Evidence-Based Lifestyle Guidelines and Self-Management Strategies Utilized by Women with Polycystic Ovary Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Population
2.2. Data Collection
2.2.1. Demographics
2.2.2. Knowledge and Sources of Diet and Physical Activity Information
2.2.3. Self-Management Questionnaire
2.3. Data Analysis
3. Results
3.1. Demographics
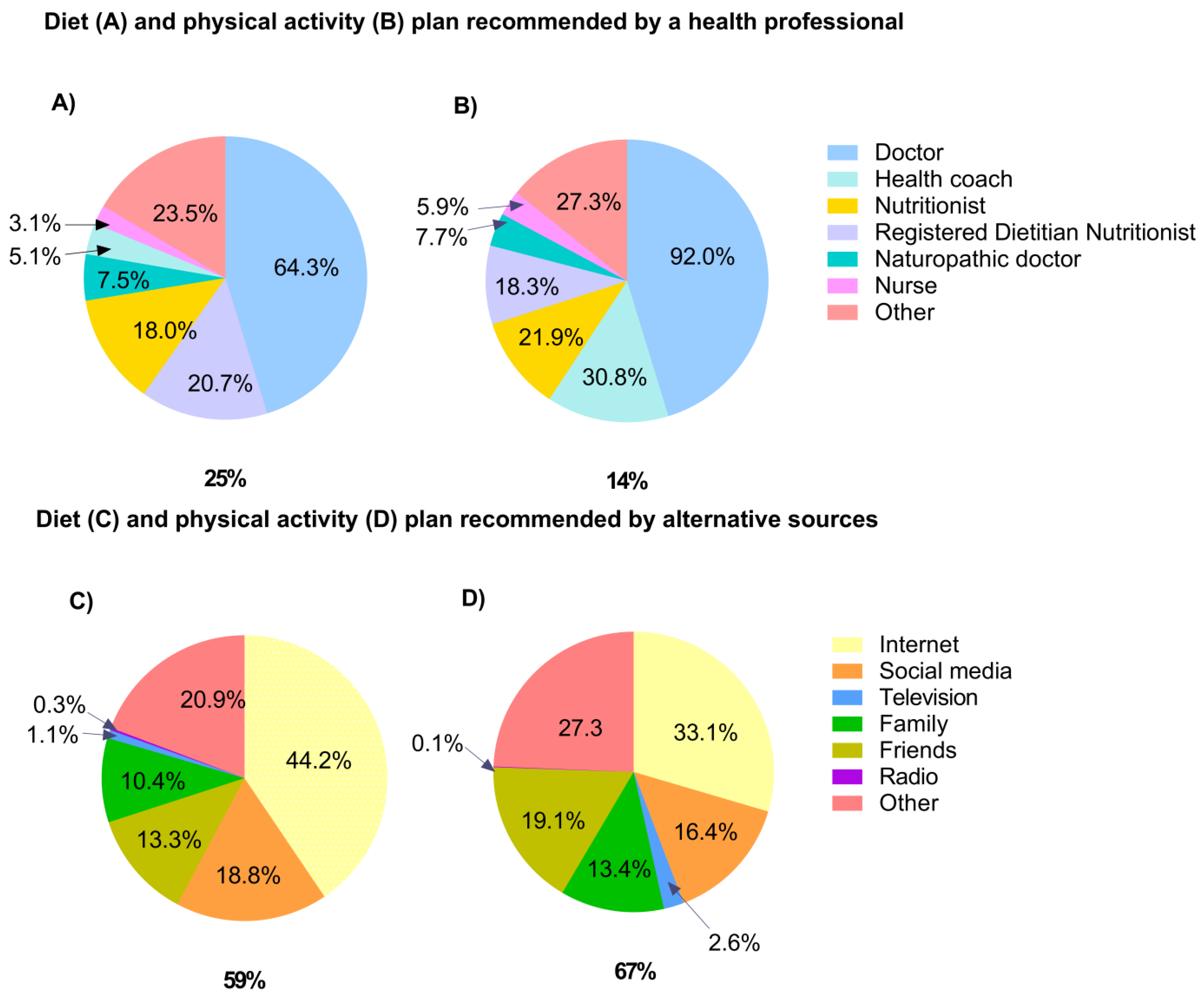
3.2. Knowledge and Sources of Diet and Physical Activity Information
3.3. Dietary and Physical Activity Self-Management Strategies
4. Discussion
5. Strengths and Limitations
6. Conclusions
7. Future Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A—Questions Included in Survey Instrument Relating to Knowledge and Sources of Diet and Physical Activity Information
- Yes
- No
- Yes
- No
- The Dietary Guidelines for Americans
- My Plate
- Dietary Approaches to Stop Hypertension (DASH)
- American Heart Association
- American Diabetes Association
- American Cancer Association
- Other
- Yes
- No
- Low energy/calories
- Low fat
- Low carbohydrate/high protein
- Low glycemic/glycemic load
- Gluten free
- Dairy free
- Soy free
- Ketogenic
- Vegetarian/vegan
- Paleolithic/paleo diet
- High omega-3
- Low FODMAPs
- Yes
- No
- Doctor
- Nurse
- Registered Dietitian
- Nutritionist
- Health Coach
- Naturopathic Doctor
- Other
- Family
- Friends
- Websites
- Social Media
- Television
- Radio
- Other
- Yes
- No
- Yes
- No
- Yes
- No
- Yes
- No
- Family
- Friends
- Websites
- Social Media
- Television
- Radio
- Other
- Doctor
- Nurse
- Registered Dietitian
- Nutritionist
- Health Coach
- Naturopathic doctor
- Other
Appendix B
| Category a | Value b |
|---|---|
| ‘Other’ health professionals (not listed as pre-defined answers) that provided diet advice | |
| Endocrinologist | 5.8 (4) |
| Acupuncturist | 2.9 (2) |
| Allergist | 1.4 (1) |
| Fertility specialist | 1.4 (1) |
| Functional medical doctor | 1.4 (1) |
| Personal trainer | 1.4 (1) |
| Holistic practitioner | 1.4 (1) |
| Did not provide a written response | 84.1 (58) |
| ‘Other’ health professionals (not listed as pre-defined answers) that provided physical activity advice | |
| Exercise physiologist or physiotherapist | 30.6 (15) |
| Personal trainer | 24.5 (12) |
| Endocrinologist | 8.2 (4) |
| Chiropractor or kinesiologist | 6.1 (3) |
| PCOS forum | 2.0 (1) |
| Did not provide a written response | 71.4 (35) |
| ‘Other’ alternative sources (not listed as pre-defined answers) that provided diet advice | |
| Books or magazines | 20.0 (29) |
| Conducted own research | 17.2 (25) |
| Personal trainer | 3.4 (5) |
| Weight loss program | 2.1 (3) |
| Combination (e.g., books, friends, and websites) | 1.4 (2) |
| Others with PCOS | 1.4 (2) |
| PCOS forum | 0.7 (1) |
| Did not provide a written response | 46.2 (67) |
| ‘Other’ alternative sources (not listed as pre-defined answers) that provided physical activity advice | |
| Conducted own research | 72.8 (155) |
| Personal trainer | 12.7 (27) |
| Employment | 3.3 (7) |
| Books or magazines | 1.9 (4) |
| Government guidelines (e.g., NHS) | 0.9 (2) |
| Wii fit console | 0.5 (1) |
| Did not provide a written response | 92.0 (196) |
References
- Ricardo, A.; Enrico, C.; ZiJiang, C.; Andrea, D.; Joop, L. Polycystic ovary syndrome. Nat. Rev. Dis. Prim. 2016, 2, 16057. [Google Scholar]
- Bozdag, G.; Mumusoglu, S.; Zengin, D.; Karabulut, E.; Yildiz, B.O. The prevalence and phenotypic features of polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. 2016, 31, 2841–2855. [Google Scholar] [CrossRef]
- Goodarzi, M.O.; Dumesic, D.A.; Chazenbalk, G.; Azziz, R. Polycystic ovary syndrome: Etiology, pathogenesis and diagnosis. Nat. Rev. Endocrinol. 2011, 7, 219–231. [Google Scholar] [CrossRef]
- Moran, L.J.; Misso, M.L.; Wild, R.A.; Norman, R.J. Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. Update 2010, 16, 347–363. [Google Scholar] [CrossRef]
- Blay, S.L.; Aguiar, J.V.A.; Passos, I.C. Polycystic ovary syndrome and mental disorders: A systematic review and exploratory meta-analysis. Neuropsychiatr. Dis. Treat. 2016, 12, 2895. [Google Scholar] [CrossRef]
- Cooney, L.G.; Lee, I.; Sammel, M.D.; Dokras, A. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. 2017, 32, 1075–1091. [Google Scholar] [CrossRef]
- Stepto, N.K.; Cassar, S.; Joham, A.E.; Hutchison, S.K.; Harrison, C.L.; Goldstein, R.F.; Teede, H.J. Women with polycystic ovary syndrome have intrinsic insulin resistance on euglycaemic–hyperinsulaemic clamp. Hum. Reprod. 2013, 28, 777–784. [Google Scholar] [CrossRef] [PubMed]
- Teede, H.J.; Joham, A.E.; Paul, E.; Moran, L.J.; Loxton, D.; Jolley, D.; Lombard, C. Longitudinal weight gain in women identified with polycystic ovary syndrome: Results of an observational study in young women. Obesity 2013, 21, 1526–1532. [Google Scholar] [CrossRef]
- Lim, S.S.; Davies, M.J.; Norman, R.J.; Moran, L.J. Overweight, obesity and central obesity in women with polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. Update 2012, 18, 618–637. [Google Scholar] [CrossRef]
- Moran, L.J.; Lombard, C.B.; Lim, S.; Noakes, M.; Teede, H.J. Polycystic ovary syndrome and weight management. Women’s Health 2010, 6, 271–283. [Google Scholar] [CrossRef]
- Patterson, R.E.; Satia, J.A.; Kristal, A.R.; Neuhouser, M.L.; Drewnowski, A. Is there a consumer backlash against the diet and health message? J. Am. Diet. Assoc. 2001, 101, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Moran, L.J.; Pasquali, R.; Teede, H.J.; Hoeger, K.M.; Norman, R.J. Treatment of obesity in polycystic ovary syndrome: A position statement of the Androgen Excess and Polycystic Ovary Syndrome Society. Fertil. Steril. 2009, 92, 1966–1982. [Google Scholar] [CrossRef] [PubMed]
- Teede, H.J.; Misso, M.L.; Costello, M.F.; Dokras, A.; Laven, J.; Moran, L.; Piltonen, T.; Norman, R.J. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum. Reprod. 2018, 33, 1602–1618. [Google Scholar] [CrossRef] [PubMed]
- Cowan, S.; Lim, S.; Alycia, C.; Pirotta, S.; Thomson, R.; Gibson-Helm, M.; Blackmore, R.; Naderpoor, N.; Bennett, C.; Ee, C.; et al. Lifestyle management in polycystic ovary syndrome–beyond diet and physical activity. BMC Endocr. Disord. 2023, 23, 14. [Google Scholar] [CrossRef] [PubMed]
- Lamb, J.D.; Johnstone, E.B.; Rousseau, J.A.; Jones, C.L.; Pasch, L.A.; Cedars, M.I.; Huddleston, H.G. Physical activity in women with polycystic ovary syndrome: Prevalence, predictors, and positive health associations. Am. J. Obstet. Gynecol. 2011, 204, 352.e1–352.e6. [Google Scholar] [CrossRef]
- Qublan, H.S.; Yannakoula, E.K.; Al-Qudah, M.A.; El-Uri, F.I. Dietary intervention versus metformin to improve the reproductive outcome in women with polycystic ovary syndrome. Saudi Med. J. 2007, 28, 1694–1699. [Google Scholar]
- Stamets, K.; Taylor, D.S.; Kunselman, A.; Demers, L.M.; Pelkman, C.L.; Legro, R. SA randomized trial of the effects of two types of short-term hypocaloric diets on weight loss in women with polycystic ovary syndrome. Fertil. Steril. 2004, 81, 630–637. [Google Scholar] [CrossRef]
- Eiben, G.; Lissner, L. Health Hunters—An intervention to prevent overweight and obesity in young high-risk women. Int. J. Obes. 2006, 30, 691–696. [Google Scholar] [CrossRef]
- Lim, S.S.; Hutchison, S.K.; Van Ryswyk, E.; Norman, R.J.; Teede, H.J.; Moran, L.J. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst. Rev. 2019, 2019, CD007506. [Google Scholar] [CrossRef]
- Lombard, C.B.; Deeks, A.A.; Ball, K.; Jolley, D.; Teede, H.J. Weight, physical activity and dietary behavior change in young mothers: Short term results of the HeLP-her cluster randomized controlled trial. Nutr. J. 2009, 8, 17. [Google Scholar] [CrossRef]
- Gibson-Helm, M.; Teede, H.; Dunaif, A.; Dokras, A. Delayed diagnosis and a lack of information associated with dissatisfaction in women with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 2017, 102, 604–612. [Google Scholar] [CrossRef]
- Humphreys, L.; Costarelli, V. Implementation of dietary and general lifestyle advice among women with polycystic ovarian syndrome. J. R. Soc. Promot. Health 2008, 128, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Mousiolis, A.; Michala, L.; Antsaklis, A. Polycystic ovary syndrome: Double click and right check. What do patients learn from the Internet about PCOS? Eur. J. Obstet. Gynecol. Reprod. Biol. 2012, 163, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, D.; Kite, J.; Vassallo, A.J.; Chau, J.Y.; Partridge, S.R.; Freeman, B.; Gill, T. Food trends and popular nutrition advice online–implications for public health. Online J. Public Health Inform. 2018, 10, e213. [Google Scholar] [CrossRef]
- Lorig, K.R.; Holman, H.R. Self-Management education: History, definition, outcomes, and mechanisms. Ann. Behav. Med. 2003, 26, 1–7. [Google Scholar] [CrossRef]
- Chrvala, C.A.; Sherr, D.; Lipman, R.D. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ. Couns. 2016, 99, 926–943. [Google Scholar] [CrossRef]
- Bailey, R.R. Promoting physical activity and nutrition in people with stroke. Am. J. Occup. Ther. 2017, 71, 7105360010p1–7105360010p5. [Google Scholar] [CrossRef] [PubMed]
- Norris, S.L.; Engelgau, M.M.; Narayan, K.V. Effectiveness of self-management training in type 2 diabetes: A systematic review of randomized controlled trials. Diabetes Care 2001, 24, 561–587. [Google Scholar] [CrossRef]
- Marks, R.; Allegrante, J.P. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: Implications for health education practice (part II). Health Promot. Pract. 2005, 6, 148–156. [Google Scholar] [CrossRef]
- Saelens, B.E.; Gehrman, C.A.; Sallis, J.F.; Calfas, K.J.; Sarkin, J.A.; Caparosa, S. Use of self-management strategies in a 2-year cognitive-behavioral intervention to promote physical activity. Behav. Ther. 2000, 31, 365–379. [Google Scholar] [CrossRef]
- Chang, M.W.; Nitzke, S.; Guilford, E.; Adair, C.H.; Hazard, D. L Motivators and barriers to healthful eating and physical activity among low-income overweight and obese mothers. J. Am. Diet. Assoc. 2008, 108, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Forster, J.L.; Jeffrey, R.W. Gender differences related to weight history, eating patterns, efficacy expectations, self-esteem, and weight loss among participants in a weight reduction program. Addict. Behav. 1986, 11, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Htet, T.; Cassar, S.; Boyle, J.A.; Kuczynska-Burggraf, M.; Gibson-Helm, M.; Chiu, W.L.; Stepto, N.K.; Moran, L.J. Informing Translation: The Accuracy of Information on Websites for Lifestyle Management of Polycystic Ovary Syndrome. Semin. Reprod. Med. 2018, 36, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Pirotta, S.; Lim, S.S.; Grassi, A.; Couch, L.M.; Jeanes, Y.M.; Joham, A.J.; Teede, H.; Moran, L.J. Relationships between self-management strategies and physical activity and diet quality in women with polycystic ovary syndrome. Patient Educ. Couns. 2022, 105, 190–197. [Google Scholar] [CrossRef] [PubMed]
- DeSalvo, K.B.; Olson, R.; Casavale, K.O. Dietary guidelines for Americans. JAMA 2016, 315, 457–458. [Google Scholar] [CrossRef] [PubMed]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The physical activity guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Sacks, F.M.; Obarzanek, E.; Windhauser, M.M.; Svetkey, L.P.; Vollmer, W.M.; McCullough, M.; Karanja, N.; Lin, P.-H.; Steele, P.; Proschan, M.A.; et al. Rationale and design of the Dietary Approaches to Stop Hypertension trial (DASH): A multicenter controlled-feeding study of dietary patterns to lower blood pressure. Ann. Epidemiol. 1995, 5, 108–118. [Google Scholar] [CrossRef]
- Bantle, J.P.; Wylie-Rosett, J.; Albright, A.L.; Apovian, C.M.; Clark, N.G.; Franz, M.J.; Hoogwerf, B.J.; Lichtenstein, A.H.; Mayer-Davis, E.; Mooradian, A.D.; et al. Nutrition recommendations and interventions for diabetes: A position statement of the American Diabetes Association. Diabetes Care 2008, 31, S61–S78. [Google Scholar]
- Hsieh, H.-F.; Shannon, S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef]
- Kay, M.C.; Carroll, D.D.; Carlson, S.A.; Fulton, J.E. Awareness and knowledge of the 2008 Physical Activity Guidelines for Americans. J. Phys. Act. Health 2014, 11, 693–698. [Google Scholar] [CrossRef]
- Wright, J.D.; Wang, C.-Y. Awareness of federal dietary guidance in persons aged 16 years and older: Results from the National Health and Nutrition Examination Survey 2005–2006. J. Am. Diet. Assoc. 2011, 111, 295–300. [Google Scholar] [CrossRef]
- Adamski, M.; Truby, H.M.; Klassen, K.; Cowan, S.; Gibson, S. Using the Internet: Nutrition Information-Seeking Behaviours of Lay People Enrolled in a Massive Online Nutrition Course. Nutrients 2020, 12, 750. [Google Scholar] [CrossRef]
- Jeanes, Y.M.; Barr, S.; Smith, K.; Hart, K.H. Dietary management of women with polycystic ovary syndrome in the United Kingdom: The role of dietitians. J. Hum. Nutr. Diet. 2009, 22, 551–558. [Google Scholar] [CrossRef]
- Lin, A.W.; Dollahite, J.S.; Sobal, J.; Lujan, M.E. Health-Related knowledge, beliefs and self-efficacy in women with polycystic ovary syndrome. Hum. Reprod. 2018, 33, 91–100. [Google Scholar] [CrossRef]
- Institute, A.S. Britons Say No to Nanny! Modern Attitudes to Paternalism and State Provision; Adam Smith Institute: London, UK, 2012. [Google Scholar]
- Tomlinson, J.; Pinkney, J.; Adams, L.; Stenhouse, E.; Bendall, A.; Corrigan, O.; Letherby, G. The diagnosis and lived experience of polycystic ovary syndrome: A qualitative study. J. Adv. Nurs. 2017, 73, 2318–2326. [Google Scholar] [CrossRef]
- Cussons, A.J.; Stuckey, B.G.; Walsh, J.P.; Burke, V.; Norman, R.J. Polycystic ovarian syndrome: Marked differences between endocrinologists and gynaecologists in diagnosis and management. Clin. Endocrinol. 2005, 62, 289–295. [Google Scholar] [CrossRef]
- Pirotta, S.; Joham, A.J.; Moran, L.J.; Skouteris, H.; Lim, S.S. Implementation of evidence-based PCOS lifestyle management guidelines: Perceived barriers and facilitators by consumers using the Theoretical Domains Framework and COM-B Model. Patient Educ. Couns. 2021, 104, 2080–2088. [Google Scholar] [CrossRef]
- Cowan, S.; Sood, S.; Truby, H.; Dordevic, A.; Adamski, M.; Gibson, S. Inflaming Public Interest: A qualitative study of adult learners’ perceptions on nutrition and inflammation. Nutrients 2020, 12, 345. [Google Scholar] [CrossRef] [PubMed]
- Wansink, B. Position of the American Dietetic Association: Food and nutrition misinformation. J. Am. Diet. Assoc. 2005, 106, 601–607. [Google Scholar]
- Wang, Y.; McKee, M.; Torbica, A.; Stuckler, D. Systematic literature review on the spread of health-related misinformation on social media. Soc. Sci. Med. 2019, 240, 112552. [Google Scholar] [CrossRef] [PubMed]
- Chiu, W.L.; Kuczynska-Burggraf, M.; Gibson-Helm, M.; Teede, H.J.; Vincent, A.; Boyle, J.A. What can you find about polycystic ovary syndrome (PCOS) online? Assessing online information on PCOS: Quality, content, and user-friendliness. Semin. Reprod. Med. 2018, 36, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Moran, L.J.; Brown, W.J.; McNaughton, S.A.; Joham, A.E.; Teede, H.J. Weight management practices associated with PCOS and their relationships with diet and physical activity. Hum. Reprod. 2017, 32, 669–678. [Google Scholar] [CrossRef] [PubMed]
- Moran, L.J.; Ko, H.; Misso, M.; Marsh, K.; Noakes, M.; Talbot, M.; Frearson, M.; Thondan, M.; Stepto, N.; Teede, H.J. Dietary composition in the treatment of polycystic ovary syndrome: A systematic review to inform evidence-based guidelines. J. Acad. Nutr. Diet. 2013, 113, 520–545. [Google Scholar] [CrossRef] [PubMed]
- Ball, K.; Crawford, D.; Warren, N. How feasible are healthy eating and physical activity for young women? Public Health Nutr. 2004, 7, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Gormally, J.; Rardin, D. Weight loss and maintenance and changes in diet and exercise for behavioral counseling and nutrition education. J. Couns. Psychol. 1981, 28, 295. [Google Scholar] [CrossRef]
- Trost, S.G.; Hutley, J. Use of physical activity self-management strategies by high school students. Pediatr. Exerc. Sci. 2015, 27, 168–174. [Google Scholar] [CrossRef]
- Young, D.R.; Cohen, D.; Koebnick, C.; Mohan, Y.; Saksvig, B.I.; Sidell, M.; Wu, T. Longitudinal associations of physical activity among females from adolescence to young adulthood. J. Adolesc. Health 2018, 63, 466–473. [Google Scholar] [CrossRef]
- Spahn, J.M.; Reeves, R.S.; Keim, K.S.; Laquatra, I.; Kellogg, M.; Jortberg, B.; Clark, N.A. State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. J. Am. Diet. Assoc. 2010, 110, 879–891. [Google Scholar] [CrossRef]
- Creer, T.L.; Wigal, J.K. Self-efficacy. Chest 1993, 103, 1316–1318. [Google Scholar] [CrossRef]
- Curry, K.; Jaffe, A. Nutrition Counseling & Communication Skills; WB Saunders: Philadelphia, PA, USA, 1998. [Google Scholar]
- Thomson, P. Exercise and health: A review of the usefulness of behavioural change theories in helping patients to become habitually active. Int. J. Health Promot. Educ. 2000, 38, 10–18. [Google Scholar] [CrossRef]
- Bandura, A. Social cognitive theory: An agentic perspective. Annu. Rev. Psychol. 2001, 52, 1–26. [Google Scholar] [CrossRef] [PubMed]
- Kanfer, F.H.; Gaelick-Buys, L. Self-management methods. In Helping People Change: A Textbook of Methods; Pergamon Press: Oxford, UK, 1991. [Google Scholar]
- Blackshaw, L.C.; Chhour, I.; Stepto, N.K.; Lim, S.S. Barriers and facilitators to the implementation of evidence-based lifestyle management in polycystic ovary syndrome: A narrative review. Med. Sci. 2019, 7, 76. [Google Scholar] [CrossRef] [PubMed]
- Berciano, S.; Figueiredo, J.; Brisbois, T.D.; Alford, S.; Koecher, K.; Eckhouse, S.; Ciati, R.; Kussmann, M.; Ordovas, J.M.; Stebbins, K.; et al. Precision nutrition: Maintaining scientific integrity while realizing market potential. Front. Nutr. 2022, 9, 979665. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, K.M.; Ramos-Lopez, O.; Perusse, L.; Kato, H.; Ordovas, J.M.; Martínez, J.A. Precision nutrition: A review of current approaches and future endeavors. Trends Food Sci. Technol. 2022, 128, 253–264. [Google Scholar] [CrossRef]
- Kirk, D.; Catal, C.; Tekinerdogan, B. Precision nutrition: A systematic literature review. Comput. Biol. Med. 2021, 133, 104365. [Google Scholar] [CrossRef] [PubMed]
- Win, K.T.; Hassan, N.M.; Bonney, A.; Iverson, D. Benefits of online health education: Perception from consumers and health professionals. J. Med. Syst. 2015, 39, 27. [Google Scholar] [CrossRef]
| Variable | Value a |
|---|---|
| Weight (lb.) | 206.0 ± 56.4 |
| BMI (kg/m2) | 34.3 ± 8.9 |
| Weight category | |
| Underweight | 0.02 (13) |
| Normal | 14.7 (169) |
| Overweight | 18.2 (209) |
| Obesity | 65.0 (747) |
| Class I | 33.6 (251) |
| Class II | 28.9 (216) |
| Class III | 37.5 (280) |
| Experienced weight change > 5 lb. in last 3 months | 71.0 (892) |
| Weight loss | 30.5 (356) |
| Weight gain | 42.7 (498) |
| Race | |
| White | 78.4 (905) |
| Black | 6.7 (77) |
| Asian | 3.5 (40) |
| Other | 11.4 (101) |
| Country of birth | |
| United States | 70.0 (817) |
| Australia | 4.7 (55) |
| United Kingdom | 4.3 (50) |
| Canada | 3.3 (38) |
| Other | 17.7 (207) |
| Variable | Value a |
|---|---|
| Has a PCOS diagnosis from a health practitioner | 98.5 (1150) |
| By a general practitioner | 54.5 (636) |
| By a gynecologist | 20.7 (241) |
| By an endocrinologist | 18.6 (217) |
| By other | 5.1 (60) |
| Prescribed medication to regulate menstrual cycle or promote ovulation | 62.0 (724) |
| Metformin | 37.6 (439) |
| Oral Contraceptives | 30.7 (358) |
| Clomid or Letrozole | 7.0 (82) |
| Injectable insulin sensitizers | 0.4 (5) |
| Other | 11.8 (138) |
| Currently have excess body hair | 80.7 (942) |
| Currently has acne | 56.2 (656) |
| Current periods | |
| Regular (1/month) | 33.8 (394) |
| Irregular (>1/month) | 38.0 (443) |
| Irregular (<1/month) | 9.9 (115) |
| Absent (none within last 6 months) | 18.2 (212) |
| Presence of comorbidity | |
| Infertility | 38.2 (446) |
| Hypercholesterolemia | 15.0 (175) |
| Hypertension | 15.0 (175) |
| Hypothyroidism | 13.3 (155) |
| Gastro-esophageal reflux disease | 12.7 (148) |
| Irritable bowel syndrome with GERD | 10.3 (120) |
| Hypertriglyceridemia | 10.1 (118) |
| Eating Disorder | 8.5 (99) |
| Steatosis | 7.5 (88) |
| Irritable bowel syndrome without GERD | 5.5 (64) |
| Type 2 Diabetes | 5.0 (58) |
| Other | 19.1 (223) |
| Variable | Value a |
|---|---|
| Aware of national or international government guidelines for a healthy lifestyle in PCOS | 6.4 (75) |
| Currently follows formal dietary guidelines to manage PCOS | 33.3 (389) |
| American Diabetes Association | 23.9 (93) |
| MyPlate | 13.4 (52) |
| Dietary Guidelines for Americans | 10.5 (41) |
| DASH | 10.0 (39) |
| American Heart Association | 7.7 (30) |
| American Cancer Association Society | 0.8 (3) |
| Other b | 58.4 (227) |
| Low energy/low calories (includes Weight Watchers and other | 18.9 (43) |
| popular diet industry programs) | |
| Combination of diets (e.g., a plant-based ketogenic diet) | 14.5 (33) |
| Paleo | 9.7 (22) |
| Low-glycemic | 8.8 (20) |
| Low-carbohydrate/high-protein | 8.4 (19) |
| PCOS specific plans (includes | 6.6 (15) |
| Specialized (includes IBS friendly, autoimmune, or GAPS) | 5.3 (12) |
| Ketogenic | 4.4 (10) |
| Own research (though specific diet not defined) | 4.0 (9) |
| Whole food diet | 2.6 (6) |
| Low carb only | 2.2 (5) |
| Mediterranean | 0.9 (2) |
| Vegetarian | 0.9 (2) |
| Bariatric surgery | 0.9 (2) |
| Dietary principles outlined by NHS and/or WHO | 0.9 (2) |
| Sugar free | 0.4 (1) |
| Did not provide a written response | 10.6 (24) |
| Currently follows a special diet to manage PCOS | 57.3 (667) |
| Low-carbohydrate/high-protein | 63.4 (423) |
| Low-glycemic | 36.6 (244) |
| Gluten-free | 31.8 (212) |
| Dairy-free | 30.4 (203) |
| Low-energy/calorie | 19.8 (132) |
| Soy-free | 17.5 (117) |
| Paleolithic/Paleo | 13.5 (90) |
| Low-fat | 12.7 (85) |
| Vegetarian/vegan | 12.0 (80) |
| High omega-3 | 9.3 (62) |
| Ketogenic | 4.6 (31) |
| Low-FODMAP | 2.7 (18) |
| Aware of 2008 Physical Activity Guidelines for Americans | 13.4 (156) |
| Currently follows formal PA guidelines to manage PCOS | 16.2 (189) |
| Engages in regular physical activity c | 52.4 (611) |
| Combination of strength and cardio training (including HIIT) | 58.8 (359) |
| Combination of cardio (including walking and swimming, walking | 16.4 (100) |
| and cycling, running and cycling, etc.) | |
| Walking only | 13.9 (85) |
| Yoga/Pilates | 3.3 (20) |
| Strength training only | 2.3 (14) |
| Running only | 1.1 (7) |
| Cycling only | 1.1 (7) |
| Aqua aerobics/swimming only | 0.5 (3) |
| Horse riding | 0.3 (2) |
| Manual work (including gardening and cleaning) | 0.3 (2) |
| Organized sport (including basketball and football) | 0.3 (2) |
| Did not provide a written response | 1.6 (10) |
| Diet | Overall Dietary Management Score | 2.99 ± 1.22 | |
| Cognitive strategies | Mean ± SD | Behavioral strategies | Mean ± SD |
| I make plans to change my diet/drinking habits. | 3.39 ± 1.10 | I read labels to help me choose healthy foods | 3.50 ± 1.23 |
| I look for information about nutrition and healthy eating from books, magazines, internet etc. | 3.30 ± 1.31 | I eat healthy food | 3.24 ± 0.91 |
| If I don’t eat healthy foods, I think about ways to do better next time. | 3.21 ± 1.19 | I watch what I eat | 3.19 ± 1.13 |
| I can stop myself from over eating | 2.97 ± 1.17 | I watch my weight | 3.23 ± 1.25 |
| I make sure I have time to prepare healthy meals | 2.84 ± 1.17 | I have food available for quick healthy meals | 2.87 ± 1.15 |
| I decide what to eat at the last minute | 2.79 ± 1.01 | I replace snacks with healthy alternatives | 2.98 ± 1.00 |
| I say positive things to myself about eating healthy food | 2.79 ± 1.28 | I weigh myself regularly | 2.94 ± 1.37 |
| I seek information about my weight from my GP | 2.09 ± 1.19 | I keep track of what I eat and how much I should eat | 2.62 ± 1.23 |
| Physical activity | Overall physical activity management score | 2.96 ± 1.27 | |
| Cognitive strategies | Mean ± SD | Behavioral strategies | Mean ± SD |
| I know when I should do more activity | 3.64 ± 1.14 | I do things to make walking or other activities enjoyable | 2.90 ± 1.19 |
| I think about the benefits of being active | 3.64 ± 1.10 | I plan ahead of time to be active | 2.78 ± 1.25 |
| I try to think more about the benefits of physical activity and less the hassles of being active | 3.28 ± 1.11 | I can stick to my plans and be active each week | 2.68 ± 1.09 |
| When I set goals I choose activities that I enjoy | 3.17 ± 1.12 | I keep track of how much physical activity I do each week | 3.39 ± 1.24 |
| I read articles about the benefits of being active from magazines, books or the internet. | 3.06 ± 1.20 | When I get off track with my physical activity I find ways to get back on track | 2.54 ± 1.23 |
| I ask my friends and family to walk with me to help me stay active | 2.40 ± 1.30 | ||
| I make back up plans to make sure I get enough physical activity | 2.10 ± 1.20 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cowan, S.; Grassi, A.; Monahan Couch, L.; Jeanes, Y.; Lim, S.; Pirotta, S.; Harris, J.; McGirr, C.; Moran, L. Evidence-Based Lifestyle Guidelines and Self-Management Strategies Utilized by Women with Polycystic Ovary Syndrome. Nutrients 2023, 15, 589. https://doi.org/10.3390/nu15030589
Cowan S, Grassi A, Monahan Couch L, Jeanes Y, Lim S, Pirotta S, Harris J, McGirr C, Moran L. Evidence-Based Lifestyle Guidelines and Self-Management Strategies Utilized by Women with Polycystic Ovary Syndrome. Nutrients. 2023; 15(3):589. https://doi.org/10.3390/nu15030589
Chicago/Turabian StyleCowan, Stephanie, Angela Grassi, Lynn Monahan Couch, Yvonne Jeanes, Siew Lim, Stephanie Pirotta, Jeff Harris, Caroline McGirr, and Lisa Moran. 2023. "Evidence-Based Lifestyle Guidelines and Self-Management Strategies Utilized by Women with Polycystic Ovary Syndrome" Nutrients 15, no. 3: 589. https://doi.org/10.3390/nu15030589
APA StyleCowan, S., Grassi, A., Monahan Couch, L., Jeanes, Y., Lim, S., Pirotta, S., Harris, J., McGirr, C., & Moran, L. (2023). Evidence-Based Lifestyle Guidelines and Self-Management Strategies Utilized by Women with Polycystic Ovary Syndrome. Nutrients, 15(3), 589. https://doi.org/10.3390/nu15030589








