Sleep Pathologies and Eating Disorders: A Crossroad for Neurology, Psychiatry and Nutrition
Abstract
1. Introduction
2. Eating Disorders and Sleep: What the Sleep Expert Should Know
2.1. Anorexia Nervosa (AN)
2.2. Bulimia Nervosa (BN)
2.3. Binge Eating Disorder (BED)
2.4. Obesity
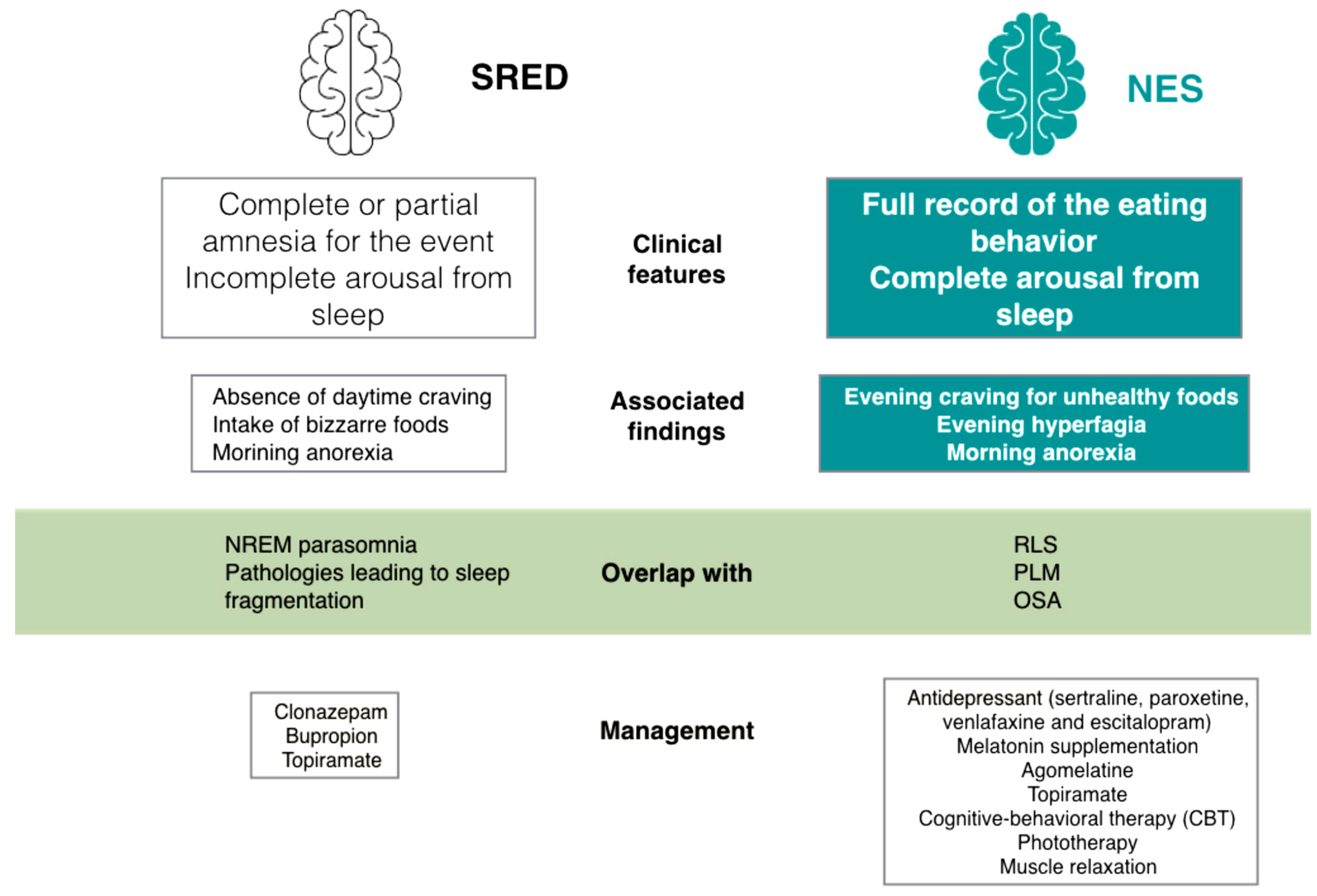
3. Sleep-Related Eating Behaviors: What the Psychiatric Should Know
3.1. Nocturnal Eating Syndrome
3.1.1. NES Management
3.1.2. NES and Coexistent Sleep Disorders
3.2. Sleep-Related Eating Disorder (SRED)
SRED and Coexistent Sleep Disorders
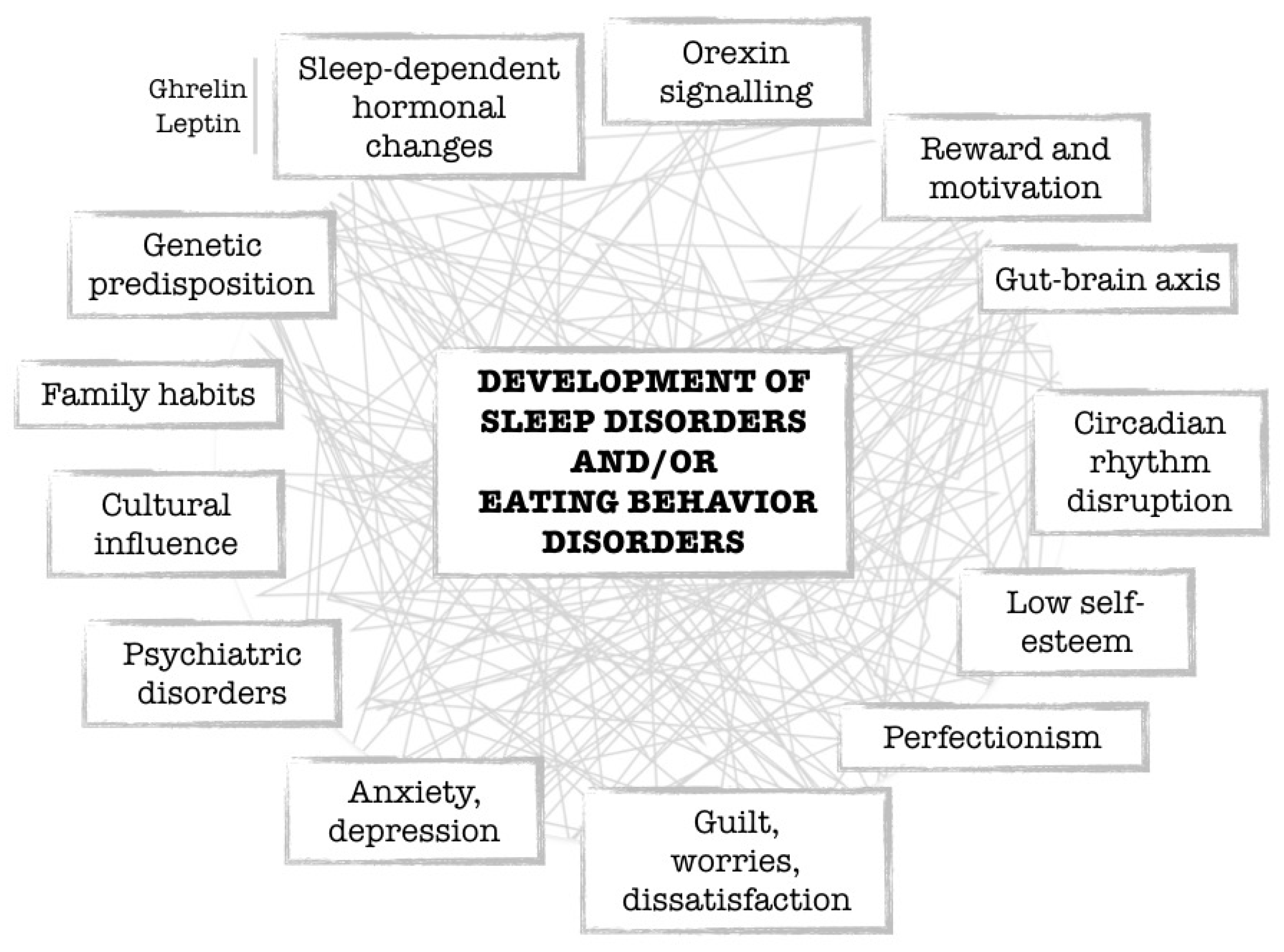
4. Sleep Disorders Associated with Eating Disorders: A Cross-Road for Neurologist, Psychiatrist and Nutritionist
4.1. Narcolepsy and Eating Disorders
4.2. Kleine-Levin Syndrome
4.3. Sleep Deprivation and Eating Behaviors
5. Sleep and Microbiota
6. COVID-19, Sleep and Eating Behaviors
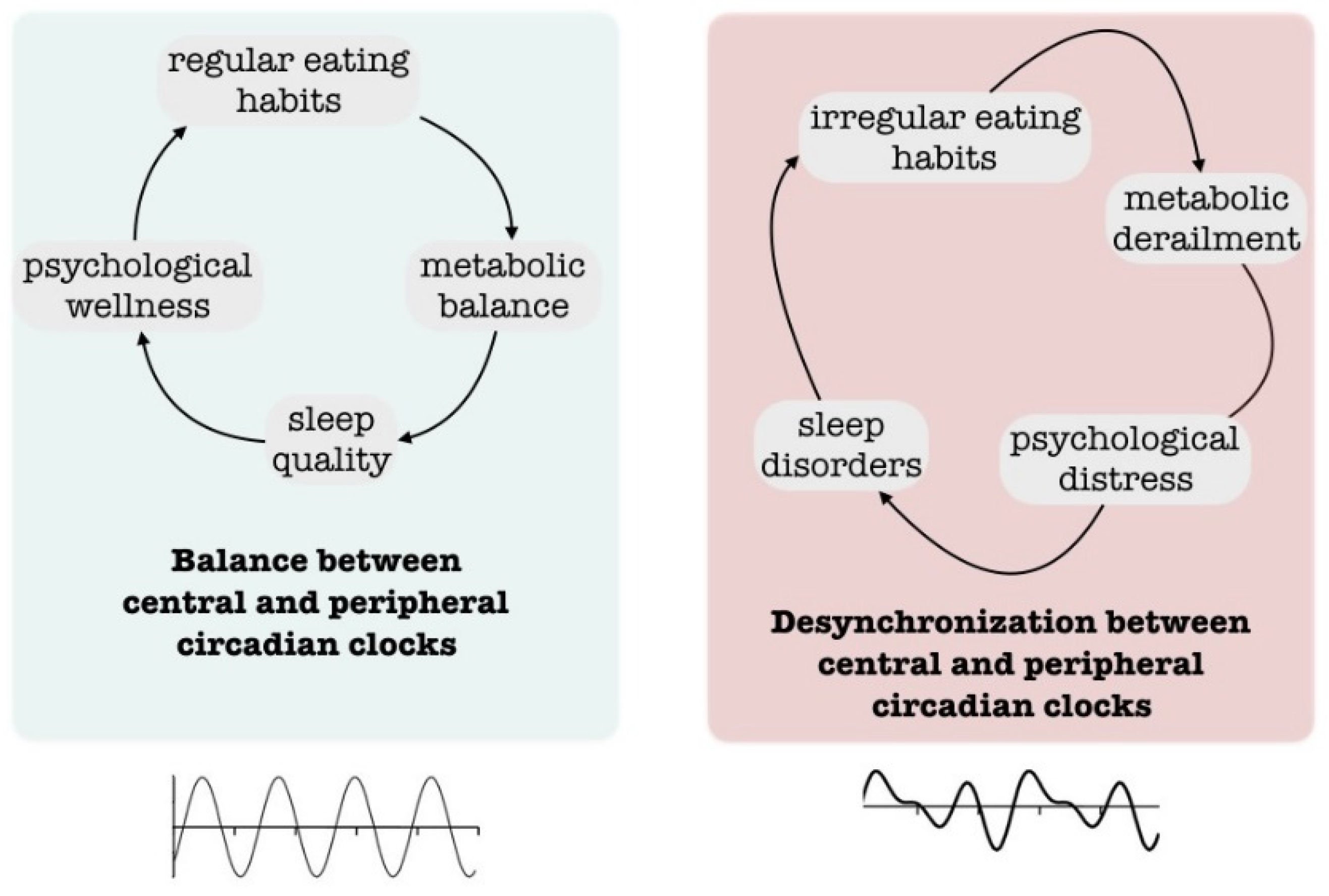
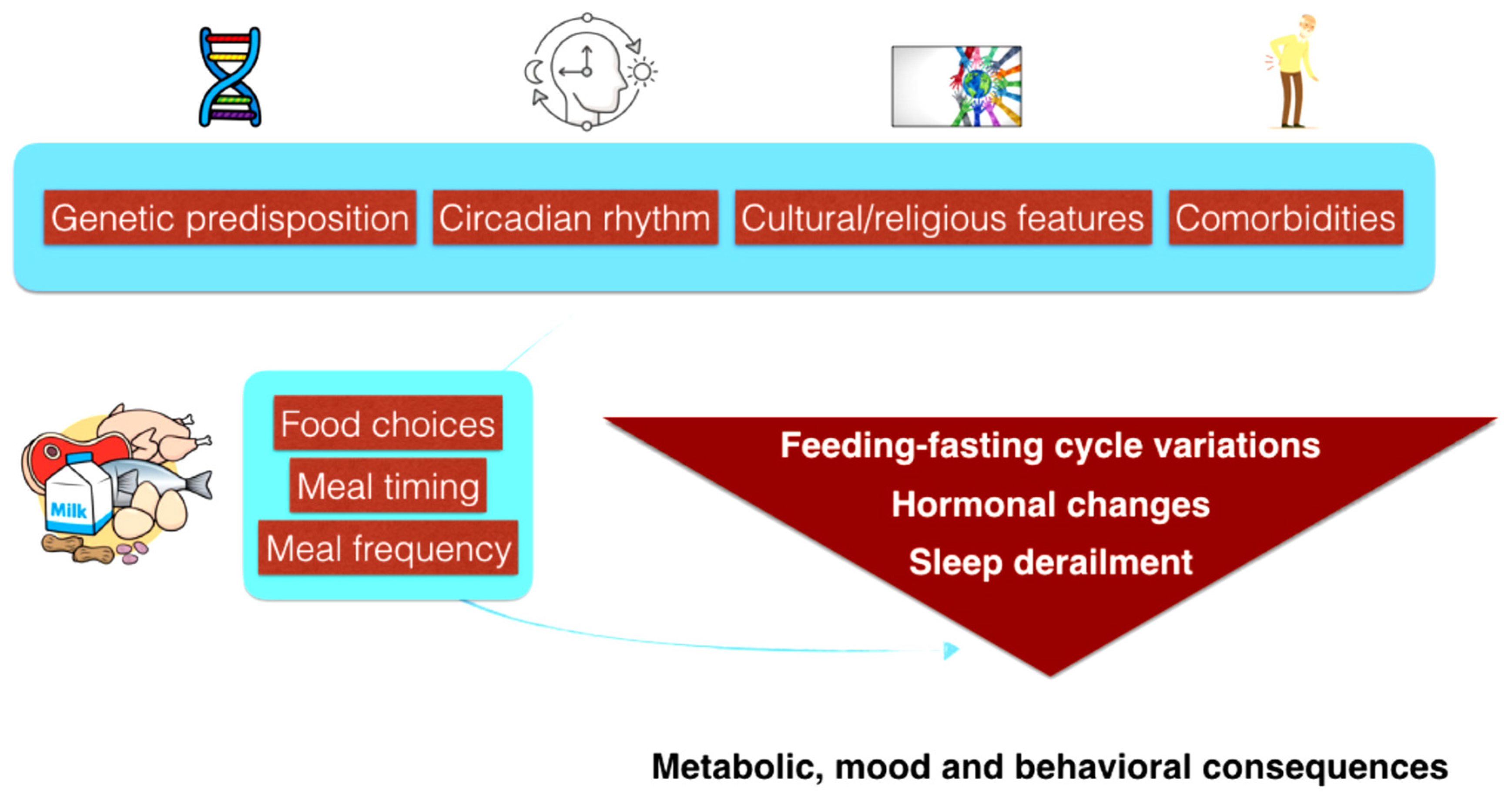
7. Impact of Culture and Chronobiology
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Wrangham, R. The evolution of human nutrition. Curr. Biol. CB 2013, 23, R354–R355. [Google Scholar] [CrossRef] [PubMed]
- Nunn, C.L.; Samson, D.R.; Krystal, A.D. Shining evolutionary light on human sleep and sleep disorders. Evol. Med. Public Health 2016, 2016, 227–243. [Google Scholar] [CrossRef] [PubMed]
- Samson, D.R.; Nunn, C.L. Sleep intensity and the evolution of human cognition. Evol. Anthropol. 2015, 24, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Mutti, C.; Misirocchi, F.; Zilioli, A.; Rausa, F.; Pizzarotti, S.; Spallazzi, M.; Parrino, L. Sleep and brain evolution across the human lifespan: A mutual embrace. Front. Netw. Physiol. 2022, 2, 938012. [Google Scholar] [CrossRef]
- Cornélio, A.M.; de Bittencourt-Navarrete, R.E.; de Bittencourt Brum, R.; Queiroz, C.M.; Costa, M.R. Human Brain Expansion during Evolution Is Independent of Fire Control and Cooking. Front. Neurosci. 2016, 10, 167. [Google Scholar] [CrossRef]
- Ennos, R. The Age of Wood: Our Most Useful Material and the Construction of Civilization; Scriber: New York, NY, USA, 2020. [Google Scholar]
- Suzman, J. Work: A History of How We Spend Our Time; Bloomsbury: London, UK, 2020. [Google Scholar]
- Vilar-Compte, M.; Burrola-Méndez, S.; Lozano-Marrufo, A.; Ferré-Eguiluz, I.; Flores, D.; Gaitán-Rossi, P.; Teruel, G.; Pérez-Escamilla, R. Urban poverty and nutrition challenges associated with accessibility to a healthy diet: A global systematic literature review. Int. J. Equity Health 2021, 20, 40. [Google Scholar] [CrossRef]
- World Health Organization. Healthy Diet for Adults. Available online: http://www.emro.who.int/noncommunicable-diseases/campaigns/healthy-diet-for-adults.html (accessed on 20 August 2023).
- Leger, D.; Guilleminault, C.; Bader, G.; Levy, E.; Paillard, M. Medical and Socio-professional impact of insomnia. Sleep 2002, 25, 621–625. [Google Scholar] [CrossRef]
- Fuller, C.; Lehman, E.; Hicks, S.; Novick, M.B. Bedtime Use of Technology and Associated Sleep Problems in Children. Glob. Pediatr. Health 2017, 4, 2333794X17736972. [Google Scholar] [CrossRef]
- Fassino, S.; Abbate Daga, G.; Defilippi, S.; Gianotti, L.; Gastaldi, F.; Delsedime, N. Sleep and eating disorders: A review. G. Ital. Psicopatol. 2005, 11, 354–362. [Google Scholar]
- Ellis, J.G.; Perlis, M.L.; Espie, C.A.; Grandner, M.A.; Bastien, C.H.; Barclay, N.L.; Altena, E.; Gardani, M. The natural history of insomnia: Predisposing, precipitating, coping, and perpetuating factors over the early developmental course of insomnia. Sleep 2021, 44, zsab095. [Google Scholar] [CrossRef]
- Capovani, B.; Mauri, M.; Borri, C.; Baldassarri, M.; Miniati, M.; Cassano, G.B. Comorbidità nei disturbi del comportamento alimentare. G. Ital. Psicopatol. 1999, 5, 38–44. [Google Scholar]
- Milos, G.F.; Spindler, A.M.; Buddeberg, C.; Crameri, A. Axis I and II comorbidity and treatment experiences in eating disorder subjects. Psychoter. Psychosom. 2003, 72, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Goel, N.J.; Sadeh-Sharvit, S.; Trockel, M.; Flatt, R.E.; Fitzsimmons-Craft, E.E.; Balantekin, K.N.; Monterubio, G.E.; Firebaugh, M.L.; Wilfley, D.E.; Taylor, C.B. Depression and anxiety mediate the relationship between insomnia and eating disorders in college women. J. Am. Coll. Health 2021, 69, 976–981. [Google Scholar] [CrossRef] [PubMed]
- Galmiche, M.; Déchelotte, P.; Lambert, G.; Tavolacci, M.P. Prevalence of eating disorders over the 2000–2018 period: A systematic literature review. Am. J. Clin. Nutr. 2019, 109, 1402–1413. [Google Scholar] [CrossRef]
- Leproult, R.; Van Cauter, E. Role of sleep and sleep loss in hormonal release and metabolism. Endocr. Dev. 2010, 17, 11–21. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5): Feeding and Eating Disorders; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Heimann, P.M.; Konrad, K.; Vloet, T.D. Anorexia nervosa bei Jungen [Anorexia nervosa in males]. Z Kinder Jugendpsychiatr. Psychother. 2018, 46, 478–487. [Google Scholar] [CrossRef]
- Munno, D.; Sterpone, S.C.M.; Zullo, G. L’anoressia nervosa maschile. Una review. G. Ital. Psicopatol. 2005, 11, 215–224. [Google Scholar]
- Ralph-Nearman, C.; Williams, B.M.; Ortiz, A.; Smith, A.R.; Levinson, C.A. Pinpointing core and pathway symptoms among sleep disturbance, anxiety, worry, and eating disorder symptoms in anorexia nervosa and atypical anorexia nervosa. J. Affect. Disord. 2021, 294, 24–32. [Google Scholar] [CrossRef]
- Malcolm, A.; Toh, W.L.; Crocker, K.; Phillipou, A. The contribution of sleep to anorexia nervosa severity. Eat. Weight. Disord. 2021, 27, 1563–1568. [Google Scholar] [CrossRef]
- Lacey, J.H.; Crisp, A.H.; Kalucy, R.S.; Hartmann, M.; Chien, C. Study of EEG sleep characteristics in patients with anorexia nervosa before and after restoration of matched population mean weight consequent on ingestion of a “normal” diet. Postgrad. Med. J. 1976, 52, 45–49. [Google Scholar] [CrossRef][Green Version]
- Menculini, G.; Brufani, F.; Del Bello, V.; Moretti, P.; Tortorella, A. Circadian rhythms disruptions and eating disorders: Clinical impact and possible psychopathological correlates. Psychiatr. Danub. 2019, 31 (Suppl. S3), 497–502. [Google Scholar] [PubMed]
- Guirguis, W.R. Sleepwalking as a symptom of bulimia. Br. Med. J. 1986, 293, 587–588. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Asaad Abdou, T.; Esawy, H.I.; Abdel Razek Mohamed, G.; Hussein Ahmed, H.; Elhabiby, M.M.; Khalil, S.A.; El-Hawary, Y.A. Sleep profile in anorexia and bulimia nervosa female patients. Sleep Med. 2018, 48, 113–116. [Google Scholar] [CrossRef] [PubMed]
- Trace, S.E.; Thornton, L.M.; Runfola, C.D.; Lichtenstein, P.; Pedersen, N.L.; Bulik, C.M. Sleep problems are associated with binge eating in women. Int. J. Eat. Disord. 2012, 45, 695–703. [Google Scholar] [CrossRef] [PubMed]
- Ulman, T.F.; Von Holle, A.; Torgersen, L.; Stoltenberg, C.; Reichborn-Kjennerud, T.; Bulik, C.M. Sleep disturbances and binge eating disorder symptoms during and after pregnancy. Sleep 2012, 35, 1403–1411. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.R.; Jung, Y.C.; Shin, M.Y.; Namkoong, K.; Kim, J.K.; Lee, J.H. Sleep disturbance in women with eating disorder: Prevalence and clinical characteristics. Psychiatry Res. 2010, 176, 88–90. [Google Scholar] [CrossRef] [PubMed]
- Della Marca, G.; Farina, B.; Di Giannantonio, M.; De Risio, S.; Ciocca, A.; Mazza, M. Microstructure of sleep in eating disorders: Preliminary results. Eat. Weight. Disord. 2004, 9, 77–80. [Google Scholar] [CrossRef]
- Dippel, B.; Lauer, C.; Riemann, D. Sleep and dreams in eating disorders. Psychoter. Psychosom. 1987, 48, 165–169. [Google Scholar] [CrossRef]
- Di Matteo, A.; Bossi, E.; Amianto, F.; Leombruni, P.; Abbate, D.; de Dominicis, F.; Rambaudi, A.; Fiori, L.; Fassino, S. La qualità della vita nei sogni delle pazienti bulimarexiche. In La Qualità Della Vita. Percorsi Psicologici, Biomedici e Transculturali; Fasino, S., Leombruni, P., Rovera, G.G., Eds.; CSE: Torino, Piedmont, 2000; pp. 243–260. [Google Scholar]
- Brink, S.; Allan, J. Dreams of anorexic and bulimic woman: A research study. J. Ann. Psychol. 1992, 37, 275–297. [Google Scholar] [CrossRef]
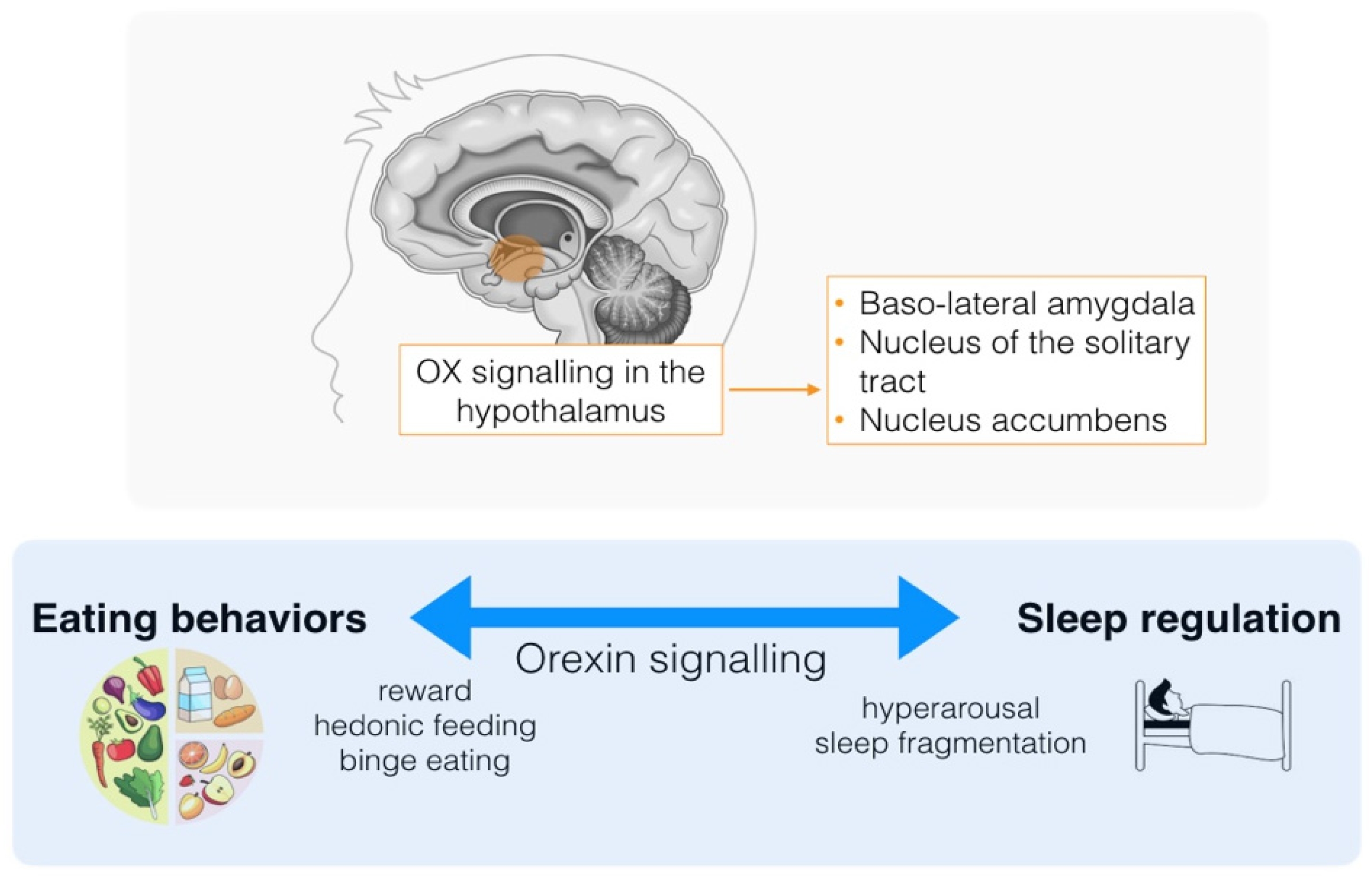
- Mehr, J.B.; Mitchison, D.; Bowrey, H.E.; James, M.H. Sleep dysregulation in binge eating disorder and “food addiction”: The orexin (hypocretin) system as a potential neurobiological link. Neuropsychopharmacology 2021, 46, 2051–2061. [Google Scholar] [CrossRef]
- Li, J.; Hu, Z.; de Lecea, L. The hypocretins/orexins: Integrators of multiple physiological functions. Br. J. Pharmacol. 2014, 171, 332–350. [Google Scholar] [CrossRef] [PubMed]
- Muehlan, C.; Vaillant, C.; Zenklusen, I.; Kraehenbuehl, S.; Dingemanse, J. Clinical pharmacology, efficacy, and safety of orexin receptor antagonists for the treatment of insomnia disorders. Expert Opin. Drug Metab. Toxicol. 2020, 16, 1063–1078. [Google Scholar] [CrossRef] [PubMed]
- Perez-Campos, E.; Mayoral, L.P.-C.; Andrade, G.M.; Mayoral, E.P.-C.; Huerta, T.H.; Canseco, S.P.; Canales, F.J.R.; Cabrera-Fuentes, H.A.; Cruz, M.M.; Santiago, A.D.P.; et al. Obesity subtypes, related biomarkers & heterogeneity. Indian J. Med. Res. 2020, 151, 11–21. [Google Scholar] [CrossRef]
- St-Onge, M.P.; Wolfe, S.; Sy, M.; Shechter, A.; Hirsch, J. Sleep restriction increases the neuronal response to unhealthy food in normal-weight individuals. Int. J. Obes. 2014, 38, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Taheri, S.; Lin, L.; Austin, D.; Young, T.; Mignot, E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004, 1, e62. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.L.; Lumeng, J.C.; LeBourgeois, M.K. Sleep patterns and obesity in childhood. Curr. Opin. Endocrinol. Diabetes Obes. 2015, 22, 41–47. [Google Scholar] [CrossRef]
- Meurling, I.J.; Shea, D.O.; Garvey, J.F. Obesity and sleep: A growing concern. Curr. Opin. Pulm. Med. 2019, 25, 602–608. [Google Scholar] [CrossRef]
- Vgontzas, A.N.; Papanicolaou, D.A.; Bixler, E.O.; Kales, A.; Tyson, K.; Chrousos, G.P. Elevation of plasma cytokines in disorders of excessive daytime sleepiness: Role of sleep disturbance and obesity. J. Clin. Endocrinol. Metab. 1997, 82, 1313–1316. [Google Scholar] [CrossRef]
- Vgontzas, A.N.; Bixler, E.O.; Chrousos, G.P. Obesity-related sleepiness and fatigue: The role of the stress system and cytokines. Ann. N Y Acad. Sci. 2006, 1083, 329–344. [Google Scholar] [CrossRef]
- Pace, M.; Falappa, M.; Freschi, A.; Balzani, E.; Berteotti, C.; Martire, V.L.; Kaveh, F.; Hovig, E.; Zoccoli, G.; Amici, R.; et al. Loss of Snord116 impacts lateral hypothalamus, sleep, and food-related behaviors. JCI Insight. 2020, 5, e137495. [Google Scholar] [CrossRef]
- Duis, J.; Pullen, L.C.; Picone, M.; Friedman, N.; Hawkins, S.; Sannar, E.; Pfalzer, A.C.; Shelton, A.R.; Singh, D.; Zee, P.C.; et al. Diagnosis and management of sleep disorders in Prader-Willi syndrome. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2022, 18, 1687–1696. [Google Scholar] [CrossRef] [PubMed]
- Vinai, P.; Cardetti, S.; Studt, S.; Carpegna, G.; Ferrato, N.; Vallauri, P.; Casey, H.; Vinai, L.; Vinai, P.; Strambi, L.F.; et al. Clinical validity of the descriptor “Presence of a belief that one must eat in order to get to sleep” in diagnosing the night eating syndrome. Appetite 2014, 75, 46–48. [Google Scholar] [CrossRef] [PubMed]
- Spaggiari, M.C.; Granella, F.; Parrino, L.; Marchesi, C.; Melli, I.; Terzano, M.G. Nocturnal eating syndrome in adults. Sleep 1994, 17, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Lundgren, J.D.; Allison, K.C.; O’Reardon, J.P.; Stunkard, A.J. A descriptive study of non-obese persons with night eating syndrome and a weight-matched comparison group. Eat. Behav. 2008, 9, 343–351. [Google Scholar] [CrossRef] [PubMed]
- O’Reardon, J.P.; Ringel, B.L.; Dinges, D.F.; Allison, K.C.; Rogers, N.L.; Martino, N.S.; Stunkard, A.J. Circadian eating and sleeping patterns in the night eating syndrome. Obes. Res. 2004, 12, 1789–1796. [Google Scholar] [CrossRef]
- Yoshida, J.; Eguchi, E.; Nagaoka, K.; Ito, T.; Ogino, K. Association of night eating habits with metabolic syndrome and its components: A longitudinal study. BMC Public Health 2018, 18, 1366. [Google Scholar] [CrossRef]
- Wal, J.S.V. The Treatment of Night Eating Syndrome: A Review and Theoretical Model. Curr. Obes. Rep. 2014, 3, 137–144. [Google Scholar] [CrossRef]
- O’Reardon, J.P.; Allison, K.C.; Martino, N.S.; Lundgren, J.D.; Heo, M.; Stunkard, A.J. A randomized, placebo-controlled trial of sertraline in the treatment of night eating syndrome. Am. J. Psychiatry 2006, 163, 893–898. [Google Scholar] [CrossRef]
- Vander Wal, J.S.; Gang, C.H.; Griffing, G.T.; Gadde, K.M. Escitalopram for treatment of night eating syndrome: A 12-week, randomized, placebo-controlled trial. J. Clin. Psychopharmacol. 2012, 32, 341–345. [Google Scholar] [CrossRef]
- Friedman, S.; Even, C.; Dardennes, R.; Guelfi, J.D. Light therapy, obesity, and night-eating syndrome. Am. J. Psychiatry 2002, 159, 875–876. [Google Scholar] [CrossRef]
- Zapp, A.A.; Fischer, E.C.; Deuschle, M. The effect of agomelatine and melatonin on sleep-related eating: A case report. J. Med. Case Rep. 2017, 11, 275. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Winkelman, J.W. Treatment of nocturnal eating syndrome and sleep-related eating disorder with topiramate. Sleep Med. 2003, 4, 243–246. [Google Scholar] [CrossRef]
- Charalambous, A.; Giannakopoulou, M.; Bozas, E.; Paikousis, L. A randomized controlled trial for the effectiveness of progressive muscle relaxation and guided imagery as anxiety reducing interventions in breast and prostate cancer patients undergoing chemotherapy. Evid.-Based Complement. Altern. Med. 2015, 2015, 270876. [Google Scholar] [CrossRef]
- McCune, A.M.; Lundgren, J.D. Bright light therapy for the treatment of night eating syndrome: A pilot study. Psychiatry Res. 2015, 229, 577–579. [Google Scholar] [CrossRef] [PubMed]
- Allison, K.C.; Lundgren, J.D.; Moore, R.H.; O’reardon, J.P.; Stunkard, A.J. Cognitive behavior therapy for night eating syndrome: A pilot study. Am. J. Psychother. 2010, 64, 91–106. [Google Scholar] [CrossRef] [PubMed]
- Costa, M.B.; Melnik, T. Effectiveness of psychosocial interventions in eating disorders: An overview of Cochrane systematic reviews. Einstein 2016, 14, 235–277. [Google Scholar] [CrossRef] [PubMed]
- Thorpy, M.J. Classification of sleep disorders. Neurotherapeutics 2012, 9, 687–701. [Google Scholar] [CrossRef]
- Hening, W.A.; Walters, A.S.; Wagner, M.; Rosen, R.; Chen, V.; Kim, S.; Shah, M.; Thai, O. Circadian rhythm of motor restlessness and sensory symptoms in the idiopathic restless legs syndrome. Sleep 1999, 22, 901–912. [Google Scholar] [CrossRef]
- Trenkwalder, C.; Hening, W.A.; Walters, A.S.; Campbell, S.S.; Rahman, K.; Chokroverty, S. Circadian rhythm of periodic limb movements and sensory symptoms of restless legs syndrome. Mov. Disord. 1999, 14, 102–110. [Google Scholar] [CrossRef]
- Sforza, E.; Jouny, C.; Ibanez, V. Time course of arousal response during periodic leg movements in patients with periodic leg movements and restless legs syndrome. Clin. Neurophysiol. 2003, 114, 1116–1124. [Google Scholar] [CrossRef] [PubMed]
- Geliebter, A.; McOuatt, H.; Tetreault, C.B.; Kordunova, D.; Rice, K.; Zammit, G.; Gluck, M. Is night eating syndrome associated with obstructive sleep apnea, BMI, and depressed mood in patients from a sleep laboratory study? Eat. Behav. 2016, 23, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Olbrich, K.; Mühlhans, B.; Allison, K.C.; Hahn, E.G.; Schahin, S.P.; de Zwaan, M. Night eating, binge eating and related features in patients with obstructive sleep apnea syndrome. Eur. Eat. Disord. Review 2009, 17, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Nirenberg, M.J.; Waters, C. Compulsive eating and weight gain related to dopamine agonist use. Mov. Disord. 2006, 21, 524–529. [Google Scholar] [CrossRef] [PubMed]
- Paquet, V.; Strul, J.; Servais, L.; Pelc, I.; Fossion, P. Sleep-related eating disorder induced by olanzapine. J. Clin. Psychiatry 2002, 63, 597. [Google Scholar] [CrossRef] [PubMed]
- Wallace, D.M.; Maze, T.; Shafazand, S. Sodium oxybate-induced sleep driving and sleep-related eating disorder. J. Clin. Sleep Med. 2011, 7, 310–311. [Google Scholar] [CrossRef]
- Schenck, C.H.; Connoy, D.A.; Castellanos, M.; Johnson, B.; Werner, R.; Willis, L.; Bornemann, M.A.; Mahowald, M.W. Zolpidem-induced Sleep-Related Eating Disorder (SRED) in 19 patients. Sleep 2005, 28, a259. [Google Scholar]
- Winkelman, J.W. Clinical and polysomnographic features of sleep-related eating disorder. J. Clin. Psychiatry 1998, 59, 14–19. [Google Scholar] [CrossRef]
- Sanger, D.J. The pharmacology and mechanisms of action of new generation, non-benzodiazepine hypnotic agents. CNS Drugs 2004, 18 (Suppl. S1), 9. [Google Scholar] [CrossRef]
- Greenblatt, D.J.; Roth, T. Zolpidem for insomnia. Expert Opin. Pharmacother. 2012, 13, 879–893. [Google Scholar] [CrossRef]
- Uygun, D.S.; Ye, Z.; Zecharia, A.Y.; Harding, E.C.; Yu, X.; Yustos, R.; Vyssotski, A.L.; Brickley, S.G.; Franks, N.P.; Wisden, W. Bottom-Up versus Top-Down Induction of Sleep by Zolpidem Acting on Histaminergic and Neocortex Neurons. J. Neurosci. 2016, 36, 11171–11184. [Google Scholar] [CrossRef]
- Ho, T.; Jimenez, A.; Sanchez, I.; Seeger, C.; Joseph, M. Sleep-related eating disorder associated with zolpidem: Cases compiled from a literature review. Sleep Med. X 2020, 2, 100019. [Google Scholar] [CrossRef] [PubMed]
- Kaur, H.; Jahngir, M.U.; Siddiqui, J.H. Sleep-related Eating Disorder in a Patient with Parkinson’s Disease. Cureus 2018, 10, e3345. [Google Scholar] [CrossRef] [PubMed]
- Provini, F.; Albani, F.; Vetrugno, R.; Vignatelli, L.; Lombardi, C.; Plazzi, G.; Montagna, P. A pilot double-blind placebo-controlled trial of low-dose pramipexole in sleep-related eating disorder. Eur. J. Neurol. 2005, 12, 432–436. [Google Scholar] [CrossRef] [PubMed]
- Chopra, A.; Patel, R.S.; Baliga, N.; Narahari, A.; Das, P. Sleepwalking and sleep-related eating associated with atypical antipsychotic medications: Case series and systematic review of literature. Gen. Hosp. Psychiatry 2020, 65, 74–81. [Google Scholar] [CrossRef]
- Jeong, J.H.; Bahk, W.M. Sleep-related eating disorder associated with mirtazapine. J. Clin. Psychopharmacol. 2014, 34, 752–753. [Google Scholar] [CrossRef]
- Sheng, Z.; Santiago, A.M.; Thomas, M.P.; Routh, V.H. Metabolic regulation of lateral hypothalamic glucose-inhibited orexin neurons may influence midbrain reward neurocircuitry. Mol. Cell. Neurosci. 2014, 62, 30–41. [Google Scholar] [CrossRef]
- Schenck, C.H.; Mahowald, M.W. Combined bupropion-levodopa-trazodone therapy of sleep-related eating and sleep disruption in two adults with chemical dependency. Sleep 2000, 23, 587–588. [Google Scholar]
- Winkelman, J.W.; Wipper, B.; Purks, J.; Mei, L.; Schoerning, L. Topiramate reduces nocturnal eating in sleep-related eating disorder. Sleep 2020, 43, zsaa060. [Google Scholar] [CrossRef]
- Berridge, K.C.; Ho, C.Y.; Richard, J.M.; DiFeliceantonio, A.G. The tempted brain eats: Pleasure and desire circuits in obesity and eating disorders. Brain Res. 2010, 1350, 43–64. [Google Scholar] [CrossRef]
- Bayard, S.; Dauvilliers, Y.A. Reward-based behaviors and emotional processing in humans with narcolepsy-cataplexy. Front. Behav. Neurosci. 2013, 7, 50. [Google Scholar] [CrossRef]
- Truzzi, G.M.; Cremaschi, R.C.; Coelho, F.M. Human hypocretin-deficient narcolepsy-aberrant food choice due to impaired taste? Sleep Sci. 2017, 10, 78–79. [Google Scholar] [CrossRef] [PubMed]
- BaHammam, A.S.; Alnakshabandi, K.; Pandi-Perumal, S.R. Neuropsychiatric Correlates of Narcolepsy. Curr. Psychiatry Rep. 2020, 22, 36. [Google Scholar] [CrossRef]
- Kok, S.W.; Overeem, S.; Visscher, T.L.; Lammers, G.J.; Seidell, J.C.; Pijl, H.; Meinders, A.E. Hypocretin deficiency in narcoleptic humans is associated with abdominal obesity. Obes. Res. 2003, 11, 1147–1154. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, S.; Moosaie, F.; Saghazadeh, A.; Mahmoudi, M.; Rezaei, N. Metabolic profile in patients with narcolepsy: A systematic review and meta-analysis. Sleep Med. 2021, 81, 268–284. [Google Scholar] [CrossRef] [PubMed]
- Van Holst, R.J.; Van Der Cruijsen, L.; Van Mierlo, P.; Lammers, G.J.; Cools, R.; Overeem, S.; Aarts, E. Aberrant food choices after satiation in human orexin-deficient narcolepsy type 1. Sleep 2016, 39, 1951–1959. [Google Scholar] [CrossRef]
- Palaia, V.; Poli, F.; Pizza, F.; Antelmi, E.; Franceschini, C.; Moghadam, K.K.; Provini, F.; Pagotto, U.; Montagna, P.; Schenck, C.H.; et al. Narcolepsy with cataplexy associated with nocturnal compulsive behaviors: A case-control study. Sleep 2011, 34, 1365–1371. [Google Scholar] [CrossRef]
- Scolnick, B. Antihistamine agents and pitolisant might be useful for anorexia nervosa. Med. Hypotheses 2019, 132, 109342. [Google Scholar] [CrossRef]
- Critchley, M. Periodic hypersomnia and megaphagia in adolescent males. Brain 1962, 85, 627–657. [Google Scholar] [CrossRef]
- Gadoth, N.; Oksenberg, A. Kleine-Levin syndrome: An update and mini-review. Brain Dev. 2017, 39, 665–671. [Google Scholar] [CrossRef]
- Ambati, A.; Hillary, R.; Leu-Semenescu, S.; Ollila, H.M.; Lin, L.; During, E.H.; Farber, N.; Rico, T.J.; Faraco, J.; Leary, E.; et al. Kleine-Levin syndrome is associated with birth difficulties and genetic variants in the TRANK1 gene loci. Proc. Natl. Acad. Sci. USA 2021, 118, e2005753118. [Google Scholar] [CrossRef]
- de Oliviera, M.M.; Conti, C.; Prado, G.F. Pharmacological treatment for Kleine-Levin syndrome. Cochrane Database Syst. Rev. 2016, 2016, CD006685. [Google Scholar] [CrossRef] [PubMed]
- Dauvilliers, Y.; Mayer, G.; Lecendreux, M.; Neidhart, E.; Peraita-Adrados, R.; Sonka, K.; Billiard, M.; Tafti, M. Kleine-Levin syndrome: An autoimmune hypothesis based on clinical and genetic analyses. Neurology 2002, 59, 1739–1745. [Google Scholar] [CrossRef] [PubMed]
- Melpignano, A.; Milioli, G.; Bertelè, A.; Vaudano, A.E.; Ghetti, C.; Parrino, L.; Ruffini, L. Kleine-Levin syndrome: The contribution of PET scan and hydrogen breath test for small intestinal bacterial overgrowth. Sleep Med. 2018, 46, 95–97. [Google Scholar] [CrossRef] [PubMed]
- Arnulf, I.; Groos, E.; Dodet, P. Kleine-Levin syndrome: A neuropsychiatric disorder. Rev. Neurol. 2018, 174, 216–227. [Google Scholar] [CrossRef] [PubMed]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Katz, E.S.; Kheirandish-Gozal, L.; et al. National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health 2015, 1, 40–43. [Google Scholar] [CrossRef]
- Matricciani, L.; Olds, T.; Petkov, J. In search of lost sleep: Secular trends in the sleep time of school-aged children and adolescents. Sleep Med. Reviews 2012, 16, 203–211. [Google Scholar] [CrossRef]
- Chang, A.M.; Aeschbach, D.; Duffy, J.F.; Czeisler, C.A. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc. Natl. Acad. Sci. USA 2015, 112, 1232–1237. [Google Scholar] [CrossRef]
- Miller, M.A.; Bates, S.; Ji, C.; Cappuccio, F.P. Systematic review and meta-analyses of the relationship between short sleep and incidence of obesity and effectiveness of sleep interventions on weight gain in preschool children. Obes. Rev. 2021, 22, e13113. [Google Scholar] [CrossRef]
- Boege, H.L.; Bhatti, M.Z.; St-Onge, M.P. Circadian rhythms and meal timing: Impact on energy balance and body weight. Curr. Opin. Biotechnol. 2020, 70, 1–6. [Google Scholar] [CrossRef]
- Kandeger, A.; Selvi, Y.; Tanyer, D.K. The effects of individual circadian rhythm differences on insomnia, impulsivity, and food addiction. Eat. Weight. Disord. 2019, 24, 47–55. [Google Scholar] [CrossRef]
- Meng, H.; Zhu, L.; Kord-Varkaneh, H.; Santos, H.O.; Tinsley, G.M.; Fu, P. Effects of intermittent fasting and energy-restricted diets on lipid profile: A systematic review and meta-analysis. Nutrition 2020, 77, 110801. [Google Scholar] [CrossRef] [PubMed]
- McEown, K.; Takata, Y.; Cherasse, Y.; Nagata, N.; Aritake, K.; Lazarus, M. Chemogenetic inhibition of the medial prefrontal cortex reverses the effects of REM sleep loss on sucrose consumption. Elife 2016, 5, e20269. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Wang, Y.; Cai, L.; Li, Y.; Chen, B.; Dong, Y.; Huang, Y.H. Prefrontal Cortex to Accumbens Projections in Sleep Regulation of Reward. J. Neurosci. 2016, 36, 7897–7910. [Google Scholar] [CrossRef] [PubMed]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef] [PubMed]
- Arab, A.; Karimi, E.; Garaulet, M.; Scheer, F.A. Social jetlag and dietary intake: A systematic review. Sleep Med. Rev. 2023, 71, 101820. [Google Scholar] [CrossRef]
- Haupt, S.; Eckstein, M.L.; Wolf, A.; Zimmer, R.T.; Wachsmuth, N.B.; Moser, O. Eat, Train, Sleep-Retreat? Hormonal Interactions of Intermittent Fasting, Exercise and Circadian Rhythm. Biomolecules 2021, 11, 516. [Google Scholar] [CrossRef]
- Fagnani, C.; Toccaceli, V.; Delfino, D.; Medda, E.; Stazi, M.A. Determinanti del comportamento alimentare: Il contributo degli studi sui gemelli. Epidemiol. Prev. 2015, 39, 350–359. [Google Scholar]
- Palanza, P.; Parmigiani, S. Why human evolution should be a basic science for medicine and psychology students. J. Anthropol. Sci. 2016, 94, 183–192. [Google Scholar] [CrossRef]
- Fulling, C.; Dinan, T.G.; Cryan, J.F. Gut microbe to brain signaling: What happens in Vagus. Neuron 2019, 101, 998–1002. [Google Scholar] [CrossRef]
- Furness, J.B. The enteric nervous system and neurogastroenterology. Nat. Rev. Gastroenterol. Hepatol. 2012, 9, 286–294. [Google Scholar] [CrossRef]
- Fung, T.C.; Olson, C.A.; Hsiao, E.Y. Interactions between the microbiota, immune and nervous systems in health and disease. Nat. Neurosci. 2017, 20, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Juszczak, H.M.; Cope, E.K.; Goldberg, A.N. The Microbiome in Obstructive Sleep Apnea. Sleep 2021, 44, zsab061. [Google Scholar] [CrossRef]
- Han, S.; Cai, L.; Chen, P.; Kuang, W. A study of the correlation between stroke and gut microbiota over the last 20years: A bibliometric analysis. Front. Microbiol. 2023, 14, 1191758. [Google Scholar] [CrossRef] [PubMed]
- Camara-Lemarroy, C.R.; Metz, L.M.; Yong, V.W. Focus on the gut-brain axis: Multiple sclerosis, the intestinal barrier and the microbiome. World J. Gastroenterol. 2018, 24, 4217–4223. [Google Scholar] [CrossRef] [PubMed]
- Carloni, S.; Rescigno, M. The gut-brain vascular axis in neuroinflammation. Semin. Immunol. 2023, 69, 101802. [Google Scholar] [CrossRef]
- Schmitt, V.; Masanetz, R.K.; Weidenfeller, M.; Ebbinghaus, L.S.; Süß, P.; Rosshart, S.P.; von Hörsten, S.; Zunke, F.; Winkler, J.; Xiang, W. Gut-to-brain spreading of pathology in synucleinopathies: A focus on molecular signalling mediators. Behav Brain Res. 2023, 452, 114574. [Google Scholar] [CrossRef]
- Huang, B.; Chau, S.W.H.; Liu, Y.; Chan, J.W.Y.; Wang, J.; Ma, S.L.; Zhang, J.; Chan, P.K.S.; Yeoh, Y.K.; Chen, Z.; et al. Gut microbiome dysbiosis across early Parkinson’s disease, REM sleep behavior disorder and their first-degree relatives. Nat. Commun. 2023, 14, 2501. [Google Scholar] [CrossRef]
- Flor-Alemany, M.; Nestares, T.; Alemany-Arrebola, I.; Marín-Jiménez, N.; Borges-Cosic, M.; Aparicio, V.A. Influence of Dietary Habits and Mediterranean Diet Adherence on Sleep Quality during Pregnancy. The GESTAFIT Project. Nutrients 2020, 12, 3569. [Google Scholar] [CrossRef]
- Isaura, E.R.; Chen, Y.-C.; Su, H.-Y.; Yang, S.-H. The Relationship between Food Security Status and Sleep Disturbance among Adults: A Cross-Sectional Study in an Indonesian Population. Nutrients 2020, 12, 3411. [Google Scholar] [CrossRef]
- Li, Y.; Zhang, B.; Zhou, Y.; Wang, D.; Liu, X.; Li, L.; Wang, T.; Zhang, Y.; Jiang, M.; Tang, H.; et al. Gut Microbiota Changes and Their Relationship with Inflammation in Patients with Acute and Chronic Insomnia. Nat. Sci. Sleep 2020, 12, 895–905. [Google Scholar] [CrossRef]
- Fetissov, S.O.; Hökfelt, T. On the origin of eating disorders: Altered signaling between gut microbiota, adaptive immunity and the brain melanocortin system regulating feeding behavior. Curr. Opin. Pharmacol. 2019, 48, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Fetissov, S.O.; Hamze Sinno, M.; Coquerel, Q.; Do Rego, J.C.; Coëffier, M.; Gilbert, D.; Hökfelt, T.; Déchelotte, P. Emerging role of autoantibodies against appetite-regulating neuropeptides in eating disorders. Nutrition 2008, 24, 854–859. [Google Scholar] [CrossRef]
- Zeigler, Z. COVID-19 Self-quarantine and Weight Gain Risk Factors in Adults. Curr. Obes. Rep. 2021, 10, 423–433. [Google Scholar] [CrossRef] [PubMed]
- Lotti, S.; Dinu, M.; Pagliai, G.; Giangrandi, I.; Colombini, B.; Sofi, F. Adherence to the Mediterranean diet increased during the COVID-19 lockdown in Italy: Results from the web-based Medi-Lite questionnaire. Int. J. Food Sci. Nutr. 2022, 73, 650–656. [Google Scholar] [CrossRef] [PubMed]
- Barrea, L.; Pugliese, G.; Framondi, L.; Di Matteo, R.; Laudisio, D.; Savastano, S.; Colao, A.; Muscogiuri, G. Does SARS-CoV-2 threaten our dreams? Effect of quarantine on sleep quality and body mass index. J. Transl. Med. 2020, 18, 318. [Google Scholar] [CrossRef]
- Bosi Bağcı, T.A.; Kanadıkırık, A.; Somyürek, E.; Gerçek, G.; Tanrıkulu, H.B.; Öntaş, E.; Uzun, S. Impact of COVID-19 on eating habits, sleeping behaviour and physical activity status of final-year medical students in Ankara, Turkey. Public Health Nutr. 2021, 24, 6369–6376. [Google Scholar] [CrossRef]
- Grant, F.; Scalvedi, M.L.; Scognamiglio, U.; Turrini, A.; Rossi, L. Eating Habits during the COVID-19 Lockdown in Italy: The Nutritional and Lifestyle Side Effects of the Pandemic. Nutrients 2021, 13, 2279. [Google Scholar] [CrossRef]
- Prete, M.; Luzzetti, A.; Augustin, L.; Porciello, G.; Montagnese, C.; Calabrese, I.; Ballarin, G.; Coluccia, S.; Patel, L.; Vitale, S.; et al. Changes in Lifestyle and Dietary Habits during COVID-19 Lockdown in Italy: Results of an Online Survey. Nutrients 2021, 13, 1923. [Google Scholar] [CrossRef]
- Angelidi, A.M.; Kokkinos, A.; Katechaki, E.; Ros, E.; Mantzoros, C.S. Mediterranean diet as a nutritional approach for COVID-19. Metab. Clin. Exp. 2021, 114, 154407. [Google Scholar] [CrossRef]
- Georgoulis, M.; Yiannakouris, N.; Tenta, R.; Fragopoulou, E.; Kechribari, I.; Lamprou, K.; Perraki, E.; Vagiakis, E.; Kontogianni, M.D. A weight-loss Mediterranean diet/lifestyle intervention ameliorates inflammation and oxidative stress in patients with obstructive sleep apnea: Results of the “MIMOSA” randomized clinical trial. Eur. J. Nutr. 2021, 60, 3799–3810. [Google Scholar] [CrossRef]
- Gupta, C.C.; Irwin, C.; Vincent, G.E.; Khalesi, S. The Relationship Between Diet and Sleep in Older Adults: A Narrative Review. Curr. Nutr. Rep. 2021, 10, 166–178. [Google Scholar] [CrossRef] [PubMed]
- Godos, J.; Grosso, G.; Castellano, S.; Galvano, F.; Caraci, F.; Ferri, R. Association between diet and sleep quality: A systematic review. Sleep Med. Rev. 2021, 57, 101430. [Google Scholar] [CrossRef] [PubMed]
- Dibner, C.; Schibler, U.; Albrecht, U. The mammalian circadian timing system: Organization and coordination of central and peripheral clocks. Annu. Rev. Physiol. 2010, 72, 517–549. [Google Scholar] [CrossRef] [PubMed]
- Olejniczak, I.; Pilorz, V.; Oster, H. Circle(s) of Life: The Circadian Clock from Birth to Death. Biology 2023, 12, 383. [Google Scholar] [CrossRef] [PubMed]
- BaHammam, A.S.; Alghannam, A.F.; Aljaloud, K.S.; Aljuraiban, G.S.; AlMarzooqi, M.A.; Dobia, A.M.; Alothman, S.A.; Aljuhani, O.; Alfawaz, R.A. Joint consensus statement of the Saudi Public Health Authority on the recommended amount of physical activity, sedentary behavior, and sleep duration for healthy Saudis: Background, methodology, and discussion. Ann. Thorac. Med. 2021, 16, 225–238. [Google Scholar] [CrossRef] [PubMed]
- BaHammam, A.S.; Pirzada, A. Timing Matters: The Interplay between Early Mealtime, Circadian Rhythms, Gene Expression, Circadian Hormones, and Metabolism-A Narrative Review. Clocks Sleep 2023, 5, 507–535. [Google Scholar] [CrossRef]
- Skeer, M.R.; Yantsides, K.E.; Eliasziw, M.; Tracy, M.R.; Carlton-Smith, A.R.; Spirito, A. Sociodemographic characteristics associated with frequency and duration of eating family meals: A cross-sectional analysis. SpringerPlus 2016, 5, 2062. [Google Scholar] [CrossRef]
- Yang, Y.; Li, S.X.; Zhang, Y.; Wang, F.; Jiang, D.J.; Wang, S.J.; Cao, P.; Gong, Q.H. Chronotype is associated with eating behaviors, physical activity and overweight in school-aged children. Nutr. J. 2023, 22, 50. [Google Scholar] [CrossRef]
- Godos, J.; Castellano, S.; Ferri, R.; Caraci, F.; Lanza, G.; Scazzina, F.; Alanazi, A.M.; Marx, W.; Galvano, F.; Grosso, G. Mediterranean diet and chronotype: Data from Italian adults and systematic review of observational studies. Exp. Gerontol. 2023, 181, 112284. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mutti, C.; Malagutti, G.; Maraglino, V.; Misirocchi, F.; Zilioli, A.; Rausa, F.; Pizzarotti, S.; Spallazzi, M.; Rosenzweig, I.; Parrino, L. Sleep Pathologies and Eating Disorders: A Crossroad for Neurology, Psychiatry and Nutrition. Nutrients 2023, 15, 4488. https://doi.org/10.3390/nu15204488
Mutti C, Malagutti G, Maraglino V, Misirocchi F, Zilioli A, Rausa F, Pizzarotti S, Spallazzi M, Rosenzweig I, Parrino L. Sleep Pathologies and Eating Disorders: A Crossroad for Neurology, Psychiatry and Nutrition. Nutrients. 2023; 15(20):4488. https://doi.org/10.3390/nu15204488
Chicago/Turabian StyleMutti, Carlotta, Giulia Malagutti, Valentina Maraglino, Francesco Misirocchi, Alessandro Zilioli, Francesco Rausa, Silvia Pizzarotti, Marco Spallazzi, Ivana Rosenzweig, and Liborio Parrino. 2023. "Sleep Pathologies and Eating Disorders: A Crossroad for Neurology, Psychiatry and Nutrition" Nutrients 15, no. 20: 4488. https://doi.org/10.3390/nu15204488
APA StyleMutti, C., Malagutti, G., Maraglino, V., Misirocchi, F., Zilioli, A., Rausa, F., Pizzarotti, S., Spallazzi, M., Rosenzweig, I., & Parrino, L. (2023). Sleep Pathologies and Eating Disorders: A Crossroad for Neurology, Psychiatry and Nutrition. Nutrients, 15(20), 4488. https://doi.org/10.3390/nu15204488





