A Systematic Review of Healthy Nutrition Intervention Programs in Kindergarten and Primary Education
Abstract
1. Introduction
1.1. Influence of the Socialization
1.2. Consequences of Diet-Related Health Problems
1.3. Healthy Nutrition Intervention Programs at Schools
1.4. Objetive
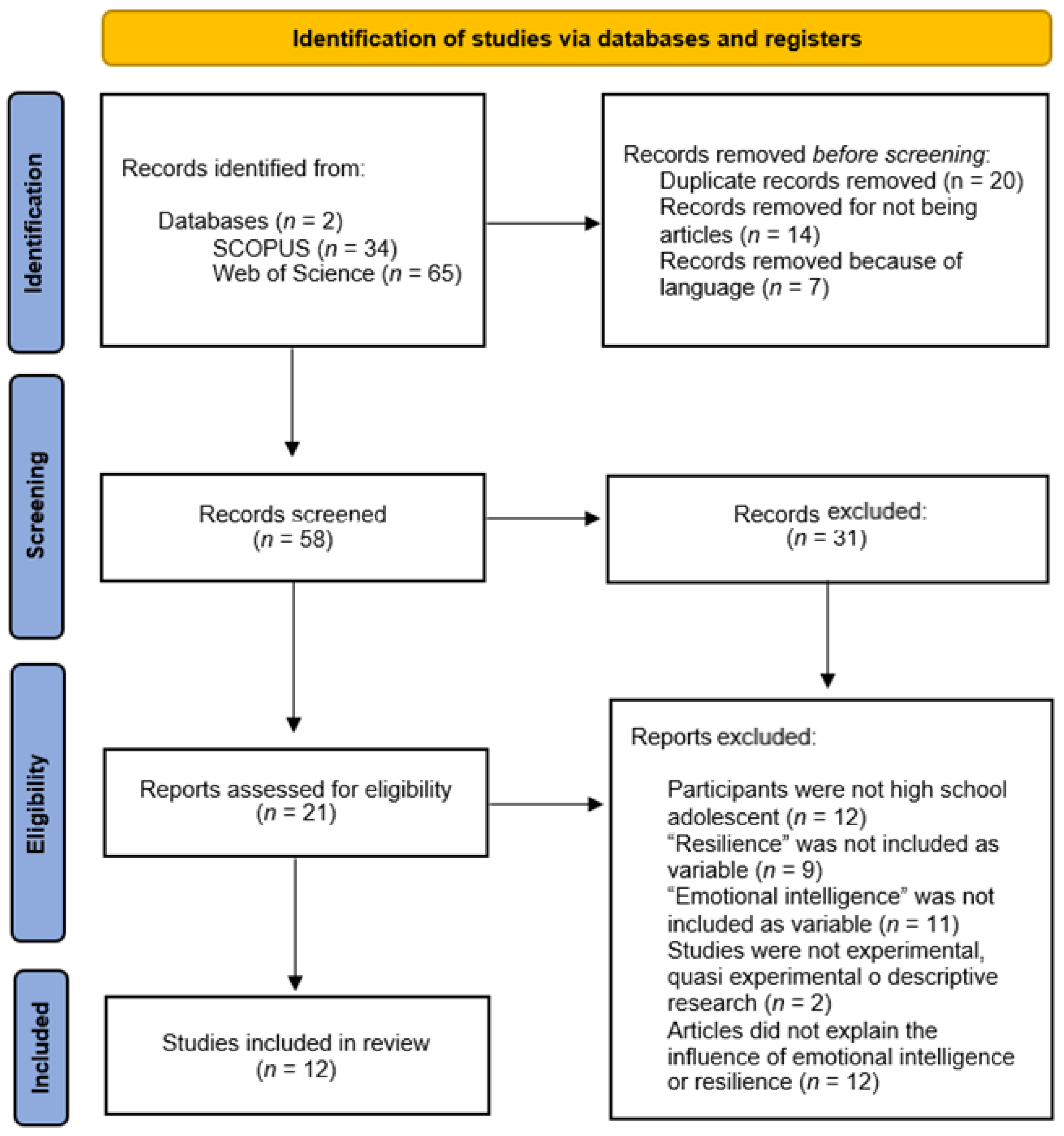
2. Materials and Methods
2.1. Literature Search
- (“PRE” AND “POST” OR “intervention program”) AND (“dietary behaviour” OR “healthy food” OR “healthy eating” OR “healthy diet” OR “healthy nutrition” OR “healthy habits”) AND (“children” “education” OR “early childhood education” OR “childhood education” OR “childhood school” OR “pre-primary education” OR “infant education” OR “infant school” OR “kindergarten education” OR “nursery education” OR “preschool education” OR “early education”);
- (“PRE” AND “POST”) AND (“dietary behavior” OR “healthy food” OR “healthy eating” OR “healthy diet” OR “healthy nutrition” OR “healthy habits”) AND (“primary school” OR “elementary school” OR “primary education” OR “elementary education” OR “primary students” OR “elementary students”).
2.2. Inclusion and Exclusion Criteria
- Articles from scientific journals were accepted, whereas other types of studies such as gray literature were refused;
- Participants sample had to be made up of preschool of school children, and studies with post-primary, teachers or families as samples were refused;
- Experimental or quasi-experimental articles were accepted, while articles without an intervention program, a pre- and post-intervention, or experimental group were refused;
- Nutrition intervention programs in pre-primary or primary schools were included, whereas we refused articles whose variables were different from eating diet, for instance, physical activity, food wasted, smart devices, hand washing, academic achievement, or teachers’ attitudes, among others;
- Articles with open access and the Spanish or English language were included. We refused articles to which we did not have full access or which were written in other languages.
2.3. Article Selection and Data Extraction
2.4. Study Quality Assessment
3. Results
3.1. Study Characteristics
3.2. Outcomes
3.2.1. Nutritional Knowledge
3.2.2. Body Weight and Body Mass Index (BMI)
3.2.3. Eating Behaviors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 25 November 2022).
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Willett, W.C. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Australian Dietary Guidelines: Eat for Health; National Health and Medical Research Council: Canberra, Australia, 2013; pp. 1–226.
- LaCaille, L. Eating Behavior. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 641–642. [Google Scholar]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Family Med. Prim. Care 2015, 4, 187–192. [Google Scholar] [PubMed]
- Jaacks, L.M.; Kavle, J.; Perry, A.; Nyaku, A. Programming maternal and child overweight and obesity in the context of undernutrition: Current evidence and key considerations for low- and middle-income countries. Public Health Nutr. 2017, 20, 1286–1296. [Google Scholar] [CrossRef] [PubMed]
- Romieu, I.; Dossus, L.; Barquera, S.; Blottière, H.M.; Franks, P.W.; Gunter, M.; Hwala, N.; Hursting, S.D.; Leitzmann, M.; Margetts, B.; et al. Energy balance and obesity: What are the main drivers? Cancer Causes Control 2017, 28, 247–258. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Levels and Trends in child Malnutrition: UNICEF/WHO/The World Bank Group Joint Child Malnutrition Estimates: Key Findings of the 2021 Edition. Available online: https://www.who.int/publications/i/item/9789240025257 (accessed on 25 November 2022).
- Guevara, R.M.; Urchaga, J.D.; Cabaco, A.S.; Moral-García, J.E. The quality of breakfast and healthy diet in school-aged adolescents and their association with bmi, weight loss diets and the practice of physical activity. Nutrients 2020, 12, 2294. [Google Scholar] [CrossRef]
- Popkin, B.M. Nutrition transition and the global diabetes epidemic. Curr. Diab. Rep. 2015, 15, 64–78. [Google Scholar] [CrossRef]
- Indrayana, S.; Palupi, N.S. Strategi implementasi pencantuman informasi kandungan gula, garam, dan lemak untuk pencegahan risiko penyakit Tidak Menular. Mutu Pangan 2014, 1, 156–164. [Google Scholar]
- Pervin, R.; Hossain, M.A.; Debnath, D.; Nath, B.D. Epidemiological perspectives of dietary sugars, salts and fats. Diet Sugar Salt Fat. Hum. Health 2020, 3, 3–23. [Google Scholar]
- Bentley, G.F.; Turner, K.M.; Jago, R. Mothers’ views of their preschool child’s screen-viewing behaviour: A qualitative study. BMC Public Health 2016, 16, 718. [Google Scholar] [CrossRef]
- Gomes, T.N.; Katzmarzyk, P.T.; Hedeker, D.; Fogelholm, M.; Standage, M.; Onywera, V.; Lambert, E.; Tremblay, M.S.; Chaput, J.-P.; Tudor-Locke, C.; et al. Correlates of compliance with recommended levels of physical activity in children. Sci. Rep. 2017, 7, 16507. [Google Scholar] [CrossRef]
- Kilanowski, J.F. Influences on healthy-eating decision making in latino adolescent children of migrant and seasonal agricultural workers. J. Pediatr. Health Care 2016, 30, 224–230. [Google Scholar] [CrossRef]
- Baker, S.; Morawska, A.; Mitchell, A. Promoting children’s healthy habits through self-regulation via parenting. Clin. Child Fam. Psychol. Rev. 2019, 22, 52–62. [Google Scholar] [CrossRef]
- Saraiva, J.F.K.; Slonczewski, T.; Clisnei, I.M.M. Estratégias interdisciplinares na abordagem do risco cardiovascular para combate à obesidade infantil. Rev. Soc. Bras. Clin. Med. 2017, 15, 214–220. [Google Scholar]
- Muftuoglu, S.; Bayram, S. Determination of the relationship between nutrition habits, social physique anxiety, and physical activity levels of adolescent students. World Nutr. 2020, 11, 62–74. [Google Scholar] [CrossRef]
- López, L.M.J. Condición física y rendimiento académico. J. Sport Health Res. 2018, 10, 349–360. [Google Scholar]
- UNICEF Indonesia. Indonesia: Obesity Rates among Adults Double over Past Two Decades. Indonesia: UNICEF Indonesia-Press Release. Available online: https://www.unicef.org/indonesia/press-releases/indonesia-obesity-rates-among-adults-double-over-past-two-decades (accessed on 26 November 2022).
- World Health Organization WHO. Report of the Comission on Ending Childhood Obesity. Available online: https://www.who.int/publications/i/item/9789241510066 (accessed on 26 November 2022).
- World Health Organization. Cardiovascular Diseases. Available online: https://www.who.int/health-topics/cardiovascular-diseases/#tab=tab_1 (accessed on 26 November 2022).
- American Heart Association. Coronary Heart Disease. Available online: https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/coronary-artery-disease (accessed on 26 November 2022).
- de Ferranti, S.D.; Steinberger, J.; Ameduri, R.; Baker, A.; Gooding, H.; Kelly, A.S.; Mietus-Snyder, M.; Mitsnefes, M.M.; Peterson, A.L.; St-Pierre, J.; et al. Cardiovascular risk reduction in high-risk pediatric patients: A scientific statement from the American Heart Association. Circulation 2019, 139, e603–e634. [Google Scholar] [CrossRef]
- Delgado-Noguera, M.; Tort, S.; Martinez-Zapata, M.J.; Bonfill, X. Primary school interventions to promote fruit and vegetable consumption: A systematic review and meta-analysis. Prev. Med. 2011, 53, 3–9. [Google Scholar] [CrossRef]
- Nathan, N.; Wolfenden, L.; Butler, M.; Bell, A.C.; Wyse, R.; Campbell, E.; Milat, A.J.; Wiggers, J. Vegetable and fruit breaks in Australian primary schools: Prevalence, attitudes, barriers and implementation strategies. Health Educ. Res. 2011, 26, 722–731. [Google Scholar] [CrossRef]
- Oostindjer, M.; Aschemann-Witzel, J.; Wang, Q.; Skuland, S.E.; Egelandsdal, B.; Amdam, G.V.; Schjøll, A.; Pachucki, M.C.; Rozin, P.; Stein, J.; et al. Are school meals a viable and sustainable tool to improve the healthiness and sustainability of children´s diet and food consumption? A cross-national comparative perspective. Crit. Rev. Food Sci. Nutr. 2017, 57, 3942–3958. [Google Scholar] [CrossRef]
- Ismail, M.R.; Seabrook, J.A.; Gilliland, J.A. Outcome evaluation of fruits and vegetables distribution interventions in schools: A systematic review and meta-analysis. Public Health Nutr. 2021, 19, 1–13. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Nutrition Education in US Schools. Available online: https://www.cdc.gov/healthyschools/nutrition/school_nutrition_education.htm (accessed on 28 November 2022).
- Craigie, A.M.; Lake, A.A.; Kelly, S.A.; Adamson, A.J.; Mathers, J.C. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas 2011, 70, 266–284. [Google Scholar] [CrossRef] [PubMed]
- Langford, R.; Bonell, C.; Jones, H.; Pouliou, T.; Murphy, S.; Waters, E.; Komro, K.; Gibbs, L.; Magnus, D.; Campbell, R. The World Health Organization’s Health Promoting Schools framework: A Cochrane systematic review and meta-analysis. BMC Public Health 2015, 15, 130. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Expert Committee on Comprehensive School Health Education and Promotion. In Promoting Health through Schools: Report of a WHO Expert Committee on Comprehensive School Health Education and Promotion; World Health Organization: Geneva, Switzerland, 1997; Available online: https://apps.who.int/iris/handle/10665/41987 (accessed on 15 December 2022).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Marshall, A.N.; Markham, C.; Ranjit, N.; Bounds, G.; Chow, J.; Sharma, S.V. Long-term impact of a school-based nutrition intervention on home nutrition environment and family fruit and vegetable intake: A two year follow-up study. PRM 2020, 20, 101247. [Google Scholar] [CrossRef] [PubMed]
- Fisher, M.C.; Villegas, E.; Sutter, C.; Musaad, S.M.; Koester, B.; Fiese, B.H. Sprouts Growing Healthy Habits: Curriculum Development and Pilot Study. Front. Public Health 2019, 7, 65. [Google Scholar] [CrossRef]
- Lynch, B.A.; Gentile, N.; Maxson, J.; Quigg, S.; Swenson, L.; Kaufman, T. Elementary School-Based Obesity Intervention Using an Educational Curriculum. J. Prim. Care Community Health 2016, 7, 265–271. [Google Scholar] [CrossRef]
- Sharma, S.V.; Shegog, R.; Chow, J.; Finley, C.; Pomeroy, M.; Smith, C.; Hoelscher, D.M. Effects of the Quest to Lava Mountain Computer Game on Dietary and Physical Activity Behaviors of Elementary School Children: A Pilot Group-Randomized Controlled Trial. J. Acad. Nutr. Diet. 2015, 115, 1260–1271. [Google Scholar] [CrossRef]
- Song, H.-J.; Grutzmacher, S.; Munger, A.L. Project ReFresh: Testing the Efficacy of a School-Based Classroom and Cafeteria Intervention in Elementary School Children. J. School Health 2016, 86, 543–551. [Google Scholar] [CrossRef]
- Teo, C.H.; Chin, Y.S.; Lim, P.Y.; Masrom, S.A.H.; Shariff, Z.M. Impacts of a School-Based Intervention That Incorporates Nutrition Education and a Supportive Healthy School Canteen Environment among Primary School Children in Malaysia. Nutrients 2021, 13, 1712. [Google Scholar] [CrossRef]
- Siew, C.Y.; Siong, T.E.; Hashim, Z.; Raqi, R.A.; Karim, N.A. Effectiveness of a Nutrition Education Intervention for Primary School Children: The Healthy Kids Programme, Malaysia. Mal. J. Med. Health Sci. 2020, 16, 1–10. [Google Scholar]
- Qian, L.; Newman, I.M.; Yuen, L.W.; Du, W.; Shell, D. Effects of a comprehensive nutrition education programme to change grade 4 primary-school students’ eating behaviours in China. Public Health Nutr. 2019, 22, 903–911. [Google Scholar] [CrossRef]
- Zhou, J. Results form a Quasi-experimental Study of a Training Intervention for Healthy Eating Behaviors of Students. NeuroQuantology 2018, 16, 19–24. [Google Scholar] [CrossRef]
- García, E.; Fernández, G. Educational intervention through a gamification proposal to improve the adherence to the Mediterranean diet in Galician primary schools students. Reto 2022, 44, 128–135. [Google Scholar] [CrossRef]
- Øvrebø, B.; Stea, T.H.; Bergh, I.H.; Bere, E.; Surén, P.; Magnus, P.; Juliusson, P.B.; Wills, A.K. A nationwide school fruit and vegetable policy and childhood and adolescent overweight: A quasi-natural experimental study. PLoS Med. 2022, 19, e1003881. [Google Scholar] [CrossRef]
- Karpouzis, F.; Lindberg, R.; Walsh, A.; Shah, S.; Abbott, G.; Lai, J.; Berner, A.; Ball, K. Evaluating OzHarvest’s primary-school Food Education and Sustainability Training (FEAST) program in 10-12-year-old children in Australia: Protocol for a pragmatic cluster non-randomized controlled trial. BMC Public Health 2021, 21, 967. [Google Scholar] [CrossRef]
- Franceschi, R.; Fornari, E.; Ghezzi, M.; Buzzi, E.; Toschi, M.; Longhi, S.; Maimone, R.; Forti, S.; Carneri, S.; Pirous, F.M.; et al. Educational Intervention of Healthy Life Promotion for Children with a Migrant Background or at Socioeconomic Disadvantage in the Nort of Italy: Efficacy of Telematic Tools in Improving Nutritional and Physical Activity Knowledge. Nutrients 2021, 13, 3634. [Google Scholar] [CrossRef]
- Nickel, N.C.; Doupe, M.; Enns, J.E.; Brownell, M.; Sarkar, J.; Chateau, D.; Burland, E.; Chartier, M.; Katz, A.; Crockett, L.; et al. Differential effects of a school-based obesity prevention program: A cluster randomized trial. Matern. Child Nutr. 2021, 17, e13009. [Google Scholar] [CrossRef]
- Ben Cheikh, A.; Maatoug, J.; Ghammam, R.; Chouikha, F.; Mallat, A.; Ghannem, H. Effect of a school-based intervention in eating habits among school children: Quasi experimental study, Tunisia. Adoles. Med. Health 2020, 33, 157–164. [Google Scholar] [CrossRef]
- Verdonschot, A.; de Vet, E.; van Rossum, J.; Mesch, A.; Collins, C.E.; Bucher, T.; Haveman-Nies, A. Education or Provision? A Comparison of Two School-Based Fruit and Vegetable Nutrition Education Programs in the Netherlands. Nutrients 2020, 12, 3280. [Google Scholar] [CrossRef]
- Lin, Y.-C.; Chen, H.-J.; Wang, Y.; Min, J.; Wu, H.-C.; Carvajal, N.A.; Yang, H.-Y. NASA Mission X program for healthy eating and active living among Taiwanese elementary school students. J. Pediatr. Nurs. 2019, 49, E8–E14. [Google Scholar] [CrossRef]
- Kim, J.; Kim, G.; Park, J.; Wang, Y.; Lim, H. Effectiveness of Teacher-Led Nutritional Status in Preschool Children: Adoption of a NASA Mission X-Based Program. Nutrients 2019, 11, 1590. [Google Scholar] [CrossRef] [PubMed]
- Brown, E.C.; Buchan, D.S.; Drignei, D.; Wyatt, F.B.; Kilgore, L.; Cavana, J.; Baker, J.S. Primary School Children’s Health Behaviors, Attitudes, and Body Mass Index After a 10-Week Lifestyle Intervention with Follow-up. Front. Pediatr. 2018, 6, 178–181. [Google Scholar] [CrossRef] [PubMed]
- Dudley, D.A.; Cotton, W.G.; Peralta, L.R. Teaching approaches and strategies that promote healthy eating in primary school children: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Antwi, J. Nutrition education impact on nutrition knowledge, attitude and practice of schoolchildren: A pilot study in Ghana. Curr. Dev. Nutr. 2020, 4, 1287. [Google Scholar] [CrossRef]
- Morano, M.; Robazza, C.; Bortoli, L.; Rutigliano, I.; Ruiz, M.C.; Campanozzi, A. Physical activity and physical competence in overweight and obese children: An intervention study. Int. J. Environ. Res. Public Health 2020, 17, 6370. [Google Scholar] [CrossRef]
- Habib-Mourad, C.; Ghandour, L.A.; Maliha, C.; Dagher, M.; Kharroubi, S.; Hwalla, N. Impact of a three-year obesity prevention study on healthy behaviors and BMI among Lebanese schoolchildren: Findings from ajyal salima program. Nutrients 2020, 12, 2687. [Google Scholar] [CrossRef]
- Murimi, M.W.; Moyeda-Carabaza, A.F.; Nguyen, B.; Saha, S.; Amin, R.; Njike, V. Factors that contribute to effective nutrition education interventions in children: A systematic review. Nutr. Rev. 2018, 76, 553–580. [Google Scholar] [CrossRef]
- Qian, Y.; Nayga, R.M.; Thomsen, J.M.R.; Rouse, H.L. The effect of the Fresh Fruit and Vegetable Program on childhood obesity. Appl. Econ. Perspect. Policy 2016, 38, 260–275. [Google Scholar] [CrossRef]
- Fogarty, A.W.; Antoniak, M.; Venn, A.J.; Davies, L.; Goodwin, A.; Salfield, N.; Stocks, J.; Britton, J.; Lewis, S.A. Does participation in a population- based dietary intervention scheme have a lasting impact on fruit intake in young children? Int. J. Epidemiol. 2007, 36, 1080–1085. [Google Scholar] [CrossRef]
- Bere, E.; Hilsen, M.; Klepp, K.I. Effect of the nationwide free school fruit scheme in Norway. Br. J. Nutr. 2010, 104, 589–594. [Google Scholar] [CrossRef]
- Evans, C.E.; Christian, M.S.; Cleghorn, C.L.; Greenwood, D.C.; Cade, J.E. Systematic review and meta-analysis of school-based interventions to improve daily fruit and vegetable intake in children aged 5 to 12 y. Am. J. Clin. Nutr. 2012, 96, 889–901. [Google Scholar] [CrossRef]
- Arnotti, K.; Bamber, M. Fruit and vegetable consumption in overweight or obese individuals: A meta-analysis. West J. Nurs. Res. 2020, 42, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Guyenet, S.J. Impact of whole, fresh fruit consumption on energy intake and adiposity: A systematic review. Front. Nutr. 2019, 6, 66. [Google Scholar] [CrossRef]
- Fries, M.; van Dongen, E.; Haveman-Nies, A. Evaluatie van Smaaklessen: Heeft Smaaklessen Eect op Determinanten van Gezond en Bewust Eetgedrag? Leerstoelgroep Humane Voeding: Wageningen, The Netherlands, 2013. [Google Scholar]
- De Villiers, A.; Steyn, N.P.; Draper, C.E.; Hill, J.; Gwebushe, N.; Lambert, E.V.; Lombard, C. Primary school children’s nutrition knowledge, self-ecacy, and behavior, after a three-year healthy lifestyle intervention (HealthKick). Ethn. Dis. 2016, 26, 171. [Google Scholar] [CrossRef]
- Godino, J.G.; Merchant, G.; Norman, G.; Donohue, M.C.; Marshall, S.J.; Fowler, J.H.; Calfas, K.J.; Huang, J.; Rock, C.L.; Griswold, W.G.; et al. Using social and mobile tools for weight loss in overweight and obese young adults (Project SMART): A 2 year, parallel-group, randomised, controlled trial. Lancet Diabetes Endocrinol. 2016, 4, 747–755. [Google Scholar] [CrossRef]
- Raaijmakers, L.C.; Pouwels, S.; Berghuis, K.A.; Nienhuijs, S.W. Technology-based interventions in the treatment of overweight and obesity: A systematic review. Appetite 2015, 95, 138–151. [Google Scholar] [CrossRef]
- David, T.; Julien, A.; Laurie, I.; Nordine, L.; Sébastien, R.; Eric, D.; Martine, M.; Pascale, D. Are eating habits associated with physical fitness in primary school children? Eat. Behav. 2013, 14, 83–86. [Google Scholar] [CrossRef]
- Meyer, P.A.; Yoon, P.W.; Kaufmann, R.B. Introduction: CDC Health Disparities and Inequalities Report-United States. In CDC Health Disparities and Inequalities Report–US, 2013; Moolenaar, R.L., Ed.; MMWR: NJ, USA, 2013; Volume 62, pp. 3–5. [Google Scholar]
- Jones, M.; Pitt, H.; Oxford, L.; Bray, I.; Kimberlee, R.; Orme, J. Association between Food for Life, a whole setting healthy and sustainable food programme, and primary school children’s consumption of fruit and vegetables: A cross-sectional study in England. Int. J. Environ. Res. Public Health 2017, 14, 639. [Google Scholar] [CrossRef]
- Aarestrup, A.K.; Jørgensen, T.S.; Jørgensen, S.E.; Hoelscher, D. Implementation of strategies to increase adolescents’ access to fruit and vegetables at school: Process evaluation findings from the Boost study. BMC Public Health 2015, 15, 86. [Google Scholar] [CrossRef]
- Weber, K.S.; Eitner, J.; Dauben, L.; Spörkel, O.; Strassburger, K.; Sommer, J.; Kaiser, B.; Buyken, A.E.; Kronsbein, P.; Müssig, K. Positive Effects of Practical Nutrition Lessons in a Primary School Setting with a High Proportion of Migrant School Children. Exp. Clin. Endocrinol. Diabetes 2020, 128, 111–118. [Google Scholar] [CrossRef]
- Sharif Ishak, S.; Chin, Y.S.; Mohd Taib, M.N.; Chan, Y.M.; Shariff, Z.M. Effectiveness of a school-based intervention on knowledge, attitude and practice on healthy lifestyle and body composition in Malaysian adolescents. BMC Pediatr. 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Asakura, K.; Todoriki, H.; Sasaki, S. Relationship between nutrition knowledge and dietary intake among primary school children in Japan: Combined effect of children’s and their guardians’ knowledge. J. Epidemiol. 2017, 27, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Mistretta, A.; Turconi, G.; Cena, H.; Roggi, C.; Galvano, F. Nutrition knowledge and other determinants of food intake and lifestyle habits in children and young adolescents living in a rural area of Sicily, South Italy. Public Health Nutr. 2013, 16, 1827–1836. [Google Scholar] [CrossRef] [PubMed]
- Durlak, J.A.; Weissberg, R.P.; Dymnicki, A.B.; Taylor, R.D.; Schellinger, K.B. The impact of enhancing students’ social and emotional learning: A meta-analysis of school-based universal interventions. Child. Dev. 2011, 82, 405–432. [Google Scholar] [CrossRef] [PubMed]
- Reilly, K.L.; Nathan, N.; Wiggers, J.; Yoong, S.L.; Wolfenden, L. Scale up of a multi-strategic intervention to increase implementation of a school healthy canteen policy: Findings of an intervention trial. BMC Public Health 2018, 18, 860. [Google Scholar] [CrossRef]
- Øverby, N.C.; Klepp, K.-I.; Bere, E. Introduction of a school fruit program is associated with reduced frequency of consumption of unhealthy snacks. Am. J. Clin. Nutr. 2012, 96, 1100–1103. [Google Scholar] [CrossRef]
- Makeeva, A. What can be changed by nutrition education? Evaluation of the educational influence on children’s behaviour and nutritional knowledge. Educ. Health 2015, 33, 14–19. [Google Scholar]
- Roberts, K.C.; Shields, M.; de Groh, M.; Aziz, A.; Gilbert, J.-A. Overweight and obesity in children and adolescents: Results from the 2009 to 2011 Canadian Health Measures Survey. Health Rep. 2012, 23, 37–41. [Google Scholar]
- Aday, L.A.; Cornelius, L.J. Designing and Conducting Health Surveys: A Comprehensive Guide; John Wiley & Sons: Hoboken, NJ, USA, 2006. [Google Scholar]
- Sutherland, R.; Campbell, E.; Lubans, D.R.; Morgan, P.J.; Okely, A.D.; Nathan, N.; Wolfenden, L.; Wiese, J.; Gillham, K.; Hollis, J.; et al. ‘Physical Activity 4 Everyone’ school-based intervention to prevent decline in adolescent physical activity levels: 12 month (mid-intervention) report on a cluster randomised trial. Br. J. Sports Med. 2015, 50, 488–495. [Google Scholar] [CrossRef]
- Kothandan, S.K. School based interventions versus family based interventions in the treatment of childhood obesity—A systematic review. Arch. Public Health 2014, 72, 3. [Google Scholar] [CrossRef]
- Sobol-Goldberg, S.; Rabinowitz, J.; Gross, R. School-based obesity prevention programs: A meta-analysis of randomized controlled trials. Obesity 2013, 21, 2422–2428. [Google Scholar] [CrossRef]
- Dobbins, M.; Husson, H.; DeCorby, K.; LaRocca, R.L. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2013, 2, CD007651. [Google Scholar] [CrossRef]
- Williams, A.J.; Henley, W.E.; Williams, C.A.; Hurst, A.J.; Logan, S.; Wyatt, K.M. Systematic review and meta-analysis of the association between childhood overweight and obesity and primary school diet and physical activity policies. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 101. [Google Scholar] [CrossRef]
- Tucker, S.; Lanningham-Foster, L.; Murphy, J.; Olsen, G.; Orth, K.; Voss, J.; Aleman, M.; Lohse, C. A school-based community partnership for promoting healthy habits for life. J. Community Health 2011, 36, 414–422. [Google Scholar] [CrossRef]
- Waters, E.; De Silva-Sanigorski, A.; Burford, B.J.; Brown, T.; Campbell, K.J.; Gao, Y.; Armstrong, R.; Prosser, L.; Summerbell, C.D. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2011, 12, CD001871. [Google Scholar] [CrossRef]
- Wind, M.; Bjelland, M.; Pérez-Rodrigo, C.; Te Velde, S.J.; Hildonen, C.; Bere, E.; Klepp, K.I.; Brug, J. Appreciation and implementation of a school-based intervention are associated with changes in fruit and vegetable intake in 10- to 13-year old schoolchildren–the Pro Children study. Health Educ. Res. 2008, 23, 997–1007. [Google Scholar] [CrossRef]
- Schlechter, C.R.; Rosenkranz, R.R.; Guagliano, J.M.; Dzewaltowski, D.A. A systematic review of children’s dietary interventions with parents as change agents: Application of the RE-AIM framework. Prev. Med. 2016, 91, 233–243. [Google Scholar] [CrossRef]
- Sharifah, S.I.; Chin, Y.S.; Mohd, M.T.; Zalilah, M.S. School-based intervention to prevent overweight and disordered eating in secondary school Malaysian adolescents: A study protocol. BMC Public Health 2016, 16, 1101. [Google Scholar]
- Sabramani, V.; Idayu, I.; Rosnah, S.; Zaleha, M.I.; Saidatul, N.B.; Hasanain, F.G. Managing obesity in Malaysian schools: Are we doing the right strategies? Mal. J. Public Health Med. 2015, 15, 75–83. [Google Scholar]
- Van Stralen, M.M.; Yildirim, M.; te Velde, S.J.; Brug, J.; van Mechelen, W.; Chinapaw, M.J. What works in school-based energy balance behaviour interventions and what does not: A systematic review of mediating mechanisms. Int. J. Obes. 2011, 35, 1251–1265. [Google Scholar] [CrossRef]
| Authors | Sample | Country | Variables | Instruments |
|---|---|---|---|---|
| García and Fernández 2022 [43] | 38 students 6–7 years old | Spain | - Gamification experience and gender - Adherence to the Mediterranean diet | - Mediterranean diet adherence questionnaire to analyze participants’ nutritional variables |
| Øvrebø et al. 2022 [44] | 11215 students 8–13 years old | Norway | - Age - Weight - Height - Waist circumference (WC) - Parents’ education level | - Tape measure - Electronic fat control scale - Wall-mounted stadiometer with 0.1 cm accuracy for height measurement - Questionnaire for parents on level of education |
| Karpouzis et al. 2021 [45] | 20 students 10–12 years old | Australia | - Dietary patterns - Nutrition knowledge - Cooking skills - Food-wasting behaviors | - Surveys and questionnaires on child nutrition, cooking skills, and food waste behavior |
| Franceschi et al. 2021 [46] | 695 students 6–14 years old | Italy | - Weight - Height - BMI - Socio-economic status - Physical activity level - Nutritional habits | - Questionnaires on knowledge about nutrition and physical activity - Questionnaires on children’s eating habits |
| Teo et al. 2021 [39] | 523 students 7–11 years old | Malaysia | - Socio-demographic data - Dietary behavior - Physical activity level - Weight - Height - Cognitive performance | - Questionnaires for parents on the demographic characteristics of their children - Eating Behavior Questionnaire (EBQ) - Physical Activity Questionnaire for Children (PAQ-C) - Seca scale to measure body weight - Seca stadiometer to measure the height - Raven’s Colored Progressive Matrices (CPM) |
| Nickel et al. 2021 [47] | 311 students 6–12 years old | Canada | - Height - Weight - BMI - Sex - Family income level - Urban/rural residence - Dietary intake - Knowledge of healthy living - Level of self-efficacy | - Flexible measuring tape - Portable floor scale - Stadiometer - 26 questions on knowledge of healthy or unhealthy behaviors - 2-point scale to report how often they eat certain foods and to evaluate their level of self-efficacy |
| Ben Cheikh et al. 2020 [48] | 558 students 6–12 years old | Tunisia | - Calories consumed in the morning snack | - Questionnaire for parents on demographic characteristics and eating habits of their children - Questionnaire for children on snacks consumed and their composition |
| Marshall et al. 2020 [34] | 717 students 5–7 years old | United States | - Socio-demographic data - Dietary intake | - Food Frequency Questionnaire - Block Kids Food Screener (BKFS) - Surveys for parents to collect information on fruit and vegetable intake and the home nutrition environment |
| Verdonschot et al. 2020 [49] | 1237 students 7–12 years old | Netherlands | - Nutrition knowledge - Fruit and vegetable intake - Personal characteristics - School characteristics - School Food Policy | - 24 questions about nutrition knowledge - 24 h recall suggested by Haraldsdóttir et al. (2005) - Child questionnaire about age, sex, and grade - Questionnaire for teachers about school characteristics |
| Siew et al. 2020 [40] | 152 students 9 years old | Malaysia | - Nutritional issues and concerns - Body weight and height - Socio-demographic data | - Immediate Impact Survey (IIS) - Nutrition Knowledge, Attitude, and Practices survey (KAP) - Nutritional status assessment |
| Fisher et al. 2019 [35] | 57 students 5–6 years old | United States | - Children’s nutrition knowledge | - Oral questions and direct observation |
| Lin et al. 2019 [50] | 201 students 8–12 years old | Taiwan | - Interest and satisfaction with the program - Nutrition Knowledge - Healthy Eating Active Living (HEAL) - Children’s height and weight | - MX’s routine questionnaire - 5-point Likert scale about satisfaction - Six multiple-choice questions for physical activity knowledge - Eight multiple-choice questions on healthy diet knowledge |
| Qian et al. 2019 [41] | 4482 students 8–9 years old | China | - Eating behaviors | - Nine outcome measures based on The Guidelines for Nutrition and Diet for Chinese Residents |
| Kim et al. 2019 [51] | 524 students 4–5 years old | South Korea | - Health - Weight - BMI - Eating behaviors | - Height was measured to the nearest tenth of a centimeter (cm) with a mobile - The weight was measured to the nearest tenth of a kilogram (kg) on a portable digital scale - BMI was calculated with the standard equation (body weight [kg]/height [m]2) - Children’s eating behavior was assessed by nutritional quotient (NQ) |
| Brown et al. 2018 [52] | 404 students 6–11 years old | Scotland | - Health behaviors | - Height and weight test based on Child Measurement Program Operational Guidance - Questionnaire about health attitudes and behaviors |
| Zhou, 2018 [42] | 65 students 10–12 years old | China | - Age - Mother’s and father’s jobs and education - Nutritional knowledge - Nutritional attitude - Nutritional behavior | - Demographic questionnaire - Nutrition Behavior Inventory |
| Lynch et al. 2016 [36] | 51 students 7–9 years old | United States | - Health habits - Number of steps | - Healthy Habits Survey - Pedometer - Demographic Survey |
| Sharma et al. 2015 [37] | 94 students 8–12 years old | United States | - Dietary intake - Nutrition habits - Physical Activity habits - Attitudes toward computer-assisted instruction - Height and weight | - Two random 24 h dietary recalls using the validated Coordinated Approach to Child Health (CATCH) - Child self-report surveys about nutrition and physical activity habits - Attitude Toward Computer-Assisted Learning Scale - Standard protocols to measure child height and weight |
| Song et al. 2015 [38] | 665 students 8–11 years old | United States | - Self-reported FV intake - The perceptions of food service staff about what children eat | - Student preference and consumption survey - Food service staff survey |
| Authors | Description Intervention | Duration of Sessions |
|---|---|---|
| García and Fernández 2022 [43] | Effectiveness of the gamified proposal “Save the Mediterranean Diet”. EG. The contents are presented to the students through audiovisual support. Then, they have to overcome the gamified mission. CG. Nothing was provided. | 5 sessions (1 per week in consecutive weeks). |
| Øvrebø et al. 2022 [44] | Effectiveness of a program based on free fruit and vegetable (FFV) school policies. EG. Provide a daily serving of free fruit or vegetable at lunchtime. CG. Nothing was provided. | One piece of FV per day for 4 years (follow-up during the years 2010, 2012, 2015, and 2017). |
| Karpouzis et al. 2021 [45] | Effectiveness of the Food Education and Sustainability Training (FEAST) program. EG. Inquiry learning and role model concepts are used to incorporate classroom cooking activities into the English and STEM curriculum. CG. Nothing was provided. | 10 sessions in consecutive weeks (1 session per week, 1.5 h per lesson). |
| Franceschi et al. 2021 [46] | Effectiveness of the project “Smuovi La Salute”. EG. Activities that help to reduce cultural and socio-economic inequalities. The use of an app, a cookbook with healthy multicultural recipes, nutritional video lessons, and video laboratories, and physical activities in urban settings. CG. Video viewing. | 30 months (Phase 1, 19 months; phase 2, 11 months). |
| Teo et al. 2021 [39] | Effectiveness of the School Nutrition Program (SNP) through the presentation of 17 topics, which included 4 aspects worked on through nutrition practices: health, nutrition, physical activity, and food hygiene. EG. Participation in school nutrition campaigns and healthy menu serving during school breaks. CG. Nothing was provided. | 6 h monthly campaigns every 3 months and a menu with cereals, vegetables, fruits, and protein foods every day for 3 months. |
| Nickel et al. 2021 [47] | Effectiveness of the Healthy Buddies intervention. EG. 21 healthy living lessons. CG. Standard health curriculum. | 21 lessons in consecutive weeks. |
| Ben Cheikh et al. 2020 [48] | Effectiveness of a nutritional intervention program. EG. Several workshops (tasting, labeling, cooking…). Open day for children and parents with workshops to choose the best healthy and balanced dish. Drawing, writing, and poetry contests on healthy nutrition. SMS to parents focuses on the importance of promoting healthy eating. Facebook group to disseminate educational messages on healthy eating. CG. Nothing was provided. | 5 months. |
| Marshall et al. 2020 [34] | Effectiveness of the Brighter Bites program. EG. Nutrition education lessons and weekly recipe tastings. CG. Nothing was provided. | 16 weeks during a school year. |
| Verdonschot et al. 2020 [49] | Effectiveness of two different nutrition education programs. EG1. FV provision and education. EG2. FV provision. CG. Nothing was provided. | EG1: five lessons (including experiments, cooking, and tasting). EG2: three pieces of fruit per week for 20 weeks. |
| Siew et al. 2020 [40] | Effectiveness of a nutrition educational package. EG. HKP educational package with three educational modules (including health awareness, nutrition, physical activity, and hygiene), and supportive educational materials (such as games, PowerPoint presentations, goal cards…). CG. Nothing was provided. | Six times a year for 3 years (each session lasts one hour). |
| Fisher et al. 2019 [35] | Effectiveness of Sprouts’ curriculum. EG. Activities and book-reading about energy balance, healthy sleep habits, and food groups. CG. Nothing was provided. | 8 lessons. |
| Lin et al. 2019 [50] | Effectiveness of “Train Like an Astronaut Program” EG. 8 challenges about training students with exercises, improving their knowledge, and completing circuit training. CG. Nothing was provided. | 8 sessions in consecutive weeks (40 min per session). |
| Qian et al. 2019 [41] | Effectiveness of a comprehensive nutrition education program. EG. Nutrition lessons and activities integrated into students. CG. Nothing was provided. | For 1 school year with flexibility in the duration and number of sessions to accommodate local conditions. |
| Kim et al. 2019 [51] | Effectiveness of the Mission X program (train like an astronaut). EG. Activities and materials (including food-balanced meals, observation methods, educational movie clips, and healthy/unhealthy snacks) on four thematic nutrition components: energy on an astronaut, hydration station, living bones, and reduced gravity. CG. Key concepts of the nutrition sessions. | 4 sessions for 10 weeks. |
| Brown et al. 2018 [52] | Effectiveness of 10-week lifestyle intervention. EG. 45 min aligned with the Scottish Curriculum and 45 min consisted of fun games, exercises, and sports. CG. Nothing was provided. | 10 sessions in consecutive weeks (90 min per session). |
| Zhou, 2018 [42] | Effectiveness of nutritional behaviors intervention program. EG. Videos, and role play, among other activities about healthy and unhealthy food. CG. Nothing was provided. | 4 sessions on consecutive days (45 min per session). |
| Lynch et al. 2016 [36] | Effectiveness of 5-2-1-0 Educational curriculum. EG. The standardized 5-2-1-0 curriculum was taught. CG. Nothing was provided. | 8 sessions for a 4-month period. |
| Sharma et al. 2015 [37] | Effectiveness of the Quest to Lava Mountain (QTLM). EG. They used an immersive three-dimensional action-adventure game CG. Nothing was provided. | 90 min per week for 6 weeks. |
| Song et al. 2015 [38] | Effectiveness of a multilevel intervention EG1. Comprehensive group. They received the ReFresh program (nutrition education and behavioral economics-based cafeteria changes). EG2. The cafeteria group. They only received behavioral economics-based cafeteria changes. CG. Nothing was provided. | 8 classroom-based nutrition education units (4 lessons per unit) for 1 scholar year. |
| Authors | Results |
|---|---|
| Franceschi et al. 2021 [46] | - There was a significant increase of 35% (from 69.3 to 93.5%) in nutritional knowledge about the correct daily frequency of vegetable and fruit consumption. |
| Nickel et al. 2021 [47] | - EG participants who were boys had improved knowledge of healthy living (5.9; 95% CI [2.3, 9.5]). - EG participants who lived in low-income neighborhoods had improved knowledge of healthy living. |
| Verdonschot et al. 2020 [49] | - There was a significant increase in EG1 children’s nutrition knowledge (p < 0.01) and there was a significant difference with CG (p < 0.05). In EG2 the differences were not significative. |
| Siew et al. 2020 [40] | - In the mean knowledge score there was a significant increment in EG (p < 0.01) and there was a significant difference between groups (p < 0.05) over the 3 years in favor of EG. |
| Fisher et al. 2019 [35] | - In EG, there were significant differences between pre- and post-test in farm-to-table knowledge (p < 0.001), and sugar content of beverages knowledge (p = 0.01). |
| Lin et al. 2019 [50] | - The nutrition knowledge increased in both groups. However, the differences between groups are significant in healthy diet knowledge (p = 0.044) and in active lifestyle knowledge (p = 0.002), in favor of EG. |
| Zhou, 2018 [42] | - In EG there was a significant increase in nutritional knowledge (p = 0.04). |
| Sharma et al. 2015 [37] | - The EG showed a decrease in nutrition/physical activity knowledge with significant differences in comparison to CG (p = 0.0338). |
| Authors | Results |
|---|---|
| Øvrebø et al. 2022 [44] | - Boys exposed to the FFV policy (EG) had a 0.05 higher BMI (95%CI: −0.04, 0.14). - Girls exposed to the FFV policy (EG) had a 0.04 higher BMI (95% CI: −0.04, 0.13). - Boys of parents without higher education had elevated BMI (+0.12, p = 0.004), increased odds ratio (OR) of overweight/obesity (OR 1.66, p = 0.002), and higher overweight (+0.7 cm, p = 0.05). - Girls of parents without higher education had lower BMI (−0.20; 95% CI: −0.41, 0.01) and lower odds of overweight/obesity (OR 0.55; 95% CI: 0.27, 1.12) if they had attended a school with this program (p = 0.05). |
| Franceschi et al. 2021 [46] | - There was an increase in physical activity by 63% after the project (from 54.5 to 88.9%, p < 0.001) in EG. - Overweight children and adolescents reduced their BMI score by −0.17 ± 0.63. |
| Nickel et al. 2021 [47] | - EG participants who were low-income, boys, or living in rural areas experienced a greater reduction in WC (−1.7 cm; 95% CI [−2.8, −0.5 cm]) |
| Teo et al. 2021 [39] | - The EG showed more frequent physical activity compared to the CG (p < 0.05). - At a 3-month follow-up, the EG showed lower BMI scores (p < 0.05). |
| Siew et al. 2020 [40] | -Significant changes in weight and BMI over time occurred in each group (p < 0.05): The prevalence of normal weight increased in the EG at the post-test, but not in the CG. The prevalence of overweight decreased in the EG at the post-test, but not in the CG. The prevalence of thinness at post-test decreased in both groups, but in the EG the decrease was greater. The CG had a higher prevalence of obesity and overweight than the EG at the post-test. |
| Kim et al. 2019 [51] | - There were significant changes in anthropometric variables in the EG (p < 0.05). |
| Lin et al. 2019 [50] | - The prevalence of overweight and obesity decreased in EG at post-test, but not in CG. |
| Sharma et al. 2015 [37] | - Physical activity attitude had significant differences between groups (p = 0.041), and it increased from pre- to postintervention. - There were no significant effects of Quest to Lava Mountain (QTLM) on physical activity. CG and EG improved their results but there were no significant differences between the groups. |
| Authors | Results |
|---|---|
| García and Fernández, 2022 [43] | - Adherence to the Mediterranean diet was slightly higher in the EG (pre-test 6.7 and post-test 7.8) than in the CG (pre-test 8.1. and post-test 8.1). - Adherence to the Mediterranean diet is slightly higher in the group of girls (pre-test 7.8 and post-test 8.4) compared to the group of boys (pretest 6.9 and posttest 7.6). |
| Karpouzis et al. 2021 [45] | - In EG there was an increase in self-confidence in cooking, the pleasure in food and cooking, the intake of fruits and vegetables, and in the frequency of cooking at home. - Food waste was reduced. Children ate more of the contents of their lunch boxes and they were willing to eat imperfect fruits and vegetables post-intervention. |
| Franceschi et al. 2021 [46] | - Daily frequency of vegetable and/or fruit consumption was significantly increased (from 36.6 to 51.7%; p < 0.001). |
| Teo et al. 2021 [39] | - At post-intervention, the EG increased their breakfast, lunch, dinner, and snack consumption frequency. |
| Nickel et al. 2021 [47] | - Urban children in EG improved dietary intake (4.6; 95% CI [0.9, 8.3]), and self-efficacy (5.3; 95% CI [1.0, 9.5]). - Boys who lived in higher-income neighborhoods in EG improved dietary intake. |
| Ben Cheikh et al. 2020 [48] | - Morning snack consumption decreased significantly in the EG (p = 0.009). - The proportion of children who had a morning snack habit decreased significantly between pre- and post-intervention (p = 0.000). - The consumption of cookies, cakes, and chocolates decreased significantly in the EG (p = 0.000). |
| Marshall et al. 2020 [34] | - There was a significant increase in FV intake and fiber intake in the EG. - There was a significant decrease in total fat intake and in the percentage of daily calories from sugar-sweetened beverages (p < 0.05). - Dietary data from parents showed significant increases in the combined fruit and vegetable intake (p < 0.05). - There were changes in the home nutrition environment which included: an increase in the frequency of cooking behaviors, in the use of nutrition facts labels, and in the availability of fruit and vegetable foods (p < 0.05). |
| Verdonschot et al. 2020 [49] | - There were no significant differences in (FV) consumption between EG1 and CG, and EG2 and CG. However, in EG2 there was an increase in FV consumption, and in EG1 and CG there was a decrease. |
| Siew et al. 2020 [40] | - In the attitude score, there were no significant changes for both groups over time. |
| Fisher et al. 2019 [35] | - In EG, there were significant differences between pre- and post-test in the knowledge of bedtime routines (p = 0.002). - Between groups, they only found significant differences in bedtime routines knowledge (p = 0.004). |
| Lin et al. 2019 [50] | -There were no significant differences in children’s healthy eating behaviors or active lifestyle behaviors between groups. - Children increased their interest in NASA space at the post-test, but this interest did not moderate the effect of Healthy Eating Active Living (HEAL) behaviors. |
| Qian et al. 2019 [41] | - The EG improved healthy eating behaviors at the post-test. There were significant differences between the pre- and post-test (p = 0.001). Moreover, the EG showed significantly higher scores than the CG (p = 0.025) in healthy eating behaviors. - In the EG there was a significantly larger portion of students who met the recommended level for several eating behaviors at the post-test. Here, there were differences between provinces. In Shandong, they met the recommended level for each of the nine eating behaviors (p < 0.001), and in Qinghay (lower family incomes), they met the recommended level for three of the nine behaviors (p < 0.05). |
| Kim et al. 2019 [51] | - There were significant changes in anthropometric variables in the EG (p < 0.05). - Total NQ score of the EG significantly increased (from 64.1 to 66.0, p < 0.05) - There was a higher fruit intake in EG than in CG (2.0 vs. 1.5, p < 0.05). - Moderation in the intake of hypercaloric foods was greater in the EG than in CG (0.5 vs. 1.2, p < 0.05). - Changes in meal regularity were significantly greater in EG than in CG (3.4 vs. 1.2, p < 0.05). |
| Brown et al. 2018 [52] | - There was a significant difference between the pre- and post-test in healthy snack attitude. |
| Zhou, 2018 [42] | - In EG there was a significant increase in nutritional attitude (p = 0.02) and nutritional behavior (p = 0.03) at post-test, but not in CG (p > 0.05). |
| Sharma et al. 2015 [37] | - There was a significant decrease in the amount of sugar consumed among children in EG compared to CG (p = 0.021). |
| Song et al. 2015 [38] | - Eating fruit for lunch is the unique factor that increased in the three groups with significant differences (p = 0.002 in CG, p = 0.006 in EG2, p = 0.011 in EG1). - EG1 significantly changed in eating vegetables for lunch (p = 0.007), eating any fruits the day before (p = 0.023), the number of days that they ate vegetables and fruits the previous week (p < 0.001), the self-efficacy to prepare FV at home (p = 0.034) and the perceptions of their peers’ fruit consumption (p = 0.025). Regarding the preference of students; berries and cherries had a significant increase only in CG (p=.006), while pears had a significant increase only in EG2 (p = 0.032). Oatmeal and granola had a significant change in EG2 (p = 0.036) and EG1 (p < 0.001), and grapes had a highly significant increase in the three groups (p < 0.001). Moreover, EG1 had significant differences in whole-grain noodles (p = 0.011), vegetables (p = 0.003), apples (p = 0.008), peaches and nectarines (p = 0.015), and squash, zucchini, and pumpkin (p = 0.032). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Collado-Soler, R.; Alférez-Pastor, M.; Torres, F.L.; Trigueros, R.; Aguilar-Parra, J.M.; Navarro, N. A Systematic Review of Healthy Nutrition Intervention Programs in Kindergarten and Primary Education. Nutrients 2023, 15, 541. https://doi.org/10.3390/nu15030541
Collado-Soler R, Alférez-Pastor M, Torres FL, Trigueros R, Aguilar-Parra JM, Navarro N. A Systematic Review of Healthy Nutrition Intervention Programs in Kindergarten and Primary Education. Nutrients. 2023; 15(3):541. https://doi.org/10.3390/nu15030541
Chicago/Turabian StyleCollado-Soler, Rocio, Marina Alférez-Pastor, Francisco L. Torres, Rubén Trigueros, Jose M. Aguilar-Parra, and Noelia Navarro. 2023. "A Systematic Review of Healthy Nutrition Intervention Programs in Kindergarten and Primary Education" Nutrients 15, no. 3: 541. https://doi.org/10.3390/nu15030541
APA StyleCollado-Soler, R., Alférez-Pastor, M., Torres, F. L., Trigueros, R., Aguilar-Parra, J. M., & Navarro, N. (2023). A Systematic Review of Healthy Nutrition Intervention Programs in Kindergarten and Primary Education. Nutrients, 15(3), 541. https://doi.org/10.3390/nu15030541









