Susceptibility to COVID-19 Nutrition Misinformation and Eating Behavior Change during Lockdowns: An International Web-Based Survey
Highlights
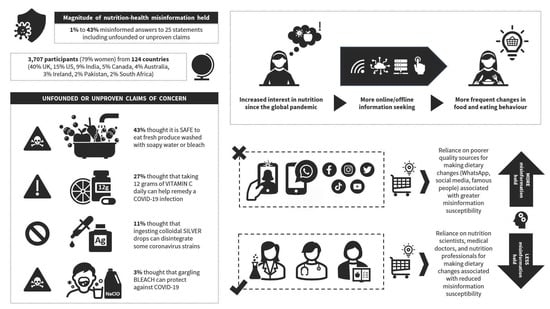
- This study identified significant nutrition health misinformation during the early COVID-19 lockdowns, with up to 43% of participants endorsing potentially harmful practices, such as washing produce with soap or bleach.
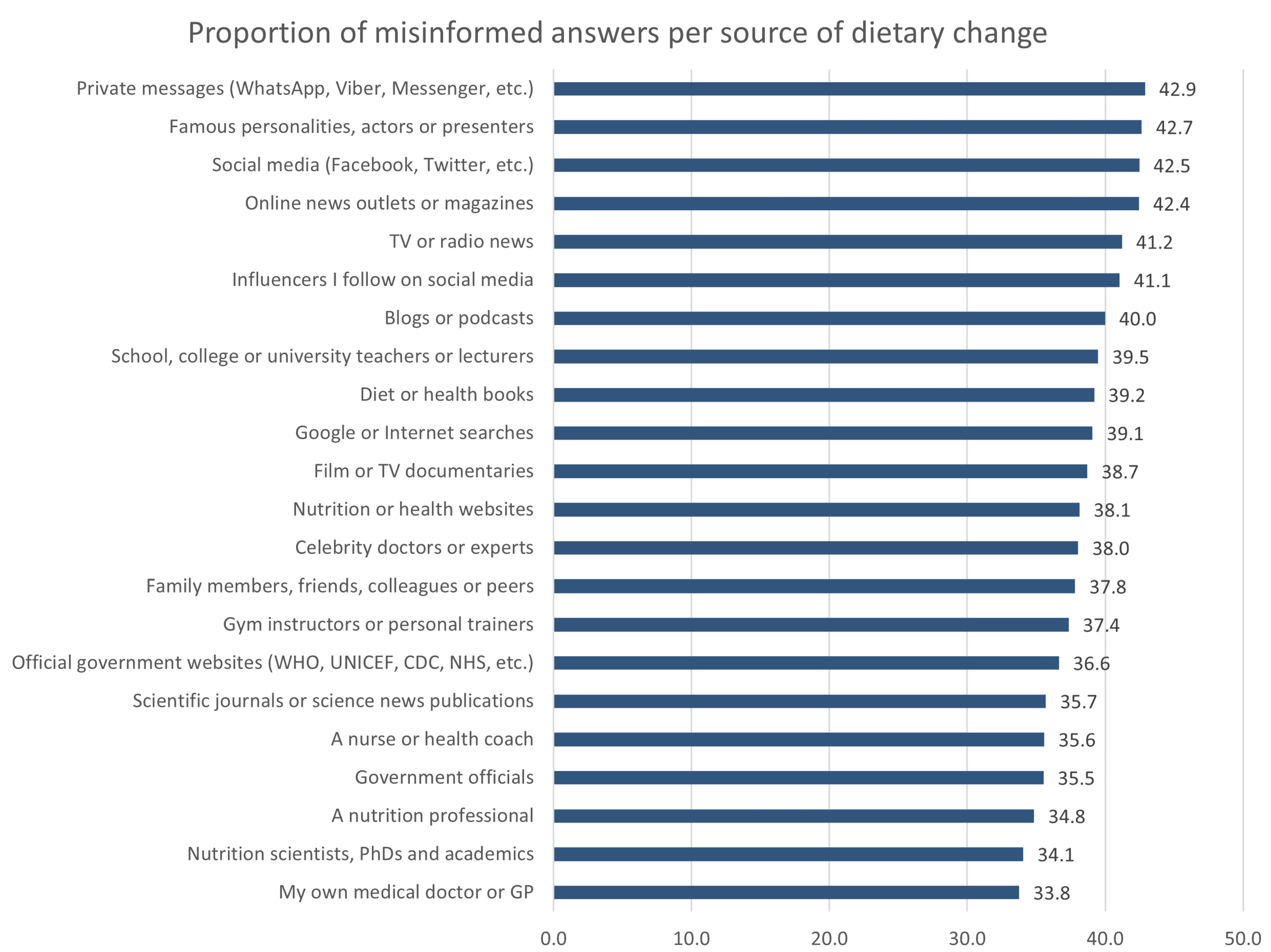
- Participants relying on lower-quality sources like WhatsApp, social media, and famous personalities were more misinformed, whereas those consulting nutrition scientists/professionals and medical doctors demonstrated better discernment.
- The increased interest in nutrition since the onset of the pandemic, reported by 56% of the participants, correlated with more frequent dietary changes influenced by both high- and poor-quality information sources, heightening the risk of harmful health behaviors.
- The findings highlight the urgent need for public health education initiatives to counteract health-threatening misinformation and promote the use of science-based quality sources, especially during global health crises.
Abstract
1. Introduction
- The respondents’ views about certain substances, foods, nutrients, dietary approaches, and health practices in relation to the transmission, infection, protection, or treatment of COVID-19 (i.e., nutrition-health misinformation discernment).
- The self-reported influence of different interpersonal and generic sources of diet and nutrition information or advice on the frequency of changes in food and eating behaviors (i.e., reliance on an information source for making dietary changes).
- Trends in online information seeking and dietary change frequency amongst respondents whose interest in nutrition increased since the pandemic, compared to those whose interest did not increase (i.e., interest in nutrition, online information seeking, and dietary changes).
- The relationship between the use of information sources of varying quality for changing eating behavior and the proportion of misinformed views about food, diet, nutrition, and health practices concerning COVID-19 during the first-wave of lockdowns around the world (i.e., nutrition-health misinformation susceptibility when relying on lower versus higher quality sources for changing diet).
2. Materials and Methods
2.1. Study Design and Population
2.2. Ethical Considerations
2.3. Instrument Measures and Outcomes
2.3.1. General Demographics and Characteristics
2.3.2. Views about Food, Eating, and Health Practices Related to COVID-19
2.3.3. Eating Behavior Change Frequency per Information Source
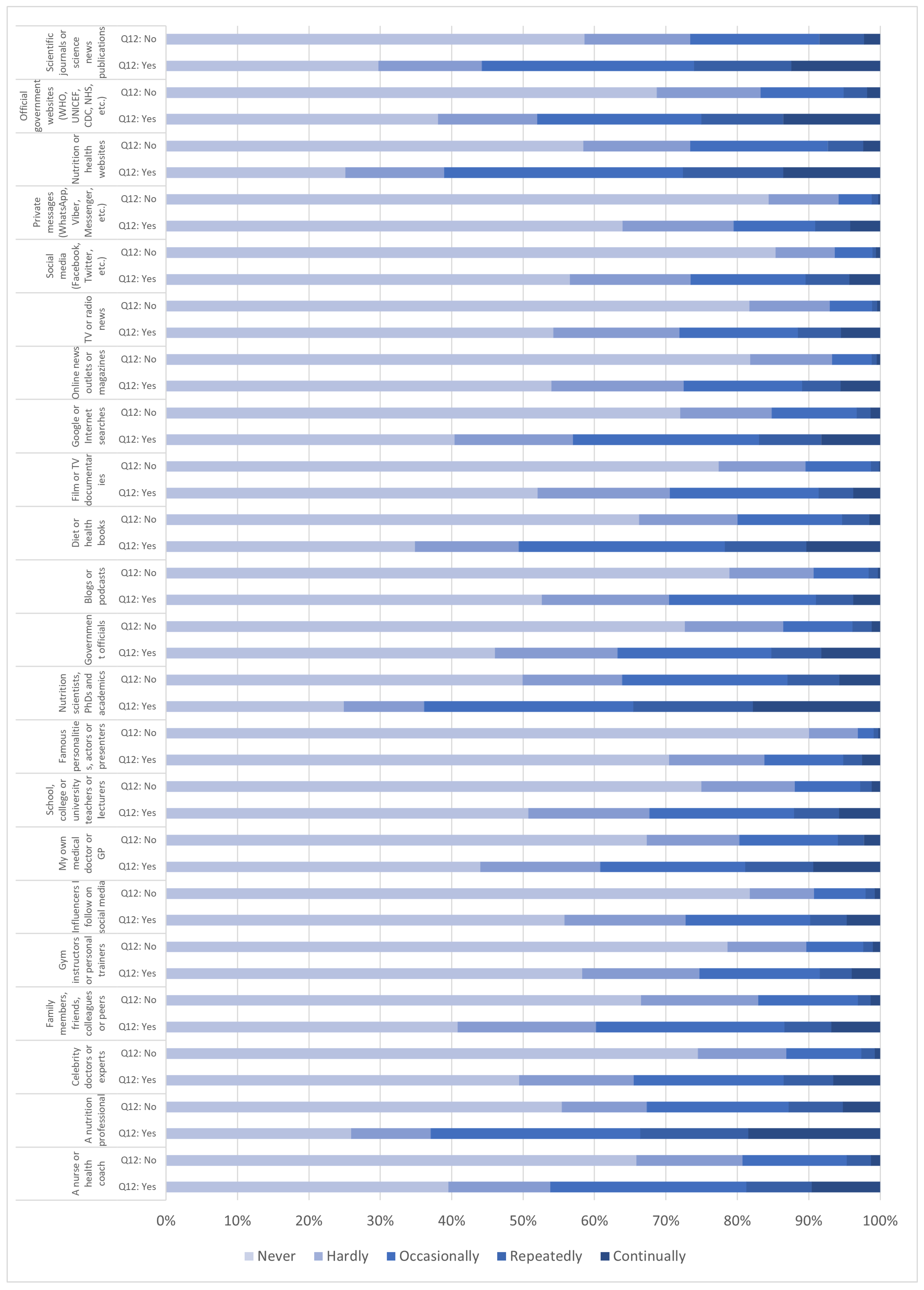
- Eleven of these sources were interpersonal (individuals such as one’s medical doctor or GP, nutrition professionals, government officials, influencers followed on social media, family members, friends, colleagues, or peers).
- The other 11 were general sources of nutrition information or dietary advice (such as Google or Internet searches, Facebook, Twitter, and other social media, WhatsApp, Viber, Messenger, or other kinds of private messages, WHO, UNICEF, CDC, NHS, or other official government websites).
- Possible sources were listed in a randomly rotated order for each participant within a matrix-style question asking: “Since the COVID-19 outbreak, have you changed the way you eat or what you eat based on nutrition information/dietary advice from the following sources?”
2.4. Statistical Analysis
3. Results
3.1. Misinformed Views about Food, Eating, and Health Practices Related to COVID-19
3.2. Eating Behavior Change Frequency per Information Source
Increased Interest in Nutrition and Subsequent Dietary Change
3.3. Proportion of Misinformed Views per Information Source for Dietary Changes
4. Discussion
4.1. Magnitude of COVID-19 Nutrition and Health Misinformation Held
4.2. Influence of Different Information Sources on Eating Behavior Changes
4.3. Dietary Changes Based on Information from Lower Quality Sources
4.4. Interest in Nutrition, Online Information Seeking, and Dietary Changes
4.5. Greater Misinformation Susceptibility when Relying on Lower Quality Sources for Changing Diet
4.6. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Do Nascimento, I.J.B.; Pizarro, A.B.; Almeida, J.M.; Azzopardi-Muscat, N.; Gonçalves, M.A.; Björklund, M.; Novillo-Ortiz, D. Infodemics and Health Misinformation: A Systematic Review of Reviews. Bull. World Health Organ. 2022, 100, 544. [Google Scholar] [CrossRef] [PubMed]
- Nicomedes, C.J.C.; Avila, R.M.A. An Analysis on the Panic during COVID-19 Pandemic through an Online Form. J. Affect. Disord. 2020, 276, 14. [Google Scholar] [CrossRef] [PubMed]
- Che Abdul Rahim, N.; Manjit Singh, J.S.; Pardi, M.; Zainuddin, A.A.; Salleh, R. Analysis of Available Nutrition Recommendations to Combat COVID-19: A Scoping Review. Malays. J. Med. Sci. 2021, 28, 18. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Medical Product Alert N°3/2020: Falsified Medical Products That Claim to Prevent, Detect, Treat or Cure COVID-19. Available online: https://www.who.int/news/item/31-03-2020-medical-product-alert-n-3-2020 (accessed on 14 December 2022).
- Bin Naeem, S.; Bhatti, R.; Khan, A. An Exploration of How Fake News Is Taking over Social Media and Putting Public Health at Risk. Health Info. Libr. J. 2021, 38, 143. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Sarkar, T.; Khan, S.H.; Kamal, A.H.M.; Murshid Hasan, S.M.; Kabir, A.; Yeasmin, D.; Islam, M.A.; Chowdhury, K.I.A.; Anwar, K.S.; et al. COVID-19-Related Infodemic and Its Impact on Public Health: A Global Social Media Analysis. Am. J. Trop. Med. Hyg. 2020, 103, 1621–1629. [Google Scholar] [CrossRef]
- President Trump Claims Injecting People with Disinfectant Could Treat Coronavirus—YouTube. Available online: https://www.youtube.com/watch?v=33QdTOyXz3w (accessed on 14 December 2022).
- Fernández: “The WHO Recommends Drinking Hot Beverages” | Coronavirus. Available online: https://chequeado.com/ultimas-noticias/alberto-fernandez-la-organizacion-mundial-de-la-salud-entre-las-cosas-que-recomienda-es-que-uno-tome-muchas-bebidas-calientes-porque-el-calor-mata-el-virus/ (accessed on 14 December 2022).
- OSG. Confronting Health Misinformation; US Department of Health and Human Services: Washington, DC, USA, 2021; pp. 1–22. [Google Scholar]
- Pan American Health Organization. Understanding the Infodemic and Misinformation in the Fight against COVID-19—PAHO/WHO. Available online: https://www.paho.org/en/documents/understanding-infodemic-and-misinformation-fight-against-covid-19 (accessed on 14 December 2022).
- World Health Organization. Novel Coronavirus (2019-NCoV): Situation Report, 13. Available online: https://apps.who.int/iris/handle/10665/330778 (accessed on 14 December 2022).
- Van der Linden, S. Misinformation: Susceptibility, Spread, and Interventions to Immunize the Public. Nat. Med. 2022, 28, 460–467. [Google Scholar] [CrossRef]
- Gharpure, R.; Hunter, C.M.; Schnall, A.H.; Barrett, C.E.; Kirby, A.E.; Kunz, J.; Berling, K.; Mercante, J.W.; Murphy, J.L.; Garcia-Williams, A.G. Knowledge and Practices Regarding Safe Household Cleaning and Disinfection for COVID-19 Prevention—United States, May 2020. MMWR. Morb. Mortal. Wkly. Rep. 2022, 69, 705–709. [Google Scholar] [CrossRef]
- Hassanian-Moghaddam, H.; Zamani, N.; Kolahi, A.A.; McDonald, R.; Hovda, K.E. Double Trouble: Methanol Outbreak in the Wake of the COVID-19 Pandemic in Iran—A Cross-Sectional Assessment. Crit. Care 2020, 24, 1–3. [Google Scholar] [CrossRef]
- Al-Zaman, M.S. Prevalence and Source Analysis of COVID-19 Misinformation in 138 Countries. IFLA J. 2022, 48, 189–204. [Google Scholar] [CrossRef]
- Coronavirus: Half of Humanity Now on Lockdown as 90 Countries Call for Confinement | Euronews. Available online: https://www.euronews.com/2020/04/02/coronavirus-in-europe-spain-s-death-toll-hits-10-000-after-record-950-new-deaths-in-24-hou (accessed on 14 December 2022).
- Mertens, G.; Gerritsen, L.; Duijndam, S.; Salemink, E.; Engelhard, I.M. Fear of the Coronavirus (COVID-19): Predictors in an Online Study Conducted in March 2020. J. Anxiety Disord. 2020, 74, 102258. [Google Scholar] [CrossRef]
- World Health Organization. WHO Statement on Cases of COVID-19 Surpassing 100,000. Available online: https://www.who.int/news/item/07-03-2020-who-statement-on-cases-of-covid-19-surpassing-100-000 (accessed on 14 December 2022).
- Li, H.; Liu, S.M.; Yu, X.H.; Tang, S.L.; Tang, C.K. Coronavirus Disease 2019 (COVID-19): Current Status and Future Perspectives. Int. J. Antimicrob. Agents 2020, 55, 105951. [Google Scholar] [CrossRef]
- World Health Organization. Public Statement for Collaboration on COVID-19 Vaccine Development. Available online: https://www.who.int/news/item/13-04-2020-public-statement-for-collaboration-on-covid-19-vaccine-development (accessed on 14 December 2022).
- The Health Sciences Academy. Available online: https://thehealthsciencesacademy.org/ (accessed on 14 December 2022).
- Tagliabue, F.; Galassi, L.; Mariani, P. The “Pandemic” of Disinformation in COVID-19. Sn Compr. Clin. Med. 2020, 2, 1287. [Google Scholar] [CrossRef]
- Florença, S.G.; Ferreira, M.; Lacerda, I.; Maia, A.; Varzakas, T.; Raposo, A.; Braz, R.; Botelho, A.; Zandonadi, R.P. Food Myths or Food Facts? Study about Perceptions and Knowledge in a Portuguese Sample. Foods 2021, 10, 2746. [Google Scholar] [CrossRef]
- Geldsetzer, P. Use of Rapid Online Surveys to Assess People’s Perceptions During Infectious Disease Outbreaks: A Cross-Sectional Survey on COVID-19. J. Med. Internet Res. 2020, 22, e18790. [Google Scholar] [CrossRef]
- Latkovikj, M.T.; Popovska, M.B. Online Research about Online Research: Advantages and Disadvantages. E-Methodol. 2019, 6, 44–56. [Google Scholar] [CrossRef]
- Reyneke, G.; Hughes, J.; Grafenauer, S. Consumer Understanding of the Australian Dietary Guidelines: Recommendations for Legumes and Whole Grains. Nutrients 2022, 14, 1753. [Google Scholar] [CrossRef]
- Dos Santos Quaresma, M.V.; Marques, C.G.; Magalhães, A.C.O.; dos Santos, R.V.T. Emotional Eating, Binge Eating, Physical Inactivity, and Vespertine Chronotype Are Negative Predictors of Dietary Practices during COVID-19 Social Isolation: A Cross-Sectional Study. Nutrition 2021, 90, 111223. [Google Scholar] [CrossRef]
- Smith, W.G. Does Gender Influence Online Survey Participation? A Record-Linkage Analysis of University Faculty Online Survey Response Behavior; San Jose State University: San Jose, CA, USA, 2008. [Google Scholar]
- Hathcock, J.N.; Azzi, A.; Blumberg, J.; Bray, T.; Dickinson, A.; Frei, B.; Jialal, I.; Johnston, C.S.; Kelly, F.J.; Kraemer, K.; et al. Vitamins E and C Are Safe across a Broad Range of Intakes. Am. J. Clin. Nutr. 2005, 81, 736–745. [Google Scholar] [CrossRef]
- European Food Safety Authority. Scientific Committee on Food, S.P. on D.P. Tolerable Upper Intake Levels for Vitamins and Minerals, 2006. Available online: https://www.efsa.europa.eu/sites/default/files/efsa_rep/blobserver_assets/ndatolerableuil.pdf (accessed on 15 December 2022).
- Carr, A.C.; Lykkesfeldt, J. Discrepancies in Global Vitamin C Recommendations: A Review of RDA Criteria and Underlying Health Perspectives. Crit. Rev. Food Sci. Nutr. 2020, 61, 742–755. [Google Scholar] [CrossRef]
- Kaźmierczak-Barańska, J.; Boguszewska, K.; Adamus-Grabicka, A.; Karwowski, B.T. Two Faces of Vitamin C—Antioxidative and Pro-Oxidative Agent. Nutrients 2020, 12, 1501. [Google Scholar] [CrossRef]
- Slaughter, R.J.; Watts, M.; Vale, J.A.; Grieve, J.R.; Schep, L.J. The Clinical Toxicology of Sodium Hypochlorite. Clin. Toxicol. 2019, 57, 303–311. [Google Scholar] [CrossRef]
- Hall, A.H.; Jacquemin, D.; Henny, D.; Mathieu, L.; Josset, P.; Meyer, B. Corrosive Substances Ingestion: A Review. Crit. Rev. Toxicol. 2019, 49, 637–669. [Google Scholar] [CrossRef] [PubMed]
- Arellano-Gutiérrez, G.; Aldana-Zaragoza, E.H.; Pérez-Fabián, A. Intestinal Perforation Associated with Chlorine Dioxide Ingestion: An Adult Chronic Consumer during COVID-19 Pandemic. Clin. J. Gastroenterol. 2021, 14, 1655. [Google Scholar] [CrossRef] [PubMed]
- Cook, M.A.; Brooke, N. Event-Based Surveillance of Poisonings and Potentially Hazardous Exposures over 12 Months of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 11133. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration (FDA). Coronavirus Update: FDA and FTC Warn Seven Companies Selling Fraudulent Products That Claim to Treat or Prevent COVID-19 | FDA. Available online: https://www.fda.gov/news-events/press-announcements/coronavirus-update-fda-and-ftc-warn-seven-companies-selling-fraudulent-products-claim-treat-or (accessed on 14 December 2022).
- Bramstedt, K.A. Unicorn Poo and Blessed Waters: COVID-19 Quackery and FDA Warning Letters. Ther. Innov. Regul. Sci. 2021, 55, 239. [Google Scholar] [CrossRef]
- CDC. Agency for Toxic Substances and Disease Registry. Toxicological Profile for Silver | ATSDR. Available online: https://wwwn.cdc.gov/TSP/ToxProfiles/ToxProfiles.aspx?id=539&tid=97 (accessed on 14 December 2022).
- Tobarran, N.; Hieger, M.A. Acute Silver Toxicity From Colloidal Silver Overdose. Am. J. Ther. 2020, 27, E682–E684. [Google Scholar] [CrossRef]
- Jayawardena, R.; Sooriyaarachchi, P.; Chourdakis, M.; Jeewandara, C.; Ranasinghe, P. Enhancing Immunity in Viral Infections, with Special Emphasis on COVID-19: A Review. Diabetes Metab. Syndr. 2020, 14, 367. [Google Scholar] [CrossRef]
- Nilashi, M.; Samad, S.; Yusuf, S.Y.M.; Akbari, E. Can Complementary and Alternative Medicines Be Beneficial in the Treatment of COVID-19 through Improving Immune System Function? J. Infect. Public Health 2020, 13, 893. [Google Scholar] [CrossRef]
- Zabetakis, I.; Lordan, R.; Norton, C.; Tsoupras, A. COVID-19: The Inflammation Link and the Role of Nutrition in Potential Mitigation. Nutrients 2020, 12, 1466. [Google Scholar] [CrossRef]
- Hakeem, R.; Sheikh, M.A. Beyond Transmission: Dire Need for Integration of Nutrition Interventions in COVID-19 Pandemic-Response Strategies in Developing Countries like Pakistan. Pakistan J. Med. Sci. 2020, 36, S85. [Google Scholar] [CrossRef]
- Fernández-Quintela, A.; Milton-Laskibar, I.; Trepiana, J.; Gómez-Zorita, S.; Kajarabille, N.; Léniz, A.; González, M.; Portillo, M.P. Key Aspects in Nutritional Management of COVID-19 Patients. J. Clin. Med. 2020, 9, 2589. [Google Scholar] [CrossRef]
- Budhwar, S.; Sethi, K.; Chakraborty, M. A Rapid Advice Guideline for the Prevention of Novel Coronavirus Through Nutritional Intervention. Curr. Nutr. Rep. 2020, 9, 119. [Google Scholar] [CrossRef]
- Rodriguez-leyva, D.; Pierce, G.N. The Impact of Nutrition on the COVID-19 Pandemic and the Impact of the COVID-19 Pandemic on Nutrition. Nutrients 2021, 13, 1752. [Google Scholar] [CrossRef]
- Taylor, P.N.; Davies, J.S. A Review of the Growing Risk of Vitamin D Toxicity from Inappropriate Practice. Br. J. Clin. Pharmacol. 2018, 84, 1121. [Google Scholar] [CrossRef]
- Parsons, I.T.; Gifford, R.M.; Stacey, M.J.; Lamb, L.E.; O’Shea, M.K.; Woods, D.R. Does Vitamin D Supplementation Prevent SARS-CoV-2 Infection in Military Personnel? Review of the Evidence. BMJ Mil. Health 2021, 167, 280–286. [Google Scholar] [CrossRef]
- Doseděl, M.; Jirkovský, E.; Macáková, K.; Krčmová, L.K.; Javorská, L.; Pourová, J.; Mercolini, L.; Remião, F.; Nováková, L.; Mladěnka, P. Vitamin C—Sources, Physiological Role, Kinetics, Deficiency, Use, Toxicity, and Determination. Nutrients 2021, 13, 615. [Google Scholar] [CrossRef]
- Khan, A.H.; Nasir, N.; Nasir, N.; Maha, Q.; Rehman, R. Vitamin D and COVID-19: Is There a Role? J. Diabetes Metab. Disord. 2021, 20, 931. [Google Scholar] [CrossRef]
- De Faria Coelho-Ravagnani, C.; Corgosinho, F.C.; Sanches, F.L.F.Z.; Prado, C.M.M.; Laviano, A.; Mota, J.F. Dietary Recommendations during the COVID-19 Pandemic. Nutr. Rev. 2021, 79, 382–393. [Google Scholar] [CrossRef]
- BourBour, F.; Mirzaei Dahka, S.; Gholamalizadeh, M.; Akbari, M.E.; Shadnoush, M.; Haghighi, M.; Taghvaye-Masoumi, H.; Ashoori, N.; Doaei, S. Nutrients in Prevention, Treatment, and Management of Viral Infections—Special Focus on Coronavirus. Arch. Physiol. Biochem. 2020, 1–10. [Google Scholar] [CrossRef]
- Kenneth Weir, E.; Thenappan, T.; Bhargava, M.; Chen, Y. Does Vitamin D Deficiency Increase the Severity of COVID-19? Clin. Med. (Northfield. Il). 2020, 20, e107. [Google Scholar] [CrossRef]
- Da Rocha, A.P.; Atallah, A.N.; Aldrighi, J.M.; Pires, A.L.R.; dos Santos Puga, M.E.; Pinto, A.C.P.N. Insufficient Evidence for Vitamin D Use in COVID-19: A Rapid Systematic Review. Int. J. Clin. Pract. 2021, 75, 14649. [Google Scholar] [CrossRef] [PubMed]
- Asif, A.; Farooq, N. Vitamin D Toxicity. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- European Food Safety Authority. Guidance on the Scientific Requirements for Health Claims Related to the Immune System, the Gastrointestinal Tract and Defence against Pathogenic Microorganisms. EFSA J. 2016, 14, 4369. [Google Scholar] [CrossRef]
- Calder, P.C.; Carr, A.C.; Gombart, A.F.; Eggersdorfer, M. Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections. Nutrients 2020, 12, 1181. [Google Scholar] [CrossRef] [PubMed]
- Molloy, E.J.; Murphy, N. Vitamin D, Covid-19 and Children. Ir. Med. J. 2020, 113, 59. [Google Scholar]
- Calder, P.C.; Development, H. Nutrition Immunity and COVID-19. BMJ Nutr. Prev. Health 2020, 3, 74–92. [Google Scholar] [CrossRef]
- Iddir, M.; Brito, A.; Dingeo, G.; Del Campo, S.S.F.; Samouda, H.; La Frano, M.R.; Bohn, T. Strengthening the Immune System and Reducing Inflammation and Oxidative Stress through Diet and Nutrition: Considerations during the COVID-19 Crisis. Nutrients 2020, 12, 1562. [Google Scholar] [CrossRef]
- Carr, A.C.; Rowe, S. Factors Affecting Vitamin C Status and Prevalence of Deficiency: A Global Health Perspective. Nutrients 2020, 12, 1963. [Google Scholar] [CrossRef]
- Meltzer, D.O.; Best, T.J.; Zhang, H.; Vokes, T.; Arora, V.; Solway, J. Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results. JAMA Netw. Open 2020, 3, e2019722. [Google Scholar] [CrossRef]
- Carr, A.C.; Rowe, S. The Emerging Role of Vitamin C in the Prevention and Treatment of COVID-19. Nutrients 2020, 12, 3286. [Google Scholar] [CrossRef]
- Santaolalla, A.; Beckmann, K.; Kibaru, J.; Josephs, D.; Van Hemelrijck, M.; Irshad, S. Association Between Vitamin D and Novel SARS-CoV-2 Respiratory Dysfunction—A Scoping Review of Current Evidence and Its Implication for COVID-19 Pandemic. Front. Physiol. 2020, 11, 564387. [Google Scholar] [CrossRef]
- Hemilä, H.; de Man, A.M.E. Vitamin C and COVID-19. Front. Med. 2020, 7, 559811. [Google Scholar] [CrossRef]
- Moscatelli, F.; Sessa, F.; Valenzano, A.; Polito, R.; Monda, V.; Cibelli, G.; Villano, I.; Pisanelli, D.; Perrella, M.; Daniele, A.; et al. COVID-19: Role of Nutrition and Supplementation. Nutrients 2021, 13, 976. [Google Scholar] [CrossRef]
- Ghasemian, R.; Shamshirian, A.; Heydari, K.; Malekan, M.; Alizadeh-Navaei, R.; Ebrahimzadeh, M.A.; Ebrahimi Warkiani, M.; Jafarpour, H.; Razavi Bazaz, S.; Rezaei Shahmirzadi, A.; et al. The Role of Vitamin D in the Age of COVID-19: A Systematic Review and Meta-analysis. Int. J. Clin. Pract. 2021, 75, 14675. [Google Scholar] [CrossRef]
- Lordan, R. Notable Developments for Vitamin D Amid the COVID-19 Pandemic, but Caution Warranted Overall: A Narrative Review. Nutrients 2021, 13, 740. [Google Scholar] [CrossRef]
- Milani, G.P.; Macchi, M.; Guz-Mark, A. Vitamin C in the Treatment of COVID-19. Nutrients 2021, 13, 1172. [Google Scholar] [CrossRef]
- Hemilä, H.; Carr, A.; Chalker, E. Vitamin C May Increase the Recovery Rate of Outpatient Cases of SARS-CoV-2 Infection by 70%: Reanalysis of the COVID A to Z Randomized Clinical Trial. Front. Immunol. 2021, 12, 674681. [Google Scholar] [CrossRef]
- Grove, A.; Osokogu, O.; Al-Khudairy, L.; Mehrabian, A.; Zanganeh, M.; Brown, A.; Court, R.; Taylor-Phillips, S.; Uthman, O.A.; McCarthy, N.; et al. Association between Vitamin D Supplementation or Serum Vitamin D Level and Susceptibility to SARS-CoV-2 Infection or COVID-19 Including Clinical Course, Morbidity and Mortality Outcomes? A Systematic Review. BMJ Open 2021, 11, e043737. [Google Scholar] [CrossRef]
- Bae, J.H.; Choe, H.J.; Holick, M.F.; Lim, S. Association of Vitamin D Status with COVID-19 and Its Severity: Vitamin D and COVID-19: A Narrative Review. Rev. Endocr. Metab. Disord. 2022, 23, 579. [Google Scholar] [CrossRef]
- Carr, A.C.; Gombart, A.F. Multi-Level Immune Support by Vitamins C and D during the SARS-CoV-2 Pandemic. Nutrients 2022, 14, 689. [Google Scholar] [CrossRef]
- Dror, A.A.; Morozov, N.; Daoud, A.; Namir, Y.; Yakir, O.; Shachar, Y.; Lifshitz, M.; Segal, E.; Fisher, L.; Mizrachi, M.; et al. Pre-Infection 25-Hydroxyvitamin D3 Levels and Association with Severity of COVID-19 Illness. PLoS ONE 2022, 17, e0263069. [Google Scholar] [CrossRef]
- Pedrosa, L.F.C.; Barros, A.N.A.B.; Leite-Lais, L. Nutritional Risk of Vitamin D, Vitamin C, Zinc, and Selenium Deficiency on Risk and Clinical Outcomes of COVID-19: A Narrative Review. Clin. Nutr. Espen 2022, 47, 9. [Google Scholar] [CrossRef] [PubMed]
- Gruber-Bzura, B.M. High-Dose Vitamin C Supplementation as a Legitimate Anti-SARS-CoV-2 Prophylaxis in Healthy Subjects—Yes or No? Nutrients 2022, 14, 979. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, B.; El Abd, A.; Ducharme, F.M. Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis. Nutrients 2022, 14, 2134. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Eshaghian, E.; Chuang, J.; Covasa, M. Do Diet and Dietary Supplements Mitigate Clinical Outcomes in COVID-19? Nutrients 2022, 14, 1909. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.R. Vitamin C for COVID-19 Treatment: Have We Got Enough Evidence? Front. Nutr. 2022, 9, 892561. [Google Scholar] [CrossRef]
- Galmés, S.; Palou, A.; Serra, F. Suboptimal Consumption of Relevant Immune System Micronutrients Is Associated with a Worse Impact of COVID-19 in Spanish Populations. Nutrients 2022, 14, 2254. [Google Scholar] [CrossRef]
- Renata, R.B.N.; Arely, G.R.A.; Gabriela, L.M.A.; Esther, M.L.M. Immunomodulatory Role of Microelements in COVID-19 Outcome: A Relationship with Nutritional Status. Biol. Trace Elem. Res. 2022, 1, S12011–S12022. [Google Scholar] [CrossRef]
- Houghton, C.C.; Lew, S.Q. Case Report: Long-Term Hypervitaminosis D-Induced Hypercalcaemia Treated with Glucocorticoids and Bisphosphonates. BMJ Case Rep. 2020, 13, 233853. [Google Scholar] [CrossRef]
- Frischknecht, L.; von Rappard, J. Severe Vitamin D Intoxication. MMW Fortschr. Med. 2020, 162, 54–57. [Google Scholar] [CrossRef]
- Reyes, G.M.L.; Seiltgens, S.C. Hypervitaminosis D, a Note of Caution. Is the Increase Associate to Pandemic Covid19? Report of 5 Cases. Andes Pediatr. Rev. Chil. Pediatr. 2021, 92, 317–318. [Google Scholar] [CrossRef]
- Feghali, K.; Papamarkakis, K.; Clark, J.; Malhotra, N.; Stoddart, L.; Osakwe, I. Vitamin D Toxicity Managed with Peritoneal Dialysis. Case Rep. Endocrinol. 2021, 2021, 1–6. [Google Scholar] [CrossRef]
- Alkundi, A.; Momoh, R.; Musa, A.; Nwafor, N. Vitamin D Intoxication and Severe Hypercalcaemia Complicating Nutritional Supplements Misuse. BMJ Case Rep. 2022, 15, e250553. [Google Scholar] [CrossRef]
- Vitamin D Supplement “overdosing” Is Possible and Harmful, Warn Doctors | BMJ. Available online: https://www.bmj.com/company/newsroom/vitamin-d-supplement-overdosing-is-possible-and-harmful-warn-doctors/ (accessed on 17 December 2022).
- Hashemipour, S.; Ghobadi, A.; Hadizadeh Khairkhah, S.M.R.; Ranjbaran, M.; Badri, M.; Ghafelehbashi, S.H.; Gheraati, M. Association of Weekly or Biweekly Use of 50 000 IU Vitamin D3 with Hypervitaminosis D. Br. J. Clin. Pharmacol. 2022, 88, 3506–3509. [Google Scholar] [CrossRef]
- Bendezu-Quispe, G.; Benites-Meza, J.K.; Urrunaga-Pastor, D.; Herrera-Añazco, P.; Uyen-Cateriano, A.; Rodriguez-Morales, A.J.; Toro-Huamanchumo, C.J.; Hernandez, A.V.; Benites-Zapata, V.A. Consumption of Herbal Supplements or Homeopathic Remedies to Prevent COVID-19 and Intention of Vaccination for COVID-19 in Latin America and the Caribbean. Trop. Med. Infect. Dis. 2022, 7, 95. [Google Scholar] [CrossRef]
- Hornsey, M.J.; Lobera, J.; Díaz-Catalán, C. Vaccine Hesitancy Is Strongly Associated with Distrust of Conventional Medicine, and Only Weakly Associated with Trust in Alternative Medicine. Soc. Sci. Med. 2020, 255, 113019. [Google Scholar] [CrossRef]
- Makrufardi, F.; Saputri, A.; Phillabertha, P.S. COVID-19 vaccine: The challenge of herbal medicine community belief in a developing country—letter to the editor. African J. Infect. Dis. 2021, 15, 1. [Google Scholar] [CrossRef]
- Bearth, A.; Berthold, A.; Siegrist, M. People’s Perceptions of, Willingness-to-Take Preventive Remedies and Their Willingness-to-Vaccinate during Times of Heightened Health Threats. PLoS One 2022, 17, e0263351. [Google Scholar] [CrossRef]
- Scott, S.E.; Rozin, P.; Small, D.A. Consumers Prefer “Natural” More for Preventatives Than for Curatives. J. Consum. Res. 2020, 47, 454–471. [Google Scholar] [CrossRef]
- Soveri, A.; Karlsson, L.C.; Antfolk, J.; Lindfelt, M.; Lewandowsky, S. Unwillingness to Engage in Behaviors That Protect against COVID-19: The Role of Conspiracy Beliefs, Trust, and Endorsement of Complementary and Alternative Medicine. BMC Public Health 2021, 21, 684. [Google Scholar] [CrossRef]
- Pavela Banai, I.; Banai, B.; Mikloušić, I. Beliefs in COVID-19 Conspiracy Theories, Compliance with the Preventive Measures, and Trust in Government Medical Officials. Curr. Psychol. 2022, 41, 7448. [Google Scholar] [CrossRef]
- Essar, M.Y.; Kazmi, S.K.; Hasan, M.M.; dos Santos Costa, A.C.; Ahmad, S. The Rampant Use of Cow Dung to Treat COVID-19: Is India at the Brink of a Zoonotic Disease Outbreak? J. Med. Virol. 2021, 93, 6471. [Google Scholar] [CrossRef] [PubMed]
- Daria, S.; Islam, M.R. The Use of Cow Dung and Urine to Cure COVID-19 in India: A Public Health Concern. Int. J. Health Plann. Manag. 2021, 36, 1950. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Coronavirus Disease (COVID-19) Advice for the Public: Mythbusters. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters (accessed on 15 December 2022).
- World Health Organization. 12 Myths About Covid-19. Available online: https://www.who.int/docs/default-source/searo/thailand/12myths-final099bfbf976c54d5fa3407a65b6d9fa9d.pdf (accessed on 15 December 2022).
- World Health Organization. COVID-19 Fact or Fiction. Available online: https://www.who.int/southeastasia/outbreaks-and-emergencies/covid-19/What-can-we-do-to-keep-safe/fact-or-fiction (accessed on 15 December 2022).
- World Health Organization. COVID-19 Advice—Mythbusters | WHO Western Pacific. Available online: https://www.who.int/westernpacific/emergencies/covid-19/information/mythbusters (accessed on 15 December 2022).
- World Health Organization. COVID-19 Facts and Myths | WHO South-East Asia. Available online: https://www.who.int/southeastasia/outbreaks-and-emergencies/covid-19/What-can-we-do-to-keep-safe/facts-and-myths (accessed on 15 December 2022).
- World Health Organization. WHO EMRO | Alcohol Does Not Protect against COVID-19 and Its Access Should Be Restricted during Lock down | News | Mental Health. Available online: https://www.emro.who.int/mnh/news/alcohol-does-not-protect-against-covid-19-and-its-access-should-be-restricted-during-lock-down.html (accessed on 15 December 2022).
- Lebin, J.A.; Mudan, A.; Wu, A.H.B. Chronic Alcohol Use Does Not Protect against COVID-19 Infection. Am. J. Emerg. Med. 2021, 45, 640. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Fighting Misinformation in the Time of COVID-19, One Click at a Time. Available online: https://www.who.int/news-room/feature-stories/detail/fighting-misinformation-in-the-time-of-covid-19-one-click-at-a-time (accessed on 15 December 2022).
- World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report, 32. Available online: https://apps.who.int/iris/bitstream/handle/10665/331686/nCoVsitrep02Apr2020-eng.pdf (accessed on 14 December 2022).
- Hu, L.; Gao, J.; Yao, L.; Zeng, L.; Liu, Q.; Zhou, Q.; Zhang, H.; Lu, D.; Fu, J.; Liu, Q.S.; et al. Evidence Foodborne Transmission of the Coronavirus (COVID-19) through the Animal Products Food Supply Chain. Environ. Sci. Technol. 2021, 55, 2713. [Google Scholar] [CrossRef] [PubMed]
- Iftekhar, A.; Cui, X. Blockchain-Based Traceability System That Ensures Food Safety Measures to Protect Consumer Safety and COVID-19 Free Supply Chains. Foods 2021, 10, 1289. [Google Scholar] [CrossRef]
- Han, J.; Zhang, X.; He, S.; Jia, P. Can the Coronavirus Disease Be Transmitted from Food? A Review of Evidence, Risks, Policies and Knowledge Gaps. Environ. Chem. Lett. 2021, 19, 5. [Google Scholar] [CrossRef]
- Jia, M.; Taylor, T.M.; Senger, S.M.; Ovissipour, R.; Bertke, A.S. SARS-CoV-2 Remains Infectious on Refrigerated Deli Food, Meats, and Fresh Produce for up to 21 Days. Foods 2022, 11, 286. [Google Scholar] [CrossRef]
- Yekta, R.; Vahid-Dastjerdi, L.; Norouzbeigi, S.; Mortazavian, A.M. Food Products as Potential Carriers of SARS-CoV-2. Food Control 2021, 123, 107754. [Google Scholar] [CrossRef]
- Euromonitor International. Plant-Based Eating and Alternative Proteins | Market Research Report. Available online: https://www.euromonitor.com/plant-based-eating-and-alternative-proteins/report?recid=2027519376365&id=728898 (accessed on 15 December 2022).
- Mintel The Impact of COVID-19 on Food and Drink-UK-2020: Consumer Market Research Report | Mintel.Com. Available online: https://store.mintel.com/report/the-impact-of-covid-19-on-food-and-drink-uk-june-2020?utm_source=reports.mintel.com&utm_medium=redirect&utm_campaign=301redir (accessed on 17 December 2022).
- Sandhu, H.S.; Arora, A.; Sarker, S.I.; Shah, B.; Sivendra, A.; Winsor, E.S.; Luthra, A. Pandemic Prevention and Unsustainable Animal-Based Consumption. Bull. World Health Organ. 2021, 99, 603. [Google Scholar] [CrossRef]
- Gibbs, J.; Cappuccio, F.P. Plant-Based Dietary Patterns for Human and Planetary Health. Nutrients 2022, 14, 1614. [Google Scholar] [CrossRef]
- Crosby, L.; Davis, B.; Joshi, S.; Jardine, M.; Paul, J.; Neola, M.; Barnard, N.D. Ketogenic Diets and Chronic Disease: Weighing the Benefits Against the Risks. Front. Nutr. 2021, 8, 702802. [Google Scholar] [CrossRef]
- Noce, A.; Marrone, G.; Wilson Jones, G.; Di Lauro, M.; Pietroboni Zaitseva, A.; Ramadori, L.; Celotto, R.; Mitterhofer, A.P.; Di Daniele, N. Nutritional Approaches for the Management of Metabolic Acidosis in Chronic Kidney Disease. Nutrients 2021, 13, 2534. [Google Scholar] [CrossRef]
- Tahreem, A.; Rakha, A.; Rabail, R.; Nazir, A.; Socol, C.T.; Maerescu, C.M.; Aadil, R.M. Fad Diets: Facts and Fiction. Front. Nutr. 2022, 9, 960922. [Google Scholar] [CrossRef]
- Ali, S.H.; Foreman, J.; Tozan, Y.; Capasso, A.; Jones, A.M.; DiClemente, R.J. Trends and Predictors of COVID-19 Information Sources and Their Relationship With Knowledge and Beliefs Related to the Pandemic: Nationwide Cross-Sectional Study. JMIR Public Health Surveill. 2020, 6, e21071. [Google Scholar] [CrossRef]
- Myrick, J.G.; Erlichman, S. How Audience Involvement and Social Norms Foster Vulnerability to Celebrity-Based Dietary Misinformation. Psychol. Pop. Media 2020, 9, 367–379. [Google Scholar] [CrossRef]
- Adamski, M.; Truby, H.; Klassen, K.M.; Cowan, S.; Gibson, S. Using the Internet: Nutrition Information-Seeking Behaviours of Lay People Enrolled in a Massive Online Nutrition Course. Nutrients 2020, 12, 750. [Google Scholar] [CrossRef]
- Alvarez-Galvez, J.; Suarez-Lledo, V.; Rojas-Garcia, A. Determinants of Infodemics During Disease Outbreaks: A Systematic Review. Front. Public Health 2021, 9, 603603. [Google Scholar] [CrossRef]
- Kabata, P.; Winniczuk-Kabata, D.; Kabata, P.M.; Jaśkiewicz, J.; Połom, K. Can Social Media Profiles Be a Reliable Source of Information on Nutrition and Dietetics? Healthcare 2022, 10, 397. [Google Scholar] [CrossRef]
- Frampton, G.; Woods, L.; Scott, D.A. Inconsistent and Incomplete Retraction of Published Research: A Cross-Sectional Study on Covid-19 Retractions and Recommendations to Mitigate Risks for Research, Policy and Practice. PLoS ONE 2021, 16, e0258935. [Google Scholar] [CrossRef]
- Henrina, J.; Lim, M.A.; Pranata, R. COVID-19 and Misinformation: How an Infodemic Fuelled the Prominence of Vitamin D. Br. J. Nutr. 2021, 125, 1. [Google Scholar] [CrossRef]
- McCully, S.N.; Don, B.P.; Updegraff, J.A. Using the Internet to Help with Diet, Weight, and Physical Activity: Results From the Health Information National Trends Survey (HINTS). J. Med. Internet Res. 2013, 15, e148. [Google Scholar] [CrossRef] [PubMed]
- Jackson, K.; Knippen, K.; Haar, C. Social Media and Diet-Nutrition Information Seeking Behavior Among College Students. J. Acad. Nutr. Diet. 2019, 119, A148. [Google Scholar] [CrossRef]
- Midthassel, T.C.; Hansen, A.H. Are Lifestyle Changes from Online Information Associated with Discussing the Information with a Doctor? A Cross -Sectional Study. PLoS ONE 2021, 16, e0261471. [Google Scholar] [CrossRef]
- Mayasari, N.R.; Ho, D.K.N.; Lundy, D.J.; Skalny, A.V.; Tinkov, A.A.; Teng, I.C.; Wu, M.C.; Faradina, A.; Mohammed, A.Z.M.; Park, J.M.; et al. Impacts of the COVID-19 Pandemic on Food Security and Diet-Related Lifestyle Behaviors: An Analytical Study of Google Trends-Based Query Volumes. Nutrients 2020, 12, 3103. [Google Scholar] [CrossRef] [PubMed]
- Kushwaha, S.; Khanna, P.; Jain, R.; Srivastava, R. Determining the Nutritional Immunity Information-Seeking Behaviour during the COVID-19 Pandemic in India: A Google Trends Data Analysis. Public Health Nutr. 2021, 24, 5338–5349. [Google Scholar] [CrossRef]
- Lordan, R. Dietary Supplements and Nutraceuticals Market Growth during the Coronavirus Pandemic—Implications for Consumers and Regulatory Oversight. PharmaNutrition 2021, 18, 100282. [Google Scholar] [CrossRef]
- Jordan, I.; Keding, G.B.; Stosius, L.; Hawrysz, I.; Janiszewska, K.; Heil, E.A. Changes in Vegetable Consumption in Times of COVID-19—First Findings from an International Civil Science Project. Front. Nutr. 2021, 8, 686786. [Google Scholar] [CrossRef]
- Mazidi, M.; Leeming, E.R.; Merino, J.; Nguyen, L.H.; Selvachandran, S.; Pujal, J.C.; Maher, T.; Kadé, K.; Murray, B.; Graham, M.S.; et al. Diet and Lifestyle Behaviour Disruption Related to the Pandemic Was Varied and Bidirectional among US and UK Adults Participating in the ZOE COVID Study. Nat. Food 2021, 2, 957–969. [Google Scholar] [CrossRef]
- Dicken, S.J.; Mitchell, J.J.; Newberry Le Vay, J.; Beard, E.; Kale, D.; Herbec, A.; Shahab, L. Impact of the COVID-19 Pandemic on Diet Behaviour Among UK Adults: A Longitudinal Analysis of the HEBECO Study. Front. Nutr. 2022, 8, 788043. [Google Scholar] [CrossRef]
- Nan, X.; Wang, Y.; Thier, K. Why Do People Believe Health Misinformation and Who Is at Risk? A Systematic Review of Individual Differences in Susceptibility to Health Misinformation. Soc. Sci. Med. 2022, 314, 115398. [Google Scholar] [CrossRef]
- Aldayel, A.; Magdy, W. Characterizing the Role of Bots’ in Polarized Stance on Social Media. Soc. Netw. Anal. Min. 2022, 12, 1–24. [Google Scholar] [CrossRef]
- Gisondi, M.A.; Barber, R.; Faust, J.S.; Raja, A.; Strehlow, M.C.; Westafer, L.M.; Gottlieb, M. A Deadly Infodemic: Social Media and the Power of COVID-19 Misinformation. J Med. Internet Res. 2022, 24, e35552. [Google Scholar] [CrossRef]
- Reuters Types, Sources, and Claims of COVID-19 Misinformation | Reuters Institute for the Study of Journalism. Available online: https://reutersinstitute.politics.ox.ac.uk/types-sources-and-claims-covid-19-misinformation (accessed on 17 December 2022).
- Suarez-Lledo, V.; Alvarez-Galvez, J. Prevalence of Health Misinformation on Social Media: Systematic Review. J. Med. Internet Res. 2021, 23, e17187. [Google Scholar] [CrossRef]
- Hoffman, S.J.; Tan, C. Following Celebrities’ Medical Advice: Meta-Narrative Analysis. BMJ 2013, 347, f7151. [Google Scholar] [CrossRef]
- Ruxton, C.H.; Ruani, M.A.; Evans, C.E. Promoting and Disseminating Consistent and Effective Nutrition Messages: Challenges and Opportunities. Proc. Nutr. Soc. 2023, 1–27. [Google Scholar] [CrossRef]
- Reiss, M.J. Michael J. Food and Nutrition. In Rethinking Biology: Public Understandings; Reiss, M.J., Michael, J., Watts, F.N., Wiseman, H., Eds.; World Scientific: Hackensack, NJ, USA, 2020; pp. 213–230. ISBN 9811207488. [Google Scholar]
- Chen, X.; Hay, J.L.; Waters, E.A.; Kiviniemi, M.T.; Biddle, C.; Schofield, E.; Li, Y.; Kaphingst, K.; Orom, H. Health Literacy and Use and Trust in Health Information. J. Health Commun. 2018, 23, 724. [Google Scholar] [CrossRef]
- Svendsen, K.; Torheim, L.E.; Fjelberg, V.; Sorprud, A.; Narverud, I.; Retterstøl, K.; Bogsrud, M.P.; Holven, K.B.; Myhrstad, M.C.W.; Telle-Hansen, V.H. Gender Differences in Nutrition Literacy Levels among University Students and Employees: A Descriptive Study. J. Nutr. Sci. 2021, 10, e56. [Google Scholar] [CrossRef]
- Barua, Z.; Barua, S.; Aktar, S.; Kabir, N.; Li, M. Effects of Misinformation on COVID-19 Individual Responses and Recommendations for Resilience of Disastrous Consequences of Misinformation. Prog. Disaster Sci. 2020, 8, 100119. [Google Scholar] [CrossRef]
- Viskupič, F.; Wiltse, D.L.; Meyer, B.A. Trust in Physicians and Trust in Government Predict COVID-19 Vaccine Uptake. Soc. Sci. Q. 2022, 103, 509. [Google Scholar] [CrossRef]
- Roozenbeek, J.; Schneider, C.R.; Dryhurst, S.; Kerr, J.; Freeman, A.L.J.; Recchia, G.; Van Der Bles, A.M.; Van Der Linden, S. Susceptibility to Misinformation about COVID-19 around the World. R. Soc. Open Sci. 2020, 7, 201199. [Google Scholar] [CrossRef]
- Reiss, M.J. Trust, Science Education and Vaccines. Sci. Educ. 2022, 31, 1263–1280. [Google Scholar] [CrossRef] [PubMed]
- Perreault, W.D. Controlling Order-Effect Bias. Public Opin. Q. 1975, 39, 544–551. [Google Scholar] [CrossRef]
- Musi, E.; Reed, C. From Fallacies to Semi-Fake News: Improving the Identification of Misinformation Triggers across Digital Media. Discourse Soc. 2022, 33, 349–370. [Google Scholar] [CrossRef]
- Ecker, U.K.H.; Lewandowsky, S.; Cook, J.; Schmid, P.; Fazio, L.K.; Brashier, N.; Kendeou, P.; Vraga, E.K.; Amazeen, M.A. The Psychological Drivers of Misinformation Belief and Its Resistance to Correction. Nat. Rev. Psychol. 2022, 1, 13–29. [Google Scholar] [CrossRef]
- Lewandowsky, S.; Ecker, U.K.H.; Seifert, C.M.; Schwarz, N.; Cook, J. Misinformation and Its Correction: Continued Influence and Successful Debiasing. Psychol. Sci. Public Interest 2012, 13, 106–131. [Google Scholar] [CrossRef]
- Alter, A.L. The Benefits of Cognitive Disfluency. Curr. Dir. Psychol. Sci. 2013, 22, 437–442. [Google Scholar] [CrossRef]
- Fazio, L.K.; Brashier, N.M.; Keith Payne, B.; Marsh, E.J. Knowledge Does Not Protect against Illusory Truth. J. Exp. Psychol. Gen. 2015, 144, 993–1002. [Google Scholar] [CrossRef]
- Scott, A.; Jeon, S.H.; Joyce, C.M.; Humphreys, J.S.; Kalb, G.; Witt, J.; Leahy, A. A Randomised Trial and Economic Evaluation of the Effect of Response Mode on Response Rate, Response Bias, and Item Non-Response in a Survey of Doctors. BMC Med. Res. Methodol. 2011, 11, 126. [Google Scholar] [CrossRef]
- Greszki, R.; Meyer, M.; Schoen, H. Exploring the Effects of Removing “Too Fast” Responses and Respondents from Web Surveys. Public Opin. Q. 2015, 79, 471–503. [Google Scholar] [CrossRef]
- Tan, H.C.; Ho, J.A.; Kumarusamy, R.; Sambasivan, M. Measuring Social Desirability Bias: Do the Full and Short Versions of the Marlowe-Crowne Social Desirability Scale Matter? J. Empir. Res. Hum. Res. Ethics 2021, 17, 382–400. [Google Scholar] [CrossRef]
- Larsen, M.; Nyrup, J.; Petersen, M.B. Do Survey Estimates of the Public’s Compliance with COVID-19 Regulations Suffer from Social Desirability Bias? J. Behav. Public Adm. 2020, 3, 1–9. [Google Scholar] [CrossRef]
- Kreuter, F.; Presser, S.; Tourangeau, R. Social Desirability Bias in CATI, IVR, and Web Surveys—The Effects of Mode and Question Sensitivity. Public Opin. Q. 2008, 72, 847–865. [Google Scholar] [CrossRef]
- Ajdžanović, V.; Filipović, B.; Šošić-Jurjević, B.; Miler, M.; Milošević, V. Margins of Beneficial Daily Dosage of Supplements in Prevention of COVID-19. EXCLI J. 2021, 20, 828. [Google Scholar] [CrossRef]
- Lewis, S.L.; Chizmar, L.R.; Liotta, S. COVID-19 and Micronutrient Deficiency Symptoms—Is There Some Overlap? Clin. Nutr. Espen 2022, 48, 275. [Google Scholar] [CrossRef]
- Gombart, A.F.; Pierre, A.; Maggini, S. A Review of Micronutrients and the Immune System–Working in Harmony to Reduce the Risk of Infection. Nutrients 2020, 12, 236. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19 and Food Safety: Guidance for Food Businesses. Available online: https://www.who.int/publications/i/item/covid-19-and-food-safety-guidance-for-food-businesses (accessed on 14 December 2022).
| Statement | Misinformed Answers | Appropriate Answers | Unsure Answers | |
|---|---|---|---|---|
| Unfounded or Unproven Claims of Concern | % Who Regarded the Statement as being ‘Correct’ | % Who Regarded the Statement as being ‘Incorrect’ | % Who Were ‘Not Sure’ about This | |
| S4 | You can protect yourself from the novel coronavirus by gargling bleach. | 3.3 | 89.2 | 7.5 |
| S8 | It has been proven that taking 12 g (12,000 mg) of concentrated vitamin C daily can help remedy a COVID-19 infection. | 27.3 | 40.0 | 32.7 |
| S13 | Ingesting colloidal silver drops can increase the number of immune cells in the body and disintegrate some strains of coronavirus within 12 h. | 10.5 | 42.7 | 46.8 |
| S19 | It is safe to eat fruits and vegetables that have been washed with soap or diluted bleach to remove potential COVID-19 viral particles. | 43.1 | 40.6 | 16.3 |
| Other Unfounded or Unproven Claims | % Who Regarded the Statement as being ‘Correct’ | % Who Regarded the Statement as being ‘Incorrect’ | % Who Were ‘Not Sure’ about This | |
| S1 | Because the alcohol in vodka acts as a steriliser, taking a few sips can kill COVID-19 viruses sitting in the throat. | 7.4 | 69.3 | 23.3 |
| S2 | The COVID-19 virus cannot resist heat and dies when exposed to temperatures above 40 °C (104 °F). Therefore, sipping hot beverages such as tea and broth can help neutralise it. | 29.3 | 48.1 | 22.7 |
| S3 | Drinking water flushes all COVID-19 viral particles into the oesophagus and then the stomach, where they will be completely disintegrated by gastric acid. | 21.0 | 57.1 | 22.0 |
| S5 | Gargling with warm water and salt, apple cider vinegar, or lemon in hot water can eliminate the novel coronavirus from your throat. | 27.1 | 47.3 | 25.6 |
| S6 | Gargling with Listerine mouthwash can help reduce the risk of novel coronavirus infection due to its proven antiviral and antiseptic properties. | 17.5 | 52.6 | 30.0 |
| S7 | The antiviral properties of garlic and ginger have protective effects against COVID-19. | 39.4 | 30.8 | 29.8 |
| S9 | Antiviral herbs and spices such as chilli boost immunity and may help prevent novel coronavirus infection. | 39.7 | 31.7 | 28.6 |
| S10 | Taking high-dose vitamin C and D supplements will stop you from catching COVID-19. | 14.7 | 67.6 | 17.7 |
| S11 | Immune-boosting supplements such as zinc, green tea, oregano oil, Chaga mushroom blends, cow urine, bear bile, and echinacea have been shown to stop a COVID-19 infection. | 12.9 | 60.7 | 26.5 |
| S14 | Cold drinks and cold foods such as ice-cream help the novel coronavirus remain active in your body for longer, so it is important to avoid these. | 19.6 | 59.2 | 21.2 |
| S15 | Keep your mouth and throat always moist, as saliva can encapsulate and deactivate the COVID-19 virus. | 24.6 | 46.2 | 29.2 |
| S17 | It has been shown that the novel coronavirus is foodborne and transmitted through the consumption of meat, even when the meat has been thoroughly cooked. | 5.6 | 75.3 | 19.2 |
| S20 | Oreganol P73, from oregano oil, has a direct killing effect and ability to stop replication of the novel coronavirus in vitro. | 11.4 | 36.2 | 52.5 |
| S22 | Eating non-acidic (i.e., alkaline) foods that have a pH level higher than the novel coronavirus (that is, above 8.5) can help neutralise it. | 14.8 | 47.5 | 37.7 |
| S23 | Ketosis achieved through high-fat, low-carbohydrate ketogenetic eating helps activate immune T-cells in the lungs and provides a higher survival chance against the novel coronavirus than a carbohydrate-loaded diet. | 17.2 | 36.7 | 46.1 |
| S24 | Only people who eat meat are affected by the novel coronavirus. | 1.1 | 93.2 | 5.7 |
| S25 | A plant-based diet providing a variety of fruits and vegetables, herbs and spices, wholegrains, legumes, nuts, and seeds can provide immunity against the novel coronavirus and help ‘flatten the curve’. | 39.7 | 38.7 | 21.6 |
| Precautionary Guidance at the Time | % Who Regarded the Statement as being ‘Incorrect’ | % Who Regarded the Statement as being ‘Correct’ | % Who Were ‘Not Sure’ about This | |
| S12 | Although the risk is extremely low, undercooked meat contaminated with active COVID-19 viral particles could be a potential source of novel coronavirus transmission. | 20.9 | 43.6 | 35.5 |
| S16 | When your daily intake of vitamin C adequately supports your immune system, it might help you recover faster from COVID-19 than if you were deficient in this essential vitamin. | 6.9 | 79.3 | 13.8 |
| S18 | To reduce the risk of transmission of coronaviruses through food, the consumption of raw meat, raw milk, or undercooked animal products should be avoided, especially during the peak of an outbreak. | 30.1 | 47.0 | 22.9 |
| S21 | To reduce the risk of COVID-19 infection, try to avoid direct contact with the person delivering groceries or packages, and wash your hands thoroughly after bringing in packages or grocery deliveries. | 2.0 | 95.8 | 2.3 |
| Weighted Average of Answers across All 25 Statements (%) | 27.2 | 61.5 | 31.1 | |
| Frequency of Eating Behavior Changes per Source | ||||||||
|---|---|---|---|---|---|---|---|---|
| Sources Used for Eating Behavior Changes | Never | Hardly | Occasionally | Repeatedly | Continually | WAVG * | Total Responses n | |
| % | ||||||||
| 1 | Nutrition scientists, PhDs, and academics | 35.9 | 12.4 | 26.7 | 12.5 | 12.5 | 1.53 | 2675 |
| 2 | A nutrition professional | 39.0 | 11.5 | 25.2 | 11.8 | 12.5 | 1.47 | 2680 |
| 3 | Nutrition or health websites | 39.9 | 14.3 | 27.2 | 10.0 | 8.6 | 1.33 | 2684 |
| 4 | Scientific journals or science news publications | 42.6 | 14.6 | 24.6 | 10.3 | 7.9 | 1.27 | 2684 |
| 5 | Diet or health books | 48.7 | 14.3 | 22.6 | 8.0 | 6.4 | 1.09 | 2687 |
| 6 | Official government websites (WHO, UNICEF, CDC, NHS, etc.) | 51.7 | 14.2 | 18.0 | 7.8 | 8.4 | 1.07 | 2685 |
| 7 | A nurse or health coach | 51.1 | 14.5 | 21.9 | 6.6 | 5.9 | 1.02 | 2668 |
| 8 | My own medical doctor or GP | 54.3 | 15.0 | 17.6 | 6.9 | 6.3 | 0.96 | 2673 |
| 9 | Google or Internet searches | 54.4 | 14.9 | 19.8 | 5.7 | 5.2 | 0.92 | 2682 |
| 10 | Family members, friends, colleagues or peers | 52.1 | 18.1 | 21.0 | 4.4 | 4.4 | 0.91 | 2680 |
| 11 | Government officials | 57.7 | 15.7 | 16.4 | 5.1 | 5.1 | 0.84 | 2672 |
| 12 | Celebrity doctors or experts | 60.5 | 14.4 | 16.4 | 4.7 | 4.0 | 0.77 | 2667 |
| 13 | School, college, or university teachers or lecturers | 61.4 | 15.3 | 15.4 | 4.2 | 3.7 | 0.73 | 2665 |
| 14 | Film or TV documentaries | 63.3 | 15.8 | 15.6 | 3.2 | 2.2 | 0.65 | 2679 |
| 15 | Blogs or podcasts | 64.3 | 15.1 | 14.9 | 3.4 | 2.2 | 0.64 | 2673 |
| 16 | TV or radio news | 66.3 | 14.8 | 12.0 | 3.6 | 3.2 | 0.63 | 2666 |
| 17 | Online news outlets or magazines | 66.3 | 15.3 | 11.8 | 3.3 | 3.3 | 0.62 | 2679 |
| 18 | Influencers I follow on social media | 67.2 | 13.4 | 12.9 | 3.5 | 3.0 | 0.62 | 2679 |
| 19 | Gym instructors or personal trainers | 67.2 | 14.0 | 13.0 | 3.1 | 2.7 | 0.60 | 2670 |
| 20 | Social media (Facebook, Twitter, etc.) | 69.2 | 13.1 | 11.4 | 3.7 | 2.7 | 0.58 | 2678 |
| 21 | Private messages (WhatsApp, Viber, Messenger, etc.) | 72.9 | 13.0 | 8.5 | 3.1 | 2.5 | 0.49 | 2677 |
| 22 | Famous personalities, actors, or presenters | 79.1 | 10.5 | 7.2 | 1.8 | 1.5 | 0.36 | 2664 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruani, M.A.; Reiss, M.J. Susceptibility to COVID-19 Nutrition Misinformation and Eating Behavior Change during Lockdowns: An International Web-Based Survey. Nutrients 2023, 15, 451. https://doi.org/10.3390/nu15020451
Ruani MA, Reiss MJ. Susceptibility to COVID-19 Nutrition Misinformation and Eating Behavior Change during Lockdowns: An International Web-Based Survey. Nutrients. 2023; 15(2):451. https://doi.org/10.3390/nu15020451
Chicago/Turabian StyleRuani, Maria A., and Michael J. Reiss. 2023. "Susceptibility to COVID-19 Nutrition Misinformation and Eating Behavior Change during Lockdowns: An International Web-Based Survey" Nutrients 15, no. 2: 451. https://doi.org/10.3390/nu15020451
APA StyleRuani, M. A., & Reiss, M. J. (2023). Susceptibility to COVID-19 Nutrition Misinformation and Eating Behavior Change during Lockdowns: An International Web-Based Survey. Nutrients, 15(2), 451. https://doi.org/10.3390/nu15020451