Change in Diet Quality and Meal Sources during the COVID-19 Pandemic in a Diverse Subset of Men and Women in the Cancer Prevention Study-3
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Assessment of Dietary Changes
2.3. Statistical Analysis
3. Results
3.1. Participants’ Sociodemographic Characteristics
3.2. Change in Diet Quality
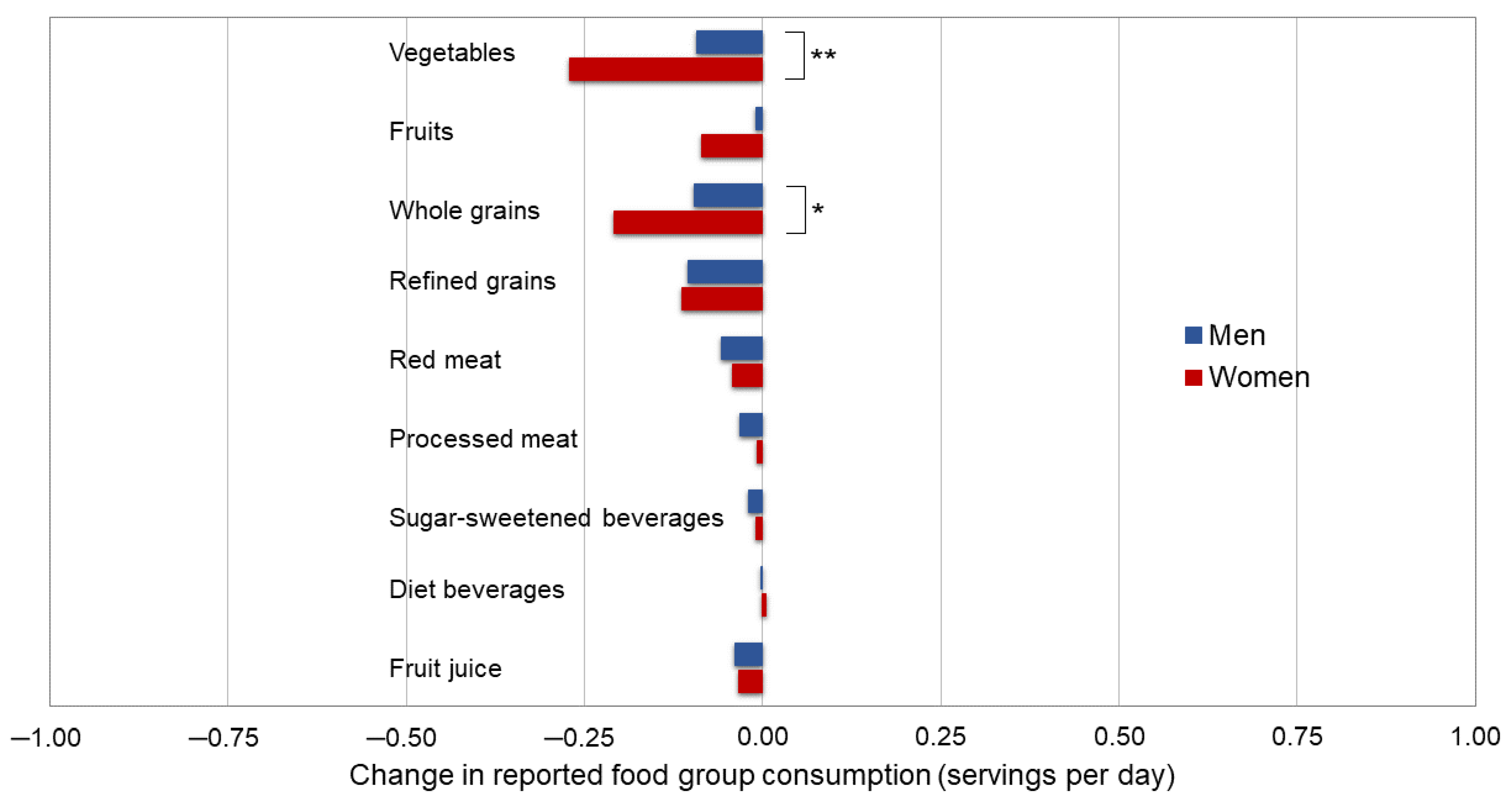
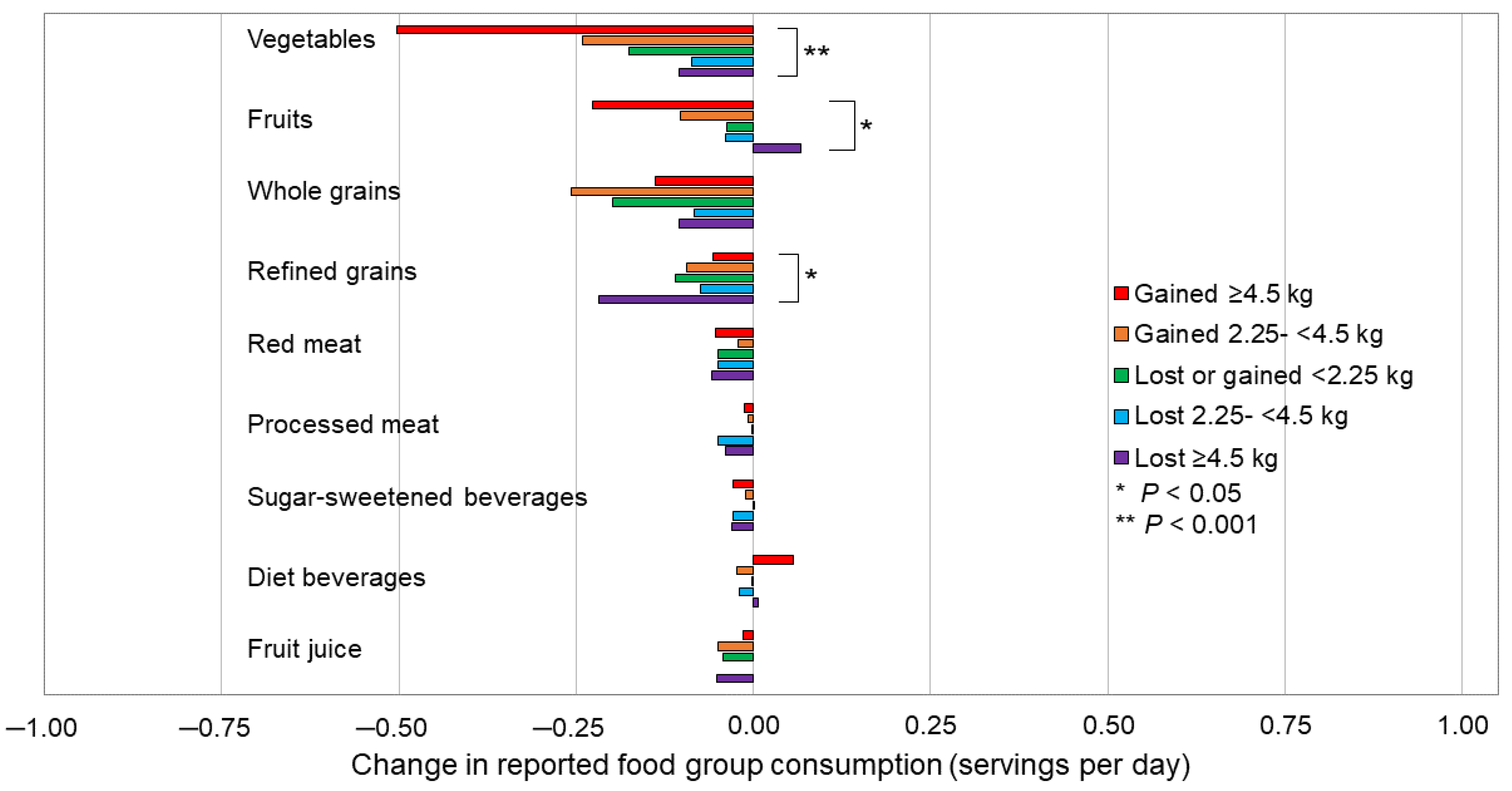
Change in Diet Quality among Subgroups
3.3. Perceived Change in Dietary Intake
3.4. Change in Meal Source
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 23 January 2023).
- Centers for Disease Control and Prevention. COVID Data Tracker. Available online: https://www.cdc.gov/coronavirus/2019-nCoV/index.html (accessed on 23 January 2023).
- Taylor, S. Understanding and managing pandemic-related panic buying. J. Anxiety Disord. 2021, 78, 102364. [Google Scholar] [CrossRef] [PubMed]
- Boyaciota-Gunduz, C.P.; Ibrahim, S.A.; Wei, O.C.; Galanakis, C.M. Transformation of the Food Sector: Security and Resilience during the COVID-19 Pandemic. Foods 2021, 10, 497. [Google Scholar] [CrossRef] [PubMed]
- Mead, D.; Ransom, K.; Reed, S.; Sager, S. The Impact of the COVID-19 Pandemic on Food Price Indexes and Data Collection; U.S. Bureau of Labor Statistics: Washington, DC, USA, 2020. [Google Scholar]
- International Labour Organization. ILO Monitor on the World of Work (ILOMONITOR), ILOSTAT. Available online: https://ilostat.ilo.org/topics/covid-19/# (accessed on 23 January 2023).
- Falk, G.; Carter, J.; Nicchitta, I.; Nyhof, E.; Romero, P. Unemployment Rates during the COVID-19 Pandemic: In Brief; R46554; U.S. Congressional Research Service: Washington, DC, USA, 2021. [Google Scholar]
- Soric, T.; Brodic, I.; Mertens, E.; Sagastume, D.; Dolanc, I.; Jonjic, A.; Delale, E.A.; Mavar, M.; Missoni, S.; Penalvo, J.L.; et al. Evaluation of the Food Choice Motives before and during the COVID-19 Pandemic: A Cross-Sectional Study of 1232 Adults from Croatia. Nutrients 2021, 13, 3165. [Google Scholar] [CrossRef]
- Brady, P.J.; Askelson, N.M.; Thompson, H.; Kersten, S.; Hopkins, H.; Ashida, S.; Nothwehr, F.; Janssen, B.; Frisvold, D. A Qualitative Study of Factors Influencing Food Choices and Food Sources Among Adults Aged 50 Years and Older During the Coronavirus Disease 2019 Pandemic. J. Acad. Nutr. Diet. 2022, in press. [Google Scholar] [CrossRef]
- Mertens, E.; Sagastume, D.; Soric, T.; Brodic, I.; Dolanc, I.; Jonjic, A.; Delale, E.A.; Mavar, M.; Missoni, S.; Coklo, M.; et al. Food Choice Motives and COVID-19 in Belgium. Foods 2022, 11, 842. [Google Scholar] [CrossRef]
- Liboredo, J.C.; Anastacio, L.R.; Ferreira, L.G.; Oliveira, L.A.; Della Lucia, C.M. Quarantine During COVID-19 Outbreak: Eating Behavior, Perceived Stress, and Their Independently Associated Factors in a Brazilian Sample. Front. Nutr. 2021, 8, 704619. [Google Scholar] [CrossRef] [PubMed]
- McAtamney, K.; Mantzios, M.; Egan, H.; Wallis, D.J. Emotional eating during COVID-19 in the United Kingdom: Exploring the roles of alexithymia and emotion dysregulation. Appetite 2021, 161, 105120. [Google Scholar] [CrossRef]
- Hadar-Shoval, D.; Alon-Tirosh, M.; Asraf, K.; Tannous-Haddad, L.; Tzischinsky, O. Lifestyle Changes, Emotional Eating, Gender, and Stress during COVID-19 Lockdown. Nutrients 2022, 14, 3868. [Google Scholar] [CrossRef]
- Rodriguez-Perez, C.; Molina-Montes, E.; Verardo, V.; Artacho, R.; Garcia-Villanova, B.; Guerra-Hernandez, E.J.; Ruiz-Lopez, M.D. Changes in Dietary Behaviours during the COVID-19 Outbreak Confinement in the Spanish COVIDiet Study. Nutrients 2020, 12, 1730. [Google Scholar] [CrossRef]
- Bhutani, S.; Cooper, J.A.; vanDellen, M.R. Self-reported Changes in Energy Balance Behaviors during COVID-19-related Home Confinement: A Cross-sectional Study. Am. J. Health Behav. 2021, 45, 756–770. [Google Scholar] [CrossRef]
- Imaz-Aramburu, I.; Fraile-Bermudez, A.B.; Martin-Gamboa, B.S.; Cepeda-Miguel, S.; Doncel-Garcia, B.; Fernandez-Atutxa, A.; Irazusta, A.; Zarrazquin, I. Influence of the COVID-19 Pandemic on the Lifestyles of Health Sciences University Students in Spain: A Longitudinal Study. Nutrients 2021, 13, 1958. [Google Scholar] [CrossRef] [PubMed]
- Steele, E.M.; Rauber, F.; Costa, C.D.S.; Leite, M.A.; Gabe, K.T.; Louzada, M.; Levy, R.B.; Monteiro, C.A. Dietary changes in the NutriNet Brasil cohort during the covid-19 pandemic. Rev. Saude Publica 2020, 54, 91. [Google Scholar] [CrossRef] [PubMed]
- Husain, W.; Ashkanani, F. Does COVID-19 change dietary habits and lifestyle behaviours in Kuwait: A community-based cross-sectional study. Environ. Health Prev. Med. 2020, 25, 61. [Google Scholar] [CrossRef] [PubMed]
- Bracale, R.; Vaccaro, C.M. Changes in food choice following restrictive measures due to COVID-19. Nutr. Metab. Cardiovasc. Dis. NMCD 2020, 30, 1423–1426. [Google Scholar] [CrossRef]
- Deschasaux-Tanguy, M.; Druesne-Pecollo, N.; Esseddik, Y.; de Edelenyi, F.S.; Alles, B.; Andreeva, V.A.; Baudry, J.; Charreire, H.; Deschamps, V.; Egnell, M.; et al. Diet and physical activity during the coronavirus disease 2019 (COVID-19) lockdown (March–May 2020): Results from the French NutriNet-Sante cohort study. Am. J. Clin. Nutr. 2021, 113, 924–938. [Google Scholar] [CrossRef]
- Matsungo, T.M.; Chopera, P. Effect of the COVID-19-induced lockdown on nutrition, health and lifestyle patterns among adults in Zimbabwe. BMJ Nutr. Prev. Health 2020, 3, 205–212. [Google Scholar] [CrossRef]
- Mitchell, E.S.; Yang, Q.; Behr, H.; Deluca, L.; Schaffer, P. Adherence to healthy food choices during the COVID-19 pandemic in a U.S. population attempting to lose weight. Nutr. Metab. Cardiovasc. Dis. NMCD 2021, 31, 2165–2172. [Google Scholar] [CrossRef]
- Naughton, F.; Ward, E.; Khondoker, M.; Belderson, P.; Marie Minihane, A.; Dainty, J.; Hanson, S.; Holland, R.; Brown, T.; Notley, C. Health behaviour change during the UK COVID-19 lockdown: Findings from the first wave of the C-19 health behaviour and well-being daily tracker study. Br. J. Health Psychol. 2021, 26, 624–643. [Google Scholar] [CrossRef]
- Sato, K.; Kobayashi, S.; Yamaguchi, M.; Sakata, R.; Sasaki, Y.; Murayama, C.; Kondo, N. Working from home and dietary changes during the COVID-19 pandemic: A longitudinal study of health app (CALO mama) users. Appetite 2021, 165, 105323. [Google Scholar] [CrossRef]
- Romeo-Arroyo, E.; Mora, M.; Vazquez-Araujo, L. Consumer behavior in confinement times: Food choice and cooking attitudes in Spain. Int. J. Gastron. Food Sci. 2020, 21, 100226. [Google Scholar] [CrossRef]
- Scarmozzino, F.; Visioli, F. COVID-19 and the Subsequent Lockdown Modified Dietary Habits of Almost Half the Population in an Italian Sample. Foods 2020, 9, 675. [Google Scholar] [CrossRef] [PubMed]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef] [PubMed]
- Gallo, L.A.; Gallo, T.F.; Young, S.L.; Moritz, K.M.; Akison, L.K. The Impact of Isolation Measures Due to COVID-19 on Energy Intake and Physical Activity Levels in Australian University Students. Nutrients 2020, 12, 1865. [Google Scholar] [CrossRef] [PubMed]
- Pellegrini, M.; Ponzo, V.; Rosato, R.; Scumaci, E.; Goitre, I.; Benso, A.; Belcastro, S.; Crespi, C.; De Michieli, F.; Ghigo, E.; et al. Changes in Weight and Nutritional Habits in Adults with Obesity during the “Lockdown” Period Caused by the COVID-19 Virus Emergency. Nutrients 2020, 12, 2016. [Google Scholar] [CrossRef] [PubMed]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef] [PubMed]
- Zachary, Z.; Brianna, F.; Brianna, L.; Garrett, P.; Jade, W.; Alyssa, D.; Mikayla, K. Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obes. Res. Clin. Pract. 2020, 14, 210–216. [Google Scholar] [CrossRef]
- Maffoni, S.; Brazzo, S.; De Giuseppe, R.; Biino, G.; Vietti, I.; Pallavicini, C.; Cena, H. Lifestyle Changes and Body Mass Index during COVID-19 Pandemic Lockdown: An Italian Online-Survey. Nutrients 2021, 13, 1117. [Google Scholar] [CrossRef]
- Czenczek-Lewandowska, E.; Wyszynska, J.; Leszczak, J.; Baran, J.; Weres, A.; Mazur, A.; Lewandowski, B. Health behaviours of young adults during the outbreak of the Covid-19 pandemic—A longitudinal study. BMC Public Health 2021, 21, 1038. [Google Scholar] [CrossRef]
- Hosomi, Y.; Munekawa, C.; Hashimoto, Y.; Okamura, T.; Takahashi, F.; Kawano, R.; Nakajima, H.; Majima, S.; Senmaru, T.; Nakanishi, N.; et al. The effect of COVID-19 pandemic on the lifestyle and glycemic control in patients with type 1 diabetes: A retrospective cohort study. Diabetol. Int. 2022, 13, 85–90. [Google Scholar] [CrossRef]
- Barone Gibbs, B.; Kline, C.E.; Huber, K.A.; Paley, J.L.; Perera, S. COVID-19 shelter-at-home and work, lifestyle and well-being in desk workers. Occup. Med. 2021, 71, 86–94. [Google Scholar] [CrossRef]
- Khubchandani, J.; Kandiah, J.; Saiki, D. The COVID-19 Pandemic, Stress, and Eating Practices in the United States. Eur. J. Investig. Health Psychol. Educ. 2020, 10, 950–956. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.V.; Jacobs, E.J.; Dudas, D.M.; Briggs, P.J.; Lichtman, C.J.; Bain, E.B.; Stevens, V.L.; McCullough, M.L.; Teras, L.R.; Campbell, P.T.; et al. The American Cancer Society’s Cancer Prevention Study 3 (CPS-3): Recruitment, study design, and baseline characteristics. Cancer 2017, 123, 2014–2024. [Google Scholar] [CrossRef] [PubMed]
- Troeschel, A.N.; Hartman, T.J.; Flanders, W.D.; Wang, Y.; Hodge, R.A.; McCullough, L.E.; Mitchell, D.C.; Sampson, L.; Patel, A.V.; McCullough, M.L. The American Cancer Society Cancer Prevention Study-3 FFQ Has Reasonable Validity and Reproducibility for Food Groups and a Diet Quality Score. J. Nutr. 2020, 150, 1566–1578. [Google Scholar] [CrossRef] [PubMed]
- McCullough, M.L.; Wang, Y.; Hartman, T.J.; Hodge, R.A.; Flanders, W.D.; Stevens, V.L.; Sampson, L.; Mitchell, D.C.; Patel, A.V. The Cancer Prevention Study-3 FFQ Is a Reliable and Valid Measure of Nutrient Intakes among Racial/Ethnic Subgroups, Compared with 24-Hour Recalls and Biomarkers. J. Nutr. 2021, 151, 636–648. [Google Scholar] [CrossRef]
- Kushi, L.H.; Doyle, C.; McCullough, M.; Rock, C.L.; Demark-Wahnefried, W.; Bandera, E.V.; Gapstur, S.; Patel, A.V.; Andrews, K.; Gansler, T.; et al. American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: Reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J. Clin. 2012, 62, 30–67. [Google Scholar] [CrossRef] [PubMed]
- Rees-Punia, E.; Newton, C.C.; Westmaas, J.L.; Chantaprasopsuk, S.; Patel, A.V.; Leach, C.R. Prospective COVID-19 related changes in physical activity and sedentary time and associations with symptoms of depression and anxiety. Ment. Health Phys. Act. 2021, 21, 100425. [Google Scholar] [CrossRef]
- Leach, C.R.; Rees-Punia, E.; Newton, C.C.; Chantaprasopsuk, S.; Patel, A.V.; Westmaas, J.L. Stressors and Other Pandemic-related Predictors of Prospective Changes in Psychological Distress. Lancet Reg. Health Am. 2021, 4, 100069. [Google Scholar] [CrossRef]
- Rees-Punia, E.; Newton, C.C.; Rittase, M.H.; Hodge, R.A.; Nielsen, J.; Cunningham, S.; Teras, L.R.; Patel, A. Prospective changes in physical activity, sedentary time and sleep during the COVID-19 pandemic in a US-based cohort study. BMJ Open 2021, 11, e053817. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Rock, C.L.; Thomson, C.; Gansler, T.; Gapstur, S.M.; McCullough, M.L.; Patel, A.V.; Andrews, K.S.; Bandera, E.V.; Spees, C.K.; Robien, K.; et al. American Cancer Society guideline for diet and physical activity for cancer prevention. CA Cancer J. Clin. 2020, 70, 245–271. [Google Scholar] [CrossRef]
- Gundersen, C.; Engelhard, E.E.; Crumbaugh, A.S.; Seligman, H.K. Brief assessment of food insecurity accurately identifies high-risk US adults. Public Health Nutr. 2017, 20, 1367–1371. [Google Scholar] [CrossRef] [PubMed]
- Pereira, M.A.; O’Reilly, E.; Augustsson, K.; Fraser, G.E.; Goldbourt, U.; Heitmann, B.L.; Hallmans, G.; Knekt, P.; Liu, S.; Pietinen, P.; et al. Dietary fiber and risk of coronary heart disease: A pooled analysis of cohort studies. Arch. Intern. Med. 2004, 164, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Threapleton, D.E.; Greenwood, D.C.; Evans, C.E.; Cleghorn, C.L.; Nykjaer, C.; Woodhead, C.; Cade, J.E.; Gale, C.P.; Burley, V.J. Dietary fibre intake and risk of cardiovascular disease: Systematic review and meta-analysis. BMJ 2013, 347, f6879. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, A.; Mann, J.; Cummings, J.; Winter, N.; Mete, E.; Te Morenga, L. Carbohydrate quality and human health: A series of systematic reviews and meta-analyses. Lancet 2019, 393, 434–445. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Chan, D.S.; Lau, R.; Vieira, R.; Greenwood, D.C.; Kampman, E.; Norat, T. Dietary fibre, whole grains, and risk of colorectal cancer: Systematic review and dose-response meta-analysis of prospective studies. BMJ 2011, 343, d6617. [Google Scholar] [CrossRef] [PubMed]
- Bennett, G.; Young, E.; Butler, I.; Coe, S. The Impact of Lockdown During the COVID-19 Outbreak on Dietary Habits in Various Population Groups: A Scoping Review. Front. Nutr. 2021, 8, 626432. [Google Scholar] [CrossRef]
- Gonzalez-Monroy, C.; Gomez-Gomez, I.; Olarte-Sanchez, C.M.; Motrico, E. Eating Behaviour Changes during the COVID-19 Pandemic: A Systematic Review of Longitudinal Studies. Int. J. Environ. Res. Public Health 2021, 18, 11130. [Google Scholar] [CrossRef]
- Lamarche, B.; Brassard, D.; Lapointe, A.; Laramee, C.; Kearney, M.; Cote, M.; Belanger-Gravel, A.; Desroches, S.; Lemieux, S.; Plante, C. Changes in diet quality and food security among adults during the COVID-19-related early lockdown: Results from NutriQuebec. Am. J. Clin. Nutr. 2021, 113, 984–992. [Google Scholar] [CrossRef]
- Marty, L.; de Lauzon-Guillain, B.; Labesse, M.; Nicklaus, S. Food choice motives and the nutritional quality of diet during the COVID-19 lockdown in France. Appetite 2021, 157, 105005. [Google Scholar] [CrossRef]
- Pfeifer, D.; Resetar, J.; Gajdos Kljusuric, J.; Panjkota Krbavcic, I.; Vranesic Bender, D.; Rodriguez-Perez, C.; Ruiz-Lopez, M.D.; Satalic, Z. Cooking at Home and Adherence to the Mediterranean Diet During the COVID-19 Confinement: The Experience From the Croatian COVIDiet Study. Front. Nutr. 2021, 8, 617721. [Google Scholar] [CrossRef]
- Szymczak, H.; Keller, L.; Debbeler, L.J.; Kollmann, J.; Lages, N.C.; Sproesser, G.; Gollwitzer, P.M.; Schupp, H.T.; Renner, B. “I’m eating healthy now”: The relationship between perceived behavior change and diet. Food Qual. Prefer. 2021, 89, 104142. [Google Scholar] [CrossRef]
- Variyam, J.N.; Shim, Y.; Blaylock, J. Consumer misperceptions of diet quality. J. Nutr. Educ. 2001, 33, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Powell-Wiley, T.M.; Miller, P.E.; Agyemang, P.; Agurs-Collins, T.; Reedy, J. Perceived and objective diet quality in US adults: A cross-sectional analysis of the National Health and Nutrition Examination Survey (NHANES). Public Health Nutr. 2014, 17, 2641–2649. [Google Scholar] [CrossRef] [PubMed]
- Special Report, America Gets Cooking: The Impact of COVID-19 on Americans’; Food Habits; HUNTER: Hunter Region, Australia, 2020; Available online: https://www.slideshare.net/HUNTERNY/hunter-food-study-special-report-america-gets-cooking-231713331 (accessed on 17 March 2021).
- Special Report Wave Two, America Keeps on Cooking: The Impact of COVID-19 on Americans’; Food Habits; HUNTER: Hunter Region, Australia, 2021; Available online: https://www.slideshare.net/HUNTERNY/hunter-food-study-special-report-wave-two-america-keeps-on-cooking-241251030 (accessed on 17 March 2021).
- Almandoz, J.P.; Xie, L.; Schellinger, J.N.; Mathew, M.S.; Gazda, C.; Ofori, A.; Kukreja, S.; Messiah, S.E. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin. Obes. 2020, 10, e12386. [Google Scholar] [CrossRef]
- Farmer, N.; Wallen, G.R.; Yang, L.; Middleton, K.R.; Kazmi, N.; Powell-Wiley, T.M. Household Cooking Frequency of Dinner Among Non-Hispanic Black Adults is Associated with Income and Employment, Perceived Diet Quality and Varied Objective Diet Quality, HEI (Healthy Eating Index): NHANES Analysis 2007–2010. Nutrients 2019, 11, 2057. [Google Scholar] [CrossRef]
- U.S. Census Bureau QuickFacts. Available online: https://www.census.gov/quickfacts/fact/table/US/LFE046221 (accessed on 23 January 2023).
- Semega, J.K.M. Income in the United States: 2021; U.S. Census Bureau, Current Population Reports; U.S. Government Publishing Office: Washington, DC, USA, 2022; pp. 60–276. [Google Scholar]
- Coleman-Jensen, A.; Rabbitt, M.P.; Gregory, C.A.; Singh, A. Household Food Security in the United States in 2021, ERR-309; U.S. Department of Agriculture, Economic Research Service: Washington, DC, USA, 2022. [Google Scholar]
- Hodge, J.M.; Shah, R.; McCullough, M.L.; Gapstur, S.M.; Patel, A.V. Validation of self-reported height and weight in a large, nationwide cohort of U.S. adults. PLoS ONE 2020, 15, e0231229. [Google Scholar] [CrossRef]
| Overall | Change in Diet Quality Score 1 | ||||
|---|---|---|---|---|---|
| Improved | No Change | Declined | p3 | ||
| N = 2335 2 | N = 1041 2 | N = 382 2 | N = 912 2 | ||
| Change in diet score | 0.2 (2.8) | 2.6 (1.7) | 0.0 (0.0) | −2.4 (1.6) | <0.001 |
| Range | −10 to 13 | 1 to 13 | 0 | −10 to −1 | |
| Age, years | 55.6 (9.7) | 55.8 (9.5) | 56.1 (9.6) | 55.1 (9.9) | 0.20 |
| Sex | 0.12 | ||||
| Male | 816 | 385 (47%) | 134 (16%) | 297 (36%) | |
| Female | 1519 | 656 (43%) | 248 (16%) | 615 (40%) | |
| Race/Ethnicity | 0.18 | ||||
| White | 1777 | 806 (45%) | 294 (17%) | 677 (38%) | |
| Latino/a | 298 | 118 (40%) | 50 (17%) | 130 (44%) | |
| Asian/Pacific Islander | 88 | 40 (45%) | 12 (14%) | 36 (41%) | |
| Black | 81 | 43 (53%) | 7 (8.6%) | 31 (38%) | |
| American Indian/Alaskan Native | 44 | 13 (30%) | 9 (20%) | 22 (50%) | |
| Other/missing | 47 | 21 (45%) | 10 (21%) | 16 (34%) | |
| Education | 0.38 | ||||
| <4-year college | 516 | 229 (44%) | 76 (15%) | 211 (41%) | |
| College graduate | 872 | 406 (47%) | 137 (16%) | 329 (38%) | |
| Graduate school | 947 | 406 (43%) | 169 (18%) | 372 (39%) | |
| Household income in 2018 | 0.76 | ||||
| <$50,000 | 228 | 105 (46%) | 35 (15%) | 88 (39%) | |
| $50,000–$99,999 | 701 | 319 (46%) | 110 (16%) | 272 (39%) | |
| $100,000–$149,999 | 656 | 291 (44%) | 100 (15%) | 265 (40%) | |
| ≥$150,000 | 750 | 326 (43%) | 137 (18%) | 287 (38%) | |
| Smoking status in 2020 | 0.48 | ||||
| Never | 1678 | 751 (45%) | 268 (16%) | 659 (39%) | |
| Current | 31 | 12 (39%) | 3 (9.7%) | 16 (52%) | |
| Former | 626 | 278 (44%) | 111 (18%) | 237 (38%) | |
| Alcohol in 2020, g/day | 0.6 (0.8) | 0.6 (0.8) | 0.6 (0.8) | 0.6 (0.8) | 0.97 |
| Physical activity, total MET-hrs/week | 7.2 (6.5) | 7.2 (6.5) | 7.1 (6.1) | 7.2 (6.8) | 0.90 |
| Body mass index in 2018, kg/m2 | 27.5 (6.0) | 27.5 (5.7) | 27.5 (6.4) | 27.5 (6.1) | 0.53 |
| Body mass index in 2020, kg/m2 | 27.5 (6.1) | 27.3 (5.8) | 27.4 (6.4) | 27.8 (6.3) | 0.24 |
| Change in weight, kg | <0.001 | ||||
| Lost ≥ 4.5 kg | 333 | 180 (54%) | 57 (17%) | 96 (29%) | |
| Lost 2.25 -<4.5 kg | 321 | 168 (52%) | 53 (17%) | 100 (31%) | |
| Lost or gained < 2.25 kg | 1029 | 437 (42%) | 180 (17%) | 412 (40%) | |
| Gained 2.25 -<4.5 kg | 320 | 126 (39%) | 42 (13%) | 152 (48%) | |
| Gained ≥ 4.5 kg | 332 | 130 (39%) | 50 (15%) | 152 (46%) | |
| Self-reported COVID-19 infection 4 | 58 | 22 (38%) | 8 (14%) | 28 (48%) | 0.35 |
| Risk of COVID-19 complications 5 | 0.42 | ||||
| Low | 645 | 274 (42%) | 110 (17%) | 261 (40%) | |
| Medium | 850 | 401 (47%) | 134 (16%) | 315 (37%) | |
| High | 840 | 366 (44%) | 138 (16%) | 336 (40%) | |
| History of cancer | 124 | 62 (50%) | 26 (21%) | 36 (29%) | 0.05 |
| Marital status in 2018 | 0.18 | ||||
| Married/w partner | 1858 | 830 (45%) | 306 (16%) | 722 (39%) | |
| Never married | 173 | 81 (47%) | 18 (10%) | 74 (43%) | |
| Divorced, separated, or widowed | 304 | 130 (43%) | 58 (19%) | 116 (38%) | |
| Living situation during pandemic | 0.69 | ||||
| Lives alone | 278 | 119 (43%) | 50 (18%) | 109 (39%) | |
| Lives with other people | 2057 | 922 (45%) | 332 (16%) | 803 (39%) | |
| Number of people in home | 2.4 (1.4) | 2.4 (1.4) | 2.4 (1.5) | 2.3 (1.3) | 0.60 |
| Caregiver for other adults or children in home | 534 | 231 (43%) | 94 (18%) | 209 (39%) | 0.60 |
| Change in meal sources (times/week) | |||||
| Fast food | −0.1 (0.9) | −0.2 (1.0) | −0.2 (0.8) | −0.03 (0.8) | <0.001 |
| Full service | −0.5 (1.2) | −0.5 (1.2) | −0.4 (1.2) | −0.4 (1.0) | 0.54 |
| Prepared | −0.7 (1.1) | −0.4 (1.1) | −0.3 (1.1) | −0.3 (1.0) | 0.09 |
| Home cooked | −0.1 (1.7) | 0.001 (1.7) | −0.2 (1.7) | −0.2 (1.7) | 0.01 |
| Points 1 | Servings Per Day | |||||||
|---|---|---|---|---|---|---|---|---|
| 2018 2 | 2020 2 | Mean Change 2 | p3 | 2018 4 | 2020 4 | Mean Change 4 | p3 | |
| Diet quality score 5 | 12.24 ± 3.63 | 12.45 ± 3.57 | 0.20 | <0.001 | -- | -- | -- | -- |
| Vegetables | 2.08 ± 0.96 | 1.99 ± 0.95 | −0.09 | <0.001 | 1.79 ± 1.35 | 1.58 ± 1.23 | −0.21 | <0.001 |
| Fruits | 1.95 ± 0.97 | 1.92 ± 0.97 | −0.03 | 0.10 | 1.50 ± 1.20 | 1.45 ± 1.15 | −0.06 | 0.01 |
| Whole grains | 1.45 ± 0.97 | 1.29 ± 0.94 | −0.16 | <0.001 | 0.98 ± 1.03 | 0.81 ± 0.91 | −0.17 | <0.001 |
| Refined grains | 1.40 ± 1.06 | 1.55 ± 1.05 | 0.15 | <0.001 | 0.59 ± 0.72 | 0.48 ± 0.60 | −0.11 | <0.001 |
| Red meat | 1.55 ± 0.94 | 1.65 ± 0.95 | 0.10 | <0.001 | 0.41 ± 0.46 | 0.37 ± 0.41 | −0.05 | <0.001 |
| Processed meat | 2.16 ± 0.94 | 2.18 ± 0.92 | 0.03 | 0.12 | 0.23 ± 0.34 | 0.21 ± 0.30 | −0.02 | 0.03 |
| Sugar-sweetened beverages | 0.55 ± 0.50 | 0.65 ± 0.48 | 0.09 | <0.001 | 0.16 ± 0.45 | 0.14 ± 0.43 | −0.01 | 0.17 |
| Diet beverages | 0.59 ± 0.49 | 0.61 ± 0.49 | 0.02 | 0.04 | 0.34 ± 0.81 | 0.34 ± 0.77 | 0.003 | 0.83 |
| Fruit juice | 0.52 ± 0.50 | 0.61 ± 0.49 | 0.09 | <0.001 | 0.22 ± 0.46 | 0.18 ± 0.41 | −0.04 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Um, C.Y.; Hodge, R.A.; McCullough, M.L. Change in Diet Quality and Meal Sources during the COVID-19 Pandemic in a Diverse Subset of Men and Women in the Cancer Prevention Study-3. Nutrients 2023, 15, 849. https://doi.org/10.3390/nu15040849
Um CY, Hodge RA, McCullough ML. Change in Diet Quality and Meal Sources during the COVID-19 Pandemic in a Diverse Subset of Men and Women in the Cancer Prevention Study-3. Nutrients. 2023; 15(4):849. https://doi.org/10.3390/nu15040849
Chicago/Turabian StyleUm, Caroline Y., Rebecca A. Hodge, and Marjorie L. McCullough. 2023. "Change in Diet Quality and Meal Sources during the COVID-19 Pandemic in a Diverse Subset of Men and Women in the Cancer Prevention Study-3" Nutrients 15, no. 4: 849. https://doi.org/10.3390/nu15040849
APA StyleUm, C. Y., Hodge, R. A., & McCullough, M. L. (2023). Change in Diet Quality and Meal Sources during the COVID-19 Pandemic in a Diverse Subset of Men and Women in the Cancer Prevention Study-3. Nutrients, 15(4), 849. https://doi.org/10.3390/nu15040849






