Comparison of Effectiveness regarding a Culinary Medicine Elective for Medical Students in Germany Delivered Virtually versus In-Person
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Culinary Medicine Elective
2.4. Evaluation Tools
2.5. Data Collection and Analysis
2.6. Ethics Approval
3. Results
3.1. Participants
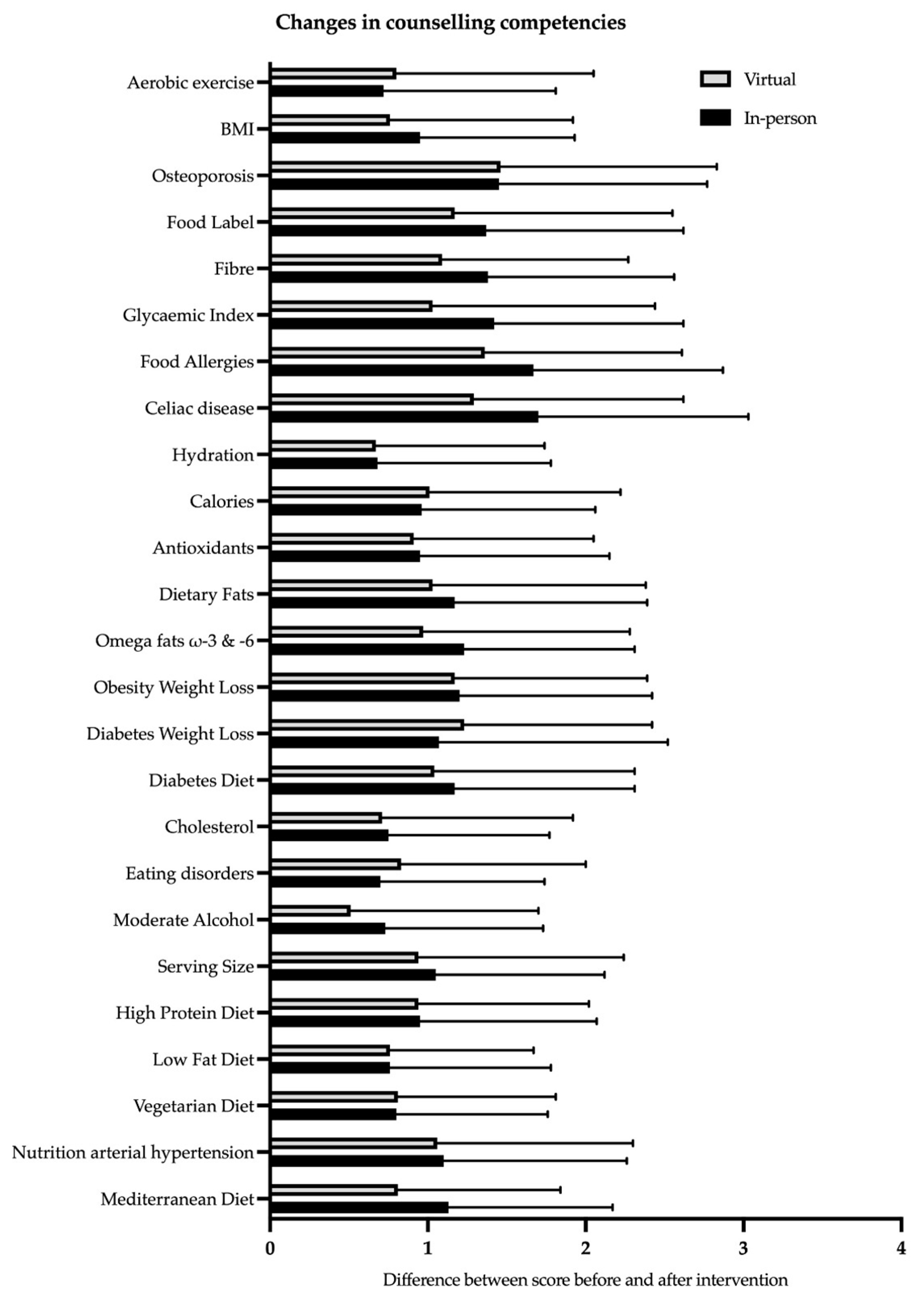
3.2. Counselling Competencies
3.3. Attitudes towards Nutrition Counselling in Medical Practice
3.4. Nutrition Knowledge
3.5. WHO-5 Well-Being Index
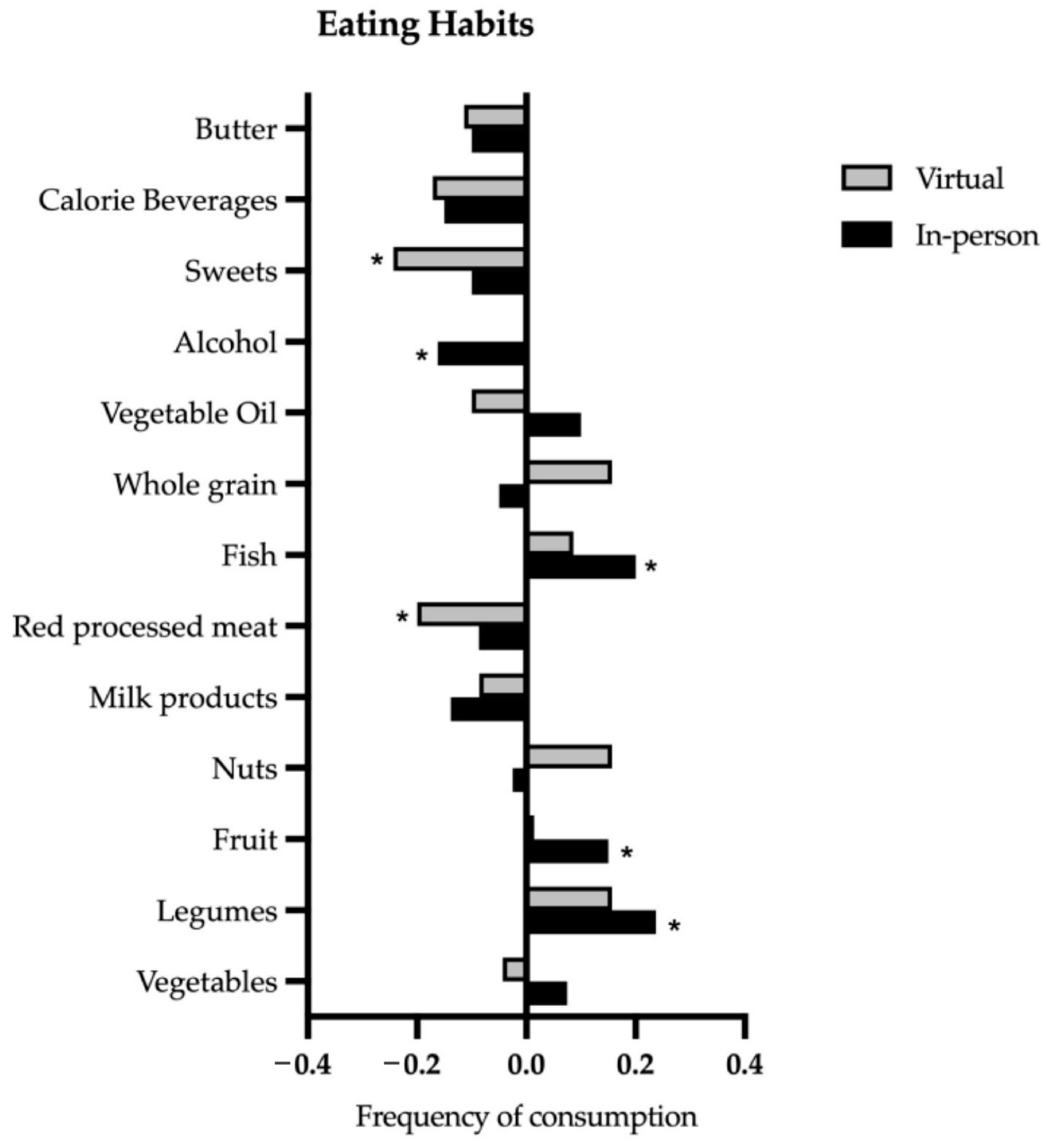
3.6. Eating Habits
4. Discussion
“Culinary medicine programs give medical students the experience necessary to translate nutrition knowledge learned in typical medical school curricula into practical advice. Culinary experiences allow medical students to provide their patients with individualized food and nutrition ideas that are easier to translate into actionable changes than the typical generalities of healthy eating imparted during many patient visits [21]”.
Limitations of the Study
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; GBD 2015 Obesity Collaborators; et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [PubMed]
- Mokdad, A.H.; Ballestros, K.; Echko, M.; Glenn, S.; Olsen, H.E.; Mullany, E.; Lee, A.; Khan, A.R.; Ahmadi, A.; US Burden of Disease Collaborators; et al. The State of US Health, 1990–2016: Burden of Diseases, Injuries, and Risk Factors Among US States. JAMA 2018, 319, 1444–1472. [Google Scholar] [PubMed]
- Devries, S. A global deficiency of nutrition education in physician training: The low hanging fruit in medicine remains on the vine. Lancet Planet Health 2019, 3, e371–e372. [Google Scholar] [CrossRef] [PubMed]
- Storz, M.A.; Oksche, A.; Schlasius-Ratter, U.; Schillings, V.; Beckschulte, K.; Huber, R. Nutrition Coverage in Medical Licensing Examinations in Germany: An Analysis of Six Nationwide Exams. Nutrients 2022, 14, 5333. [Google Scholar] [CrossRef] [PubMed]
- Kushner, R.F.; Sorensen, K.W. Lifestyle medicine: The future of chronic disease management. Curr. Opin. Endocrinol. Diabetes Obes. 2013, 20, 389–395. [Google Scholar] [CrossRef]
- Phillips, E.M.; Frates, E.P.; Park, D.J. Lifestyle Medicine. Phys. Med. Rehabil. Clin. N. Am. 2020, 31, 515–526. [Google Scholar] [CrossRef]
- Chung, M.; van Buul, V.J.; Wilms, E.; Nellessen, N.; Brouns, F.J. Nutrition education in European medical schools: Results of an international survey. Eur. J. Clin. Nutr. 2014, 68, 844–846. [Google Scholar] [CrossRef]
- Blunt, S.B.; Kafatos, A. Clinical Nutrition Education of Doctors and Medical Students: Solving the Catch 22. Adv. Nutr. 2019, 10, 345–350. [Google Scholar] [CrossRef]
- Sierpina, V.S.; Welch, K.; Devries, S.; Eisenberg, D.; Levine, L.; McKee, J.; Dalal, M.; Mendoza, P.; Gutierrez, J.; Robertson, S.; et al. What Competencies Should Medical Students Attain in Nutritional Medicine? Explore 2016, 12, 146–147. [Google Scholar] [CrossRef]
- Kahan, S.; Manson, J.E. Nutrition Counseling in Clinical Practice: How Clinicians Can Do Better. JAMA 2017, 318, 1101–1102. [Google Scholar] [CrossRef]
- Weinstein, O.; McManus, C.R.; Badaracco, C.; MacLaren, J.; Mason, A.; McWhorter, J.W. Registered Dietitian Nutritionists Taking the Lead in Teaching Kitchens. J. Acad. Nutr. Diet. 2023, 123, 1393–1405. [Google Scholar]
- Razavi, A.C.; Latoff, A.; Dyer, A.; Albin, J.L.; Artz, K.; Babcock, A.; Cimino, F.; Daghigh, F.; Dollinger, B.; Fiellin, M.; et al. Virtual teaching kitchen classes and cardiovascular disease prevention counselling among medical trainees. BMJ Nutr. Prev. Health 2023, 6, 6–13. [Google Scholar] [CrossRef] [PubMed]
- La Puma, J. What Is Culinary Medicine and What Does It Do? Popul. Health Manag. 2016, 19, 1–3. [Google Scholar] [CrossRef]
- Eisenberg, D.M.; Imamura, B.A. Teaching Kitchens in the Learning and Work Environments: The Future Is Now. Glob. Adv. Health Med. 2020, 9, 2164956120962442. [Google Scholar] [PubMed]
- Eisenberg, D.M.; Pacheco, L.S.; McClure, A.C.; McWhorter, J.W.; Janisch, K.; Massa, J. Perspective: Teaching Kitchens: Conceptual Origins, Applications and Potential for Impact within Food Is Medicine Research. Nutrients 2023, 15, 2859. [Google Scholar] [CrossRef] [PubMed]
- Health Meets Food: The Culinary Medicine Curriculum. Available online: https://culinarymedicine.org (accessed on 24 August 2023).
- Hauser, M.E.; Nordgren, J.R.; Adam, M.; Gardner, C.D.; Rydel, T.; Bever, A.M.; Steinberg, E. The First, Comprehensive, Open-Source Culinary Medicine Curriculum for Health Professional Training Programs: A Global Reach. Am. J. Lifestyle Med. 2020, 14, 369–373. [Google Scholar] [CrossRef]
- Neumann, U. Cooking Courses in Higher Education: A Method to Foster Education for Sustainable Development and Promoting Sustainable Development Goals. In Handbook of Sustainability Science and Research; World Sustainability Series; Springer: Cham, Switzerland, 2018. [Google Scholar] [CrossRef]
- Ellrott, T.; Neumann, U. Innovation for Medical Studies: Culinary Medicine Piloted as a Compulsory Elective Subject at Göttingen University Medical Center. Available online: https://idw-online.de/de/news759813 (accessed on 24 August 2023).
- Razavi, A.C.; Monlezun, D.J.; Sapin, A.; Stauber, Z.; Schradle, K.; Schlag, E.; Dyer, A.; Gagen, B.; McCormack, I.G.; Akhiwu, O.; et al. Multisite Culinary Medicine Curriculum Is Associated With Cardioprotective Dietary Patterns and Lifestyle Medicine Competencies Among Medical Trainees. Am. J. Lifestyle Med. 2020, 14, 225–233. [Google Scholar] [CrossRef]
- Newman, C.; Yan, J.; Messiah, S.E.; Albin, J. Culinary Medicine as Innovative Nutrition Education for Medical Students: A Scoping Review. Acad. Med. 2023, 98, 274–286. [Google Scholar]
- Hauner, H.; Beyer-Reiners, E.; Bischoff, G.; Breidenassel, C.; Ferschke, M.; Gebhardt, A.; Holzapfel, C.; Lambeck, A.; Meteling-Eeken, M.; Paul, C.; et al. Leitfaden für Ernährungstherapie in Klinik und Praxis. Akutelle Ernährungsmedizin 2019, 44, 384–419. [Google Scholar]
- DGE-Ernährungsempfehlungen. 10 Rules of Healthy Nutrition by DGE. Available online: https://www.dge.de/gesunde-ernaehrung/dge-ernaehrungsempfehlungen/10-regeln/ (accessed on 24 August 2023).
- Ferguson, C.J. An Effect Size Primer: A Guide for Clinicians and Researchers. Prof. Psychol. Res. Pract. 2009, 40, 532–538. [Google Scholar] [CrossRef]
- Jaroudi, S.S.; Sessions, W.S., 2nd; Wang, V.S.; Shriver, J.L.; Helekar, A.S.; Santucci, M.; Cole, L.; Ruiz, J.; Fackrell, J.; Chauncey, K. Impact of culinary medicine elective on medical students’ culinary knowledge and skills. Proc. Bayl. Univ. Med. Cent. 2018, 31, 439–442. [Google Scholar] [CrossRef]
- Pang, B.; Memel, Z.; Diamant, C.; Clarke, E.; Chou, S.; Gregory, H. Culinary medicine and community partnership: Hands-on culinary skills training to empower medical students to provide patient-centered nutrition education. Med. Educ. Online 2019, 24, 1630238. [Google Scholar] [CrossRef] [PubMed]
- Rothman, J.M.; Bilici, N.; Mergler, B.; Schumacher, R.; Mataraza-Desmond, T.; Booth, M.; Olshan, M.; Bailey, M.; Mascarenhas, M.; Duffy, W.; et al. A Culinary Medicine Elective for Clinically Experienced Medical Students: A Pilot Study. J. Altern. Complement Med. 2020, 26, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Wattick, R.A.; Saurborn, E.G.; Olfert, M.D. Impact of a Brief Culinary Medicine Elective on Medical Students’ Nutrition Knowledge, Self-efficacy, and Attitudes. Med. Sci. Educ. 2022, 32, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Magallanes, E.; Sen, A.; Siler, M.; Albin, J. Nutrition from the kitchen: Culinary medicine impacts students’ counseling confidence. BMC Med. Educ. 2021, 21, 88. [Google Scholar]
- Wechsler, J.G. Lehrstühle Ernährungsmedizin. Akutelle Ernährungsmedizin 2023, 48, 139–156. [Google Scholar]
- Mogre, V.; Stevens, F.C.J.; Aryee, P.A.; Amalba, A.; Scherpbier, A. Future doctors’ perspectives on health professionals’ responsibility regarding nutrition care and why doctors should learn about nutrition: A qualitative study. Educ. Health 2019, 32, 91–94. [Google Scholar] [CrossRef]
- Conroy, M.B.; Delichatsios, H.K.; Hafler, J.P.; Rigotti, N.A. Impact of a preventive medicine and nutrition curriculum for medical students. Am. J. Prev. Med. 2004, 27, 77–80. [Google Scholar] [CrossRef]
- Helbach, A.; Dumm, M.; Moll, K.; Bottrich, T.; Leineweber, C.G.; Mueller, W.; Matthes, J.; Polidori, M.C. Improvement of Dietary Habits among German Medical Students by Attending a Nationwide Online Lecture Series on Nutrition and Planetary Health (“Eat This!”). Nutrients 2023, 15, 580. [Google Scholar]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- Cancello, R.; Soranna, D.; Zambra, G.; Zambon, A.; Invitti, C. Determinants of the Lifestyle Changes during COVID-19 Pandemic in the Residents of Northern Italy. Int. J. Environ. Res. Public Health 2020, 17, 6287. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Parmenter, K.; Waller, J. Nutrition knowledge and food intake. Appetite 2000, 34, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Topp, C.W.; Ostergaard, S.D.; Sondergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother Psychosom 2015, 84, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Reeves, S.; Pelone, F.; Harrison, R.; Goldman, J.; Zwarenstein, M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2017, 6, CD000072. [Google Scholar] [PubMed]
- Kaiser, L.; Conrad, S.; Neugebauer, E.A.M.; Pietsch, B.; Pieper, D. Interprofessional collaboration and patient-reported outcomes in inpatient care: A systematic review. Syst. Rev. 2022, 11, 169. [Google Scholar] [CrossRef]
| Virtual (Full Hours) | In-Person (Full Hours) | |
|---|---|---|
| Planning session | 1 | 1 |
| 7 × shopping for groceries | 3.5 | - |
| 7 × preparing home kitchen | 3.5 | - |
| Setting up digital equipment in home kitchen (one time) | 1 | - |
| 7 modules at 3 h each, virtual | 21 | - |
| 7 modules at 3 h each, in-person | - | 21 |
| 7 × cleaning home kitchen | 3.5 | - |
| 7 × cleaning teaching kitchen | - | 3.5 |
| Mandatory case report | 3.5 | 3.5 |
| Total | 37 | 29 |
| Participant Demographics | Virtual Cohort | In-Person Cohort | p-Value |
|---|---|---|---|
| Mean age (years ± SD) | 24.3 (±6.7) | 24.5 (±6.53) | 0.55 |
| Female/male/other (n) | 57/13/0 | 57/23/0 | 0.147/0.147/- |
| Mean semester (±SD) | 6.3 (±5.3) | 6.26 (±4.26) | 0.826 |
| Completed professional training before starting medical studies (n) | 29 | 31 | 0.998 |
| Completed academic degree before starting medical studies (n) | 5 | 8 | 0.556 |
| City: Göttingen (n) | 42 (60%) | 22 (40.1%) | <0.001 |
| City: Gießen (n) | 12 (22.9%) | 32 (27.5%) | 0.002 |
| City: Brandenburg (n) | 16 (17.1%) | 26 (32.5%) | 0.085 |
| N (total) | 70 | 80 |
| Topic | Before-Virtual M (SD) | After-Virtual M (SD) | Before-In-Person M (SD) | After-In-Person M (SD) | Virtual MD (SD) | In-Person MD (SD) |
|---|---|---|---|---|---|---|
| Mediterranean diet | 3.41 (1.08) | 4.23 (0.66) | 3.18 (1.15) | 4.3 (0.64) | 0.81 (1.03) * | 1.13 (1.04) * |
| Arterial hypertension diet | 3.07 (1.21) | 4.13 (0.74) | 3.26 (1.09) | 4.36 (0.57) | 1.06 (1.24) * | 1.1 (1.16) * |
| Vegetarian diet | 3.60 (0.92) | 4.41 (0.67) | 3.54 (1.09) | 4.34 (0.71) | 0.81 (1.00) * | 0.8 (0.96) * |
| Low-fat diet | 3.37 (0.98) | 4.13 (0.64) | 3.43 (0.99) | 4.19 (0.73) | 0.76 (0.91) * | 0.76 (1.02) * |
| High-protein diet | 3.09 (1.02) | 4.03 (0.72) | 3.23 (1.06) | 4.18 (0.67) | 0.94 (1.08) * | 0.95 (1.12) * |
| Serving size | 3.06 (1.17) | 4.00 (0.85) | 2.9 (1.15) | 3.95(0.72) | 0.94 (1.30) * | 1.05 (1.07) * |
| Moderate alcohol | 3.71 (0.92) | 4.23 (0.75) | 3.70 (1.07) | 4.44 (0.65) | 0.51 (1.19) * | 0.73 (1.00) * |
| Eating disorders | 3.27 (1.12) | 4.10 (0.80) | 3.4 (1.05) | 4.1 (0.73) | 0.83 (1.17) * | 0.7 (1.04) * |
| Cholesterol | 3.30 (1.12) | 4.01 (0.84) | 3.19 (1.08) | 3.94 (0.73) | 0.71 (1.21) * | 0.75 (1.02) * |
| Diabetes diet | 3.22 (1.13) | 4.27 (0.80) | 3.04 (1.16) | 4.21 (0.61) | 1.04 (1.27) * | 1.17 (1.14) * |
| Diabetes weight loss | 3.14 (1.27) | 4.37 (0.73) | 3.29 (1.13) | 4.36 (0.68) | 1.23 (1.19) * | 1.07 (1.45) * |
| Obesity weight loss | 3.23 (1.13) | 4.40 (0.67) | 3.23 (1.18) | 4.43 (0.63) | 1.17 (1.22) * | 1.20 (1.22) * |
| Omega fats ω-3 and -6 | 2.76 (1.26) | 3.73 (0.82) | 2.56 (1.15) | 3.8 (0.84) | 0.97 (1.31) * | 1.23 (1.08) * |
| Dietary fats | 2.84 (1.20) | 3.87 (0.90) | 2.65 (1.13) | 3.83 (0.79) | 1.03 (1.35) * | 1.17 (1.22) * |
| Antioxidants | 2.76 (1.13) | 3.67 (0.94) | 2.6 (1.15) | 3.55 (0.89) | 0.91 (1.14) * | 0.95 (1.2) * |
| Calories | 2.90 (1.23) | 3.91 (0.81) | 2.96 (1.14) | 3.93 (0.89) | 1.01 (1.21) * | 0.96 (1.10) * |
| Hydration | 3.6 (0.95) | 4.27 (0.68) | 3.7 (1.01) | 4.43 (0.65) | 0.67 (1.07) * | 0.68 (1.10) * |
| Celiac disease | 2.57 (1.23) | 3.86 (0.86) | 2.49 (1.28) | 4.19 (0.79) | 1.29 (1.33) * | 1.7 (1.33) * |
| Food allergies | 2.37 (1.12) | 3.73 (0.78) | 2.26 (1.12) | 3.94 (0.78) | 1.36 (1.25) * | 1.67 (1.20) * |
| Glycaemic index | 2.53 (1.28) | 3.56 (0.97) | 2.24 (1.16) | 3.65 (0.87) | 1.03 (1.41) * | 1.42 (1.2) * |
| Fibre | 3.11 (1.23) | 4.20 (0.71) | 2.9 (1.18) | 4.29 (0.71) | 1.09 (1.18) * | 1.38 (1.18) * |
| Food label | 2.87 (1.21) | 4.04 (0.86) | 2.79 (1.33) | 4.16 (0.70) | 1.17 (1.38) * | 1.37 (1.25) * |
| Osteoporosis | 2.40 (1.22) | 3.86 (0.84) | 2.44 (1.27) | 3.89 (0.74) | 1.46 (1.37) * | 1.45 (1.32) * |
| BMI | 3.61 (1.01) | 4.37 (0.85) | 3.60 (0.97) | 4.55 (0.59) | 0.76 (1.16) * | 0.95 (0.98) * |
| Aerobic exercise | 3.49 (1.14) | 4.29 (0.84) | 4.53 (1.1) | 4.25 (0.75) | 0.80 (1.25) * | 0.72 (1.09) * |
| Overall | 3.09 (1.13) | 4.06 (0.78) | 3.08 (1.17) | 4.14 (0.72) | 0.97 (1.20) | 1.05 (1.13) |
| Question | Before-Virtual M (SD) | After-Virtual M (SD) | Virtual MD (SD) | Before- In-Person M (SD) | After- In-Person M (SD) | In-Person MD (SD) |
|---|---|---|---|---|---|---|
| Nutrition counselling should be routine | 4.36 (0.68) | 4.56 (0.63) | 0.2 (0.60) * | 4.36 (0.815) | 4.59 (0.650) | 0.22 (0.94) * |
| Specific counselling can improve patients’ diet | 4.76 (0.49) | 4.86 (0.39) | 0.1 (0.35) * | 4.61 (0.72) | 4.84 (0.37) | 0.22 (0.71) * |
| Physicians’ counselling can improve patients’ diets | 4.24 (0.79) | 4.57 (0.65) | 0.33 (0.76) * | 4.38 (0.83) | 4.74 (0.54) | 0.36 (0.76) * |
| M of Right-Answering Participants before Virtual (%) | M of Right-Answering Participants after Virtual (%) | M of Right-Answering Participants before In-Person (%) | M of Right-Answering Participants after In-Person (%) | Virtual MD | In-Person MD | |
|---|---|---|---|---|---|---|
| 1. Recommended diet form | 74.3 | 97.1 | 71.3 | 92.5 | 22.8 * | 21.3 * |
| 2. Carbohydrate percentage | 31.4 | 84.3 | 38.8 | 61.3 | 52.9 * | 22.5 * |
| 3. Salt | 34.3 | 81.4 | 25.0 | 61.3 | 47.1 * | 36.3 * |
| 4. Free sugars | 62.9 | 70.0 | 56.3 | 76.3 | 7.1 | 20.0 * |
| 5. Recommended protein | 47.1 | 74.3 | 48.8 | 85.0 | 27.2 * | 36.2 * |
| 6. Malnutrition syndrome | 58.6 | 81.4 | 65.0 | 85.0 | 22.8 * | 20.0 * |
| 7. Therapy obesity | 81.4 | 91.4 | 68.8 | 86.3 | 10.0 * | 17.5 * |
| 8. Gout | 62.9 | 77.1 | 67.5 | 66.3 | 14.2 * | -1.2 |
| 9. Monosaccharide gout | 30.0 | 71.4 | 25.0 | 51.2 | 41.4 * | 26.2 * |
| 10. Dyslipoproteinemia | 50.0 | 44.3 | 26.3 | 28.7 | −5.7 | 2.4 |
| 11. Cereals for celiac disease | 51.4 | 84.3 | 55.4 | 73.8 | 32.9 * | 18.4 * |
| 12. Chronic kidney disease therapy | 58.6 | 68.6 | 56.3 | 61.3 | 10.0 | 5.0 |
| 13. Calcium oxalate stones | 21.4 | 51.4 | 17.5 | 51.2 | 30.0 * | 33.7 * |
| 14. Fructose malabsorption | 35.7 | 74.3 | 37.5 | 53.8 | 38.6 * | 16.3 * |
| 15. Omega-3 fatty acid | 60.0 | 78.6 | 46.3 | 72.5 | 28.6 * | 26.2 * |
| 16. Calcium and Vitamin D | 34.3 | 45.7 | 33.8 | 36.3 | 11.4 | 2.5 |
| Overall | 49.6 | 73.5 | 46.2 | 65.17 | 23.8 | 18.9 |
| Before-Virtual M (SD) | After-Virtual M (SD) | Virtual MD (SD) | Before-In-Person M (SD) | After-In-Person M (SD) | In-Person MD (SD) | |
|---|---|---|---|---|---|---|
| Favourable foods | 24.4 (4.07) | 22.09 (3.83) | 1.50 (3.09) * | 20.83 (3.83) | 21.52 (3.52) | −0.68 (3.37) |
| Unfavourable foods | 10.72 (2.80) | 10.0 (2.54) | 0.72 (1.76) * | 10.48 (2.79) | 9.88 (2.21) | 0.6 (1.76) * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Böttcher, S.; Schonebeck, L.J.; Drösch, L.; Plogmann, A.M.; Leineweber, C.G.; Puderbach, S.; Buhre, C.; Schmöcker, C.; Neumann, U.; Ellrott, T. Comparison of Effectiveness regarding a Culinary Medicine Elective for Medical Students in Germany Delivered Virtually versus In-Person. Nutrients 2023, 15, 4281. https://doi.org/10.3390/nu15194281
Böttcher S, Schonebeck LJ, Drösch L, Plogmann AM, Leineweber CG, Puderbach S, Buhre C, Schmöcker C, Neumann U, Ellrott T. Comparison of Effectiveness regarding a Culinary Medicine Elective for Medical Students in Germany Delivered Virtually versus In-Person. Nutrients. 2023; 15(19):4281. https://doi.org/10.3390/nu15194281
Chicago/Turabian StyleBöttcher, Selina, Louisa Josefa Schonebeck, Laura Drösch, Anna Manuela Plogmann, Can Gero Leineweber, Seraphina Puderbach, Charlotte Buhre, Christoph Schmöcker, Uwe Neumann, and Thomas Ellrott. 2023. "Comparison of Effectiveness regarding a Culinary Medicine Elective for Medical Students in Germany Delivered Virtually versus In-Person" Nutrients 15, no. 19: 4281. https://doi.org/10.3390/nu15194281
APA StyleBöttcher, S., Schonebeck, L. J., Drösch, L., Plogmann, A. M., Leineweber, C. G., Puderbach, S., Buhre, C., Schmöcker, C., Neumann, U., & Ellrott, T. (2023). Comparison of Effectiveness regarding a Culinary Medicine Elective for Medical Students in Germany Delivered Virtually versus In-Person. Nutrients, 15(19), 4281. https://doi.org/10.3390/nu15194281






