Risk Factors of Low Bone Mineral Density in Newly Diagnosed Pediatric Inflammatory Bowel Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Data Collection
2.2.1. General Characteristics and Anthropometric Measurements
2.2.2. Bone Assessment
2.2.3. Laboratory Assessment
2.3. Statistics
3. Results
3.1. Demographic and Clinical Characteristics
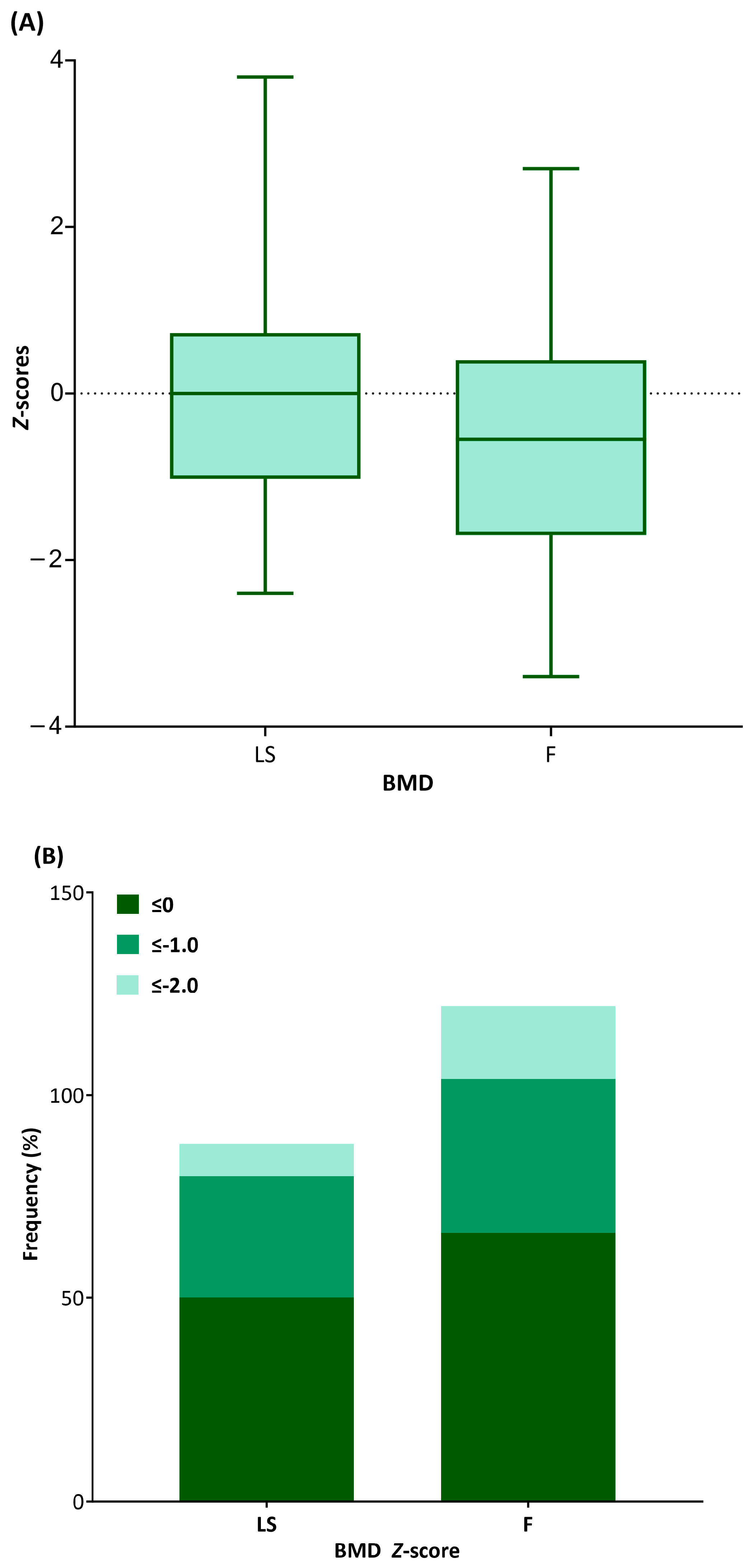
3.2. BMD Status at IBD Diagnosis
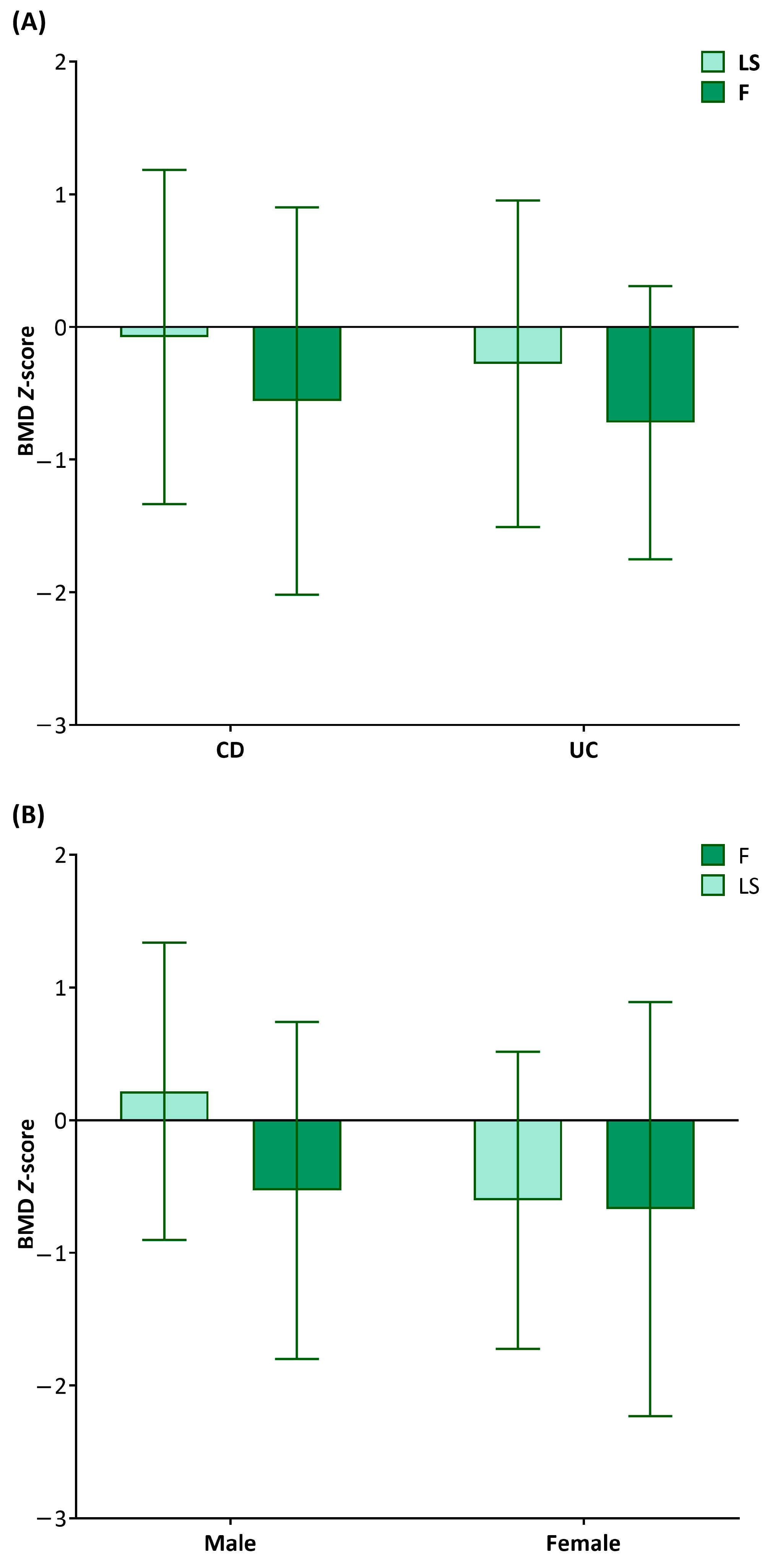
3.3. Clinical Factors Affecting BMD
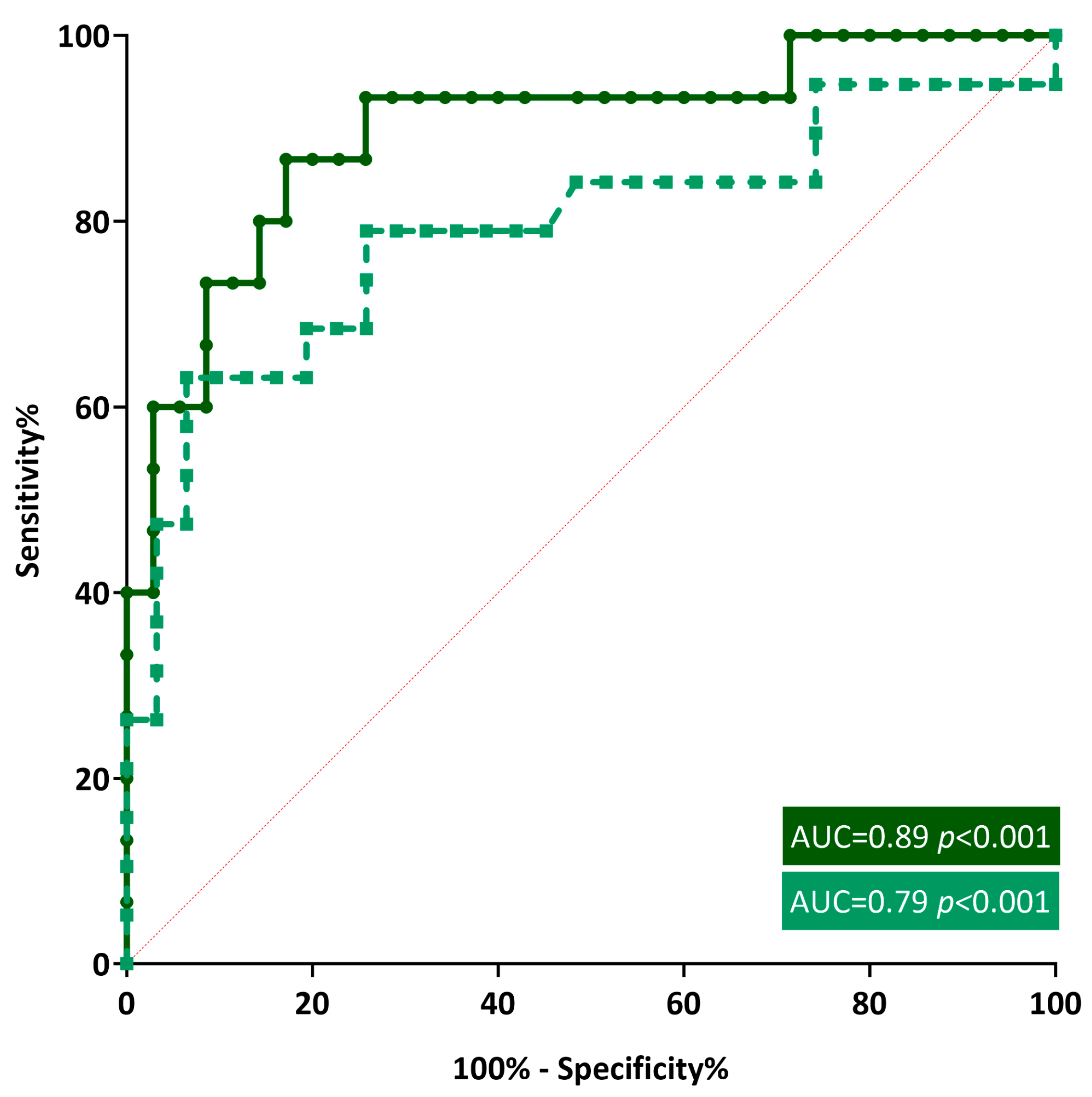
3.4. BMI as a Low BMD Indicator
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ng, S.C.; Tang, W.; Ching, J.Y.; Wong, M.; Chow, C.M.; Hui, A.J.; Wong, T.C.; Leung, V.K.; Tsang, S.W.; Yu, H.H.; et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-pacific Crohn’s and colitis epidemiology study. Gastroenterology 2013, 145, 158–165.e2. [Google Scholar] [CrossRef]
- Abramson, O.; Durant, M.; Mow, W.; Finley, A.; Kodali, P.; Wong, A.; Tavares, V.; McCroskey, E.; Liu, L.; Lewis, J.D.; et al. Incidence, prevalence, and time trends of pediatric inflammatory bowel disease in Northern California, 1996 to 2006. J. Pediatr. 2010, 157, 233–239.e1. [Google Scholar] [CrossRef]
- Choe, J.Y.; Choi, S.; Song, K.H.; Jang, H.J.; Choi, K.H.; Yi, D.Y.; Hong, S.J.; Hwang, J.H.; Cho, S.M.; Kim, Y.J.; et al. Incidence and Prevalence Trends of Pediatric Inflammatory Bowel Disease in the Daegu-Kyungpook Province from 2017 to 2020. Front. Pediatr. 2021, 9, 810173. [Google Scholar] [CrossRef]
- Baldassano, R.N.; Piccoli, D.A. Inflammatory bowel disease in pediatric and adolescent patients. Gastroenterol. Clin. N. Am. 1999, 28, 445–458. [Google Scholar] [CrossRef]
- Rosen, M.J.; Dhawan, A.; Saeed, S.A. Inflammatory Bowel Disease in Children and Adolescents. JAMA Pediatr. 2015, 169, 1053–1060. [Google Scholar] [CrossRef]
- Jang, M.J.; Shin, C.; Kim, S.; Lee, J.W.; Chung, N.G.; Cho, B.; Jung, M.H.; Suh, B.K.; Ahn, M.B. Factors affecting bone mineral density in children and adolescents with secondary osteoporosis. Ann. Pediatr. Endocrinol. Metab. 2023, 28, 34–41. [Google Scholar] [CrossRef]
- Lee, Y.A.; Kwon, A.; Kim, J.H.; Nam, H.K.; Yoo, J.H.; Lim, J.S.; Cho, S.Y.; Cho, W.K.; Shim, K.S. Clinical practice guidelines for optimizing bone health in Korean children and adolescents. Ann. Pediatr. Endocrinol. Metab. 2022, 27, 5–14. [Google Scholar] [CrossRef]
- Heuschkel, R.; Salvestrini, C.; Beattie, R.M.; Hildebrand, H.; Walters, T.; Griffiths, A. Guidelines for the management of growth failure in childhood inflammatory bowel disease. Inflamm. Bowel Dis. 2008, 14, 839–849. [Google Scholar] [CrossRef]
- Gupta, N.; Lustig, R.H.; Andrews, H.; Gokhale, R.; Goyal, A.; Patel, A.S.; Guthery, S.; Sylvester, F.; Siebold, L.; Leu, C.S. Clinical Variables Associated with Statural Growth in Pediatric Crohn’s Disease Differ by Sex (The Growth Study). Inflamm. Bowel Dis. 2021, 27, 751–759. [Google Scholar] [CrossRef]
- Wong, S.C.; Macrae, V.E.; McGrogan, P.; Ahmed, S.F. The role of pro-inflammatory cytokines in inflammatory bowel disease growth retardation. J. Pediatr. Gastroenterol. Nutr. 2006, 43, 144–155. [Google Scholar] [CrossRef]
- Pappa, H.; Thayu, M.; Sylvester, F.; Leonard, M.; Zemel, B.; Gordon, C. Skeletal health of children and adolescents with inflammatory bowel disease. J. Pediatr. Gastroenterol. Nutr. 2011, 53, 11–25. [Google Scholar] [CrossRef]
- Rufo, P.A.; Denson, L.A.; Sylvester, F.A.; Szigethy, E.; Sathya, P.; Lu, Y.; Wahbeh, G.T.; Sena, L.M.; Faubion, W.A. Health supervision in the management of children and adolescents with IBD: NASPGHAN recommendations. J. Pediatr. Gastroenterol. Nutr. 2012, 55, 93–108. [Google Scholar] [CrossRef]
- DeFilippis, E.M.; Sockolow, R.; Barfield, E. Health Care Maintenance for the Pediatric Patient with Inflammatory Bowel Disease. Pediatrics 2016, 138, e20151971. [Google Scholar] [CrossRef]
- Harpavat, M.; Greenspan, S.L.; O’Brien, C.; Chang, C.C.; Bowen, A.; Keljo, D.J. Altered bone mass in children at diagnosis of Crohn disease: A pilot study. J. Pediatr. Gastroenterol. Nutr. 2005, 40, 295–300. [Google Scholar] [CrossRef]
- Theintz, G.; Buchs, B.; Rizzoli, R.; Slosman, D.; Clavien, H.; Sizonenko, P.C.; Bonjour, J.P. Longitudinal monitoring of bone mass accumulation in healthy adolescents: Evidence for a marked reduction after 16 years of age at the levels of lumbar spine and femoral neck in female subjects. J. Clin. Endocrinol. Metab. 1992, 75, 1060–1065. [Google Scholar]
- Heyman, M.B.; Kirschner, B.S.; Gold, B.D.; Ferry, G.; Baldassano, R.; Cohen, S.A.; Winter, H.S.; Fain, P.; King, C.; Smith, T.; et al. Children with early-onset inflammatory bowel disease (IBD): Analysis of a pediatric IBD consortium registry. J. Pediatr. 2005, 146, 35–40. [Google Scholar] [CrossRef]
- Bischoff, S.C.; Herrmann, A.; Goke, M.; Manns, M.P.; von zur Muhlen, A.; Brabant, G. Altered bone metabolism in inflammatory bowel disease. Am. J. Gastroenterol. 1997, 92, 1157–1163. [Google Scholar]
- Gokhale, R.; Favus, M.J.; Karrison, T.; Sutton, M.M.; Rich, B.; Kirschner, B.S. Bone mineral density assessment in children with inflammatory bowel disease. Gastroenterology 1998, 114, 902–911. [Google Scholar] [CrossRef]
- Sylvester, F.A.; Wyzga, N.; Hyams, J.S.; Davis, P.M.; Lerer, T.; Vance, K.; Hawker, G.; Griffiths, A.M. Natural history of bone metabolism and bone mineral density in children with inflammatory bowel disease. Inflamm. Bowel Dis. 2007, 13, 42–50. [Google Scholar] [CrossRef]
- Dubner, S.E.; Shults, J.; Baldassano, R.N.; Zemel, B.S.; Thayu, M.; Burnham, J.M.; Herskovitz, R.M.; Howard, K.M.; Leonard, M.B. Longitudinal assessment of bone density and structure in an incident cohort of children with Crohn’s disease. Gastroenterology 2009, 136, 123–130. [Google Scholar] [CrossRef]
- Vestergaard, P.; Mosekilde, L. Fracture risk in patients with celiac Disease, Crohn’s disease, and ulcerative colitis: A nationwide follow-up study of 16,416 patients in Denmark. Am. J. Epidemiol. 2002, 156, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Masip, E.; Donat, E.; Polo Miquel, B.; Ribes-Koninckx, C. Bone mineral density in spanish children at the diagnosis of inflammatory bowel disease. Arch. Osteoporos. 2021, 16, 96. [Google Scholar] [CrossRef] [PubMed]
- Yin, Y.; Lu, X.; Li, Z.; Liu, S.; Shao, L.; Cao, L.; Liu, R.Q.; Huang, L.Y.; Zhu, Z.X.; Guo, Z.; et al. Risk Factors for Worsening of Bone Loss in Patients Newly Diagnosed with Inflammatory Bowel Disease. Gastroenterol. Res. Pract. 2022, 2022, 1498293. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Lee, H.S.; Jang, B.I.; Kim, E.S.; Kim, S.K.; Kim, K.O.; Lee, Y.J.; Lee, H.J.; Kim, E.Y.; Jung, Y.J.; et al. Low Bone Mineral Density in Young Patients Newly Diagnosed with Inflammatory Bowel Disease. Dig. Dis. Sci. 2021, 66, 605–611. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.Y.; Lim, J.S.; Lee, Y.; Choi, Y.; Oh, S.H.; Kim, K.M.; Yoo, H.W.; Choi, J.H. Growth, puberty, and bone health in children and adolescents with inflammatory bowel disease. BMC Pediatr. 2021, 21, 35. [Google Scholar] [CrossRef] [PubMed]
- Levine, A.; Koletzko, S.; Turner, D.; Escher, J.C.; Cucchiara, S.; de Ridder, L.; Kolho, K.L.; Veres, G.; Russell, R.K.; Paerregaard, A.; et al. ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 795–806. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Yun, S.; Hwang, S.S.; Shim, J.O.; Chae, H.W.; Lee, Y.J.; Lee, J.H.; Kim, S.C.; Lim, D.; Yang, S.W.; et al. The 2017 Korean National Growth Charts for children and adolescents: Development, improvement, and prospects. Korean J. Pediatr. 2018, 61, 135–149. [Google Scholar] [CrossRef]
- Yi, K.H.; Hwang, J.S.; Kim, E.Y.; Lee, J.A.; Kim, D.H.; Lim, J.S. Reference values for bone mineral density according to age with body size adjustment in Korean children and adolescents. J. Bone Miner. Metab. 2014, 32, 281–289. [Google Scholar] [CrossRef]
- Friedrich, M.; Pohin, M.; Powrie, F. Cytokine Networks in the Pathophysiology of Inflammatory Bowel Disease. Immunity 2019, 50, 992–1006. [Google Scholar] [CrossRef] [PubMed]
- Ali, T.; Lam, D.; Bronze, M.S.; Humphrey, M.B. Osteoporosis in inflammatory bowel disease. Am. J. Med. 2009, 122, 599–604. [Google Scholar] [CrossRef]
- Chedid, V.G.; Kane, S.V. Bone Health in Patients with Inflammatory Bowel Diseases. J. Clin. Densitom. 2020, 23, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.H.; Choi, Y.; Lee, Y.; Yoo, H.W.; Choi, J.H. Efficacy and safety of intravenous pamidronate infusion for treating osteoporosis in children and adolescents. Ann. Pediatr. Endocrinol. Metab. 2021, 26, 105–111. [Google Scholar] [CrossRef]
- Jahnsen, J.; Falch, J.A.; Mowinckel, P.; Aadland, E. Body composition in patients with inflammatory bowel disease: A population-based study. Am. J. Gastroenterol. 2003, 98, 1556–1562. [Google Scholar] [CrossRef]
- Feakins, R.; Torres, J.; Borralho-Nunes, P.; Burisch, J.; Cúrdia Gonçalves, T.; De Ridder, L.; Driessen, A.; Lobatón, T.; Menchén, L.; Mookhoek, A.; et al. ECCO Topical Review on Clinicopathological Spectrum and Differential Diagnosis of Inflammatory Bowel Disease. J. Crohns Colitis 2022, 16, 343–368. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, J.; Xiao, J. Selenoproteins and selenium status in bone physiology and pathology. Biochim. Biophys. Acta 2014, 1840, 3246–3256. [Google Scholar] [CrossRef]
- Poursadegh, F.; Ahadi, M.; Vosoughinia, H.; Salehi, M.; Beheshti Namdar, A.; Farzanehfar, M.R.; Memar, B.; Ziaolhagh, R. A STROBE compliant observational study on trace elements in patients with ulcerative colitis and their relationship with disease activity. Medicine 2018, 97, e13523. [Google Scholar] [CrossRef]
- Yang, T.; Lee, S.Y.; Park, K.C.; Park, S.H.; Chung, J.; Lee, S. The Effects of Selenium on Bone Health: From Element to Therapeutics. Molecules 2022, 27, 392. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.M.; Yoon, H.; Lim, S.; Sung, M.K.; Shin, C.M.; Park, Y.S.; Kim, N.; Lee, D.H.; Kim, J.S. Risk Factors for Vitamin D, Zinc, and Selenium Deficiencies in Korean Patients with Inflammatory Bowel Disease. Gut Liver 2017, 11, 363–369. [Google Scholar] [CrossRef]
- Ratajczak, A.E.; Rychter, A.M.; Zawada, A.; Dobrowolska, A.; Krela-Kaźmierczak, I. Do Only Calcium and Vitamin D Matter? Micronutrients in the Diet of Inflammatory Bowel Diseases Patients and the Risk of Osteoporosis. Nutrients 2021, 13, 525. [Google Scholar] [CrossRef] [PubMed]
- Guz-Mark, A.; Rinawi, F.; Egotubov, O.; Shimon, I.; Shamir, R.; Assa, A. Pediatric-onset inflammatory bowel disease poses risk for low bone mineral density at early adulthood. Dig. Liver Dis. 2017, 49, 639–642. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.J.; Ryu, K.H.; Park, B.J.; Yoon, B.H. Osteoporosis and Osteoporotic Fractures in Gastrointestinal Disease. J. Bone Metab. 2018, 25, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, S.; Mellström, D.; Norjavaara, E.; Sundh, S.V.; Saalman, R. Low bone mineral density in children and adolescents with inflammatory bowel disease: A population-based study from Western Sweden. Inflamm. Bowel Dis. 2009, 15, 1844–1850. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 51) | |||
|---|---|---|---|
| CD (n = 42) | UC (n = 9) | p | |
| Male, n (%) | 26 (61.9) | 4 (44.4) | 0.346 |
| Age, y | 13.77 ± 2.35 | 14.45 ± 2.46 | 0.437 |
| Family history of IBD, n (%) | 6 (14.3) | 1 (11.1) | 0.82 |
| Anthropometry, Z-score | |||
| Height | 0.32 ± 0.49 | 0.05 ± 1.25 | 0.557 |
| Weight | −0.229 ± 1.42 | −1.03 ± 1.62 | 0.266 |
| Body mass index | −0.54 ± 1.41 | −1.28 ± 1.54 | 0.169 |
| Clinical manifestation | |||
| Gastrointestinal-associated, n (%) | |||
| Abdominal pain | 33 (78.6) | 8 (88.9) | 0.495 |
| Diarrhea | 27 (64.3) | 8 (88.9) | 0.157 |
| Bloody stool | 7 (16.7) | 8 (88.9) | <0.001 |
| Weight loss | 0.697 | ||
| None | 10 (23.8) | 3 (33.3) | |
| ≤10% | 16 (38.1) | 6 (66.7) | |
| >10% | 15 (35.7) | 6 (66.7) | |
| * Extra-GI-associated, n (%) | 2 (3.9) | 0 (0) | 0.532 |
| Duration, y | 0.58 ± 0.58 | 0.58 ± 0.57 | 0.708 |
| Involvement, n (%) | <0.001 | ||
| Colon | 2 (4.8) | 9 (100) | |
| Colon and ileum | 13 (30.9) | 0 (0) | |
| Colon, ileum, and duodenum or jejunum | 27 (64.3) | 0 (0) | |
| † Luminal behavior, n (%) | † L | ||
| None | 39 (92.9) | ||
| Stricturing | 3 (7.1) | ||
| Penetrating | 0 (0) | ||
| † Perianal disease, n (%) | † p | ||
| Yes | 16 (38.1) | ||
| No | 26 (61.9) | ||
| ‡ Severity of scoring | ‡ | ‡ | 0.792 |
| Mild | 13 (30.9) | 1 (11.1) | |
| Moderate | 15 (35.7) | 6 (66.7) | |
| Severe | 14 (33.3) | 2 (22.2) | |
| BMD Z-Scores | ||||
|---|---|---|---|---|
| LS | RF | |||
| r | p | r | p | |
| Age | 0.046 | 0.752 | 0.109 | 0.451 |
| Height | 0.463 | <0.001 | 0.350 | 0.013 |
| Weight | 0.704 | <0.001 | 0.649 | <0.001 |
| BMI | 0.652 | <0.001 | 0.646 | <0.001 |
| Duration of CM | −0.483 | <0.001 | −0.367 | 0.009 |
| WBC | −0.049 | 0.736 | −0.055 | 0.704 |
| Hb | 0.242 | 0.091 | 0.239 | 0.095 |
| Plt | −0.039 | 0.79 | −0.166 | 0.248 |
| Glucose | 0.178 | 0.215 | 0.283 | 0.047 |
| Albumin | 0.229 | 0.11 | 0.328 | 0.02 |
| TB | 0.199 | 0.165 | 0.111 | 0.443 |
| AST | 0.238 | 0.096 | 0.274 | 0.054 |
| ALT | 0.315 | 0.026 | 0.34 | 0.016 |
| Calcium | 0.166 | 0.249 | 0.214 | 0.136 |
| Phosphorus | 0.162 | 0.261 | −0.008 | 0.956 |
| BS-ALP | −0.068 | 0.764 | −0.174 | 0.438 |
| ESR | −0.173 | 0.229 | −0.244 | 0.088 |
| CRP | −0.07 | 0.628 | −0.105 | 0.47 |
| Calcidiol | 0.046 | 0.753 | −0.008 | 0.956 |
| Parathyroid hormone | −0.256 | 0.165 | −0.015 | 0.937 |
| Cyanocobalamin | −0.048 | 0.745 | 0.091 | 0.536 |
| Ferritin | 0.038 | 0.791 | −0.022 | 0.878 |
| Prealbumin | 0.099 | 0.5 | 0.15 | 0.305 |
| Zinc | 0.143 | 0.327 | 0.26 | 0.156 |
| Selenium | 0.477 | <0.001 | 0.375 | 0.009 |
| Presepsin | −0.047 | 0.762 | 0.107 | 0.488 |
| Procalcitonin | −0.098 | 0.503 | −0.103 | 0.48 |
| Calprotectin | −0.038 | 0.791 | −0.151 | 0.295 |
| BMD Z-Scores | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LS | RF | |||||||||||
| ≤0 | ≤−1.0 | ≤−2.0 | ≤0 | ≤−1.0 | ≤−2.0 | |||||||
| χ2 | p | χ2 | p | χ2 | p | χ2 | p | χ2 | p | χ2 | p | |
| Family history of IBD | 0.76 | 0.384 | 0.04 | 0.849 | 0.59 | 0.441 | 0.91 | 0.339 | 0.06 | 0.802 | 0.01 | 0.928 |
| Abdominal pain | 2 | 0.157 | 0.59 | 0.44 | 2.45 | 0.118 | 1.43 | 0.232 | 4.16 | 0.041 | 0.54 | 0.462 |
| Diarrhea | 0.37 | 0.544 | 1.42 | 0.234 | 0.09 | 0.754 | 0.13 | 0.72 | 1.69 | 0.194 | 0.48 | 0.487 |
| Bloody stool | 0.09 | 0.758 | 0.11 | 0.736 | 0.83 | 0.363 | 1.53 | 0.216 | 1.17 | 0.28 | 4.7 | 0.03 |
| Weight loss | 9.1 | 0.011 | 8.98 | 0.011 | 1.57 | 0.455 | 22.9 | <0.001 | 11.3 | 0.003 | 4.17 | 0.125 |
| Extragastrointestinal manifestation | 2.08 | 0.149 | 4.86 | 0.027 | 4.99 | 0.025 | 1.07 | 0.3 | 3.4 | 0.065 | 9.49 | 0.002 |
| Involvement | 0.13 | 0.938 | 0.49 | 0.783 | 1.92 | 0.383 | 0.57 | 0.751 | 0.21 | 0.901 | 2.78 | 0.249 |
| † Luminal behavior | 0.41 | 0.52 | 2.19 | 0.139 | 3.23 | 0.072 | 1.68 | 0.195 | 5.06 | 0.025 | 0.39 | 0.53 |
| † Perianal disease | 0.27 | 0.606 | 1.4 | 0.236 | 1.04 | 0.308 | 0.13 | 0.717 | 2.17 | 0.141 | 0.82 | 0.365 |
| ‡ Scoring | 3.62 | 0.164 | 4.86 | 0.088 | 2.62 | 0.27 | 4.64 | 0.098 | 7.86 | 0.02 | 1.7 | 0.427 |
| ASCA | 0.29 | 0.588 | 3.47 | 0.063 | 0.03 | 0.869 | 1.12 | 0.289 | 1.04 | 0.308 | 3.93 | 0.047 |
| ANCA | 1.63 | 0.201 | 1.17 | 0.28 | 0.69 | 0.404 | 0.25 | 0.617 | 2.23 | 0.136 | 5.09 | 0.024 |
| Univariate | Multivariate | |||||||
|---|---|---|---|---|---|---|---|---|
| Z-Scores | ||||||||
| LSBMD | FBMD | LSBMD | FBMD | |||||
| β (95% CI) | p | β (95% CI) | p | β (95% CI) | p | β (95% CI) | p | |
| Height | 0.45 (0.2–0.7) | <0.001 | 0.38 (0.08–0.67) | 0.013 | ||||
| Weight | 0.59 (0.42–0.76) | <0.001 | 0.61 (0.39–0.81) | <0.001 | ||||
| BMI | 0.56 (0.37–0.75) | <0.001 | 0.62 (0.4–0.83) | <0.001 | 0.39 (0.19–0.58) | <0.001 | 0.45 (0.19–0.69) | <0.001 |
| Duration of CM | −1.05 (−1.61–−0.5) | <0.001 | −0.89 (−1.54–−0.24) | 0.009 | −0.56 (−1.09–−0.08) | 0.024 | −0.09 (−0.7–0.52) | 0.763 |
| Glucose | 0.01 (0–0.03) | 0.215 | 0.02 (0–0.04) | 0.047 | 0.02 (0–0.04) | 0.014 | ||
| Albumin | 0.43 (−0.1–0.98) | 0.11 | 0.69 (0.12–1.28) | 0.02 | 0.26 (−0.31–0.82) | 0.361 | ||
| ALT | 0.03 (0–0.06) | 0.026 | 0.04 (0–0.06) | 0.016 | 0.01 (−0.01–0.03) | 0.411 | 0.01 (−0.02–0.04) | 0.414 |
| Selenium | 0.01 (0–0.03) | <0.001 | 0.01 (0–0.03) | 0.009 | 0.01 (0–0.02) | 0.003 | 0.01 (0–0.02) | 0.051 |
| BMD Z-Score ≤ −1.0 | ||||||
|---|---|---|---|---|---|---|
| LS | F | |||||
| OR (95% CI) | SE | p | OR (95% CI) | SE | p | |
| BMI | ||||||
| Unadjusted | ||||||
| † <−1 SD | 11.79 (1.39–99.69) | 1.09 | 0.024 | 4.39 (1.06–18.19) | 0.73 | 0.041 |
| ‡ <−2 SD | 21.33 (4.32–105.43) | 0.82 | <0.001 | 19.94 (3.65–108.89) | 0.87 | <0.001 |
| * Adjusted | ||||||
| <−1 SD | 7.93 (0.57–110.68) | 1.34 | 0.124 | 1.33 (0.19–9) | 0.98 | 0.769 |
| <−2 SD | 31.97 (3.34–306.46) | 1.15 | 0.003 | 41.45 (2.37–725.9) | 1.46 | 0.011 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahn, M.B.; Yoo, I.H. Risk Factors of Low Bone Mineral Density in Newly Diagnosed Pediatric Inflammatory Bowel Disease. Nutrients 2023, 15, 5048. https://doi.org/10.3390/nu15245048
Ahn MB, Yoo IH. Risk Factors of Low Bone Mineral Density in Newly Diagnosed Pediatric Inflammatory Bowel Disease. Nutrients. 2023; 15(24):5048. https://doi.org/10.3390/nu15245048
Chicago/Turabian StyleAhn, Moon Bae, and In Hyuk Yoo. 2023. "Risk Factors of Low Bone Mineral Density in Newly Diagnosed Pediatric Inflammatory Bowel Disease" Nutrients 15, no. 24: 5048. https://doi.org/10.3390/nu15245048
APA StyleAhn, M. B., & Yoo, I. H. (2023). Risk Factors of Low Bone Mineral Density in Newly Diagnosed Pediatric Inflammatory Bowel Disease. Nutrients, 15(24), 5048. https://doi.org/10.3390/nu15245048






