Chronic Illness, Nutritional Status, and Factors Associated with Malnutrition among Various Age Groups Residing in Urban Areas of Telangana and Rural Areas of Andhra Pradesh
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Variables
2.3. Ethics Approval and Consent
2.4. Statistical Analysis
Mixed-Effect Logistic Regression
3. Results
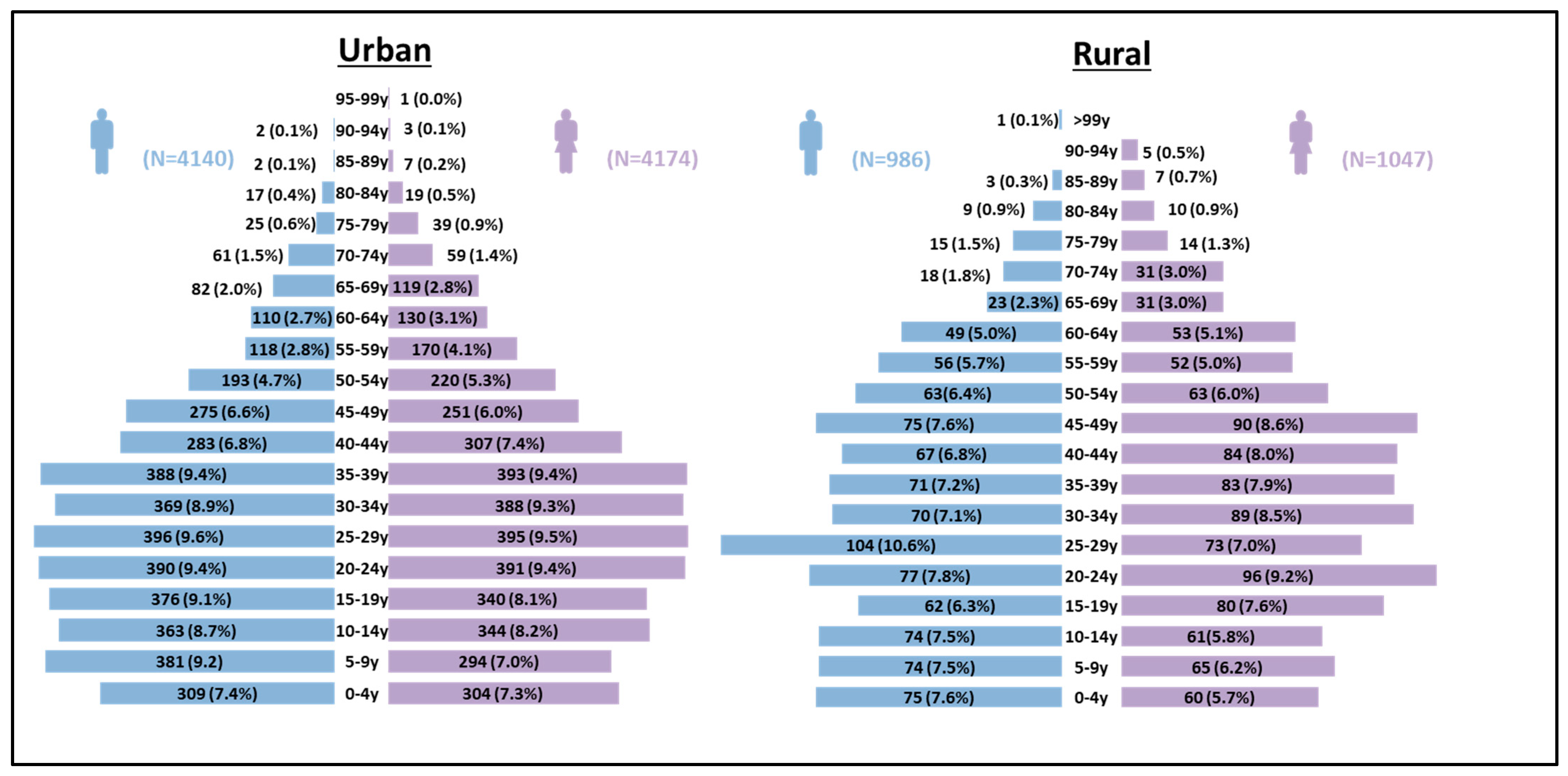
3.1. General Characteristics of the Respondents
3.2. Malnutrition Status
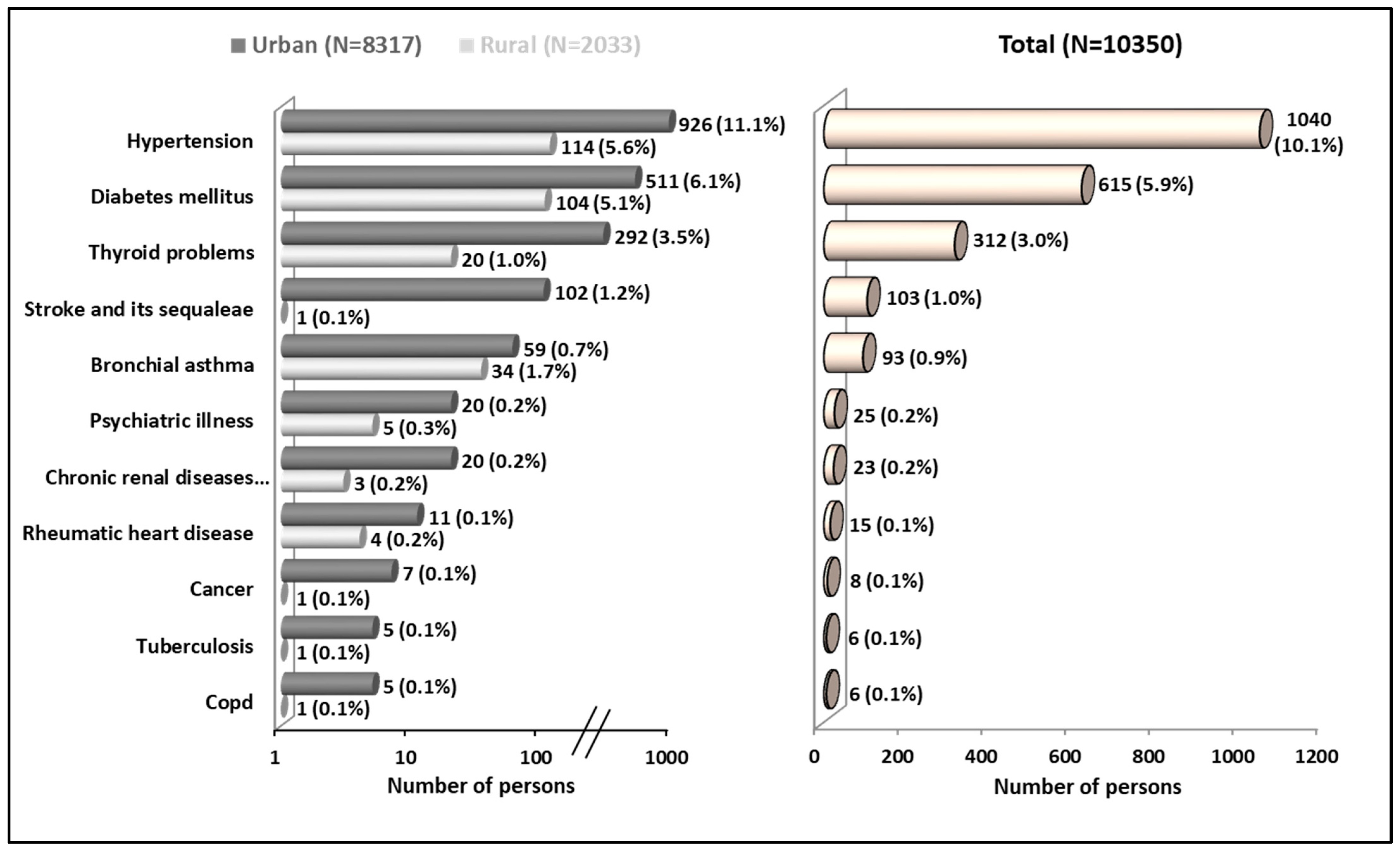
3.3. Chronic Illness among Study Participants
3.4. Factors Associated with Stunting among Under-Five Children
3.5. Factors Associated with Thinness among Adolescents
3.6. Factors Associated with Malnutrition among Adults
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; De Onis, M.; Ezzati, M.; Grantham-Mcgregor, S.; Katz, J.; Martorell, R.; et al. Maternal and Child Undernutrition and Overweight in Low-Income and Middle-Income Countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef] [PubMed]
- Victora, C.G.; Adair, L.; Fall, C.; Hallal, P.C.; Martorell, R.; Richter, L.; Sachdev, H.S. Maternal and Child Undernutrition: Consequences for Adult Health and Human Capital. Lancet 2008, 371, 340–357. [Google Scholar] [CrossRef] [PubMed]
- Independent Expert Group of the Global Nutrition Report. Action on Equity to End Malnutrition; Global Nutrition Report; Development Initiatives Poverty Research Ltd.: Bristol, UK, 2020; ISBN 9780896295643. [Google Scholar]
- Bhurosy, T.; Jeewon, R. Overweight and Obesity Epidemic in Developing Countries: A Problem with Diet, Physical Activity, or Socioeconomic Status? Sci. World J. 2014, 2014, 964236. [Google Scholar] [CrossRef]
- Abdullah, A. The Double Burden of Undernutrition and Overnutrition in Developing Countries: An Update. Curr. Obes. Rep. 2015, 4, 337–349. [Google Scholar] [CrossRef]
- Caballero, B. The Global Epidemic of Obesity: An Overview. Epidemiol. Rev. 2007, 29, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Letamo, G. Dual Burden of Underweight and Overweight/Obesity among Adults in Botswana: Prevalence, Trends and Sociodemographic Correlates: A Cross-Sectional Survey. BMJ Open 2020, 10, e038614. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Kapil, U.; Khandelwal, R.; Khenduja, P.; Sareen, N.; Pandey, R.M.; Upadhyay, A.D. Prevalence and Risk Factors of Underweight, Overweight and Obesity among a Geriatric Population Living in a High-Altitude Region of Rural Uttarakhand, India. Public Health Nutr. 2018, 21, 1904–1911. [Google Scholar] [CrossRef]
- GBD 2015 Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef]
- Agrawal, P.; Gupta, K.; Mishra, V.; Agrawal, S. Effects of Sedentary Lifestyle and Dietary Habits on Body Mass Index Change among Adult Women in India: Findings from a Follow-Up Study. Ecol. Food Nutr. 2013, 52, 387–406. [Google Scholar] [CrossRef]
- Fact Sheets-Malnutrition. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 9 August 2023).
- Stanaway, J.D.; Afshin, A.; Gakidou, E.; Lim, S.S.; Abate, D.; Abate, K.H.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; et al. Global, Regional, and National Comparative Risk Assessment of 84 Behavioural, Environmental and Occupational, and Metabolic Risks or Clusters of Risks for 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Stu. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health Effects of Dietary Risks in 195 Countries, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [PubMed]
- Cawley, J.; Meyerhoefer, C. The Medical Care Costs of Obesity: An Instrumental Variables Approach. J. Health Econ. 2012, 31, 219–230. [Google Scholar] [CrossRef] [PubMed]
- Daniels, S.R. Complications of Obesity in Children and Adolescents. Int. J. Obes. 2009, 33, S60–S65. [Google Scholar] [CrossRef]
- Reilly, J.J.; Methven, E.; McDowell, Z.C.; Hacking, B.; Alexander, D.; Stewart, L.; Kelnar, C.J.H. Health Consequences of Obesity. Arch. Dis. Child. 2003, 88, 748–752. [Google Scholar] [CrossRef] [PubMed]
- Razak, F.; Corsi, D.J.; Slutsky, A.S.; Kurpad, A.; Berkman, L.; Laupacis, A.; Subramanian, S.V. Prevalence of Body Mass Index Lower Than 16 Among Women in Low- and Middle-Income Countries. JAMA 2015, 314, 2164–2171. [Google Scholar] [CrossRef] [PubMed]
- Di Cesare, M.; Bentham, J.; Stevens, G.A.; Zhou, B.; Danaei, G.; Lu, Y.; Bixby, H.; Cowan, M.J.; Riley, L.M.; Hajifathalian, K.; et al. Trends in Adult Body-Mass Index in 200 Countries from 1975 to 2014: A Pooled Analysis of 1698 Population-Based Measurement Studies with 19.2 Million Participants. Lancet 2016, 387, 1377–1396. [Google Scholar] [CrossRef]
- International Institute for Population Sciences. NFSH-5 Compendium of Fact Sheets India and 14 States/UTs (Phase-11); International Institute for Population Sciences: Mumbai, India, 2021; pp. 1–116. [Google Scholar]
- MacMahon, S.; Baigent, C.; Duffy, S.; Rodgers, A.; Tominaga, S.; Chambless, L.; De Backer, G.; De Bacquer, D.; Kornitzer, M.; Whincup, P.; et al. Body-Mass Index and Cause-Specific Mortality in 900,000 Adults: Collaborative Analyses of 57 Prospective Studies. Lancet 2009, 373, 1083–1096. [Google Scholar] [CrossRef]
- Prabhakaran, D.; Jeemon, P.; Sharma, M.; Roth, G.A.; Johnson, C.; Harikrishnan, S.; Gupta, R.; Pandian, J.D.; Naik, N.; Roy, A.; et al. The Changing Patterns of Cardiovascular Diseases and Their Risk Factors in the States of India: The Global Burden of Disease Study 1990–2016. Lancet Glob. Health 2018, 6, e1339–e1351. [Google Scholar] [CrossRef] [PubMed]
- Hossain, P.; Kawar, B.; El Nahas, M. Obesity and Diabetes in the Developing World—A Growing Challenge. N. Engl. J. Med. 2007, 356, 213–215. [Google Scholar] [CrossRef]
- Arokiasamy, P.; Uttamacharya, U.; Jain, K.; Biritwum, R.B.; Yawson, A.E.; Wu, F.; Guo, Y.; Maximova, T.; Espinoza, B.M.; Salinas Rodríguez, A.; et al. The Impact of Multimorbidity on Adult Physical and Mental Health in Low- and Middle-Income Countries: What Does the Study on Global Ageing and Adult Health (SAGE) Reveal? BMC Med. 2015, 13, 178. [Google Scholar] [CrossRef]
- Agborsangaya, C.B.; Ngwakongnwi, E.; Lahtinen, M.; Cooke, T.; Johnson, J.A. Multimorbidity Prevalence in the General Population: The Role of Obesity in Chronic Disease Clustering. BMC Public Health 2013, 13, 1161. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, K.F.; Su, Y.P.; Gretebeck, R.J.; Black, D.R.; Badylak, S.F. Body Mass Index and Disability in Adulthood: A 20-Year Panel Study. Am. J. Public Health 2002, 92, 834–840. [Google Scholar] [CrossRef]
- Selvamani, Y.; Singh, P. Socioeconomic Patterns of Underweight and Its Association with Self-Rated Health, Cognition and Quality of Life among Older Adults in India. PLoS ONE 2018, 13, e0193979. [Google Scholar] [CrossRef]
- Pednekar, M.S.; Hakama, M.; Hebert, J.R.; Gupta, P.C. Association of Body Mass Index with All-Cause and Cause-Specific Mortality: Findings from a Prospective Cohort Study in Mumbai (Bombay), India. Int. J. Epidemiol. 2008, 37, 524–535. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. State of the World’s Children 2019: Children, Food and Nutrition; UNICEF: New York, NY, USA, 2019; ISBN 9789280650037. [Google Scholar]
- Nkosi, V.; Haman, T.; Naicker, N.; Mathee, A. Overcrowding and Health in Two Impoverished Suburbs of Johannesburg, South Africa. BMC Public Health 2019, 19, 1358. [Google Scholar] [CrossRef] [PubMed]
- De Onis, M.; Onyango, A.W.; Borghi, E.; Garza, C.; Yang, H. Comparison of the World Health Organization (WHO) Child Growth Standards and the National Center for Health Statistics/WHO International Growth Reference: Implications for Child Health Programmes. Public Health Nutr. 2006, 9, 942–947. [Google Scholar] [CrossRef] [PubMed]
- Bhargava, M.; Bhargava, A.; Ghate, S.D.; Shyama Prasad Rao, R. Nutritional Status of Indian Adolescents (15–19 Years) from National Family Health Surveys 3 and 4: Revised Estimates Using WHO 2007 Growth Reference. PLoS ONE 2020, 15, e0234570. [Google Scholar] [CrossRef]
- Mitra, M.P.P. National Policy for Senior Citizens; Government of India: New Delhi, India, 2011. [Google Scholar]
- Lim, J.U.; Lee, J.H.; Kim, J.S.; Hwang, Y.I.; Kim, T.H.; Lim, S.Y.; Yoo, K.H.; Jung, K.S.; Kim, Y.K.; Rhee, C.K. Comparison of World Health Organization and Asia-Pacific Body Mass Index Classifications in COPD Patients. Int. J. Chronic Obstr. Pulm. Dis. 2017, 12, 2465–2475. [Google Scholar] [CrossRef]
- Tesema, G.A.; Yeshaw, Y.; Kasie, A.; Liyew, A.M.; Teshale, A.B.; Alem, A.Z. Spatial Clusters Distribution and Modelling of Health Care Autonomy among Reproductive-age Women in Ethiopia: Spatial and Mixed-effect Logistic Regression Analysis. BMC Health Serv. Res. 2021, 21, 74. [Google Scholar] [CrossRef]
- Ministry of Health and Family Welfare. National Family Health Survey-5 State Fact Sheet Telangana (2019–2020); International Institute for Population Sciences: Mumbai, India, 2021; pp. 1–7. [Google Scholar]
- International Institute for Population Sciences. National Family Health Survey (NFHS-5) Andhra Pradesh 2019–2021; International Institute for Population Sciences: Mumbai, India, 2021. [Google Scholar]
- Ministry of Health and Family Welfare. Government of India Comprehensive National Nutrition Survey 2016–2018; Ministry of Health and Family: New Delhi, India, 2019; Volume 4, p. 290. [Google Scholar]
- Sidenur, B.; Gowrishankar; Mupparapu, S. Prevalence of Obesity and Overweight and Its Correlates among 20–40 Year Old Population in an Urban Area in Southern India. Natl. J. Community Med. 2022, 13, 114–119. [Google Scholar] [CrossRef]
- Rengma, M.S.; Sen, J.; Mondal, N. Socio-Economic, Demographic and Lifestyle Determinants of Overweight and Obesity among Adults of Northeast India. Ethiop. J. Health Sci. 2015, 25, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Bharati, D.R.; Pal, R.; Rekha, R.; Yamuna, T.V.; Kar, S.; Radjou, A.N. Ageing in Puducherry, South India: An Overview of Morbidity Profile. J. Pharm. Bioallied Sci. 2011, 3, 537–542. [Google Scholar] [CrossRef] [PubMed]
- Amuna, P.; Zotor, F.B. Epidemiological and Nutrition Transition in Developing Countries: Impact on Human Health and Development. Proc. Nutr. Soc. 2008, 67, 82–90. [Google Scholar] [CrossRef] [PubMed]
| Variable | Category | Urban (N = 8317) n (%) | Rural (N = 2033) n (%) | Total (N = 10,350) n (%) |
|---|---|---|---|---|
| Gender | Male | 4140 (49.8) | 986 (48.5) | 5126 (49.6) |
| Female | 4174 (50.2) | 1047 (51.5) | 5221 (50.4) | |
| Transgender | 3 (0.0) | – | 3 (0.0) | |
| Religion | Hindu | 6617 (79.6) | 1950 (95.9) | 8567 (82.8) |
| Muslim | 1120 (13.5) | 73 (3.6) | 1193 (11.5) | |
| Christianity | 564 (6.7) | 10 (0.5) | 574 (5.5) | |
| Others | 16 (0.2) | – | 16 (0.2) | |
| General | 219 (2.6) | 817 (40.2) | 1036 (10.0) | |
| House ownership | Own | 5366 (64.5) | 1790 (88.1) | 7156 (69.1) |
| Rented/leased/others | 2951 (35.5) | 243 (11.9) | 3194 (30.9) | |
| Type of family | Nuclear | 5646 (67.9) | 1193 (58.7) | 6839 (66.1) |
| Extended/three-generation family | 2280 (27.4) | 596 (29.3) | 2876 (27.8) | |
| Joint | 391 (4.7) | 244 (12.0) | 635 (6.1) | |
| Type of house | Pucca | 5495 (66.1) | 1547 (76.1) | 7042 (68.0) |
| Mixed | 2772 (33.3) | 281 (13.8) | 3053 (29.5) | |
| Kutcha | 50 (0.6) | 205 (10.1) | 255 (2.5) | |
| Overcrowding | Not overcrowded | 3666 (44.1) | 1175 (57.8) | 4841 (46.8) |
| Overcrowded | 4651 (55.9) | 858 (42.2) | 5509 (53.2) | |
| Place of cooking | Separate kitchen | 4939 (59.4) | 240 (11.8) | 5179 (50.1) |
| No separate kitchen | 3378 (40.6) | 1793 (88.2) | 5171 (49.9) | |
| Cooking fuel | Gas | 8307 (99.9) | 1742 (85.7) | 10,049 (97.1) |
| Firewood/others | 10 (0.1) | 291 (14.3) | 301 (2.9) | |
| Source of water for drinking and cooking | Piped water into residence/buying water with cans/water purifier in the house | 8273 (99.5) | 1029 (50.6) | 9302 (89.9) |
| Public tap/public well/bore/well on residence/plot | 44 (0.5) | 1004 (49.4) | 1048 (10.1) | |
| Most common method of defecation | Use toilet at home | 8025 (96.5) | 1602 (78.8) | 9627 (93.0) |
| Public/community/shared toilet | 232 (2.8) | 6 (0.3) | 238 (2.3) | |
| Open field | 60 (0.7) | 425 (20.9) | 485 (4.7) | |
| Method of garbage disposal | Panchayat/corporation garbage disposal services/garbage dump/public pits | 8208 (98.7) | 725 (35.7) | 8933 (86.3) |
| Drainage/vacant/ abandoned house/burning | 2 (0.0) | 781 (38.4) | 783 (7.6) | |
| No designated place | 107 (1.3) | 527 (25.9) | 634 (6.1) | |
| Occupation code | Professional/semi-professional | 157 (1.9) | 71 (3.5) | 228 (2.2) |
| Clerk/skilled workers/semi-skilled workers | 3932 (47.3) | 910 (44.8) | 4842 (46.8) | |
| Unskilled worker | 832 (9.9) | 292 (14.4) | 1124 (10.8) | |
| Unemployed | 189 (2.3) | 39 (1.8) | 228 (2.2) | |
| Student/preschool/Balwadi school | 3207 (38.6) | 721 (35.5) | 3928 (38) | |
| Literate (age > 7 years) * | Illiterate | 1601 (21.6) | 446 (24.2) | 2047 (22.0) |
| Read | 16 (0.2) | 30 (1.6) | 46 (0.5) | |
| Read and write | 5817 (78.1) | 1370 (74.1) | 7187 (77.4) | |
| Preschool/Balwadi school | 10 (0.1) | 1 (0.1) | 11 (0.1) | |
| Wealth Index | Lowest | 3649 (43.9) | 820 (40.3) | 4469 (43.2) |
| Middle | 2041 (24.5) | 393 (19.4) | 2434 (23.5) | |
| Highest | 2627 (31.6) | 820 (40.3) | 3447 (33.3) |
| Malnutrition Status | Urban | Rural | Total | ||||
|---|---|---|---|---|---|---|---|
| N = 8317 | N = 2033 | N =10,350 | |||||
| Proportion | % Prevalence | Proportion | % Prevalence | Proportion | % Prevalence | ||
| (n/N) | (95% CI) | (n/N) | (95% CI) | (n/N) | (95% CI) | ||
| Under-5 Children | Stunting | 143/423 | 33.8 (29.4–38.5) | 31/94 | 33.0 (24.1–43.3) | 174/517 | 33.7 (29.7–37.9) |
| Wasting | 83/423 | 19.6 (16.1–23.7) | 20/94 | 21.3 (14.1–30.9) | 103/517 | 19.9 (16.7–23.6) | |
| Overweight | 17/423 | 4.0 (2.5–6.4) | 2/94 | 2.1 (0.5–8.3) | 19/517 | 3.7 (2.4–5.7) | |
| Underweight | 138/438 | 31.5 (27.3–36.0) | 30/96 | 31.3 (22.7–41.4) | 168/534 | 31.5 (27.6–35.5) | |
| 5–19 Years | Stunting | 131/802 | 16.3 (13.9–19.1) | 25/145 | 17.2 (11.9–24.4) | 156/947 | 16.5 (14.2–19) |
| Thinness | 254/801 | 31.7 (28.6–35.0) | 23/145 | 15.9 (10.7–22.8) | 277/946 | 29.3 (26.5–32.3) | |
| Overweight | 95/801 | 11.9 (9.8–14.3) | 24/145 | 16.6 (11.3–23.6) | 119/946 | 12.6 (10.6–14.9) | |
| Obese | 35/801 | 4.4 (3.2–6.0) | 10/145 | 6.9 (3.7–12.4) | 45/946 | 4.8 (3.6–6.3) | |
| Adults (19–59 years) | Underweight (<18.5 Kg/m2) | 301/2590 | 11.6 (10.4–12.9) | 104/847 | 12.3 (10.2–14.7) | 405/3437 | 11.8 (10.7–12.9) |
| Normal (18.5–22.9 Kg/m2) | 671/2590 | 25.9 (24.3–27.6) | 222/847 | 26.2 (23.4–29.9) | 893/3437 | 26.0 (24.5–27.5) | |
| Overweight (23–24.9 Kg/m2) | 384/2590 | 14.8 (13.5–16.3) | 125/847 | 14.8 (12.5–17.3) | 509/3437 | 14.8 (13.7–16) | |
| Obese (≥25 Kg/m2) | 1234/2590 | 47.7 (45.7–49.6) | 396/847 | 46.7 (43.4–50.1) | 1630/3437 | 47.4 (45.8–49.1) | |
| Geriatric (60 years and above) | Underweight (<18.5 Kg/m2) | 36/465 | 7.7 (5.6–10.6) | 46/217 | 21.2 (16.2–27.2) | 82/682 | 12.0 (9.8–14.7) |
| Normal (18.5–22.9 Kg/m2) | 126/465 | 27.1 (23.2–31.3) | 71/217 | 32.7 (26.8–39.3) | 197/682 | 28.9 (25.6–32.4) | |
| Overweight (23–24.9 Kg/m2) | 68/465 | 14.6 (11.7–18.2) | 28/217 | 12.9 (9.0–18.1) | 96/682 | 14.1 (11.7–16.9) | |
| Obese (≥25 Kg/m2) | 235/465 | 50.6 (46.0–55.1) | 72/217 | 33.2 (27.2–39.8) | 307/682 | 45 (41.3–48.8) | |
| Variable | Category | Under-5 Children | 5–19 Years | Adult (19–59 Years) | |||
|---|---|---|---|---|---|---|---|
| Stunting (Yes/No = 174/343) | Thinness (Yes/No = 277/669) | Obese (Yes/No = 1630/1807) | |||||
| Adjusted OR (95% CI) | p–Value | Adjusted OR (95% CI) | p–Value | Adjusted OR (95% CI) | p–Value | ||
| Place of residence | Urban | 1.14 (0.43–2.98) | 0.795 | 2.52 (1.10–5.75) | 0.028 * | 0.84 (0.61–1.16) | 0.290 |
| Rural | Ref | – | Ref | – | Ref | – | |
| Age group in years | 0–2 | 2.32 (1.29–4.18) | 0.005 * | – | – | – | – |
| 3–5 | Ref | – | – | – | – | – | |
| 5–9 | – | Ref | – | – | – | ||
| 10–14 | – | 1.13 (0.68–1.86) | 0.639 | – | – | ||
| 15–19 | – | 1.01 (0.61–1.66) | 0.974 | – | – | ||
| 20–39 | – | – | – | Ref | – | ||
| 40–59 | – | – | – | 1.91 (1.59–2.28) | <0.001 * | ||
| Gender | Male | 1.54 (0.85–2.80) | 0.156 | 2.62 (1.75–3.93) | <0.001 * | 0.79 (0.66–0.93) | 0.006 * |
| Female | Ref | – | Ref | – | Ref | – | |
| Religion | Hindu | Ref | – | Ref | – | Ref | – |
| Muslim | 0.45 (0.17–1.22) | 0.118 | 1.16 (0.60–2.26) | 0.659 | 1.73 (1.28–2.34) | <0.001 * | |
| Christianity | 1.63 (0.52–5.13) | 0.407 | 0.85 (0.34–2.09) | 0.719 | 1.17 (0.79–1.72) | 0.435 | |
| House ownership | Own | Ref | – | Ref | – | Ref | – |
| Rented/leased/others | 1.40 (0.66–2.95) | 0.383 | 0.96 (0.60–1.55) | 0.876 | 0.78 (0.63–0.97) | 0.023 * | |
| Type of family | Nuclear | Ref | – | – | – | Ref | – |
| Extended/three-generation family | 0.82 (0.39–1.72) | 0.594 | – | – | 0.91 (0.73–1.14) | 0.415 | |
| Joint | 1.16 (0.35–3.92) | 0.806 | – | – | 1.16 (0.78–1.73) | 0.476 | |
| Type of house | Pucca | Ref | – | Ref | – | Ref | – |
| Mixed | 2.48 (1.12–5.47) | 0.024 * | 0.86 (0.54–1.36) | 0.513 | 0.85 (0.69–1.05) | 0.129 | |
| Kutcha | 2.91 (0.27–31.88) | 0.382 | 0.61 (0.12–3.10) | 0.547 | 0.76 (0.41–1.42) | 0.390 | |
| Overcrowding | Not overcrowded | Ref | – | Ref | – | Ref | – |
| Overcrowded | 1.17 (0.58–2.37) | 0.656 | 1.68 (1.04–2.71) | 0.035 * | 0.83 (0.68–0.99) | 0.048 * | |
| Place of cooking | Separate kitchen | Ref | – | – | – | Ref | – |
| No separate kitchen | 1.00 (0.51–1.95) | 0.992 | – | – | 0.80 (0.66–0.98) | 0.033 * | |
| Cooking fuel | Gas | Ref | – | – | – | Ref | – |
| Firewood/others | 1.50 (0.15–14.83) | 0.731 | – | – | 0.41 (0.23–0.74) | 0.003 * | |
| Source of water for drinking and cooking | Piped water into residence/buying water with cans/water purifier in the house | – | – | Ref | – | Ref | – |
| Public tap /public well/bore/well on residence/plot | – | – | 0.87 (0.27–2.78) | 0.809 | 0.79 (0.56–1.13) | 0.195 | |
| Most common method of defecation | Use toilet at home | – | – | – | – | Ref | – |
| Public/community/shared Toilet | – | – | – | – | 1.05 (0.59–1.88) | 0.859 | |
| Open field | – | – | – | – | 0.97 (0.56–1.66) | 0.900 | |
| Occupation code | Professional/semi- professional | – | – | – | – | 1.14 (0.65–2.01) | 0.649 |
| Clerk/skilled workers/semi-skilled workers | – | – | – | – | 1.32 (1.02–1.71) | 0.034 * | |
| Unskilled worker | – | – | – | – | Ref | – | |
| Unemployed | – | – | – | – | 0.81 (0.49–1.35) | 0.416 | |
| Student | – | – | – | – | 0.49 (0.33–0.73) | <0.001 * | |
| Wealth Index | Lowest | 3.46 (1.32–9.06) | 0.012 * | 1.34 (0.77–2.34) | 0.294 | 0.59 (0.46–0.74) | <0.001 * |
| Middle | 3.47 (1.27–9.45) | 0.015 * | 0.88 (0.48–1.63) | 0.683 | 0.79 (0.62–1.1) | 0.052 | |
| Highest | Ref | – | Ref | – | Ref | – | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramanujam, K.; Mergu, N.; Kondeth, H.; Reddy, G.V.R.; Venkata Prasad, U.; Sadasivuni, R.; Geddam, J.B.; Rajkumar, H.; Reddy, N.S. Chronic Illness, Nutritional Status, and Factors Associated with Malnutrition among Various Age Groups Residing in Urban Areas of Telangana and Rural Areas of Andhra Pradesh. Nutrients 2023, 15, 4470. https://doi.org/10.3390/nu15204470
Ramanujam K, Mergu N, Kondeth H, Reddy GVR, Venkata Prasad U, Sadasivuni R, Geddam JB, Rajkumar H, Reddy NS. Chronic Illness, Nutritional Status, and Factors Associated with Malnutrition among Various Age Groups Residing in Urban Areas of Telangana and Rural Areas of Andhra Pradesh. Nutrients. 2023; 15(20):4470. https://doi.org/10.3390/nu15204470
Chicago/Turabian StyleRamanujam, Karthikeyan, Nagaraju Mergu, Henna Kondeth, Garlapati Venkat Raji Reddy, Upadrasta Venkata Prasad, Renuka Sadasivuni, Jagajeevan Babu Geddam, Hemalatha Rajkumar, and Nusi Samarasimha Reddy. 2023. "Chronic Illness, Nutritional Status, and Factors Associated with Malnutrition among Various Age Groups Residing in Urban Areas of Telangana and Rural Areas of Andhra Pradesh" Nutrients 15, no. 20: 4470. https://doi.org/10.3390/nu15204470
APA StyleRamanujam, K., Mergu, N., Kondeth, H., Reddy, G. V. R., Venkata Prasad, U., Sadasivuni, R., Geddam, J. B., Rajkumar, H., & Reddy, N. S. (2023). Chronic Illness, Nutritional Status, and Factors Associated with Malnutrition among Various Age Groups Residing in Urban Areas of Telangana and Rural Areas of Andhra Pradesh. Nutrients, 15(20), 4470. https://doi.org/10.3390/nu15204470





