking, alcohol drinking, activity), and health status using standard self-reported questionnaires [30]. Using the information from these questionnaires, residential areas were defined as either urban or rural, according to the addresses of the participants. Smoking and alcohol drinking status were defined as never, past, or current. Physical activity was assessed through the International Physical Activity Questionnaire (IPAQ) [41,42]; participants were defined as having low, medium, or high levels of physical activity if their activity level was <600 metabolic equivalent (MET) minutes per week (min/week), 600–3000 MET (min/week), or ≥3000 MET (min/week) [41]. Height and weight were measured by trained staff, and BMI was calculated as the square (kg/m2) of weight (kg) over height (m). Comorbidities were defined by counting the number of existing chronic disease conditions, including diabetes mellitus, hypertension, dyslipidemia, stroke, myocardial infarction, angina pectoris, pulmonary tuberculosis, tuberculosis, and asthma [24,43]. Dietary data were collected via 24 h recall with the assistance of trained interviewers and converted to individual nutrient intakes based on the national standard food composition table [44].
3. Statistical Analyses
Sampling weights were applied to all analyses to yield unbiased national estimates of the KNHANES. The characteristics of the study population according to the food security level were averaged ± standard deviation using the SURVEYMEANS procedure for continuous variables, and the categorical variables were measured as numbers and percentages using the SURVEYFREQ procedure.
The analysis evaluated the association of food security with the DII score using the SURVEYREG procedure, while the association between food security and low muscle strength was evaluated using the SURVEYLOGISTIC procedure. To address the potential for confounding, well-known risk factors of muscle strength and food security were selected a priori from previous studies [16,17] and adjusted in the multivariable model as follows: age (continuous, year), sex (male, female), marital status (married, never married), residence (urban, rural), education level (less than elementary school, middle school graduate, high school graduate, college graduate or higher, missing), income (quartiles, missing), BMI (underweight, normal, overweight, obese, missing), smoking status (never, past, current, missing), alcohol drinking status (never, past, current), physical activity (high, medium, low), and number of chronic disease (0, 1, ≥2, missing). An indicator for missing responses in the covariates was created, if applicable. The P-trend was tested by modeling the median value for each food insecurity category as a continuous term. We also conducted several sensitivity analyses, defining low muscle strength by using age-specific criteria to take into account the variability of muscle strength with aging [45] and including protein intake, which was primarily not adjusted for because it could mediate the association between food insecurity and muscle strength. To examine whether associations varied by population characteristics, stratified analyses were conducted by sex, age, physical activity level, BMI, and smoking status. P for interaction was tested using the cross-product term between food security levels and stratification factors.
All analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA). All statistical tests were two-sided at a significance level <0.05.
4. Results
The characteristics of the study population are described in Table 1. Of the 8624 Korean adults in our study, 7995 (92.4%) were food secure, 529 (6.4%) were mildly food insecure, and 100 (1.2%) were moderate-to-severe food insecure. The mean age of our study population was 46.6 ± 0.3 years, and 50.8% were male. The majority were married (78.5%), never smokers (54.1%), and current alcoholic drinkers (73.0%) and lived in rural regions (69.7%), engaged in a low level of physical activity (63.8%), and had no chronic disease condition (75.3%). Participants with a greater level of food insecurity were more likely to be older, have less than college or higher education, earn a lower income, be overweight, and currently smoke, while also drinking less alcohol, being less physically active, and having a greater number of chronic disease conditions. They were also more likely to have greater DII and lower HGS levels (Supplementary Table S1) Sex, marital status, and residence were similar regardless of food security levels.

Table 1.
Study population characteristics 1 (N = 8624).
Table 2 shows the association between food insecurity and the DII score. In our analyses estimating the mean difference in DII score when comparing groups with increasing levels of food insecurity, we observed a significant positive dose-response trend for the association between food insecurity and DII score in both the age-adjusted and multivariable-adjusted models. Compared to the food secure group, the mean DII (95% CI) was higher by 0.36 (0.21–0.51) for the mildly food insecure group and by 0.69 (0.28–1.10) for the moderate-to-severe food insecure group in an age-adjusted model (P-trend 0.01). Similarly, the mean DII (95% CI) was higher by 0.15 (0.01–0.30) for the mildly food insecure group and 0.43 (0.06–0.80) for the moderate-to-severe food insecure group compared to the food secure group in the multivariable-adjusted model (P-trend < 0.001).

Table 2.
Age-adjusted and multivariable-adjusted 1 mean differences of dietary inflammatory index (DII) (95% confidence interval) according to food insecurity levels.
Table 3 shows the results for the association between food insecurity and the risk of low muscle strength. We observed a statistically significant positive dose-response trend for the association between food insecurity and the risk of low muscle strength in both age-adjusted and multivariable-adjusted models. The age-adjusted OR (95% CI) compared to the food secure group was 1.38 (0.98–1.95) for the mildly food insecure group and 2.76 (1.55–4.92) for the moderate-to-severe food insecure group (P-trend: <0.001). The multivariable-adjusted OR (95% CI) compared with the food secure group was 1.18 (0.83–1.70) for the mildly food insecure group and 2.06 (1.07–3.96) for the moderate-to-severe food insecure group (P-trend: 0.005). In our sensitivity analyses to test the robustness of our results, the inverse associations did not change substantially when protein intakes were further adjusted in the model (Supplementary Table S2) or when an age-specific cut-off was used to define low muscle strength [45] (Supplementary Table S3).

Table 3.
Age- and multivariable-adjusted 1 odds ratios (95% confidence intervals) of low muscle strength according to food insecurity levels.
We further explored possible effect modification by population characteristics for the association between food insecurity and the risk of low muscle strength (Table 4). However, the positive association observed between food insecurity and the risk of low muscle strength was not significantly modified by sex, age, physical activity, BMI, or smoking status (all P-interaction ≥ 0.43).

Table 4.
Multivariable-adjusted 1 odds ratios (95% confidence intervals) of low muscle strength according to food insecurity levels by population characteristics.
5. Discussion
In this nationally representative cross-sectional study of Korean adults, greater food insecurity was associated with diets with greater inflammatory potential, as measured by the DII, and an elevated risk of low muscle strength. The positive association of food insecurity with risk of low muscle strength did not significantly vary by sex, age, BMI, smoking status, or physical activity. Given the increased risk of morbidity and mortality associated with weak muscle strength [2,3,4,5], the identification of individuals at risk of muscle loss and its underlying mechanisms is important. Our results reinforce findings on the adverse health impact of food insecurity [12] and further expand the literature suggesting greater susceptibility to pro-inflammatory processes and muscle decline among individuals with lower food security.
Food insecurity refers to limited or uncertain access to or availability of nutritionally adequate and safe foods [12], which may lead to suboptimal, inadequate diets and compensatory reliance on affordable low-cost energy-dense foods. The increased risk of poor diet among food insecure groups is well established [11,34,46]. However, there are few studies on the inflammatory potential of the diet consumed by food insecure groups [28,29], which may underlie the poor health outcomes associated with food insecurity [12]. To date, two cross-sectional studies have examined the association between food insecurity and the DII [28,29]. A previous study of 10,630 low-income adults in the US reported a greater DII score, by 0.31, among the very low food secure group compared to the high food secure group (p = 0.0033) [28]. Similarly, results from 525 high school girls in Iran showed a greater DII score, by 0.025, for every one unit increase in the food insecurity score [29]. A recent Hungarian study also observed a greater DII level among the Hungarian Rome region population at risk of greater food insecurity [47] than the general population [48]. Our positive association of food insecurity with the DII adds to the consistent, though limited, literature.
Previous studies that examined the intake of individual nutrients [11,49] or diet patterns [11,34] in relation to food insecurity further support our positive association of food insecurity with the DII. A systematic review of 26 previous studies [11] and subsequent large national representative studies in the US [50], Canada [50], Brazil [51], and Korea [34,49] consistently reported that food insecure adults adhere less to a healthy diet and consume fewer vegetables and fruits and less fiber and polyunsaturated fat, but have a greater intake of calories, sugars, and saturated fat, which are associated with pro-inflammation [18,52]. This evidence thus indicates that a lack of food availability and disturbed access to food may induce an adverse change in diet quality, which may translate into a diet with greater inflammatory potential, thereby explaining our results, and predispose individuals to greater risk of chronic inflammation.
An altered inflammatory state has been implicated in many chronic diseases, including metabolic syndrome, type 2 diabetes, cardiovascular diseases, and various cancers [53], but relatively little attention has been paid to muscle strength. However, proinflammatory cytokines have been speculated to contribute to skeletal muscle loss [21] by impairing insulin signaling associated with protein synthesis [54] through the transcriptional activation of NF-kB or the induction of JK that contributes to phosphorylation of serine residue in IRS-1 [55]. Indeed, substantial evidence from animal and human studies shows that greater inflammatory milieu negatively affects muscle protein metabolism and skeletal muscle maintenance [19,21,22]. For example, in experimental studies, rats administered IL-6 or TNF-α were shown to have elevated skeletal muscle protein breakdown, decreased protein synthesis, and reduced total skeletal muscle amino acid concentration [56,57]. Similarly, a systematic review and meta-analysis of 149 cross-sectional studies and 19 longitudinal studies reported associations between higher levels of C-reactive protein (CRP), IL-6, and TNF-α and decreasing muscle strength [46]. These results were further confirmed in subsequent large, national, cross-sectional studies of 8232 adults [22], 2127 postmenopausal women [27], and 917 adolescents [26], which found significantly lower HGS with increasing inflammatory biomarker profiles, such as white blood cell counts [26], CRP [27], and systemic immune-inflammation index scores, which combine platelets, neutrophils, and lymphocytes [22].
Thus, food insecurity associated with a poor diet with greater inflammatory potential may accelerate degradation of muscle strength partly through the inflammatory pathway. Indeed, the majority of the previous four cross-sectional studies that evaluated the associations of DII with the risk of low muscle strength showed lower HGS among those with greater DII [23,24,25], although not all [58]. However, few studies have precisely evaluated the association between food insecurity and the risk of low muscle strength [16,17]. Our results, which indicate a positive association between food insecurity and the risk of low HGS, contribute to this limited literature, aligning with three previous studies’ results [16,17,59]. In the first, a National Health and Nutrition Examination Surveys study of the elderly (n = 3632) revealed a significantly increased association between food insecurity and risk of low HGS (OR:1.51, 95% CI: 1.03–2.22) [16]. In the second, a cross-sectional analysis of 664 Iranian adults, the odds ratios for food insecurity in men and women with low HGS were 5.46 and 3.12, respectively (p < 0.001) [17]. In the third, the Global Aging and Adult Health study of 14,585 adults also showed a significant 2.05 times increased risk of sarcopenia, defined as low muscle mass and either low muscle strength or slow gait [59].
Our study has several strengths. It is the first study to evaluate the plausibility of an inflammatory mechanism possibly mediated by diet through the association between food insecurity and muscle strength. Household food insecurity levels were measured using the most accurate instrument, that is, the full 18 items of the USHFSSM [32], the reliability and validity of which have previously been demonstrated in Korea [33]. Across the wide range of the USHFSSM’s food insecurity scale, we were able to evaluate the dose-response associations of food insecurity with diet and the risk of low muscle strength for various levels of food insecurity. Moreover, the quality of our HGS data was high given the multiple measurements of HGS performed by trained staff following the KCDC’s standardized HGS test protocols. We also used the most up-to-date diagnostic criteria to define low muscle strength in Asians, which account for the relatively small body size and adiposity compared to Caucasians [39]. Using the DII, we examined the possible impact of food insecurity across the overall inflammatory potential of the diet, accounting for complex interactions of nutrients beyond individual nutrients or food items [60]. Finally, utilizing data on food security, grip strength, diet, demographics, medical conditions, and lifestyle from the KNHANES, we comprehensively adjusted for the known possible confounding factors of low muscle strength and food insecurity and tested the robustness of our results by conducting several subgroup and sensitivity analyses.
There are several limitations to our study. First, the cross-sectional nature of our study design makes it difficult to determine the temporality between food insecurity and muscle strength data, which limits the causal interpretations of our results. Our inverse association between food insecurity and the risk of muscle strength can be alternatively interpreted as the consequence of low muscle strength limiting individuals’ behaviors and worsening their food insecurity. Second, although the use of 24 h recall in national nutritional surveys is common and has proven validity, precision, and high response rates [61], our 24 h recall dietary data are susceptible to random measurement error when estimating usual diets due to the inability to capture the day-to-day variations in food consumption. We calculated the DII using only 23 out of the 45 food parameters that comprise the DII due to the lack of dietary data in the KNHANES. Nonetheless, missing food parameters such as turmeric and saffron are likely to make up only a small proportion of total nutrients consumed by the general population. Furthermore, the significant association of the DII with circulating levels of inflammatory markers observed in previous studies with a limited number of food parameters, as in the present study, validates the use of the DII without the full 45 food parameters [25]. Finally, despite our comprehensive adjustment of potential confounding factors, we cannot rule out the possibility of unknown or residual confounding variables.
6. Conclusions
In conclusion, food insecurity was associated with diets with a greater DII score and an increased risk of low muscle strength in this nationally representative adult population in Korea. These findings support the notion that inflammation is likely to be elevated among those at risk of food insecurity, in part due to their nutritiously poor, pro-inflammatory diets, which may negatively affect muscle maintenance and muscle strength. Further large cohort studies confirming our results are warranted and will assist in generating useful information to support the design of evidence-based nutritional strategies to reduce the health burden among populations at risk of food insecurity.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu15051120/s1, Table S1: Median and interquartile range of DII and hand group strength according to food insecurity level; Table S2: Age- and multivariable-adjusted odds ratios (95% confidence intervals) of low muscle strength according to food insecurity levels additionally including protein intakes; Table S3: Age- and multivariable-adjusted odds ratios (95% confidence intervals) of low muscle strength according to food insecurity levels using an age-specific cut-off to define low muscle strength [45].
Author Contributions
S.M.K. analyzed the data and drafted the original manuscript. S.J. designed the research and critically reviewed and revised the manuscript. O.K., Y.J.P., H.K., K.S.K., Y.K. (Yuri Kim), Y.K. (Yangha Kim) and H.P. critically reviewed the manuscript and contributed to the interpretation of data. S.J. had primary responsibility for the final content. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the Ministry of Education and National Research Foundation of Korea (NRF-5199990614253–the BK21 FOUR [Fostering Outstanding Universities for Research] project to “Education Research Center for 4IR-Based Health Care” and NRF-2021R1A2C2095343), and by an Ewha Womans University Research Grant (1-2020-0325-001-1).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and the institutional review boards of the KCDC have approved all KNHANES protocols. The present study was exempt from review by the institutional review board of Ewha Womans University because it used de-identified and publicly available data (IRB no. 202209-0020-01).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data described in the article and codebook are publicly and freely available without restriction at https://knhanes.kdca.go.kr/knhanes/main.do (accessed on 1 September 2020).
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
BMI: body mass index; DII, dietary inflammatory index.
References
- Wolfe, R.R. The underappreciated role of muscle in health and disease. Am. J. Clin. Nutr. 2006, 84, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Celis-Morales, C.A.; Welsh, P.; Lyall, D.M.; Steell, L.; Petermann, F.; Anderson, J.; Iliodromiti, S.; Sillars, A.; Graham, N.; Mackay, D.F.; et al. Associations of grip strength with cardiovascular, respiratory, and cancer outcomes and all cause mortality: Prospective cohort study of half a million UK Biobank participants. Bmj 2018, 361, k1651. [Google Scholar] [CrossRef] [PubMed]
- Leong, D.P.; Teo, K.K.; Rangarajan, S.; Lopez-Jaramillo, P.; Avezum, A.J.; Orlandini, A.; Seron, P.; Ahmed, S.H.; Rosengren, A.; Kelishadi, R.; et al. Prognostic value of grip strength: Findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet 2015, 386, 266–273. [Google Scholar] [CrossRef]
- Artero, E.G.; Lee, D.C.; Lavie, C.J.; España-Romero, V.; Sui, X.; Church, T.S.; Blair, S.N. Effects of muscular strength on cardiovascular risk factors and prognosis. J. Cardiopulm. Rehabil. Prev. 2012, 32, 351–358. [Google Scholar] [CrossRef]
- Newman, A.B.; Kupelian, V.; Visser, M.; Simonsick, E.M.; Goodpaster, B.H.; Kritchevsky, S.B.; Tylavsky, F.A.; Rubin, S.M.; Harris, T.B. Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J. Gerontol. A Biol. Sci. Med. Sci. 2006, 61, 72–77. [Google Scholar] [CrossRef]
- Bohannon, R.W. Muscle strength: Clinical and prognostic value of hand-grip dynamometry. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Wang, D.X.M.; Yao, J.; Zirek, Y.; Reijnierse, E.M.; Maier, A.B. Muscle mass, strength, and physical performance predicting activities of daily living: A meta-analysis. J. Cachexia Sarcopenia Muscle 2020, 11, 3–25. [Google Scholar] [CrossRef]
- Kim, Y.S.; Lee, Y.; Chung, Y.S.; Lee, D.J.; Joo, N.S.; Hong, D.; Song, G.; Kim, H.J.; Choi, Y.J.; Kim, K.M. Prevalence of sarcopenia and sarcopenic obesity in the Korean population based on the Fourth Korean National Health and Nutritional Examination Surveys. J. Gerontol. A Biol. Sci. Med. Sci. 2012, 67, 1107–1113. [Google Scholar] [CrossRef]
- Moon, S.W.; Kim, K.J.; Lee, H.S.; Yun, Y.M.; Kim, J.E.; Chun, Y.J.; Kim, C.O. Low muscle mass, low muscle function, and sarcopenia in the urban and rural elderly. Sci. Rep. 2022, 12, 14314. [Google Scholar] [CrossRef]
- Hanson, K.L.; Connor, L.M. Food insecurity and dietary quality in US adults and children: A systematic review. Am. J. Clin. Nutr. 2014, 100, 684–692. [Google Scholar] [CrossRef]
- Food Insecurity And Health Outcomes. Health Affairs 2015, 34, 1830–1839. [CrossRef] [PubMed]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2022 Repurposing Food and Agricultural Policies to Make Healthy Diets More Affordable; FAO: Rome, Italy, 2022. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Dawson Hughes, B.; Scott, D.; Sanders, K.M.; Rizzoli, R. Nutritional strategies for maintaining muscle mass and strength from middle age to later life: A narrative review. Maturitas 2020, 132, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.R.; Philp, A. Editorial: Nutritional Strategies to Promote Muscle Mass and Function Across the Health Span. Front. Nutr. 2020, 7, 569270. [Google Scholar] [CrossRef]
- Lynch, D.H.; Petersen, C.L.; Van Dongen, M.J.; Spangler, H.B.; Berkowitz, S.A.; Batsis, J.A. Association between food insecurity and probable sarcopenia: Data from the 2011–2014 National Health and nutrition examination survey. Clin. Nutr. 2022, 41, 1861–1873. [Google Scholar] [CrossRef] [PubMed]
- Dassie, G.A.; Motlagh, A.D.; Chamari, M.; Mohammadreza, E. Prevalence of Food Insecurity and its Association with Muscle Mass, Hand Grip Strength and Gait Speed among Elderly In Tehran. Int. J. Pharm. Sci. Res. 2016, 7, 2889–2895. [Google Scholar] [CrossRef]
- Shivappa, N.; Steck, S.E.; Hurley, T.G.; Hussey, J.R.; Hébert, J.R. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014, 17, 1689–1696. [Google Scholar] [CrossRef]
- Wiedmer, P.; Jung, T.; Castro, J.P.; Pomatto, L.C.D.; Sun, P.Y.; Davies, K.J.A.; Grune, T. Sarcopenia—Molecular mechanisms and open questions. Ageing Res. Rev. 2021, 65, 101200. [Google Scholar] [CrossRef]
- Afzali, A.M.; Müntefering, T.; Wiendl, H.; Meuth, S.G.; Ruck, T. Skeletal muscle cells actively shape (auto)immune responses. Autoimmun. Rev. 2018, 17, 518–529. [Google Scholar] [CrossRef]
- Costamagna, D.; Costelli, P.; Sampaolesi, M.; Penna, F. Role of Inflammation in Muscle Homeostasis and Myogenesis. Mediators Inflamm. 2015, 2015, 805172. [Google Scholar] [CrossRef]
- Wu, D.; Gao, X.; Shi, Y.; Wang, H.; Wang, W.; Li, Y.; Zheng, Z. Association between Handgrip Strength and the Systemic Immune-Inflammation Index: A Nationwide Study, NHANES 2011–2014. Int. J. Environ. Res. Public Health 2022, 19, 13616. [Google Scholar] [CrossRef] [PubMed]
- Bawaked, R.A.; Schröder, H.; Ribas-Barba, L.; Izquierdo-Pulido, M.; Pérez-Rodrigo, C.; Fíto, M.; Serra-Majem, L. Association of diet quality with dietary inflammatory potential in youth. Food Nutr. Res. 2017, 61, 1328961. [Google Scholar] [CrossRef]
- Bagheri, A.; Soltani, S.; Hashemi, R.; Heshmat, R.; Motlagh, A.D.; Esmaillzadeh, A. Inflammatory potential of the diet and risk of sarcopenia and its components. Nutr. J. 2020, 19, 129. [Google Scholar] [CrossRef]
- Shin, D.; Lee, K.W.; Brann, L.; Shivappa, N.; Hébert, J.R. Dietary inflammatory index is positively associated with serum high-sensitivity C-reactive protein in a Korean adult population. Nutrition 2019, 63–64, 155–161. [Google Scholar] [CrossRef] [PubMed]
- López-Gil, J.F.; Ramírez-Vélez, R.; Izquierdo, M.; García-Hermoso, A. Handgrip Strength and Its Relationship with White Blood Cell Count in U.S. Adolescents. Biology 2021, 10, 884. [Google Scholar] [CrossRef] [PubMed]
- Son, D.H.; Song, S.A.; Lee, Y.J. Association between C-Reactive Protein and Relative Handgrip Strength in Postmenopausal Korean Women Aged 45–80 Years: A Cross-Sectional Study. Clin. Interv. Aging 2022, 17, 971–978. [Google Scholar] [CrossRef] [PubMed]
- Bergmans, R.S.; Palta, M.; Robert, S.A.; Berger, L.M.; Ehrenthal, D.B.; Malecki, K.M. Associations between Food Security Status and Dietary Inflammatory Potential within Lower-Income Adults from the United States National Health and Nutrition Examination Survey, Cycles 2007 to 2014. J. Acad. Nutr. Diet 2018, 118, 994–1005. [Google Scholar] [CrossRef]
- Daneshzad, E.; Ghorabi, S.; Hasani, H.; Omidian, M.; Jane Pritzl, T.; Yavari, P. Food Insecurity is positively related to Dietary Inflammatory Index in Iranian high school girls. Int. J. Vitam. Nutr. Res. 2020, 90, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef]
- Lee, H.S. Food Insecurity and Related Risk Factors in the Elderly: Korea National Health and Nutrition Examination Survey 2013 Data. J. Korean Diet. Assoc. 2015, 21, 308–319. [Google Scholar] [CrossRef]
- Bickel, G.; Nord, M.; Price, C.; Hamilton, W.; Cook, J. Guide to Measuring Household Food Security, Revised 2000; U.S. Department of Agriculture, Food and Nutrition Service: Alexandria VA, USA, March 2000. [Google Scholar]
- Kim, K.; Hong, S.A.; Kwon, S.O.; Choi, B.Y.; Kim, G.-Y.; Oh, S.-Y. Validation of Food Security Measures for the Korean National Health and Nutrition Examination Survey. Korean J. Community Nutr. 2011, 16, 771–781. [Google Scholar] [CrossRef]
- Kang, M.G.; Yook, S.M.; Hwang, J.Y. Is It What They Eat or How Much They Eat That Matters More in Adults with Food Insecurity in a Wealthy-Country Context? Nutrients 2021, 13, 851. [Google Scholar] [CrossRef] [PubMed]
- Shivappa, N.; Steck, S.E.; Hurley, T.G.; Hussey, J.R.; Ma, Y.; Ockene, I.S.; Tabung, F.; Hébert, J.R. A population-based dietary inflammatory index predicts levels of C-reactive protein in the Seasonal Variation of Blood Cholesterol Study (SEASONS). Public Health Nutr. 2014, 17, 1825–1833. [Google Scholar] [CrossRef]
- Shivappa, N.; Hébert, J.R.; Rietzschel, E.R.; De Buyzere, M.L.; Langlois, M.; Debruyne, E.; Marcos, A.; Huybrechts, I. Associations between dietary inflammatory index and inflammatory markers in the Asklepios Study. Br. J. Nutr. 2015, 113, 665–671. [Google Scholar] [CrossRef]
- Kang, Y.; Kim, J.; Kim, S.; Park, S.; Lim, H.; Koh, H. Trends in measures of handgrip strength from 2014 to 2017 among Korean adolescents using the Korean National Health and Nutrition Examination Survey Data. BMC Res. Notes 2020, 13, 307. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.R.; Jeon, Y.J.; Kim, M.C.; Jeong, T.; Koo, W.R. Reference values for hand grip strength in the South Korean population. PLoS ONE 2018, 13, e0195485. [Google Scholar] [CrossRef]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e302. [Google Scholar] [CrossRef]
- de Almeida Marques, R.; de Souza, V.F.; do Rosario, T.C.; da Silva Garcia, M.R.P.; Pereira, T.S.S.; Marques-Rocha, J.L.; Guandalini, V.R. Agreement between maximum and mean handgrip strength measurements in cancer patients. PLoS ONE 2022, 17, e0270631. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sport. Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Oh, J.Y.; Yang, Y.J.; Kim, B.S.; Kang, J.H. Validity and Reliability of Korean Version of International Physical Activity Questionnaire (IPAQ) Short Form. J. Korean Acad. Fam. Med. 2007, 28, 532–541. [Google Scholar]
- Schaap, L.A.; Pluijm, S.M.; Deeg, D.J.; Harris, T.B.; Kritchevsky, S.B.; Newman, A.B.; Colbert, L.H.; Pahor, M.; Rubin, S.M.; Tylavsky, F.A.; et al. Higher inflammatory marker levels in older persons: Associations with 5-year change in muscle mass and muscle strength. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64, 1183–1189. [Google Scholar] [CrossRef]
- Korean National Academy of Agricultural Science. Food Composition Table, 7th ed.; Rural Development Administration, Republic of Korea: Suwon, Republic of Korea, 2006. [Google Scholar]
- Lee, Y.L.; Lee, B.H.; Lee, S.Y. Handgrip Strength in the Korean Population: Normative Data and Cutoff Values. Ann. Geriatr. Med. Res. 2019, 23, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Leung, C.W.; Wolfson, J.A. Food Insecurity among Older Adults: 10-Year National Trends and Associations with Diet Quality. J. Am. Geriatr. Soc. 2021, 69, 964–971. [Google Scholar] [CrossRef] [PubMed]
- Llanaj, E.; Vincze, F.; Kósa, Z.; Sándor, J.; Diószegi, J.; Ádány, R. Dietary Profile and Nutritional Status of the Roma Population Living in Segregated Colonies in Northeast Hungary. Nutrients 2020, 12, 2836. [Google Scholar] [CrossRef] [PubMed]
- Llanaj, E.; Vincze, F.; Kósa, Z.; Bárdos, H.; Diószegi, J.; Sándor, J.; Ádány, R. Deteriorated Dietary Patterns with Regards to Health and Environmental Sustainability among Hungarian Roma Are Not Differentiated from Those of the General Population. Nutrients 2021, 13, 721. [Google Scholar] [CrossRef]
- Lee, S.E.; Song, Y.J.; Kim, Y.; Choe, J.; Paik, H.Y. Household food insufficiency is associated with dietary intake in Korean adults. Public Health Nutr. 2016, 19, 1112–1121. [Google Scholar] [CrossRef]
- Kirkpatrick, S.I.; Dodd, K.W.; Parsons, R.; Ng, C.; Garriguet, D.; Tarasuk, V. Household Food Insecurity Is a Stronger Marker of Adequacy of Nutrient Intakes among Canadian Compared to American Youth and Adults. J. Nutr. 2015, 145, 1596–1603. [Google Scholar] [CrossRef]
- Kubo, S.; da Costa, T.H.M.; Gubert, M.B. Intakes of energy, macronutrients and micronutrients of a population in severe food insecurity risk in Brazil. Public Health Nutr. 2020, 23, 649–659. [Google Scholar] [CrossRef] [PubMed]
- Hart, M.J.; Torres, S.J.; McNaughton, S.A.; Milte, C.M. Dietary patterns and associations with biomarkers of inflammation in adults: A systematic review of observational studies. Nutr. J. 2021, 20, 24. [Google Scholar] [CrossRef]
- Furman, D.; Campisi, J.; Verdin, E.; Carrera-Bastos, P.; Targ, S.; Franceschi, C.; Ferrucci, L.; Gilroy, D.W.; Fasano, A.; Miller, G.W.; et al. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 2019, 25, 1822–1832. [Google Scholar] [CrossRef]
- Wang, X.; Hu, Z.; Hu, J.; Du, J.; Mitch, W.E. Insulin resistance accelerates muscle protein degradation: Activation of the ubiquitin-proteasome pathway by defects in muscle cell signaling. Endocrinology 2006, 147, 4160–4168. [Google Scholar] [CrossRef]
- Shoelson, S.E.; Lee, J.; Goldfine, A.B. Inflammation and insulin resistance. J. Clin. Investig. 2006, 116, 1793–1801. [Google Scholar] [CrossRef] [PubMed]
- Goodman, M.N. Interleukin-6 induces skeletal muscle protein breakdown in rats. Proc. Soc. Exp. Biol. Med. 1994, 205, 182–185. [Google Scholar] [CrossRef] [PubMed]
- Tayek, J.A. Effects of tumor necrosis factor alpha on skeletal muscle amino acid metabolism studied in-vivo. J. Am. Coll. Nutr. 1996, 15, 164–168. [Google Scholar] [CrossRef]
- Amakye, W.K.; Zhang, Z.; Wei, Y.; Shivappa, N.; Hebert, J.R.; Wang, J.; Su, Y.; Mao, L. The relationship between dietary inflammatory index (DII) and muscle mass and strength in Chinese children aged 6–9 years. Asia. Pac. J. Clin. Nutr. 2018, 27, 1315–1324. [Google Scholar] [CrossRef]
- Smith, L.; Jacob, L.; Barnett, Y.; Butler, L.T.; Shin, J.I.; López-Sánchez, G.F.; Soysal, P.; Veronese, N.; Haro, J.M.; Koyanagi, A. Association between Food Insecurity and Sarcopenia among Adults Aged ≥65 Years in Low- and Middle-Income Countries. Nutrients 2021, 13, 1879. [Google Scholar] [CrossRef]
- Hu, F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Huang, K.; Zhao, L.; Guo, Q.; Yu, D.; Yang, Y.; Cao, Q.; Yuan, X.; Ju, L.; Li, S.; Cheng, X.; et al. Comparison of the 24 h Dietary Recall of Two Consecutive Days, Two Non-Consecutive Days, Three Consecutive Days, and Three Non-Consecutive Days for Estimating Dietary Intake of Chinese Adult. Nutrients 2022, 14, 1960. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).