Breakfast Size and Prevalence of Metabolic Syndrome in the European Prospective Investigation into Cancer and Nutrition (EPIC) Spanish Cohort
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection
2.3. Biological Samples
2.4. Metabolic Syndrome Definition
2.5. Dietary Information
2.6. Statistical Analysis
3. Results
3.1. Descriptive Statistics
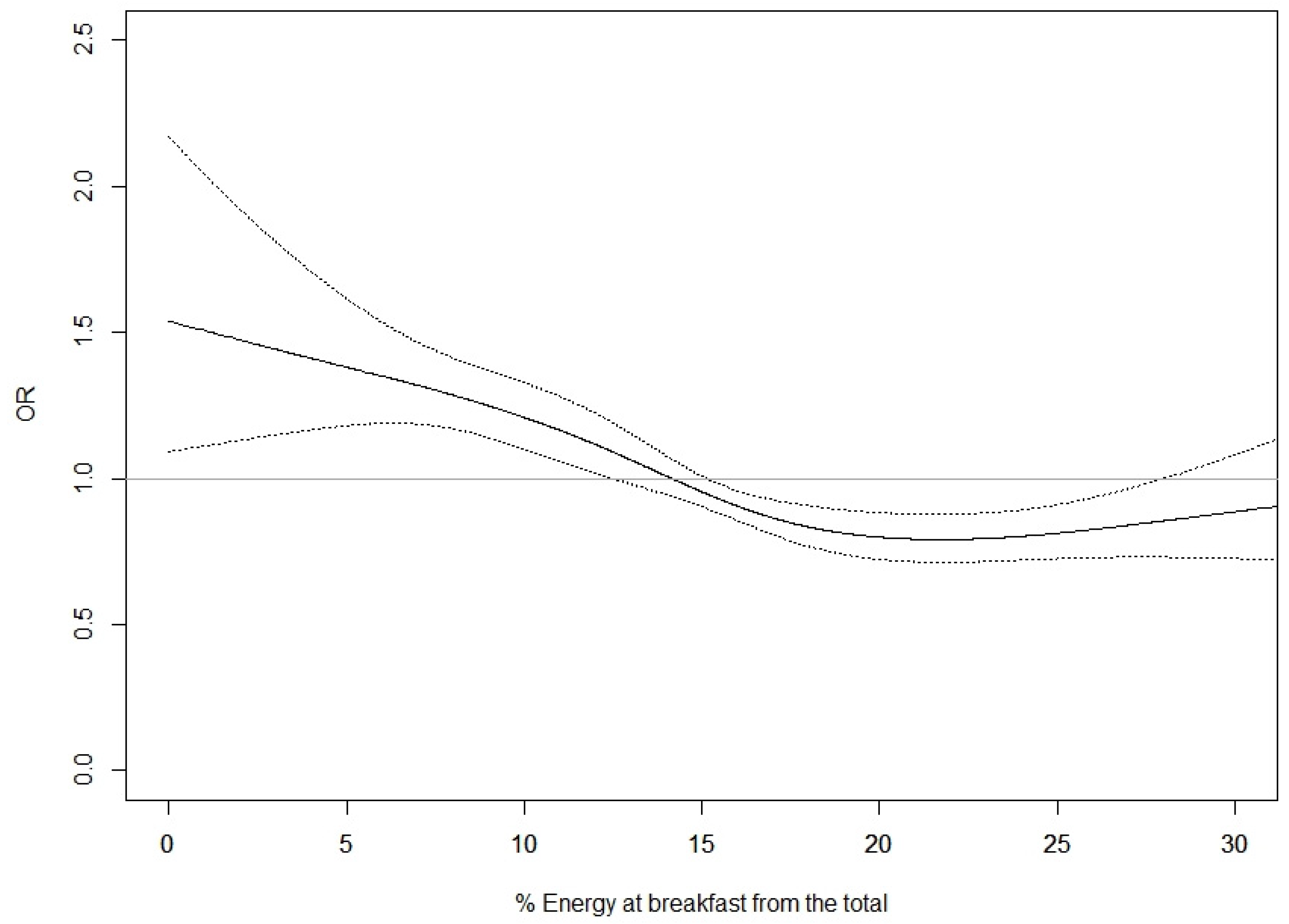
3.2. Breakfast Size and Prevalence of Metabolic Syndrome
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef]
- Subías-Perié, J.; Navarrete-Villanueva, D.; Fernández-García, Á.I.; Moradell, A.; Gesteiro, E.; Pérez-Gómez, J.; Ara, I. Prevalence of Metabolic Syndrome and Association with Physical Activity and Frailty Status in Spanish Older Adults with Decreased Functional Capacity: A Cross-Sectional Study. Nutrients 2022, 14, 2302. [Google Scholar] [CrossRef]
- World Health Organization. Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications: Report of a Who Consultation. Part 1, Diagnosis and Classification of Diabetes Mellitus; World Health Organization: Geneva, Switzerland, 1999; p. WHO/NCD/NCS/99.2.
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497.
- Alberti, G.; Zimmet, P.; Shaw, J.; Grundy, S.M. The IDF Consensus Wordlwide Definition of the Metabolic Syndrome; International Diabetes Federation: Brussels, Belgium, 2006. [Google Scholar]
- Scuteri, A.; Laurent, S.; Cucca, F.; Cockcroft, J.; Cunha, P.G.; Mañas, L.R.; Raso, F.U.M.; Muiesan, M.L.; Ryliškytė, L.; Rietzschel, E.; et al. Metabolic syndrome across Europe: Different clusters of risk factors. Eur. J. Prev. Cardiol. 2015, 22, 486–491. [Google Scholar] [CrossRef]
- Garaulet, M.; Madrid, J.A. Chronobiology, genetics and metabolic syndrome. Curr. Opin. Lipidol. 2009, 20, 127–134. [Google Scholar] [CrossRef]
- Gibney, M.J.; Barr, S.I.; Bellisle, F.; Drewnowski, A.; Fagt, S.; Livingstone, B.; Masset, G.; Moreiras, G.V.; Moreno, L.A.; Smith, J.; et al. Breakfast in Human Nutrition: The International Breakfast Research Initiative. Nutrients 2018, 10, E559. [Google Scholar] [CrossRef]
- Lopez-Minguez, J.; Gómez-Abellán, P.; Garaulet, M. Timing of Breakfast, Lunch, and Dinner. Effects on Obesity and Metabolic Risk. Nutrients 2019, 11, E2624. [Google Scholar] [CrossRef]
- Smith, K.J.; Gall, S.L.; McNaughton, S.A.; Blizzard, L.; Dwyer, T.; Venn, A.J. Skipping breakfast: Longitudinal associations with cardiometabolic risk factors in the Childhood Determinants of Adult Health Study. Am. J. Clin. Nutr. 2010, 92, 1316–1325. [Google Scholar] [CrossRef]
- Reutrakul, S.; Hood, M.M.; Crowley, S.J.; Morgan, M.K.; Teodori, M.; Knutson, K.L. The relationship between breakfast skipping, chronotype, and glycemic control in type 2 diabetes. Chronobiol. Int. 2014, 31, 64–71. [Google Scholar] [CrossRef]
- Nakajima, K.; Suwa, K. Association of hyperglycemia in a general Japanese population with late-night-dinner eating alone, but not breakfast skipping alone. J. Diabetes Metab. Disord. 2015, 14, 16. [Google Scholar] [CrossRef]
- Kutsuma, A.; Nakajima, K.; Suwa, K. Potential Association between Breakfast Skipping and Concomitant Late-Night-Dinner Eating with Metabolic Syndrome and Proteinuria in the Japanese Population. Scientifica 2014, 2014, 253581. [Google Scholar] [CrossRef]
- Mekary, R.A.; Giovannucci, E.; Willett, W.C.; van Dam, R.M.; Hu, F.B. Eating patterns and type 2 diabetes risk in men: Breakfast omission, eating frequency, and snacking. Am. J. Clin. Nutr. 2012, 95, 1182–1189. [Google Scholar] [CrossRef]
- Dashti, H.S.; Merino, J.; Lane, J.M.; Song, Y.; Smith, C.E.; Tanaka, T.; McKeown, N.M.; Tucker, C.; Sun, D.; Bartz, T.M.; et al. Genome-wide association study of breakfast skipping links clock regulation with food timing. Am. J. Clin. Nutr. 2019, 110, 473–484. [Google Scholar] [CrossRef]
- Wang, W.; Grech, A.; Gemming, L.; Rangan, A. Breakfast size is associated with daily energy intake and diet quality. Nutr. Burbank 2020, 75–76, 110764. [Google Scholar] [CrossRef]
- Nicholl, A.; du Heaume, M.; Mori, T.A.; Beilin, L.J.; Oddy, W.H.; Bremner, A.P.; O’Sullivan, T.A. Higher breakfast glycaemic load is associated with increased metabolic syndrome risk, including lower HDL-cholesterol concentrations and increased TAG concentrations, in adolescent girls. Br. J. Nutr. 2014, 112, 1974–1983. [Google Scholar] [CrossRef]
- Yoo, K.B.; Suh, H.J.; Lee, M.; Kim, J.H.; Kwon, J.A.; Park, E.C. Breakfast eating patterns and the metabolic syndrome: The Korea National Health and Nutrition Examination Survey (KNHANES) 2007–2009. Asia Pac. J. Clin. Nutr. 2014, 23, 128–137. [Google Scholar]
- Iqbal, K.; Schwingshackl, L.; Gottschald, M.; Knüppel, S.; Stelmach-Mardas, M.; Aleksandrova, K.; Boeing, H. Breakfast quality and cardiometabolic risk profiles in an upper middle-aged German population. Eur. J. Clin. Nutr. 2017, 71, 1312–1320. [Google Scholar] [CrossRef]
- Almoosawi, S.; Prynne, C.J.; Hardy, R.; Stephen, A.M. Time-of-day and nutrient composition of eating occasions: Prospective association with the metabolic syndrome in the 1946 British birth cohort. Int. J. Obes. 2013, 37, 725–731. [Google Scholar] [CrossRef]
- Akter, S.; Nanri, A.; Pham, N.M.; Kurotani, K.; Mizoue, T. Dietary patterns and metabolic syndrome in a Japanese working population. Nutr. Metab. 2013, 10, 30. [Google Scholar] [CrossRef]
- Garaulet, M.; Gómez-Abellán, P.; Alburquerque-Béjar, J.J.; Lee, Y.C.; Ordovás, J.M.; Scheer, F.A.J.L. Timing of food intake predicts weight loss effectiveness. Int. J. Obes. 2013, 37, 604–611. [Google Scholar] [CrossRef]
- Min, C.; Noh, H.; Kang, Y.S.; Sim, H.J.; Baik, H.W.; Song, W.O.; Yoon, J.; Park, Y.-H.; Joung, H. Breakfast patterns are associated with metabolic syndrome in Korean adults. Nutr. Res. Pract. 2012, 6, 61–67. [Google Scholar] [CrossRef]
- Félix, P.V.; Pereira, J.L.; Leme, A.C.B.; de Castro, M.A.; Fisberg, R.M. Nutritional breakfast quality and cardiometabolic risk factors: Health Survey of São Paulo, a population-based study. Public Health Nutr. 2021, 24, 4102–4112. [Google Scholar] [CrossRef] [PubMed]
- Bandín, C.; Scheer, F.A.J.L.; Luque, A.J.; Ávila-Gandía, V.; Zamora, S.; Madrid, J.A.; Gómez-Abellán, P.; Garaulet, M. Meal timing affects glucose tolerance, substrate oxidation and circadian-related variables: A randomized, crossover trial. Int. J. Obes. 2015, 39, 828–833. [Google Scholar] [CrossRef] [PubMed]
- Collado, M.C.; Engen, P.A.; Bandín, C.; Cabrera-Rubio, R.; Voigt, R.M.; Green, S.J.; Naqib, A.; Keshavarzian, A.; Scheer, F.A.J.L.; Garaulet, M. Timing of food intake impacts daily rhythms of human salivary microbiota: A randomized, crossover study. FASEB J. 2018, 32, 2060–2072. [Google Scholar] [CrossRef]
- Garaulet, M.; Vera, B.; Bonnet-Rubio, G.; Gómez-Abellán, P.; Lee, Y.C.; Ordovás, J.M. Lunch eating predicts weight-loss effectiveness in carriers of the common allele at PERILIPIN1: The ONTIME (Obesity, Nutrigenetics, Timing, Mediterranean) study. Am. J. Clin. Nutr. 2016, 104, 1160–1166. [Google Scholar] [CrossRef]
- Ruiz-Lozano, T.; Vidal, J.; de Hollanda, A.; Scheer, F.A.J.L.; Garaulet, M.; Izquierdo-Pulido, M. Timing of food intake is associated with weight loss evolution in severe obese patients after bariatric surgery. Clin. Nutr. 2016, 35, 1308–1314. [Google Scholar] [CrossRef]
- Yoshida, J.; Eguchi, E.; Nagaoka, K.; Ito, T.; Ogino, K. Association of night eating habits with metabolic syndrome and its components: A longitudinal study. BMC Public Health 2018, 18, 1366. [Google Scholar] [CrossRef]
- O’Neil, C.E.; Byrd-Bredbenner, C.; Hayes, D.; Jana, L.; Klinger, S.E.; Stephenson-Martin, S. The role of breakfast in health: Definition and criteria for a quality breakfast. J. Acad. Nutr. Diet. 2014, 114 (Suppl. 12), S8–S26. [Google Scholar] [CrossRef]
- de Castro, J.M. The time of day and the proportions of macronutrients eaten are related to total daily food intake. Br. J. Nutr. 2007, 98, 1077–1083. [Google Scholar] [CrossRef]
- González, C.A.; Navarro, C.; Martínez, C.; Quirós, J.R.; Dorronsoro, M.; Barricarte, A.; Tormo, M.J.; Agudo, A.; Chirlaque, M.D.; Amiano, P.; et al. [The European prospective investigation about cancer and nutrition (EPIC)]. Rev. Esp. Salud. Pública 2004, 78, 167–176. [Google Scholar] [CrossRef]
- Riboli, E.; Hunt, K.J.; Slimani, N.; Ferrari, P.; Norat, T.; Fahey, M.; Charrondière, U.; Hémon, B.; Casagrande, C.; Vignat, J.; et al. European Prospective Investigation into Cancer and Nutrition (EPIC): Study populations and data collection. Public Health Nutr. 2002, 5, 1113–1124. [Google Scholar] [CrossRef] [PubMed]
- Molina-Montes, E.; Rodríguez-Barranco, M.; Ching-López, A.; Artacho, R.; Huerta, J.M.; Amiano, P.; Lasheras, C.; Moreno-Iribas, C.; Jimenez-Zabala, A.; Chirlaque, M.D.; et al. Circadian clock gene variants and their link with chronotype, chrononutrition, sleeping patterns and obesity in the European prospective investigation into cancer and nutrition (EPIC) study. Clin. Nutr. 2022, 41, 1977–1990. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Roenneberg, T.; Allebrandt, K.V.; Merrow, M.; Vetter, C. Social jetlag and obesity. Curr. Biol. 2012, 22, 939–943. [Google Scholar] [CrossRef]
- Zavada, A.; Gordijn, M.C.M.; Beersma, D.G.M.; Daan, S.; Roenneberg, T. Comparison of the Munich Chronotype Questionnaire with the Horne-Ostberg’s Morningness-Eveningness Score. Chronobiol. Int. 2005, 22, 267–278. [Google Scholar] [CrossRef]
- Morgan, L.M.; Shi, J.W.; Hampton, S.M.; Frost, G. Effect of meal timing and glycaemic index on glucose control and insulin secretion in healthy volunteers. Br. J. Nutr. 2012, 108, 1286–1291. [Google Scholar] [CrossRef]
- Chen, K.Y.; Hsiao, C.F.; Chang, G.C.; Tsai, Y.H.; Su, W.C.; Perng, R.P.; Huang, M.; Hsiung, C.A.; Chen, C.-J.; Yang, P.-C.; et al. Hormone replacement therapy and lung cancer risk in Chinese. Cancer 2007, 110, 1768–1775. [Google Scholar] [CrossRef]
- Taetzsch, A.; Roberts, S.B.; Bukhari, A.; Lichtenstein, A.H.; Gilhooly, C.H.; Martin, E.; Krauss, A.J.; Hatch-McChesney, A.; Das, S.K. Eating Timing: Associations with Dietary Intake and Metabolic Health. J. Acad. Nutr. Diet. 2021, 121, 738–748. [Google Scholar] [CrossRef]
- Hermenegildo-López, Y.; Donat-Vargas, C.; Sandoval-Insausti, H.; Moreno-Franco, B.; Rodríguez-Ayala, M.; Rey-García, J.; Banegas, J.R.; Rodríguez-Artalejo, F.; Guallar-Castillón, P. A Higher Intake of Energy at Dinner Is Associated with Incident Metabolic Syndrome: A Prospective Cohort Study in Older Adults. Nutrients 2021, 13, 3035. [Google Scholar] [CrossRef]
- de Castro, J.M. The time of day of food intake influences overall intake in humans. J. Nutr. 2004, 134, 104–111. [Google Scholar] [CrossRef]
- de Castro, J.M. When, how much and what foods are eaten are related to total daily food intake. Br. J. Nutr. 2009, 102, 1228–1237. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, A.; Bechtold, D.A.; Pot, G.K.; Johnston, J.D. Chrono-nutrition: From molecular and neuronal mechanisms to human epidemiology and timed feeding patterns. J. Neurochem. 2021, 157, 53–72. [Google Scholar] [CrossRef] [PubMed]
- Raynor, H.A.; Li, F.; Cardoso, C. Daily pattern of energy distribution and weight loss. Physiol. Behav. 2018, 192, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Bo, S.; Fadda, M.; Castiglione, A.; Ciccone, G.; De Francesco, A.; Fedele, D.; Guggino, A.; Parasiliti-Caprino, M.; Ferrara, S.; Boggio, M.V.; et al. Is the timing of caloric intake associated with variation in diet-induced thermogenesis and in the metabolic pattern? A randomized cross-over study. Int. J. Obes. 2015, 39, 1689–1695. [Google Scholar] [CrossRef]
- Morris, C.J.; Garcia, J.I.; Myers, S.; Yang, J.N.; Trienekens, N.; Scheer, F.A.J.L. The Human Circadian System Has a Dominating Role in Causing the Morning/Evening Difference in Diet-Induced Thermogenesis. Obesity 2015, 23, 2053–2058. [Google Scholar] [CrossRef]
- Jakubowicz, D.; Barnea, M.; Wainstein, J.; Froy, O. High caloric intake at breakfast vs. dinner differentially influences weight loss of overweight and obese women. Obesity 2013, 21, 2504–2512. [Google Scholar] [CrossRef]
| Metabolic Syndrome (MetS) 1 | |||
|---|---|---|---|
| No (n = 2160) | Yes (n = 1484) | p Value 2 | |
| Number of Diagnostic Criteria | |||
| 0 | 70 | ||
| 1 | 888 | ||
| 2 | 1202 | ||
| 3 | 989 | ||
| 4 | 395 | ||
| 5 | 100 | ||
| Presence of individual diagnostic of MetS | |||
| Waist circumference, yes | 510 (28.1) | 1305 (71.9) | <0.001 |
| Triglycerides, yes | 87 (13.1) | 579 (86.9) | <0.001 |
| HDL-Cholesterol, yes | 36 (9.1) | 359 (90.9) | <0.001 |
| Hypertension, yes | 1973 (57.2) | 1476 (42.8) | <0.001 |
| Hyperglycemia, yes | 686 (34.1) | 1328 (65.9) | <0.001 |
| Study center | |||
| Asturias | 538 (61.1) | 343 (38.9) | <0.001 |
| Granada | 436 (59.8) | 293 (40.2) | |
| Murcia | 370 (46.8) | 421 (53.2) | |
| Navarra | 359 (59.7) | 242 (40.3) | |
| Guipuzkoa | 457 (71.2) | 185 (28.8) | |
| Sex | |||
| Men | 880 (60.7) | 569 (39.3) | 0.146 |
| Women | 1280 (58.3) | 915 (41.7) | |
| Age (years) | 65.00 (61.68–68.54) | 65.94 (62.12–69.11) | <0.001 |
| Educational level | |||
| None | 327 (48.7) | 344 (51.3) | <0.001 |
| Primary school | 737 (55.9) | 581 (44.1) | |
| Technical studies | 310 (62.9) | 183 (37.1) | |
| Secondary school | 267 (61.5) | 167 (38.5) | |
| Higher education | 513 (72.0) | 200 (28.1) | |
| Missing | 6 (40.0) | 9 (60.0) | |
| Smoking history | |||
| Never | 1080 (59.4) | 737 (40.6) | 0.872 |
| Current | 259 (57.6) | 191 (42.4) | |
| Former | 819 (59.6) | 555 (40.4) | |
| Missing | 1 (50.0) | 1 (50.0) | |
| Body Mass Index (kg/m2) | 26.29 (24.10–28.60) | 30.80 (28.30–33.70) | <0.001 |
| % Body fat | 29.15 (23.60–35.15) | 35.50 (29.60–40.10) | <0.001 |
| Non-laboral physical activity (MET-h/week) | 80.00 (58.75–104.30) | 77.55 (53.50–102.25) | 0.007 |
| At home | 39.90 (21.00–62.30) | 44.05 (23.10–66.48) | <0.001 |
| Recreation | 36.00 (22.50–51.00) | 30.00 (18.00–44.38) | <0.001 |
| Sleep quality | |||
| Good | 2109 (59.6) | 1430 (40.4) | 0.024 |
| Poor | 51 (48.6) | 54 (51.4) | |
| Time of sleep (h/workdays) | 6:25 (7:10–7:55) | 6:25 (7:15–7:55) | 0.475 |
| Time of sleep (h/freedays) | 6:35 (7:29–8:10) | 6:30 (7:25–8:15) | 0.503 |
| Chronotype | |||
| Moderate/extreme early type | 54 (57.5) | 40 (42.6) | 0.245 |
| Slight early type | 151 (59.2) | 104 (40.8) | |
| Normal type | 1717 (60.0) | 1147 (40.1) | |
| Slight late type | 155 (58.5) | 110 (41.5) | |
| Moderate/extreme late type | 45 (49.5) | 46 (50.6) | |
| Missing | 38 (50.7) | 37 (49.3) | |
| Breakfast time (h) | |||
| ≤9:00 | 1686 (62.1) | 1028 (37.9) | <0.001 |
| >9:00 | 468 (51.2) | 446 (48.8) | |
| Missing | 6 (37.5) | 10 (62.5) | |
| Lunch time (h) | |||
| ≤14:00 | 1041 (60.4) | 680 (39.6) | 0.039 |
| >14:00–15:00 | 774 (57.1) | 580 (42.9) | |
| >15:00 | 165 (65.5) | 87 (34.5) | |
| Missing | 180 (56.8) | 137 (43.2) | |
| Dinner time (h) | |||
| ≤21:00 | 677 (58.6) | 477 (41.3) | 0.364 |
| 21:00 | 577 (60.7) | 372 (39.2) | |
| >21:00 | 667 (59.8) | 447 (40.2) | |
| Missing | 239 (56.0) | 188 (44.0) | |
| Number of eating occasions | 0.004 | ||
| ≤3 | 93 (64.6) | 51 (35.4) | |
| 4–5 | 990 (61.8) | 612 (38.2) | |
| >5 | 1077 (56.7) | 821 (43.3) | |
| Breakfast size (×2000 kcal) 3 | 306.85 (229.81–391.63) | 280.42 (205.36–368.18) | <0.001 |
| Dietary intake at breakfast | |||
| Energy at breakfast from the total (%) | 15.34 (11.49–19.58) | 14.02 (10.27–18.41) | <0.001 |
| Macronutrient composition (%) | |||
| Proteins | 13.73 (11.17–16.96) | 14.28 (11.46–17.51) | 0.005 |
| Carbohydrates | 56.59 (48.84–64.70) | 55.09 (47.58–62.81) | <0.001 |
| Fats | 28.26 (18.97–37.16) | 29.49 (19.98–38.01) | 0.059 |
| Total energy at entire day (kcal/day) | 2386.2 (2140.9–2678.9) | 2489.3 (2218.0–2788.6) | <0.001 |
| Breakfast Size (×2000 kcal) 1 | |||||
|---|---|---|---|---|---|
| Q1 (<222) (n =911) | Q2 (222–296.3) (n = 911) | Q3 (296.4–384) (n = 911) | Q4 (>384) (n = 911) | p Value 2 | |
| Number of diagnostic criteria | |||||
| 0 | 9 (1.0) | 19 (2.1) | 14 (1.5) | 28 (3.1) | <0.001 |
| 1 | 157 (17.2) | 212 (23.3) | 247 (27.1) | 272 (29.9) | |
| 2 | 308 (33.8) | 303 (33.3) | 300 (32.9) | 291 (31.9) | |
| 3 | 286 (31.4) | 238 (26.1) | 247 (27.1) | 218 (23.9) | |
| 4 | 118 (13.0) | 109 (12.0) | 80 (8.8) | 88 (9.7) | |
| 5 | 33 (3.6) | 30 (3.3) | 23 (2.5) | 14 (1.5) | |
| MetS 3, yes | 437 (48.0) | 377 (41.4) | 350 (38.4) | 320 (35.1) | <0.001 |
| Presence of individual components of MetS 3 | |||||
| Abdominal obesity, yes | 509 (55.9) | 473 (51.9) | 439 (48.2) | 394 (43.3) | <0.001 |
| Triglycerides, yes | 195 (21.4) | 170 (18.7) | 149 (16.4) | 152 (16.7) | 0.020 |
| HDL-Cholesterol, yes | 113 (12.4) | 103 (11.3) | 87 (9.6) | 92 (10.1) | 0.204 |
| Hypertension, yes | 865 (95.0) | 859 (94.3) | 871 (95.6) | 854 (93.7) | 0.317 |
| Hyperglycemia, yes | 586 (64.3) | 513 (56.3) | 477 (52.4) | 438 (48.1) | <0.001 |
| Study center | |||||
| Asturias | 245 (26.9) | 222 (24.4) | 215 (23.6) | 199 (21.8) | <0.001 |
| Granada | 116 (12.7) | 170 (18.7) | 233 (25.6) | 210 (23.1) | |
| Murcia | 194 (21.3) | 231 (25.4) | 183 (20.1) | 183 (20.1) | |
| Navarra | 190 (20.9) | 138 (15.2) | 128 (14.1) | 145 (15.9) | |
| Guipúzcoa | 166 (18.2) | 150 (16.5) | 152 (16.7) | 174 (19.1) | |
| Sex | |||||
| Men | 429 (47.1) | 377 (41.4) | 321 (35.2) | 322 (35.4) | <0.001 |
| Women | 482 (52.9) | 534 (58.6) | 590 (64.8) | 589 (64.7) | |
| Age (year) | 65.25 (61.91–68.62) | 65.31 (62.00–68.53) | 65.09 (61.82–68.47) | 65.92 (62.00–69.54) | 0.044 |
| Educational level | |||||
| None | 154 (16.9) | 174 (19.1) | 179 (19.7) | 164 (18.0) | <0.001 |
| Primary school | 367 (40.3) | 367 (40.3) | 279 (30.6) | 305 (33.5) | |
| Technical studies | 115 (12.6) | 122 (13.4) | 133 (14.6) | 123 (13.5) | |
| Secondary school | 122 (13.4) | 105 (11.5) | 110 (12.1) | 97 (10.7) | |
| Higher education | 150 (16.5) | 142 (15.6) | 206 (22.6) | 215 (23.6) | |
| Missing | 3 (0.3) | 1 (0.1) | 4 (0.4) | 7 (0.8) | |
| Smoking history | |||||
| Never | 369 (40.5) | 472 (51.8) | 486 (53.4) | 490 (53.9) | <0.001 |
| Current | 169 (18.6) | 102 (11.2) | 95 (10.4) | 84 (9.2) | |
| Former | 373 (40.9) | 337 (37.0) | 329 (36.1) | 335 (36.8) | |
| Missing | 1 (0.1) | 1 (0.1) | |||
| Body Mass Index (kg/m2) | 28.82 (26.10–31.90) | 28.20 (25.60–31.30) | 27.84 (25.40–30.70) | 26.90 (24.50–30.30) | <0.001 |
| % Body fat | 32.00 (25.90–37.70) | 31.70 (25.70–37.30) | 32.40 (25.60–37.70) | 31.80 (25.90–36.80) | 0.543 |
| Non-laboral Physical activity (MET-h/week) | 76.60 (53.80–100.80) | 79.80 (55.20–105.00) | 77.80 (56.20–102.30) | 81.30 (61.10–104.85) | 0.023 |
| At home | 41.20 (20.80–62.30) | 42.70 (20.30–65.80) | 43.20 (23.60–65.60) | 42.00 (22.60–63.53) | 0.456 |
| Recreational | 31.50 (19.50–48.00) | 33.00 (21.00–48.00) | 31.50 (21.00–48.00) | 36.00 (21.00–51.00) | 0.0002 |
| Sleep quality | |||||
| Good | 878 (96.4) | 884 (97.0) | 895 (98.2) | 882 (96.8) | 0.101 |
| Poor | 33 (3.6) | 27 (3.0) | 16 (1.8) | 29 (3.2) | |
| Time of sleep (h/workdays) | 6:25 (7:15–7:55) | 6:25 (7:05–7:55) | 6:30 (7:10–7:55) | 6:25 (7:10–7:55) | 0.748 |
| Time of sleep (h/freedays) | 6:30 (7:25–8:10) | 6:30 (7:25–8:10) | 6:45 (7:30–8:10) | 6:30 (7:28–8:10) | 0.283 |
| Chronotype | |||||
| Moderate/extreme early type | 23 (2.5) | 21 (2.3) | 23 (2.5) | 27 (3.0) | 0.003 |
| Slight early type | 54 (5.9) | 58 (6.4) | 71 (7.8) | 72 (7.9) | |
| Normal type | 696 (76.4) | 731 (80.2) | 710 (77.9) | 727 (79.8) | |
| Slight late type | 82 (9.0) | 58 (6.4) | 72 (7.9) | 53 (5.8) | |
| Moderate/extreme late type | 34 (3.7) | 25 (2.7) | 24 (2.6) | 8 (0.9) | |
| Missing | 22 (2.4) | 18 (2.0) | 11 (1.2) | 24 (2.6) | |
| Breakfast time (h) | |||||
| ≤9:00 | 690 (75.7) | 683 (75.0) | 653 (71.7) | 688 (75.5) | 0.075 |
| >9:00 | 207 (22.7) | 227 (24.9) | 257 (28.2) | 223 (24.5) | |
| Missing | 14 (1.5) | 1 (0.1) | 1 (0.1) | ||
| Lunch time (h) | |||||
| ≤14:00 | 450 (49.4) | 415 (45.6) | 416 (45.7) | 440 (48.3) | 0.114 |
| >14:00–15:00 | 304 (33.4) | 349 (38.3) | 361 (39.6) | 340 (37.3) | |
| >15:00 | 60 (6.6) | 66 (7.2) | 63 (6.9) | 63 (6.9) | |
| Missing | 97 (10.7) | 81 (8.9) | 71 (7.8) | 68 (7.5) | |
| Dinner time (h) | |||||
| ≤21:00 | 295 (32.4) | 295 (32.4) | 271 (29.8) | 293 (32.2) | 0.028 |
| 21:00 | 222 (24.4) | 221 (24.3) | 229 (25.1) | 277 (30.4) | |
| >21:00 | 286 (31.4) | 279 (30.6) | 297 (32.6) | 252 (27.7) | |
| Missing | 108 (11.9) | 116 (12.7) | 114 (12.5) | 89 (9.8) | |
| Number of eating occasions | 0.0001 | ||||
| ≤3 | 32 (3.5) | 32 (3.5) | 25 (2.7) | 55 (6.0) | |
| 4–5 | 385 (42.3) | 373 (40.9) | 413 (45.3) | 431 (47.3) | |
| >5 | 494 (54.2) | 506 (55.5) | 473 (51.9) | 425 (46.7) | |
| Dietary intake at breakfast | |||||
| Energy at breakfast from the total (%) | 7.80 (5.07–9.73) | 13.05 (12.08–13.91) | 16.80 (15.72–17.88) | 22.83 (20.57–26.31) | |
| Macronutrient composition (%) | |||||
| Proteins | 16.08 (11.73–20.65) | 14.63 (12.23–17.20) | 13.66 (11.63–16.17) | 12.40 (10.24–15.04) | <0.001 |
| Carbohydrates | 58.33 (50.29–68.01) | 56.78 (49.60–64.29) | 55.63 (48.07–63.55) | 53.36 (44.44–60.45) | <0.001 |
| Fats | 23.03 (9.95–31.87) | 27.83 (19.38–35.87) | 29.57 (21.02–38.39) | 33.38 (25.32–42.37) | <0.001 |
| Total energy intake (kcal/day) | 2494.1 (2239.2–2847.7) | 2458.6 (2204.7–2749.2) | 2396.2 (2155.7–2685.2) | 2322.3 (2070.8–2626.3) | <0.001 |
| Breakfast Size 2 | ||||
|---|---|---|---|---|
| Q1 (<222) | Q2 (222–296.3) | Q3 (296.4–384) | Q4 (>384) | |
| Prevalence of MetS | ||||
| Model 1 | 1.00 (referent) | 0.72 (0.60–0.88) | 0.65 (0.53–0.78) | 0.55 (0.45–0.67) |
| Model 2 | 1.00 (referent) | 0.74 (0.61–0.90) | 0.70 (0.56–0.83) | 0.62 (0.51–0.76) |
| Presence of individual components of MetS | ||||
| Abdominal obesity 3 | 1.00 (referent) | 0.78 (0.64–0.95) | 0.68 (0.56–0.83) | 0.59 (0.48–0.72) |
| Triglycerides 3 | 1.00 (referent) | 0.88 (0.70–1.11) | 0.75 (0.59–0.96) | 0.84 (0.66–1.07) |
| HDL-Cholesterol 3 | 1.00 (referent) | 0.92 (0.57–1.04) | 0.77 (0.57–1.04) | 0.87 (0.65–1.18) |
| Hypertension 3 | 1.00 (referent) | 0.75 (0.49–1.16) | 0.83 (0.53–1.32) | 0.57 (0.37–0.88) |
| Hyperglycemia 3 | 1.00 (referent) | 0.73 (0.60–0.89) | 0.67 (0.54–0.81) | 0.56 (0.46–0.68) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lujan-Barroso, L.; Iglesias, L.; Zamora-Ros, R.; Lasheras, C.; Sánchez, M.-J.; Cabrera-Castro, N.; Delfrad, J.; Amiano, P.; Molina-Montes, E.; Colorado-Yohar, S.; et al. Breakfast Size and Prevalence of Metabolic Syndrome in the European Prospective Investigation into Cancer and Nutrition (EPIC) Spanish Cohort. Nutrients 2023, 15, 630. https://doi.org/10.3390/nu15030630
Lujan-Barroso L, Iglesias L, Zamora-Ros R, Lasheras C, Sánchez M-J, Cabrera-Castro N, Delfrad J, Amiano P, Molina-Montes E, Colorado-Yohar S, et al. Breakfast Size and Prevalence of Metabolic Syndrome in the European Prospective Investigation into Cancer and Nutrition (EPIC) Spanish Cohort. Nutrients. 2023; 15(3):630. https://doi.org/10.3390/nu15030630
Chicago/Turabian StyleLujan-Barroso, Leila, Lucia Iglesias, Raúl Zamora-Ros, Cristina Lasheras, María-José Sánchez, Natalia Cabrera-Castro, Josu Delfrad, Pilar Amiano, Esther Molina-Montes, Sandra Colorado-Yohar, and et al. 2023. "Breakfast Size and Prevalence of Metabolic Syndrome in the European Prospective Investigation into Cancer and Nutrition (EPIC) Spanish Cohort" Nutrients 15, no. 3: 630. https://doi.org/10.3390/nu15030630
APA StyleLujan-Barroso, L., Iglesias, L., Zamora-Ros, R., Lasheras, C., Sánchez, M.-J., Cabrera-Castro, N., Delfrad, J., Amiano, P., Molina-Montes, E., Colorado-Yohar, S., Moreno-Iribas, C., Dorronsoro, A., Rodríguez-Barranco, M., Chirlaque, M. D., Aizpurua, A., Agudo, A., Quirós, J. R., & Jakszyn, P. (2023). Breakfast Size and Prevalence of Metabolic Syndrome in the European Prospective Investigation into Cancer and Nutrition (EPIC) Spanish Cohort. Nutrients, 15(3), 630. https://doi.org/10.3390/nu15030630









