Association of Maternal Pre-Pregnancy Overweight and Obesity with Childhood Anthropometric Factors and Perinatal and Postnatal Outcomes: A Cross-Sectional Study
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Study Design
2.3. Statistical Analysis
3. Results
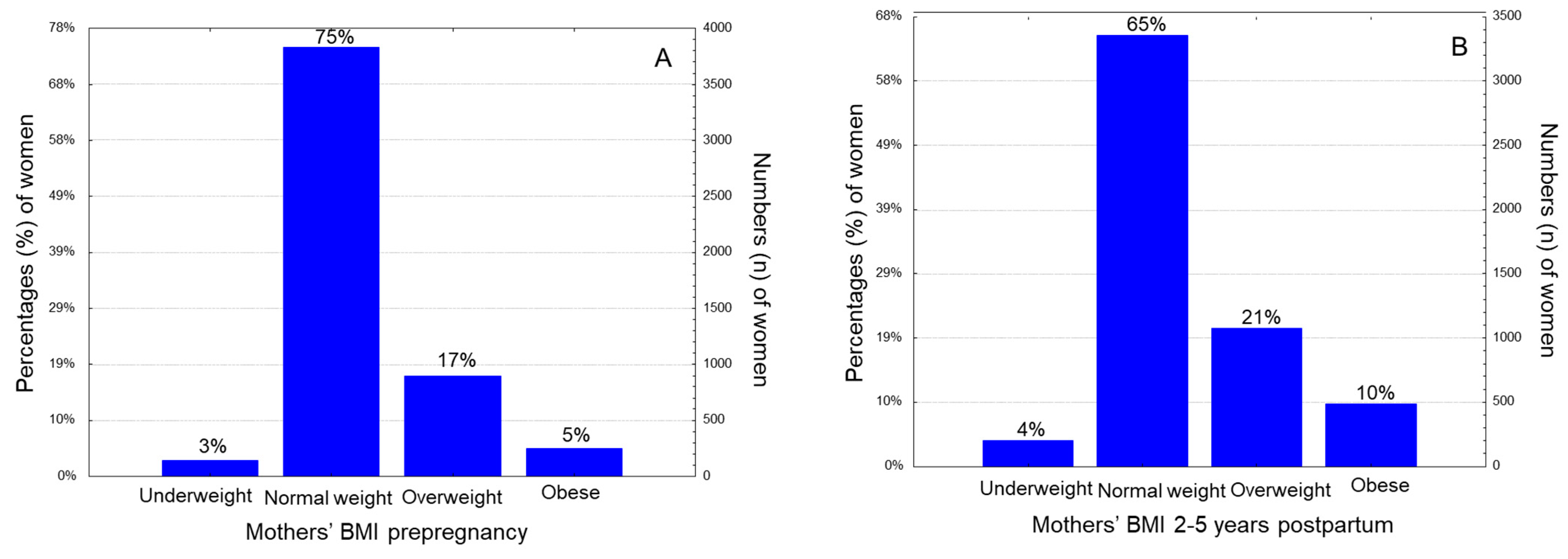
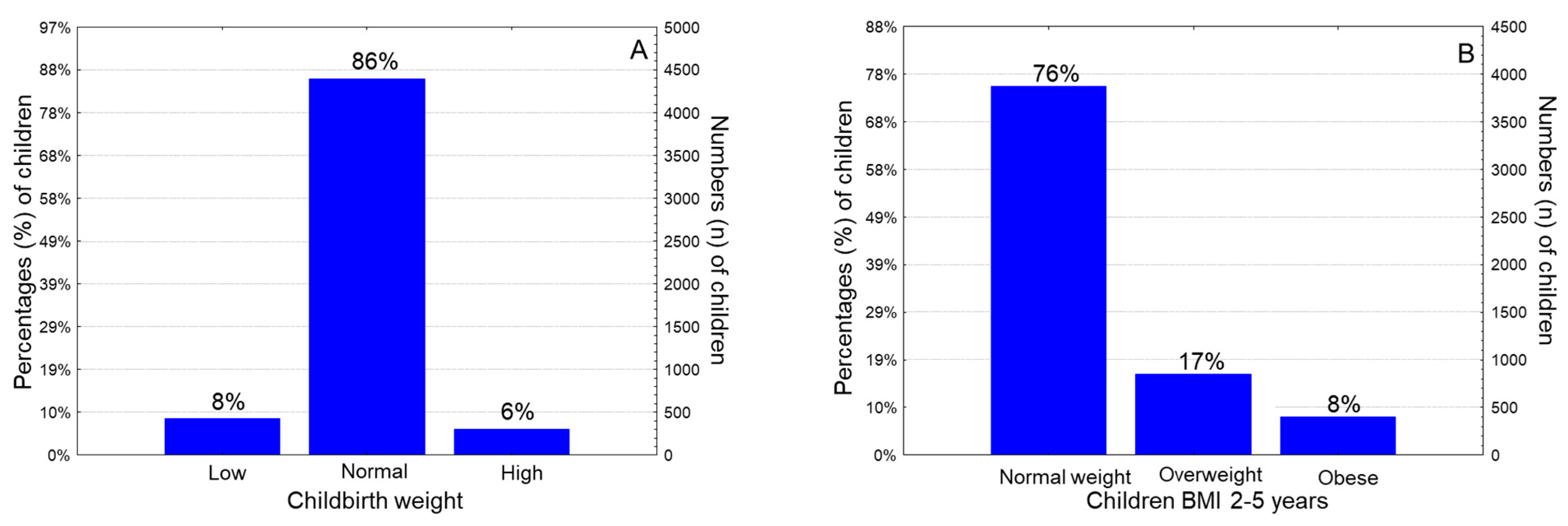
3.1. Anthropometry Data and Perinatal and Postnatal Outcomes of the Study Population
3.2. Maternal Pre-Pregnancy Excess Weight in Association with Antrhopometric and Demographic Characteristics of the Participant Children
3.3. Maternal BMI Status before Gestation in Relation with Childhood Perinatal and Postnatal Outcomes
3.4. Pre-Pregnancy BMI Status-Multivariate Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kim, S.Y.; Dietz, P.M.; England, L.; Morrow, B.; Callaghan, W.M. Trends in Pre-Pregnancy Obesity in Nine States, 1993–2003. Obesity 2007, 15, 986–993. [Google Scholar] [CrossRef]
- Stival, C.; Lugo, A.; Odone, A.; van den Brandt, P.A.; Fernandez, E.; Tigova, O.; Soriano, J.B.; López, M.J.; Scaglioni, S.; Gallus, S.; et al. Prevalence and Correlates of Overweight and Obesity in 12 European Countries in 2017–2018. Obes. Facts 2022, 15, 655–665. [Google Scholar] [CrossRef]
- Tambalis, K.D.; Panagiotakos, D.B.; Psarra, G.; Sidossis, L.S. Current Data in Greek Children Indicate Decreasing Trends of Obesity in the Transition from Childhood to Adolescence; Results from the National Action for Children’s Health (EYZHN) Program. J. Prev. Med. Hyg. 2018, 59, E36–E47. [Google Scholar] [CrossRef]
- Tambalis, K.D.; Panagiotakos, D.B.; Kavouras, S.A.; Kallistratos, A.A.; Moraiti, I.P.; Douvis, S.J.; Toutouzas, P.K.; Sidossis, L.S. Eleven-Year Prevalence Trends of Obesity in Greek Children: First Evidence That Prevalence of Obesity Is Leveling Off. Obesity 2010, 18, 161–166. [Google Scholar] [CrossRef]
- State of Inequality: Reproductive, Maternal, Newborn and Child Health. Available online: https://www.who.int/data/inequality-monitor/publications/report_2015_rmnch (accessed on 2 September 2022).
- Wei, Y.-M.; Yang, H.-X.; Zhu, W.-W.; Liu, X.-Y.; Meng, W.-Y.; Wang, Y.-Q.; Shang, L.-X.; Cai, Z.-Y.; Ji, L.-P.; Wang, Y.-F.; et al. Risk of Adverse Pregnancy Outcomes Stratified for Pre-Pregnancy Body Mass Index. J. Matern. Fetal Neonatal Med. 2016, 29, 2205–2209. [Google Scholar] [CrossRef]
- Faucett, A.M.; Metz, T.D.; DeWitt, P.E.; Gibbs, R.S. Effect of Obesity on Neonatal Outcomes in Pregnancies with Preterm Premature Rupture of Membranes. Am. J. Obstet. Gynecol. 2016, 214, 287.e1–287.e5. [Google Scholar] [CrossRef]
- Langley-Evans, S.C.; Pearce, J.; Ellis, S. Overweight, Obesity and Excessive Weight Gain in Pregnancy as Risk Factors for Adverse Pregnancy Outcomes: A Narrative Review. J. Hum. Nutr. Diet. 2022, 35, 250–264. [Google Scholar] [CrossRef]
- Mokdad, A.H.; Ford, E.S.; Bowman, B.A.; Dietz, W.H.; Vinicor, F.; Bales, V.S.; Marks, J.S. Prevalence of Obesity, Diabetes, and Obesity-Related Health Risk Factors, 2001. JAMA 2003, 289, 76–79. [Google Scholar] [CrossRef]
- Baeten, J.M.; Bukusi, E.A.; Lambe, M. Pregnancy Complications and Outcomes among Overweight and Obese Nulliparous Women. Am. J. Public. Health 2001, 91, 436–440. [Google Scholar] [CrossRef] [Green Version]
- Abenhaim, H.A.; Kinch, R.A.; Morin, L.; Benjamin, A.; Usher, R. Effect of Prepregnancy Body Mass Index Categories on Obstetrical and Neonatal Outcomes. Arch. Gynecol. Obstet. 2007, 275, 39–43. [Google Scholar] [CrossRef]
- Kalk, P.; Guthmann, F.; Krause, K.; Relle, K.; Godes, M.; Gossing, G.; Halle, H.; Wauer, R.; Hocher, B. Impact of Maternal Body Mass Index on Neonatal Outcome. Eur. J. Med. Res. 2009, 14, 216–222. [Google Scholar] [CrossRef] [Green Version]
- Briese, V.; Voigt, M.; Wisser, J.; Borchardt, U.; Straube, S. Risks of Pregnancy and Birth in Obese Primiparous Women: An Analysis of German Perinatal Statistics. Arch. Gynecol. Obstet. 2011, 283, 249–253. [Google Scholar] [CrossRef] [Green Version]
- Pedersen, J.; Bojsen-Møller, B.; Poulsen, H. Blood Sugar in Newborn Infants of Diabetic Mothers. Acta Endocrinol. 1954, 15, 33–52. [Google Scholar] [CrossRef]
- Ronnenberg, A.G.; Wang, X.; Xing, H.; Chen, C.; Chen, D.; Guang, W.; Guang, A.; Wang, L.; Ryan, L.; Xu, X. Low Preconception Body Mass Index Is Associated with Birth Outcome in a Prospective Cohort of Chinese Women. J. Nutr. 2003, 133, 3449–3455. [Google Scholar] [CrossRef] [Green Version]
- Heslehurst, N.; Simpson, H.; Ells, L.J.; Rankin, J.; Wilkinson, J.; Lang, R.; Brown, T.J.; Summerbell, C.D. The Impact of Maternal BMI Status on Pregnancy Outcomes with Immediate Short-Term Obstetric Resource Implications: A Meta-Analysis. Obes. Rev. 2008, 9, 635–683. [Google Scholar] [CrossRef] [Green Version]
- Choi, H.; Lim, J.-Y.; Lim, N.-K.; Ryu, H.M.; Kwak, D.W.; Chung, J.H.; Park, H.J.; Park, H.-Y. Impact of Pre-Pregnancy Body Mass Index and Gestational Weight Gain on the Risk of Maternal and Infant Pregnancy Complications in Korean Women. Int. J. Obes. 2022, 46, 59–67. [Google Scholar] [CrossRef]
- Papachatzi, E.; Dimitriou, G.; Dimitropoulos, K.; Vantarakis, A. Pre-Pregnancy Obesity: Maternal, Neonatal and Childhood Outcomes. J. Neonatal Perinatal Med. 2013, 6, 203–216. [Google Scholar] [CrossRef]
- Håberg, S.E.; Stigum, H.; London, S.J.; Nystad, W.; Nafstad, P. Maternal Obesity in Pregnancy and Respiratory Health in Early Childhood. Paediatr. Perinat. Epidemiol. 2009, 23, 352–362. [Google Scholar] [CrossRef] [Green Version]
- Gutierrez, M.J.; Nino, G.; Hong, X.; Wang, X. Maternal Pre-Pregnancy Weight and Early Life Lower Respiratory Tract Infections in a Low-Income Urban Minority Birth Cohort. Sci. Rep. 2021, 11, 9790. [Google Scholar] [CrossRef]
- Lindell, N.; Carlsson, A.; Josefsson, A.; Samuelsson, U. Maternal Obesity as a Risk Factor for Early Childhood Type 1 Diabetes: A Nationwide, Prospective, Population-Based Case-Control Study. Diabetologia 2018, 61, 130–137. [Google Scholar] [CrossRef] [Green Version]
- Moschonis, G.; Kaliora, A.C.; Karatzi, K.; Michaletos, A.; Lambrinou, C.-P.; Karachaliou, A.K.; Chrousos, G.P.; Lionis, C.; Manios, Y. Perinatal, Sociodemographic and Lifestyle Correlates of Increased Total and Visceral Fat Mass Levels in Schoolchildren in Greece: The Healthy Growth Study. Public Health Nutr. 2017, 20, 660–670. [Google Scholar] [CrossRef] [Green Version]
- Papandreou, D.; Mantzorou, M.; Tyrovolas, S.; Pavlidou, E.; Antasouras, G.; Psara, E.; Poulios, E.; Vasios, G.K.; Giaginis, C. Pre-Pregnancy Excess Weight Association with Maternal Sociodemographic, Anthropometric and Lifestyle Factors and Maternal Perinatal Outcomes. Nutrients 2022, 14, 3810. [Google Scholar] [CrossRef]
- Mantzorou, M.; Papandreou, D.; Vasios, G.K.; Pavlidou, E.; Antasouras, G.; Psara, E.; Taha, Z.; Poulios, E.; Giaginis, C. Exclusive Breastfeeding for at Least Four Months Is Associated with a Lower Prevalence of Overweight and Obesity in Mothers and Their Children after 2–5 Years from Delivery. Nutrients 2022, 14, 3599. [Google Scholar] [CrossRef]
- World Health Organization. Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee; WHO Technical Report Series; World Health Organization: Geneva, Switzerland, 1995; Volume 854.
- Papadopoulou, S.K.; Mentzelou, M.; Pavlidou, E.; Vasios, G.K.; Spanoudaki, M.; Antasouras, G.; Sampani, A.; Psara, E.; Voulgaridou, G.; Tsourouflis, G.; et al. Caesarean Section Delivery Is Associated with Childhood Overweight and Obesity, Low Childbirth Weight and Postnatal Complications: A Cross-Sectional Study. Medicina 2023, 59, 664. [Google Scholar] [CrossRef]
- Koutelidakis, A.E.; Alexatou, O.; Kousaiti, S.; Gkretsi, E.; Vasios, G.; Sampani, A.; Tolia, M.; Kiortsis, D.N.; Giaginis, C. Higher Adherence to Mediterranean Diet Prior to Pregnancy Is Associated with Decreased Risk for Deviation from the Maternal Recommended Gestational Weight Gain. Int. J. Food Sci. Nutr. 2018, 69, 84–92. [Google Scholar] [CrossRef]
- World Health Organization. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2006.
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a Standard Definition for Child Overweight and Obesity Worldwide: International Survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef] [Green Version]
- Rosa, M.J.; Hartman, T.J.; Adgent, M.; Gardner, K.; Gebretsadik, T.; Moore, P.E.; Davis, R.L.; LeWinn, K.Z.; Bush, N.R.; Tylavsky, F.; et al. Prenatal Polyunsaturated Fatty Acids and Child Asthma: Effect Modification by Maternal Asthma and Child Sex. J. Allergy Clin. Immunol. 2020, 145, 800–807.e4. [Google Scholar] [CrossRef]
- Olson, C.M.; Demment, M.M.; Carling, S.J.; Strawderman, M.S. Associations Between Mothers’ and Their Children’s Weights at 4 Years of Age. Child. Obes. 2010, 6, 201–207. [Google Scholar] [CrossRef]
- Williams, C.B.; Mackenzie, K.C.; Gahagan, S. The Effect of Maternal Obesity on the Offspring. Clin. Obstet. Gynecol. 2014, 57, 508–515. [Google Scholar] [CrossRef]
- Chen, F.; Wang, J.; Liao, Z.; Zong, X.; Zhang, T.; Xie, X.; Liu, G. Body Composition in Preschool Children and the Association with Prepregnancy Weight and Gestational Weight Gain: An Ambispective Cohort Study. Front. Nutr. 2022, 9, 881452. [Google Scholar] [CrossRef]
- Radaelli, T.; Lepercq, J.; Varastehpour, A.; Basu, S.; Catalano, P.M.; Hauguel-De Mouzon, S. Differential Regulation of Genes for Fetoplacental Lipid Pathways in Pregnancy with Gestational and Type 1 Diabetes Mellitus. Am. J. Obstet. Gynecol. 2009, 201, 209.e1–209.e10. [Google Scholar] [CrossRef] [Green Version]
- Catalano, P.M.; Farrell, K.; Thomas, A.; Huston-Presley, L.; Mencin, P.; de Mouzon, S.H.; Amini, S.B. Perinatal Risk Factors for Childhood Obesity and Metabolic Dysregulation. Am. J. Clin. Nutr. 2009, 90, 1303–1313. [Google Scholar] [CrossRef] [Green Version]
- Birbilis, M.; Moschonis, G.; Mougios, V.; Manios, Y. Obesity in Adolescence Is Associated with Perinatal Risk Factors, Parental BMI and Sociodemographic Characteristics. Eur. J. Clin. Nutr. 2013, 67, 115–121. [Google Scholar] [CrossRef] [Green Version]
- Chu, S.Y.; Kim, S.Y.; Schmid, C.H.; Dietz, P.M.; Callaghan, W.M.; Lau, J.; Curtis, K.M. Maternal Obesity and Risk of Cesarean Delivery: A Meta-Analysis. Obes. Rev. 2007, 8, 385–394. [Google Scholar] [CrossRef]
- Bebeau, K.A.; Edenfield, A.L.; Hill, A.; Van Buren, E.; Finneran, M.M.; Meglin, M.F. Impact of Pre-Pregnancy Obesity on Cesarean Delivery Rates in Nulliparous Pregnant People Undergoing Induction of Labor. J. Matern. Fetal Neonatal Med. 2022, 35, 9934–9939. [Google Scholar] [CrossRef]
- Azeredo, C.M.; Cortese, M.; Munger, K.L.; Ascherio, A. Maternal Prepregnancy BMI and Physical Activity and Type 1 Diabetes in the Offspring. Pediatr. Diabetes 2021, 22, 992–1002. [Google Scholar] [CrossRef]
- Shrestha, A.; Prowak, M.; Berlandi-Short, V.-M.; Garay, J.; Ramalingam, L. Maternal Obesity: A Focus on Maternal Interventions to Improve Health of Offspring. Front. Cardiovasc. Med. 2021, 8, 696812. [Google Scholar] [CrossRef]
- Babili, M.G.; Amerikanou, C.; Papada, E.; Christopoulos, G.; Tzavara, C.; Kaliora, A.C. The Effect of Prenatal Maternal Physical Activity and Lifestyle in Perinatal Outcome: Results from a Greek Study. Eur. J. Public Health 2020, 30, 328–332. [Google Scholar] [CrossRef]
- Iglesia Altaba, I.; Larqué, E.; Mesa, M.D.; Blanco-Carnero, J.E.; Gomez-Llorente, C.; Rodríguez-Martínez, G.; Moreno, L.A. Early Nutrition and Later Excess Adiposity during Childhood: A Narrative Review. Horm. Res. Paediatr. 2022, 95, 112–119. [Google Scholar] [CrossRef]
- López-Gil, J.F.; García-Hermoso, A.; Sotos-Prieto, M.; Cavero-Redondo, I.; Martínez-Vizcaíno, V.; Kales, S.N. Mediterranean Diet-Based Interventions to Improve Anthropometric and Obesity Indicators in Children and Adolescents: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2023, 14, 858–869. [Google Scholar] [CrossRef]
- Kim, J.; Lim, H. Nutritional Management in Childhood Obesity. J. Obes. Metab. Syndr. 2019, 28, 225–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naureen, Z.; Dhuli, K.; Donato, K.; Aquilanti, B.; Velluti, V.; Matera, G.; Iaconelli, A.; Bertelli, M. Foods of the Mediterranean diet: Tomato, olives, chili pepper, wheat flour and wheat germ. J. Prev. Med. Hyg. 2022, 63 (Suppl. S3), E4–E11. [Google Scholar] [CrossRef] [PubMed]
- Antonopoulou, M.; Mantzorou, M.; Serdari, A.; Bonotis, K.; Vasios, G.; Pavlidou, E.; Trifonos, C.; Vadikolias, K.; Petridis, D.; Giaginis, C. Evaluating Mediterranean diet adherence in university student populations: Does this dietary pattern affect students’ academic performance and mental health? Int. J. Health Plann. Manag. 2020, 35, 5–21. [Google Scholar] [CrossRef] [PubMed]
| Characteristics (n = 5198) | Pre-Pregnancy BMI Status * | ||
|---|---|---|---|
| Underweight and Normal Weight (69.4%) | Overweight and Obese (30.6%) | p-Value | |
| Maternal Age (years ± SD) | 33.1 ± 1.12 | 36.8 ± 1.21 | p = 0.0001 |
| Offspring Gender (n, %) | p = 0.0001 | ||
| Male | 2053 (50.9) | 510 (43.7) | |
| Female | 1979 (49.1) | 656 (56.3) | |
| Childhood BMI categories at the age of 2–5 years (n, %) | p < 0.0001 | ||
| Normal weight | 3103 (77.0) | 826 (70.8) | |
| Overweight | 675 (16.7) | 184 (15.8) | |
| Obese | 254 (6.3) | 153 (13.4) | |
| Birth weight (g) | 3107 ± 412 | 3269 ± 483 | p = 0.0172 |
| Birth weight status (n, %) | p = 0.0001 | ||
| Low newborn weight (<2500 g) | 341 (8.5) | 92 (7.9) | |
| Normal newborn weight (2500–4000 g) | 3480 (86.3) | 972 (83.4) | |
| High newborn weight (>4000 g) | 211 (5.2) | 102 (8.7) | |
| Birth height (cm) | 46.4 ± 2.9 | 46.5 ± 1.9 | p = 0.8457 |
| Birth head circumference (cm) | 36.0 ± 2.1 | 36.1 ± 1.6 | p = 0.5107 |
| Preterm childbirth (<37th week, n, %) | p < 0.0001 | ||
| No | 1920 (84.9) | 1701 (58.3) | |
| Yes | 342 (15.1) | 1219 (41.7) | |
| Newborn ponderal index (n, %) | p < 0.0001 | ||
| Low | 2327 (57.7) | 485 (41.6) | |
| High | 1805 (42.3) | 681 (58.4) | |
| Type of delivery (n, %) | p < 0.0001 | ||
| Vaginal | 1845 (45.8) | 426 (36.5) | |
| Caesarean section | 2187 (54.2) | 740 (63.5) | |
| Childhood asthma (n, %) | 0.5292 | ||
| No | 3845 (95.4) | 1117 (95.8) | |
| Yes | 187 (4.6) | 49 (4.2) | |
| Childhood diabetes type 1 (n, %) | p = 0.0009 | ||
| No | 3881 (96.3) | 1096 (94.0) | |
| Yes | 151 (3.7) | 70 (6.0) | |
| Characteristics | Pre-Pregnancy Overweight and Obesity | |
|---|---|---|
| OR * (95% CI **) | p-Value | |
| Maternal age (Under/Above mean value) | 1.62 (0.89–2.12) | p = 0.0884 |
| Childhood Gender (Boys/Girls) | 1.07 (0.32–1.88) | p = 0.3029 |
| Childhood BMI at the age of 2–5 years (Normal/Overweight or obese) | 2.11 (1.80–2.42) | p = 0.0001 |
| Childbirth weight status (Low & normal/High newborn weight) | 1.95 (1.61–2.53) | p = 0.0009 |
| Preterm childbirth (<37th week, No/Yes) | 1.34 (0.58–2.34) | p = 0.4378 |
| Newborn ponderal index (Low/High) | 1.47 (0.69–2.10) | p = 0.5745 |
| Type of delivery (Vaginal/Caesarean section) | 1.71 (1.33–2.19) | p = 0.0175 |
| Diabetes type 1 (No/Yes) | 1.27 (1.04–1.53) | p = 0.0014 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pavlidou, E.; Papandreou, D.; Taha, Z.; Mantzorou, M.; Tyrovolas, S.; Kiortsis, D.N.; Psara, E.; Papadopoulou, S.K.; Yfantis, M.; Spanoudaki, M.; et al. Association of Maternal Pre-Pregnancy Overweight and Obesity with Childhood Anthropometric Factors and Perinatal and Postnatal Outcomes: A Cross-Sectional Study. Nutrients 2023, 15, 3384. https://doi.org/10.3390/nu15153384
Pavlidou E, Papandreou D, Taha Z, Mantzorou M, Tyrovolas S, Kiortsis DN, Psara E, Papadopoulou SK, Yfantis M, Spanoudaki M, et al. Association of Maternal Pre-Pregnancy Overweight and Obesity with Childhood Anthropometric Factors and Perinatal and Postnatal Outcomes: A Cross-Sectional Study. Nutrients. 2023; 15(15):3384. https://doi.org/10.3390/nu15153384
Chicago/Turabian StylePavlidou, Eleni, Dimitrios Papandreou, Zainab Taha, Maria Mantzorou, Stefanos Tyrovolas, Dimitrios N. Kiortsis, Evmorfia Psara, Sousana K. Papadopoulou, Marios Yfantis, Maria Spanoudaki, and et al. 2023. "Association of Maternal Pre-Pregnancy Overweight and Obesity with Childhood Anthropometric Factors and Perinatal and Postnatal Outcomes: A Cross-Sectional Study" Nutrients 15, no. 15: 3384. https://doi.org/10.3390/nu15153384
APA StylePavlidou, E., Papandreou, D., Taha, Z., Mantzorou, M., Tyrovolas, S., Kiortsis, D. N., Psara, E., Papadopoulou, S. K., Yfantis, M., Spanoudaki, M., Antasouras, G., Mentzelou, M., & Giaginis, C. (2023). Association of Maternal Pre-Pregnancy Overweight and Obesity with Childhood Anthropometric Factors and Perinatal and Postnatal Outcomes: A Cross-Sectional Study. Nutrients, 15(15), 3384. https://doi.org/10.3390/nu15153384











