Relevance of Serum Levels and Functional Genetic Variants in Vitamin D Receptor Gene among Saudi Women with Gestational Diabetes Mellitus
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Concerns
2.2. Patients
2.3. Sample Size Calculation
2.4. Data Collection
2.5. Blood and Serum Analysis
2.6. Molecular Analysis for the VDR Gene
2.7. Statistical Analysis
3. Results
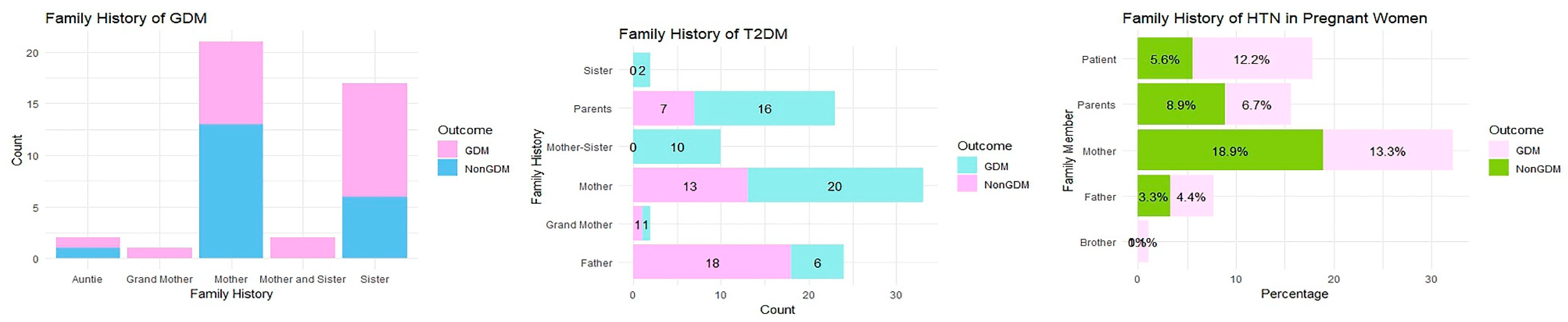
3.1. Characteristics of the Studied Traits in Saudi Women
3.2. Interaction of the Studied SNPs with the VDR Gene in Pregnant Women
3.3. Serum Levels of Vitamin D along with the BMI Levels in Pregnant Women Groups
3.4. Comparison of Vitamin D Levels with Baseline Characteristics
3.5. Relationship between the Vitamin D Levels and VDR SNPs in Women with GDM
3.6. Regression Model of the GDM Covariates and SNPs in the VDR Gene
3.7. ANOVA of the GDM Covariates and SNPs in the VDR Gene
3.8. Haplotype Analysis of VDR SNPs
3.9. Analysis of Linkage Disequilibrium (LD)
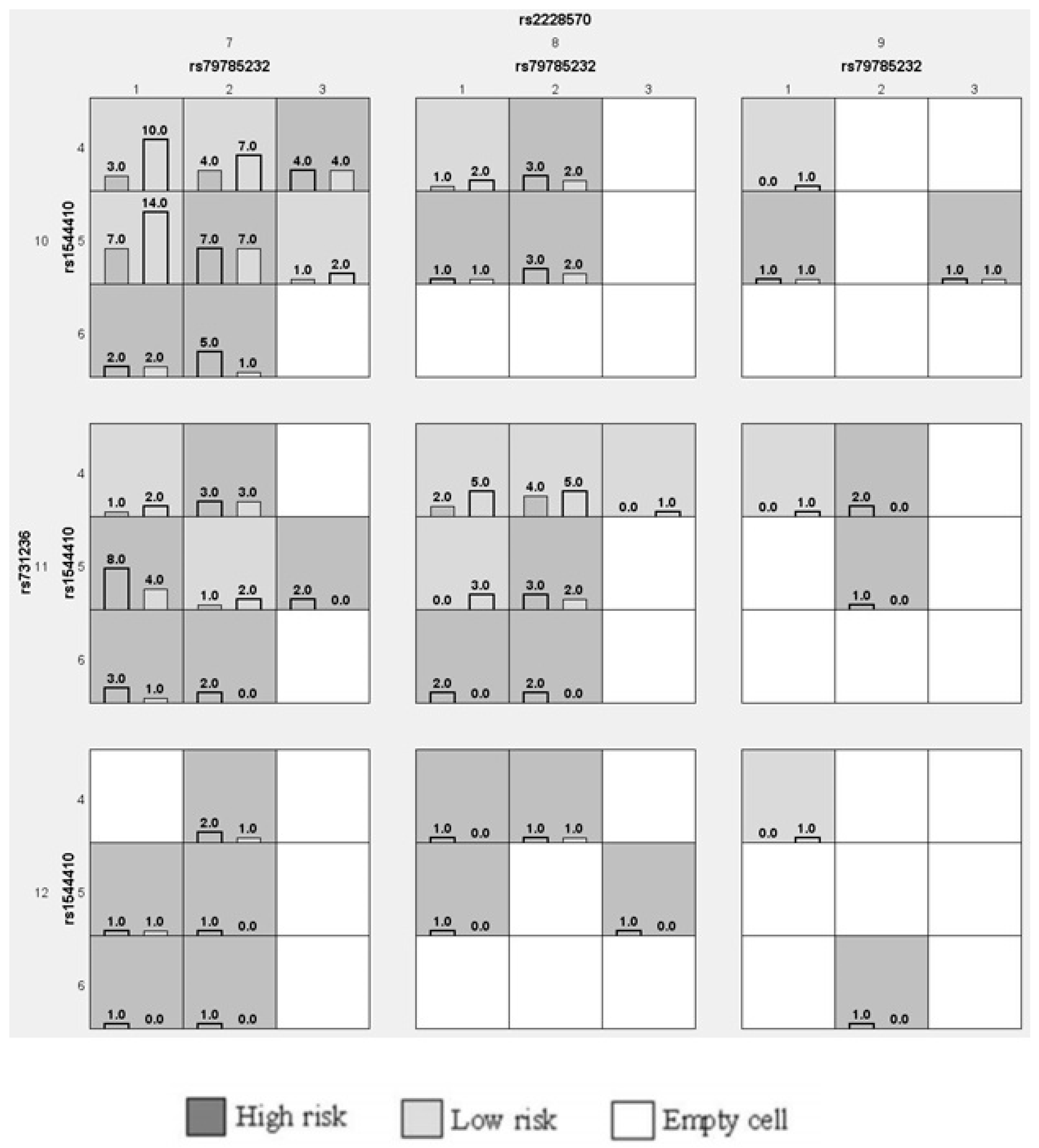
3.10. Analysis of the GMDR Model in GDM Women
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mulyani, D.E.; Maksum, I.P. Detection of Biomarker Using Aptasensors to Determine the Type of Diabetes. Diagnostics 2023, 13, 2035. [Google Scholar] [CrossRef]
- Association, A.D. 2. Classification and diagnosis of diabetes: Standards of medical care in diabetes—2020. Diabetes Care 2020, 43, S14–S31. [Google Scholar]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L. 3. Prevention or Delay of Type 2 Diabetes and Associated Comorbidities: Standards of Care in Diabetes—2023. Diabetes Care 2023, 46, S41–S48. [Google Scholar] [CrossRef] [PubMed]
- Majcher, S.; Ustianowski, P.; Malinowski, D.; Czerewaty, M.; Tarnowski, M.; Safranow, K.; Dziedziejko, V.; Pawlik, A. KCNJ11 and KCNQ1 Gene Polymorphisms and Placental Expression in Women with Gestational Diabetes Mellitus. Genes 2022, 13, 1315. [Google Scholar] [CrossRef] [PubMed]
- Gong, Y.; Shi, J.; Li, J.; Liu, L. Growth differentiation factor-15 in patients with gestational diabetes mellitus and its relationship with microalbuminuria. Exp. Ther. Med. 2023, 26, 427. [Google Scholar] [CrossRef]
- Quaresima, P.; Saccone, G.; Pellegrino, R.; Vaccarisi, S.; Taranto, L.; Mazzulla, R.; Bernardo, S.; Venturella, R.; Di Carlo, C.; Morelli, M. Incidental diagnosis of a pancreatic adenocarcinoma in a woman affected by gestational diabetes mellitus: Case report and literature review. Am. J. Obstet. Gynecol. MFM 2021, 3, 100471. [Google Scholar] [CrossRef]
- Linares-Pineda, T.; Peña-Montero, N.; Fragoso-Bargas, N.; Gutiérrez-Repiso, C.; Lima-Rubio, F.; Suarez-Arana, M.; Sánchez-Pozo, A.; Tinahones, F.J.; Molina-Vega, M.; Picón-César, M.J. Epigenetic marks associated with gestational diabetes mellitus across two time points during pregnancy. Clin. Epigenetics 2023, 15, 110. [Google Scholar]
- Ornoy, A. Prenatal origin of obesity and their complications: Gestational diabetes, maternal overweight and the paradoxical effects of fetal growth restriction and macrosomia. Reprod. Toxicol. 2011, 32, 205–212. [Google Scholar] [CrossRef]
- Sirico, A.; Rossi, E.D.; Degennaro, V.A.; Arena, V.; Rizzi, A.; Tartaglione, L.; Di Leo, M.; Pitocco, D.; Lanzone, A. Placental diabesity: Placental VEGF and CD31 expression according to pregestational BMI and gestational weight gain in women with gestational diabetes. Arch. Gynecol. Obstet. 2023, 307, 1823–1831. [Google Scholar]
- Sirico, A.; Dell’Aquila, M.; Tartaglione, L.; Moresi, S.; Farì, G.; Pitocco, D.; Arena, V.; Lanzone, A. PTH-rP and PTH-R1 expression in Placentas from Pregnancies complicated by gestational diabetes: New Insights into the pathophysiology of hyperglycemia in pregnancy. Diagnostics 2021, 11, 1356. [Google Scholar] [CrossRef]
- Walker, A.F.; Graham, S.; Maple-Brown, L.; Egede, L.E.; Campbell, J.A.; Walker, R.J.; Wade, A.N.; Mbanya, J.C.; Long, J.A.; Yajnik, C. Interventions to address global inequity in diabetes: International progress. Lancet 2023. [Google Scholar]
- Agarwal, S.; Wade, A.N.; Mbanya, J.C.; Yajnik, C.; Thomas, N.; Egede, L.E.; Campbell, J.A.; Walker, R.J.; Maple-Brown, L.; Graham, S. The role of structural racism and geographical inequity in diabetes outcomes. Lancet 2023. [Google Scholar]
- Renugasundari, M.; Pal, G.K.; Chaturvedula, L.; Nanda, N.; Harichandrakumar, K.; Durgadevi, T. Inflammation and decreased cardiovagal modulation are linked to stress and depression at 36th week of pregnancy in gestational diabetes mellitus. Sci. Rep. 2023, 13, 10348. [Google Scholar] [PubMed]
- OuYang, H.; Chen, B.; Abdulrahman, A.-M.; Li, L.; Wu, N. Associations between gestational diabetes and anxiety or depression: A systematic review. J. Diabetes Res. 2021, 2021, 9959779. [Google Scholar] [CrossRef]
- Wu, P.; Wang, Y.; Ye, Y.; Yang, X.; Huang, Y.; Ye, Y.; Lai, Y.; Ouyang, J.; Wu, L.; Xu, J. Liver biomarkers, lipid metabolites, and risk of gestational diabetes mellitus in a prospective study among Chinese pregnant women. BMC Med. 2023, 21, 150. [Google Scholar] [CrossRef]
- Ma, H.-Z.; Chen, Y.; Guo, H.-H.; Wang, J.; Xin, X.-L.; Li, Y.-C.; Liu, Y.-F. Effect of resveratrol in gestational diabetes mellitus and its complications. World J. Diabetes 2023, 14, 808. [Google Scholar] [CrossRef]
- Alsaedi, S.A.; Altalhi, A.A.; Nabrawi, M.F.; Aldainy, A.A.; Wali, R.M. Prevalence and risk factors of gestational diabetes mellitus among pregnant patients visiting National Guard primary health care centers in Saudi Arabia. Saudi Med. J. 2020, 41, 144. [Google Scholar] [CrossRef]
- Saudi Health Council. Saudi Diabetes Clinical Practice Guideline (SDCPG). Saudi National Diabetes Center (SNDC). 2021. Available online: https://shc.gov.sa/Arabic/Documents/SDCP%20Guidelines.pdf (accessed on 5 October 2023).
- Jiang, Z.; Pu, R.; Li, N.; Chen, C.; Li, J.; Dai, W.; Wang, Y.; Hu, J.; Zhu, D.; Yu, Q. High prevalence of vitamin D deficiency in Asia: A systematic review and meta-analysis. Crit. Rev. Food Sci. Nutr. 2023, 63, 3602–3611. [Google Scholar] [CrossRef]
- AlFaris, N.A.; AlKehayez, N.M.; AlMushawah, F.I.; AlNaeem, A.N.; AlAmri, N.D.; AlMudawah, E.S. Vitamin D deficiency and associated risk factors in women from Riyadh, Saudi Arabia. Sci. Rep. 2019, 9, 20371. [Google Scholar] [CrossRef]
- AlQuaiz, A.M.; Kazi, A.; Fouda, M.; Alyousefi, N. Age and gender differences in the prevalence and correlates of vitamin D deficiency. Arch. Osteoporos. 2018, 13, 49. [Google Scholar] [CrossRef]
- Al-Ajlan, A.; Al-Musharaf, S.; Fouda, M.A.; Krishnaswamy, S.; Wani, K.; Aljohani, N.J.; Al-Serehi, A.; Sheshah, E.; Alshingetti, N.M.; Turkistani, I.Z.; et al. Lower vitamin D levels in Saudi pregnant women are associated with higher risk of developing GDM. BMC Pregnancy Childbirth 2018, 18, 86. [Google Scholar] [CrossRef] [PubMed]
- Al-Faris, N.A. High Prevalence of Vitamin D Deficiency among Pregnant Saudi Women. Nutrients 2016, 8, 77. [Google Scholar] [CrossRef] [PubMed]
- Al-Khaldy, N.S.; Al-Musharaf, S.; Aljazairy, E.A.; Hussain, S.D.; Alnaami, A.M.; Al-Daghri, N.; Aljuraiban, G. Serum Vitamin D Level and Gut Microbiota in Women. Healthcare 2023, 11, 351. [Google Scholar] [CrossRef] [PubMed]
- Al-Musharaf, S.; Fouda, M.A.; Turkestani, I.Z.; Al-Ajlan, A.; Sabico, S.; Alnaami, A.M.; Wani, K.; Hussain, S.D.; Alraqebah, B.; Al-Serehi, A.; et al. Vitamin D Deficiency Prevalence and Predictors in Early Pregnancy among Arab Women. Nutrients 2018, 10, 489. [Google Scholar] [CrossRef]
- Ali, A.M.; Rafique, M.; Saleem, Z. Association of vitamin D deficiency to the risk of preeclampsia in Saudi Arabia. J. Pak. Med. Assoc. 2021, 71, 257–261. [Google Scholar] [CrossRef]
- Bindayel, I.A. Low Vitamin D Level in Saudi Women with Polycystic Ovary Syndrome. Front. Nutr. 2021, 8, 611351. [Google Scholar] [CrossRef]
- Dias, S.; Pheiffer, C.; Abrahams, Y.; Rheeder, P.; Adam, S. Molecular biomarkers for gestational diabetes mellitus. Int. J. Mol. Sci. 2018, 19, 2926. [Google Scholar] [CrossRef]
- Wu, L.; Cui, L.; Tam, W.H.; Ma, R.C.; Wang, C.C. Genetic variants associated with gestational diabetes mellitus: A meta-analysis and subgroup analysis. Sci. Rep. 2016, 6, 30539. [Google Scholar] [CrossRef]
- Shaat, N.; Ekelund, M.; Lernmark, Å.; Ivarsson, S.; Almgren, P.; Berntorp, K.; Groop, L. Association of the E23K polymorphism in the KCNJ11 gene with gestational diabetes mellitus. Diabetologia 2005, 48, 2544–2551. [Google Scholar] [CrossRef]
- Zhou, Q.; Zhang, K.; Li, W.; Liu, J.; Hong, J.; Qin, S.; Ping, F.; Sun, M.; Nie, M. Association of KCNQ1 gene polymorphism with gestational diabetes mellitus in a Chinese population. Diabetologia 2009, 52, 2466–2468. [Google Scholar] [CrossRef]
- Pappa, K.I.; Gazouli, M.; Anastasiou, E.; Loutradis, D.; Anagnou, N.P. The Q192R polymorphism of the paraoxonase-1 (PON1) gene is associated with susceptibility to gestational diabetes mellitus in the Greek population. Gynecol. Endocrinol. 2017, 33, 617–620. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Wen, S.; Liu, M.; Zhang, S.; Jin, X.; Liu, A. Association between gene polymorphisms of vitamin D receptor and gestational diabetes mellitus: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2021, 18, 205. [Google Scholar] [CrossRef] [PubMed]
- Al-Alyani, H.; Al-Turki, H.A.; Al-Essa, O.N.; Alani, F.M.; Sadat-Ali, M. Vitamin D deficiency in Saudi Arabians: A reality or simply hype: A meta-analysis (2008–2015). J. Fam. Community Med. 2018, 25, 1. [Google Scholar]
- Mondockova, V.; Kovacova, V.; Zemanova, N.; Babikova, M.; Martiniakova, M.; Galbavy, D.; Omelka, R. Vitamin D Receptor Gene Polymorphisms Affect Osteoporosis-Related Traits and Response to Antiresorptive Therapy. Genes 2023, 14, 193. [Google Scholar] [PubMed]
- Standage-Beier, C.S.; Garcia, L.A.; De Filippis, E.; Shaibi, G.Q.; Mandarino, L.J.; Coletta, D.K. Association of Vitamin D Receptor Gene Polymorphisms with Cardiometabolic Phenotypes in Hispanics: A Life Course Approach. Nutrients 2023, 15, 2118. [Google Scholar] [CrossRef] [PubMed]
- Smolders, J.; Peelen, E.; Thewissen, M.; Menheere, P.; Tervaert, J.W.C.; Hupperts, R.; Damoiseaux, J. The relevance of vitamin D receptor gene polymorphisms for vitamin D research in multiple sclerosis. Autoimmun. Rev. 2009, 8, 621–626. [Google Scholar] [CrossRef]
- Abouzid, M.; Kruszyna, M.; Burchardt, P.; Kruszyna, Ł.; Główka, F.K.; Karaźniewicz-Łada, M. Vitamin D Receptor Gene Polymorphism and Vitamin D Status in Population of Patients with Cardiovascular Disease—A Preliminary Study. Nutrients 2021, 13, 3117. [Google Scholar] [CrossRef]
- Arabi, A.; Mahfoud, Z.; Zahed, L.; El-Onsi, L.; El-Hajj Fuleihan, G. Effect of age, gender and calciotropic hormones on the relationship between vitamin D receptor gene polymorphisms and bone mineral density. Eur. J. Clin. Nutr. 2010, 64, 383–391. [Google Scholar]
- Li, Y.; Xi, B.; Li, K.; Wang, C. Association between vitamin D receptor gene polymorphisms and bone mineral density in Chinese women. Mol. Biol. Rep. 2012, 39, 5709–5717. [Google Scholar]
- Ogunkolade, B.-W.; Boucher, B.J.; Prahl, J.M.; Bustin, S.A.; Burrin, J.M.; Noonan, K.; North, B.V.; Mannan, N.; McDermott, M.F.; DeLuca, H.F. Vitamin D receptor (VDR) mRNA and VDR protein levels in relation to vitamin D status, insulin secretory capacity, and VDR genotype in Bangladeshi Asians. Diabetes 2002, 51, 2294–2300. [Google Scholar] [CrossRef]
- Jain, R.; von Hurst, P.R.; Stonehouse, W.; Love, D.R.; Higgins, C.M.; Coad, J. Association of vitamin D receptor gene polymorphisms with insulin resistance and response to vitamin D. Metabolism 2012, 61, 293–301. [Google Scholar] [CrossRef]
- El-Beshbishy, H.A.; Tawfeek, M.A.; Taha, I.M.; FadulElahi, T.; Shaheen, A.Y.; Bardi, F.A.; Sultan, I.I. Association of vitamin D receptor gene BsmI (A > G) and FokI (C > T) polymorphism in gestational diabetes among Saudi Women. Pak. J. Med. Sci. 2015, 31, 1328–1333. [Google Scholar] [CrossRef] [PubMed]
- Tawfeek, M.; Habib, F.; Saultan, E.M. Vitamin D receptor BsmI gene polymorphisms and gestational diabetes mellitus: A Saudi study. Br. J. Med. Med. Res. 2011, 1, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Ghamdi, A.M. Association of vitamin D receptor gene polymorphisms with gestational diabetes in pregnant women. Wulfenia 2014, 21, 7. [Google Scholar]
- Metzger, B.E.; Gabbe, S.G.; Persson, B.; Lowe, L.P.; Dyer, A.R.; Oats, J.J.; Buchanan, T.A. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy: Response to Weinert. Diabetes Care 2010, 33, e98. [Google Scholar] [CrossRef]
- Zeng, Q.; Zou, D.; Liu, N.; Wei, Y.; Yang, J.; Wu, W.; Han, F.; He, R.; Guo, R. Association of miR-196a2 and miR-27a polymorphisms with gestational diabetes mellitus susceptibility in a Chinese population. Front. Endocrinol. 2023, 14, 1127336. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.; Fu, Y.; Lu, S.; Shuai, M.; Miao, Z.; Gou, W.; Shen, L.; Liang, Y.; Xu, F.; Tian, Y. Continuous glucose monitoring-derived glycemic metrics and adverse pregnancy outcomes among women with gestational diabetes: A prospective cohort study. Lancet Reg. Health–West. Pac. 2023. [Google Scholar]
- Alfadhli, E.M.; Osman, E.N.; Basri, T.H.; Mansuri, N.S.; Youssef, M.H.; Assaaedi, S.A.; Aljohani, B.A. Gestational diabetes among Saudi women: Prevalence, risk factors and pregnancy outcomes. Ann. Saudi Med. 2015, 35, 222–230. [Google Scholar]
- Pourhoseingholi, M.A.; Vahedi, M.; Rahimzadeh, M. Sample size calculation in medical studies. Gastroenterol. Hepatol. Bed Bench 2013, 6, 14. [Google Scholar]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation; World Health Organization: Geneva, Switzerland, 2000.
- Oben, A.; Moore, M.; Wallace, E.; Muntner, P.; Oparil, S.; Tita, A.; Sinkey, R. Validation of a Remote Monitoring Blood Pressure Device in Pregnancy. Am. J. Hypertens. 2023, 36, 341–347. [Google Scholar] [CrossRef]
- Kannan, S.; Mahadevan, S.; Ramji, B.; Jayapaul, M.; Kumaravel, V. LDL-cholesterol: Friedewald calculated versus direct measurement-study from a large Indian laboratory database. Indian J. Endocrinol. Metab. 2014, 18, 502. [Google Scholar] [PubMed]
- Coetzee, A.; Hall, D.R.; van de Vyver, M.; Conradie, M. Early postpartum HbA1c after hyperglycemia first detected in pregnancy—Imperfect but not without value. PLoS ONE 2023, 18, e0282446. [Google Scholar]
- Solé, X.; Guinó, E.; Valls, J.; Iniesta, R.; Moreno, V. SNPStats: A web tool for the analysis of association studies. Bioinformatics 2006, 22, 1928–1929. [Google Scholar] [CrossRef] [PubMed]
- T.j.p.j.V.C.S.R.f. Available online: https://www.jamovi.org (accessed on 5 October 2023).
- Iniesta, R.; Guinó, E.; Moreno, V. Análisis estadístico de polimorfismos genéticos en estudios epidemiológicos. Gac. Sanit. 2005, 19, 333–341. [Google Scholar] [CrossRef]
- Zhu, Y.; Zhang, C. Prevalence of gestational diabetes and risk of progression to type 2 diabetes: A global perspective. Curr. Diabetes Rep. 2016, 16, 7. [Google Scholar]
- Shahgheibi, S.; Farhadifar, F.; Pouya, B. The effect of vitamin D supplementation on gestational diabetes in high-risk women: Results from a randomized placebo-controlled trial. J. Res. Med. Sci. Off. J. Isfahan Univ. Med. Sci. 2016, 21, 2. [Google Scholar]
- John, A.N.; Jiang, F.-X. An overview of type 2 diabetes and importance of vitamin D3-vitamin D receptor interaction in pancreatic β-cells. J. Diabetes Complicat. 2018, 32, 429–443. [Google Scholar]
- Li, J.; Guo, M.; Li, W.; Ren, Q.; Feng, Y.; Yang, H.; Zhang, Y.; Wang, S.; Wu, W. Relationship between vitamin D receptor gene polymorphisms and gestational diabetes mellitus: A case-control study. Zhonghua Liu Xing Bing Xue Za Zhi Zhonghua Liuxingbingxue Zazhi 2022, 43, 1455–1461. [Google Scholar]
- Zeng, Q.; Zou, D.; Wei, Y.; Ouyang, Y.; Lao, Z.; Guo, R. Association of vitamin D receptor gene rs739837 polymorphism with type 2 diabetes and gestational diabetes mellitus susceptibility: A systematic review and meta-analysis. Eur. J. Med. Res. 2022, 27, 65. [Google Scholar]
- Aravindhan, S.; Almasoody, M.F.M.; Selman, N.A.; Andreevna, A.N.; Ravali, S.; Mohammadi, P.; Eslami, M.M.; Razi, B.; Aslani, S.; Imani, D. Vitamin D Receptor gene polymorphisms and susceptibility to type 2 diabetes: Evidence from a meta-regression and meta-analysis based on 47 studies. J. Diabetes Metab. Disord. 2021, 20, 845–867. [Google Scholar]
- Daly, B.; Toulis, K.A.; Thomas, N.; Gokhale, K.; Martin, J.; Webber, J.; Keerthy, D.; Jolly, K.; Saravanan, P.; Nirantharakumar, K. Increased risk of ischemic heart disease, hypertension, and type 2 diabetes in women with previous gestational diabetes mellitus, a target group in general practice for preventive interventions: A population-based cohort study. PLoS Med. 2018, 15, e1002488. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Song, C.; Li, C.; Liu, P.; Sun, Z.; Yang, X. Increased risk of cardiovascular disease in women with prior gestational diabetes: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2018, 140, 324–338. [Google Scholar] [CrossRef] [PubMed]
- Sentinelli, F.; Bertoccini, L.; Barchetta, I.; Capoccia, D.; Incani, M.; Pani, M.; Loche, S.; Angelico, F.; Arca, M.; Morini, S. The vitamin D receptor (VDR) gene rs11568820 variant is associated with type 2 diabetes and impaired insulin secretion in Italian adult subjects, and associates with increased cardio-metabolic risk in children. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 407–413. [Google Scholar] [CrossRef]
- Alzaim, M.; Al-Daghri, N.M.; Sabico, S.; Fouda, M.A.; Al-Musharaf, S.; Khattak, M.N.K.; Mohammed, A.K.; Al-Ajlan, A.; Binjawhar, D.N.; Wood, R. The Association Between FokI Vitamin D Receptor Polymorphisms with Metabolic Syndrome Among Pregnant Arab Women. Front. Endocrinol. 2022, 13, 844472. [Google Scholar] [CrossRef]
- Apaydın, M.; Beysel, S.; Eyerci, N.; Pinarli, F.A.; Ulubay, M.; Kizilgul, M.; Ozdemir, O.; Caliskan, M.; Cakal, E. The VDR gene FokI polymorphism is associated with gestational diabetes mellitus in Turkish women. BMC Med. Genet. 2019, 20, 82. [Google Scholar] [CrossRef]
- Aslani, S.; Hossein-Nezhad, A.; Mirzaei, K.; Maghbooli, Z.; Afshar, A.N.; Karimi, F. VDR FokI polymorphism and its potential role in the pathogenesis of gestational diabetes mellitus and its complications. Gynecol. Endocrinol. 2011, 27, 1055–1060. [Google Scholar] [CrossRef] [PubMed]
- Javorski, N.; Lima, C.A.D.; Silva, L.V.C.; Crovella, S.; de Azêvedo Silva, J. Vitamin D receptor (VDR) polymorphisms are associated to spontaneous preterm birth and maternal aspects. Gene 2018, 642, 58–63. [Google Scholar] [CrossRef]
- Liu, J.; Dai, Q.; Li, W.; Guo, Y.; Dai, A.; Wang, Y.; Deng, M.; Tang, Z.; She, L.; Chen, X.; et al. Association of vitamin D receptor gene polymorphisms with gestational diabetes mellitus-a case control study in Wuhan, China. BMC Pregnancy Childbirth 2021, 21, 142. [Google Scholar] [CrossRef]
- Rahmannezhad, G.; Mashayekhi, F.J.; Goodarzi, M.T.; Rezvanfar, M.R.; Sadeghi, A. Association between vitamin D receptor ApaI and TaqI gene polymorphisms and gestational diabetes mellitus in an Iranian pregnant women population. Gene 2016, 581, 43–47. [Google Scholar] [CrossRef]
- Shaat, N.; Katsarou, A.; Shahida, B.; Prasad, R.B.; Kristensen, K.; Planck, T. Association between the rs1544410 polymorphism in the vitamin D receptor (VDR) gene and insulin secretion after gestational diabetes mellitus. PLoS ONE 2020, 15, e0232297. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, O.; Li, W.; Ma, L.; Ping, F.; Chen, L.; Nie, M. Variants in Vitamin D Binding Protein Gene Are Associated with Gestational Diabetes Mellitus. Medicine 2015, 94, e1693. [Google Scholar] [CrossRef] [PubMed]
- Radwan, M.E.-H.; Taha, H.S.; ElSayed, A.I.; Omar, A.A. Evaluation of VDR gene FokI polymorphism and serum vitamin D level in gestational diabetes mellitus (Egyptian case-control study). Meta Gene 2021, 29, 100908. [Google Scholar]
- Siqueira, T.W.; Araujo Júnior, E.; Mattar, R.; Daher, S. Assessment of Polymorphism of the VDR Gene and Serum Vitamin D Values in Gestational Diabetes Mellitus. Rev. Bras. Ginecol. Obstet. 2019, 41, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Zhu, B.; Huang, K.; Yan, S.; Hao, J.; Zhu, P.; Chen, Y.; Ye, A.; Tao, F. VDR Variants rather than Early Pregnancy Vitamin D Concentrations Are Associated with the Risk of Gestational Diabetes: The Ma’anshan Birth Cohort (MABC) Study. J. Diabetes Res. 2019, 2019, 8313901. [Google Scholar] [CrossRef]
- Beysel, S.; Eyerci, N.; Ulubay, M.; Caliskan, M.; Kizilgul, M.; Hafızoğlu, M.; Cakal, E. Maternal genetic contribution to pre-pregnancy obesity, gestational weight gain, and gestational diabetes mellitus. Diabetol. Metab. Syndr. 2019, 11, 37. [Google Scholar]
- AbdulKhaliq¹, R.J.; Farhan, S.H.; AlKhateeb, H.M. The relationship of Taq I (rs731236) polymorphism in vitamin D receptor gene besidesgestational diabetes mellitus in Iraqi prenatal women. Ann. Trop Med. Public Health 2020, 23, SP231833. [Google Scholar]
- Al-Mawla, R.H.; Ali, H.H.; Al-Ani, W.Y. Association between Vitamin D Receptor Gene Foki Polymorphism and Gestational Diabetes Mellitus among Iraqi Pregnant Women. Indian J. Forensic Med. Toxicol. 2020, 14, 1894–1899. [Google Scholar]
- Liu, S. The role of vitamin D receptor gene polymorphisms in gestational diabetes mellitus susceptibility: A meta-analysis. Diabetol. Metab. Syndr. 2021, 13, 144. [Google Scholar]
- Wang, B.; Xue, X. Investigations of associations between seven gene polymorphisms and gestational diabetes mellitus: Evidence from a meta-analysis. Gynecol. Obstet. Investig. 2020, 85, 229–236. [Google Scholar] [CrossRef]
- Chen, X.; Wang, W.; Wang, Y.; Han, X.; Gao, L. Vitamin D receptor polymorphisms associated with susceptibility to obesity: A meta-analysis. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019, 25, 8297. [Google Scholar]
- Tabaei, S.; Motallebnezhad, M.; Tabaee, S.S. Vitamin D receptor (VDR) gene polymorphisms and risk of coronary artery disease (CAD): Systematic review and meta-analysis. Biochem. Genet. 2021, 59, 813–836. [Google Scholar] [CrossRef] [PubMed]
- Shahmoradi, A.; Aghaei, A.; Ghaderi, K.; Rezaei, M.J.; Azarnezhad, A. A meta-analysis of the association of ApaI, BsmI, FokI, and TaqI polymorphisms in the vitamin D receptor gene with the risk of polycystic ovary syndrome in the Eastern Mediterranean Regional Office population. Int. J. Reprod. Biomed. 2022, 20, 433. [Google Scholar] [CrossRef] [PubMed]
- Poel, Y.; Hummel, P.; Lips, P.; Stam, F.; Van Der Ploeg, T.; Simsek, S. Vitamin D and gestational diabetes: A systematic review and meta-analysis. Eur. J. Intern. Med. 2012, 23, 465–469. [Google Scholar] [PubMed]
- Agüero-Domenech, N.; Jover, S.; Sarrión, A.; Baranda, J.; Quesada-Rico, J.A.; Pereira-Expósito, A.; Gil-Guillén, V.; Cortés-Castell, E.; García-Teruel, M.J. Vitamin D deficiency and gestational diabetes mellitus in relation to body mass index. Nutrients 2021, 14, 102. [Google Scholar] [PubMed]
- Özdemir, A.A.; Gündemir, Y.E.; Küçük, M.; Sarıcı, D.Y.; Elgörmüş, Y.; Çağ, Y.; Bilek, G. Vitamin D deficiency in pregnant women and their infants. J. Clin. Res. Pediatr. Endocrinol. 2018, 10, 44. [Google Scholar] [CrossRef] [PubMed]
- Yue, C.-Y.; Ying, C.-M. Sufficience serum vitamin D before 20 weeks of pregnancy reduces the risk of gestational diabetes mellitus. Nutr. Metab. 2020, 17, 89. [Google Scholar]
- Ibrahim, G.A.; Salem, I.M.A.; Bakr, H.G.; Al Naggar, A.M.T.; Omar, R.E.H. Low Vitamin D as A Risk Factor for Gestational Diabetes in Egyptian Pregnant Women. Egypt. J. Hosp. Med. 2020, 78, 311–316. [Google Scholar] [CrossRef]
- Rangaraju, H.; Sankar, S.L. Vitamin D Levels in Gestational Diabetes Mellitus and its Influence on Future Type 2 Diabetes Mellitus-An Observational Study. J. Clin. Diagn. Res. 2020, 14, BC17–BC20. [Google Scholar] [CrossRef]
- Xia, J.; Song, Y.; Rawal, S.; Wu, J.; Hinkle, S.N.; Tsai, M.Y.; Zhang, C. Vitamin D status during pregnancy and the risk of gestational diabetes mellitus: A longitudinal study in a multiracial cohort. Diabetes Obes. Metab. 2019, 21, 1895–1905. [Google Scholar] [CrossRef]
- Triunfo, S.; Lanzone, A.; Lindqvist, P. Low maternal circulating levels of vitamin D as potential determinant in the development of gestational diabetes mellitus. J. Endocrinol. Investig. 2017, 40, 1049–1059. [Google Scholar]
- Zuhur, S.S.; Erol, R.S.; Kuzu, I.; Altuntas, Y. The relationship between low maternal serum 25-hydroxyvitamin D levels and gestational diabetes mellitus according to the severity of 25-hydroxyvitamin D deficiency. Clinics 2013, 68, 658–664. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Gong, Y.; Xue, H.; Xiong, J.; Cheng, G. Vitamin D and gestational diabetes mellitus: A systematic review based on data free of Hawthorne effect. BJOGInternational J. Obstet. Gynaecol. 2018, 125, 784–793. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.; Zhang, Y.; Wang, X.; You, L.; Xu, P.; Cui, X.; Zhu, L.; Ji, C.; Guo, X.; Wen, J. Maternal vitamin D status and risk of gestational diabetes: A meta-analysis. Cell. Physiol. Biochem. 2018, 45, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhang, C.; Song, Y.; Zhang, Z. Serum vitamin D deficiency and risk of gestational diabetes mellitus: A meta-analysis. Arch. Med. Sci. 2020, 16, 742–751. [Google Scholar] [CrossRef] [PubMed]
- Milajerdi, A.; Abbasi, F.; Mousavi, S.M.; Esmaillzadeh, A. Maternal vitamin D status and risk of gestational diabetes mellitus: A systematic review and meta-analysis of prospective cohort studies. Clin. Nutr. 2021, 40, 2576–2586. [Google Scholar] [PubMed]
- Amraei, M.; Mohamadpour, S.; Sayehmiri, K.; Mousavi, S.F.; Shirzadpour, E.; Moayeri, A. Effects of vitamin D deficiency on incidence risk of gestational diabetes mellitus: A systematic review and meta-analysis. Front. Endocrinol. 2018, 9, 7. [Google Scholar] [CrossRef]
- Wu, C.; Song, Y.; Wang, X. Vitamin D Supplementation for the Outcomes of Patients with Gestational Diabetes Mellitus and Neonates: A Meta-Analysis and Systematic Review. Int. J. Clin. Pract. 2023, 2023, 1907222. [Google Scholar]
- Lei, W.; Tian, H.; Xia, Y. Association between the Taq I (rs731236 T > C) gene polymorphism and dental caries risk: A meta-analysis. Genet. Test. Mol. Biomark. 2021, 25, 368–375. [Google Scholar] [CrossRef]
- Almidani, E.; Barkoumi, A.; Elsaidawi, W.; Al Aliyan, S.; Kattan, A.; Alhazzani, F.; bin Jabr, M.; Binmanee, A.; Alsahan, N.; Alazmeh, S. Maternal Vitamin D Levels and Its Correlation with Low Birth Weight in Neonates: A Tertiary Care Hospital Experience in Saudi Arabia. Cureus 2021, 13, e14528. [Google Scholar] [CrossRef]
- Alsrhani, A. Prevalence of Vitamin D Deficiency in Pregnant women of Al Jouf region, Kingdom of Saudi Arabia. Pak. J. Med. Health Sci. 2020, 14, 734–737. [Google Scholar]
- Anouti, F.A.; Ahmed, L.A.; Riaz, A.; Grant, W.B.; Shah, N.; Ali, R.; Alkaabi, J.; Shah, S.M. Vitamin D deficiency and its associated factors among female migrants in the United Arab Emirates. Nutrients 2022, 14, 1074. [Google Scholar]
- Marozik, P.M.; Tamulaitiene, M.; Rudenka, E.; Alekna, V.; Mosse, I.; Rudenka, A.; Samokhovec, V.; Kobets, K. Association of vitamin D receptor gene variation with osteoporosis risk in Belarusian and Lithuanian postmenopausal women. Front. Endocrinol. 2018, 9, 305. [Google Scholar] [CrossRef]
- Cauci, S.; Migliozzi, F.; Trombetta, C.; Venuto, I.; Saccheri, P.; Travan, L. Low back pain and FokI (rs2228570) polymorphism of vitamin D receptor in athletes. BMC Sports Science. Med. Rehabil. 2017, 9, 4. [Google Scholar]
- Meza-Meza, M.R.; Vizmanos, B.; Rivera-Escoto, M.; Ruiz-Ballesteros, A.I.; Pesqueda-Cendejas, K.; Parra-Rojas, I.; Montoya-Buelna, M.; Luquín, S.; Campos-López, B.; Mora-García, P.E. Vitamin D Receptor (VDR) Genetic Variants: Relationship of FokI Genotypes with VDR Expression and Clinical Disease Activity in Systemic Lupus Erythematosus Patients. Genes 2022, 13, 2016. [Google Scholar]
- AbdElneam, A.I.; Al-Dhubaibi, M.S.; Bahaj, S.S.; Mohammed, G.F. TaqI polymorphism T/t genotypes at the vitamin D receptor gene (VDR) are associated with increased serum vitamin D levels in mild and moderate psoriasis vulgaris: A pilot study. J. Gene Med. 2022, 24, e3449. [Google Scholar] [CrossRef] [PubMed]
- AbdElneam, A.I.; Al-Dhubaibi, M.S.; Bahaj, S.S.; Mohammed, G.F. The vitamin D receptor gene polymorphism rs1544410 T/T genotype as a predictor of factor vitamin D thresholds deficiency in patients with psoriasis vulgaris-A preliminary study. J. Cosmet. Dermatol. 2023, 22, 1642–1646. [Google Scholar] [CrossRef] [PubMed]
- Abo-Amer, Y.E.; Mohamed, A.A.; Elhoseeny, M.M.; Rezk, S.M.; Abdel-Salam, S.; Alrohaimi, A.H.; Abdelgeliel, A.S.; Alzahrani, S.S.; Jafri, I.; Alqahtani, L.S.; et al. Association Between Vitamin D Receptor Polymorphism and the Response to Helicobacter Pylori Treatment. Infect. Drug Resist. 2023, 16, 4463–4469. [Google Scholar] [CrossRef]
- Al Thomali, A.; Daghestani, M.H.; Daghestani, M.H.; Kaya, N.; Warsy, A. Polymorphic Variations in VDR Gene in Saudi Women with and without Polycystic Ovary Syndrome (PCOS) and Significant Influence of Seven Polymorphic Sites on Anthropometric and Hormonal Parameters. J. Med. Biochem. 2018, 37, 415–425. [Google Scholar] [CrossRef]
- Al-Daghri, N.M.; Al-Attas, O.; Alokail, M.S.; Alkharfy, K.M.; Draz, H.M.; Agliardi, C.; Mohammed, A.K.; Guerini, F.R.; Clerici, M. Vitamin D receptor gene polymorphisms and HLA DRB1*04 cosegregation in Saudi type 2 diabetes patients. J. Immunol. 2012, 188, 1325–1332. [Google Scholar] [CrossRef] [PubMed]
- Al-Daghri, N.M.; Al-Attas, O.S.; Alkharfy, K.M.; Khan, N.; Mohammed, A.K.; Vinodson, B.; Ansari, M.G.; Alenad, A.; Alokail, M.S. Association of VDR-gene variants with factors related to the metabolic syndrome, type 2 diabetes and vitamin D deficiency. Gene 2014, 542, 129–133. [Google Scholar] [CrossRef]
- Al-Ghafari, A.B.; Balamash, K.S.; Al Doghaither, H.A. Relationship between Serum Vitamin D and Calcium Levels and Vitamin D Receptor Gene Polymorphisms in Colorectal Cancer. Biomed. Res. Int. 2019, 2019, 8571541. [Google Scholar] [CrossRef]
- Al-Ghafari, A.B.; Balamash, K.S.; Al Doghaither, H.A. TaqI and ApaI Variants of Vitamin D Receptor Gene Increase the Risk of Colorectal Cancer in a Saudi Population. Saudi J. Med. Med. Sci. 2020, 8, 188–195. [Google Scholar] [CrossRef]
- Al-Hazmi, A.S. Association of Vitamin D deficiency and Vitamin D Receptor Gene Polymorphisms with Type 2 diabetes mellitus Saudi patients. Afr. Health Sci. 2019, 19, 2812–2818. [Google Scholar] [CrossRef]
- Al-Hazmi, A.S.; Al-Mehmadi, M.M.; Al-Bogami, S.M.; Shami, A.A.; Al-Askary, A.A.; Alomery, A.M.; Al-Shehri, S.S.; Dahlawi, H.; Abdulrazag, K.; Ali, T.; et al. Vitamin D receptor gene polymorphisms as a risk factor for obesity in Saudi men. Electron. Physician 2017, 9, 5427–5433. [Google Scholar] [CrossRef]
- Alhetheli, G.; Al-Dhubaibi, M.S.; Bahaj, S.S.; AbdElneam, A.I. Vitamin D Receptor Gene Polymorphism ApaI as a Predisposing Factor for Psoriasis and Its Relation with Serum Vitamin D Levels and Psoriasis Severity. Cureus 2022, 14, e32715. [Google Scholar] [CrossRef] [PubMed]
- Ali, R.; Fawzy, I.; Mohsen, I.; Settin, A. Evaluation of vitamin D receptor gene polymorphisms (Fok-I and Bsm-I) in T1DM Saudi children. J. Clin. Lab. Anal. 2018, 32, e22397. [Google Scholar] [CrossRef] [PubMed]
- Alkhayal, K.A.; Awadalia, Z.H.; Vaali-Mohammed, M.A.; Al Obeed, O.A.; Al Wesaimer, A.; Halwani, R.; Zubaidi, A.M.; Khan, Z.; Abdulla, M.H. Association of Vitamin D Receptor Gene Polymorphisms with Colorectal Cancer in a Saudi Arabian Population. PLoS ONE 2016, 11, e0155236. [Google Scholar] [CrossRef]
- Alkhedaide, A.Q.; Mergani, A.; Aldhahrani, A.A.; Sabry, A.; Soliman, M.M.; Nassan, M.A.; Ismail, T.A. Association of vitamin D receptor gene polymorphisms with type 2 diabetes mellitus in Taif population: A case-control study. Braz. J. Biol. 2021, 84, e250739. [Google Scholar] [CrossRef]
- Ansari, M.G.A.; Mohammed, A.K.; Wani, K.A.; Hussain, S.D.; Alnaami, A.M.; Abdi, S.; Aljohani, N.J.; Al-Daghri, N.M. Vitamin D Receptor Gene Variants Susceptible to Osteoporosis in Arab Post-Menopausal Women. Curr. Issues Mol. Biol. 2021, 43, 1325–1334. [Google Scholar] [CrossRef]
- Areeshi, M.Y.; Mandal, R.K.; Dar, S.A.; Alshahrani, A.M.; Ahmad, A.; Jawed, A.; Wahid, M.; Lohani, M.; Panda, A.K.; Haque, S. A reappraised meta-analysis of the genetic association between vitamin D receptor BsmI (rs1544410) polymorphism and pulmonary tuberculosis risk. Biosci. Rep. 2017, 37, BSR20170247. [Google Scholar] [CrossRef]
- Jawadi, A.H.; Wakeel, A.; Tamimi, W.; Nasr, A.; Iqbal, Z.; Mashhour, A.; Fattah, M.A.; Alkhanein, N.; Abu Jaffal, A.S. Association analysis between four vitamin D receptor gene polymorphisms and developmental dysplasia of the hip. J. Genet. 2018, 97, 925–930. [Google Scholar] [PubMed]
- Jayaraj, J.M.; Kuriakose, B.B.; Alhazmi, A.H.; Muthusamy, K. Structural and functional insights on vitamin D receptor and CYP24A1 deleterious single nucleotide polymorphisms: A computational and pharmacogenomics perpetual approach. Cell Biochem. Funct. 2021, 39, 874–885. [Google Scholar] [CrossRef] [PubMed]
- Karras, S.N.; Koufakis, T.; Antonopoulou, V.; Goulis, D.G.; Alaylıoğlu, M.; Dursun, E.; Gezen-Ak, D.; Annweiler, C.; Pilz, S.; Fakhoury, H.; et al. Vitamin D receptor Fokl polymorphism is a determinant of both maternal and neonatal vitamin D concentrations at birth. J. Steroid Biochem. Mol. Biol. 2020, 199, 105568. [Google Scholar] [CrossRef]
- Lin, J.J.; Loucks, C.M.; Trueman, J.N.; Drögemöller, B.I.; Wright, G.E.B.; Yoshida, E.M.; Ford, J.A.; Lee, S.S.; Kim, R.B.; Al-Judaibi, B.; et al. Novel variant in glycophorin c gene protects against ribavirin-induced anemia during chronic hepatitis C treatment. Biomed. Pharmacother. 2021, 143, 112195. [Google Scholar] [CrossRef]
- Lin, N.U.; Malloy, P.J.; Sakati, N.; al-Ashwal, A.; Feldman, D. A novel mutation in the deoxyribonucleic acid-binding domain of the vitamin D receptor causes hereditary 1,25-dihydroxyvitamin D-resistant rickets. J. Clin. Endocrinol. Metab. 1996, 81, 2564–2569. [Google Scholar] [CrossRef][Green Version]
- Lone, N.M.; Riaz, S.; Eusaph, A.Z.; Mein, C.A.; Wozniak, E.L.; Xenakis, T.; Wu, Z.; Younis, S.; Jolliffe, D.A.; Junaid, K.; et al. Genotype-independent association between vitamin D deficiency and polycystic ovarian syndrome in Lahore, Pakistan. Sci. Rep. 2020, 10, 2290. [Google Scholar] [CrossRef]
- Mansy, W.; Ibrahim, N.H.; Al-Gawhary, S.; Alsubaie, S.S.; Abouelkheir, M.M.; Fatani, A.; Abd Al Reheem, F.; El Awady, H.; Zakaria, E.A. Vitamin D status and vitamin D receptor gene polymorphism in Saudi children with acute lower respiratory tract infection. Mol. Biol. Rep. 2019, 46, 1955–1962. [Google Scholar] [CrossRef]
- Miettinen, M.E.; Smart, M.C.; Kinnunen, L.; Harjutsalo, V.; Reinert-Hartwall, L.; Ylivinkka, I.; Surcel, H.M.; Lamberg-Allardt, C.; Hitman, G.A.; Tuomilehto, J. Genetic determinants of serum 25-hydroxyvitamin D concentration during pregnancy and type 1 diabetes in the child. PLoS ONE 2017, 12, e0184942. [Google Scholar] [CrossRef]
- Miettinen, M.E.; Smart, M.C.; Kinnunen, L.; Keinänen-Kiukaanniemi, S.; Moilanen, L.; Puolijoki, H.; Saltevo, J.; Oksa, H.; Hitman, G.A.; Tuomilehto, J.; et al. The effect of age and gender on the genetic regulation of serum 25-hydroxyvitamin D—The FIN-D2D population-based study. J. Steroid Biochem. Mol. Biol. 2018, 178, 229–233. [Google Scholar] [CrossRef]
- Miettinen, M.E.; Smart, M.C.; Kinnunen, L.; Mathews, C.; Harjutsalo, V.; Surcel, H.M.; Lamberg-Allardt, C.; Tuomilehto, J.; Hitman, G.A. Maternal VDR variants rather than 25-hydroxyvitamin D concentration during early pregnancy are associated with type 1 diabetes in the offspring. Diabetologia 2015, 58, 2278–2283. [Google Scholar] [CrossRef]
- Mosaad, Y.M.; Hammad, E.M.; Fawzy, Z.; Abdal Aal, I.A.; Youssef, H.M.; ElSaid, T.O.; Monir, R.; El-Deek, B.S. Vitamin D receptor gene polymorphism as possible risk factor in rheumatoid arthritis and rheumatoid related osteoporosis. Hum. Immunol. 2014, 75, 452–461. [Google Scholar] [CrossRef] [PubMed]
- Mostafa-Hedeab, G.; Sabry, D.; Abdelaziz, G.M.; Ewaiss, M.; Adli, N.; Fathy, W. Influence of Vitamin D Receptor Gene Polymorphisms on Response to Pegylated Interferon in Chronic Hepatitis B Egyptian Patients. Rep. Biochem. Mol. Biol. 2018, 6, 186–196. [Google Scholar]
- Nemenqani, D.M.; Karam, R.A.; Amer, M.G.; Abd El Rahman, T.M. Vitamin D receptor gene polymorphisms and steroid receptor status among Saudi women with breast cancer. Gene 2015, 558, 215–219. [Google Scholar] [CrossRef]
- Sahmoud, S.; Ibrahim, M.S.; Toraih, E.A.; Kamel, N.; Fawzy, M.S.; Elfiky, S. Association of VDBP rs4701 Variant, but not VDR/RXR-α Over-Expression with Bone Mineral Density in Pediatric Well-Chelated β-Thalassemia Patients. Mediterr. J. Hematol. Infect. Dis. 2020, 12, e2020037. [Google Scholar] [CrossRef] [PubMed]
- Salem, D.A.; Alghamdi, M.A.; Al-Ghamdi, H.S.; Alghamdi, B.A.; Elsamanoudi, A.Z.E.; Hasan, A. Vitamin D status, vitamin D receptor gene polymorphism, and haplotype in patients with cutaneous leishmaniasis: Correlation with susceptibility and parasite load index. PLoS Negl. Trop. Dis. 2023, 17, e0011393. [Google Scholar] [CrossRef]
- Shafie, A.; Askary, A.E.; Almehmadi, M.; Allam, H.H.; Elsayyad, L.K.; Hassan, A.F.; Althobaiti, B.B.; Nadheef, A.; Alharthi, A.H.; Gharib, A.F. Association of Vitamin D Deficiency and Vitamin D Receptor Genetic Variants with Coronary Artery Disease in Type 2 Diabetic Saudi Patients. Vivo 2022, 36, 1444–1452. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, I.A.; Aboukhalil, R.; Abulata, N.; Abdel-Raouf, R.; Meligy, B.; Abdel-Dayem, O. Vitamin D Insufficiency is Not Associated with Pediatric and Adolescent Immune Thrombocytopenia: A Study in Conjunction with its Receptor Genetic Polymorphisms. J. Pediatr. Hematol. Oncol. 2021, 43, e1–e6. [Google Scholar] [CrossRef]
- Taha, I.M.; Allah, A.M.A.; El Tarhouny, S. Association of Vitamin D Gene Polymorphisms and Bone Mineral Density in Healthy young Saudi Females. Curr. Mol. Med. 2019, 19, 196–205. [Google Scholar] [CrossRef]
- Tayeb, M.T.; Clark, C.; Haites, N.E.; Sharp, L.; Murray, G.I.; McLeod, H.L. Vitamin D receptor, HER-2 polymorphisms and risk of prostate cancer in men with benign prostate hyperplasia. Saudi Med. J. 2004, 25, 447–451. [Google Scholar]
- Zeidan, N.M.S.; Lateef, H.; Selim, D.M.; Razek, S.A.; Abd-Elrehim, G.A.B.; Nashat, M.; ElGyar, N.; Waked, N.M.; Soliman, A.A.; Elhewala, A.A.; et al. Vitamin D deficiency and vitamin D receptor FokI polymorphism as risk factors for COVID-19. Pediatr. Res. 2023, 93, 1383–1390. [Google Scholar] [CrossRef]
- Farhat, K.H.; Arafa, M.A.; Rabah, D.M.; Amin, H.S.; Ibrahim, N.K. Vitamin D status and its correlates in Saudi male population. BMC Public Health 2019, 19, 211. [Google Scholar]
- Al-Shafei, A.I.; Rayis, D.A.; Mohieldein, A.H.; El-Gendy, O.A.; Adam, I. Maternal early pregnancy serum level of 25-Hydroxyvitamin D and risk of gestational diabetes mellitus. Int. J. Gynecol. Obstet. 2021, 152, 382–385. [Google Scholar]
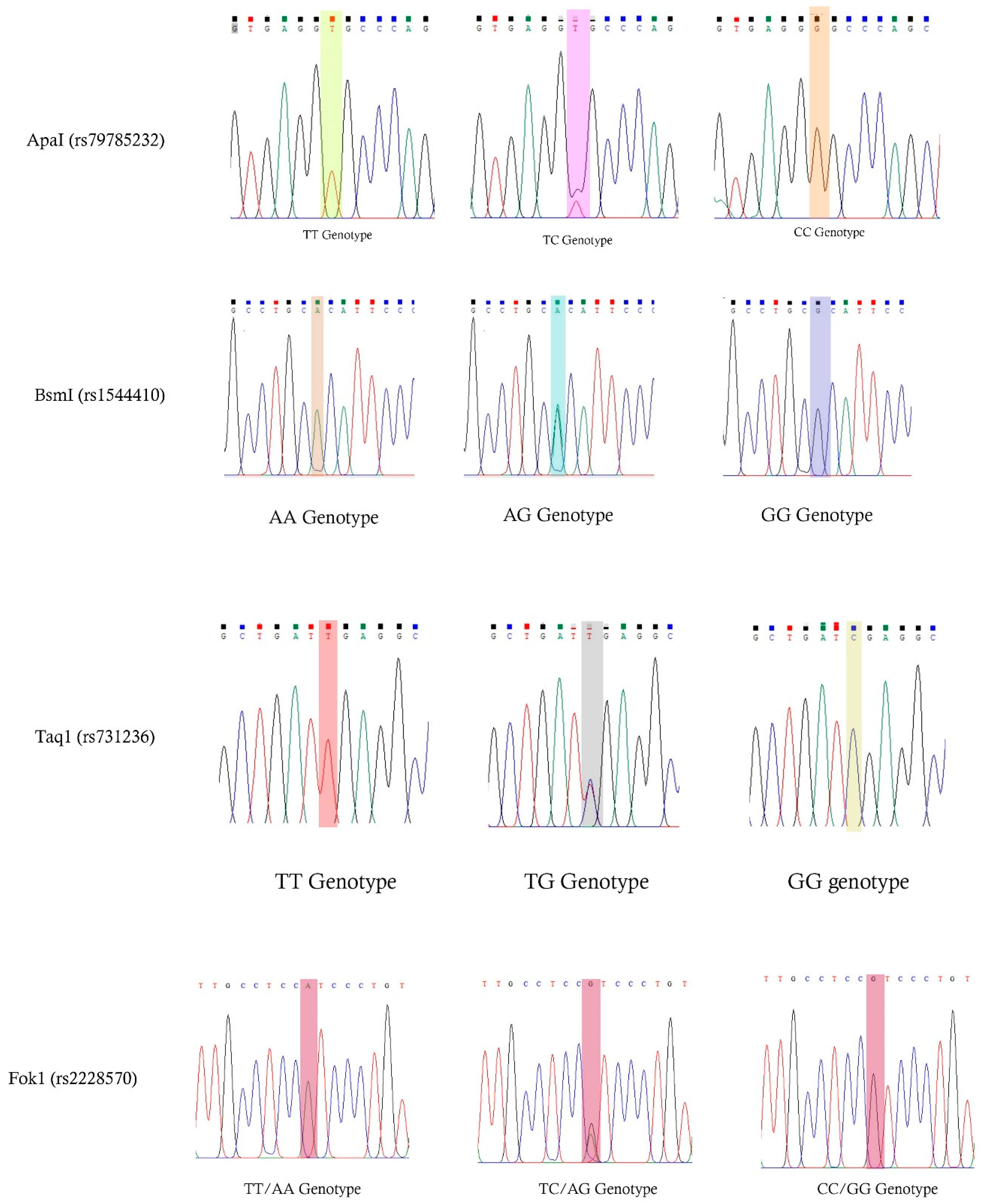


| SNP | rs Number | Region | Position | Variant | Forward Primer | Reverse Primer | Tm | PCR | Restriction Enzyme |
|---|---|---|---|---|---|---|---|---|---|
| ApaI | rs79785232 | Intron-8 | 11740553 | A > C | AGAGCATGGACAGGGAGC | GCAACTCCTCATGGCTGAGGTC | 68 °C | 746 bp | ApaI [GGGCC↑C] |
| BsmI | rs1544410 | Intron-8 | 154441349 | A > G | CAACCAAGACTACAACCG | AACCAGCGGAAGAGGTCAAGG | 66 °C | 872 bp | BsmI [G↑CATTC] |
| FokI | rs2228570 | Exon-2 | 154441452 | C > T | AGAGCATGGACAGGGAGC | GCAACTCCTCATGGCTGAGGTC | 68 °C | 267 bp | FokI [CGATG(N)9↑] |
| TaqI | rs731236 | Exon-9 | 1540309 | T > C | AGCTGGCCCTGGCACTGAC | ATGGAAACACCTTGCTTCTTCT | 68 °C | 746 bp | TaqI [T↑CGA] |
| Pregnant Women Parameters | GDM (n = 90) | Non-GDM (n = 90) | p-Values |
|---|---|---|---|
| Age (Years) | 32.34 ± 5.42 | 28.26 ± 6.39 | 0.0001 |
| Weight (kgs) | 76.75 ± 12.85 | 73.57 ± 12.38 | 0.092 |
| Height (cm) | 158.03 ± 5.84 | 157.86 ± 5.11 | 0.835 |
| BMI (kg/m2) | 30.60 ± 4.87 | 29.39 ± 4.38 | 0.081 |
| SBP (mmHg) | 130.20 ± 11.95 | 120.77 ± 6.10 | <0.0001 |
| DBP (mmHg) | 81.47 ± 7.84 | 78.00 ± 5.02 | 0.0005 |
| FPG (mmol/L) | 5.54 ± 1.69 | 4.55 ± 0.62 | 0.0004 |
| PPBG (mmol/L) | 8.51 ± 17.63 | 4.79 ± 0.83 | <0.0001 |
| OGTT-1h (mmol/L) | 11.45 ± 1.42 | 7.05 ± 1.46 | <0.0001 |
| OGTT-2h (mmol/L) | 9.81 ± 1.58 | 6.31 ± 1.54 | <0.0001 |
| HbA1c (%) | 5.59 ± 0.52 | 5.26 ± 0.33 | 0.0008 |
| TG (mmol/L) | 1.87 ± 1.07 | 1.54 ± 2.11 | 0.187 |
| TC (mmol/L) | 5.39 ± 1.14 | 5.70 ± 1.27 | 0.086 |
| HDLc (mmol/L) | 0.71 ± 0.36 | 0.92 ± 0.44 | 0.0005 |
| LDLc (mmol/L) | 3.83 ± 0.86 | 3.71 ± 0.98 | 0.383 |
| 25 hydroxyvitamin-D (nmol/L) | 47.83 ± 21.23 | 50.51 ± 20.59 | 0.391 |
| Rx (Diet: Insulin) | 86 (95.6%): 04 (4.4%) | NA | NA |
| Family History of GDM | 23 (25.6%) | 20 (22.2%) | 0.087 |
| Family History of T2DM | 46 (51.1%) | 39 (43.3%) | 0.042 |
| Family History of HTN | 34 (37.8%) | 33 (36.7%) | 0.966 |
| rs Number | Alleles | GDM (n = 90) | Non-GDM (n = 90) | OR (95%CI) and p-Value |
|---|---|---|---|---|
| ApaI (rs79785232) | A | 116 (64.4%) | 131 (72.8%) | Reference |
| C | 64 (35.6%) | 49 (27.2%) | OR-1.47 (95%CI: 0.94–42.31) p = 0.088 | |
| BsmI (rs1544410) | A | 102 (71.1%) | 132 (73.3%) | Reference |
| G | 78 (28.9%) | 48 (26.7%) | OR-2.10 (95%CI: 1.35–3.24) p = 0.0009 | |
| FokI (rs2228570) | C | 143 (79.4%) | 146 (81.1%) | Reference |
| T | 37 (20.6%) | 34 (18.9%) | OR-1.11 (95%CI: 0.66–1.86) p = 0.691 | |
| TaqI (rs731236) | T | 122 (67.8%) | 143 (79.4%) | Reference |
| C | 58 (32.2%) | 37 (20.6%) | OR-1.83 (95%CI: 1.13–2.96) p = 0.012 |
| Specific rs Number | Genotypes | GDM (n = 90) | Non-GDM (n = 90) | OR (95%CI) and p-Value |
|---|---|---|---|---|
| ApaI (rs79785232) | AA (Wild type) | 35 (38.9%) | 49 (54.4%) | Reference |
| AC (Heterozygous co-dominant) | 46 (51.1%) | 33 (36.7%) | OR-1.95 (95%CI: 1.04–3.63) p = 0.034 | |
| CC (Homozygous co-dominant) | 09 (10%) | 08 (8.9%) | OR-1.47 (95%CI: 0.51–4.22) p = 0.463 | |
| AC + CC vs. AA (Dominant) | 55 (61.1%) | 41 (45.6%) | OR-1.87 (95%CI: 1.03–3.39) p = 0.036 | |
| AA + CC vs. AC (Co-Dominant model) | 44 (48.9%) | 57 (63.3%) | OR-0.55 (95%CI: 0.30–1.01) p = 0.050 | |
| CC vs. AC + AA (Recessive) | 09 (10%) | 08 (8.9%) | OR-1.13 (95%CI: 0.41–3.09) p = 0.798 | |
| HWE analysis | ꭓ2 = 1.19; p = 0.27 | ꭓ2 = 0.03; p = 0.85 | ||
| BsmI (rs1544410) | AA (Wild type) | 31 (34.4%) | 46 (51.1%) | Reference |
| AG (Heterozygous co-dominant) | 40 (44.5%) | 40 (44.5%) | OR-1.48 (95%CI: 0.78–2.79) p = 0.220 | |
| GG (Homozygous co-dominant) | 19 (21.1%) | 04 (4.4%) | OR-7.04 (95%CI: 2.18–22.72) p = 0.0003 | |
| AG + GG vs. AA (Dominant) | 59 (65.6%) | 44 (48.9%) | OR-1.99 (95%CI: 1.09–3.62) p = 0.023 | |
| AA + GG vs. AG (Co-dominant model) | 50 (55.6%) | 50 (55.6%) | OR-1.00 (95%CI: 0.55–1.80) p = 0.999 | |
| GG vs. AG + AA (Recessive) | 19 (21.1%) | 4 (4.4%) | OR-5.75 (95%CI: 1.87–17.69) p = 0.0008 | |
| HWE analysis | ꭓ2 = 0.81; p = 0.36 | ꭓ2 = 1.67; p = 0.19 | ||
| FokI (rs2228570) | CC (Wild type) | 59 (65.5%) | 61 (67.8%) | Reference |
| CT (Heterozygous co-dominant) | 25 (27.8%) | 24 (26.7%) | OR-1.07 (95%CI: 0.55–2.09) p = 0.826 | |
| TT (Homozygous co-dominant) | 06 (6.7%) | 05 (5.5%) | OR-1.24 (95%CI: 0.35–4.28) p = 0.099 | |
| TC + CC vs. TT (Dominant model) | 31 (34.4%) | 29 (32.2%) | OR-1.10 (95%CI: 0.59–2.05) p = 0.751 | |
| CC + TT vs. CT (Co-dominant model) | 65 (72.2%) | 66 (73.3%) | OR-0.94 (95%CI: 0.49–1.82) p = 0.867 | |
| CC vs. TC + TT (Recessive model) | 19 (21.1%) | 11 (12.2%) | OR-1.92 (95%CI: 0.85–4.31) p = 0.109 | |
| HWE analysis | ꭓ2 = 2.01; p = 0.15 | ꭓ2 = 1.51; p = 0.21 | ||
| TaqI (rs731236) | TT (Wild type) | 43 (47.8%) | 57 (63.3%) | Reference |
| TC (Heterozygous co-dominant) | 36 (40.0%) | 29 (32.2%) | OR-1.64 (95%CI: 0.87–3.08) p = 0.119 | |
| CC (Homozygous mutant) | 11 (12.2%) | 04 (4.5%) | OR-3.64 (95%CI: 1.08–12.23) p = 0.028 | |
| TC + CC vs. TT (Dominant model) | 47 (52.2%) | 33 (36.7%) | OR-1.88 (95%CI: 1.04–3.42) p = 0.035 | |
| CC + TT vs. TC (Co-dominant model) | 54 (60%) | 61 (67.8%) | OR-0.71 (95%CI: 0.38–1.31) p = 0.278 | |
| CC vs. TC + TT (Recessive model) | 11 (12.2%) | 04 (4.5%) | OR-2.99 (95%CI: 0.91–9.78) p = 0.059 | |
| HWE analysis | ꭓ2 = 0.63; p = 0.42 | ꭓ2 = 0.01; p = 0.89 |
| Pregnant Women | Vitamin D (Categories) | Total | ꭓ2 | p-Value | |||
|---|---|---|---|---|---|---|---|
| Deficient (<30 nmol/L) | Insufficient (30–50 nmol/L) | Sufficient (>50 nmol/L) | |||||
| GDM (n = 90) | 24 (26.7%) | 28 (31.1%) | 38 (42.2%) | 90 (100%) | |||
| Non-GDM (n = 90) | 17 (18.9%) | 25 (27.8%) | 48 (53.3%) | 90 (100%) | 2.528 | 0.283 | |
| Total (n = 180) | 41 (22.8%) | 53 (29.4%) | 86 (47.8%) | 180 (100%) | |||
| Pregnant Women | BMI (Categories) | Total | ꭓ2 | p-Value | |||
| Normal BMI | Overweight | Obese | Morbidly Obese | ||||
| GDM (n = 90) | 13 (14.4%) | 25 (27.8%) | 37 (41.1%) | 15 (16.7%) | 90 (100%) | ||
| Non-GDM (n = 90) | 15 (16.7%) | 31 (34.4%) | 38 (42.2%) | 06 (6.7%) | 90 (100%) | 4.656 | 0.199 |
| Total (n = 180) | 28 (15.6%) | 56 (31.1%) | 75 (41.7%) | 21 (11.7%) | 180 (100%) | ||
| Covariates | Deficient Levels: <30 nmol/L (n = 24) | Insufficient Levels: 30–50 nmol/L (n = 28) | Sufficient Levels: >50 nmol/L (n = 38) | p-Value |
|---|---|---|---|---|
| Age (years) | 33.42 ± 5.06 | 30.13 ± 4.80 | 29.21 ± 4.00 | 0.402 |
| Weight (kgs) | 76.62 ± 13.95 | 75.99 ± 13.32 | 77.39 ± 12.07 | 0.722 |
| BMI (kg/m2) | 30.64 ± 4.89 | 29.96 ± 4.89 | 31.05 ± 4.92 | 0.992 |
| SBP (mmHg) | 130.42 ± 12.07 | 129.18 ± 11.62 | 130.82 ± 12.38 | 0.940 |
| DBP (mmHg) | 82.79 ± 7.92 | 79.75 ± 7.61 | 81.89 ± 7.95 | 0.967 |
| FPG (mmol/L) | 5.30 ± 2.08 | 5.30 ± 0.71 | 5.87 ± 1.91 | 0.0001 |
| PPBG (mmol/L) | 6.70 ± 2.53 | 6.90 ± 2.80 | 10.81 ± 26.99 | <0.0001 |
| OGTT-1h (mmol/L) | 11.20 ± 0.91 | 11.50 ± 1.33 | 11.58 ± 1.73 | 0.005 |
| OGTT-2h (mmol/L) | 9.48 ± 1.36 | 9.81 ± 1.27 | 10.01 ±1.88 | 0.060 |
| HbA1c (%) | 5.58 ± 0.56 | 5.65 ± 0.49 | 5.55 ± 0.52 | 0.802 |
| TG (mmol/L) | 1.77 ± 1.16 | 2.13 ± 1.15 | 1.74 ± 0.93 | 0.385 |
| TC (mmol/L) | 5.70 ± 1.23 | 5.41 ± 0.97 | 5.17 ± 1.19 | 0.435 |
| HDLc (mmol/L) | 0.77 ± 0.43 | 0.70 ± 0.41 | 0.66 ± 0.27 | 0.022 |
| LDLc (mmol/L) | 4.09 ± 0.97 | 3.79 ± 0.50 | 3.70 ± 0.98 | 0.001 |
| ApaI AA Genotypes (n = 35) | ApaI AC Genotypes (n = 46) | ApaI CC Genotypes (n = 09) | p-Value | |
|---|---|---|---|---|
| Deficient levels (<30 nmol/L) | 24.0 ± 1.22 | 23.43 ± 3.41 | 24.0 ± 2.64 | 0.601 |
| Insufficient levels (30–50 nmol/L) | 39.01 ± 5.92 | 38.64 ± 4.48 | 37.67 ± 4.04 | 0.775 |
| Sufficient levels (>50 nmol/L) | 67.26 ± 11.51 | 71.93 ± 10.94 | 72.00 ± 17.43 | <0.0001 |
| BsmI AA Genotypes (n = 31) | BsmI AG Genotypes (n = 40) | BsmI GG Genotypes (n = 19) | ||
| Deficient levels (<30 nmol/L) | 23.55 ± 2.61 | 23.37 ± 3.29 | 24.00 ± 3.26 | 0.762 |
| Insufficient levels (30–50 nmol/L) | 38.22 ± 4.73 | 38.67 ± 4.87 | 42.25 ± 5.73 | 0.016 |
| Sufficient levels (>50 nmol/L) | 71.15 ± 11.83 | 68.94 ± 11.19 | 68.50 ± 13.43 | 0.667 |
| FokI CC Genotypes (n = 59) | FokI CT Genotypes (n = 25) | FokI TT Genotypes (n = 06) | ||
| Deficient levels (<30 nmol/L) | 23.35 ± 2.97 | 23.75 ± 3.10 | 25.00 ± 2.82 | 0.415 |
| Insufficient levels (30–50 nmol/L) | 39.56 ± 5.12 | 39.60 ± 4.19 | 32.00 ± 1.41 | 0.001 |
| Sufficient levels (>50 nmol/L) | 70.48 ± 11.92 | 67.57 ± 11.75 | 64.00 ± 8.48 | 0.309 |
| TaqI TT Genotypes (n = 43) | TaqI TC Genotypes (n = 36) | TaqI CC Genotypes (n = 11) | ||
| Deficient levels (<30 nmol/L) | 23.83 ± 2.75 | 23.00 ± 3.26 | 25.50 ± 2.12 | 0.045 |
| Insufficient levels (30–50 nmol/L) | 37.75 ± 4.31 | 38.63 ± 5.55 | 43.00 ± 3.46 | 0.152 |
| Sufficient levels (>50 nmol/L) | 71.52 ± 12.21 | 66.93 ± 11.46 | 70.50 ± 9.88 | 0.216 |
| Covariates | R-Value a | Adjusted R Square Value | Standardized β-Coefficient for rs79785232 | Standardized β-Coefficient for rs1544410 | Standardized β-Coefficient for rs2228570 | Standardized β-Coefficient for rs731236 | F | p-Value b |
|---|---|---|---|---|---|---|---|---|
| Age | 0.188 | −0.010 | 0.117 | −0.025 | 0.106 | −0.084 | 0.775 | 0.544 |
| Weight | 0.175 | −0.015 | −0.173 | 0.007 | 0.032 | 0.009 | 0.672 | 0.613 |
| BMI | 0.205 | −0.003 | −0.190 | −0.078 | 0.088 | −0.036 | 0.936 | 0.447 |
| SBP | 0.142 | −0.026 | 0.009 | −0.014 | −0.085 | 0.134 | 0.439 | 0.780 |
| DBP | 0.117 | −0.033 | 0.027 | 0.037 | −0.109 | 0.029 | 0.294 | 0.881 |
| FPG | 0.195 | −0.007 | 0.152 | −0.068 | −0.060 | −0.054 | 0.840 | 0.504 |
| PPBG | 0.154 | −0.022 | −0.121 | −0.022 | −0.036 | −0.089 | 0.520 | 0.722 |
| OGTT-1h | 0.400 | 0.120 | −0.158 | −0.103 | 0.372 | −0.066 | 4.041 | 0.005 |
| OGTT-2h | 0.234 | 0.010 | −0.076 | −0.110 | 0.196 | −0.058 | 1.230 | 0.304 |
| HbA1c | 0.198 | −0.006 | 0.094 | 0.181 | 0.024 | −0.070 | 0.871 | 0.485 |
| TC | 0.190 | −0.009 | 0.096 | 0.055 | −0.162 | −0.007 | 0.797 | 0.531 |
| TG | 0.187 | −0.010 | 0.142 | 0.034 | −0.128 | −0.020 | 0.770 | 0.548 |
| HDLc | 0.108 | −0.035 | −0.023 | 0.018 | 0.084 | 0.050 | 0.250 | 0.909 |
| LDLc | 0.281 | 0.036 | 0.112 | −0.049 | −0.242 | −0.068 | 1.825 | 0.131 |
| 25 hydroxyvitamin-D | 0.248 | 0.018 | −0.150 | −0.067 | −0.190 | 0.013 | 1.398 | 0.242 |
| ApaI (rs79785232) | BsmI (rs1544410) | FokI (rs2228570) | TaqI (rs731236) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AA (n = 35) | AC (n = 46) | CC (n = 09) | TT (n = 43) | TT (n = 43) | TT (n = 43) | TT (n = 43) | p-Value | CC (n = 59) | CT (n = 25) | TT (n=06) | p-Value | TT (n = 43) | TC (n = 36) | CC (n = 11) | p-Value | |
| Age | 31.94 ± 5.64 | 32.02 ± 5.39 | 35.56 ± 3.88 | 32.93 ± 5.51 | 32.93 ± 5.51 | 32.93 ± 5.51 | 32.93 ± 5.51 | 0.255 | 31.95 ± 5.17 | 32.96 ± 5.00 | 33.67 ± 9.31 | 0.095 | 32.93 ± 5.51 | 31.64 ± 5.34 | 32.36 ± 5.57 | 0.976 |
| Weight | 79.08 ± 12.96 | 75.94 ± 12.97 | 71.84 ± 11.04 | 77.33 ± 12.27 | 77.33 ± 12.27 | 77.33 ± 12.27 | 77.33 ± 12.27 | 0.139 | 76.20 ± 12.87 | 78.95 ± 13.29 | 73.04 ± 11.13 | 0.890 | 77.33 ± 12.27 | 74.71 ± 12.24 | 81.16 ± 16.56 | 0.401 |
| BMI | 31.56 ± 5.01 | 30.13 ± 4.76 | 29.28 ± 4.96 | 30.96 ± 4.46 | 30.96 ± 4.46 | 30.96 ± 4.46 | 30.96 ± 4.46 | 0.822 | 30.32 ± 4.73 | 31.16 ± 4.64 | 31.02 ± 7.48 | 0.273 | 30.96 ± 4.46 | 29.83 ± 4.65 | 31.75 ± 6.90 | 0.151 |
| SBP | 130.57 ± 12.64 | 129.76 ± 11.20 | 131.01 ± 14.20 | 128.44 ± 11.75 | 128.44 ± 11.75 | 128.44 ± 11.75 | 128.44 ± 11.75 | 0.941 | 130.92 ± 12.30 | 128.32 ± 11.21 | 131.01 ± 12.57 | 0.863 | 128.44 ± 11.75 | 132.03 ± 12.58 | 131.09 ± 10.55 | 0.782 |
| DBP | 82.09 ± 7.31 | 80.46 ± 8.05 | 84.22 ± 8.73 | 81.05 ± 7.90 | 81.05 ± 7.90 | 81.05 ± 7.90 | 81.05 ± 7.90 | 0.922 | 82.05 ± 8.01 | 80.52 ± 7.58 | 79.67 ± 7.94 | 0.952 | 81.05 ± 7.90 | 82.36 ± 7.77 | 80.18 ± 8.30 | 0.966 |
| FPG | 5.29 ± 0.89 | 5.58 ± 1.75 | 6.30 ± 3.22 | 5.63 ± 2.22 | 5.63 ± 2.22 | 5.63 ± 2.22 | 5.63 ± 2.22 | 0.030 | 5.64 ± 2.00 | 5.23 ± 0.67 | 5.83 ± 1.43 | 0.0001 | 5.63 ± 2.22 | 5.56 ± 0.97 | 5.12 ± 1.12 | 0.0002 |
| PPBG | 11.27 ± 28.10 | 6.77 ± 2.79 | 6.58 ± 1.79 | 10.38 ± 25.36 | 10.38 ± 25.36 | 10.38 ± 25.36 | 10.38 ± 25.36 | 0.0001 | 9.39 ± 21.70 | 6.73 ± 2.68 | 7.12 ± 2.29 | 0.0005 | 10.38 ± 25.36 | 6.65 ± 2.70 | 7.21 ± 3.16 | 0.00001 |
| OGTT-1h | 11.51 ± 1.18 | 11.53 ± 1.62 | 10.83 ± 1.19 | 11.40 ± 1.41 | 11.40 ± 1.41 | 11.40 ± 1.41 | 11.40 ± 1.41 | 0.068 | 11.11 ± 1.21 | 11.96 ± 1.34 | 12.72 ± 2.41 | 0.045 | 11.40 ± 1.41 | 11.56 ± 1.31 | 11.32 ± 1.90 | 0.296 |
| OGTT-2h | 9.84 ± 1.71 | 9.81 ± 1.62 | 9.63 ± 0.75 | 9.81 ± 1.61 | 9.81 ± 1.61 | 9.81 ± 1.61 | 9.81 ± 1.61 | 0.332 | 9.59 ± 1.51 | 10.18 ± 1.60 | 10.40 ± 1.99 | 0.664 | 9.81 ± 1.61 | 9.86 ± 1.60 | 9.62 ± 1.21 | 0.549 |
| HbA1c | 5.53 ± 0.54 | 5.63 ± 0.52 | 5.59 ± 0.47 | 5.61 ± 0.56 | 5.61 ± 0.56 | 5.61 ± 0.56 | 5.61 ± 0.56 | 0.797 | 5.58 ± 0.49 | 5.64 ± 0.61 | 5.47 ± 0.42 | 0.355 | 5.61 ± 0.56 | 5.58 ± 0.49 | 5.51 ± 0.47 | 0.641 |
| TG | 1.89 ± 1.11 | 1.74 ± 1.01 | 2.44 ± 1.14 | 1.88 ± 1.08 | 1.88 ± 1.08 | 1.88 ± 1.08 | 1.88 ± 1.08 | 0.455 | 1.98 ± 1.15 | 1.73 ± 0.96 | 1.36 ± 0.33 | 0.017 | 1.88 ± 1.08 | 1.91 ± 1.16 | 1.68 ± 0.70 | 0.204 |
| TC | 5.31 ± 0.90 | 5.33 ± 1.32 | 5.99 ± 0.93 | 5.36 ± 1.00 | 5.36 ± 1.00 | 5.36 ± 1.00 | 5.36 ± 1.00 | 0.839 | 5.49 ± 1.28 | 5.20 ± 0.80 | 5.13 ± 0.89 | 0.034 | 5.36 ± 1.00 | 5.55 ± 1.29 | 4.95 ± 1.15 | 0.296 |
| HDLc | 0.69 ± 0.40 | 0.74 ± 0.35 | 0.58 ± 0.23 | 0.68 ± 0.35 | 0.68 ± 0.35 | 0.68 ± 0.35 | 0.68 ± 0.35 | 0.366 | 0.69 ± 0.40 | 0.69 ± 0.28 | 0.88 ± 0.07 | 0.0005 | 0.68 ± 0.35 | 0.71 ± 0.31 | 0.77 ± 0.54 | 0.056 |
| LDLc | 3.81 ± 0.65 | 3.76 ± 0.98 | 4.29 ± 0.90 | 3.87 ± 0.79 | 3.87 ± 0.79 | 3.87 ± 0.79 | 3.87 ± 0.79 | 0.419 | 3.98 ± 0.95 | 3.59 ± 0.62 | 3.41 ± 0.47 | 0.022 | 3.87 ± 0.79 | 3.93 ± 0.88 | 3.38 ± 1.01 | 0.561 |
| Vitamin D | 52.49 ± 19.32 | 44.93 ± 22.03 | 44.56 ± 23.25 | 48.79 ± 22.75 | 48.79 ± 22.75 | 48.79 ± 22.75 | 48.79 ± 22.75 | 0.814 | 50.92 ± 22.09 | 42.36 ± 18.65 | 40.33 ± 19.03 | 0.611 | 48.79 ± 22.75 | 46.08 ± 20.50 | 49.82 ± 18.63 | 0.675 |
| S. No | rs79785232 | rs1544410 | rs2228570 | rs731236 | Freq | OR (95%CI) | p-Value |
|---|---|---|---|---|---|---|---|
| 1 | A | A | C | T | 0.2556 | 1.00 | - |
| 2 | A | G | C | T | 0.1799 | 1.59 (0.62–4.07) | 0.33 |
| 3 | C | A | C | T | 0.1534 | 1.51 (0.67–3.41) | 0.32 |
| 4 | A | A | T | C | 0.0674 | 0.97 (0.29–3.17) | 0.95 |
| 5 | A | G | C | C | 0.0612 | 5.30 (1.34–21.01) | 0.019 |
| 6 | A | A | C | C | 0.0558 | 1.81 (0.31–10.55) | 0.51 |
| 7 | C | G | C | T | 0.0529 | 3.62 (0.92–14.17) | 0.067 |
| 8 | A | A | T | T | 0.0441 | 0.59 (0.08–4.51) | 0.61 |
| 9 | C | A | C | C | 0.0341 | 3.30 (0.48–22.83) | 0.23 |
| 10 | C | A | T | T | 0.0294 | 6.91(0.78–32.19) | <0.0001 |
| 11 | C | G | T | C | 0.0145 | 12.1(3.67–46.9) | <0.0001 |
| 12 | A | G | T | T | 0.0114 | 5.38 (0.20–146.61) | 0.32 |
| 13 | A | G | T | C | 0.0107 | 2.86 (0.81–16.75) | <0.0001 |
| 14 | C | A | T | C | 0.0103 | 0.47 (0.29–2.17) | 0.86 |
| 15 | C | G | T | T | 0.0095 | 1.29 (0.62–3.07) | 0.32 |
| 16 | C | A | T | T | 0.0099 | 4.30 (0.88–29.83) | <0.0001 |
| Pregnant Women | L1 | L2 | D’ | r2 |
|---|---|---|---|---|
| GDM women | rs731236 | rs2228570 | 0.256 | 0.036 |
| GDM women | rs731236 | rs1544410 | 0.068 | 0.003 |
| GDM women | rs731236 | rs79785232 | 0.159 | 0.007 |
| GDM women | rs2228570 | rs1544410 | 0.231 | 0.011 |
| GDM women | rs2228570 | rs79785232 | 0.174 | 0.014 |
| GDM women | rs1544410 | rs79785232 | 0.221 | 0.021 |
| Non-GDM women | rs731236 | rs2228570 | 0.414 | 0.154 |
| Non-GDM women | rs731236 | rs1544410 | 0.509 | 0.024 |
| Non-GDM women | rs731236 | rs79785232 | 0.232 | 0.005 |
| Non-GDM women | rs2228570 | rs1544410 | 0.581 | 0.029 |
| Non-GDM women | rs2228570 | rs79785232 | 0.062 | 0.001 |
| Non-GDM women | rs1544410 | rs79785232 | 0.388 | 0.021 |
| Model No. | Best Combination of Genes | Training Accuracy | Testing Accuracy | CVC | p-Value | Total Sensitivity | Total Specificity | ꭓ2 | OR (95%CI) | F-Measure | Kappa |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | rs1544410 | 0.5965 | 0.5001 | 7/10 | 0.015 | 0.6629 | 0.5165 | 5.91 | 2.10 (1.15–3.83) | 0.614 | 0.179 |
| 2 | rs1544410, rs731236 | 0.6336 | 0.5544 | 7/10 | 0.002 | 0.4719 | 0.7912 | 13.90 | 3.38 (1.75–6.51) | 0.56 | 0.264 |
| 3 | rs1544410, rs2228570, rs731236 | 0.6658 | 0.5714 | 9/10 | <0.001 | 0.573 | 0.7473 | 19.06 | 3.96 (2.10–7.46) | 0.625 | 0.321 |
| 4 | rs79785232, rs1544410, rs2228570, rs731236 | 0.6881 | 0.5951 | 10/10 | <0.001 | 0.7416 | 0.6264 | 24.67 | 4.81 (2.54–9.09) | 0.698 | 0.367 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ali Khan, I.; Alhaizan, M.A.; Neyazi, S.M.; Al-Hakeem, M.M.; Alshammary, A.F. Relevance of Serum Levels and Functional Genetic Variants in Vitamin D Receptor Gene among Saudi Women with Gestational Diabetes Mellitus. Nutrients 2023, 15, 4288. https://doi.org/10.3390/nu15194288
Ali Khan I, Alhaizan MA, Neyazi SM, Al-Hakeem MM, Alshammary AF. Relevance of Serum Levels and Functional Genetic Variants in Vitamin D Receptor Gene among Saudi Women with Gestational Diabetes Mellitus. Nutrients. 2023; 15(19):4288. https://doi.org/10.3390/nu15194288
Chicago/Turabian StyleAli Khan, Imran, Maysoon Abdulhadi Alhaizan, Salwa Mohamed Neyazi, Malak Mohammed Al-Hakeem, and Amal F. Alshammary. 2023. "Relevance of Serum Levels and Functional Genetic Variants in Vitamin D Receptor Gene among Saudi Women with Gestational Diabetes Mellitus" Nutrients 15, no. 19: 4288. https://doi.org/10.3390/nu15194288
APA StyleAli Khan, I., Alhaizan, M. A., Neyazi, S. M., Al-Hakeem, M. M., & Alshammary, A. F. (2023). Relevance of Serum Levels and Functional Genetic Variants in Vitamin D Receptor Gene among Saudi Women with Gestational Diabetes Mellitus. Nutrients, 15(19), 4288. https://doi.org/10.3390/nu15194288






