Effects of Fish Oil, Lipid Mediators, Derived from Docosahexaenoic Acid, and Their Co-Treatment against Lipid Metabolism Dysfunction and Inflammation in HFD Mice and HepG2 Cells
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Animals and Treatments
2.3. Biochemical Parameters Assay
2.4. Histological Analysis
2.5. Cell Culture and Treatment
2.6. TG Assay in HepG2 Cells
2.7. qRT-PCR
2.8. Western Blotting
2.9. Statistical Analysis
3. Results
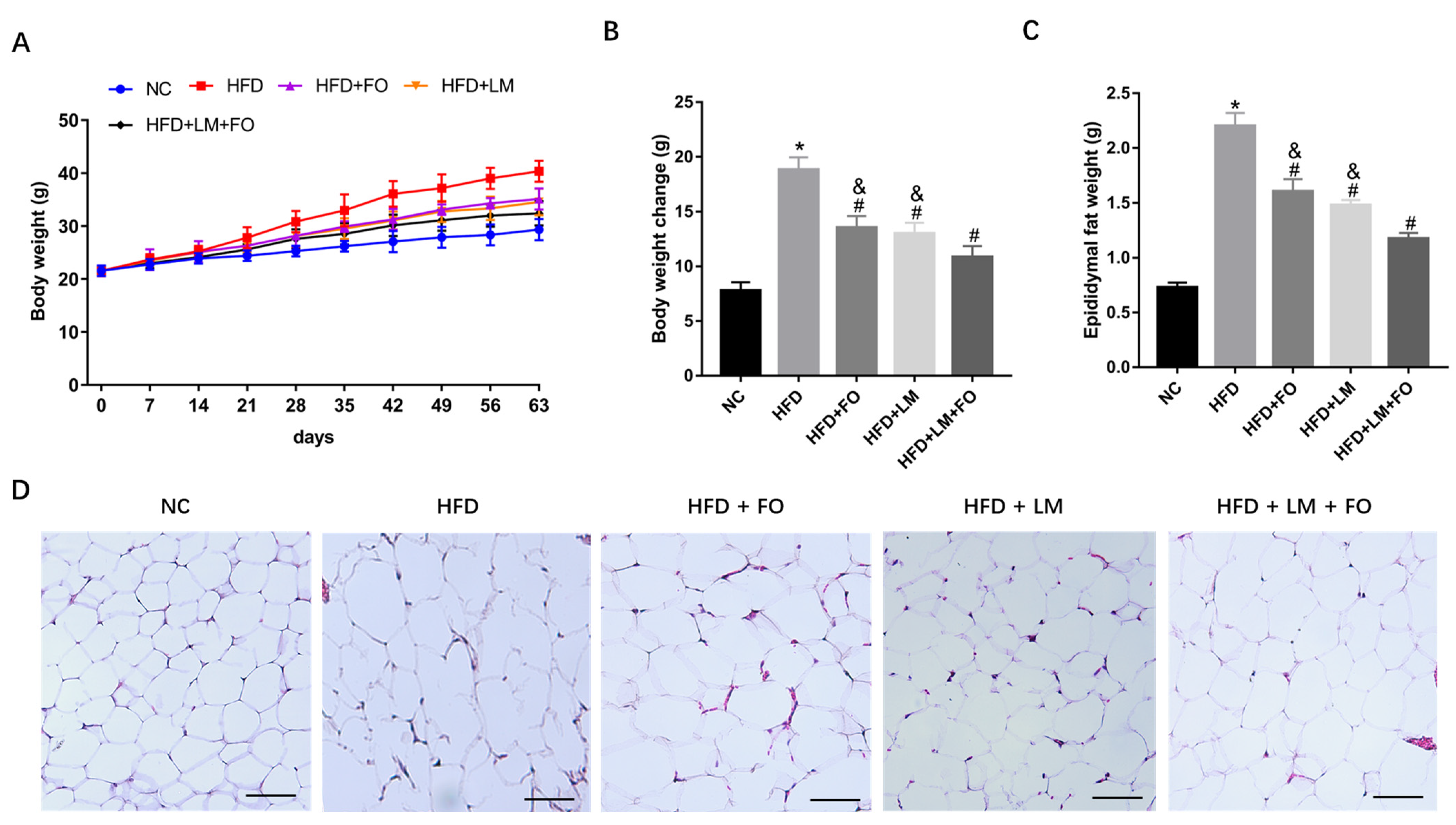
3.1. Diet with FO and LM Reduced the Body Weight and Adipose Tissue of HFD Mice
3.2. Diet with FO and LM Reversed Serum Lipid Profile in HFD-Fed Mice
3.3. Diet with FO and LM Recovered Fatty Liver in HFD-Fed Mice
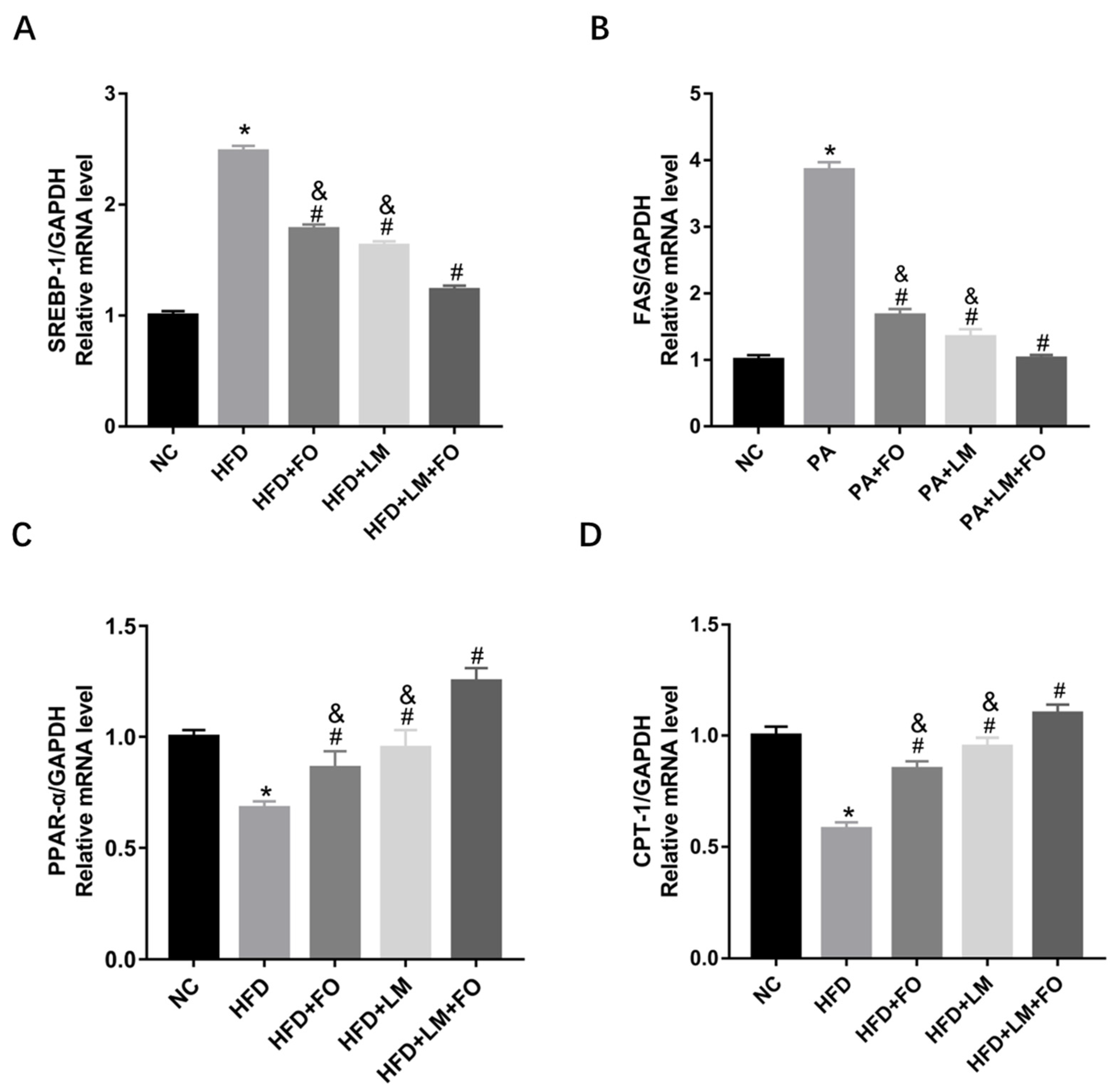
3.4. Diet with FO and LM Improved Lipid Metabolism Dysfunction in HFD-Fed Mice
3.5. Diet with FO and LM Ameliorated Liver Inflammation in HFD-Fed Mice
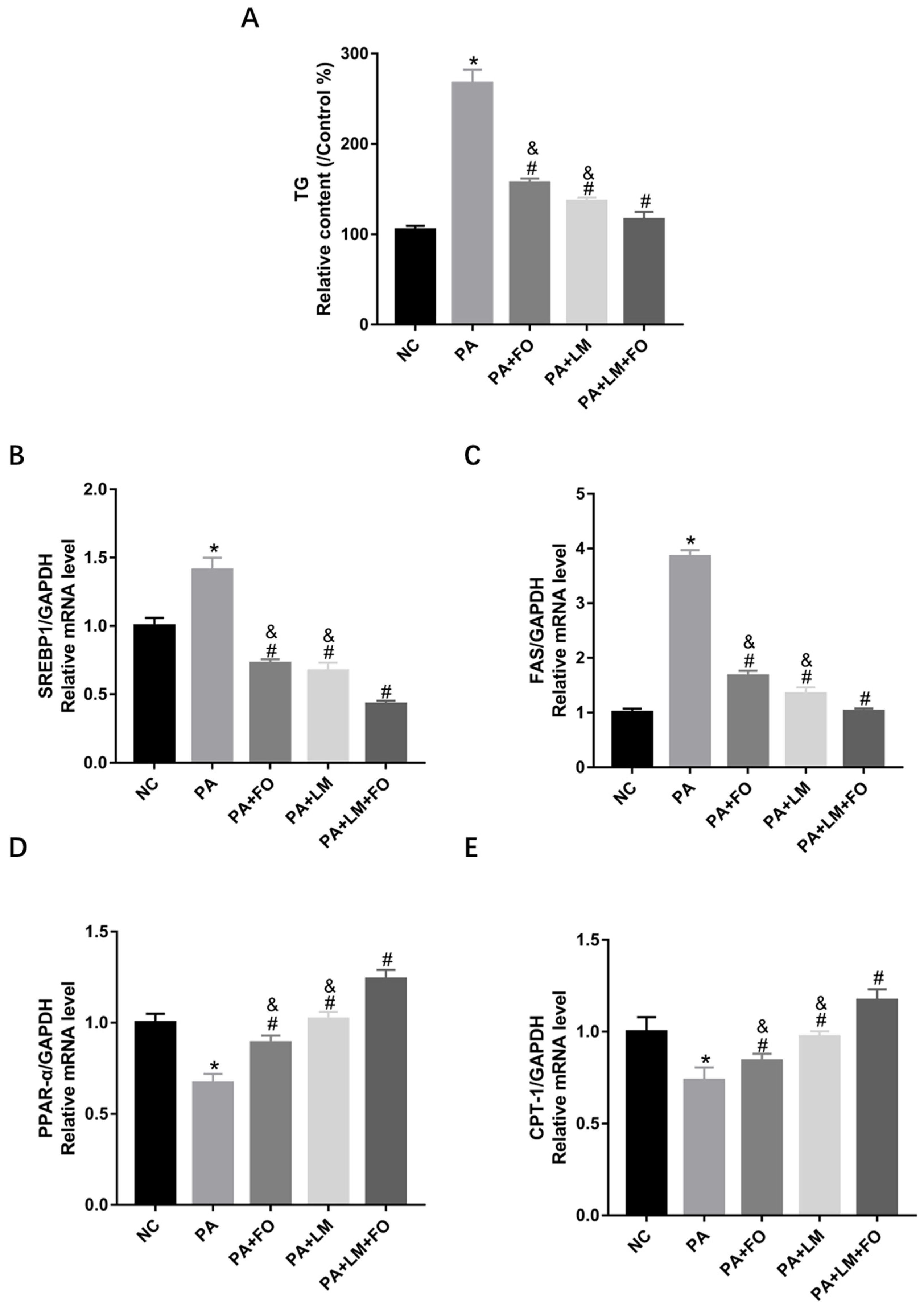
3.6. FO and LM Controlled PA-Induced Lipid Accumulation and Lipid Metabolism in HepG2 Cells
3.7. FO and LM Altered PA-Induced Inflammation in HepG2 Cells
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Younossi, Z.M.; Blissett, D.; Blissett, R.; Henry, L.; Stepanova, M.; Younossi, Y.; Racila, A.; Hunt, S.; Beckerman, R. The Economic and Clinical Burden of Nonalcoholic Fatty Liver Disease in the United States and Europe. Hepatology 2016, 64, 1577–1586. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Mark, H.E.; Anstee, Q.M.; Arab, J.P.; Batterham, R.L.; Castera, L.; Cortez-Pinto, H.; Crespo, J.; Cusi, K.; Dirac, M.A.; et al. Advancing the Global Public Health Agenda for NAFLD: A Consensus Statement. Nat. Rev. Gastroenterol. Hepatol. 2022, 19, 60–78. [Google Scholar] [CrossRef] [PubMed]
- Buzzetti, E.; Pinzani, M.; Tsochatzis, E.A. The Multiple-Hit Pathogenesis of Non-Alcoholic Fatty Liver Disease (NAFLD). Metabolism 2016, 65, 1038–1048. [Google Scholar] [CrossRef] [PubMed]
- Onakpoya, I.J.; Heneghan, C.J.; Aronson, J.K. Post-Marketing Withdrawal of Anti-Obesity Medicinal Products Because of Adverse Drug Reactions: A Systematic Review. BMC Med. 2016, 14, 191. [Google Scholar] [CrossRef]
- Zhang, C.; Yang, M. Current Options and Future Directions for NAFLD and NASH Treatment. Int. J. Mol. Sci. 2021, 22, 7571. [Google Scholar] [CrossRef]
- Estes, C.; Razavi, H.; Loomba, R.; Younossi, Z.; Sanyal, A.J. Modeling the Epidemic of Nonalcoholic Fatty Liver Disease Demonstrates an Exponential Increase in Burden of Disease. Hepatology 2018, 67, 123–133. [Google Scholar] [CrossRef]
- Tung, Y.-T.; Zeng, J.-L.; Ho, S.-T.; Xu, J.-W.; Li, S.; Wu, J.-H. Anti-NAFLD Effect of Djulis Hull and Its Major Compound, Rutin, in Mice with High-Fat Diet (HFD)-Induced Obesity. Antioxidants 2021, 10, 1694. [Google Scholar] [CrossRef]
- Reddy, J.K.; Rao, M.S. Lipid Metabolism and Liver Inflammation. II. Fatty Liver Disease and Fatty Acid Oxidation. Am. J. Physiol. Gastrointest. Liver Physiol. 2006, 290, G852–G858. [Google Scholar] [CrossRef]
- Tan, B.L.; Norhaizan, M.E. Effect of High-Fat Diets on Oxidative Stress, Cellular Inflammatory Response and Cognitive Function. Nutrients 2019, 11, 2579. [Google Scholar] [CrossRef]
- Ferré, P.; Foufelle, F. Hepatic Steatosis: A Role for de Novo Lipogenesis and the Transcription Factor SREBP-1c. Diabetes Obes. Metab. 2010, 12, 83–92. [Google Scholar] [CrossRef]
- So, W.Y.; Leung, P.S. Irisin Ameliorates Hepatic Glucose/Lipid Metabolism and Enhances Cell Survival in Insulin-Resistant Human HepG2 Cells through Adenosine Monophosphate-Activated Protein Kinase Signaling. Int. J. Biochem. Cell Biol. 2016, 78, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.G.; Hayden, M.S.; Ghosh, S. NF-ΚB, Inflammation, and Metabolic Disease. Cell Metab. 2011, 13, 11–22. [Google Scholar] [CrossRef]
- Zhou, Y.-J.; Xu, N.; Zhang, X.-C.; Zhu, Y.-Y.; Liu, S.-W.; Chang, Y.-N. Chrysin Improves Glucose and Lipid Metabolism Disorders by Regulating the AMPK/PI3K/AKT Signaling Pathway in Insulin-Resistant HepG2 Cells and HFD/STZ-Induced C57BL/6J Mice. J. Agric. Food Chem. 2021, 69, 5618–5627. [Google Scholar] [CrossRef] [PubMed]
- Fki, I.; Sayadi, S.; Mahmoudi, A.; Daoued, I.; Marrekchi, R.; Ghorbel, H. Comparative Study on Beneficial Effects of Hydroxytyrosol- and Oleuropein-Rich Olive Leaf Extracts on High-Fat Diet-Induced Lipid Metabolism Disturbance and Liver Injury in Rats. BioMed Res. Int. 2020, 2020, e1315202. [Google Scholar] [CrossRef] [PubMed]
- Horrocks, L.A.; Yeo, Y.K. HEALTH BENEFITS OF DOCOSAHEXAENOIC ACID (DHA). Pharmacol. Res. 1999, 40, 211–225. [Google Scholar] [CrossRef]
- Chiu, C.-Y.; Wang, L.-P.; Liu, S.-H.; Chiang, M.-T. Fish Oil Supplementation Alleviates the Altered Lipid Homeostasis in Blood, Liver, and Adipose Tissues in High-Fat Diet-Fed Rats. J. Agric. Food Chem. 2018, 66, 4118–4128. [Google Scholar] [CrossRef]
- Lima Rocha, J.É.; Mendes Furtado, M.; Mello Neto, R.S.; da Silva Mendes, A.V.; Brito, A.K.d.S.; Sena de Almeida, J.O.C.; Rodrigues Queiroz, E.I.; de Sousa França, J.V.; Silva Primo, M.G.; Cunha Sales, A.L.d.C.; et al. Effects of Fish Oil Supplementation on Oxidative Stress Biomarkers and Liver Damage in Hypercholesterolemic Rats. Nutrients 2022, 14, 426. [Google Scholar] [CrossRef]
- Liu, Y.; Li, Q.; Wang, H.; Zhao, X.; Li, N.; Zhang, H.; Chen, G.; Liu, Z. Fish Oil Alleviates Circadian Bile Composition Dysregulation in Male Mice with NAFLD. J. Nutr. Biochem. 2019, 69, 53–62. [Google Scholar] [CrossRef]
- Markworth, J.F.; Kaur, G.; Miller, E.G.; Larsen, A.E.; Sinclair, A.J.; Rao Maddipati, K.; Cameron-Smith, D. Divergent Shifts in Lipid Mediator Profile Following Supplementation with N-3 Docosapentaenoic Acid and Eicosapentaenoic Acid. FASEB J. 2016, 30, 3714–3725. [Google Scholar] [CrossRef]
- Guo, X.; Sinclair, A.J.; Kaur, G.; Li, D. Differential Effects of EPA, DPA and DHA on Cardio-Metabolic Risk Factors in High-Fat Diet Fed Mice. Prostaglandins Leukot. Essent. Fatty Acids 2018, 136, 47–55. [Google Scholar] [CrossRef]
- Castilla-Madrigal, R.; Gil-Iturbe, E.; López de Calle, M.; Moreno-Aliaga, M.J.; Lostao, M.P. DHA and Its Derived Lipid Mediators MaR1, RvD1 and RvD2 Block TNF-α Inhibition of Intestinal Sugar and Glutamine Uptake in Caco-2 Cells. J. Nutr. Biochem. 2020, 76, 108264. [Google Scholar] [CrossRef] [PubMed]
- Hellmann, J.; Tang, Y.; Kosuri, M.; Bhatnagar, A.; Spite, M. Resolvin D1 Decreases Adipose Tissue Macrophage Accumulation and Improves Insulin Sensitivity in Obese-diabetic Mice. FASEB J. 2011, 25, 2399–2407. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Fernández, L.; González-Muniesa, P.; Laiglesia, L.M.; Sáinz, N.; Prieto-Hontoria, P.L.; Escoté, X.; Odriozola, L.; Corrales, F.J.; Arbones-Mainar, J.M.; Martínez, J.A.; et al. Maresin 1 Improves Insulin Sensitivity and Attenuates Adipose Tissue Inflammation in Ob/Ob and Diet-induced Obese Mice. FASEB J. 2017, 31, 2135–2145. [Google Scholar] [CrossRef]
- Valenzuela, R.; Videla, L.A. Impact of the Co-Administration of N-3 Fatty Acids and Olive Oil Components in Preclinical Nonalcoholic Fatty Liver Disease Models: A Mechanistic View. Nutrients 2020, 12, 499. [Google Scholar] [CrossRef] [PubMed]
- Illesca, P.; Valenzuela, R.; Espinosa, A.; Echeverría, F.; Soto-Alarcón, S.; Ortiz, M.; Campos, C.; Vargas, R.; Videla, L.A. The Metabolic Dysfunction of White Adipose Tissue Induced in Mice by a High-Fat Diet Is Abrogated by Co-Administration of Docosahexaenoic Acid and Hydroxytyrosol. Food Funct. 2020, 11, 9086–9102. [Google Scholar] [CrossRef]
- Wang, L.; Choi, H.S.; Su, Y.; Ju, J.-H.; Heo, S.-Y.; Yi, J.-J.; Oh, B.-R.; Jang, Y.-S.; Seo, J.-W. The Docosahexaenoic Acid Derivatives, DiHEP-DPA and TH-DPA, Synthesized via Recombinant Lipoxygenase, Ameliorate Disturbances in Lipid Metabolism and Liver Inflammation in High Fat Diet-Fed Mice. Life Sci. 2022, 291, 120219. [Google Scholar] [CrossRef]
- Kołakowski, A.; Kurzyna, P.F.; Bzdęga, W.; Żywno, H.; Harasim-Symbor, E.; Chabowski, A.; Konstantynowicz-Nowicka, K. Influence of Vitamin K2 on Lipid Precursors of Inflammation and Fatty Acids Pathway Activities in HepG2 Cells. Eur. J. Cell Biol. 2021, 100, 151188. [Google Scholar] [CrossRef]
- Szkudelski, T.; Dłużewicz, K.; Sadoch, J.; Szkudelska, K. Effects of the Activation of Heme Oxygenase-1 on Hormonal and Metabolic Changes in Rats Fed a High-Fat Diet. Biomed. Pharmacother. 2017, 87, 375–380. [Google Scholar] [CrossRef]
- Qu, J.; Huang, P.; Zhang, L.; Qiu, Y.; Qi, H.; Leng, A.; Shang, D. Hepatoprotective Effect of Plant Polysaccharides from Natural Resources: A Review of the Mechanisms and Structure-Activity Relationship. Int. J. Biol. Macromol. 2020, 161, 24–34. [Google Scholar] [CrossRef]
- Guelinckx, I.; Devlieger, R.; Mullie, P.; Vansant, G. Effect of Lifestyle Intervention on Dietary Habits, Physical Activity, and Gestational Weight Gain in Obese Pregnant Women: A Randomized Controlled Trial. Am. J. Clin. Nutr. 2010, 91, 373–380. [Google Scholar] [CrossRef]
- Postic, C.; Girard, J. Contribution of de Novo Fatty Acid Synthesis to Hepatic Steatosis and Insulin Resistance: Lessons from Genetically Engineered Mice. J. Clin. Investig. 2008, 118, 829–838. [Google Scholar] [CrossRef] [PubMed]
- Salsinha, A.S.; Rodríguez-Alcalá, L.M.; Relvas, J.B.; Pintado, M.E. Fatty Acids Role on Obesity Induced Hypothalamus Inflammation: From Problem to Solution—A Review. Trends Food Sci. Technol. 2021, 112, 592–607. [Google Scholar] [CrossRef]
- Fernandez, M.L.; Webb, D. The LDL to HDL Cholesterol Ratio as a Valuable Tool to Evaluate Coronary Heart Disease Risk. J. Am. Coll. Nutr. 2008, 27, 1–5. [Google Scholar] [CrossRef]
- Kasper, P.; Martin, A.; Lang, S.; Kütting, F.; Goeser, T.; Demir, M.; Steffen, H.-M. NAFLD and Cardiovascular Diseases: A Clinical Review. Clin. Res. Cardiol. 2021, 110, 921–937. [Google Scholar] [CrossRef] [PubMed]
- Yuan, F.; Wang, H.; Tian, Y.; Li, Q.; He, L.; Li, N.; Liu, Z. Fish Oil Alleviated High-Fat Diet–Induced Non-Alcoholic Fatty Liver Disease via Regulating Hepatic Lipids Metabolism and Metaflammation: A Transcriptomic Study. Lipids Health Dis. 2016, 15, 20. [Google Scholar] [CrossRef]
- Neuhofer, A.; Zeyda, M.; Mascher, D.; Itariu, B.K.; Murano, I.; Leitner, L.; Hochbrugger, E.E.; Fraisl, P.; Cinti, S.; Serhan, C.N.; et al. Impaired Local Production of Proresolving Lipid Mediators in Obesity and 17-HDHA as a Potential Treatment for Obesity-Associated Inflammation. Diabetes 2013, 62, 1945–1956. [Google Scholar] [CrossRef]
- Videla, L.A.; Pettinelli, P. Misregulation of PPAR Functioning and Its Pathogenic Consequences Associated with Nonalcoholic Fatty Liver Disease in Human Obesity. PPAR Res. 2012, 2012, 107434. [Google Scholar] [CrossRef]
- Ning, C.; Liu, L.; Lv, G.; Yang, Y.; Zhang, Y.; Yu, R.; Wang, Y.; Zhu, J. Lipid Metabolism and Inflammation Modulated by Vitamin D in Liver of Diabetic Rats. Lipids Health Dis. 2015, 14, 31. [Google Scholar] [CrossRef]




| Genes | Sequences (5′ → 3′) |
|---|---|
| Human PPAR-α | Forward: TCGGCGAGGATAGTTCTGGAAG |
| Reverse: GACCACAGGATAAGTCACCGAG | |
| Human CPT-1 | Forward: GATCCTGGACAATACCTCGGAG |
| Reverse: CTCCACAGCATCAAGAGACTGC | |
| Human SREBP-1 | Forward: ACTTCTGGAGGCATCGCAAGCA |
| Reverse: AGGTTCCAGAGGAGGCTACAAG | |
| Human FAS | Forward: TTCTACGGCTCCACGCTCTTCC |
| Reverse: GAAGAGTCTTCGTCAGCCAGGA | |
| Human GAPDH | Forward: GTCTCCTCTGACTTCAACAGCG |
| Reverse: ACCACCCTGTTGCTGTAGCCAA | |
| Mouse PPAR-α | Forward: TCATCAAGAAGACCGAGTCC |
| Reverse: CCTCTTCATCCCCAAGCGT | |
| Mouse CPT-1 | Forward: CATCCACGCCATACTGCT |
| Reverse: GACCTTGAAGTAACGGCCTC | |
| Mouse SREBP-1 | Forward: GGCACTAAGTGCCCTCAACCT |
| Reverse: GCCACATAGATCTCTGCCAGTGT | |
| Mouse FAS | Forward: GGCACCTATGGCGAGGACTT |
| Reverse: GCCCTCCCGTACACTCACTC | |
| Mouse GAPDH | Forward: CATCACTGCCACCCAGAAGACTG |
| Reverse: ATGCCAGTGAGCTTCCCGTTCAG | |
| Human PPAR-α | Forward: TCGGCGAGGATAGTTCTGGAAG |
| Reverse: GACCACAGGATAAGTCACCGAG | |
| Human CPT-1 | Forward: GATCCTGGACAATACCTCGGAG |
| Reverse: CTCCACAGCATCAAGAGACTGC | |
| Human SREBP-1 | Forward: ACTTCTGGAGGCATCGCAAGCA |
| Reverse: AGGTTCCAGAGGAGGCTACAAG | |
| Human FAS | Forward: TTCTACGGCTCCACGCTCTTCC |
| Reverse: GAAGAGTCTTCGTCAGCCAGGA | |
| Human GAPDH | Forward: GTCTCCTCTGACTTCAACAGCG |
| Reverse: ACCACCCTGTTGCTGTAGCCAA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, Y.; Choi, H.-S.; Choi, J.-H.; Kim, H.-S.; Lee, G.-Y.; Cho, H.-W.; Choi, H.; Jang, Y.-S.; Seo, J.-W. Effects of Fish Oil, Lipid Mediators, Derived from Docosahexaenoic Acid, and Their Co-Treatment against Lipid Metabolism Dysfunction and Inflammation in HFD Mice and HepG2 Cells. Nutrients 2023, 15, 427. https://doi.org/10.3390/nu15020427
Su Y, Choi H-S, Choi J-H, Kim H-S, Lee G-Y, Cho H-W, Choi H, Jang Y-S, Seo J-W. Effects of Fish Oil, Lipid Mediators, Derived from Docosahexaenoic Acid, and Their Co-Treatment against Lipid Metabolism Dysfunction and Inflammation in HFD Mice and HepG2 Cells. Nutrients. 2023; 15(2):427. https://doi.org/10.3390/nu15020427
Chicago/Turabian StyleSu, Yan, Hack-Sun Choi, Jong-Hyun Choi, Hee-Sik Kim, Gil-Yong Lee, Hee-Won Cho, Heonsik Choi, Yong-Suk Jang, and Jeong-Woo Seo. 2023. "Effects of Fish Oil, Lipid Mediators, Derived from Docosahexaenoic Acid, and Their Co-Treatment against Lipid Metabolism Dysfunction and Inflammation in HFD Mice and HepG2 Cells" Nutrients 15, no. 2: 427. https://doi.org/10.3390/nu15020427
APA StyleSu, Y., Choi, H.-S., Choi, J.-H., Kim, H.-S., Lee, G.-Y., Cho, H.-W., Choi, H., Jang, Y.-S., & Seo, J.-W. (2023). Effects of Fish Oil, Lipid Mediators, Derived from Docosahexaenoic Acid, and Their Co-Treatment against Lipid Metabolism Dysfunction and Inflammation in HFD Mice and HepG2 Cells. Nutrients, 15(2), 427. https://doi.org/10.3390/nu15020427






