Prevalence of Eating Disorders and Disordered Eating Behaviours amongst Adolescents and Young Adults in Saudi Arabia: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Retrieval Strategies
2.2. Inclusion and Exclusion Criteria
2.3. Screening and Data Extraction
2.4. Quality Assessment Tool
2.5. Data Synthesis
3. Results
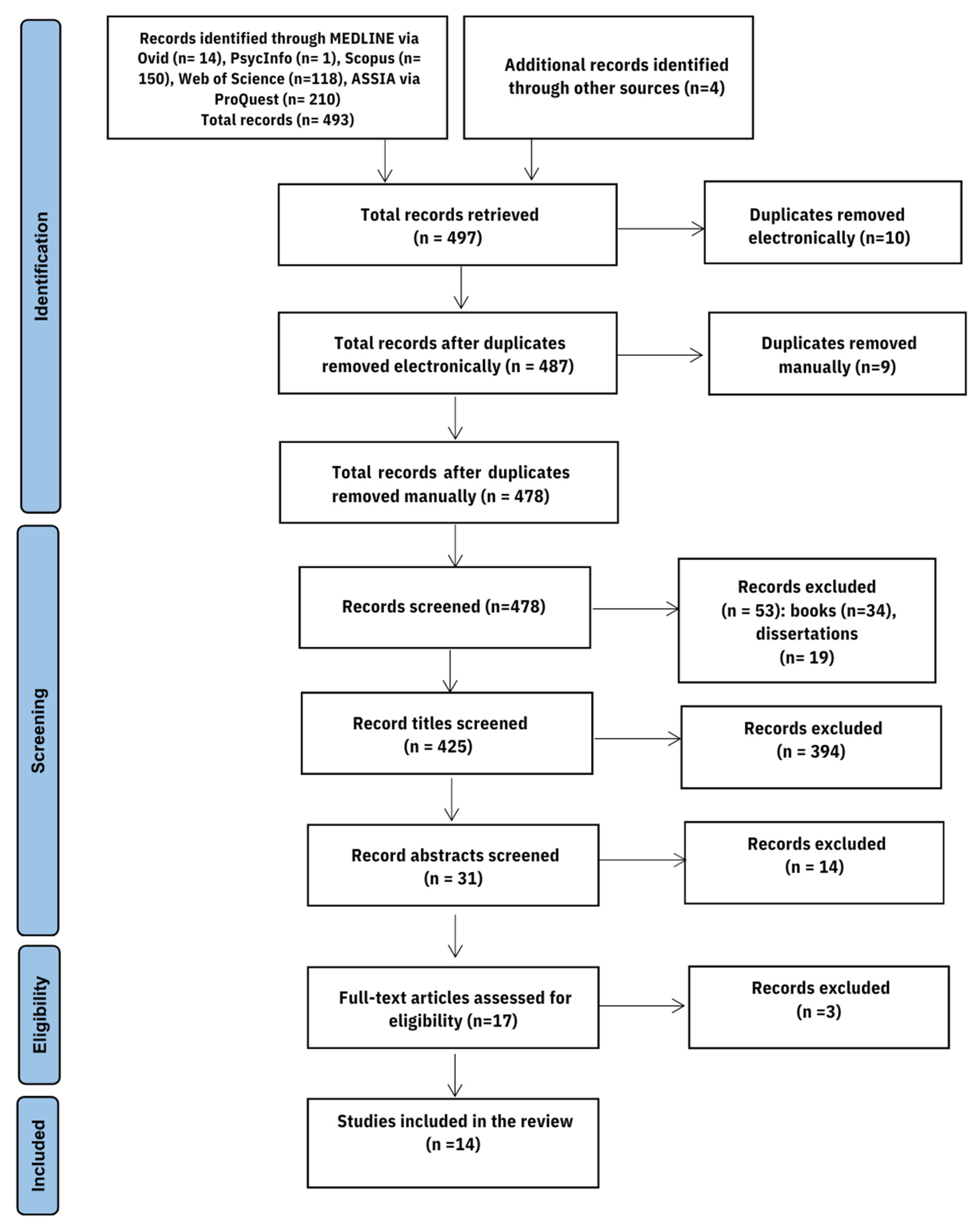
3.1. Study Selection
3.2. Quality Appraisal
3.3. Study Characteristics
3.4. Questionnaires
3.4.1. Prevalence of Disorders Assessed by the EAT-26
3.4.2. Prevalence of Disorders Assessed by the EDI-DT
| Author (Year) | City/ Area | Study Design | Setting | Sample Size | Sex Distribution (F/M) | Age Group (Mean Age ± SD) | Screening Tool | Disorder Screened | Prevalence (N and/or %) | Quality Assessment Score |
|---|---|---|---|---|---|---|---|---|---|---|
| Albrahim et al. (2019) [74] | Riyadh/central | Cross- sectional | Undergraduate students from Prince Nora University | 396 | 396/0 | 18–24 (20.1 ± 1.55) | EAT-26 | DEAs | EAT-26: ≥20 (n = 145, 36.8%), impulse to vomit after meals (2.08 ± 1.14), dieting (0.26 ± 0.66), binging (0.52 ± 0.92) | High |
| AlHazmi and AlJohani (2019) [65] | Madina/west | Cross-sectional | Health specialties students at Taiba University | 342 | 171/171 | NR (NR) ≤22 (n = 221, 64.4%) | EAT-26 | EDs | EAT-26: ≥20 (n = 75, 33.9%), F (n = 65, 38%), M (n = 33, 19.3%) | High |
| Allihaibi (2015) [66] | Makkah/west | Cross-sectional | Secondary schools | 180 | 180/0 | 15–19 (16.83 ± 0.94) | EAT-26 | DEAs | EAT-26: ≥20 (n = 47, 26.1%) | Medium |
| Almuhlafi et al. (2018) [64] | Tabuk/northwest | Cross-sectional | High schools | 399 | 399/0 | NR (16.8 ± 0.9) | EAT-26 | DEBs: Binge eating, purging, laxatives | EAT-26: ≥20 (n = 192, 48.1%) DEB: Binge eating (n = 123, 30.8%), purging (n = 28, 7%), laxative use (n = 21, 5.3%) | High |
| Al-Qahtani and Al-Harbi (2020) [69] | Madina/west | Cross-sectional | Secondary schools | 393 | 393/0 | 15–20 (17.24 ± 1.03) | EAT-26 | DEBs | EAT-26: ≥20 (n = 167, 42.5%), self-reported frequency of EA in the last 6 months (binge eating: (≤3 = 43.4%, >3 = 56.6%) SIV: (≤3 = 44.1%, >3 = 55.9%), laxatives or diuretics: (≤3 = 45.8%, >3 = 54.2%) | High |
| Alsubaie et al. (2017) [67] | Abha/southwest | Cross-sectional | Intermediate and secondary schools | 224 | 224/0 | 12–19 (15.9 ± 3.7) | EAT-26 | EDs | EAT-26: ≥20 (n = 85, 34%), older age females (17–19) had a significantly higher score of EAT-26 (n = 35, 43.8%) than the younger age (12–16) group (n = 50, 29.4%) | High |
| Al-Subaie (2000) [68] | Riyadh/central | Cross-sectional | Grades 7 to 11 from Intermediate and Secondary schools | 1179 | 1179/0 | 12–21 (16.13 ± 2.09) | EDI-DT | DEB: Dieting | EDI-DT > 14 (n = 188, 15.9%) | High |
| Alwosaifer et al. (2018) [73] | Dammam/East | Cross-sectional | Imam Abdulrahman bin Faisal university | 656 | 656/0 | 18–23 (18.7 ± 0.74) | EAT-26 | EDs | EAT-26: ≥20 (n = 179, 29.4%), problematic eating behaviours (n = 277, 45.5%) | High |
| ElShikieri (2022) [75] | Madina/west | Cross-sectional | Public and private female elementary, intermediate, and high schools | 381 | 381/0 | 10–18 (M = 13.6, SD = 2.6) | EAT-26 | DEAs | EAT-26: ≥20 (n = 39, 10.2%) | High |
| Fallatah et al. (2015) [76] | Jeddah/west | Cross-sectional | Secondary schools | 425 | 425/0 | 15–18 (16.6 ± 0.98) | EAT-26 | EDs | EAT-26: ≥20 (n = 140, 32.9%) | High |
| Fatima and Ahmed (2018) [71] | Arar/north | Cross-sectional | Schools | 314 | 314/0 | 15–19 (17.0 ± 1.14) | EAT-26 | DEAs | EAT-26: ≥20 (n = 80, 25.4%) | High |
| Ghafouri et al. (2021) [70] | Makkah/west | Cross-sectional | Private and public secondary schools | 471 | 399/72 | NR (17.28 ± 1.27) | SCOFF | EDs | SCOFF ≥ 2 (n = 136, 46%), SCOFF 0 or 1 (n = 216, 29%) | High |
| Loni et al. (2022) [77] | Majmaah/central | Cross-sectional | Majmaah University | 125 | 90/35 | 18–25 (F (22.9 ± 4.9)), M (25.6 ± 5.1) | EAT-26 | EDs | EAT-26: ≥20 (n = 44, 35.2%), M (n = 14, 40%), F (n = 30, 33.3%), binge eating (M = 42.9%, F = 57.8%), exercised more than 60 min (M = 60%, F = 54.4%), SIV (M = 5.7%, F = 13.3%) | High |
| Tomar and Antony (2022) [72] | Dhahran/East | Cross-sectional | King Fahad University for petroleum and minerals | 60 (obese participants (BMI) ≥ 30 kg/m2) | 0/60 | 18–25 (19.67 ± 0.90) | EDE-Q | EDs | High EDE-Q global score (n = 36, 65.5%) | High |
3.4.3. Prevalence of Disorders Assessed by the EDE-Q
3.4.4. Prevalence of Disorders Assessed by SCOFF
3.4.5. Region
3.4.6. Sex
3.4.7. Age
4. Discussion
4.1. Region
4.2. Sex
4.3. Age
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rikani, A.A.; Choudhry, Z.; Maqsood Choudhry, A.; Ikram, H.; Waheed Asghar, M.; Kajal, D.; Waheed, A.; Jahan Mobassarah, N. A Critique of the Literature on Etiology of Eating Disorders. Ann. Neurosci. 2013, 20, 157–161. [Google Scholar] [CrossRef]
- Herpertz-Dahlmann, B. Adolescent Eating Disorders: Update on Definitions, Symptomatology, Epidemiology, and Comorbidity. Child Adolesc. Psychiatr. Clin. N. Am. 2015, 24, 177–196. [Google Scholar] [CrossRef] [PubMed]
- Perris, F. ICD-11 Sessions at the 19th World Congress of Psychiatry. World Psychiatry 2020, 19, 263–264. [Google Scholar] [CrossRef] [PubMed]
- Smolak, L.; Levine, M.P. Body Image, Disordered Eating, and Eating Disorders. In The Wiley Handbook of Eating Disorders; John Wiley & Sons, Ltd.: West Sussex, NJ, USA, 2015; Volume 1, pp. 1–10. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-5, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar] [CrossRef]
- Giallonardo, V. ICD-11 Sessions within the 18th World Congress of Psychiatry. World Psychiatry 2019, 18, 115–116. [Google Scholar] [CrossRef] [PubMed]
- Wilfley, D.E.; Bishop, M.E.; Wilson, G.T.; Agras, W.S. Classification of Eating Disorders: Toward DSM-V. Int. J. Eat. Disord. 2007, 40, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Van Eeden, A.E.; Van Hoeken, D.; Hoek, H.W. Incidence, Prevalence and Mortality of Anorexia Nervosa and Bulimia Nervosa. Curr. Opin. Psychiatry 2021, 34, 515–524. [Google Scholar] [CrossRef]
- Weaver, L.; Liebman, R. Assessment of Anorexia Nervosa in Children and Adolescents. Curr. Psychiatry Rep. 2011, 13, 93–98. [Google Scholar] [CrossRef]
- Moskowitz, L.; Weiselberg, E. Anorexia Nervosa/Atypical Anorexia Nervosa. Curr. Probl. Pediatr. Adolesc. Health Care 2017, 47, 70–84. [Google Scholar] [CrossRef]
- Abebe, D.S.; Lien, L.; Torgersen, L.; Von Soest, T. Binge Eating, Purging and Non-Purging Compensatory Behaviours Decrease from Adolescence to Adulthood: A Population-Based, Longitudinal Study. BMC Public Health 2012, 12, 32. [Google Scholar] [CrossRef]
- Hoste, R.R.; Labuschagne, Z.; Le Grange, D. Adolescent Bulimia Nervosa. Curr. Psychiatry Rep. 2012, 14, 391–397. [Google Scholar] [CrossRef]
- Pereira, R.F.; Alvarenga, M. Disordered Eating: Identifying, Treating, Preventing, and Differentiating It from Eating Disorders. Diabetes Spectr. 2007, 20, 141–148. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; Text Revision (DSM-IV-TR); American Psychiatric Association Publishing: Washington, DC, USA, 2000. [Google Scholar] [CrossRef]
- Mancuso, S.G.; Newton, J.R.; Bosanac, P.; Rossell, S.L.; Nesci, J.B.; Castle, D.J. Classification of Eating Disorders: Comparison of Relative Prevalence Rates Using DSM-IV and DSM-5 Criteria. Br. J. Psychiatry 2015, 206, 519–520. [Google Scholar] [CrossRef]
- Le Grange, D.; Swanson, S.A.; Crow, S.J.; Merikangas, K.R. Eating Disorder Not Otherwise Specified Presentation in the US Population. Int. J. Eat. Disord. 2012, 45, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Sigel, E. Eating Disorders. In AM:STARs: Metabolic Challenges to Adolescent Health; American Academy of Pediatrics: Itasca, IL, USA, 2009; Volume 19, pp. 547–572. [Google Scholar] [CrossRef]
- dos Santos Alvarenga, M.; Scagliusi, F.B.; Philippi, S.T. Effects of multiprofessional treatment on clinical symptoms, food intake, eating patterns, eating attitudes and body image of Brazilian bulimic patients. In Anorexia Nervosa and Bulimia: New Research; Nova Science Publishers: New York, NY, USA, 2006. [Google Scholar]
- Position of the American Dietetic Association. Nutrition Intervention in the Treatment of Anorexia Nervosa, Bulimia Nervosa, and Other Eating Disorders. J. Am. Diet. Assoc. 2006, 106, 2073–2082. [Google Scholar] [CrossRef] [PubMed]
- Neumark-Sztainer, D.; Story, M.; Hannan, P.J.; Perry, C.L.; Irving, L.M. Weight-Related Concerns and Behaviors Among Overweight and Nonoverweight Adolescents. Arch. Pediatr. Adolesc. Med. 2002, 156, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Bryla, K.Y. Disordered Eating among Female Adolescents: Prevalence, Risk Factors, and Consequences. Health Educ. 2003, 35, 25–29. [Google Scholar]
- Yager, J.; Devlin, M.J.; Halmi, K.A.; Herzog, D.B.; Mitchell, J.E.; Powers, P.S.; Zerbe, K.J. Guideline Watch: Practice Guideline for the Treatment of Patients with Eating Disorders, 2nd Edition. FOCUS 2005, 3, 546–551. [Google Scholar] [CrossRef]
- Podar, I.; Allik, J. A Cross-Cultural Comparison of the Eating Disorder Inventory. Int. J. Eat. Disord. 2009, 42, 346–355. [Google Scholar] [CrossRef]
- Mallick, N.; Ray, S.; Mukhopadhyay, S. Eating Behaviours and Body Weight Concerns Among Adolescent Girls. Adv. Public Health 2014, 2014, 257396. [Google Scholar] [CrossRef]
- Torstveit, M.K.; Aagedal-Mortensen, K.; Stea, T.H. More Than Half of High School Students Report Disordered Eating: A Cross Sectional Study Among Norwegian Boys and Girls. PLoS ONE 2015, 10, e0122681. [Google Scholar] [CrossRef]
- Adesina, A.F.; Peterside, O.; Anochie, I.; Akani, N.A. Weight Status of Adolescents in Secondary Schools in Port Harcourt Using Body Mass Index (BMI). Ital. J. Pediatr. 2012, 38, 31. [Google Scholar] [CrossRef]
- Del Bibiloni, M.; Pons, A.; Tur, J.A. Prevalence of Overweight and Obesity in Adolescents: A Systematic Review. ISRN Obes. 2013, 2013, 392747. [Google Scholar] [CrossRef]
- Collison, K.S.; Zaidi, M.Z.; Subhani, S.N.; Al-Rubeaan, K.; Shoukri, M.; Al-Mohanna, F.A. Sugar-Sweetened Carbonated Beverage Consumption Correlates with BMI, Waist Circumference, and Poor Dietary Choices in School Children. BMC Public Health 2010, 10, 234. [Google Scholar] [CrossRef]
- Stang, J.S.; Stotmeister, B. Nutrition in Adolescence. In Nutrition Guide for Physicians and Related Healthcare Professionals, 2nd ed.; Humana Press: Cham, Switzerland, 2017; pp. 29–39. [Google Scholar] [CrossRef]
- Smink, F.R.E.; Van Hoeken, D.; Hoek, H.W. Epidemiology of Eating Disorders: Incidence, Prevalence and Mortality Rates. Curr. Psychiatry Rep. 2012, 14, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Micali, N.; Solmi, F.; Horton, N.J.; Crosby, R.D.; Eddy, K.T.; Calzo, J.P.; Sonneville, K.R.; Swanson, S.A.; Field, A.E. Adolescent Eating Disorders Predict Psychiatric, High-Risk Behaviors and Weight Outcomes in Young Adulthood. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 652–659.e1. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.; Saif, Z.; Faris, M.A.-I.; Levine, M.P. The Relationship Between Risk of Eating Disorders, Age, Gender and Body Mass Index in Medical Students: A Meta-Regression. Eat. Weight Disord.—Stud. Anorex. Bulim. Obes. 2018, 24, 169–177. [Google Scholar] [CrossRef]
- Ward, Z.J.; Rodriguez, P.; Wright, D.R.; Austin, S.B.; Long, M.W. Estimation of Eating Disorders Prevalence by Age and Associations with Mortality in a Simulated Nationally Representative US Cohort. JAMA Netw. Open 2019, 2, e1912925. [Google Scholar] [CrossRef]
- Pike, K.M.; Dunne, P.E. The Rise of Eating Disorders in Asia: A Review. J. Eat. Disord. 2015, 3, 33. [Google Scholar] [CrossRef]
- Van Hoeken, D.; Burns, J.K.; Hoek, H.W. Epidemiology of Eating Disorders in Africa. Curr. Opin. Psychiatry 2016, 29, 372–377. [Google Scholar] [CrossRef]
- Yeh, H.-W.; Tzeng, N.-S.; Chu, H.; Chou, Y.-H.; Lu, R.-B.; O’Brien, A.P.; Chang, Y.-C.; Hsieh, C.-J.; Chou, K.-R. The Risk of Eating Disorders Among Female Undergraduates in Taiwan. Arch. Psychiatr. Nurs. 2009, 23, 430–440. [Google Scholar] [CrossRef] [PubMed]
- Ung, E.K. Eating disorders in Singapore: A review. Ann. Acad. Med. Singap. 2003, 32, 19–24. [Google Scholar]
- Taha, A.A.A.E.-A.; Abu-Zaid, H.A.; Desouky, D.E.-S. Eating disorders among female students of Taif University, Saudi Arabia. Arch. Iran. Med. 2018, 21, 111–117. [Google Scholar]
- Afifi-Soweid, R.A.; Najem Kteily, M.B.; Shediac-Rizkallah, M.C. Preoccupation with Weight and Disordered Eating Behaviors of Entering Students at a University in Lebanon. Int. J. Eat. Disord. 2002, 32, 52–57. [Google Scholar] [CrossRef]
- Al Sabbah, H.; Vereecken, C.; Abdeen, Z.; Kelly, C.; Ojala, K.; Németh, Á.; Ahluwalia, N.; Maes, L. Weight Control Behaviors Among Overweight, Normal Weight and Underweight Adolescents in Palestine: Findings from the National Study of Palestinian Schoolchildren (HBSC-WBG2004). Int. J. Eat. Disord. 2009, 43, 326–336. [Google Scholar] [CrossRef]
- Attouche, N.; Hafdi, S.; Somali, R.; Battas, O.; Agoub, M. Factors associated with the risk of developing eating disorders among medical students in Casablanca, Morocco. Pan Afr. Med. J. 2021, 39, 270. [Google Scholar] [PubMed]
- Lesthaeghe, R. The Second Demographic Transition, 1986–2020: Sub-Replacement Fertility and Rising cohabitation—A Global Update. Genus 2020, 76, 10. [Google Scholar] [CrossRef]
- Musaiger, A.O.; Al-Mannai, M.; Tayyem, R.; Al-Lalla, O.; Ali, E.Y.; Kalam, F.; Benhamed, M.M.; Saghir, S.; Halahleh, I.; Djoudi, Z.; et al. Risk of Disordered Eating Attitudes Among Adolescents in Seven Arab Countries by Gender and Obesity: A Cross-Cultural Study. Appetite 2013, 60, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Azzeh, M.; Peachey, G.; Loney, T. Prevalence of High-Risk Disordered Eating Amongst Adolescents and Young Adults in the Middle East: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 5234. [Google Scholar] [CrossRef]
- Al-Rethaiaa, A.S.; Fahmy, A.-E.A.; Al-Shwaiyat, N.M. Obesity and Eating Habits Among College Students in Saudi Arabia: A Cross Sectional Study. Nutr. J. 2010, 9, 39. [Google Scholar] [CrossRef] [PubMed]
- Khalaf, A.; Westergren, A.; Berggren, V.; Ekblom, Ö.; Al-Hazzaa, H.M. Prevalence and Association of Female Weight Status and Dietary Habits with Sociodemographic Factors: A Cross-Sectional Study in Saudi Arabia. Public Health Nutr. 2014, 18, 784–796. [Google Scholar] [CrossRef]
- Al-Hazzaa, H.M.; Abahussain, N.A.; Al-Sobayel, H.I.; Qahwaji, D.M.; Musaiger, A.O. Physical Activity, Sedentary Behaviors and Dietary Habits Among Saudi Adolescents Relative to Age, Gender and Region. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 140. [Google Scholar] [CrossRef] [PubMed]
- Latzer, Y.; Azaiza, F.; Tzischinsky, O. Not Just a Western Girls. Int. J. Adolesc. Youth 2012, 19, 382–394. [Google Scholar] [CrossRef]
- Hay, P.; Mitchison, D. Urbanization and Eating Disorders: A Scoping Review of Studies from 2019 to 2020. Curr. Opin. Psychiatry 2020, 34, 287–292. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef] [PubMed]
- Moola, S.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Qureshi, R.; Mattis, P.; Lisy, K.; PF, M. Chapter 7: Systematic reviews of etiology and risk. Joanna Briggs Inst. 2017, 5, 217–269. [Google Scholar] [CrossRef]
- Garner, D.M.; Olmsted, M.P.; Bohr, Y.; Garfinkel, P.E. The Eating Attitudes Test: Psychometric Features and Clinical Correlates. Psychol. Med. 1982, 12, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Gleaves, D.H.; Pearson, C.A.; Ambwani, S.; Morey, L.C. Measuring Eating Disorder Attitudes and Behaviors: A Reliability Generalization Study. J. Eat. Disord. 2014, 2, 6. [Google Scholar] [CrossRef]
- Garner, D.M.; Olmstead, M.P.; Polivy, J. Development and Validation of a Multidimensional Eating Disorder Inventory for Anorexia Nervosa and Bulimia. Int. J. Eat. Disord. 1983, 2, 15–34. [Google Scholar] [CrossRef]
- Garner, D.M. Eating disorder Inventory-2; pro-fessional manual. Psychol. Assess. Resour. 1991, 39–48. [Google Scholar]
- Cooper, Z.; Fairburn, C. The Eating Disorder Examination: A Semi-Structured Interview for the Assessment of the Specific Psychopathology of Eating Disorders. Int. J. Eat. Disord. 1987, 6, 1–8. [Google Scholar] [CrossRef]
- Fairburn, C.G. Cognitive Behavior Therapy and Eating Disorders; Guilford Press: New York, NY, USA, 2008. [Google Scholar]
- Luce, K.H.; Crowther, J.H. The Reliability of the Eating Disorder examination?Self-Report Questionnaire Version (EDE-Q). Int. J. Eat. Disord. 1999, 25, 349–351. [Google Scholar] [CrossRef]
- Kagan, S. The SCOFF Questionnaire Was Less Sensitive but More Specific Than the ESP for Detecting Eating Disorders. Evid.-Based Nurs. 2003, 6, 118. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Luck, A.J.; MorganLuck, J.F.; Reid, F.; O’Brien, A.; Brunton, J.; Price, C.; Perry, L.; Lacey, J.H. The SCOFF Questionnaire and Clinical Interview for Eating Disorders in General Practice: Comparative Study. BMJ 2002, 325, 755–756. [Google Scholar] [CrossRef] [PubMed]
- Morgan, J.F.; Reid, F.; Lacey, J.H. The SCOFF Questionnaire: Assessment of a New Screening Tool for Eating Disorders. BMJ 1999, 319, 1467–1468. [Google Scholar] [CrossRef] [PubMed]
- Alfhaid, F.M.; Alraddadi, M.M.R.; Alanazi, A.S.A.; Alrashidi, A.S.M.; Alrashedi, L.S.O.; Alothaim, A.M.A.; Alqarni, M.A.M.; Almanaah, M.A.M. Eating disorders among Majmaah University Students, Saudi Arabia. Med. Sci. 2021, 25, 3007–3016. [Google Scholar]
- Naguib, R.; Tawfik, M.R.; Alsubaiei, S.; Almoallem, A.; Alajlouni, D.; Alruwaili, T.; Sendy, W.; Al Habib, Z. Study of Bodyweight and Eating Attitude Among Female University Members in the Kingdom of Saudi Arabia: A Comparison Between Different Methods of Weight Assessment. J. Fam. Med. Prim. Care 2020, 9, 2071. [Google Scholar] [CrossRef]
- Almuhlafi, M.; Abu Jamilah, K.; Almutairi, A.; Salam, M. Relationship Between Early Menarche, Obesity, and Disordered Eating Behaviors: A School-Based Cross-Sectional Survey in Northern Saudi Arabia. Diabetes Metab. Syndr. Obes. Targets Ther. 2018, 11, 743–751. [Google Scholar] [CrossRef]
- Alhazmi, A.H.; Al Johani, A. Prevalence and associated factors of eating disorders among students in Taiba University, Saudi Arabia: A cross-sectional study. Malays. J. Public Health Med. 2019, 19, 172–176. [Google Scholar] [CrossRef]
- Allihaibi, M. Disordered Eating Attitudes Among Secondary Schoolgirls in Al-Iskan Sector, Makkah Al-Mukarramah, Saudi Arabia. Int. J. Med. Sci. Public Health 2015, 4, 939. [Google Scholar] [CrossRef]
- Alsubaie, S.; Alalfard, A.; Muhaya, A.; Alalfard, H.; Abdullah, K.; Albishi, H. Prevalence of Eating Disorders and Obsessive-Compulsive Disorder among Adolescents Schoolgirls: Sample from Abha City Southern Saudi Arabia. EC Psychol. Psychiatry 2020, 9, 1–10. Available online: https://api.semanticscholar.org/CorpusID:213843839 (accessed on 26 July 2023).
- Al-Subaie, A.S. Some correlates of dieting behavior in Saudi schoolgirls. Int. J. Eat. Disord. 2000, 28, 242–246. [Google Scholar] [CrossRef]
- Al-Qahtani, A.M.; Al-Harbi, L.M. Prevalence and risk factors of disordered eating attitudes and behaviors among high-school girls in Al-Madinah City, Saudi Arabia. Curr. Nutr. Food Sci. 2020, 16, 709–717. [Google Scholar] [CrossRef]
- Ghafouri, K.J.; Qadhi, A.H.; Ghaith, M.M.; Azhar, W.F.; Azzeh, F.S.; Habibullah, M.M. Eating disorders amongst adolescents in Makkah: Effects of stress and smoking. Med. Sci. 2021, 25, 767–775. [Google Scholar]
- Fatima, W.; Ahmad, L.M. Prevalence of disordered eating attitudes among adolescent girls in Arar City, Kingdom of Saudi Arabia. Health Psychol. Res. 2018, 6, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Tomar, R.; Antony, V.C. Assessment of eating disorder and obesity among youth in Saudi Arabia. Med. Sci. 2021, 25, 2660–2669. [Google Scholar]
- Alwosaifer, A.M.; Alawadh, S.A.; Wahab, M.M.A.; Boubshait, L.A.; Almutairi, B.A. Eating disorders and associated risk factors among Imam Abdulrahman bin Faisal university preparatory year female students in Kingdom of Saudi Arabia. Saudi Med. J. 2018, 39, 910. [Google Scholar] [CrossRef]
- Albrahim, T.; Alrubaish, A.A.; Alfadhliah, J.T.S.; Alaskar, M.K.; Alatawi, M.A.; Aldekhayyil, S.A. The spectrum of disordered eating attitudes among female university students: A cross-sectional study. Curr. Res. Nutr. Food Sci. J. 2019, 7, 698–707. [Google Scholar] [CrossRef]
- El Shikieri, A.B. The prevalence and nutritional status of adolescent Saudi girls with disordered eating. J. Nutr. Sci. 2022, 11, e71. [Google Scholar] [CrossRef]
- Fallatah, A.; Al-Hemairy, M.; Al-Ghamidi, H. Eating disorders among female adolescents in Jeddah. C COOP 2015, 138, 138–147. [Google Scholar]
- Loni, S.B.; Sami, W.; Abd-Elhaleem, Z.A.; Ejiel, M.M.N.I.; Gadir, G.A.G.M.A.; Khan, M.O. Prevalence of Eating Disorders among Students of Health Science Colleges in Majamaah University, Saudi Arabia. Pak. J. Med. Health Sci. 2022, 16, 886. [Google Scholar] [CrossRef]
- Daly, A.N.; O’Sullivan, E.J.; Kearney, J.M. Considerations for health and food choice in adolescents. Proc. Nutr. Soc. 2022, 81, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Noma, S.I.; Nakai, Y.; Hamagaki, S.; Uehara, M.; Hayashi, A.; Hayashi, T. Comparison between the SCOFF questionnaire and the Eating Attitudes Test in patients with eating disorders. Int. J. Psychiatry Clin. Pract. 2006, 10, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Engelsen, B.K.; Laberg, J.C. A comparison of three questionnaires (EAT-12, EDI, and EDE-Q) for assessment of eating problems in healthy female adolescents. Nord. J. Psychiatry 2001, 55, 129–135. [Google Scholar] [CrossRef]
- Musaiger, A.O. Body size preferences among young women in five Arab countries: A cross-cultural study. Int. J. Adolesc. Med. Health 2014, 26, 417–421. [Google Scholar] [CrossRef] [PubMed]
- Eapen, V.; Mabrouk, A.A.; Bin-Othman, S. Disordered eating attitudes and symptomatology among adolescent girls in the United Arab Emirates. Eat. Behav. 2006, 7, 53–60. [Google Scholar] [CrossRef]
- Mousa, T.Y.; Al-Domi, H.A.; Mashal, R.H.; Jibril, M.A.-K. Eating disturbances among adolescent schoolgirls in Jordan. Appetite 2010, 54, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Al-Adawi, S.; Dorvlo, A.; Burke, D.; Moosa, S.; Al-Bahlani, S. A survey of anorexia nervosa using the Arabic version of the EAT-26 and “gold standard” interviews among Omani adolescents. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2002, 7, 304–311. [Google Scholar] [CrossRef]
- Garrusi, B.; Baneshi, M.R.; Pakgohar, M. Eating disorders among Iranian male adolescents. Iran. J. Psychiatry Behav. Sci. 2016, 10, e5352. [Google Scholar] [CrossRef]
- Jalali-Farahani, S.; Chin, Y.S.; Mohd Nasir, M.T.; Amiri, P. Disordered eating and its association with overweight and health-related quality of life among adolescents in selected high schools of Tehran. Child Psychiatry Hum. Dev. 2015, 46, 485–492. [Google Scholar] [CrossRef]
- Rauof, M.; Ebrahimi, H.; Jafarabadi, M.A.; Malek, A.; Kheiroddin, J.B. Prevalence of eating disorders among adolescents in the Northwest of Iran. Iran. Red Crescent Med. J. 2015, 17, e19331. [Google Scholar] [CrossRef]
- Sahlan, R.N.; Saunders, J.F.; Mond, J.M.; Fitzsimmons-Craft, E.E. Eating disorder symptoms among adolescent boys and girls in Iran. Int. J. Eat. Disord. 2021, 54, 19–23. [Google Scholar] [CrossRef] [PubMed]
- El-Bagoury, L.; Hassan, A.; AbouSeif, H. Eating attitudes and barriers to healthy eating and physical activity among a sample of university students in Egypt. J. Egypt. Public Health Assoc. 2017, 92, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Takimoto, H.; Yoshiike, N.; Kaneda, F.; Yoshita, K. Thinness among young Japanese women. Am. J. Public Health 2004, 94, 1592–1595. [Google Scholar] [CrossRef] [PubMed]
- Elgin, J.; Pritchard, M. Gender differences in disordered eating and its correlates. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2006, 11, e96–e101. [Google Scholar] [CrossRef]
- Ferreiro, F.; Seoane, G.; Senra, C. Toward understanding the role of body dissatisfaction in the gender differences in depressive symptoms and disordered eating: A longitudinal study during adolescence. J. Adolesc. 2014, 37, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Memon, A.A.; Adil, S.E.-e.-R.; Siddiqui, E.U.; Naeem, S.S.; Ali, S.A.; Mehmood, K. Eating disorders in medical students of Karachi, Pakistan-a cross-sectional study. BMC Res. Notes 2012, 5, 84. [Google Scholar] [CrossRef] [PubMed]
- Bartholdy, S.; Allen, K.; Hodsoll, J.; O’Daly, O.G.; Campbell, I.C.; Banaschewski, T.; Bokde, A.L.; Bromberg, U.; Büchel, C.; Quinlan, E.B. Identifying disordered eating behaviours in adolescents: How do parent and adolescent reports differ by sex and age? Eur. Child Adolesc. Psychiatry 2017, 26, 691–701. [Google Scholar] [CrossRef]
- Lähteenmäki, S.; Saarni, S.; Suokas, J.; Saarni, S.; Perälä, J.; Lönnqvist, J.; Suvisaari, J. Prevalence and correlates of eating disorders among young adults in Finland. Nord. J. Psychiatry 2014, 68, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Al-Kloub, M.I.; Al-Khawaldeh, O.A.; ALBashtawy, M.; Batiha, A.M.; Al-Haliq, M. Disordered eating in Jordanian adolescents. Int. J. Nurs. Pract. 2019, 25, e12694. [Google Scholar] [CrossRef]
- Al-Sheyab, N.A.; Gharaibeh, T.; Kheirallah, K. Relationship between peer pressure and risk of eating disorders among adolescents in Jordan. J. Obes. 2018, 2018, 7309878. [Google Scholar] [CrossRef]
- Katz, B. Gender and disordered eating of adolescents in Israel. Isr. J. Psychiatry Relat. Sci. 2014, 5, 137–144. [Google Scholar]
- Maor, N.R.; Sayag, S.; Dahan, R.; Hermoni, D. Eating attitudes among adolescents. IMAJ-RAMAT GAN- 2006, 8, 627. [Google Scholar]
- Mohammadi, M.R.; Mostafavi, S.A.; Hooshyari, Z.; Khaleghi, A.; Ahmadi, N.; Molavi, P.; Armani Kian, A.; Safavi, P.; Delpisheh, A.; Talepasand, S. Prevalence, correlates and comorbidities of feeding and eating disorders in a nationally representative sample of Iranian children and adolescents. Int. J. Eat. Disord. 2020, 53, 349–361. [Google Scholar] [CrossRef] [PubMed]
- Sweeting, H.; Walker, L.; MacLean, A.; Patterson, C.; Räisänen, U.; Hunt, K. Prevalence of eating disorders in males: A review of rates reported in academic research and UK mass media. Int. J. Men’s Health 2015, 14. [Google Scholar]
- Micali, N.; Hagberg, K.W.; Petersen, I.; Treasure, J.L. The incidence of eating disorders in the UK in 2000–2009: Findings from the General Practice Research Database. BMJ Open 2013, 3, e002646. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.-C.; Jung, Y.-E.; Kim, M.-D.; Lee, C.-I.; Hyun, M.-Y.; Bahk, W.-M.; Yoon, B.-H.; Lee, K.H. Prevalence of distorted body image in young Koreans and its association with age, sex, body weight status, and disordered eating behaviors. Neuropsychiatr. Dis. Treat. 2015, 11, 1043–1049. [Google Scholar] [CrossRef] [PubMed]
- Seepersad, R. The relation between eating disorders and self esteem in adolescents in Trinidad. J. Dep. Behav. Sci. 2012, 2, 102–127. [Google Scholar]
- Elal, G.; Sabol, E.; Slade, P. Abnormal eating attitudes and sexual abuse experiences in Turkish university women. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2004, 9, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Şanlier, N.; Yabanci, N.; Alyakut, Ö. An evaluation of eating disorders among a group of Turkish university students. Appetite 2008, 51, 641–645. [Google Scholar] [CrossRef]
- Sanlier, N.; Yassibas, E.; Bilici, S.; Sahin, G.; Celik, B. Does the rise in eating disorders lead to increasing risk of orthorexia nervosa? Correlations with gender, education, and body mass index. Ecol. Food Nutr. 2016, 55, 266–278. [Google Scholar] [CrossRef] [PubMed]
- Vardar, E.; Erzengın, M. The prevalence of eating disorders (EDs) and comorbid psychiatric disorders in adolescents: A two-stage community-based study. Turk. J. Psychiatry 2011, 22, 205–212. [Google Scholar]
- Nishizawa, Y.; Kida, K.; Nishizawa, K.; Hashiba, S.; Saito, K.; Mita, R. Perception of self-physique and eating behavior of high school students in Japan. Psychiatry Clin. Neurosci. 2003, 57, 189–196. [Google Scholar] [CrossRef]
- Tsai, M.-R.; Chang, Y.-J.; Lien, P.-J.; Wong, Y. Survey on eating disorders related thoughts, behaviors and dietary intake in female junior high school students in Taiwan. Asia Pac. J. Clin. Nutr. 2011, 20, 196–205. [Google Scholar]
- Yang, S.-J.; Choi, Y.; LEE, H.-Y. Eating attitude, ego-identity, and self-esteem among the urban high school girls. J. Korean Neuropsychiatr. Assoc. 2001, 40, 477–486. [Google Scholar]
- Szweda, S.; Thorne, P. The prevalence of eating disorders in female health care students. Occup. Med. 2002, 52, 113–119. [Google Scholar] [CrossRef]
- Graber, J.A.; Tyrka, A.R.; Brooks-Gunn, J. How similar are correlates of different subclinical eating problems and bulimia nervosa? J. Child Psychol. Psychiatry 2003, 44, 262–273. [Google Scholar] [CrossRef]
- Jones, J.M.; Bennett, S.; Olmsted, M.P.; Lawson, M.L.; Rodin, G. Disordered eating attitudes and behaviours in teenaged girls: A school-based study. CMAJ 2001, 165, 547–552. [Google Scholar]
- Garner, D.M.; Garfinkel, P.E. Socio-cultural factors in the development of anorexia nervosa. Psychol. Med. 1980, 10, 647–656. [Google Scholar] [CrossRef]
- Makino, M.; Tsuboi, K.; Dennerstein, L. Prevalence of eating disorders: A comparison of Western and non-Western countries. Medscape Gen. Med. 2004, 6, 49. [Google Scholar]
- Keel, P.K.; Klump, K.L. Are eating disorders culture-bound syndromes? Implications for conceptualizing their etiology. Psychol. Bull. 2003, 129, 747. [Google Scholar] [CrossRef]
- Abdollahi, P.; Mann, T. Eating disorder symptoms and body image concerns in Iran: Comparisons between Iranian women in Iran and in America. Int. J. Eat. Disord. 2001, 30, 259–268. [Google Scholar] [CrossRef] [PubMed]
- Abou-Saleh, M.T.; Younis, Y.; Karim, L. Anorexia nervosa in an Arab culture. Int. J. Eat. Disord. 1998, 23, 207–212. [Google Scholar] [CrossRef]
- Fath Al Alim, M.A.; Noon, H.A.; Abdelghani, A. Eating disorders symptoms among a university students: An exploratory study. Sudan Med. J. 2012, 48, 186–193. [Google Scholar]
- Musaiger, A.O.; Al-Mannai, M. Association between exposure to media and body weight concern among female university students in five Arab countries: A preliminary cross-cultural study. J. Biosoc. Sci. 2014, 46, 240–247. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, C.M.; Forman, S.F.; Austin, S.B. Follow-up evaluation of a high school eating disorders screening program: Knowledge, awareness and self-referral. J. Adolesc. Health 2005, 36, 208–213. [Google Scholar] [CrossRef]
- Wang, X.; Cheng, Z. Cross-sectional studies: Strengths, weaknesses, and recommendations. Chest 2020, 158, S65–S71. [Google Scholar] [CrossRef] [PubMed]
- Signal, D.M.; Hofman, P.L. Type 1 diabetes youth with disordered eating: Is there a disproportionate impact on ethnic minorities and indigenous peoples? J. Paediatr. Child Health 2022, 58, 562–565. [Google Scholar] [CrossRef]
- Colton, P.; Olmsted, M.; Daneman, D.; Rydall, A.; Rodin, G. Disturbed eating behavior and eating disorders in preteen and early teenage girls with type 1 diabetes: A case-controlled study. Diabetes Care 2004, 27, 1654–1659. [Google Scholar] [CrossRef]
- Froreich, F.V.; Vartanian, L.R.; Grisham, J.R.; Touyz, S.W. Dimensions of control and their relation to disordered eating behaviours and obsessive-compulsive symptoms. J. Eat. Disord. 2016, 4, 14. [Google Scholar] [CrossRef]
- Althubaiti, A. Information bias in health research: Definition, pitfalls, and adjustment methods. J. Multidiscip. Healthc. 2016, 9, 211–217. [Google Scholar] [CrossRef] [PubMed]
| Components | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Healthy adolescent and young adult participants aged 10–24 years. | Participants with certain metabolic or mental/psychiatric disorders (Attention Deficit Hyperactivity Disorder (ADHD), Obsessive Compulsory Disorder (OCD)). |
| Exposure | Studies assessing eating disorders, disordered eating, feeding disorders, appetite disorders, anorexia nervosa or bulimia nervosa, binge eating, disturbed eating, weight control, or purging. | Studies assessing orthorexia disorder, Pica, and rumination disorder. |
| Context | Collected samples from Saudi Arabia | Samples from outside Saudi Arabian borders |
| Outcome | Studies measuring the prevalence of EDs/DEB with a validated tool: self-reported questionnaire (EAT-26, EDE-Q…) | Studies focussed on clinical assessment, interviews, or weight-history taking to assess the prevalence of ED/DEB |
| Study design | Cross-sectional and longitudinal studies are both eligible. Journal articles published in peer-reviewed journals and conference papers. | Qualitative studies (case reports), books, editorials, dissertations, systematic/narrative reviews. Studies published in Arabic with no available English translation since English is regarded as the universal language of science. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsheweir, A.; Goyder, E.; Alnooh, G.; Caton, S.J. Prevalence of Eating Disorders and Disordered Eating Behaviours amongst Adolescents and Young Adults in Saudi Arabia: A Systematic Review. Nutrients 2023, 15, 4643. https://doi.org/10.3390/nu15214643
Alsheweir A, Goyder E, Alnooh G, Caton SJ. Prevalence of Eating Disorders and Disordered Eating Behaviours amongst Adolescents and Young Adults in Saudi Arabia: A Systematic Review. Nutrients. 2023; 15(21):4643. https://doi.org/10.3390/nu15214643
Chicago/Turabian StyleAlsheweir, Azzah, Elizabeth Goyder, Ghadah Alnooh, and Samantha J. Caton. 2023. "Prevalence of Eating Disorders and Disordered Eating Behaviours amongst Adolescents and Young Adults in Saudi Arabia: A Systematic Review" Nutrients 15, no. 21: 4643. https://doi.org/10.3390/nu15214643
APA StyleAlsheweir, A., Goyder, E., Alnooh, G., & Caton, S. J. (2023). Prevalence of Eating Disorders and Disordered Eating Behaviours amongst Adolescents and Young Adults in Saudi Arabia: A Systematic Review. Nutrients, 15(21), 4643. https://doi.org/10.3390/nu15214643






