The Interactions of Food Security, Health, and Loneliness among Rural Older Adults before and after the Onset of COVID-19
Abstract
1. Introduction
1.1. Rural Challenges for Older Americans
1.2. Connections between Food Security, Health, and Loneliness among Older Adults
2. Materials and Methods
2.1. Defining Quality of Life
2.2. Hypotheses
2.3. Research Site
2.4. Data Collection
2.5. Data Analysis
3. Results
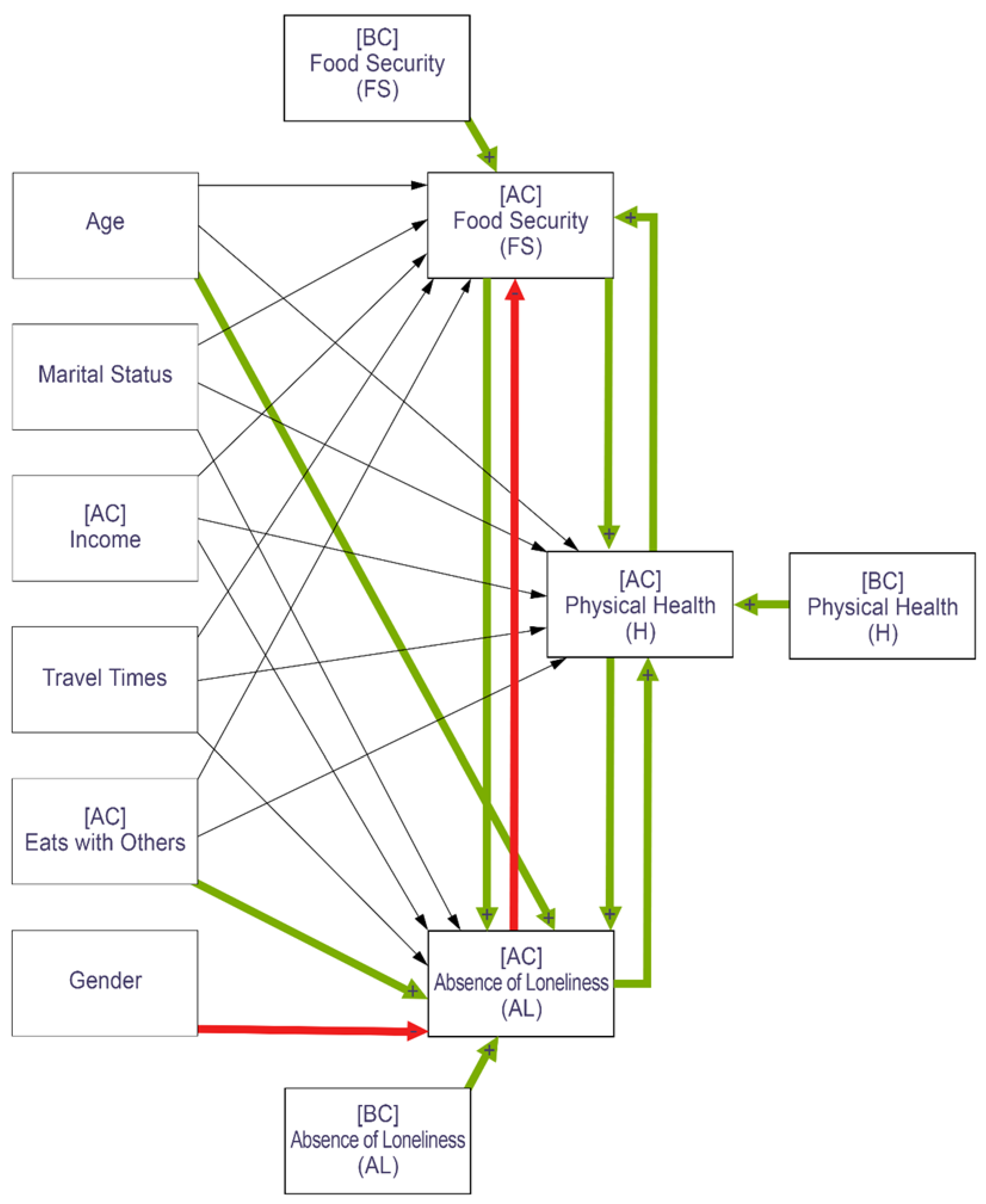
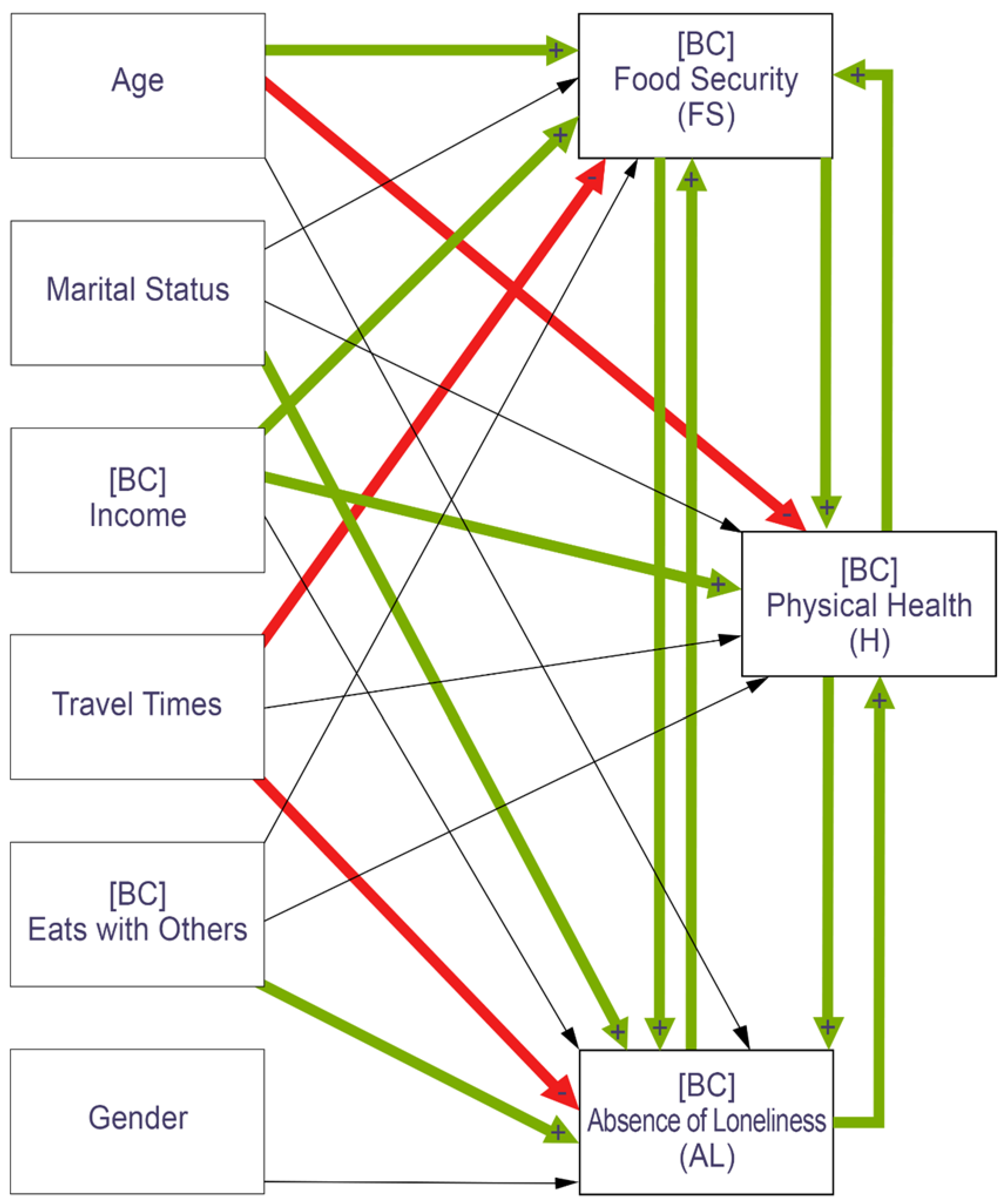
3.1. Before COVID Path Analysis
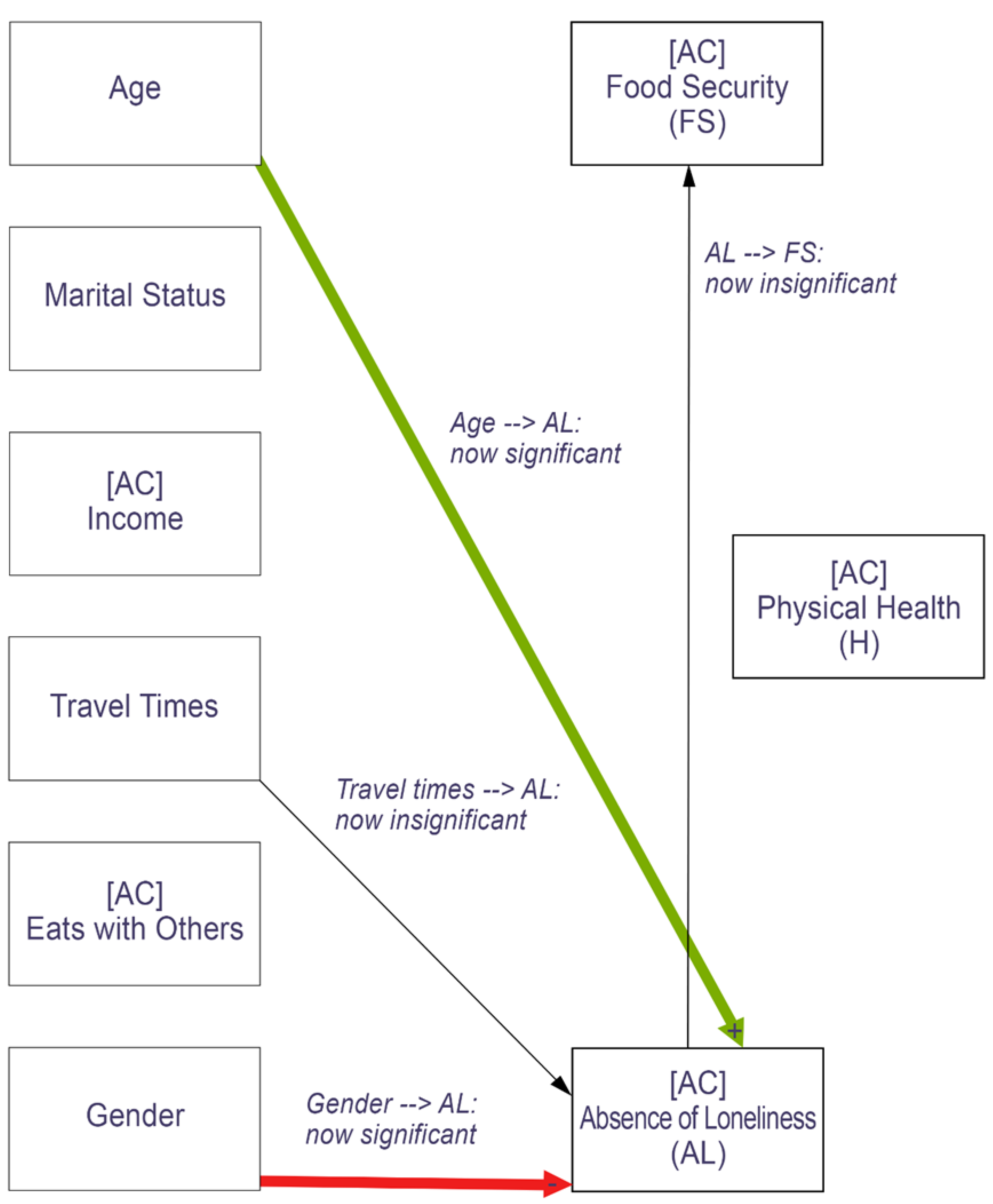
3.2. Changes during COVID-19
3.3. Controlling for Before-COVID Food Security, Health, and Loneliness
4. Discussion
4.1. Food Insecurity and Health
4.2. Food Insecurity and Loneliness
4.3. Loneliness, Health, and Gender
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Coef. | p | 95% Conf. Interval | ||
|---|---|---|---|---|
| Food Security (FS)+ | ||||
| Age | 0.07 | 0.000 | 0.04 | 0.10 |
| Marital Status | 0.04 | 0.849 | −0.41 | 0.50 |
| Income | 0.35 | 0.000 | 0.26 | 0.45 |
| Travel Times | −0.0002 | 0.023 | −0.0004 | −0.0003 |
| Eats with Others | 0.02 | 0.876 | −0.18 | 0.21 |
| Physical Health (H) | 0.05 | 0.000 | 0.03 | 0.07 |
| Absence of Loneliness (AL) | ||||
| 3 [base] | -- | -- | -- | -- |
| 4 | 0.10 | 0.899 | −1.45 | 1.65 |
| 5 | 0.14 | 0.837 | −1.22 | 1.50 |
| 6 | 0.78 | 0.214 | −0.45 | 2.01 |
| 7 | 0.63 | 0.311 | −0.58 | 1.84 |
| 8 | 1.26 | 0.047 | 0.02 | 2.51 |
| 9 | 1.60 | 0.006 | 0.45 | 2.75 |
| Physical Health (H)+ | ||||
| Age | −0.13 | 0.000 | −0.19 | −0.06 |
| Marital Status | 0.41 | 0.461 | −0.68 | 1.51 |
| Income | 0.32 | 0.001 | 0.13 | 0.51 |
| Travel Times | 0.0004 | 0.059 | −0.00002 | 0.0009 |
| Eats with Others | −0.0008 | 0.997 | −0.44 | 0.44 |
| Food Security (FS) | 5.1 | 0.000 | 3.56 | 6.63 |
| Absence of Loneliness (AL) | ||||
| 3 [base] | - | - | - | - |
| 4 | −1.93 | 0.473 | −7.20 | 3.34 |
| 5 | −0.58 | 0.803 | −5.12 | 3.96 |
| 6 | 0.85 | 0.669 | −3.04 | 4.73 |
| 7 | 1.27 | 0.518 | −2.57 | 5.10 |
| 8 | 4.03 | 0.039 | 0.21 | 7.85 |
| 9 | 4.26 | 0.021 | 0.63 | 7.90 |
| Absence of Loneliness+ | ||||
| Age | 0.007 | 0.429 | −0.01 | 0.02 |
| Gender | −0.25 | 0.098 | −0.54 | 0.05 |
| Marital Status | 0.91 | 0.000 | 0.63 | 1.19 |
| Income | 0.01 | 0.670 | −0.04 | 0.06 |
| Travel Times | −0.0001 | 0.024 | −0.0003 | −0.00002 |
| Eats with Others | 0.22 | 0.001 | 0.09 | 0.34 |
| Food Security (FS) | 0.99 | 0.000 | 0.62 | 1.37 |
| Physical Health (H) | 0.04 | 0.000 | 0.02 | 0.05 |
| Coef. | p | 95% Conf. Interval | ||
|---|---|---|---|---|
| Food Security (FS)+ | ||||
| Age | 0.05 | 0.000 | 0.03 | 0.08 |
| Marital Status | 0.12 | 0.605 | −0.33 | 0.51 |
| Income | 0.30 | 0.000 | 0.21 | 0.39 |
| Travel Times | −0.0002 | 0.015 | −0.0004 | −0.0004 |
| Eats with Others | 0.07 | 0.463 | −0.11 | 0.24 |
| Physical Health (H) | 0.06 | 0.000 | 0.04 | 0.08 |
| Absence of Loneliness (AL) | ||||
| 4 [base] | - | - | - | - |
| 5 | −0.22 | 0.768 | −1.65 | 1.21 |
| 6 | −0.12 | 0.873 | −1.55 | 1.31 |
| 7 | 0.45 | 0.541 | −1.10 | 1.90 |
| 8 | 1.14 | 0.149 | −0.41 | 2.68 |
| 9 | 0.93 | 0.210 | −0.52 | 2.38 |
| Physical Health (H)+ | ||||
| Age | −0.12 | 0.001 | −0.18 | −0.05 |
| Marital Status | 1.02 | 0.070 | −0.08 | 2.12 |
| Income | 0.35 | 0.000 | 0.16 | 0.55 |
| Travel Times | 0.0003 | 0.199 | −0.00002 | 0.0008 |
| Eats with Others | 0.15 | 0.433 | −0.23 | 0.54 |
| Food Security (FS) | 6.34 | 0.000 | 4.81 | 7.87 |
| Absence of Loneliness (AL) | ||||
| 4 [base] | -- | -- | -- | -- |
| 5 | 2.98 | 0.179 | −1.37 | 7.32 |
| 6 | 5.28 | 0.017 | 0.96 | 9.59 |
| 7 | 4.70 | 0.033 | 0.38 | 9.02 |
| 8 | 6.52 | 0.003 | 2.19 | 10.85 |
| 9 | 6.93 | 0.001 | 2.67 | 11.19 |
| Absence of Loneliness+ | ||||
| Age | 0.02 | 0.003 | 0.01 | 0.04 |
| Gender | −0.34 | 0.006 | −0.58 | −0.10 |
| Marital Status | 0.32 | 0.012 | 0.07 | 0.57 |
| Income | 0.03 | 0.244 | −0.02 | 0.07 |
| Travel Times | −0.0003 | 0.606 | −0.0001 | −0.00008 |
| Eats with Others | 0.19 | 0.000 | 0.10 | 0.27 |
| Food Security (FS) | 0.84 | 0.000 | 0.49 | 1.20 |
| Physical Health (H) | 0.04 | 0.000 | 0.02 | 0.05 |
| Coef. | p | 95% Conf. Interval | ||
|---|---|---|---|---|
| Food Security (FS)+ | ||||
| Age | 0.02 | 0.497 | −0.03 | 0.07 |
| Marital Status | −0.32 | 0.431 | −1.13 | 0.48 |
| Income | 0.05 | 0.519 | −0.10 | 0.20 |
| Travel Times | −0.0001 | 0.637 | −0.0004 | 0.0002 |
| Eats with Others | −0.04 | 0.797 | −0.31 | 0.24 |
| Physical Health (H) | 0.04 | 0.016 | 0.008 | 0.08 |
| Absence of Loneliness (AL) | ||||
| 4 [base] | - | - | - | - |
| 5 | −1.97 | 0.106 | −4.36 | 0.42 |
| 6 | −2.87 | 0.019 | −5.27 | −0.47 |
| 7 | −1.17 | 0.338 | −3.58 | 1.23 |
| 8 | −0.75 | 0.559 | −3.27 | 1.77 |
| 9 | −1.22 | 0.322 | −3.62 | 1.19 |
| [BC] Food Security | 5.84 | 0.000 | 4.96 | 6.72 |
| [BC] AL à [AC] AL | 0.81 | 0.000 | 0.72 | 0.89 |
| [BC] H à [AC] H | 0.97 | 0.000 | 0.95 | 1.05 |
| Physical Health (H)+ | ||||
| Age | −0.007 | 0.607 | −0.03 | 0.02 |
| Marital Status | 0.02 | 0.910 | −0.40 | 0.45 |
| Income | 0.39 | 0.297 | −0.03 | 0.11 |
| Travel Times | −0.00002 | 0.798 | −0.0002 | 0.0002 |
| Eats with Others | 0.04 | 0.561 | −0.010 | 0.0002 |
| Food Security (FS) | 1.63 | 0.000 | 1.03 | 2.23 |
| Absence of Loneliness (AL) | ||||
| 4 [base] | -- | -- | -- | -- |
| 5 | −1.28 | 0.132 | −2.94 | 0.38 |
| 6 | −0.04 | 0.961 | −1.70 | 1.62 |
| 7 | −0.0005 | 1.00 | −1.66 | 1.66 |
| 8 | 0.38 | 0.536 | −1.12 | 2.15 |
| 9 | 0.52 | 0.536 | −1.12 | 2.15 |
| [AC] Physical Health | 0.94 | 0.000 | 0.92 | 0.97 |
| [BC] FS à [AC] FS | 5.80 | 0.000 | 5.22 | 6.38 |
| [BC] AL à [AC] AL | 0.81 | 0.000 | 0.72 | 0.89 |
| Absence of Loneliness+ | ||||
| Age | 0.02 | 0.004 | 0.01 | 0.04 |
| Gender | −0.36 | 0.005 | −0.61 | −0.11 |
| Marital Status | −0.22 | 0.107 | −0.48 | 0.05 |
| Income | 0.01 | 0.630 | −0.03 | 0.06 |
| Travel Times | 0.0003 | 0.645 | −0.0001 | 0.0001 |
| Eats with Others | 0.18 | 0.000 | 0.01 | 0.27 |
| Food Security (FS) | 0.62 | 0.001 | 0.24 | 0.99 |
| Physical Health (H) | 0.02 | 0.002 | 0.01 | 0.04 |
| [BC] Absence of Loneliness (AL) | ||||
| 3 [base] | -- | -- | -- | -- |
| 4 | 2.25 | 0.000 | 1.08 | 3.50 |
| 5 | 1.28 | 0.027 | 0.15 | 2.42 |
| 6 | 1.30 | 0.008 | 0.34 | 2.27 |
| 7 | 2.20 | 0.000 | 1.23 | 3.17 |
| 8 | 2.96 | 0.000 | 2.00 | 3.93 |
| 9 | 4.18 | 0.000 | 3.24 | 5.12 |
| [BC] FS à [AC] FS | 5.80 | 0.000 | 5.22 | 6.38 |
| [BC] H à [AC] H | 0.97 | 0.000 | 0.95 | 1.05 |

References
- Jackson, A.M.; Weaver, R.H.; Iniguez, A.; Lanigan, J. A lifespan perspective of structural and perceived social relationships, food insecurity, and dietary behaviors during the COVID-19 pandemic. Appetite 2021, 168, 105717. [Google Scholar] [CrossRef] [PubMed]
- USDA. Definitions of Food Security. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security/ (accessed on 2 December 2018).
- Hardebeck, A. 4 Facts You Should Know About Hunger in Rural America—Feeding America Action. Available online: https://feedingamericaaction.org/blog/rural-hunger/ (accessed on 22 June 2021).
- Giroux, S.; Waldman, K.; Burris, M.; Valliant, J.C.D.; Babb, A.M.; Stafford, P.; Fobi, D.; Czebotar, K.; Knudsnen, D.C. Food security and well-being among older, rural Americans before and during the COVID-19 pandemic. PLoS ONE 2022, 17, e0274020. [Google Scholar] [CrossRef]
- Piette, J.; Solway, E.; Singer, D.; Kirch, M.; Kullgren, J.; Malani, P. Loneliness among Older Adults before and during the COVID-19 Pandemic. 2020. Available online: www.healthyagingpoll.org (accessed on 4 January 2022).
- Valliant, J.C.D.; Burris, M.E.; Czebotar, K.; Stafford, P.B.; Giroux, S.A.; Babb, A.; Waldman, K.; Knudsen, D.C. Navigating Food Insecurity as a Rural Older Adult: The Importance of Congregate Meal Sites, Social Networks and Transportation Services. J. Hunger Environ. Nutr. 2021, 17, 593–614. [Google Scholar] [CrossRef]
- Warren, A.M.; Frongillo, E.A.; Alford, S.; McDonald, E. Taxonomy of Seniors’ Needs for Food and Food Assistance in the United States. Qual. Health Res. 2020, 30, 988–1003. [Google Scholar] [CrossRef] [PubMed]
- Robinson, J.M.; Mzali, L.; Knudsen, D.; Farmer, J.; Spiewak, R.; Suttles, S.; Burris, M.; Shattuck, A.; Valliant, J.; Babb, A. Food after the COVID-19 Pandemic and the Case for Change Posed by Alternative Food: A Case Study of the American Midwest. Glob. Sustain. 2021, 4, e6. [Google Scholar] [CrossRef]
- Leddy, A.M.; Weiser, S.D.; Palar, K.; Seligman, H. A conceptual model for understanding the rapid COVID-19-related increase in food insecurity and its impact on health and healthcare. Am. J. Clin. Nutr. 2020, 112, 1162–1169. [Google Scholar] [CrossRef]
- Davis, J.C.; Rupasingha, A.; Cromartie, J.; Sanders, A. Rural America at a Glance: 2022 Edition. 2022. Available online: https://www.ers.usda.gov/webdocs/publications/105155/eib-246.pdf?v=6906.4 (accessed on 20 November 2022).
- Smith, D.T.; Mouzon, D.M.; Elliott, M. Reviewing the Assumptions about Men’s Mental Health: An Exploration of the Gender Binary. Am. J. Men’s Health 2018, 12, 78–89. [Google Scholar] [CrossRef]
- USDA. USDA ERS—Rural Poverty & Well-Being. 2021. Available online: https://www.ers.usda.gov/topics/rural-economy-population/rural-poverty-well-being/ (accessed on 14 December 2021).
- Gundersen, C.; Strayer, M.; Dewey, A.; Hake, M.; Engelhard, E. Map the Meal Gap 2022: An Analysis of County and Congressional District Food Insecurity and County Food Cost in the United States in 2020; Feeding America: Chicago, IL, USA, 2022. [Google Scholar]
- Rhone, A.; Ver Ploeg, M.; Williams, R.; Breneman, V. Understanding Low-Income and Low-Access Census Tracts across the Nation: Subnational and Subpopulation Estimates of Access to Healthy Food. 2019. Available online: www.ers.usda.gov (accessed on 14 December 2021).
- Dean, W.R.; Johnson, C.M.; Sharkey, J.R. Rural food disparities: Availability and Accessibility of Healthy Foods. In Rural Populations and Health: Determinants, Disparities, and Solutions, 1st ed.; Crosby, R.A., Wendel, M.L., Vanderpool, R.C., Casey, B.R., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2012. [Google Scholar]
- Piontak, J.R.; Schulman, M.D. Food Insecurity in Rural America. Contexts 2014, 13, 75–77. [Google Scholar] [CrossRef]
- Nantz, E.L.; Millstein, M.B.; Davis, H.F.; Kaplan, K.H.; Czebotar, K.; Babb, A.M.; Palde, L.P.R.; Grantz, T.; Knudsen, D.C. Comparing two analytical approaches to evaluate access to fresh, healthy food: A case of the Indiana Uplands. Local Environ. 2020, 25, 921–943. [Google Scholar] [CrossRef]
- Waity, J.F. Geographic variation in barriers to the usage of food assistance in Indiana. J. Hunger Environ. Nutr. 2019, 14, 511–525. [Google Scholar] [CrossRef]
- Kaplan, K.H.; Kirk, K.J.; Lich, K.M.; Palde, L.P.R.; Van Allen, C.; Nantz, E.L.; Leuthart, K.R.; Robeson, S.M.; Davis, H.F.; Blekking, J.; et al. Accessibility to emergency food systems in south-central Indiana evaluated by spatiotemporal indices of pressure at county and pantry level. Nat. Food 2020, 1, 284–291. [Google Scholar] [CrossRef]
- Fernandes, S.G.; Rodrigues, A.M.; Nunes, C.; Santos, O.; Gregório, M.J.; De Sousa, R.D.; Dias, S.; Canhão, H. Food Insecurity in Older Adults: Results From the Epidemiology of Chronic Diseases Cohort Study 3. Front. Med. 2018, 5, 203. [Google Scholar] [CrossRef] [PubMed]
- Kihlström, L.; Burris, M.; Dobbins, J.; McGrath, E.; Renda, A.; Cordier, T.; Song, Y.; Prendergast, K.; Serrano Arce, K.; Shannon, E.; et al. Food Insecurity and Health-Related Quality of Life: A Cross-Sectional Analysis of Older Adults in Florida, U.S. Ecol. Food Nutr. 2018, 58, 45–65. [Google Scholar] [CrossRef] [PubMed]
- Leung, C.W.; Zhou, M.S. Household Food Insecurity and the Association with Cumulative Biological Risk among Lower-Income Adults: Results from the National Health and Nutrition Examination Surveys 2007–2010. Nutrients 2020, 12, 1517. [Google Scholar] [CrossRef] [PubMed]
- Russell, J.C.; Flood, V.M.; Yeatman, H.; Wang, J.J.; Mitchell, P. Food insecurity and poor diet quality are associated with reduced quality of life in older adults. Nutr. Diet 2016, 73, 50–58. [Google Scholar] [CrossRef]
- Sharkey, J.R.; Johnson, C.M.; Dean, W.R. Relationship of Household Food Insecurity to Health-Related Quality of Life in a Large Sample of Rural and Urban Women. Women Health 2011, 51, 442–460. [Google Scholar] [CrossRef]
- Jih, J.; Stijacic-Cenzer, I.; Seligman, H.K.; Boscardin, W.J.; Nguyen, T.T.; Ritchie, C.S. Chronic disease burden predicts food insecurity among older adults. Public Health Nutr. 2018, 21, 1737–1742. [Google Scholar] [CrossRef]
- Himmelgreen, D.; Romero-Daza, N.; Heuer, J.; Lucas, W.; Salinas-Miranda, A.A.; Stoddard, T. Using syndemic theory to understand food insecurity and diet-related chronic diseases. Soc. Sci. Med. 2020, 295, 113124. [Google Scholar] [CrossRef]
- Ziliak, J.; Gundersen, C. The Health Consequences of Senior Hunger in the United States: Evidence from the 1999–2014 NHANES. 2017. Available online: https://www.feedingamerica.org/sites/default/files/research/senior-hunger-research/senior-health-consequences-2014.pdf (accessed on 1 December 2021).
- Schwartz, N.; Buliung, R.; Wilson, K. Disability and food access and insecurity: A scoping review of the literature. Health Place 2019, 57, 107–121. [Google Scholar] [CrossRef]
- Blake, C.E.; Frongillo, E.A.; Warren, A.M.; Constantinides, S.V.; Rampalli, K.K.; Bhandari, S. Elaborating the science of food choice for rapidly changing food systems in low-and middle-income countries. Glob. Food Secur. 2021, 28, 100503. [Google Scholar] [CrossRef]
- Bradley, S.; Vitous, C.A.; Walsh-Felz, A.; Himmelgreen, D. Food insecurity and healthcare decision making among mobile food pantry clients in Tampa Bay. Ecol. Food Nutr. 2018, 57, 206–222. [Google Scholar] [CrossRef] [PubMed]
- Feeding America. Overall (All Ages) Hunger & Poverty in the United States|Map the Meal Gap. 2020. Available online: https://map.feedingamerica.org/ (accessed on 18 August 2022).
- Lock, S.L.; Baumgart, M.; Whiting, C.G.; McGuire, L.C.; Iskander, J.K.; Thorpe, P.; Laird, S. Healthy Aging: Promoting Well-Being in Older Adults; Public Health Grand Rounds; US Department of Health and Human Services: Washington, DC, USA, 19 September 2017. Available online: https://stacks.cdc.gov/view/cdc/48335 (accessed on 1 December 2021).
- Boersma, P.; Black, L.I.; Ward, B.W. Prevalence of Multiple Chronic Conditions Among US Adults, 2018. Prev. Chronic Dis. 2020, 17, E106. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, J.L. Hunger in Older Adults: Challenges and Opportunities for the Aging Services Network. 2017. Available online: https://www.mealsonwheelsamerica.org/docs/default-source/research/hungerinolderadults-fullreport-feb2017.pdf?sfvrsn=2 (accessed on 10 March 2021).
- McLaughlin, D.; Vagenas, D.; Pachana, N.A.; Begum, N.; Dobson, A. Gender differences in social network size and satisfaction in adults in their 70s. J. Health Psychol. 2010, 15, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Burris, M.; Kihlstrom, L.; Arce, K.S.; Prendergast, K.; Dobbins, J.; McGrath, E.; Renda, A.; Shannon, E.; Cordier, T.; Song, Y.; et al. Food Insecurity, Loneliness, and Social Support among Older Adults. J. Hunger Environ. Nutr. 2019, 16, 29–44. [Google Scholar] [CrossRef]
- Hanna, K.L.; Collins, P.F. Relationship between living alone and food and nutrient intake. Nutr. Rev. 2015, 73, 594–611. [Google Scholar] [CrossRef]
- Pilgrim, A.L.; Robinson, S.M.; Sayer, A.A.; Roberts, H.C. An overview of appetite decline in older people. Nurs. Older People 2015, 27, 29. [Google Scholar] [CrossRef]
- Henning-Smith, C.; Ecklund, A.; Lahr, M.; Evenson, A.; Mozcovice, I.; Kozhimannil, K. Key Informant Perspectives on Rural Social Isolation and Loneliness. 2018. Available online: http://rhrc.umn.edu/wpcontent/files_mf/1539002382UMNpolicybriefKeyInformantPerspectivesonRuralSocialIsolationandLoneliness.pdf (accessed on 20 November 2022).
- Host, A.; McMahon, A.T.; Walton, K.; Charlton, K. Factors Influencing Food Choice for Independently Living Older People—A Systematic Literature Review. J. Nutr. Gerontol. Geriat. 2016, 35, 67–94. [Google Scholar] [CrossRef]
- Strogatz, D.; Mielenz, T.J.; Johnson, A.K.; Baker, I.R.; Robinson, M.; Mebust, S.P.; Andrews, H.F.; Betz, M.E.; Eby, D.W.; Johnson, R.M.; et al. Importance of Driving and Potential Impact of Driving Cessation for Rural and Urban Older Adults. J. Rural Health 2020, 36, 88–93. [Google Scholar] [CrossRef]
- Nicholson, N.R. A review of social isolation: An important but underassessed condition in older adults. J. Prim. Prev. 2012, 33, 137–152. [Google Scholar] [CrossRef]
- US Census Bureau. QuickFacts. 2020. Available online: https://www.census.gov/quickfacts/fact/table/orangecountyindiana,lawrencecountyindiana,greenecountyindiana,crawfordcountyindiana,US/PST045221 (accessed on 14 January 2021).
- USDA Economic Research Service. U.S. Household Food Security Survey Module: Six-Item Short Form. September 2012. Available online: https://www.ers.usda.gov/media/8271/hh2012.pdf (accessed on 14 January 2019).
- CDC. CDC HRQOL-14 “Healthy Days Measure”. 2018. Available online: https://www.cdc.gov/hrqol/hrqol14_measure.htm#1 (accessed on 6 December 2021).
- Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Cacioppo, J.T. A Short Scale for Measuring Loneliness in Large Surveys: Results From Two Population-Based Studies. Res. Aging 2004, 26, 655. [Google Scholar] [CrossRef]
- Jeon, J. The Strengths and Limitations of the Statistical Modeling of Complex Social Phenomenon: Focusing on SEM, Path Analysis, or Multiple Regression Models. Int. Sci. Index Econ. Manag. Eng. 2015, 9, 1634–1642. [Google Scholar]
- Ankuda, C.K.; Fogel, J.; Kelley, A.S.; Byhoff, E. Patterns of Material Hardship and Food Insecurity Among Older Adults During the COVID-19 Pandemic. J. Gen. Intern. Med. 2021, 36, 3639–3641. [Google Scholar] [CrossRef] [PubMed]
- FSSA: Family and Social Services Administration. Important Information about Pandemic-Related Emergency SNAP Benefits. Available online: https://www.in.gov/fssa/dfr/ebt-hoosier-works-card/find-my-local-dfr-office/important-information-about-the-transition-from-pandemic-related-emergency-snap-benefits/ (accessed on 24 August 2022).
- Reeder, N.; Tolar-Peterson, T.; Bailey, R.H.; Cheng, W.-H.; Evans, M.W. Food Insecurity and Depression among US Adults: NHANES 2005-2016. Nutrients 2022, 14, 3081. [Google Scholar] [CrossRef] [PubMed]
- Owen, A.J.; Tran, T.; Hammarberg, K.; Kirkman, M.; Fisher, J.R.W. Poor appetite and overeating reported by adults in Australia during the coronavirus-19 disease pandemic: A population-based study. Public Health Nutr. 2021, 24, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Rothenberg, E. Coronavirus Disease 19 from the Perspective of Ageing with Focus on Nutritional Status and Nutrition Management—A Narrative Review. Nutrients 2021, 13, 1294. [Google Scholar] [CrossRef]
- Gundersen, C.; Seligman, H.K. Food insecurity and health outcomes. Econ. Voice 2017, 14, 20170004. [Google Scholar] [CrossRef]
- McClintock, H.F.; Imel, B.E. Food insecurity and medication restricting behavior among persons with diabetes in the United States. Nutr. Health 2022. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness Matters: A Theoretical and Empirical Review of Consequences and Mechanisms. Ann. Behav. Med. 2010, 40, 218–227. [Google Scholar] [CrossRef]
- Schorr, A.V.; Yehuda, I.; Tamir, S. Loneliness, Malnutrition and Change in Subjective Age among Older Adults during COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 18, 106. [Google Scholar] [CrossRef]
- Visser, M.; Schaap, L.A.; Wijnhoven, H.A.H. Self-Reported Impact of the COVID-19 Pandemic on Nutrition and Physical Activity Behaviour in Dutch Older Adults Living Independently. Nutrients 2020, 12, 3708. [Google Scholar] [CrossRef]
- Fiorenzato, E.; Zabberoni, S.; Costa, A.; Cona, G. Cognitive and mental health changes and their vulnerability factors related to COVID-19 lockdown in Italy. PLoS ONE 2021, 16, e0246204. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, W.S.; Frongillo, E.A.; Valois, P. Understanding the experience of food insecurity by elders suggests ways to improve its measurement. J. Nutr. 2003, 133, 2762–2769. [Google Scholar] [CrossRef] [PubMed]
- Quandt, S.A.; Arcury, T.A.; McDonald, J.; Bell, R.A.; Vitolins, M.Z. Meaning and Management of Food Security Among Rural Elders. J. Appl. Gerontol. 2001, 20, 356–376. [Google Scholar] [CrossRef]
- Frost, M.; Wraae, K.; Gudex, C.; Nielsen, T.; Brixen, K.; Hagen, C.; Andersen, M. Chronic diseases in elderly men: Underreporting and underdiagnosis. Age Ageing 2012, 41, 177–183. [Google Scholar] [CrossRef]
- Schmier, J.; Halpern, M.T. Patient recall and recall bias of health state and health status. Expert Rev. Pharm. Outcomes Res. 2004, 4, 159–163. [Google Scholar] [CrossRef] [PubMed]

| County | % Adults Age 60+ | Median Household Income | Poverty Rate | Food Insecurity Rate 2019 | Food Insecurity Rate 2020 | Below 130% Poverty |
|---|---|---|---|---|---|---|
| Crawford | 20.10% | $41,662 | 16.50% | 16.1% | 15.4% | 61% |
| Greene | 19.80% | $51,613 | 13.50% | 14.2% | 13.3% | 53% |
| Lawrence | 20.60% | $53,610 | 10.50% | 13.6% | 12.3% | 49% |
| Orange | 19.80% | $47,917 | 14.10% | 15.4% | 16.3% | 51% |
| Variable | Definition |
|---|---|
| Age | Numerical variable defining age of respondent in years. |
| Gender | Categorical variable defining respondent gender (0 = male; 1 = female). No respondents identified as anything other than male or female. |
| Marital Status | Categorical variable defining marital status (1 = married or living with a partner; 0 = widowed, divorced, separated, or never married). |
| Income | Ordinal variable defining respondent’s household monthly income class before COVID in USD. (0 = less than $1000; 1 = $1001–$1500; 2 = $1501–$2000; 3 = $2001–$2500; 4 = $2501–$3000; 5 = $3001–$3500; 6 = $3501–$4000; 7 = $4001–$4500; 8 = greater than $4500). |
| Travel Time | Numerical variable defining total one-way household travel time to supermarkets, grocery stores, or other stores accepting SNAP in the study region and counties bordering the study region. |
| Eats with Others | Ordinal variable defining the frequency of eating with others (4 = always; 3 = sometimes; 2 = half the time; 1 = seldom; 0 = never). |
| Food Security (FS) | Numerical variable reflecting the inverse of the total score of the respondent on the U.S. Six-Item Food Security Survey Module. The unadjusted scores range from 0 to 6, and the scale scores (used for statistical procedures based on the USDA guidelines) range from 0 to 8.48. For this analysis, 8.48 indicates the highest level of food security, and 0 indicates the lowest level of food security. |
| Physical Health (H) | Numerical value denoting the number of physically healthy days out of the past 30 days reported by the respondent. This is indexed by the inverse answer to the first question of the HRQOL-4 which asks, “Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?”. We subtracted the response from 30. |
| Absence of Loneliness (AL) | Ordinal variable reflecting the inverse of the sum of the Three-Item Loneliness Scale. This score ranges from 3–9, with 3 indicating the most loneliness and 9 indicating no loneliness. |
| Variable | % or | Variable | % or |
|---|---|---|---|
| Gender | |||
| Female | 71.16% | Male | 28.84% |
| White/Caucasian | 96.5% | ||
| Age | 71.11 | ||
| Education | |||
| Less than high school | 2.10% | Some college | 22.54% |
| Some high school | 4.36% | College degree | 14.65% |
| High school diploma/GED | 38.32% | Post-college degree | 11.12% |
| Trade certification | 6.91% | ||
| Marital Status | |||
| Married or living with partner | 65.31% | Divorced or separated | 11.18% |
| Widowed | 20.51% | Never married | 2.99% |
| Variable | Before COVID | During COVID | P |
|---|---|---|---|
| Monthly Income | 0.000 | ||
| ≤$1000 | 7.13% | 8.28% | |
| $1001–$1500 | 13.61% | 15.25% | |
| $1501–$2000 | 12.64% | 12.21% | |
| $2001–$2500 | 11.35% | 11.15% | |
| $2501–$3000 | 9.89% | 9.59% | |
| $3001–$3500 | 8.27% | 8.52% | |
| $3501–$4000 | 7.78% | 6.64% | |
| $4001–$4500 | 8.91% | 8.69% | |
| >$4500 | 20.42% | 19.67% | |
| SNAP Participation | 2.63% | 4.56% | 0.000 |
| Household Size | 1.62 | 1.63 | 0.795 |
| Eats with Others | 0.000 | ||
| Never | 6.49% | 40.72% | |
| Seldom | 47.07% | 35.86% | |
| Half the time | 22.57% | 5.35% | |
| Sometimes | 13.60% | 8.90% | |
| Always | 10.28% | 9.17% | |
| Travel Times (minutes, one-way) | 16.65 | 17.03 | 0.361 |
| Food Security Scale Score | 8.19 | 8.15 | 0.019 |
| Food Insecure | 12.56% | 13.28% | 0.000 |
| Physically Healthy Days (out of the past 30 days) | 25.59 | 25.13 | 0.000 |
| (Absence of) Loneliness Score | 8.16 | 7.31 | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Howe-Burris, M.; Giroux, S.; Waldman, K.; DeBruicker Valliant, J.; Babb, A.; Czebotar, K.; Fobi, D.; Stafford, P.; Knudsen, D.C. The Interactions of Food Security, Health, and Loneliness among Rural Older Adults before and after the Onset of COVID-19. Nutrients 2022, 14, 5076. https://doi.org/10.3390/nu14235076
Howe-Burris M, Giroux S, Waldman K, DeBruicker Valliant J, Babb A, Czebotar K, Fobi D, Stafford P, Knudsen DC. The Interactions of Food Security, Health, and Loneliness among Rural Older Adults before and after the Onset of COVID-19. Nutrients. 2022; 14(23):5076. https://doi.org/10.3390/nu14235076
Chicago/Turabian StyleHowe-Burris, Mecca, Stacey Giroux, Kurt Waldman, Julia DeBruicker Valliant, Angela Babb, Kamila Czebotar, Daniel Fobi, Phil Stafford, and Daniel C. Knudsen. 2022. "The Interactions of Food Security, Health, and Loneliness among Rural Older Adults before and after the Onset of COVID-19" Nutrients 14, no. 23: 5076. https://doi.org/10.3390/nu14235076
APA StyleHowe-Burris, M., Giroux, S., Waldman, K., DeBruicker Valliant, J., Babb, A., Czebotar, K., Fobi, D., Stafford, P., & Knudsen, D. C. (2022). The Interactions of Food Security, Health, and Loneliness among Rural Older Adults before and after the Onset of COVID-19. Nutrients, 14(23), 5076. https://doi.org/10.3390/nu14235076






