Characteristics of Current Teaching Kitchens: Findings from Recent Surveys of the Teaching Kitchen Collaborative
Abstract
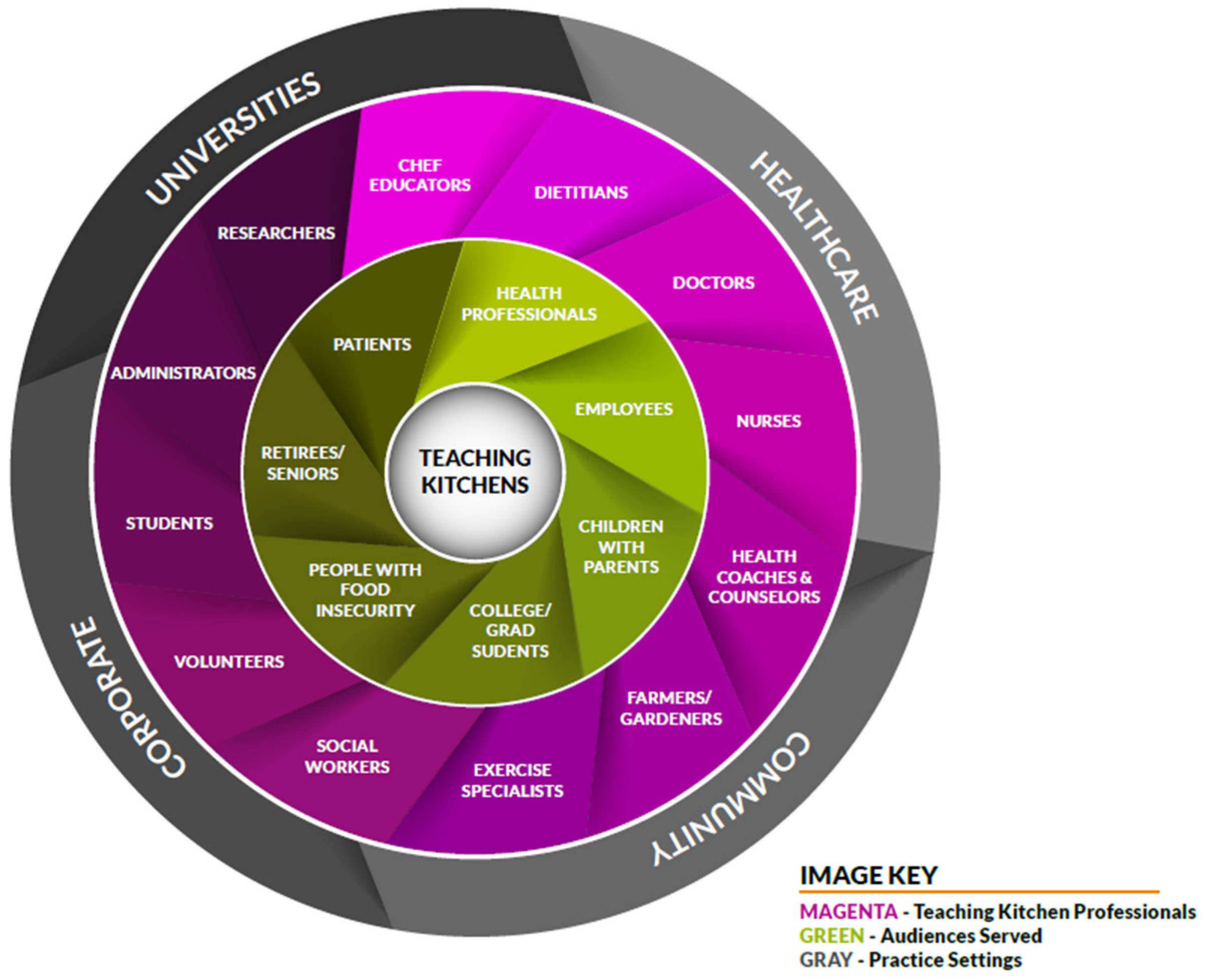
:1. Introduction
2. Materials and Methods
- Mobile cart: portable and self-contained unit
- Pop-up (or modular) kitchen: temporary kitchen, assembled in a room or commercial kitchen
- Container/Pod: contained kitchen, transported via trailer or truck
- Built-in: dedicated, permanent kitchen space
- Virtual: remote kitchen space, accessed online
2.1. Iteration 1
2.2. Iteration 2
3. Results
3.1. Survey Completion
3.2. Summary of Findings
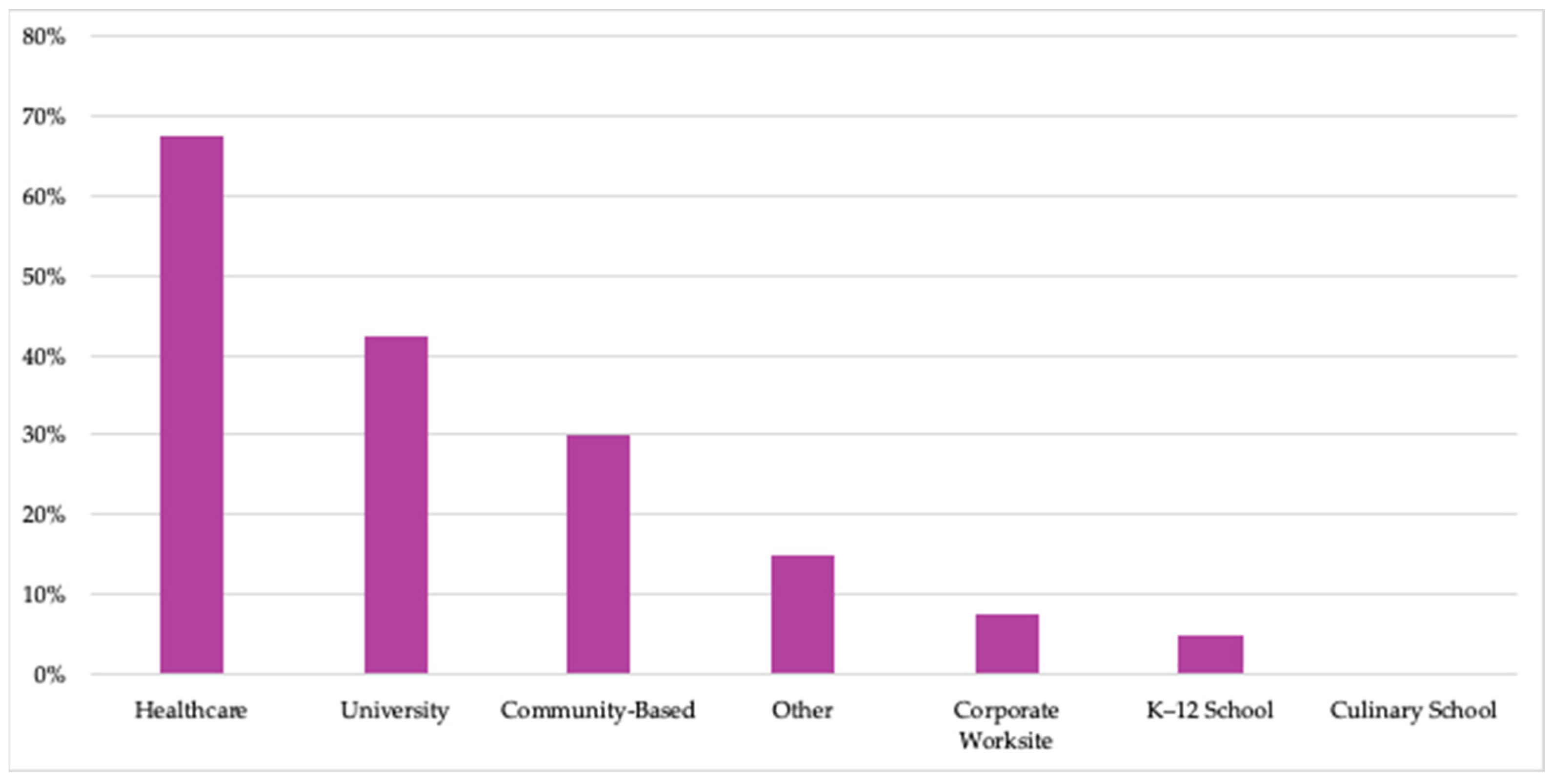
3.2.1. TK Setting(s)
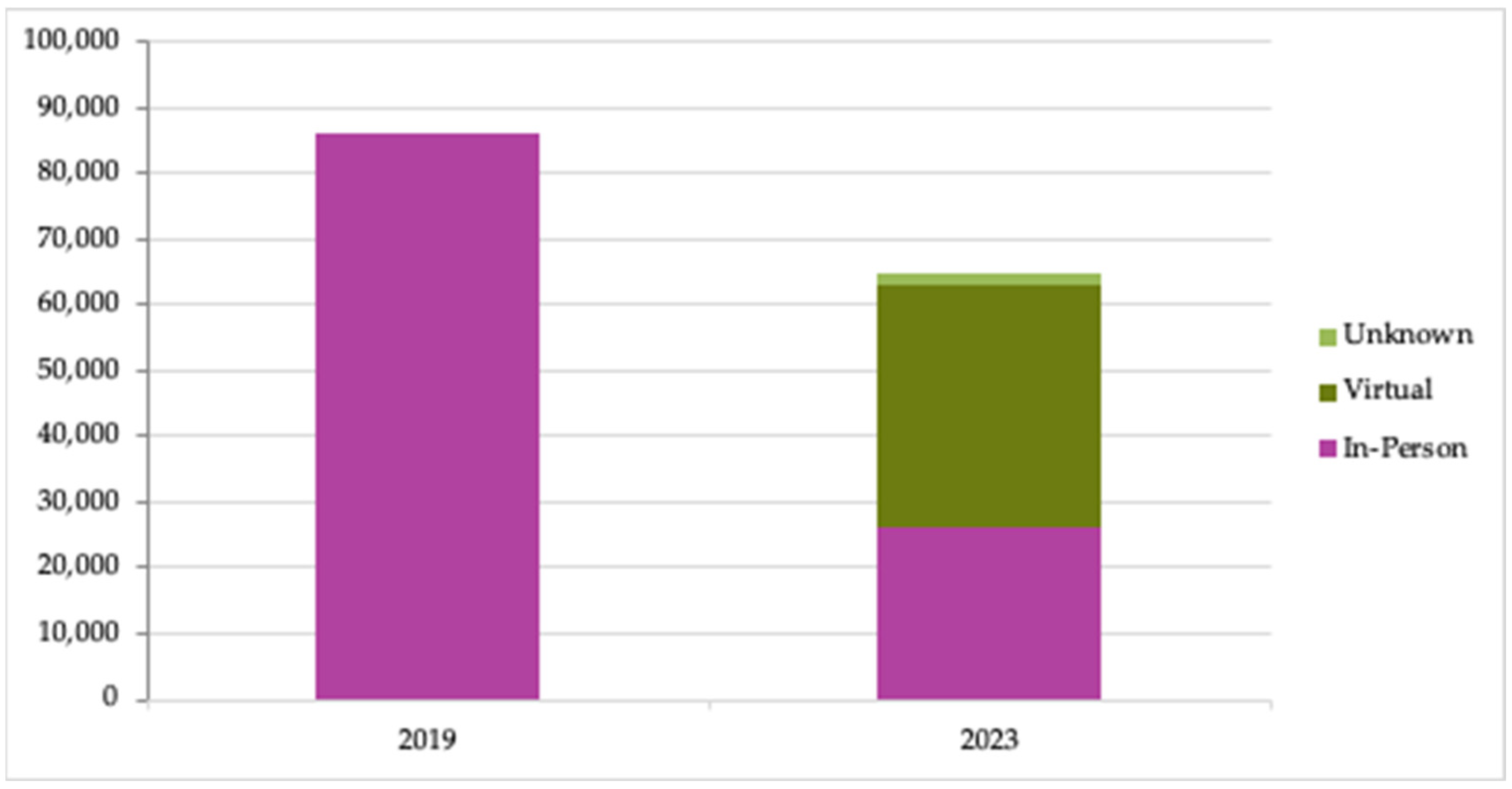
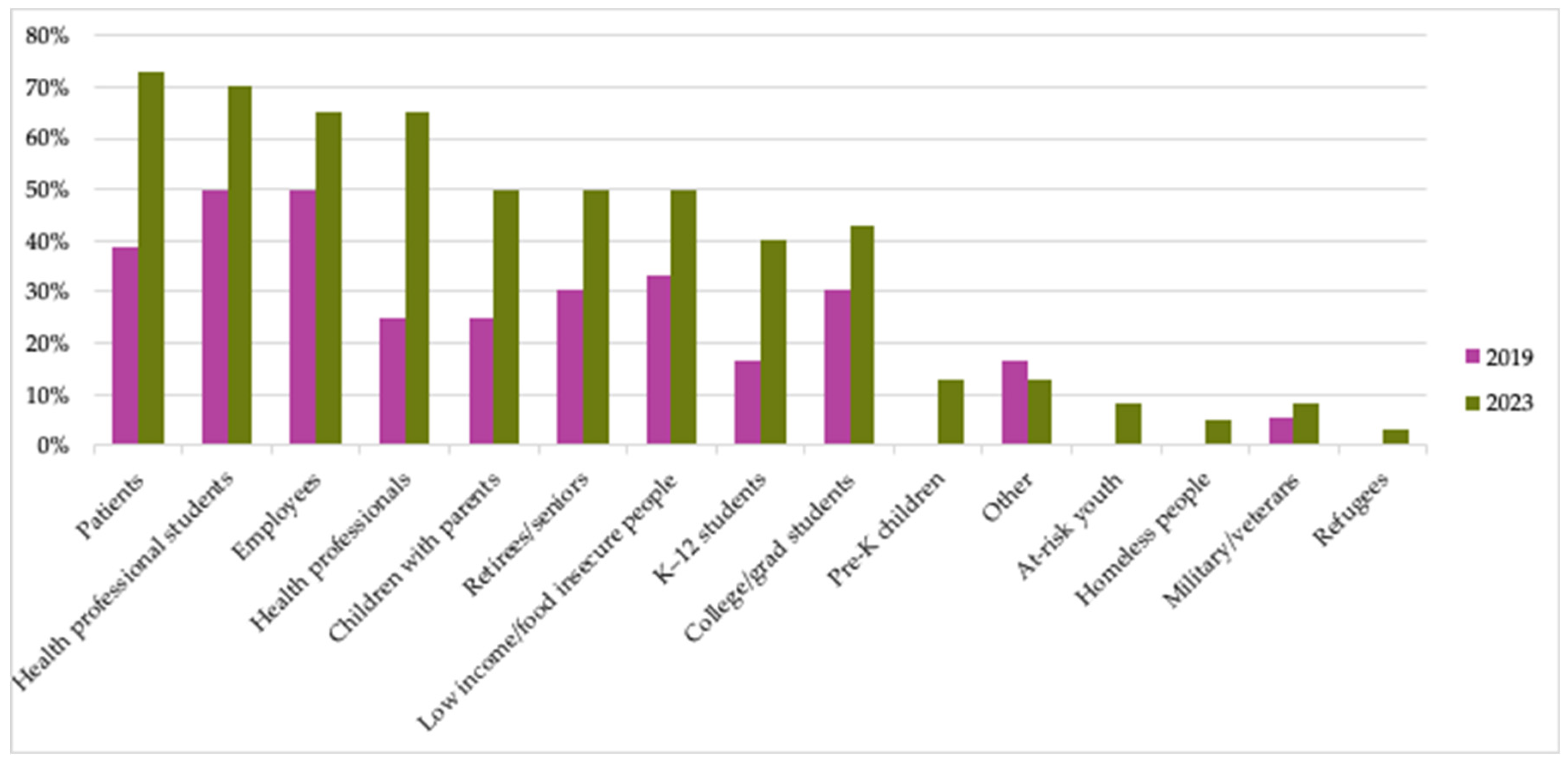
3.2.2. Audiences Served
3.2.3. TK Model(s)
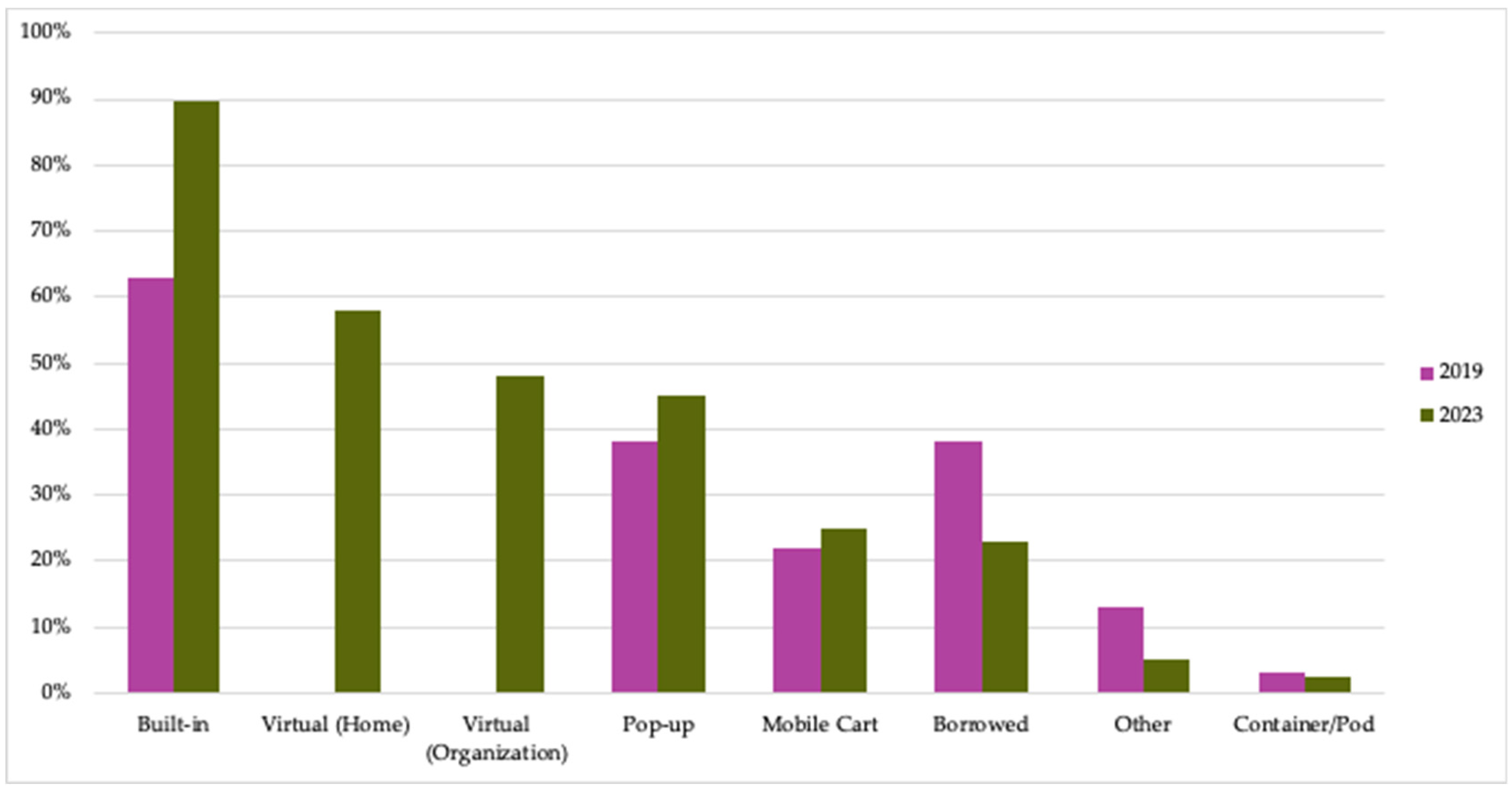
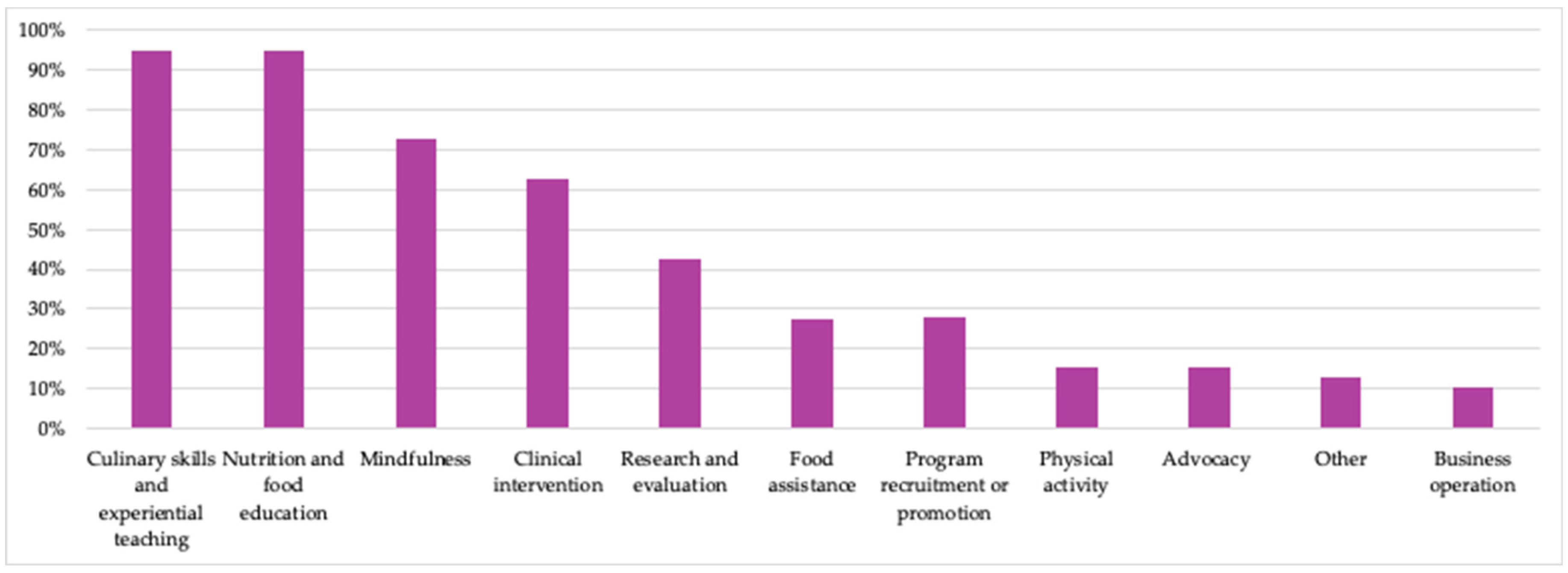
3.2.4. Key Lines of Operations
3.2.5. Professional Background of Team Member Who Manages or Directs the TK
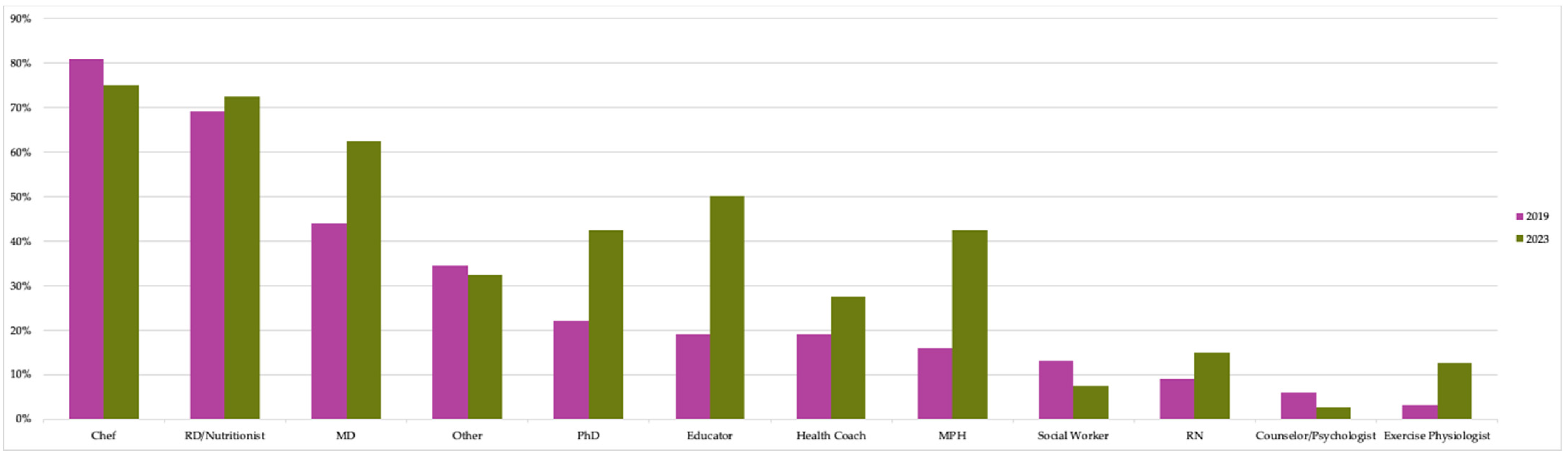
3.2.6. Team Member(s) Who Facilitate(s) TK Programming
3.2.7. Primary Funding Sources
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. First TKC Member Survey Administered through Qualtrics
- 1.
- Please provide the full name of your organization and affiliated center.
- 2.
- Who is the primary contact completing this form?
- 3.
- Have there been any significant changes to your teaching kitchen(s) and TK related programs since you joined the Teaching Kitchen Collaborative (e.g., renovations, opening of new kitchen, etc.)?
- 4.
- How many people (full or part-time) are on your teaching team?
- •
- 1
- •
- 2
- •
- 3
- •
- 4
- •
- 5 and up
- 5.
- Person #1: What type of credentials does your instructor have? (select all that apply as some may have multiple credentials)
- •
- Chef/culinary training (e.g., CEC, AAC)
- •
- Medical doctor
- •
- Dietitian (e.g., RD, CSSD, RDN, LD)
- •
- Nurse (e.g., RD, APRN, FNP)
- •
- Master of Public Health
- •
- Social work (e.g., MSW)
- •
- Counseling/psychology
- •
- Educator (e.g., Certified Diabetes Educator, Master of Education)
- •
- Health Coach
- •
- Exercise physiologist
- •
- No specific credential/volunteer
- •
- PhD or ScD
- •
- Administrative assistant/administrator
- •
- Other [write in] ____________________
- 6.
- Person #2: What type of credentials does your instructor have? (select all that apply as some may have multiple credentials)
- •
- Chef/culinary training (e.g., CEC, AAC)
- •
- Medical doctor
- •
- Dietitian (e.g., RD, CSSD, RDN, LD)
- •
- Nurse (e.g., RD, APRN, FNP)
- •
- Master of Public Health
- •
- Social work (e.g., MSW)
- •
- Counseling/psychology
- •
- Educator (e.g., Certified Diabetes Educator, Master of Education)
- •
- Health Coach
- •
- Exercise physiologist
- •
- No specific credential/volunteer
- •
- PhD or ScD
- •
- Administrative assistant/administrator
- •
- Other [write in] ____________________
- 7.
- Person #3: What type of credentials does your instructor have? (select all that apply as some may have multiple credentials)
- •
- Chef/culinary training (e.g., CEC, AAC)
- •
- Medical doctor
- •
- Dietitian (e.g., RD, CSSD, RDN, LD)
- •
- Nurse (e.g., RD, APRN, FNP)
- •
- Master of Public Health
- •
- Social work (e.g., MSW)
- •
- Counseling/psychology
- •
- Educator (e.g., Certified Diabetes Educator, Master of Education)
- •
- Health Coach
- •
- Exercise physiologist
- •
- No specific credential/volunteer
- •
- PhD or ScD
- •
- Administrative assistant/administrator
- •
- Other [write in] ____________________
- 8.
- Person #4: What type of credentials does your instructor have? (select all that apply as some may have multiple credentials)
- •
- Chef/culinary training (e.g., CEC, AAC)
- •
- Medical doctor
- •
- Dietitian (e.g., RD, CSSD, RDN, LD)
- •
- Nurse (e.g., RD, APRN, FNP)
- •
- Master of Public Health
- •
- Social work (e.g., MSW)
- •
- Counseling/psychology
- •
- Educator (e.g., Certified Diabetes Educator, Master of Education)
- •
- Health Coach
- •
- Exercise physiologist
- •
- No specific credential/volunteer
- •
- PhD or ScD
- •
- Administrative assistant/administrator
- •
- Other [write in] ____________________
- 9.
- Person #5: What type of credentials does your instructor have? (select all that apply as some may have multiple credentials)
- •
- Chef/culinary training (e.g., CEC, AAC)
- •
- Medical doctor
- •
- Dietitian (e.g., RD, CSSD, RDN, LD)
- •
- Nurse (e.g., RD, APRN, FNP)
- •
- Master of Public Health
- •
- Social work (e.g., MSW)
- •
- Counseling/psychology
- •
- Educator (e.g., Certified Diabetes Educator, Master of Education)
- •
- Health Coach
- •
- Exercise physiologist
- •
- No specific credential/volunteer
- •
- PhD or ScD
- •
- Administrative assistant/administrator
- •
- Other [write in] ____________________
- 10.
- What percent of your entire instructional team is full-time, part-time (paid), and volunteer in terms of their commitment to the TK program? [must add to 100%]
- ______ Full Time
- ______ Part Time (Paid)
- ______ Volunteer
- 11.
- Culinary Skills
| Taught in All Classes | Taught in Some Classes | Not Taught | |
| Kitchen set up and safety | 🔾 | 🔾 | 🔾 |
| Basic cooking/food preparation skills | 🔾 | 🔾 | 🔾 |
| Healthy cooking techniques | 🔾 | 🔾 | 🔾 |
| Meal planning and food shopping strategies | 🔾 | 🔾 | 🔾 |
| Guided grocery store and/or farm/farmers’ market tour | 🔾 | 🔾 | 🔾 |
- 12.
- Are there any other major topics within Culinary Skills that you cover? Please describe.
- 13.
- Nutrition & Health
| Taught in All Classes | Taught in Some Classes | Not Taught | |
| General guidelines for healthy dietary patterns | 🔾 | 🔾 | 🔾 |
| Recommendations for specific foods/nutrients | 🔾 | 🔾 | 🔾 |
| Disease-specific recommendations | 🔾 | 🔾 | 🔾 |
| Food systems, sustainability, waste considerations | 🔾 | 🔾 | 🔾 |
- 14.
- Are there any other major topics within Nutrition & Health that you cover? Please describe.
- 15.
- Exercise & Movement
| Taught in All Classes | Taught in Some Classes | Not Taught | |
| General guidelines for increased physical activity | 🔾 | 🔾 | 🔾 |
| Guided exercises/activity bursts during class session(s) | 🔾 | 🔾 | 🔾 |
- 16.
- Are there any other major topics within Exercise & Movement that you cover? Please describe.
- 17.
- Mindfulness
| Taught in All Classes | Taught in Some Classes | Not Taught | |
| Definition and benefits of mindfulness as applied to eating, cooking, exercising, sleep, etc. | 🔾 | 🔾 | 🔾 |
| Guided mindfulness exercises during class session(s) | 🔾 | 🔾 | 🔾 |
- 18.
- Are there any other major topics within Mindfulness that you cover? Please describe.
- 19.
- Health Coaching & Behavior Change
| Taught in All Classes | Taught in Some Classes | Not Taught | |
| Individual health coaching with program participants | 🔾 | 🔾 | 🔾 |
| Facilitated group discussion | 🔾 | 🔾 | 🔾 |
| Follow-up sessions after intervention period | 🔾 | 🔾 | 🔾 |
- 20.
- Are there any other major topics within Health Coaching & Behavior Change that you cover? Please describe.
- 21.
- Are there any other major topics outside of Culinary, Nutrition & Health, Exercise & Movement, Mindfulness, and Health Coaching & Behavior Change that you cover? Please describe.
- 22.
- Do you use a standard teaching kitchen curriculum that you license or purchased?
- •
- We currently use a curriculum that we purchased or license. [skip questions 24 and 25]
- •
- We considered purchasing or licensing a curriculum, but decided not to [skip to questions 23 and 25]
- •
- We have not purchased or licensed a curriculum [skip questions 23 and 24]
- 23.
- Which curriculum did you purchase/license and why?
- 24.
- Which curriculum did you consider purchasing or licensing and why did you decide not to go forward with it?
- 25.
- Please describe what curriculum you use.
- 26.
- How often are participants involved in the following activities during your teaching kitchen program?
| In Every Class | In Some Classes | Never | |
| Watching lectures | 🔾 | 🔾 | 🔾 |
| Viewing cooking demonstrations | 🔾 | 🔾 | 🔾 |
| Performing hands-on cooking | 🔾 | 🔾 | 🔾 |
| Tasting | 🔾 | 🔾 | 🔾 |
| Homework/home assignments | 🔾 | 🔾 | 🔾 |
| Other [please describe] | 🔾 | 🔾 | 🔾 |
- 27.
- Please specify the type of kitchen facility or facilities you employ (mark all that apply):
- •
- Mobile Cart: Portable and self-contained unit; can be as simple as a burner plate on a cart or a fully furnished mobile unit
- •
- Pop-Up/Modular Kitchen: Temporary kitchen for short term; pieced together with cooktops, cutting boards, kitchenware, etc.; either with or without a dedicated space
- •
- Container/pod: Contained kitchen, either transported via trailer or truck
- •
- Built-In: Dedicated, permanent kitchen space
- •
- Borrowed: Borrowing kitchen/space at another organization’s facility (e.g., local culinary institute, community center, school) [please describe] ____________________
- •
- Other [please describe] ____________________
- 28.
- What approximate level of up-front investment was made in your kitchen facility/facilities? Give your best guess estimate.
- •
- Under $1000
- •
- $1000–$10,000
- •
- $10,000–$50,000
- •
- $50,000–$100,000
- •
- $100,000–$200,000
- •
- $200,000–$300,000
- •
- $300,000–$400,000
- •
- $400,000–$500,000
- •
- Over $500,000
- 29.
- On an annual basis, approximately how much does it cost to run your teaching kitchen and associated programs (including staff, programing, facilities upkeep, etc.). Give your best guess estimate.
- •
- Under $5000
- •
- $5000–$20,000
- •
- $20,000–$35,000
- •
- $35,000–$50,000
- •
- Over $50,000
- 30.
- Approximately what percentage of the total cost of running your teaching kitchen program is in each category? [categories must sum to 100%]
- ______ Staff salaries
- ______ Programing (e.g., curriculum development, purchase)
- ______ Incremental class supplies (e.g., food, disposable supplies, printed materials, etc.)
- ______ Ongoing facilities investments and maintenance (e.g., new equipment)
- ______ Other [please describe]
- 31.
- Approximately what are the main sources of funding for your teaching kitchen programs? [categories must sum to 100%]
- ______ Participant dues and fees
- ______ Philanthropy (individual donations, foundation grants)
- ______ Corporate sponsorships
- ______ Endowment
- ______ Other [please describe]
- 32.
- Have you found any strategies to be particularly effective in securing funding for your teaching kitchen program? If so, please describe.
- 33.
- Please specify the primary audience of focus for your teaching kitchen classes (check all that apply).
- •
- Employees
- •
- Patients
- •
- Children with their parents
- •
- Students (K–12)
- •
- College/graduate students
- •
- Health professionals students (medical students, dietetic interns, etc.)
- •
- Health professionals (MD, RD, RN, etc.)
- •
- Retirees/senior citizens
- •
- Military
- •
- Low-income/food insecure
- •
- Other [please describe] ____________________
- 34.
- What is the primary reason your participants attend teaching kitchen classes? (check all that apply).
- •
- As a preventive health measure
- •
- To address health issues
- •
- To support family members (children, spouses, parents) in achieving health goals
- •
- Due to a health professional recommendation or referral
- •
- To obtain a financial incentive provided by employer or insurer (e.g., HSA money, health care premium breaks, etc.)
- •
- For fun or to learn a new skill
- •
- Other [please describe] ____________________
- 35.
- Estimate how many total participants have participated in the last 12 months?
- 36.
- Estimate how many total participants have participated since you first joined the Teaching Kitchen Collaborative?
- 37.
- Estimate what percentage of your participants have joined each type of teaching kitchen program [must sum to 100%]?
- ______ One-off classes
- ______ Mini series (2–4 classes)
- ______ Longer series (5–9 classes)
- ______ Transformation program (10+ classes)
- 38.
- What type of data, if any, do you collect on participants?
- •
- Pre/post self-reported data on knowledge and/or skills
- •
- Feedback on classes and recipes
- •
- General descriptive data (e.g., age, gender, race)
- •
- Medical history (e.g., diabetes, hypertension, heart disease)
- •
- Body measurements (height, weight)
- •
- Biometric data (e.g., lipid panel, blood sugar)
- •
- We do not collect data at this time
- •
- Other [please describe] ____________________
- 39.
- Have you or your team collaborated with any other TKC member organizations outside of organized TKC meetings and calls (e.g., sharing/brainstorming program strategies, curriculum, and/or other resources)? If so, which member organizations have you collaborated with and in what capacities?
- •
- No
- •
- Yes [please describe] ____________________
- 40.
- Have ideas from other collaborative members meaningfully impacted your teaching kitchen program? If so, please share an example or two.
- 41.
- On a scale from 0–10, how likely are you to recommend the Teaching Kitchen Collaborative to other similar organizations to yours?
- •
- 0
- •
- 1
- •
- 2
- •
- 3
- •
- 4
- •
- 5
- •
- 6
- •
- 7
- •
- 8
- •
- 9
- •
- 10
- 42.
- What has the Collaborative been most useful for?
- 43.
- What has the Collaborative been least useful for?
- 44.
- Rate the value of your TKC membership to your organization.
- •
- Extremely valuable
- •
- Very valuable
- •
- Moderately valuable
- •
- Slightly valuable
- •
- Not at all valuable
- (1)
- Expanded Best Practices: Additional documents and webinars with best practices (e.g., facility and curriculum design)
- (2)
- Cooking Videos: A library of cooking videos
- (3)
- Core Curriculum: A complete teaching kitchen curriculum
- (4)
- TK Starter Kit: A “turnkey” guide used for end-to-end creation of a TK (including facility design, curriculum, staffing etc.)
- (5)
- Research Consulting: More assistance on research (e.g., consulting on measuring program efficacy, research conferences, webinars)
- (6)
- Data Platform: Data platform accessible by members, used to track outcomes
- (7)
- Outcomes Research: Large, multi-site projects to demonstrate improvement in behaviors, clinical outcomes and cost
- (8)
- Standard Setting: Creating accreditation standards for TKs including facilities, trainers, curricula
- (9)
- Train the Trainer: Training sessions (in person or online) for TK facilitators
- 45.
- What, in your team’s opinion, are the three most important initiatives for the Teaching Kitchen Collaborative to focus on over the next 24 months? Please rank only your top 3 areas of focus.
| (1) Best Practices | (2) Cooking Videos | (3) Core Curriculum | (4) TK Starter Kit | (5) Research Consulting | (6) Data Platform | (7) Outcomes Research | (8) Standard Setting | (9) Train the Trainer | |
| Top Priority | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 |
| Second Priority | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 |
| Third Priority | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 | 🔾 |
- 46.
- Before finishing this survey, is there anything else we should know in order to make the Collaborative increasingly valuable for your organization?
Appendix B. Second TKC Member Survey Administered through Neon
- 1.
- Full Name
- 2.
- Company/Organization Name
- 3.
- Email
- 4.
- Phone
- 5.
- Address
- 6.
- In which type of setting is your teaching kitchen? Mark all that apply.
- •
- Community-Based
- •
- Corporate Worksite
- •
- Culinary School
- •
- Healthcare
- •
- K–12 School
- •
- University
- •
- Other [please describe]
- 7.
- What is the name of your teaching kitchen or program?
- 8.
- How many teaching kitchens does your organization operate?
- 9.
- Which describes your teaching kitchen facility(ies)? Mark all that apply.
- •
- Borrowed
- •
- Built-in
- •
- Container/Pod
- •
- Mobile Cart
- •
- Pop-up
- •
- Virtual (organization teaching kitchen)
- •
- Virtual (home kitchen)
- •
- Other [please describe]
- 10.
- What populations do you work with in your teaching kitchen? Mark all that apply.
- At-risk youth
- Children with parents
- K–12 students
- Pre-K children
- College/Graduate students
- Employees
- Health professional students
- Health professionals
- Homeless people
- Low-income/Food insecure people
- Military/Veterans
- Patients
- Refugees
- Retirees/Seniors
- Other [please describe]
- 11.
- What health and social factors does your teaching kitchen address? Mark all that apply.
- •
- Addiction recovery
- •
- Bariatric surgery
- •
- Brain health
- •
- Cancer
- •
- Chronic pain
- •
- Cardiovascular disease
- •
- Diabetes
- •
- Food access
- •
- Maternal and child health
- •
- Mental health
- •
- Optimizing health & wellbeing
- •
- Other [please describe]
- 12.
- What fields, programs, or therapies are involved in your teaching kitchen? Mark all that apply.
- •
- Diabetes Prevention Program
- •
- Educating health professionals
- •
- Fresh food farmacy
- •
- Integrative medicine
- •
- Lifestyle medicine
- •
- Gardening, local farms, & agriculture
- •
- Medical nutrition therapy
- •
- Medically tailored meals
- •
- Produce prescription
- •
- Shared medical appointments
- •
- Other [please describe]
- 13.
- Which is/are a key function(s) of your teaching kitchen? Mark all that apply.
- •
- Advocacy
- •
- Business operation
- •
- Clinical intervention
- •
- Culinary skills and experiential teaching
- •
- Food assistance
- •
- Nutrition and food education
- •
- Mindfulness
- •
- Physical activity
- •
- Program recruitment or promotion
- •
- Research and evaluation
- •
- Other [please describe]
- 14.
- How many professionals are included in your core teaching kitchen team, meaning involved in most essential operations of the TK?
- 15.
- Now consider the wider collaboration in your organization on the TK. How many professionals are included in your extended teaching kitchen team, meaning occasional instructors, volunteers, or researchers?
- 16.
- What type of professional is the overall teaching kitchen lead?
- •
- Administrative assistant
- •
- Administrative director or manager
- •
- Chef
- •
- Counselor/psychologist
- •
- Educator
- •
- Exercise physiologist
- •
- Health coach
- •
- MD
- •
- MPH
- •
- Nurse
- •
- PhD or ScD
- •
- Registered dietitian
- •
- Social worker
- •
- Volunteer
- •
- Other [please describe]
- 17.
- Which other types of professionals facilitate classes in the teaching kitchen? Mark all that apply.
- •
- Administrative assistant
- •
- Administrative director or manager
- •
- Chef
- •
- Counselor/psychologist
- •
- Educator
- •
- Exercise physiologist
- •
- Health coach
- •
- MD
- •
- MPH
- •
- Nurse
- •
- PhD or ScD
- •
- Registered dietitian
- •
- Social worker
- •
- Volunteer
- •
- Other [please describe]
- 18.
- Which sources contribute to funding your teaching kitchen? Mark all that apply.
- •
- Corporate sponsorship
- •
- Diabetes Prevention Program
- •
- Employer/organization paid (department chargeback)
- •
- Insurance reimbursement
- •
- Medical nutrition therapy
- •
- Participant dues and fees (participant paid)
- •
- Philanthropy (individual or foundation)
- •
- Shared medical appointments
- •
- Other
- 19.
- What primary language(s) other than English do your participants speak?
- 20.
- In what language(s) do you teach classes in your teaching kitchen?
- •
- English
- •
- Chinese
- •
- French
- •
- Spanish
- •
- Tagalog
- •
- Vietnamese
- •
- Other [please specify]
- 21.
- How many people participated in your teaching kitchen in person in 2022?
- 22.
- How many people participated in your teaching kitchen virtually in 2022?
- 23.
- Does this refer to the unique number of participants or total number of visits (including repeat visitors)?
- •
- Unique number of participants
- •
- Total number of visits including repeats
- •
- Not sure
Appendix C. List of TKC Member Organizations at the Time Each Survey Iteration Was Conducted
| 2019 | 2023 |
| 1440 Multiversity Barilla & Barilla Center for Food & Nutrition Foundation Boston Medical Center, Nutrition Resource Center’s Demonstration Kitchen and Preventive Food Pantry CancerScan (formerly Campus for H) Cleveland Clinic Compass Group, North America Dartmouth-Hitchcock Culinary Medical Program EHM Senior Solutions FamilyCook Productions Free Library of Philadelphia Culinary Literacy Center Google, Inc. Hackensack Meridian Health Harvard University Kaiser Permanente San Francisco Medical Center MaineGeneral Health Prevention and Healthy Living Medstar Health Northeastern Dining Northwell Health Northwestern University (Osher Center for Integrative Medicine) Oceania Cruises & Regent Seven Seas Cruises Palo Alto Medical Foundation Princeton University Providence Milwaukie Hospital Stanford University (Residential & Dining Enterprises) Turner Farm Inc. in collaboration with University of Cincinnati (Academic Health Center & College of Medicine, Center for Integrative Health and Wellness) University of California, Berkeley (College of Natural Resources; Health Services) University of California, Los Angeles (Chancellor Block’s Healthy Campus Initiative & UCLA Dining) University of California, San Francisco (Osher Center for Integrative Medicine) University of Michigan University of Minnesota (Center for Spirituality & Healing) University of New Hampshire University of Southern California (Keck School of Medicine) University of South Carolina School of Medicine Greenville University of Texas Health Science Center at Houston (UTHealth School of Public Health) University of Texas Medical Branch and Osher Lifelong Learning Institute, Galveston University of Vermont Medical Center Vanderbilt University Medical Center (Osher Center for Integrative Medicine and Center for Biomedical Ethics & Society) Veterans Health Administration Healthy Teaching Kitchen Program YMCA of Greater Pittsburgh-Sampson Family Branch | 1440 Multiversity Alberta Health Services/University of Calgary Apples to Zucchini Cooking School Banyan Barilla & Barilla Center for Food & Nutrition Foundation Bon Secours Richmond Boston Medical Center, Nutrition Resource Center’s Demonstration Kitchen and Preventive Food Pantry CancerScan Case Western Reserve University Children’s Healthcare of Atlanta Cincinnati Hills Christian Academy Cleveland Clinic Compass Group, North America Culinary Medicine Germany e.V. Dartmouth-Hitchcock Culinary Medical Program Emory University Lifestyle Medicine & Wellness FamilyCook Productions Free Library of Philadelphia Culinary Literacy Center Google, Inc. Griffin Health Hackensack Meridian Health Kaiser Permanente Bernard J. Tyson School of Medicine Kaiser Permanente San Francisco Medical Center MaineGeneral Health Prevention and Healthy Living Marshall University/Huntington Kitchen Medstar Health Moffitt Cancer Center Northeastern Dining Northwell Health Northwestern University (Osher Center for Integrative Medicine) Phipps Conservatory and Botanical Gardens Presbyterian Healthcare Services Providence Milwaukie Hospital Spartanburg Regional Healthcare System Spaulding Rehabilitation Network Turner Farm Inc. in collaboration with University of Cincinnati (Academic Health Center & College of Medicine, Center for Integrative Health and Wellness) University of British Columbia University of California, Berkeley (College of Natural Resources; Health Services) University of California, Irvine (Susan Samueli Integrative Health Institute) University of California, Los Angeles (Chancellor Block’s Healthy Campus Initiative & UCLA Dining) University of Minnesota (Center for Spirituality & Healing) University of South Alabama University of Southern California (Keck School of Medicine) University of Texas Health Science Center at Houston (UTHealth School of Public Health) (The Culinary Medicine Program at) University of Texas Southwestern University of Utah Center for Community Nutrition and Osher Center University of Vermont Medical Center Veterans Health Administration Healthy Teaching Kitchen Program YMCA of Greater Pittsburgh-Sampson Family Branch |
References
- Poor Nutrition. Available online: https://www.cdc.gov/chronicdisease/resources/publications/factsheets/nutrition.htm (accessed on 1 July 2023).
- Asher, R.C.; Shrewsbury, V.A.; Bucher, T.; Collins, C.E. Culinary medicine and culinary nutrition education for individuals with the capacity to influence health related behaviour change: A scoping review. J. Hum. Nutr. Diet. 2022, 35, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Irl, B.H.; Evert, A.; Fleming, A.; Gaudiani, L.M.; Guggenmos, K.J.; Kaufer, D.I.; McGill, J.B.; Verderese, C.A.; Martinez, J. Culinary Medicine: Advancing a Framework for Healthier Eating to Improve Chronic Disease Management and Prevention. Clin. Ther. 2019, 41, 2184–2198. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, D.M.; Pacheco, L.S.; McClure, A.C.; McWhorter, J.W.; Janisch, K.; Massa, J. Perspective: Teaching Kitchens: Conceptual Origins, Applications and Potential for Impact within Food Is Medicine Research. Nutrients 2023, 15, 2859. [Google Scholar] [PubMed]
- Fredericks, L.; Koch, P.A.; Liu, A.A.; Galitzdorfer, L.; Costa, A.; Utter, J. Experiential Features of Culinary Nutrition Education That Drive Behavior Change: Frameworks for Research and Practice. Health Promot. Pract. 2020, 21, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Russell, L.; Tse, J.; Bowie, J.; Richardson, C.; Trubek, A.; Maruthur, N.; Wolfson, J. Cooking Behaviours after Diabetes Prevention Program (DPP) Participation among DPP Participants in Baltimore, MD. Public Health Nutr. 2023, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Saxe-Custack, A.; Egan, S.; Sadler, R.; Wojciechowski, T. Relative impacts of a virtual cooking and nutrition program for children and families. Appetite 2023, 191, 107041. [Google Scholar] [CrossRef] [PubMed]
- Domper, J.; Gayoso, L.; Goni, L.; De la, O.V.; Etxeberria, U.; Ruiz-Canela, M. Culinary Medicine and Healthy Ageing: A Comprehensive Review. Nutr. Res. Rev. 2023, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Schneeberger, D.; Golubíc, M.; Moore, H.C.F.; Weiss, K.; Abraham, J.; Montero, A.; Doyle, J.; Sumego, M.; Roizen, M. Lifestyle Medicine-Focused Shared Medical Appointments to Improve Risk Factors for Chronic Diseases and Quality of Life in Breast Cancer Survivors. J. Altern. Complement. Med. 2019, 25, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.M.; Kaur, S.; Koo, H.C.; Mukhtar, F.; Yim, H.S. Culinary Nutrition Education Improves Home Food Availability and Psychosocial Factors Related to Healthy Meal Preparation Among Children. J. Nutr. Educ. Behav. 2022, 54, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Teaching Kitchen Research Conference Abstracts. Los Angeles, California. J. Integr. Complement. Med. 2023, 29, A1–A30. [Google Scholar]
- Tanumihardjo, J.P.; Davis, H.; Christensen, J.; Smith, R.A.; Kauffman-Smith, S.; Gunter, K.E. Hospital-Based, Community Teaching Kitchen Integrates Diabetes Education, Culinary Medicine, and Food Assistance: Case Study During the COVID-19 Pandemic. J. Gen. Intern. Med. 2023, 38 (Suppl. S1), 33–37. [Google Scholar] [CrossRef] [PubMed]
- McWhorter, J.W.; Danho, M.P.; LaRue, D.M.; Tseng, K.C.; Weston, S.R.; Moore, L.S.; Durand, C.; Hoelscher, D.M.; Sharma, S.V. Barriers and Facilitators of Implementing a Clinic-Integrated Food Prescription Plus Culinary Medicine Program in a Low-Income Food Insecure Population: A Qualitative Study. J. Acad. Nutr. Diet. 2022, 122, 1499–1513. [Google Scholar] [CrossRef] [PubMed]
- Nutrition and Obesity Policy Research and Evaluation Network (NOPREN). Supporting Food & Nutrition Security through Healthcare: A Resource for Healthcare Systems and Their Public Health and Community Partners; University of California, San Francisco: San Francisco, CA, USA, 2023; p. 19. [Google Scholar]
- Setting Up a Teaching Kitchen. Available online: https://u8l334.p3cdn1.secureserver.net/wp-content/uploads/2021/08/TKCFacility.pdf (accessed on 19 September 2023).
- Rajendran, I.; Weinstein, O.; Patel, P.; Lambert, P.; Quintiliani, L.M.; Hamburg, N. Virtual Teaching Kitchen: A Feasibility Study of a Nutrition Intervention for Patients With Food Insecurity and Metabolic Disease. Circulation 2021, 144 (Suppl. S1), A14044. [Google Scholar] [CrossRef]
- Razavi, A.C.; Latoff, A.; Dyer, A.; Albin, J.L.; Artz, K.; Babcock, A.; Cimino, F.; Daghigh, F.; Dollinger, B.; Fiellin, M.; et al. Virtual teaching kitchen classes and cardiovascular disease prevention counselling among medical trainees. BMJ Nutr. Prev. Health 2023, 6, e000477. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, O.; Donovan, K.; McCarthy, A.C.; Hiralall, L.; Allen, L.; Koh, W.; Apovian, C.M. Nourishing underserved populations despite scarcer resources: Adaptations of an urban safety net hospital during the COVID-19 pandemic. Am. J. Public Health 2021, 111, 663–666. [Google Scholar] [CrossRef] [PubMed]
- Massa, J.S. Teaching Kitchen Multisite Trial (TKMT). Identifier NCT05628649. Updated 11 September 2023. Available online: https://classic.clinicaltrials.gov/ct2/show/NCT05628649 (accessed on 17 September 2023).
- Culinary Nutrition Collaborative. Available online: https://www.culinarynutritioncollaborative.com/ (accessed on 24 August 2023).
- Health Meets Food. Available online: https://culinarymedicine.org/ (accessed on 24 August 2023).
- Food and Culinary Professionals. Available online: https://www.fcpdpg.org/home (accessed on 24 August 2023).
- Member Interest Groups. Available online: https://lifestylemedicine.org/member-interest-groups/ (accessed on 24 August 2023).
- Badaracco, C.; Faborode, O.; Mitchell, K.; Kazan, M. Payer Issues, Part 2: Health Plans’ Interventions to Address Food Insecurity. 2020. Available online: https://avalere.com/insights/payer-issues-part-2-health-plans-interventions-to-address-food-insecurity (accessed on 24 August 2023).
- Lynch, C.J. A Concept for Comprehensive Food is Medicine Networks or Centers of Excellence. Am. J. Clin. Nutr. 2023, 114, 10–12. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Badaracco, C.; Thomas, O.W.; Massa, J.; Bartlett, R.; Eisenberg, D.M. Characteristics of Current Teaching Kitchens: Findings from Recent Surveys of the Teaching Kitchen Collaborative. Nutrients 2023, 15, 4326. https://doi.org/10.3390/nu15204326
Badaracco C, Thomas OW, Massa J, Bartlett R, Eisenberg DM. Characteristics of Current Teaching Kitchens: Findings from Recent Surveys of the Teaching Kitchen Collaborative. Nutrients. 2023; 15(20):4326. https://doi.org/10.3390/nu15204326
Chicago/Turabian StyleBadaracco, Christina, Olivia W. Thomas, Jennifer Massa, Rachel Bartlett, and David M. Eisenberg. 2023. "Characteristics of Current Teaching Kitchens: Findings from Recent Surveys of the Teaching Kitchen Collaborative" Nutrients 15, no. 20: 4326. https://doi.org/10.3390/nu15204326




