Interlinkages between Climate Change and Food Systems: The Impact on Child Malnutrition—Narrative Review
Abstract
1. Introduction
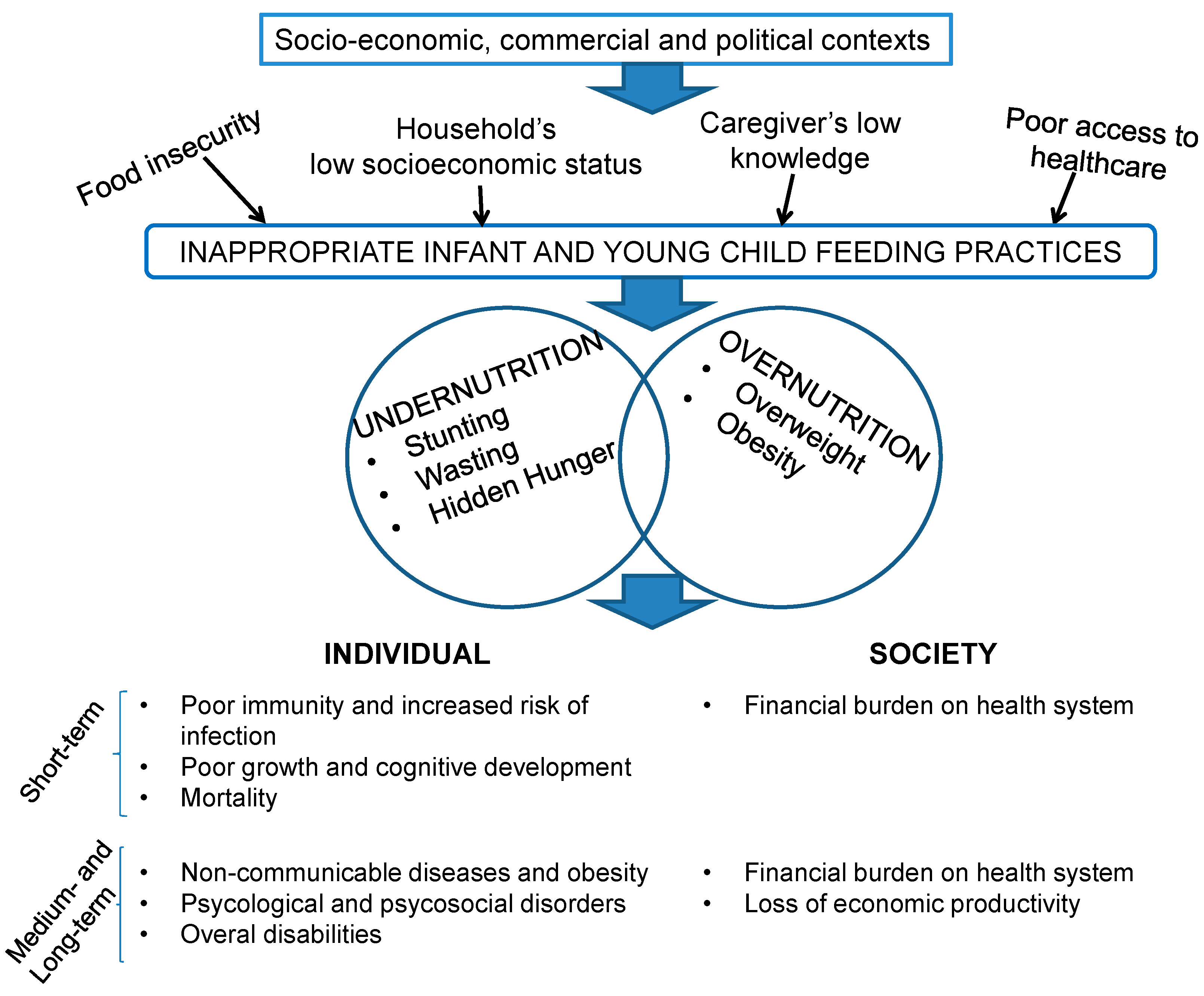
2. The Double Burden of Child Malnutrition: Epidemiology and Feeding Practices
3. Climate Change Interactions with the Agro-Ecosystem and Effects on Child Health
3.1. Effects on the Agro-Ecosystem, Food and Nutrition Security, and Livelihoods
3.2. Increasing Recurrence of Extreme Weather Events
3.3. The COVID-19 Pandemic
4. Food Systems and Sustainable Nutrition Early in Life
|
|
|
|
|
|
4.1. IYCF Practices and Food Systems: Existing Gaps
4.1.1. Sustainable Diets and IYCF
4.1.2. Market Mechanisms and IYCF
5. Approaches and Strategies
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization; United Nations Children’s Fund (UNICEF); World Bank. Levels and Trends in Child Malnutrition: UNICEF/WHO/The World Bank Group Joint Child Malnutrition Estimates: Key Findings of the 2021 Edition; World Health Organization: Geneva, Switzerland, 2021; ISBN 978-92-4-002525-7. [Google Scholar]
- Clark, H.; Ghebreyesus, T.A.; Albrectsen, A.-B.; Alcocer, J.; Alden, E.; Azoulay, A.; Billingsley, S.; Blum, R.W.; Bhushan, R.; Byanyima, W.; et al. Uniting for Adolescents in COVID-19 and Beyond. BMJ 2021, 372, n719. [Google Scholar] [CrossRef]
- Tong, S.; Bambrick, H.; Beggs, P.J.; Chen, L.; Hu, Y.; Ma, W.; Steffen, W.; Tan, J. Current and Future Threats to Human Health in the Anthropocene. Environ. Int. 2022, 158, 106892. [Google Scholar] [CrossRef] [PubMed]
- Watts, N.; Amann, M.; Arnell, N.; Ayeb-Karlsson, S.; Belesova, K.; Boykoff, M.; Byass, P.; Cai, W.; Campbell-Lendrum, D.; Capstick, S.; et al. The 2019 Report of The Lancet Countdown on Health and Climate Change: Ensuring That the Health of a Child Born Today Is Not Defined by a Changing Climate. Lancet 2019, 394, 1836–1878. [Google Scholar] [CrossRef] [PubMed]
- Watts, N.; Amann, M.; Arnell, N.; Ayeb-Karlsson, S.; Beagley, J.; Belesova, K.; Boykoff, M.; Byass, P.; Cai, W.; Campbell-Lendrum, D.; et al. The 2020 Report of The Lancet Countdown on Health and Climate Change: Responding to Converging Crises. Lancet 2021, 397, 129–170. [Google Scholar] [CrossRef]
- Victora, C.G.; Christian, P.; Vidaletti, L.P.; Gatica-Domínguez, G.; Menon, P.; Black, R.E. Revisiting Maternal and Child Undernutrition in Low-Income and Middle-Income Countries: Variable Progress towards an Unfinished Agenda. Lancet 2021, 397, 1388–1399. [Google Scholar] [CrossRef]
- Swinburn, B.A.; Kraak, V.I.; Allender, S.; Atkins, V.J.; Baker, P.I.; Bogard, J.R.; Brinsden, H.; Calvillo, A.; De Schutter, O.; Devarajan, R.; et al. The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission Report. Lancet 2019, 393, 791–846. [Google Scholar] [CrossRef]
- Grey, K.; Gonzales, G.B.; Abera, M.; Lelijveld, N.; Thompson, D.; Berhane, M.; Abdissa, A.; Girma, T.; Kerac, M. Severe Malnutrition or Famine Exposure in Childhood and Cardiometabolic Non-Communicable Disease Later in Life: A Systematic Review. BMJ Glob. Health 2021, 6, e003161. [Google Scholar] [CrossRef] [PubMed]
- Akombi, B.; Agho, K.; Hall, J.; Wali, N.; Renzaho, A.; Merom, D. Stunting, Wasting and Underweight in Sub-Saharan Africa: A Systematic Review. Int. J. Environ. Res. Public Health 2017, 14, 863. [Google Scholar] [CrossRef]
- Millward, D.J. Nutrition, Infection and Stunting: The Roles of Deficiencies of Individual Nutrients and Foods, and of Inflammation, as Determinants of Reduced Linear Growth of Children. Nutr. Res. Rev. 2017, 30, 50–72. [Google Scholar] [CrossRef]
- Vaivada, T.; Akseer, N.; Akseer, S.; Somaskandan, A.; Stefopulos, M.; Bhutta, Z.A. Stunting in Childhood: An Overview of Global Burden, Trends, Determinants, and Drivers of Decline. Am. J. Clin. Nutr. 2020, 112, 777S–791S. [Google Scholar] [CrossRef]
- Li, Z.; Kim, R.; Vollmer, S.; Subramanian, S.V. Factors Associated with Child Stunting, Wasting, and Underweight in 35 Low- and Middle-Income Countries. JAMA Netw. Open 2020, 3, e203386. [Google Scholar] [CrossRef] [PubMed]
- De Onis, M.; Branca, F. Childhood Stunting: A Global Perspective: Childhood Stunting: A Global Perspective. Matern. Child Nutr. 2016, 12, 12–26. [Google Scholar] [CrossRef] [PubMed]
- De Sanctis, V.; Soliman, A.; Alaaraj, N.; Ahmed, S.; Alyafei, F.; Hamed, N. Early and Long-Term Consequences of Nutritional Stunting: From Childhood to Adulthood: Early and Long-Term Consequences of Nutritional Stunting. Acta Bio Med. Atenei Parm. 2021, 92, 11346. [Google Scholar] [CrossRef]
- Montenegro, C.R.; Gomez, G.; Hincapie, O.; Dvoretskiy, S.; DeWitt, T.; Gracia, D.; Misas, J.D. The Pediatric Global Burden of Stunting: Focus on Latin America. Lifestyle Med. 2022, 3, e67. [Google Scholar] [CrossRef]
- UNICEF. The State of the World’s Children 2019. Children, Food and Nutrition: Growing Well in a Changing World; UNICEF: New York, NY, USA, 2019. [Google Scholar]
- Blüher, M. Obesity: Global Epidemiology and Pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef]
- Reinehr, T. Long-Term Effects of Adolescent Obesity: Time to Act. Nat. Rev. Endocrinol. 2018, 14, 183–188. [Google Scholar] [CrossRef]
- Berti, C.; Agostoni, C.; Davanzo, R.; Hyppönen, E.; Isolauri, E.; Meltzer, H.M.; Steegers-Theunissen, R.P.M.; Cetin, I. Early-Life Nutritional Exposures and Lifelong Health: Immediate and Long-Lasting Impacts of Probiotics, Vitamin D, and Breastfeeding. Nutr. Rev. 2017, 75, 83–97. [Google Scholar] [CrossRef]
- Hollis, J.L.; Collins, C.E.; DeClerck, F.; Chai, L.K.; McColl, K.; Demaio, A.R. Defining Healthy and Sustainable Diets for Infants, Children and Adolescents. Glob. Food Secur. 2020, 27, 100401. [Google Scholar] [CrossRef]
- Baker, P.; Santos, T.; Neves, P.A.; Machado, P.; Smith, J.; Piwoz, E.; Barros, A.J.D.; Victora, C.G.; McCoy, D. First-food Systems Transformations and the Ultra-processing of Infant and Young Child Diets: The Determinants, Dynamics and Consequences of the Global Rise in Commercial Milk Formula Consumption. Matern. Child Nutr. 2021, 17, e13097. [Google Scholar] [CrossRef]
- Barrera, C.M.; Hamner, H.C.; Perrine, C.G.; Scanlon, K.S. Timing of Introduction of Complementary Foods to US Infants, National Health and Nutrition Examination Survey 2009–2014. J. Acad. Nutr. Diet. 2018, 118, 464–470. [Google Scholar] [CrossRef]
- White, J.M.; Bégin, F.; Kumapley, R.; Murray, C.; Krasevec, J. Complementary Feeding Practices: Current Global and Regional Estimates. Matern. Child Nutr. 2017, 13, e12505. [Google Scholar] [CrossRef] [PubMed]
- Walters, D.D.; Phan, L.T.H.; Mathisen, R. The Cost of Not Breastfeeding: Global Results from a New Tool. Health Policy Plan. 2019, 34, 407–417. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The International Code of Marketing of Breast-Milk Substitutes: Frequently Asked Questions (2017 Update); World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Baker, P.; Machado, P.; Santos, T.; Sievert, K.; Backholer, K.; Hadjikakou, M.; Russell, C.; Huse, O.; Bell, C.; Scrinis, G.; et al. Ultra-Processed Foods and the Nutrition Transition: Global, Regional and National Trends, Food Systems Transformations and Political Economy Drivers. Obes. Rev. 2020, 21, e13126. [Google Scholar] [CrossRef]
- Hollis, J.L.; Demaio, S.; Yang, W.Y.; Trijsburg, L.; Brouwer, I.D.; Jewell, J.; Johns, P.; DeClerck, F.; Collins, C.E. Investing in Early Nutrition and Food Systems for Human and Planetary Health. Lancet Child Adolesc. Health 2021, 5, 772–774. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Corvalan, C.; Grummer-Strawn, L.M. Dynamics of the Double Burden of Malnutrition and the Changing Nutrition Reality. Lancet 2020, 395, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Fanzo, J.; Bellows, A.L.; Spiker, M.L.; Thorne-Lyman, A.L.; Bloem, M.W. The Importance of Food Systems and the Environment for Nutrition. Am. J. Clin. Nutr. 2021, 113, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Headey, D.D.; Alderman, H.H. The Relative Caloric Prices of Healthy and Unhealthy Foods Differ Systematically across Income Levels and Continents. J. Nutr. 2019, 149, 2020–2033. [Google Scholar] [CrossRef]
- Tester, J.M.; Rosas, L.G.; Leung, C.W. Food Insecurity and Pediatric Obesity: A Double Whammy in the Era of COVID-19. Curr. Obes. Rep. 2020, 9, 442–450. [Google Scholar] [CrossRef]
- Bommer, C.; Vollmer, S.; Subramanian, S.V. How Socioeconomic Status Moderates the Stunting-Age Relationship in Low-Income and Middle-Income Countries. BMJ Glob. Health 2019, 4, e001175. [Google Scholar] [CrossRef]
- Ekholuenetale, M.; Tudeme, G.; Onikan, A.; Ekholuenetale, C.E. Socioeconomic Inequalities in Hidden Hunger, Undernutrition, and Overweight among under-Five Children in 35 Sub-Saharan Africa Countries. J. Egypt. Public Health Assoc. 2020, 95, 9. [Google Scholar] [CrossRef]
- Staatz, C.B.; Kelly, Y.; Lacey, R.E.; Hardy, R. Area-Level and Family-Level Socioeconomic Position and Body Composition Trajectories: Longitudinal Analysis of the UK Millennium Cohort Study. Lancet Public Health 2021, 6, e598–e607. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Review of Social Determinants and the Health Divide in the WHO European Region: Final Report; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2013. [Google Scholar]
- Development Initiatives. Global Nutrition Report: Action on Equity to End Malnutrition; Development Initiatives Poverty Research Ltd.: Bristol, UK, 2020. [Google Scholar]
- Myers, S.S.; Smith, M.R.; Guth, S.; Golden, C.D.; Vaitla, B.; Mueller, N.D.; Dangour, A.D.; Huybers, P. Climate Change and Global Food Systems: Potential Impacts on Food Security and Undernutrition. Annu. Rev. Public Health 2017, 38, 259–277. [Google Scholar] [CrossRef] [PubMed]
- Awiti, A.O. Climate Change and Gender in Africa: A Review of Impact and Gender-Responsive Solutions. Front. Clim. 2022, 4, 895950. [Google Scholar] [CrossRef]
- Hess, J.; Boodram, L.-L.G.; Paz, S.; Stewart Ibarra, A.M.; Wasserheit, J.N.; Lowe, R. Strengthening the Global Response to Climate Change and Infectious Disease Threats. BMJ 2020, 371, m3081. [Google Scholar] [CrossRef]
- Frieler, K.; Levermann, A.; Elliott, J.; Heinke, J.; Arneth, A.; Bierkens, M.F.P.; Ciais, P.; Clark, D.B.; Deryng, D.; Döll, P.; et al. A Framework for the Cross-Sectoral Integration of Multi-Model Impact Projections: Land Use Decisions under Climate Impacts Uncertainties. Earth Syst. Dynam. 2015, 6, 447–460. [Google Scholar] [CrossRef]
- Food and Agriculture Organization of the United Nations. Climate Change and Food Security: Risks and Responses; FAO: Rome, Italy, 2015. [Google Scholar]
- Uleberg, E.; Hanssen-Bauer, I.; van Oort, B.; Dalmannsdottir, S. Impact of Climate Change on Agriculture in Northern Norway and Potential Strategies for Adaptation. Clim. Change 2014, 122, 27–39. [Google Scholar] [CrossRef]
- Salih, A.A.M.; Baraibar, M.; Mwangi, K.K.; Artan, G. Climate Change and Locust Outbreak in East Africa. Nat. Clim. Chang. 2020, 10, 584–585. [Google Scholar] [CrossRef]
- Cissé, G. Food-Borne and Water-Borne Diseases under Climate Change in Low- and Middle-Income Countries: Further Efforts Needed for Reducing Environmental Health Exposure Risks. Acta Trop. 2019, 194, 181–188. [Google Scholar] [CrossRef]
- Levy, K.; Smith, S.M.; Carlton, E.J. Climate Change Impacts on Waterborne Diseases: Moving Toward Designing Interventions. Curr. Environ. Health Rep. 2018, 5, 272–282. [Google Scholar] [CrossRef]
- Leggieri, M.C.; Toscano, P.; Battilani, P. Predicted Aflatoxin B1 Increase in Europe Due to Climate Change: Actions and Reactions at Global Level. Toxins 2021, 13, 292. [Google Scholar] [CrossRef]
- World Health Organization. Quantitative Risk Assessment of the Effects of Climate Change on Selected Causes of Death, 2030s and 2050s; World Health Organization: Geneva, Switzerland, 2014; ISBN 978-92-4-150769-1. [Google Scholar]
- Perry, A.L.; Low, P.J.; Ellis, J.R.; Reynolds, J.D. Climate Change and Distribution Shifts in Marine Fishes. Science 2005, 308, 1912–1915. [Google Scholar] [CrossRef] [PubMed]
- Pörtner, H. Ecosystem Effects of Ocean Acidification in Times of Ocean Warming: A Physiologist’s View. Mar. Ecol. Prog. Ser. 2008, 373, 203–217. [Google Scholar] [CrossRef]
- Allen, C.D.; Macalady, A.K.; Chenchouni, H.; Bachelet, D.; McDowell, N.; Vennetier, M.; Kitzberger, T.; Rigling, A.; Breshears, D.D.; Hogg, E.H.; et al. A Global Overview of Drought and Heat-Induced Tree Mortality Reveals Emerging Climate Change Risks for Forests. For. Ecol. Manag. 2010, 259, 660–684. [Google Scholar] [CrossRef]
- Hooper, D.U.; Adair, E.C.; Cardinale, B.J.; Byrnes, J.E.K.; Hungate, B.A.; Matulich, K.L.; Gonzalez, A.; Duffy, J.E.; Gamfeldt, L.; O’Connor, M.I. A Global Synthesis Reveals Biodiversity Loss as a Major Driver of Ecosystem Change. Nature 2012, 486, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Gamfeldt, L.; Snäll, T.; Bagchi, R.; Jonsson, M.; Gustafsson, L.; Kjellander, P.; Ruiz-Jaen, M.C.; Fröberg, M.; Stendahl, J.; Philipson, C.D.; et al. Higher Levels of Multiple Ecosystem Services Are Found in Forests with More Tree Species. Nat. Commun. 2013, 4, 1340. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.; Giese, M.; Chen, D. Flood Impact on Mainland Southeast Asia between 1985 and 2018—The Role of Tropical Cyclones. J. Flood Risk Manag. 2020, 13, e12598. [Google Scholar] [CrossRef]
- OXFAM. Hunger in a Heating World. How the Climate Crisis Is Fuelling Hunger in an Already Hungry World; OXFAM International: Oxford, UK, 2022. [Google Scholar]
- Molua, E.L.; Mendelsohn, R.O.; Akamin, A. Economic Vulnerability to Tropical Storms on the Southeastern Coast of Africa. Jàmbá J. Disaster Risk Stud. 2020, 12, 1–14. [Google Scholar] [CrossRef]
- Abeldaño Zuñiga, R.A.; Fanta Garrido, J. Internal Displacement Due to Disasters in Latin America and the Caribbean. In Climate Change, Hazards and Adaptation Options; Leal Filho, W., Nagy, G.J., Borga, M., Chávez Muñoz, P.D., Magnuszewski, A., Eds.; Climate Change Management; Springer International Publishing: Cham, Switzerland, 2020; pp. 389–409. ISBN 978-3-030-37424-2. [Google Scholar]
- Lieber, M.; Chin-Hong, P.; Kelly, K.; Dandu, M.; Weiser, S.D. A Systematic Review and Meta-Analysis Assessing the Impact of Droughts, Flooding, and Climate Variability on Malnutrition. Glob. Public Health 2022, 17, 68–82. [Google Scholar] [CrossRef] [PubMed]
- Park, C.S.; Vogel, E.; Larson, L.M.; Myers, S.S.; Daniel, M.; Biggs, B.-A. The Global Effect of Extreme Weather Events on Nutrient Supply: A Superposed Epoch Analysis. Lancet Planet. Health 2019, 3, e429–e438. [Google Scholar] [CrossRef] [PubMed]
- Shubravska, O.; Prokopenko, K. The Agricultural Sector of Ukraine in the Global Food Market: Pre-War State and Post-War Prospects. Res. World Agric. Econ. 2022, 3, 1. [Google Scholar] [CrossRef]
- Fanzo, J.; Rudie, C.; Sigman, I.; Grinspoon, S.; Benton, T.G.; Brown, M.E.; Covic, N.; Fitch, K.; Golden, C.D.; Grace, D.; et al. Sustainable Food Systems and Nutrition in the 21st Century: A Report from the 22nd Annual Harvard Nutrition Obesity Symposium. Am. J. Clin. Nutr. 2022, 115, 18–33. [Google Scholar] [CrossRef] [PubMed]
- United Nations Department for Economic and Social Affairs. Sustainable Development Goals Report 2022; United Nations: New York, NY, USA, 2022; ISBN 978-92-1-101448-8.
- Baral, S.; Rao, A.; Rwema, J.O.T.; Lyons, C.; Cevik, M.; Kågesten, A.E.; Diouf, D.; Sohn, A.H.; Phaswana-Mafuya, R.N.; Kamarulzaman, A.; et al. Competing Health Risks Associated with the COVID-19 Pandemic and Early Response: A Scoping Review. PLoS ONE 2022, 17, e0273389. [Google Scholar] [CrossRef] [PubMed]
- Carducci, B.; Keats, E.C.; Ruel, M.; Haddad, L.; Osendarp, S.J.M.; Bhutta, Z.A. Food Systems, Diets and Nutrition in the Wake of COVID-19. Nat. Food 2021, 2, 68–70. [Google Scholar] [CrossRef]
- Knebusch, V.; Williams, J.; Yordi Aguirre, I.; Weber, M.W.; Rakovac, I.; Breda, J. Effects of the Coronavirus Disease 2019 Pandemic and the Policy Response on Childhood Obesity Risk Factors: Gender and Sex Differences and Recommendations for Research. Obes. Rev. 2021, 22, e13222. [Google Scholar] [CrossRef]
- Pérez-Escamilla, R.; Cunningham, K.; Moran, V.H. COVID-19 and Maternal and Child Food and Nutrition Insecurity: A Complex Syndemic. Matern. Child Nutr. 2020, 16, e13036. [Google Scholar] [CrossRef]
- Verhagen, W.; Bohl, D.; Cannon, M.; Pulido, A.; Pirzadeh, A.; Nott, I.; Moyer, J.D. The Future of Food Security in the Wake of a Global Pandemic. Report; United States Agency for International Development: Washington, DC, USA, 2021.
- Adams, E.L.; Caccavale, L.J.; Smith, D.; Bean, M.K. Food Insecurity, the Home Food Environment, and Parent Feeding Practices in the Era of COVID-19. Obesity 2020, 28, 2056–2063. [Google Scholar] [CrossRef]
- Bairagi, S.; Mishra, A.K.; Mottaleb, K.A. Impacts of the COVID-19 Pandemic on Food Prices: Evidence from Storable and Perishable Commodities in India. PLoS ONE 2022, 17, e0264355. [Google Scholar] [CrossRef] [PubMed]
- Jafri, A.; Mathe, N.; Aglago, E.K.; Konyole, S.O.; Ouedraogo, M.; Audain, K.; Zongo, U.; Laar, A.K.; Johnson, J.; Sanou, D. Food Availability, Accessibility and Dietary Practices during the COVID-19 Pandemic: A Multi-Country Survey. Public Health Nutr. 2021, 24, 1798–1805. [Google Scholar] [CrossRef]
- Balakrishnan, V.S. Greater Horn of Africa’s Crown of Thorns. Lancet Child Adolesc. Health 2022, 6, 757–758. [Google Scholar] [CrossRef]
- World Food Programme. WFP Annual Review 2021; World Food Programme: Rome, Italy, 2022. [Google Scholar]
- UNICEF. Child Alert: Severe Wasting; UNICEF: New York, NY, USA, 2022. [Google Scholar]
- Headey, D.; Heidkamp, R.; Osendarp, S.; Ruel, M.; Scott, N.; Black, R.; Shekar, M.; Bouis, H.; Flory, A.; Haddad, L.; et al. Impacts of COVID-19 on Childhood Malnutrition and Nutrition-Related Mortality. Lancet 2020, 396, 519–521. [Google Scholar] [CrossRef]
- Osendarp, S.; Akuoku, J.K.; Black, R.E.; Headey, D.; Ruel, M.; Scott, N.; Shekar, M.; Walker, N.; Flory, A.; Haddad, L.; et al. The COVID-19 Crisis Will Exacerbate Maternal and Child Undernutrition and Child Mortality in Low- and Middle-Income Countries. Nat. Food 2021, 2, 476–484. [Google Scholar] [CrossRef]
- Jansen, E.; Thapaliya, G.; Aghababian, A.; Sadler, J.; Smith, K.; Carnell, S. Parental Stress, Food Parenting Practices and Child Snack Intake during the COVID-19 Pandemic. Appetite 2021, 161, 105119. [Google Scholar] [CrossRef] [PubMed]
- Food and Agriculture Organization of the United Nations. Sustainable Food Systems. Concept and Framework; FAO: Rome, Italy, 2018. [Google Scholar]
- Food and Agriculture Organization of the United Nations. Food Systems for Better Nutrition; FAO: Rome, Italy, 2013; ISBN 978-92-5-107671-2. [Google Scholar]
- Ingram, J. A Food Systems Approach to Researching Food Security and Its Interactions with Global Environmental Change. Food Sec. 2011, 3, 417–431. [Google Scholar] [CrossRef]
- International Panel of Experts on Sustainable Food Systems. The New Science of Sustainable Food Systems (No. 01). The Case for a New Science of Sustainable Food Systems; IPES-Food: Brussels, Belgium, 2015. [Google Scholar]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on Healthy Diets from Sustainable Food Systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef] [PubMed]
- Friel, S.; Schram, A.; Townsend, B. The Nexus between International Trade, Food Systems, Malnutrition and Climate Change. Nat. Food 2020, 1, 51–58. [Google Scholar] [CrossRef]
- Schram, A.; Townsend, B. International Trade and Investment and Food Systems: What We Know, What We Don’t Know, and What We Don’t Know We Don’t Know. Int. J. Health Policy Manag. 2020, 10, 886–895. [Google Scholar] [CrossRef]
- Global Panel. Rethinking Trade Policies to Support Healthier Diets. Policy Brief No. 13; Global Panel on Agriculture and Food Systems for Nutrition: London, UK, 2020. [Google Scholar]
- Wijerathna-Yapa, A.; Pathirana, R. Sustainable Agro-Food Systems for Addressing Climate Change and Food Security. Agriculture 2022, 12, 1554. [Google Scholar] [CrossRef]
- Davidove, M.E.; Dorsey, J.W. Breastfeeding: A Cornerstone of Healthy Sustainable Diets. Sustainability 2019, 11, 4958. [Google Scholar] [CrossRef]
- Mazzocchi, A.; De Cosmi, V.; Scaglioni, S.; Agostoni, C. Towards a More Sustainable Nutrition: Complementary Feeding and Early Taste Experiences as a Basis for Future Food Choices. Nutrients 2021, 13, 2695. [Google Scholar] [CrossRef]
- Scaglioni, S.; De Cosmi, V.; Ciappolino, V.; Parazzini, F.; Brambilla, P.; Agostoni, C. Factors Influencing Children’s Eating Behaviours. Nutrients 2018, 10, 706. [Google Scholar] [CrossRef]
- Donini, L.M.; Dernini, S.; Lairon, D.; Serra-Majem, L.; Amiot, M.-J.; del Balzo, V.; Giusti, A.-M.; Burlingame, B.; Belahsen, R.; Maiani, G.; et al. A Consensus Proposal for Nutritional Indicators to Assess the Sustainability of a Healthy Diet: The Mediterranean Diet as a Case Study. Front. Nutr. 2016, 3, 37. [Google Scholar] [CrossRef] [PubMed]
- Gazan, R.; Brouzes, C.M.C.; Vieux, F.; Maillot, M.; Lluch, A.; Darmon, N. Mathematical Optimization to Explore Tomorrow’s Sustainable Diets: A Narrative Review. Adv. Nutr. 2018, 9, 602–616. [Google Scholar] [CrossRef]
- Gustafson, D.; Gutman, A.; Leet, W.; Drewnowski, A.; Fanzo, J.; Ingram, J. Seven Food System Metrics of Sustainable Nutrition Security. Sustainability 2016, 8, 196. [Google Scholar] [CrossRef]
- Eme, P.; Douwes, J.; Kim, N.; Foliaki, S.; Burlingame, B. Review of Methodologies for Assessing Sustainable Diets and Potential for Development of Harmonised Indicators. Int. J. Environ. Res. Public Health 2019, 16, 1184. [Google Scholar] [CrossRef]
- Shaw, H.J. Food Deserts: Towards the Development of a Classification. Geogr. Ann. Ser. B Hum. Geogr. 2006, 88, 231–247. [Google Scholar] [CrossRef]
- Sushil, Z.; Vandevijvere, S.; Exeter, D.J.; Swinburn, B. Food Swamps by Area Socioeconomic Deprivation in New Zealand: A National Study. Int. J. Public Health 2017, 62, 869–877. [Google Scholar] [CrossRef] [PubMed]
- Zarocostas, J. Hope for Nutrition Summit as Global Hunger Spikes. Lancet 2021, 398, 2061–2062. [Google Scholar] [CrossRef]
- Hawkes, C.; Ruel, M.T.; Salm, L.; Sinclair, B.; Branca, F. Double-Duty Actions: Seizing Programme and Policy Opportunities to Address Malnutrition in All Its Forms. Lancet 2020, 395, 142–155. [Google Scholar] [CrossRef]
- Heidkamp, R.A.; Piwoz, E.; Gillespie, S.; Keats, E.C.; D’Alimonte, M.R.; Menon, P.; Das, J.K.; Flory, A.; Clift, J.W.; Ruel, M.T.; et al. Mobilising Evidence, Data, and Resources to Achieve Global Maternal and Child Undernutrition Targets and the Sustainable Development Goals: An Agenda for Action. Lancet 2021, 397, 1400–1418. [Google Scholar] [CrossRef]
- Keats, E.C.; Das, J.K.; Salam, R.A.; Lassi, Z.S.; Imdad, A.; Black, R.E.; Bhutta, Z.A. Effective Interventions to Address Maternal and Child Malnutrition: An Update of the Evidence. Lancet Child Adolesc. Health 2021, 5, 367–384. [Google Scholar] [CrossRef]
- Castaldi, S.; Dembska, K.; Antonelli, M.; Petersson, T.; Piccolo, M.G.; Valentini, R. The Positive Climate Impact of the Mediterranean Diet and Current Divergence of Mediterranean Countries towards Less Climate Sustainable Food Consumption Patterns. Sci. Rep. 2022, 12, 8847. [Google Scholar] [CrossRef] [PubMed]
- Malhi, G.S.; Kaur, M.; Kaushik, P. Impact of Climate Change on Agriculture and Its Mitigation Strategies: A Review. Sustainability 2021, 13, 1318. [Google Scholar] [CrossRef]
- Sharafi, L.; Zarafshani, K.; Keshavarz, M.; Azadi, H.; Van Passel, S. Farmers’ Decision to Use Drought Early Warning System in Developing Countries. Sci. Total Environ. 2021, 758, 142761. [Google Scholar] [CrossRef]
- Béné, C. Resilience of Local Food Systems and Links to Food Security—A Review of Some Important Concepts in the Context of COVID-19 and Other Shocks. Food Secur. 2020, 12, 805–822. [Google Scholar] [CrossRef]
- Baudron, F.; Liégeois, F. Fixing Our Global Agricultural System to Prevent the next COVID-19. Outlook Agric. 2020, 49, 111–118. [Google Scholar] [CrossRef]
- Darnhofer, I. Farm Resilience in the Face of the Unexpected: Lessons from the COVID-19 Pandemic. Agric. Hum. Values 2020, 37, 605–606. [Google Scholar] [CrossRef] [PubMed]
- Henry, R. Innovations in Agriculture and Food Supply in Response to the COVID-19 Pandemic. Mol. Plant 2020, 13, 1095–1097. [Google Scholar] [CrossRef]
- Barrett, C.B. Actions Now Can Curb Food Systems Fallout from COVID-19. Nat. Food 2020, 1, 319–320. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agostoni, C.; Baglioni, M.; La Vecchia, A.; Molari, G.; Berti, C. Interlinkages between Climate Change and Food Systems: The Impact on Child Malnutrition—Narrative Review. Nutrients 2023, 15, 416. https://doi.org/10.3390/nu15020416
Agostoni C, Baglioni M, La Vecchia A, Molari G, Berti C. Interlinkages between Climate Change and Food Systems: The Impact on Child Malnutrition—Narrative Review. Nutrients. 2023; 15(2):416. https://doi.org/10.3390/nu15020416
Chicago/Turabian StyleAgostoni, Carlo, Mattia Baglioni, Adriano La Vecchia, Giulia Molari, and Cristiana Berti. 2023. "Interlinkages between Climate Change and Food Systems: The Impact on Child Malnutrition—Narrative Review" Nutrients 15, no. 2: 416. https://doi.org/10.3390/nu15020416
APA StyleAgostoni, C., Baglioni, M., La Vecchia, A., Molari, G., & Berti, C. (2023). Interlinkages between Climate Change and Food Systems: The Impact on Child Malnutrition—Narrative Review. Nutrients, 15(2), 416. https://doi.org/10.3390/nu15020416







