Diet Is Associated with Frailty in Lung Cancer: A Possible Role of Gut Microbiota
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. Sample Size Calculation
2.3. Frailty Assessment
2.4. Dietary Intake Assessment and the Calculation of CHEI Component Scores
2.5. Plasma Leucine Determination
2.6. Gut Microbiota Analysis
2.7. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Nutrient Intakes and CHEI Component Scores of the Patients
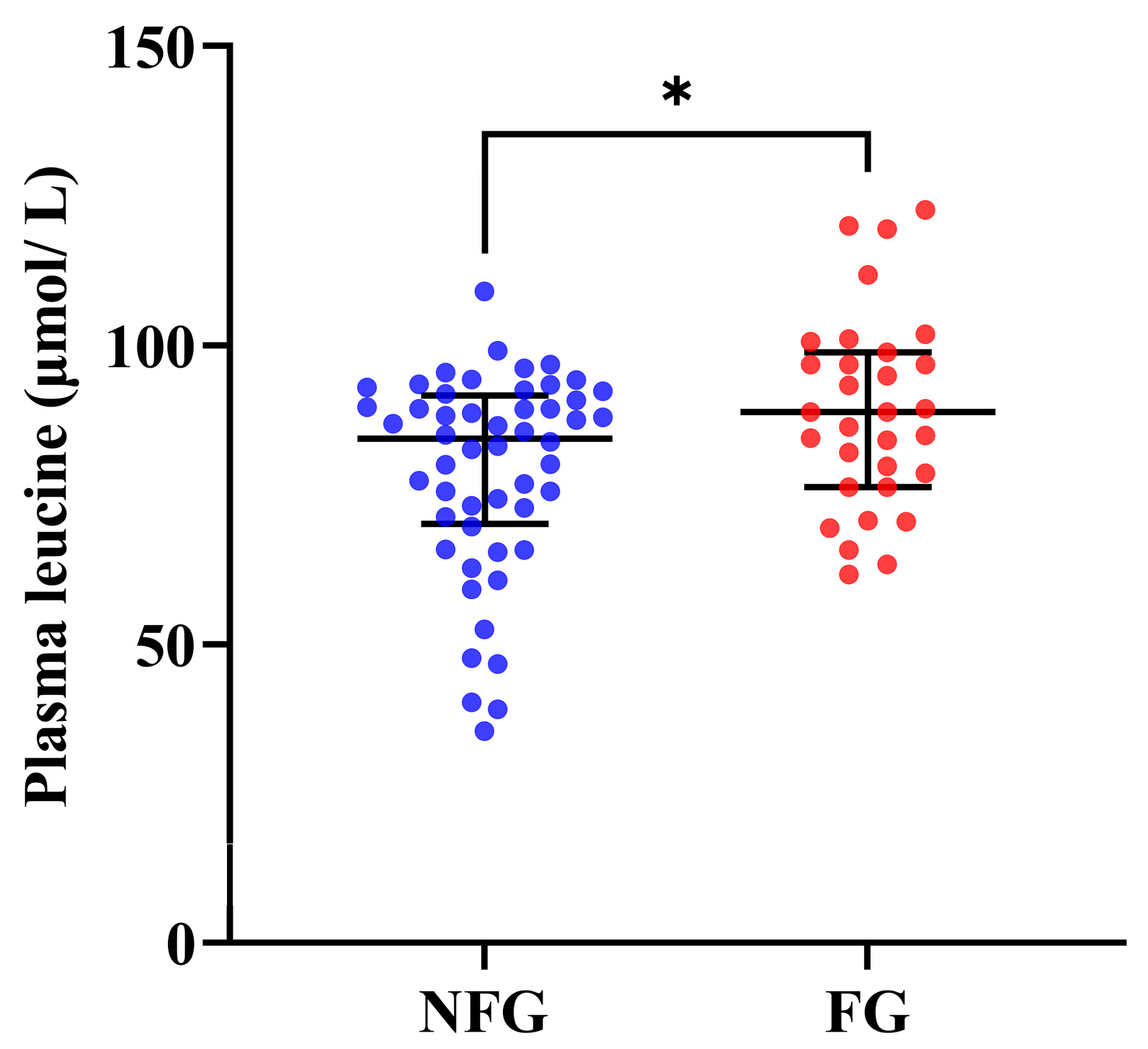
3.3. Plasma Leucine Levels of the Patients
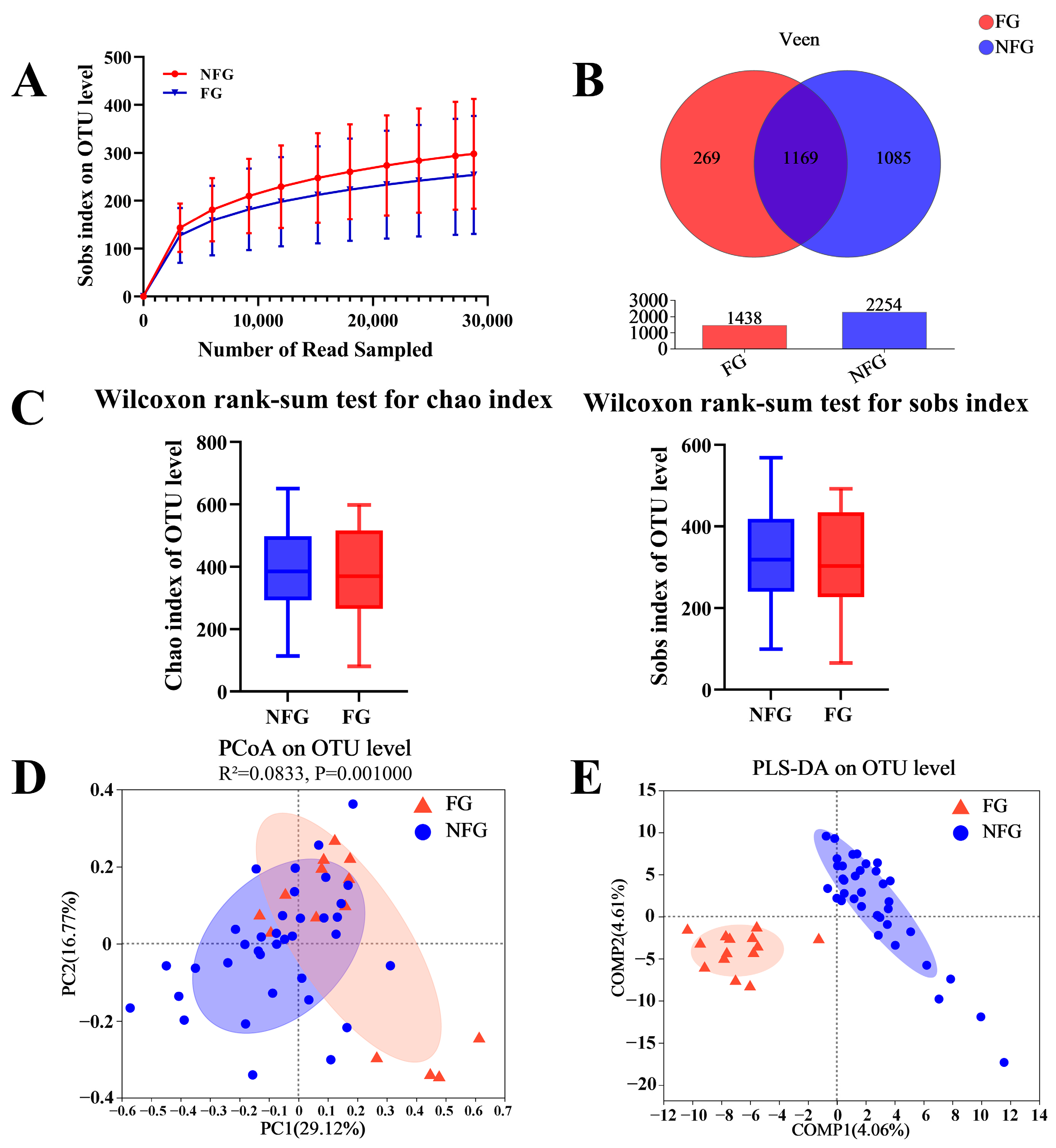
3.4. Gut Microbiota Diversity of the Patients
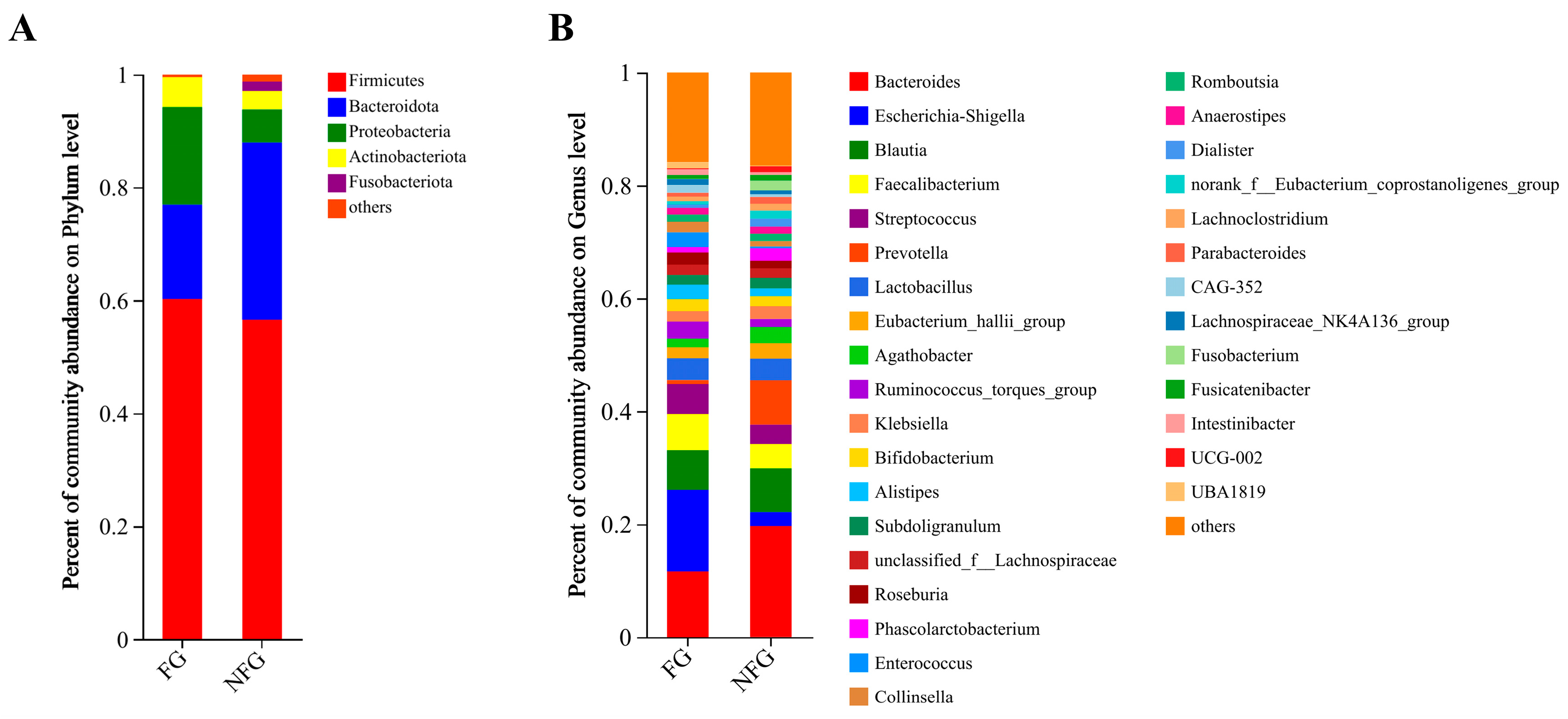
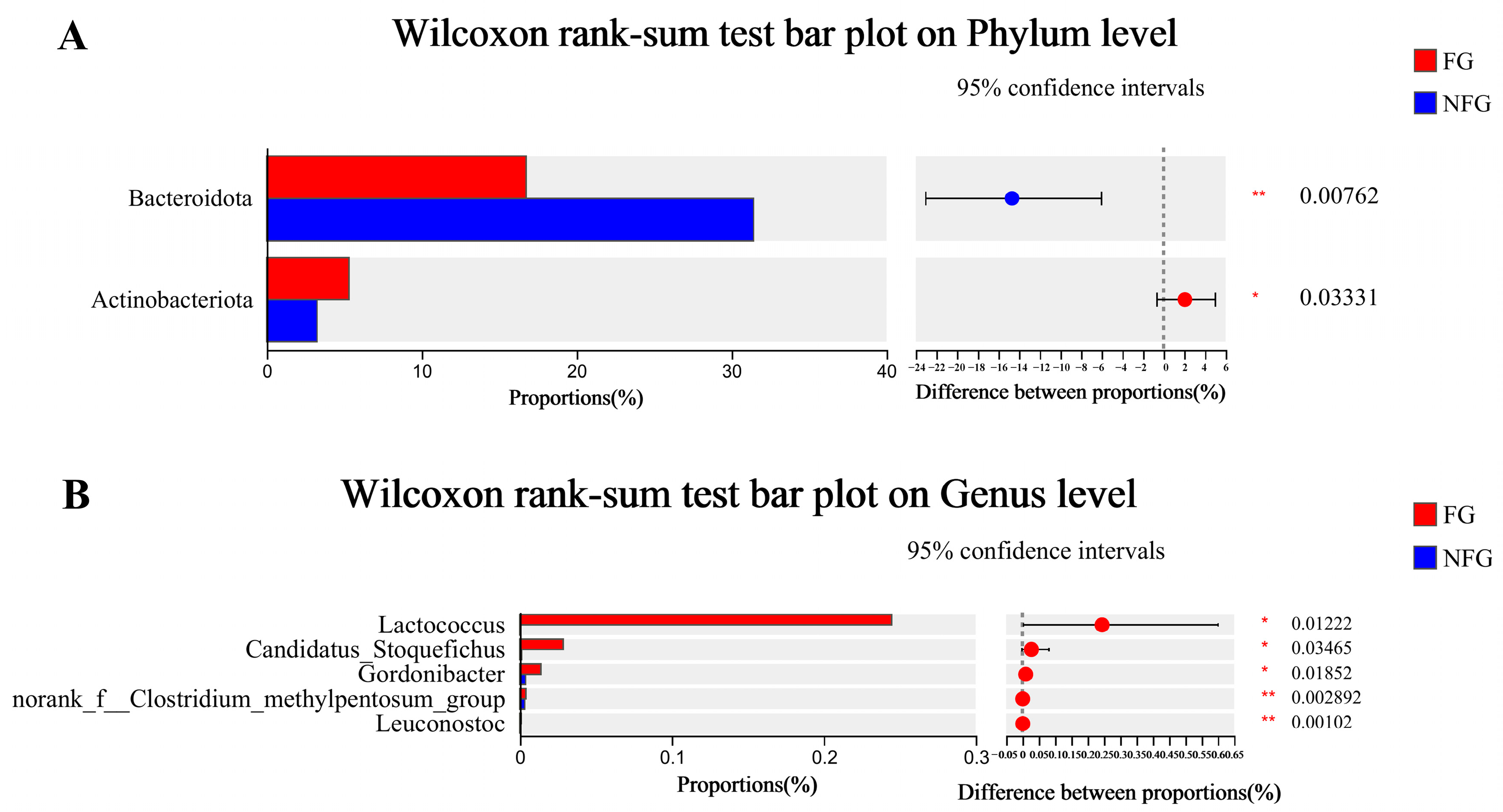
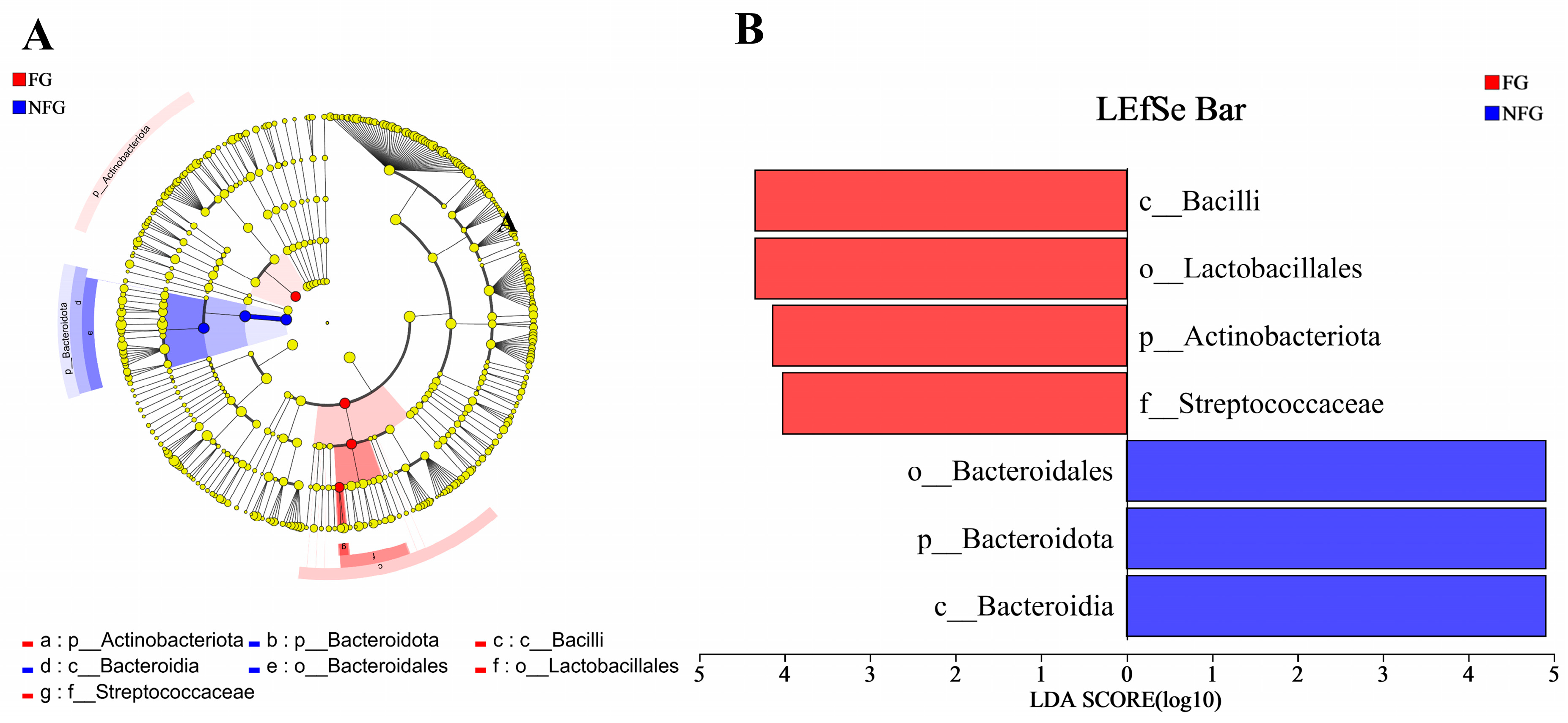
3.5. Gut Microbiota Composition of the Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Xia, C.; Dong, X.; Li, H.; Cao, M.; Sun, D.; He, S.; Yang, F.; Yan, X.; Zhang, S.; Li, N.; et al. Cancer statistics in China and United States, 2022: Profiles, trends, and determinants. Chin. Med. J. 2022, 135, 584–590. [Google Scholar] [CrossRef] [PubMed]
- Duan, L.; Cui, H.; Zhang, W.; Wu, S. Symptoms and experiences of frailty in lung cancer patients with chemotherapy: A mixed-method approach. Front. Oncol. 2022, 12, 1019006. [Google Scholar] [CrossRef]
- Walston, J.; Hadley, E.C.; Ferrucci, L.; Guralnik, J.M.; Newman, A.B.; Studenski, S.A.; Ershler, W.B.; Harris, T.; Fried, L.P. Research agenda for frailty in older adults: Toward a better understanding of physiology and etiology: Summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J. Am. Geriatr. Soc. 2006, 54, 991–1001. [Google Scholar] [CrossRef]
- Komici, K.; Bencivenga, L.; Navani, N.; D’Agnano, V.; Guerra, G.; Bianco, A.; Rengo, G.; Perrotta, F. Frailty in Patients With Lung Cancer: A Systematic Review and Meta-Analysis. Chest 2022, 162, 485–497. [Google Scholar] [CrossRef]
- Montgomery, E.; Macdonald, P.S.; Newton, P.J.; Chang, S.; Jha, S.R.; Hannu, M.K.; Thomson, C.; Havryk, A.; Malouf, M. Frailty as a Predictor of Mortality in Patients With Interstitial Lung Disease Referred for Lung Transplantation. Transplantation 2020, 104, 864–872. [Google Scholar] [CrossRef]
- Shen, Y.; Wang, Y.; Shi, Q.; Hou, L.; Chen, X.; Dong, B.; Hao, Q. The Electronic Frailty Index is Associated with Increased Infection and All-Cause Mortality Among Older Patients with Primary Lung Cancer: A Cohort Study. Clin. Interv. Aging 2021, 16, 1825–1833. [Google Scholar] [CrossRef] [PubMed]
- Dent, E.; Martin, F.C.; Bergman, H.; Woo, J.; Romero-Ortuno, R.; Walston, J.D. Management of frailty: Opportunities, challenges, and future directions. Lancet 2019, 394, 1376–1386. [Google Scholar] [CrossRef]
- Bartali, B.; Frongillo, E.A.; Bandinelli, S.; Lauretani, F.; Semba, R.D.; Fried, L.P.; Ferrucci, L. Low nutrient intake is an essential component of frailty in older persons. J. Gerontol. A Biol. Sci. Med. Sci. 2006, 61, 589–593. [Google Scholar] [CrossRef]
- Struijk, E.A.; Hagan, K.A.; Fung, T.T.; Hu, F.B.; Rodríguez-Artalejo, F.; Lopez-Garcia, E. Diet quality and risk of frailty among older women in the Nurses’ Health Study. Am. J. Clin. Nutr. 2020, 111, 877–883. [Google Scholar] [CrossRef]
- Park, S.Y.; Boushey, C.J.; Shvetsov, Y.B.; Wirth, M.D.; Shivappa, N.; Hébert, J.R.; Haiman, C.A.; Wilkens, L.R.; Le Marchand, L. Diet Quality and Risk of Lung Cancer in the Multiethnic Cohort Study. Nutrients 2021, 13, 1614. [Google Scholar] [CrossRef] [PubMed]
- Parsons, T.J.; Papachristou, E.; Atkins, J.L.; Papacosta, O.; Ash, S.; Lennon, L.T.; Whincup, P.H.; Ramsay, S.E.; Wannamethee, S.G. Physical frailty in older men: Prospective associations with diet quality and patterns. Age Ageing 2019, 48, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.Q.; Li, F.; Wu, H.; Wang, Y.C.; Chen, J.S.; He, G.S.; Li, S.G.; Chen, B. Evaluation of the Validity and Reliability of the Chinese Healthy Eating Index. Nutrients 2018, 10, 114. [Google Scholar] [CrossRef] [PubMed]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef]
- Melzer, D.; Pilling, L.C.; Ferrucci, L. The genetics of human ageing. Nat. Rev. Genet. 2020, 21, 88–101. [Google Scholar] [CrossRef]
- Maslowski, K.M.; Mackay, C.R. Diet, gut microbiota and immune responses. Nat. Immunol. 2011, 12, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Huang, Y.; Yu, X. A Narrative Review of Gut-Muscle Axis and Sarcopenia: The Potential Role of Gut Microbiota. Int. J. Gen. Med. 2021, 14, 1263–1273. [Google Scholar] [CrossRef] [PubMed]
- Lahiri, S.; Kim, H.; Garcia-Perez, I.; Reza, M.M.; Martin, K.A.; Kundu, P.; Cox, L.M.; Selkrig, J.; Posma, J.M.; Zhang, H.; et al. The gut microbiota influences skeletal muscle mass and function in mice. Sci. Transl. Med. 2019, 11, eaan5662. [Google Scholar] [CrossRef]
- Seifi, N.; Safarian, M.; Nematy, M.; Rezvani, R.; Khadem-Rezaian, M.; Sedaghat, A. Effects of synbiotic supplementation on energy and macronutrients homeostasis and muscle wasting of critical care patients: Study protocol and a review of previous studies. Trials 2020, 21, 221. [Google Scholar] [CrossRef]
- Ren, G.; Zhang, J.; Li, M.; Tang, Z.; Yang, Z.; Cheng, G.; Wang, J. Gut microbiota composition influences outcomes of skeletal muscle nutritional intervention via blended protein supplementation in posttransplant patients with hematological malignancies. Clin. Nutr. 2021, 40, 94–102. [Google Scholar] [CrossRef]
- Vega-Cabello, V.; Caballero, F.F.; Rodriguez-Artalejo, F.; Lopez-Garcia, E.; Struijk, E.A. Leucine Intake and Risk of Impaired Physical Function and Frailty in Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2023, 78, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Jayanama, K.; Theou, O.; Godin, J.; Cahill, L.; Shivappa, N.; Hébert, J.R.; Wirth, M.D.; Park, Y.M.; Fung, T.T.; Rockwood, K. Relationship between diet quality scores and the risk of frailty and mortality in adults across a wide age spectrum. BMC Med. 2021, 19, 64. [Google Scholar] [CrossRef] [PubMed]
- Drey, M.; Pfeifer, K.; Sieber, C.C.; Bauer, J.M. The Fried frailty criteria as inclusion criteria for a randomized controlled trial: Personal experience and literature review. Gerontology 2011, 57, 11–18. [Google Scholar] [CrossRef]
- Tian, X.; Wang, C.; Qiao, X.; Liu, N.; Dong, L.; Butler, M.; Si, H.; Jin, Y. Association between pain and frailty among Chinese community-dwelling older adults: Depression as a mediator and its interaction with pain. Pain 2018, 159, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Ntanasi, E.; Maraki, M.; Yannakoulia, M.; Stamelou, M.; Xiromerisiou, G.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.; Sakka, P.; Gargalionis, A.; et al. Frailty and Prodromal Parkinson’s Disease: Results From the HELIAD Study. J. Gerontol. A Biol. Sci. Med. Sci. 2021, 76, 622–629. [Google Scholar] [CrossRef]
- He, B.; Ma, Y.; Wang, C.; Jiang, M.; Geng, C.; Chang, X.; Ma, B.; Han, L. Prevalence and Risk Factors for Frailty among Community-Dwelling Older People in China: A Systematic Review and Meta-Analysis. J. Nutr. Health Aging 2019, 23, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Rietman, M.L.; van der A, D.L.; van Oostrom, S.H.; Picavet, H.S.J.; Dollé, M.E.T.; van Steeg, H.; Verschuren, W.M.M.; Spijkerman, A.M.W. The Association between BMI and Different Frailty Domains: A U-Shaped Curve? J. Nutr. Health Aging 2018, 22, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Yuan, L.; Chang, M.; Wang, J. Abdominal obesity, body mass index and the risk of frailty in community-dwelling older adults: A systematic review and meta-analysis. Age Ageing 2021, 50, 1118–1128. [Google Scholar] [CrossRef]
- Morley, J.E.; Vellas, B.; van Kan, G.A.; Anker, S.D.; Bauer, J.M.; Bernabei, R.; Cesari, M.; Chumlea, W.C.; Doehner, W.; Evans, J.; et al. Frailty consensus: A call to action. J. Am. Med. Dir. Assoc. 2013, 14, 392–397. [Google Scholar] [CrossRef]
- Griebling, T.L. Re: The Relationship between Urinary Total Polyphenols and the Frailty Phenotype in a Community-Dwelling Older Population: The InCHIANTI Study. J. Urol. 2016, 196, 465–466. [Google Scholar] [CrossRef]
- Kobayashi, S.; Asakura, K.; Suga, H.; Sasaki, S. High protein intake is associated with low prevalence of frailty among old Japanese women: A multicenter cross-sectional study. Nutr. J. 2013, 12, 164. [Google Scholar] [CrossRef] [PubMed]
- Beasley, J.M.; LaCroix, A.Z.; Neuhouser, M.L.; Huang, Y.; Tinker, L.; Woods, N.; Michael, Y.; Curb, J.D.; Prentice, R.L. Protein intake and incident frailty in the Women’s Health Initiative observational study. J. Am. Geriatr. Soc. 2010, 58, 1063–1071. [Google Scholar] [CrossRef]
- Smit, E.; Winters-Stone, K.M.; Loprinzi, P.D.; Tang, A.M.; Crespo, C.J. Lower nutritional status and higher food insufficiency in frail older US adults. Br. J. Nutr. 2013, 110, 172–178. [Google Scholar] [CrossRef]
- Yannakoulia, M.; Ntanasi, E.; Anastasiou, C.A.; Scarmeas, N. Frailty and nutrition: From epidemiological and clinical evidence to potential mechanisms. Metabolism 2017, 68, 64–76. [Google Scholar] [CrossRef] [PubMed]
- Paddon-Jones, D.; Sheffield-Moore, M.; Urban, R.J.; Sanford, A.P.; Aarsland, A.; Wolfe, R.R.; Ferrando, A.A. Essential amino acid and carbohydrate supplementation ameliorates muscle protein loss in humans during 28 days bedrest. J. Clin. Endocrinol Metab. 2004, 89, 4351–4358. [Google Scholar] [CrossRef]
- Abizanda, P.; López, M.D.; García, V.P.; Estrella Jde, D.; da Silva González, Á.; Vilardell, N.B.; Torres, K.A. Effects of an Oral Nutritional Supplementation Plus Physical Exercise Intervention on the Physical Function, Nutritional Status, and Quality of Life in Frail Institutionalized Older Adults: The ACTIVNES Study. J. Am. Med. Dir Assoc. 2015, 16, 439.e416–439.e439. [Google Scholar] [CrossRef]
- Verlaan, S.; Aspray, T.J.; Bauer, J.M.; Cederholm, T.; Hemsworth, J.; Hill, T.R.; McPhee, J.S.; Piasecki, M.; Seal, C.; Sieber, C.C.; et al. Nutritional status, body composition, and quality of life in community-dwelling sarcopenic and non-sarcopenic older adults: A case-control study. Clin. Nutr. 2017, 36, 267–274. [Google Scholar] [CrossRef] [PubMed]
- de Haas, S.C.M.; de Jonge, E.A.L.; Voortman, T.; Graaff, J.S.; Franco, O.H.; Ikram, M.A.; Rivadeneira, F.; Kiefte-de Jong, J.C.; Schoufour, J.D. Dietary patterns and changes in frailty status: The Rotterdam study. Eur. J. Nutr. 2018, 57, 2365–2375. [Google Scholar] [CrossRef]
- León-Muñoz, L.M.; García-Esquinas, E.; López-García, E.; Banegas, J.R.; Rodríguez-Artalejo, F. Major dietary patterns and risk of frailty in older adults: A prospective cohort study. BMC Med. 2015, 13, 11. [Google Scholar] [CrossRef]
- Kojima, G.; Avgerinou, C.; Iliffe, S.; Walters, K. Adherence to Mediterranean Diet Reduces Incident Frailty Risk: Systematic Review and Meta-Analysis. J. Am. Geriatr. Soc. 2018, 66, 783–788. [Google Scholar] [CrossRef]
- Watanabe, D.; Kurotani, K.; Yoshida, T.; Nanri, H.; Watanabe, Y.; Date, H.; Itoi, A.; Goto, C.; Ishikawa-Takata, K.; Kimura, M.; et al. Diet quality and physical or comprehensive frailty among older adults. Eur. J. Nutr. 2022, 61, 2451–2462. [Google Scholar] [CrossRef]
- Breen, L.; Phillips, S.M. Skeletal muscle protein metabolism in the elderly: Interventions to counteract the ‘anabolic resistance’ of ageing. Nutr. Metab. 2011, 8, 68. [Google Scholar] [CrossRef] [PubMed]
- Lustgarten, M.S.; Price, L.L.; Chale, A.; Phillips, E.M.; Fielding, R.A. Branched chain amino acids are associated with muscle mass in functionally limited older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.Y.; Wang, C.H.; Chen, W.S.; Chu, C.M.; Wu, H.P.; Liu, M.H.; Lin, Y.T.; Kao, K.C.; Liang, C.Y.; Chen, W.H.; et al. U-Shape Relationship between Plasma Leucine Level and Mortality in the Intensive Care Unit. Dis. Markers 2022, 2022, 7389258. [Google Scholar] [CrossRef] [PubMed]
- Gentile, C.L.; Weir, T.L. The gut microbiota at the intersection of diet and human health. Science 2018, 362, 776–780. [Google Scholar] [CrossRef]
- Poursalehi, D.; Lotfi, K.; Saneei, P. Adherence to the Mediterranean diet and risk of frailty and pre-frailty in elderly adults: A systematic review and dose-response meta-analysis with GRADE assessment. Ageing Res. Rev. 2023, 87, 101903. [Google Scholar] [CrossRef]
- Buigues, C.; Fernández-Garrido, J.; Pruimboom, L.; Hoogland, A.J.; Navarro-Martínez, R.; Martínez-Martínez, M.; Verdejo, Y.; Mascarós, M.C.; Peris, C.; Cauli, O. Effect of a Prebiotic Formulation on Frailty Syndrome: A Randomized, Double-Blind Clinical Trial. Int. J. Mol. Sci. 2016, 17, 932. [Google Scholar] [CrossRef]
- Zhang, L.; Liao, J.; Chen, Q.; Chen, M.; Kuang, Y.; Chen, L.; He, W. Characterization of the gut microbiota in frail elderly patients. Aging Clin. Exp. Res. 2020, 32, 2001–2011. [Google Scholar] [CrossRef]
- Kang, L.; Li, P.; Wang, D.; Wang, T.; Hao, D.; Qu, X. Alterations in intestinal microbiota diversity, composition, and function in patients with sarcopenia. Sci. Rep. 2021, 11, 4628. [Google Scholar] [CrossRef]
- Li, J.; Li, Y.; Zhou, Y.; Wang, C.; Wu, B.; Wan, J. Actinomyces and Alimentary Tract Diseases: A Review of Its Biological Functions and Pathology. Biomed Res. Int. 2018, 2018, 3820215. [Google Scholar] [CrossRef]
- Jensen, G.L. Inflammation: Roles in aging and sarcopenia. JPEN J. Parenter. Enter. Nutr. 2008, 32, 656–659. [Google Scholar] [CrossRef] [PubMed]
- Cortés-Martín, A.; García-Villalba, R.; González-Sarrías, A.; Romo-Vaquero, M.; Loria-Kohen, V.; Ramírez-de-Molina, A.; Tomás-Barberán, F.A.; Selma, M.V.; Espín, J.C. The gut microbiota urolithin metabotypes revisited: The human metabolism of ellagic acid is mainly determined by aging. Food Funct. 2018, 9, 4100–4106. [Google Scholar] [CrossRef] [PubMed]
- Zafar, H.; Saier, M.H., Jr. Gut Bacteroides species in health and disease. Gut Microbes 2021, 13, 1848158. [Google Scholar] [CrossRef] [PubMed]
- Hsu, Y.J.; Chiu, C.C.; Li, Y.P.; Huang, W.C.; Huang, Y.T.; Huang, C.C.; Chuang, H.L. Effect of intestinal microbiota on exercise performance in mice. J. Strength Cond. Res. 2015, 29, 552–558. [Google Scholar] [CrossRef] [PubMed]
| The Fried Frailty Criteria | Detailed Description | |||
|---|---|---|---|---|
| Non-expected weight loss | Unintentional loss of 4.5 kg (10 lb) in the year before the current evaluation or unintentional weight loss of at least 5% of the previous year’s body weight. | |||
| Self-reporting fatigue | Evaluation of two statements of the CES-D scale: (a) I felt that everything I did was an effort; (b) I could not get going. Criterion positive if at least one condition is present for 3 days or more during the last week. | |||
| Muscle weakness | Grip strength of the dominant hand, using hand-held dynamometer: | |||
| BMI/male | Cutoff (kg) | BMI/female | Cutoff (kg) | |
| ≤24 | ≤29 | ≤23 | ≤17 | |
| 24–26 | ≤30 | 23–26 | ≤17.3 | |
| 26–28 | ≤30 | 26–29 | ≤18 | |
| >28 | ≤32 | >29 | ≤21 | |
| Low gait | Cutoff for time to walk 4.57 m at usual pace (static protocol): | |||
| Height/male (cm) | Cutoff (s) | Height/female (cm) | Cutoff (s) | |
| ≤173 | ≥7 | ≤159 | ≥7 | |
| >173 | ≥6 | >159 | ≥6 | |
| Low physical activity level | Assessed by weekly energy expenditure by using the IPAQ-SF: 1 week’s activity < 600 MET-min/week. | |||
| CES-D, Center for Epidemiological Studies Depression; IPAQ-SF, International Physical Activity Questionnaire—Short Form. | ||||
| Frailty (n = 75) | Non-Frailty (n = 156) | p-Value | |
|---|---|---|---|
| Age (years) 1 | 67.0 (61.0, 71.0) | 64.0 (59.0, 69.0) | 0.025 |
| BMI (kg/m2) 1 | 20.9 (19.5, 23.6) | 23.6 (21.8, 29.5) | <0.001 |
| Sex, n (%) 2 | |||
| Male | 59 (78.7) | 116 (74.4) | 0.474 |
| Female | 16 (21.3) | 40 (25.6) | |
| Marital status, n (%) 2 | |||
| Married | 69 (92.0) | 142 (91.0) | 0.931 |
| Widowed/divorced/single | 6 (8.0) | 14 (9.0) | |
| Education level, n (%) 2 | |||
| Primary school or lower | 25 (33.3) | 46 (29.5) | 0.812 |
| Middle school | 37 (49.3) | 80 (51.3) | |
| High school/secondary school | 8 (10.7) | 22 (14.1) | |
| Junior college or higher | 5 (6.7) | 8 (5.1) | |
| Residence, n (%) 2 | |||
| Rural areas | 22 (29.3) | 31 (19.9) | 0.274 |
| Towns | 12 (16.0) | 27 (17.3) | |
| Urban areas | 41 (54.7) | 98 (62.8) | |
| Family monthly income (RMB), n (%) 2 | |||
| <2000 | 16 (21.3) | 16 (10.3) | 0.074 |
| 2000–5000 | 53 (70.7) | 125 (80.1) | |
| >5000 | 6 (8.0) | 15 (9.6) | |
| Smoking status, n (%) 2 | |||
| Never | 10 (13.3) | 23 (14.7) | 0.774 |
| Former/current | 65 (86.7) | 133 (85.3) | |
| Drinking status, n (%) 2 | |||
| Never | 11 (14.7) | 25 (16.0) | 0.790 |
| Former/current | 64 (85.3) | 131 (84.0) | |
| Presence of comorbidities, n (%) 3 | |||
| Yes | 38 (50.7) | 65 (41.7) | 0.644 |
| No | 37 (49.3) | 91 (58.3) | |
| Surgery, n (%) 3 | |||
| Yes | 43 (57.3) | 101 (64.7) | 0.276 |
| No | 32 (42.7) | 55 (35.3) | |
| Pathology type, n (%) 3 | |||
| Adenocarcinoma | 60 (80.0) | 117 (75.0) | 0.644 |
| Squamous cell carcinoma | 12 (16.0) | 33 (21.2) | |
| Small cell lung cancer | 3 (4.0) | 6 (3.8) | |
| Cancer stage, n (%) 2 | |||
| I | 3 (4.0) | 17 (10.9) | 0.023 |
| II | 6 (8.0) | 22 (14.1) | |
| III | 12 (16.0) | 37 (23.7) | |
| Ⅳ | 54 (72.0) | 80 (51.3) |
| Frailty (n = 75) | Non-Frailty (n = 156) | p-Value | |
|---|---|---|---|
| Energy (kcal/d) 1 | 1080.0 (907.0, 1284.0) | 1196.0 (1042.5, 1493.0) | <0.001 |
| Protein (g/d) 1 | 51.6 (41.1, 61.2) | 62.1 (46.9, 71.1) | <0.001 |
| Fat (g/d) 1 | 37.4 (28.8, 44.5) | 38.5 (31.1, 51.1) | 0.141 |
| Dietary fiber (g/d) 1 | 7.6 (5.1, 9.1) | 8.5 (6.2, 12.4) | 0.003 |
| Carbohydrate (g/d) 1 | 128.2 (105.7, 155.8) | 151.4 (128.1, 189.2) | <0.001 |
| Cholesterol (mg/d) 1 | 482.0 (256.0, 672.0) | 494.0 (327.3, 699.3) | 0.331 |
| Vitamin A (µgRAE/d) 1 | 346.0 (218.0, 517.0) | 383.0 (291.5, 576.7) | 0.093 |
| Vitamin D (µg/d) 1 | 0.9 (0.0, 1.8) | 1.3 (0.5, 4.5) | 0.031 |
| Vitamin E (mg/d) 1 | 10.7 (8.1, 15.2) | 12.4 (9.1, 17.5) | 0.083 |
| Vitamin B1 (mg/d) 1 | 0.5 (0.4, 0.7) | 0.6 (0.4, 0.8) | 0.009 |
| Vitamin B2 (mg/d) 1 | 0.7 (0.6, 1.1) | 0.8 (0.7, 1.2) | 0.026 |
| Vitamin B6 (mg/d) 1 | 0.1 (0.0, 0.2) | 0.1 (0.0, 0.2) | 0.027 |
| Vitamin C (mg/d) 1 | 74.6 (39.7, 124.5) | 100.2 (60.2, 154.3) | 0.003 |
| Folate (µg/d) 1 | 89.7 (52.4, 129.0) | 100.4 (66.7, 150.3) | 0.095 |
| Niacin (mg/d) 1 | 10.4 (7.8, 13.1) | 12.3 (9.5, 15.5) | 0.001 |
| Biotin (µg/d) 1 | 2.6 (1.0, 4,9) | 2.5 (1.2, 5.6) | 0.525 |
| Calcium (mg/d) 1 | 418.0 (266.0, 563.0) | 527.0 (371.3, 686.0) | <0.001 |
| Phosphorus (mg/d) 1 | 715.3 (571.8, 821.4) | 830.3 (681.5, 997.2) | <0.001 |
| Potassium (mg/d) 1 | 1308.8 (967.6, 1542.3) | 1552.4 (1179.7, 1904.9) | <0.001 |
| Sodium (mg/d) 2 | 4158.9 ± 1476.5 | 4211.6 ± 1490.4 | 0.788 |
| Magnesium (mg/d) 1 | 179.0 (156.0, 214.3) | 234.0 (178.5, 295.8) | 0.001 |
| Iron (mg/d) 1 | 12.7 (10.4, 16.4) | 14.6 (11.3, 18.5) | 0.017 |
| Iodine (µg/d) 1 | 21.5 (14.1, 33.9) | 26.2 (18.1, 36.8) | 0.027 |
| Zinc (mg/d) 1 | 6.7 (5.6, 8.4) | 7.9 (6.3, 9.7) | 0.001 |
| Selenium (µg/d) 1 | 35.4 (23.4, 54.3) | 41.6 (30.7, 61.5) | 0.019 |
| Copper (mg/d) 1 | 0.9 (0.7, 1.3) | 1.1 (0.8, 1.6) | 0.018 |
| Manganese (mg/d) 1 | 2.6 (2.1, 3.5) | 3.2 (2.5, 4.3) | 0.002 |
| Leucine (mg/d) 1 | 3494.9 (2955.2, 4178.6) | 4190.0 (3308.8, 5439.4) | <0.001 |
| Variables | OR | 95% CI | p-Value |
|---|---|---|---|
| Energy | 1.00 | 0.99, 1.00 | 0.149 |
| Protein | 0.98 | 0.93, 1.03 | 0.443 |
| Dietary fiber | 1.03 | 0.91, 1.17 | 0.654 |
| Carbohydrate | 0.97 | 0.96, 0.99 | 0.003 |
| Niacin | 0.93 | 0.83, 1.05 | 0.223 |
| Calcium | 0.99 | 0.99, 1.00 | 0.025 |
| Phosphorus | 1.00 | 0.99, 1.00 | 0.439 |
| Potassium | 1.00 | 0.99, 1.00 | 0.346 |
| Magnesium | 1.00 | 0.99, 1.01 | 0.636 |
| Iodine | 0.99 | 0.98, 1.01 | 0.477 |
| Zinc | 0.88 | 0.65, 1.18 | 0.399 |
| Selenium | 1.03 | 1.00, 1.06 | 0.022 |
| Copper | 0.70 | 0.40, 1.21 | 0.201 |
| Manganese | 0.83 | 0.63, 1.09 | 0.172 |
| Frailty (n = 75) | Non-Frailty (n = 156) | p-Value | |
|---|---|---|---|
| Total CHEI score 1 | 55.9 ± 8.3 | 60.4 ± 8.2 | <0.001 |
| Total grains 2 | 4.4 (3.2, 5.0) | 4.7 (3.4, 5.0) | 0.200 |
| Whole grains and mixed beans 2 | 0.0 (0.0, 1.7) | 0.0 (0.0, 1.6) | 0.942 |
| Tubers 2 | 0.0 (0.0, 3.0) | 0.0 (0.0, 1.6) | 0.504 |
| Total vegetables 2 | 3.8 (2.1, 5.0) | 3.8 (2.5, 5.0) | 0.410 |
| Dark vegetables 2 | 2.9 (0.5, 5.0) | 3.1 (1.7, 5.0) | 0.168 |
| Fruits 2 | 10.0 (6.4, 10.0) | 10.0 (10.0, 10.0) | 0.137 |
| Poultry 2 | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.128 |
| Red meat 2 | 3.4 (2.2, 5.0) | 3.6 (2.2, 4.9) | 0.952 |
| Fish and seafood 2 | 5.0 (0.0, 5.0) | 5.0 (0.0, 5.0) | 0.225 |
| Eggs 2 | 5.0 (0.0, 5.0) | 5.0 (4.6, 5.0) | 0.609 |
| Dairy 2 | 0.0 (0.0, 5.0) | 5.0 (0.0, 5.0) | 0.005 |
| Soybeans 2 | 0.0 (0.0, 4.0) | 0.0 (0.0, 5.0) | 0.833 |
| Seed and nuts 2 | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.636 |
| Cooking oils 2 | 10.0 (10.0, 10.0) | 10.0 (10.0, 10.0) | 0.022 |
| Sodium 2 | 0.0 (0.0, 2.5) | 1.2 (0.0, 3.8) | 0.021 |
| Alcohol 2 | 5.0 (5.0, 5.0) | 5.0 (5.0, 5.0) | 1.000 |
| Added sugars 2 | 5.0 (5.0, 5.0) | 5.0 (5.0, 5.0) | 0.326 |
| Variables | OR | 95% CI | p-Value |
|---|---|---|---|
| Univariate | |||
| Total CHEI score | 0.94 | 0.91, 0.97 | <0.001 |
| Dairy | 0.84 | 0.75, 0.94 | 0.002 |
| Sodium | 0.89 | 0.79, 1.00 | 0.055 |
| Cooking oils | 0.07 | 0.01, 1.25 | 0.070 |
| Multivariate | |||
| Total CHEI score | 0.94 | 0.90, 0.99 | 0.009 |
| Dairy | 0.91 | 0.79, 1.05 | 0.214 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Z.; Qian, L.; Chu, J.; Liu, Y.; Maitiniyazi, G.; Chen, Y.; Cheng, X.; He, J.; Cheng, L.; Ou, M.; et al. Diet Is Associated with Frailty in Lung Cancer: A Possible Role of Gut Microbiota. Nutrients 2023, 15, 4298. https://doi.org/10.3390/nu15194298
Li Z, Qian L, Chu J, Liu Y, Maitiniyazi G, Chen Y, Cheng X, He J, Cheng L, Ou M, et al. Diet Is Associated with Frailty in Lung Cancer: A Possible Role of Gut Microbiota. Nutrients. 2023; 15(19):4298. https://doi.org/10.3390/nu15194298
Chicago/Turabian StyleLi, Ziyuan, Lei Qian, Jianghui Chu, Yuan Liu, Gusonghan Maitiniyazi, Yue Chen, Xinxin Cheng, Jianyun He, Lan Cheng, Minmin Ou, and et al. 2023. "Diet Is Associated with Frailty in Lung Cancer: A Possible Role of Gut Microbiota" Nutrients 15, no. 19: 4298. https://doi.org/10.3390/nu15194298
APA StyleLi, Z., Qian, L., Chu, J., Liu, Y., Maitiniyazi, G., Chen, Y., Cheng, X., He, J., Cheng, L., Ou, M., Wang, J., & Xia, S. (2023). Diet Is Associated with Frailty in Lung Cancer: A Possible Role of Gut Microbiota. Nutrients, 15(19), 4298. https://doi.org/10.3390/nu15194298






