Early Pregnancy Maternal Plasma Phospholipid Saturated Fatty Acids and Fetal Growth: Findings from a Multi-Racial/Ethnic Birth Cohort in US
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Design
2.2. Assessments of Plasma Phospholipid Saturated Fatty Acids (SFAs)
2.3. Fetal Growth Measurement throughout Pregnancy (10–40 Weeks of Gestational Age)
2.4. Covariates
2.5. Statistical Analysis
3. Results
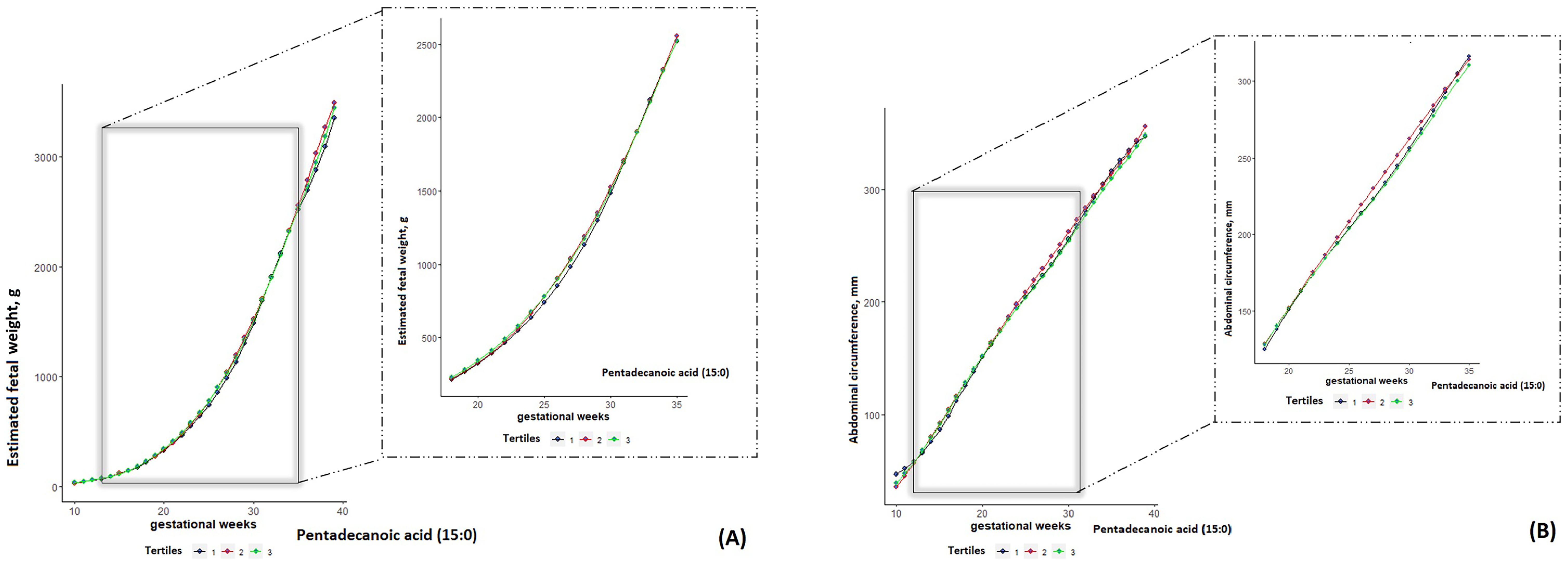
3.1. Even-Chain SFAs and Fetal Growth
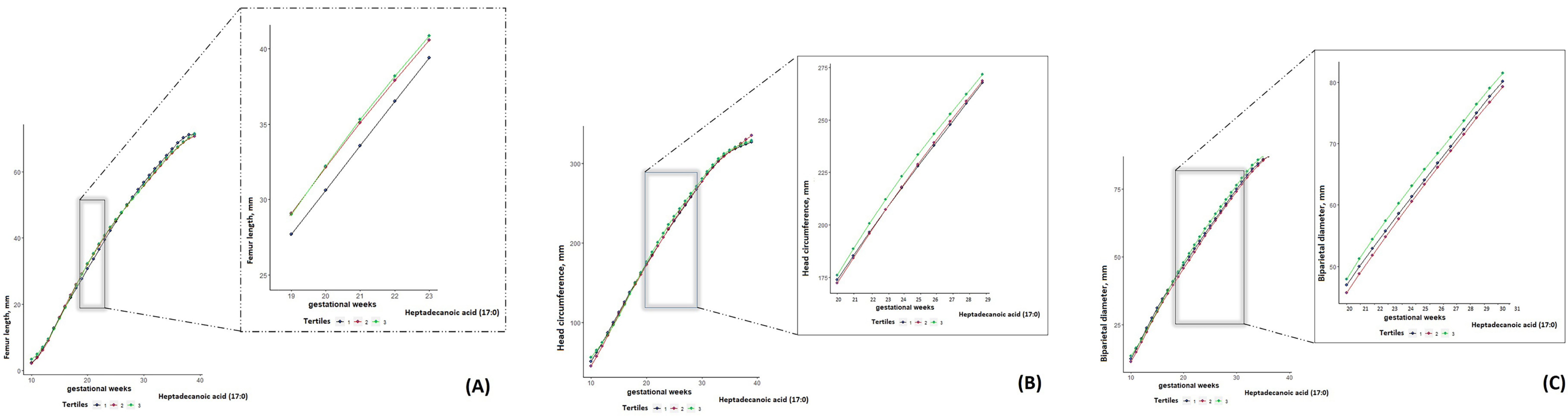
3.2. Odd-Chain SFAs and Fetal Growth
3.3. Very Long Even-Chain SFAs and Fetal Growth
4. Discussion
4.1. Clinical Implications
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mennitti, L.V.; Oliveira, J.L.; Morais, C.A.; Estadella, D.; Oyama, L.M.; Oller do Nascimento, C.M.; Pisani, L.P. Type of fatty acids in maternal diets during pregnancy and/or lactation and metabolic consequences of the offspring. J. Nutr. Biochem. 2015, 26, 99–111. [Google Scholar] [CrossRef]
- Bowman, C.E.; Arany, Z.; Wolfgang, M.J. Regulation of maternal–fetal metabolic communication. Cell. Mol. Life Sci. 2021, 78, 1455–1486. [Google Scholar] [CrossRef]
- Lewis, R.M.; Childs, C.E.; Calder, P.C. New perspectives on placental fatty acid transfer. Prostaglandins Leukot. Essent. Fat. Acids 2018, 138, 24–29. [Google Scholar] [CrossRef]
- Grootendorst-van Mil, N.H.; Tiemeier, H.; Steenweg-de Graaff, J.; Koletzko, B.; Demmelmair, H.; Jaddoe, V.W.V.; Steegers, E.A.P.; Steegers-Theunissen, R.P.M. Maternal plasma n-3 and n-6 polyunsaturated fatty acids during pregnancy and features of fetal health: Fetal growth velocity, birth weight and duration of pregnancy. Clin. Nutr. 2018, 37, 1367–1374. [Google Scholar] [CrossRef] [PubMed]
- Bernard, J.Y.; Tint, M.-T.; Aris, I.M.; Chen, L.-W.; Quah, P.L.; Tan, K.H.; Yeo, G.S.-H.; Fortier, M.V.; Yap, F.; Shek, L.; et al. Maternal plasma phosphatidylcholine polyunsaturated fatty acids during pregnancy and offspring growth and adiposity. Prostaglandins Leukot. Essent. Fat. Acids 2017, 121, 21–29. [Google Scholar] [CrossRef]
- Hamazaki, K.; Matsumura, K.; Tsuchida, A.; Kasamatsu, H.; Tanaka, T.; Ito, M.; Inadera, H.; Japan Environment and Children’s Study Group. Maternal dietary intake of fish and PUFAs and child neurodevelopment at 6 months and 1 year of age: A nationwide birth cohort-the Japan Environment and Children’s Study (JECS). Am. J. Clin. Nutr. 2020, 112, 1295–1303. [Google Scholar] [CrossRef]
- Li, L.-J.; Wu, J.; Chen, Z.; Weir, N.L.; Tsai, M.Y.; Albert, P.; Zhang, C. Plasma phospholipid polyunsaturated fatty acids composition in early pregnancy and fetal growth trajectories throughout pregnancy: Findings from the US fetal growth studies-singletons cohort. EBioMedicine 2022, 82, 104180. [Google Scholar] [CrossRef] [PubMed]
- Khaire, A.; Wadhwani, N.; Madiwale, S.; Joshi, S. Maternal fats and pregnancy complications: Implications for long-term health. Prostaglandins Leukot. Essent. Fat. Acids 2020, 157, 102098. [Google Scholar] [CrossRef]
- Gregorio, B.M.; Souza-Mello, V.; Mandarim-de-Lacerda, C.A.; Aguila, M.B. Maternal high-fat diet is associated with altered pancreatic remodelling in mice offspring. Eur. J. Nutr. 2013, 52, 759–769. [Google Scholar] [CrossRef] [PubMed]
- Strakovsky, R.S.; Zhang, X.; Zhou, D.; Pan, Y.X. Gestational high fat diet programs hepatic phosphoenolpyruvate carboxykinase gene expression and histone modification in neonatal offspring rats. J. Physiol. 2011, 589, 2707–2717. [Google Scholar] [CrossRef] [PubMed]
- Volpato, A.M.; Schultz, A.; Magalhães-Da-Costa, E.; Correia, M.L.D.G.; Águila, M.B.; Mandarim-De-Lacerda, C.A. Maternal high-fat diet programs for metabolic disturbances in offspring despite leptin sensitivity. Neuroendocrinology 2012, 96, 272–284. [Google Scholar] [CrossRef] [PubMed]
- Duque-Guimarães, D.E.; de Castro, J.; Martinez-Botas, J.; Sardinha, F.L.; Ramos, M.P.; Herrera, E.; do Carmo, M.d.G.T. Early and prolonged intake of partially hydrogenated fat alters the expression of genes in rat adipose tissue. Nutrition 2009, 25, 782–789. [Google Scholar] [CrossRef]
- Cinelli, G.; Fabrizi, M.; Ravà, L.; Signore, F.; Vernocchi, P.; Semeraro, M.; Vallone, C.; Lanciotti, R.; Ciofi degli Atti, M.; Manco, M. Association between Maternal and Foetal Erythrocyte Fatty Acid Profiles and Birth Weight. Nutrients 2018, 10, 402. [Google Scholar] [CrossRef]
- Meher, A.; Randhir, K.; Mehendale, S.; Wagh, G.; Joshi, S. Maternal Fatty Acids and Their Association with Birth Outcome: A Prospective Study. PLoS ONE 2016, 11, e0147359. [Google Scholar] [CrossRef] [PubMed]
- Kadakia, R.; Nodzenski, M.; Talbot, O.; Kuang, A.; Bain, J.R.; Muehlbauer, M.J.; Stevens, R.D.; Ilkayeva, O.R.; O’Neal, S.K.; Lowe, L.P.; et al. Maternal metabolites during pregnancy are associated with newborn outcomes and hyperinsulinaemia across ancestries. Diabetologia 2019, 62, 473–484. [Google Scholar] [CrossRef] [PubMed]
- Mani, I.; Dwarkanath, P.; Thomas, T.; Thomas, A.; Kurpad, A.V. Maternal fat and fatty acid intake and birth outcomes in a South Indian population. Int. J. Epidemiol. 2016, 45, 523–531. [Google Scholar] [CrossRef]
- Huang, L.; Lin, J.-S.; Aris, I.M.; Yang, G.; Chen, W.-Q.; Li, L.-J. Circulating Saturated Fatty Acids and Incident Type 2 Diabetes: A Systematic Review and Meta-Analysis. Nutrients 2019, 11, 998. [Google Scholar] [CrossRef]
- Ventura, A.K.; Loken, E.; Mitchell, D.C.; Smiciklas-Wright, H.; Birch, L.L. Understanding reporting bias in the dietary recall data of 11-year-old girls. Obesity 2006, 14, 1073–1084. [Google Scholar] [CrossRef]
- Carlsen, K.; Pedersen, L.; Bønnelykke, K.; Stark, K.D.; Lauritzen, L.; Bisgaard, H. Association between whole-blood polyunsaturated fatty acids in pregnant women and early fetal weight. Eur. J. Clin. Nutr. 2013, 67, 978–983. [Google Scholar] [CrossRef]
- Buck Louis, G.M.; Grewal, J.; Albert, P.S.; Sciscione, A.; Wing, D.A.; Grobman, W.A.; Newman, R.B.; Wapner, R.; D’Alton, M.E.; Skupski, D.; et al. Racial/ethnic standards for fetal growth: The NICHD Fetal Growth Studies. Am. J. Obstet. Gynecol. 2015, 213, 449.e1–449.e41. [Google Scholar] [CrossRef]
- Zhu, Y.; Li, M.; Rahman, M.L.; Hinkle, S.N.; Wu, J.; Weir, N.L.; Lin, Y.; Yang, H.; Tsai, M.Y.; Ferrara, A.; et al. Plasma phospholipid n-3 and n-6 polyunsaturated fatty acids in relation to cardiometabolic markers and gestational diabetes: A longitudinal study within the prospective NICHD Fetal Growth Studies. PLoS Med. 2019, 16, e1002910. [Google Scholar] [CrossRef]
- Zhu, Y.; Tsai, M.Y.; Sun, Q.; Hinkle, S.N.; Rawal, S.; Mendola, P.; Ferrara, A.; Albert, P.S.; Zhang, C. A prospective and longitudinal study of plasma phospholipid saturated fatty acid profile in relation to cardiometabolic biomarkers and the risk of gestational diabetes. Am. J. Clin. Nutr. 2018, 107, 1017–1026. [Google Scholar] [CrossRef] [PubMed]
- Muthayya, S.; Dwarkanath, P.; Thomas, T.; Ramprakash, S.; Mehra, R.; Mhaskar, A.; Mhaskar, R.; Thomas, A.; Bhat, S.; Vaz, M.; et al. The effect of fish and ω-3 LCPUFA intake on low birth weight in Indian pregnant women. Eur. J. Clin. Nutr. 2009, 63, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Hinkle, S.N.; Grantz, K.L.; Kim, S.; Grewal, J.; Grobman, W.A.; Skupski, D.W.; Newman, R.B.; Chien, E.K.; Sciscione, A.; et al. Glycaemic status during pregnancy and longitudinal measures of fetal growth in a multi-racial US population: A prospective cohort study. Lancet Diabetes Endocrinol. 2020, 8, 292–300. [Google Scholar] [CrossRef]
- Hadlock, F.P.; Harrist, R.B.; Sharman, R.S.; Deter, R.L.; Park, S.K. Estimation of fetal weight with the use of head, body, and femur measurements—A prospective study. Am. J. Obstet. Gynecol. 1985, 151, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Hediger, M.L.; Albert, P.S.; Grewal, J.; Sciscione, A.; Grobman, W.A.; Wing, D.A.; Newman, R.B.; Wapner, R.; D’Alton, M.E.; et al. Association of Maternal Obesity With Longitudinal Ultrasonographic Measures of Fetal Growth: Findings from the NICHD Fetal Growth Studies-Singletons. JAMA Pediatr. 2018, 172, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Samuelsen, S.O. A pseudolikelihood approach to analysis of nested case-control studies. Biometrika 1997, 84, 379–394. [Google Scholar] [CrossRef]
- Hinkle, S.N.; Rawal, S.; Liu, D.; Chen, J.; Tsai, M.Y.; Zhang, C. Maternal adipokines longitudinally measured across pregnancy and their associations with neonatal size, length, and adiposity. Int. J. Obes. 2019, 43, 1422–1434. [Google Scholar] [CrossRef]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Vickerstaff, V.; Omar, R.Z.; Ambler, G. Methods to adjust for multiple comparisons in the analysis and sample size calculation of randomised controlled trials with multiple primary outcomes. BMC Med. Res. Methodol. 2019, 19, 129. [Google Scholar] [CrossRef]
- DiNicolantonio, J.J.; O’Keefe, J.H. Good Fats versus Bad Fats: A Comparison of Fatty Acids in the Promotion of Insulin Resistance, Inflammation, and Obesity. MO Med. 2017, 114, 303–307. [Google Scholar] [PubMed]
- London, B.; Albert, C.; Anderson, M.E.; Giles, W.R.; Van Wagoner, D.R.; Balk, E.; Billman, G.E.; Chung, M.; Lands, W.; Leaf, A.; et al. Omega-3 fatty acids and cardiac arrhythmias: Prior studies and recommendations for future research: A report from the National Heart, Lung, and Blood Institute and Office Of Dietary Supplements Omega-3 Fatty Acids and their Role in Cardiac Arrhythmogenesis Workshop. Circulation 2007, 116, e320–e335. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Li, P.; Liu, H.; Prokosch, V. Oxidative Stress, Vascular Endothelium, and the Pathology of Neurodegeneration in Retina. Antioxidants 2022, 11, 543. [Google Scholar] [CrossRef] [PubMed]
- Hellerstein, M.K.; Schwarz, J.M.; Neese, R.A. Regulation of hepatic de novo lipogenesis in humans. Annu. Rev. Nutr. 1996, 16, 523–557. [Google Scholar] [CrossRef]
- Hudgins, L.C.; Hellerstein, M.; Seidman, C.; Neese, R.; Diakun, J.; Hirsch, J. Human fatty acid synthesis is stimulated by a eucaloric low fat, high carbohydrate diet. J. Clin. Investig. 1996, 97, 2081–2091. [Google Scholar] [CrossRef]
- Ishii, M.; Maeda, A.; Tani, S.; Akagawa, M. Palmitate induces insulin resistance in human HepG2 hepatocytes by enhancing ubiquitination and proteasomal degradation of key insulin signaling molecules. Arch. Biochem. Biophys. 2015, 566, 26–35. [Google Scholar] [CrossRef]
- Jin, J.; Zhang, X.; Lu, Z.; Perry, D.M.; Li, Y.; Russo, S.B.; Cowart, L.A.; Hannun, Y.A.; Huang, Y. Acid sphingomyelinase plays a key role in palmitic acid-amplified inflammatory signaling triggered by lipopolysaccharide at low concentrations in macrophages. Am. J. Physiol.-Endocrinol. Metab. 2013, 305, E853–E867. [Google Scholar] [CrossRef]
- Hu, F.B.; Willett, W.C. Optimal diets for prevention of coronary heart disease. JAMA 2002, 288, 2569–2578. [Google Scholar] [CrossRef]
- Herrera, E. Implications of dietary fatty acids during pregnancy on placental, fetal and postnatal development—A review. Placenta 2002, 23 (Suppl. SA), S9–S19. [Google Scholar] [CrossRef]
- Herrera, E.; Amusquivar, E.; López-Soldado, I.; Ortega, H. Maternal lipid metabolism and placental lipid transfer. Horm. Res. 2006, 65 (Suppl. S3), 59–64. [Google Scholar] [CrossRef]
- Hanebutt, F.L.; Demmelmair, H.; Schiessl, B.; Larqué, E.; Koletzko, B. Long-chain polyunsaturated fatty acid (LC-PUFA) transfer across the placenta. Clin. Nutr. 2008, 27, 685–693. [Google Scholar] [CrossRef] [PubMed]
- Brevik, A.; Veierod, M.B.; Drevon, C.A.; Andersen, L.F. Evaluation of the odd fatty acids 15:0 and 17:0 in serum and adipose tissue as markers of intake of milk and dairy fat. Eur. J. Clin. Nutr. 2005, 59, 1417–1422. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, B.J.; Seyssel, K.; Chiu, S.; Pan, P.-H.; Lin, S.-Y.; Stanley, E.; Ament, Z.; West, J.A.; Summerhill, K.; Griffin, J.L.; et al. Odd Chain Fatty Acids; New Insights of the Relationship Between the Gut Microbiota, Dietary Intake, Biosynthesis and Glucose Intolerance. Sci. Rep. 2017, 7, 44845. [Google Scholar] [CrossRef]
- Jenkins, B.; Aoun, M.; Feillet-Coudray, C.; Coudray, C.; Ronis, M.; Koulman, A. The Dietary Total-Fat Content Affects the In Vivo Circulating C15:0 and C17:0 Fatty Acid Levels Independently. Nutrients 2018, 10, 1646. [Google Scholar] [CrossRef]
- Jenkins, B.; West, J.A.; Koulman, A. A review of odd-chain fatty acid metabolism and the role of pentadecanoic Acid (c15:0) and heptadecanoic Acid (c17:0) in health and disease. Molecules 2015, 20, 2425–2444. [Google Scholar] [CrossRef]
- Yakoob, M.Y.; Shi, P.; Hu, F.B.; Campos, H.; Rexrode, K.M.; Orav, E.J.; Willett, W.C.; Mozaffarian, D. Circulating biomarkers of dairy fat and risk of incident stroke in U.S. men and women in 2 large prospective cohorts. Am. J. Clin. Nutr. 2014, 100, 1437–1447. [Google Scholar] [CrossRef] [PubMed]
- Khaw, K.-T.; Friesen, M.D.; Riboli, E.; Luben, R.; Wareham, N. Plasma phospholipid fatty acid concentration and incident coronary heart disease in men and women: The EPIC-Norfolk prospective study. PLoS Med. 2012, 9, e1001255. [Google Scholar] [CrossRef]
- Forouhi, N.G.; Koulman, A.; Sharp, S.J.; Imamura, F.; Kröger, J.; Schulze, M.B.; Crowe, F.L.; Huerta, J.M.; Guevara, M.; Beulens, J.W.; et al. Differences in the prospective association between individual plasma phospholipid saturated fatty acids and incident type 2 diabetes: The EPIC-InterAct case-cohort study. Lancet Diabetes Endocrinol. 2014, 2, 810–818. [Google Scholar] [CrossRef]
- Santaren, I.D.; Watkins, S.M.; Liese, A.D.; Wagenknecht, L.E.; Rewers, M.J.; Haffner, S.M.; Lorenzo, C.; Festa, A.; Bazinet, R.P.; Hanley, A.J. Individual serum saturated fatty acids and markers of chronic subclinical inflammation: The Insulin Resistance Atherosclerosis Study. J. Lipid Res. 2017, 58, 2171–2179. [Google Scholar] [CrossRef]
- Zheng, J.S.; Sharp, S.J.; Imamura, F.; Koulman, A.; Schulze, M.B.; Ye, Z.; Griffin, J.; Guevara, M.; Huerta, J.M.; Kröger, J.; et al. Association between plasma phospholipid saturated fatty acids and metabolic markers of lipid, hepatic, inflammation and glycaemic pathways in eight European countries: A cross-sectional analysis in the EPIC-InterAct study. BMC Med. 2017, 15, 203. [Google Scholar] [CrossRef]
- Lemaitre, R.N.; King, I.B. Very long-chain saturated fatty acids and diabetes and cardiovascular disease. Curr. Opin. Lipidol. 2022, 33, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Kihara, A. Very long-chain fatty acids: Elongation, physiology and related disorders. J. Biochem. 2012, 152, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.Y.; Klein, R.; Sharrett, A.R.; Schmidt, M.I.; Pankow, J.S.; Couper, D.J.; Klein, B.E.K.; Hubbard, L.D.; Duncan, B.B.; ARIC Investigators. Retinal arteriolar narrowing and risk of diabetes mellitus in middle-aged persons. JAMA 2002, 287, 2528–2533. [Google Scholar] [CrossRef]
- King, I.B.; Lemaitre, R.N.; Kestin, M. Effect of a low-fat diet on fatty acid composition in red cells, plasma phospholipids, and cholesterol esters: Investigation of a biomarker of total fat intake. Am. J. Clin. Nutr. 2006, 83, 227–236. [Google Scholar] [CrossRef]
- Borkman, M.; Storlien, L.H.; Pan, D.A.; Jenkins, A.B.; Chisholm, D.J.; Campbell, L.V. The relation between insulin sensitivity and the fatty-acid composition of skeletal-muscle phospholipids. N. Engl. J. Med. 1993, 328, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Rifas-Shiman, S.L.; Fleisch, A.; Hivert, M.-F.; Mantzoros, C.; Gillman, M.W.; Oken, E. First and second trimester gestational weight gains are most strongly associated with cord blood levels of hormones at delivery important for glycemic control and somatic growth. Metabolism 2017, 69, 112–119. [Google Scholar] [CrossRef]
- Malhotra, A.; Allison, B.J.; Castillo-Melendez, M.; Jenkin, G.; Polglase, G.R.; Miller, S.L. Neonatal Morbidities of Fetal Growth Restriction: Pathophysiology and Impact. Front. Endocrinol. 2019, 10, 55. [Google Scholar] [CrossRef]
| Saturated Fatty Acids | EFW | AC | FL | HC | BPD |
|---|---|---|---|---|---|
| Myristic acid (14:0) | ↓ | ↓ | ↓ | ↓ | ↓ |
| Pentadecanoic acid (15:0) | ↑ | ↑ | ↑ | ↑ | ↑ |
| Palmitic acid (16:0) | n.s. | ↓ | n.s. | n.s. | n.s. |
| Heptadecanoic acid (17:0) | ↑ | ↑ | ↑ | ↑ | ↑ |
| Stearic acid (18:0) | ↓ | ↓ | ↓ | ↓ | ↓ |
| Arachidic acid (20:0) | n.s. | n.s. | ↓ | ↓ | ↓ |
| Behenic acid (22:0) | ↓ | ↓ | n.s. | ↓ | ↓ |
| Lignoceric acid (24:0) | ↓ | ↓ | ↓ | ↓ | ↓ |
| Sum of even-chain SFAs (14:0 + 16:0 + 18:0) | ↓ | ↓ | ↓ | ↓ | ↓ |
| Sum of odd-chain SFAs (15:0 + 17:0) | ↑ | n.s. | ↑ | ↑ | ↑ |
| Sum of very long even-chain SFAs (20:0 + 22:0 + 24:0) | ↓ | ↓ | n.s. | ↓ | ↓ |
| GW | Estimated Fetal Weight (EFW), g | Abdominal Circumference (AC), mm | Femur Length (FL), mm | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Back-Transformed Geometric Mean g | Wald Test for Pairwise Comparison p-Value | Back-Transformed Geometric Mean mm | Wald Test for Pairwise Comparison p-Value | Back-Transformed Geometric Mean mm | Wald Test for Pairwise Comparison p-Value | ||||||||||
| 1st Tertile | 2nd Tertile | 3rd Tertile | 2nd vs. 1st Tertile | 3rd vs. 1st Tertile | 1st Tertile | 2nd Tertile | 3rd Tertile | 2nd vs. 1st Tertile | 3rd vs. 1st Tertile | 1st Tertile | 2nd Tertile | 3rd Tertile | 2nd vs. 1st Tertile | 3rd vs. 1st Tertile | |
| 10 | 35.13 | 36.03 | 40.58 | 0.715 | 0.061 | 36.05 | 39.4 | 41.87 | 0.059 | 0.004 | 2.01 | 2.42 | 2.47 | 0.002 | <0.001 |
| 11 | 43.92 | 44.69 | 47.72 | 0.628 | 0.049 | 46.55 | 47.87 | 49.18 | 0.258 | 0.050 | 3.76 | 4.26 | 4.17 | <0.001 | 0.004 |
| 12 | 55.41 | 56.03 | 57.51 | 0.552 | 0.071 | 58.04 | 57.34 | 57.49 | 0.328 | 0.482 | 6.26 | 6.78 | 6.47 | <0.0001 | 0.199 |
| 13 | 70.34 | 70.77 | 70.67 | 0.724 | 0.749 | 70.16 | 67.74 | 66.81 | <0.001 | <0.0001 | 9.41 | 9.84 | 9.31 | 0.017 | 0.661 |
| 14 | 89.54 | 89.74 | 88.09 | 0.913 | 0.348 | 82.55 | 78.95 | 77.12 | 0.0001 | <0.0001 | 12.93 | 13.20 | 12.55 | 0.313 | 0.199 |
| 15 | 113.93 | 113.85 | 110.79 | 0.970 | 0.142 | 94.88 | 90.82 | 88.35 | <0.001 | <0.0001 | 16.54 | 16.61 | 15.99 | 0.819 | 0.158 |
| 16 | 144.43 | 144.03 | 139.87 | 0.880 | 0.082 | 106.94 | 103.17 | 100.36 | <0.001 | <0.0001 | 19.97 | 19.87 | 19.45 | 0.801 | 0.260 |
| 17 | 181.81 | 181.07 | 176.34 | 0.815 | 0.074 | 118.65 | 115.76 | 112.95 | 0.016 | <0.0001 | 23.12 | 22.89 | 22.8 | 0.591 | 0.539 |
| 18 | 226.55 | 225.46 | 220.87 | 0.788 | 0.121 | 130.09 | 128.38 | 125.84 | 0.203 | <0.001 | 26.06 | 25.75 | 26.00 | 0.509 | 0.918 |
| 19 | 278.72 | 277.29 | 273.47 | 0.783 | 0.249 | 141.4 | 140.77 | 138.69 | 0.676 | 0.049 | 28.99 | 28.60 | 29.12 | 0.472 | 0.825 |
| 20 | 338.68 | 336.91 | 334.13 | 0.780 | 0.415 | 152.59 | 152.79 | 151.26 | 0.901 | 0.369 | 31.91 | 31.46 | 32.19 | 0.448 | 0.677 |
| 21 | 406.89 | 404.73 | 403.28 | 0.771 | 0.587 | 163.59 | 164.35 | 163.45 | 0.651 | 0.927 | 34.79 | 34.29 | 35.16 | 0.428 | 0.609 |
| 22 | 483.83 | 481.12 | 481.37 | 0.750 | 0.751 | 174.39 | 175.38 | 175.19 | 0.554 | 0.605 | 37.59 | 37.07 | 38.01 | 0.415 | 0.598 |
| 23 | 570.04 | 566.42 | 568.87 | 0.713 | 0.897 | 185.00 | 185.91 | 186.47 | 0.595 | 0.354 | 40.30 | 39.75 | 40.71 | 0.415 | 0.630 |
| 24 | 666.15 | 660.99 | 666.34 | 0.660 | 0.986 | 195.46 | 195.98 | 197.32 | 0.775 | 0.267 | 42.90 | 42.33 | 43.25 | 0.433 | 0.688 |
| 25 | 772.94 | 765.21 | 774.49 | 0.586 | 0.905 | 205.83 | 205.68 | 207.83 | 0.942 | 0.275 | 45.36 | 44.79 | 45.66 | 0.462 | 0.756 |
| 26 | 891.44 | 879.55 | 894.24 | 0.485 | 0.857 | 216.21 | 215.17 | 218.11 | 0.634 | 0.343 | 47.70 | 47.13 | 47.94 | 0.491 | 0.814 |
| 27 | 1022.98 | 1004.62 | 1026.83 | 0.354 | 0.833 | 226.74 | 224.64 | 228.36 | 0.362 | 0.448 | 49.92 | 49.33 | 50.13 | 0.505 | 0.841 |
| 28 | 1169.33 | 1141.22 | 1173.91 | 0.203 | 0.826 | 237.57 | 234.31 | 238.79 | 0.153 | 0.574 | 52.02 | 51.41 | 52.28 | 0.496 | 0.818 |
| 29 | 1332.26 | 1290.44 | 1337.56 | 0.082 | 0.818 | 248.84 | 244.36 | 249.65 | 0.040 | 0.699 | 54.04 | 53.39 | 54.43 | 0.463 | 0.730 |
| 30 | 1511.69 | 1453.76 | 1518.15 | 0.032 | 0.802 | 260.44 | 254.82 | 260.96 | 0.010 | 0.797 | 55.98 | 55.28 | 56.61 | 0.439 | 0.600 |
| 31 | 1706.19 | 1633.15 | 1713.46 | 0.023 | 0.808 | 272.16 | 265.72 | 272.52 | 0.007 | 0.869 | 57.86 | 57.14 | 58.75 | 0.453 | 0.481 |
| 32 | 1913.17 | 1831.17 | 1919.6 | 0.032 | 0.857 | 283.76 | 277.07 | 284.05 | 0.014 | 0.909 | 59.71 | 59.01 | 60.82 | 0.503 | 0.408 |
| 33 | 2128.69 | 2051.11 | 2130.77 | 0.077 | 0.960 | 294.98 | 288.87 | 295.25 | 0.038 | 0.922 | 61.55 | 60.94 | 62.75 | 0.581 | 0.395 |
| 34 | 2347.34 | 2297.17 | 2339.22 | 0.292 | 0.858 | 305.51 | 301.17 | 305.78 | 0.130 | 0.921 | 63.42 | 62.99 | 64.49 | 0.704 | 0.465 |
| 35 | 2563.79 | 2567.88 | 2536.39 | 0.938 | 0.575 | 315.13 | 313.79 | 315.28 | 0.639 | 0.955 | 65.31 | 65.21 | 65.98 | 0.929 | 0.663 |
| 36 | 2778.72 | 2841.97 | 2724.29 | 0.315 | 0.329 | 324.18 | 325.9 | 323.93 | 0.614 | 0.936 | 67.13 | 67.43 | 67.22 | 0.804 | 0.956 |
| 37 | 2995.99 | 3086.12 | 2914.31 | 0.221 | 0.210 | 333.14 | 336.32 | 332.4 | 0.424 | 0.834 | 68.72 | 69.39 | 68.30 | 0.626 | 0.803 |
| 38 | 3221.46 | 3258.69 | 3121.99 | 0.633 | 0.163 | 342.6 | 343.79 | 341.43 | 0.761 | 0.746 | 69.93 | 70.81 | 69.33 | 0.528 | 0.732 |
| 39 | 3463.07 | 3315.86 | 3367.49 | 0.126 | 0.229 | 353.19 | 346.99 | 351.89 | 0.202 | 0.741 | 70.59 | 71.37 | 70.42 | 0.631 | 0.925 |
| 40 | 3731.17 | 3222.27 | 3677.29 | 0.005 | 0.685 | 365.62 | 344.71 | 364.73 | 0.053 | 0.914 | 70.56 | 70.82 | 71.69 | 0.933 | 0.614 |
| GW | Head Circumference (HC), mm | Biparietal Diameter (BPD), mm | HC/AC Ratio | ||||||||||||
| Back-Transformed Geometric Mean mm | Wald Test for Pairwise Comparison p-Value | Back-Transformed Geometric Mean mm | Wald Test for Pairwise Comparison p-Value | Back-Transformed Geometric Mean | Wald Test for Pairwise Comparison p-Value | ||||||||||
| 1st Tertile | 2nd Tertile | 3rd Tertile | 2nd vs. 1st Tertile | 3rd vs. 1st Tertile | 1st Tertile | 2nd Tertile | 3rd Tertile | 2nd vs. 1st Tertile | 3rd vs. 1st Tertile | 1st Tertile | 2nd Tertile | 3rd Tertile | 2nd vs. 1st Tertile | 3rd vs. 1st Tertile | |
| 10 | 46.38 | 51.84 | 49.12 | <0.001 | 0.141 | 11.36 | 12.86 | 12.24 | <0.001 | 0.111 | 1.27 | 1.31 | 1.18 | 0.338 | 0.041 |
| 11 | 58.7 | 62.51 | 59.75 | 0.0001 | 0.402 | 15.21 | 16.13 | 15.42 | 0.003 | 0.580 | 1.26 | 1.31 | 1.22 | 0.066 | 0.080 |
| 12 | 71.87 | 73.99 | 71.25 | <0.001 | 0.394 | 19.35 | 19.64 | 18.86 | 0.131 | 0.036 | 1.25 | 1.29 | 1.24 | <0.001 | 0.427 |
| 13 | 85.46 | 86.10 | 83.40 | 0.303 | <0.001 | 23.55 | 23.29 | 22.43 | 0.174 | <0.0001 | 1.24 | 1.27 | 1.25 | <0.0001 | 0.119 |
| 14 | 99.05 | 98.64 | 96.02 | 0.613 | <0.001 | 27.61 | 26.99 | 26.06 | 0.014 | <0.0001 | 1.22 | 1.25 | 1.24 | 0.004 | 0.011 |
| 15 | 112.36 | 111.42 | 108.90 | 0.319 | <0.001 | 31.39 | 30.64 | 29.66 | 0.011 | <0.0001 | 1.21 | 1.23 | 1.23 | 0.034 | 0.009 |
| 16 | 125.19 | 124.26 | 121.87 | 0.338 | 0.003 | 34.84 | 34.20 | 33.17 | 0.037 | <0.0001 | 1.19 | 1.21 | 1.21 | 0.130 | 0.017 |
| 17 | 137.56 | 137.04 | 134.81 | 0.604 | 0.014 | 38.00 | 37.65 | 36.57 | 0.263 | <0.0001 | 1.18 | 1.18 | 1.19 | 0.419 | 0.069 |
| 18 | 149.62 | 149.66 | 147.64 | 0.975 | 0.090 | 41.00 | 40.98 | 39.88 | 0.961 | 0.002 | 1.17 | 1.17 | 1.17 | 0.929 | 0.369 |
| 19 | 161.63 | 162.06 | 160.34 | 0.727 | 0.311 | 44.01 | 44.24 | 43.14 | 0.551 | 0.027 | 1.16 | 1.15 | 1.16 | 0.634 | 0.988 |
| 20 | 173.56 | 174.16 | 172.87 | 0.651 | 0.612 | 47.06 | 47.42 | 46.37 | 0.385 | 0.096 | 1.15 | 1.14 | 1.14 | 0.357 | 0.463 |
| 21 | 185.33 | 185.88 | 185.12 | 0.689 | 0.881 | 50.13 | 50.50 | 49.54 | 0.380 | 0.170 | 1.14 | 1.13 | 1.13 | 0.197 | 0.190 |
| 22 | 196.89 | 197.18 | 197.03 | 0.830 | 0.921 | 53.20 | 53.47 | 52.65 | 0.514 | 0.206 | 1.14 | 1.12 | 1.12 | 0.118 | 0.079 |
| 23 | 208.16 | 208.05 | 208.54 | 0.940 | 0.799 | 56.24 | 56.34 | 55.68 | 0.819 | 0.203 | 1.13 | 1.12 | 1.12 | 0.096 | 0.042 |
| 24 | 219.11 | 218.50 | 219.62 | 0.693 | 0.743 | 59.24 | 59.11 | 58.62 | 0.777 | 0.184 | 1.13 | 1.12 | 1.11 | 0.127 | 0.039 |
| 25 | 229.7 | 228.59 | 230.28 | 0.507 | 0.733 | 62.18 | 61.82 | 61.48 | 0.465 | 0.169 | 1.12 | 1.11 | 1.11 | 0.236 | 0.058 |
| 26 | 239.92 | 238.4 | 240.53 | 0.401 | 0.741 | 65.02 | 64.48 | 64.26 | 0.304 | 0.165 | 1.12 | 1.11 | 1.10 | 0.470 | 0.108 |
| 27 | 249.78 | 248.03 | 250.44 | 0.360 | 0.738 | 67.77 | 67.13 | 66.97 | 0.250 | 0.173 | 1.11 | 1.11 | 1.10 | 0.879 | 0.200 |
| 28 | 259.29 | 257.63 | 260.06 | 0.385 | 0.701 | 70.39 | 69.81 | 69.64 | 0.292 | 0.201 | 1.10 | 1.10 | 1.09 | 0.548 | 0.353 |
| 29 | 268.47 | 267.25 | 269.49 | 0.509 | 0.604 | 72.87 | 72.54 | 72.26 | 0.525 | 0.284 | 1.08 | 1.09 | 1.08 | 0.100 | 0.589 |
| 30 | 277.28 | 276.73 | 278.69 | 0.770 | 0.467 | 75.22 | 75.27 | 74.85 | 0.916 | 0.504 | 1.07 | 1.09 | 1.07 | 0.006 | 0.912 |
| 31 | 285.67 | 285.91 | 287.51 | 0.909 | 0.369 | 77.45 | 77.95 | 77.36 | 0.372 | 0.876 | 1.05 | 1.08 | 1.05 | <0.001 | 0.771 |
| 32 | 293.58 | 294.56 | 295.77 | 0.668 | 0.334 | 79.58 | 80.52 | 79.74 | 0.141 | 0.810 | 1.04 | 1.06 | 1.04 | <0.001 | 0.571 |
| 33 | 300.97 | 302.48 | 303.30 | 0.530 | 0.342 | 81.65 | 82.90 | 81.94 | 0.062 | 0.668 | 1.02 | 1.05 | 1.03 | 0.002 | 0.455 |
| 34 | 307.79 | 309.43 | 309.89 | 0.485 | 0.396 | 83.66 | 85.02 | 83.93 | 0.035 | 0.703 | 1.01 | 1.03 | 1.01 | 0.013 | 0.370 |
| 35 | 313.98 | 315.23 | 315.37 | 0.597 | 0.564 | 85.64 | 86.81 | 85.64 | 0.066 | 0.997 | 1.00 | 1.00 | 1.00 | 0.356 | 0.302 |
| 36 | 319.41 | 319.81 | 319.79 | 0.883 | 0.885 | 87.50 | 88.24 | 87.08 | 0.327 | 0.569 | 0.98 | 0.98 | 0.99 | 0.561 | 0.276 |
| 37 | 323.93 | 323.15 | 323.39 | 0.795 | 0.856 | 89.10 | 89.26 | 88.26 | 0.850 | 0.336 | 0.97 | 0.96 | 0.98 | 0.255 | 0.233 |
| 38 | 327.41 | 325.27 | 326.46 | 0.472 | 0.758 | 90.33 | 89.87 | 89.23 | 0.582 | 0.219 | 0.95 | 0.95 | 0.96 | 0.568 | 0.114 |
| 39 | 329.69 | 326.16 | 329.28 | 0.334 | 0.898 | 91.04 | 90.02 | 90.03 | 0.335 | 0.272 | 0.93 | 0.94 | 0.94 | 0.119 | 0.052 |
| 40 | 330.64 | 325.86 | 332.16 | 0.515 | 0.788 | 91.13 | 89.72 | 90.69 | 0.541 | 0.810 | 0.89 | 0.95 | 0.91 | 0.009 | 0.214 |
| GW | Estimated Fetal Weight (EFW), g | Abdominal Circumference (AC), mm | Femur Length (FL), mm | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Back-Transformed Geometric Mean g | Wald Test for Pairwise Comparison p-Value | Back-Transformed Geometric Mean mm | Wald Test for Pairwise Comparison p-Value | Back-Transformed Geometric Mean | Wald Test for Pairwise Comparison p-Value | ||||||||||
| 1st Tertile | 2nd Tertile | 3rd Tertile | 2nd vs. 1st Tertile | 3rd vs. 1st Tertile | 1st Tertile | 2nd Tertile | 3rd Tertile | 2nd vs. 1st Tertile | 3rd vs. 1st Tertile | 1st Tertile | 2nd Tertile | 3rd Tertile | 2nd vs. 1st Tertile | 3rd vs. 1st Tertile | |
| 10 | 41.85 | 32.27 | 35.96 | 0.001 | 0.109 | 43.76 | 36.67 | 38.62 | <0.001 | 0.021 | 2.68 | 2.14 | 2.57 | <0.001 | 0.525 |
| 11 | 47.07 | 42.06 | 45.36 | 0.008 | 0.461 | 49.66 | 46.25 | 48.40 | 0.005 | 0.370 | 4.37 | 3.9 | 4.33 | 0.002 | 0.782 |
| 12 | 55.24 | 54.46 | 57.54 | 0.520 | 0.083 | 56.77 | 56.82 | 59.13 | 0.948 | 0.002 | 6.59 | 6.38 | 6.67 | 0.169 | 0.602 |
| 13 | 67.03 | 70.05 | 73.22 | 0.021 | <0.0001 | 65.17 | 68.13 | 70.59 | <0.0001 | <0.0001 | 9.27 | 9.47 | 9.53 | 0.321 | 0.176 |
| 14 | 83.38 | 89.46 | 93.22 | 0.001 | <0.0001 | 74.88 | 79.96 | 82.52 | <0.0001 | <0.0001 | 12.29 | 12.95 | 12.76 | 0.024 | 0.086 |
| 15 | 105.35 | 113.42 | 118.45 | 0.001 | <0.0001 | 85.83 | 92.07 | 94.68 | <0.0001 | <0.0001 | 15.49 | 16.52 | 16.16 | 0.006 | 0.058 |
| 16 | 134.02 | 142.69 | 149.83 | 0.003 | <0.0001 | 97.84 | 104.28 | 106.87 | <0.0001 | <0.0001 | 18.71 | 19.94 | 19.55 | 0.005 | 0.045 |
| 17 | 170.13 | 178.10 | 188.18 | 0.025 | <0.0001 | 110.55 | 116.46 | 118.94 | <0.0001 | <0.0001 | 21.88 | 23.08 | 22.83 | 0.014 | 0.043 |
| 18 | 213.64 | 220.47 | 234.09 | 0.125 | <0.0001 | 123.42 | 128.58 | 130.81 | <0.0001 | <0.0001 | 24.98 | 25.99 | 25.99 | 0.066 | 0.054 |
| 19 | 263.96 | 270.61 | 287.73 | 0.235 | <0.0001 | 135.99 | 140.67 | 142.49 | 0.001 | <0.0001 | 28.06 | 28.83 | 29.12 | 0.212 | 0.072 |
| 20 | 321.22 | 329.34 | 349.24 | 0.233 | <0.0001 | 148.1 | 152.67 | 153.95 | 0.004 | <0.001 | 31.09 | 31.67 | 32.21 | 0.391 | 0.085 |
| 21 | 385.65 | 397.50 | 419.03 | 0.143 | <0.0001 | 159.65 | 164.49 | 165.14 | 0.003 | 0.001 | 34.02 | 34.49 | 35.22 | 0.529 | 0.091 |
| 22 | 457.56 | 475.86 | 497.51 | 0.054 | <0.0001 | 170.60 | 176.09 | 176.03 | 0.001 | 0.002 | 36.84 | 37.25 | 38.11 | 0.600 | 0.093 |
| 23 | 537.39 | 565.13 | 585.13 | 0.013 | <0.0001 | 181.00 | 187.43 | 186.61 | 0.0001 | 0.001 | 39.51 | 39.93 | 40.86 | 0.608 | 0.095 |
| 24 | 625.81 | 665.91 | 682.42 | 0.003 | <0.0001 | 190.94 | 198.52 | 196.94 | <0.0001 | 0.001 | 42.04 | 42.53 | 43.45 | 0.575 | 0.101 |
| 25 | 723.81 | 778.66 | 790.04 | <0.001 | <0.0001 | 200.59 | 209.38 | 207.09 | <0.0001 | 0.001 | 44.43 | 45.03 | 45.89 | 0.525 | 0.116 |
| 26 | 832.86 | 903.68 | 908.87 | <0.001 | <0.0001 | 210.16 | 220.08 | 217.15 | <0.0001 | 0.002 | 46.72 | 47.44 | 48.18 | 0.477 | 0.140 |
| 27 | 955.00 | 1041.11 | 1040.08 | <0.001 | <0.0001 | 219.93 | 230.70 | 227.27 | <0.0001 | 0.002 | 48.94 | 49.77 | 50.35 | 0.445 | 0.177 |
| 28 | 1093.05 | 1190.85 | 1185.24 | <0.001 | <0.0001 | 230.24 | 241.37 | 237.64 | <0.0001 | 0.002 | 51.14 | 52.02 | 52.44 | 0.437 | 0.234 |
| 29 | 1249.44 | 1352.64 | 1346.23 | <0.001 | <0.0001 | 241.38 | 252.19 | 248.44 | <0.0001 | 0.002 | 53.38 | 54.22 | 54.48 | 0.472 | 0.328 |
| 30 | 1424.33 | 1526.24 | 1523.6 | 0.001 | <0.0001 | 253.23 | 263.13 | 259.70 | <0.0001 | 0.003 | 55.65 | 56.36 | 56.5 | 0.553 | 0.471 |
| 31 | 1616.67 | 1711.36 | 1716.02 | 0.010 | <0.0001 | 265.53 | 274.09 | 271.24 | <0.001 | 0.016 | 57.92 | 58.46 | 58.47 | 0.667 | 0.656 |
| 32 | 1824.08 | 1907.67 | 1921.04 | 0.054 | 0.003 | 277.97 | 284.97 | 282.88 | 0.008 | 0.072 | 60.13 | 60.52 | 60.39 | 0.778 | 0.845 |
| 33 | 2042.57 | 2114.8 | 2134.87 | 0.149 | 0.014 | 290.17 | 295.64 | 294.36 | 0.060 | 0.162 | 62.25 | 62.54 | 62.26 | 0.847 | 0.997 |
| 34 | 2266.30 | 2332.40 | 2352.27 | 0.231 | 0.030 | 301.70 | 305.99 | 305.42 | 0.138 | 0.214 | 64.23 | 64.52 | 64.07 | 0.847 | 0.909 |
| 35 | 2488.31 | 2559.63 | 2567.07 | 0.234 | 0.055 | 312.14 | 315.92 | 315.78 | 0.170 | 0.208 | 66.01 | 66.48 | 65.81 | 0.760 | 0.888 |
| 36 | 2703.66 | 2791.87 | 2778.00 | 0.197 | 0.137247 | 321.54 | 325.70 | 325.45 | 0.185 | 0.238 | 67.58 | 68.4 | 67.48 | 0.619 | 0.947 |
| 37 | 2908.15 | 3021.68 | 2988.34 | 0.152 | 0.194177 | 330.17 | 335.75 | 334.58 | 0.139 | 0.259 | 68.93 | 70.23 | 69.09 | 0.466 | 0.925 |
| 38 | 3097.81 | 3239.88 | 3203.25 | 0.102 | 0.104549 | 338.36 | 346.56 | 343.40 | 0.036 | 0.201 | 70.05 | 71.94 | 70.64 | 0.306 | 0.733 |
| 39 | 3269.08 | 3435.79 | 3429.89 | 0.076 | 0.039051 | 346.46 | 358.67 | 352.13 | 0.003 | 0.211 | 70.94 | 73.48 | 72.15 | 0.194 | 0.522 |
| 40 | 3418.87 | 3597.76 | 3677.57 | 0.171 | 0.129976 | 354.87 | 372.73 | 361.06 | 0.026 | 0.524 | 71.61 | 74.8 | 73.62 | 0.272 | 0.483 |
| GW | Head Circumference (HC), mm | Biparietal Diameter (BPD), mm | HC/AC Ratio | ||||||||||||
| Back-Transformed Geometric Mean mm | Wald Test for Pairwise Comparison p-Value | Back-Transformed Geometric Mean mm | Wald Test for Pairwise Comparison p-Value | Back-Transformed Geometric Mean | Wald Test for Pairwise Comparison p-Value | ||||||||||
| 1st Tertile | 2nd Tertile | 3rd Tertile | 2nd vs. 1st Tertile | 3rd vs. 1st Tertile | 1st Tertile | 2nd Tertile | 3rd Tertile | 2nd vs. 1st Tertile | 3rd vs. 1st Tertile | 1st Tertile | 2nd Tertile | 3rd Tertile | 2nd vs. 1st Tertile | 3rd vs. 1st Tertile | |
| 10 | 58.71 | 43.93 | 52.76 | <0.0001 | 0.013 | 14.20 | 10.88 | 13.10 | <0.0001 | 0.096 | 1.33 | 1.18 | 1.39 | <0.001 | 0.348 |
| 11 | 65.57 | 56.76 | 63.50 | <0.0001 | 0.155 | 16.69 | 14.64 | 16.42 | <0.0001 | 0.522 | 1.32 | 1.22 | 1.32 | <0.0001 | 0.870 |
| 12 | 73.76 | 70.50 | 75.05 | 0.0001 | 0.096 | 19.44 | 18.73 | 19.97 | 0.001 | 0.021 | 1.30 | 1.24 | 1.27 | <0.0001 | 0.053 |
| 13 | 83.29 | 84.60 | 87.23 | 0.136 | <0.0001 | 22.43 | 22.90 | 23.64 | 0.034 | <0.0001 | 1.28 | 1.25 | 1.24 | <0.001 | <0.0001 |
| 14 | 94.17 | 98.53 | 99.83 | <0.0001 | <0.0001 | 25.65 | 26.95 | 27.34 | <0.0001 | <0.0001 | 1.26 | 1.24 | 1.21 | 0.0607 | <0.0001 |
| 15 | 106.28 | 111.94 | 112.69 | <0.0001 | <0.0001 | 29.04 | 30.74 | 30.99 | <0.0001 | <0.0001 | 1.24 | 1.22 | 1.19 | 0.114 | <0.0001 |
| 16 | 119.39 | 124.62 | 125.63 | 0.0001 | <0.0001 | 32.55 | 34.19 | 34.53 | <0.0001 | <0.0001 | 1.22 | 1.20 | 1.17 | 0.032 | <0.0001 |
| 17 | 133.11 | 136.61 | 138.53 | 0.016 | <0.0001 | 36.12 | 37.33 | 37.94 | 0.002 | <0.0001 | 1.20 | 1.18 | 1.16 | 0.001 | <0.0001 |
| 18 | 146.86 | 148.17 | 151.31 | 0.412 | <0.001 | 39.65 | 40.27 | 41.24 | 0.146 | <0.0001 | 1.19 | 1.15 | 1.16 | <0.0001 | <0.001 |
| 19 | 160.18 | 159.72 | 163.93 | 0.789 | 0.007 | 43.08 | 43.20 | 44.50 | 0.799 | 0.001 | 1.18 | 1.14 | 1.15 | <0.0001 | 0.005 |
| 20 | 172.91 | 171.41 | 176.35 | 0.423 | 0.021 | 46.38 | 46.19 | 47.72 | 0.704 | 0.003 | 1.17 | 1.12 | 1.15 | <0.0001 | 0.026 |
| 21 | 184.95 | 183.16 | 188.47 | 0.367 | 0.021 | 49.52 | 49.21 | 50.90 | 0.553 | 0.003 | 1.16 | 1.11 | 1.14 | <0.0001 | 0.069 |
| 22 | 196.25 | 194.9 | 200.23 | 0.514 | 0.010 | 52.51 | 52.25 | 54.02 | 0.642 | 0.001 | 1.15 | 1.10 | 1.14 | <0.0001 | 0.141 |
| 23 | 206.85 | 206.54 | 211.59 | 0.887 | 0.003 | 55.34 | 55.30 | 57.06 | 0.940 | <0.001 | 1.14 | 1.10 | 1.13 | <0.0001 | 0.252 |
| 24 | 216.83 | 218.01 | 222.51 | 0.614 | <0.001 | 58.04 | 58.33 | 60.03 | 0.650 | 0.0001 | 1.14 | 1.10 | 1.13 | <0.0001 | 0.406 |
| 25 | 226.31 | 229.22 | 233.01 | 0.250 | <0.001 | 60.64 | 61.33 | 62.91 | 0.322 | <0.0001 | 1.13 | 1.09 | 1.13 | <0.0001 | 0.582 |
| 26 | 235.48 | 240.11 | 243.12 | 0.089 | 0.0001 | 63.19 | 64.28 | 65.70 | 0.149 | <0.0001 | 1.12 | 1.09 | 1.12 | <0.0001 | 0.751 |
| 27 | 244.58 | 250.59 | 252.88 | 0.036 | <0.0001 | 65.73 | 67.16 | 68.43 | 0.076 | <0.0001 | 1.11 | 1.08 | 1.11 | 0.0001 | 0.905 |
| 28 | 253.86 | 260.60 | 262.37 | 0.022 | <0.0001 | 68.34 | 69.94 | 71.08 | 0.052 | <0.0001 | 1.10 | 1.08 | 1.10 | <0.001 | 0.937 |
| 29 | 263.44 | 270.09 | 271.68 | 0.026 | <0.0001 | 71.04 | 72.62 | 73.69 | 0.057 | <0.0001 | 1.09 | 1.07 | 1.09 | 0.001 | 0.770 |
| 30 | 273.10 | 279.01 | 280.74 | 0.056 | <0.0001 | 73.77 | 75.18 | 76.23 | 0.100 | <0.0001 | 1.08 | 1.06 | 1.08 | 0.002 | 0.634 |
| 31 | 282.54 | 287.36 | 289.40 | 0.143 | <0.001 | 76.45 | 77.60 | 78.66 | 0.214 | <0.001 | 1.06 | 1.05 | 1.07 | 0.016 | 0.577 |
| 32 | 291.43 | 295.10 | 297.48 | 0.298 | 0.008 | 78.99 | 79.87 | 80.97 | 0.384 | 0.004 | 1.05 | 1.04 | 1.05 | 0.088 | 0.589 |
| 33 | 299.38 | 302.26 | 304.79 | 0.441 | 0.027 | 81.28 | 81.98 | 83.11 | 0.572 | 0.015 | 1.03 | 1.02 | 1.04 | 0.270 | 0.633 |
| 34 | 306.02 | 308.83 | 311.15 | 0.462 | 0.031 | 83.23 | 83.93 | 85.04 | 0.523 | 0.013 | 1.02 | 1.01 | 1.02 | 0.621 | 0.706 |
| 35 | 311.07 | 314.80 | 316.38 | 0.336 | 0.020 | 84.74 | 85.70 | 86.73 | 0.387 | 0.004 | 1.00 | 1.00 | 1.00 | 0.764 | 0.850 |
| 36 | 314.81 | 319.88 | 320.52 | 0.216 | 0.027 | 85.89 | 87.27 | 88.20 | 0.246 | 0.004 | 0.99 | 0.99 | 0.98 | 0.384 | 0.950 |
| 37 | 317.72 | 323.72 | 323.74 | 0.174 | 0.045 | 86.76 | 88.62 | 89.47 | 0.159 | 0.003 | 0.97 | 0.98 | 0.97 | 0.374 | 0.786 |
| 38 | 320.28 | 325.94 | 326.21 | 0.216 | 0.049 | 87.48 | 89.70 | 90.61 | 0.103 | 0.001 | 0.95 | 0.96 | 0.95 | 0.700 | 0.618 |
| 39 | 323.00 | 326.17 | 328.14 | 0.500 | 0.127 | 88.15 | 90.50 | 91.65 | 0.099 | 0.001 | 0.94 | 0.93 | 0.93 | 0.321 | 0.560 |
| 40 | 326.42 | 324.09 | 329.75 | 0.702 | 0.628 | 88.91 | 90.99 | 92.66 | 0.314 | 0.074 | 0.92 | 0.89 | 0.91 | 0.064 | 0.750 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, L.-J.; Du, R.; Ouidir, M.; Lu, R.; Chen, Z.; Weir, N.L.; Tsai, M.Y.; Albert, P.S.; Zhang, C. Early Pregnancy Maternal Plasma Phospholipid Saturated Fatty Acids and Fetal Growth: Findings from a Multi-Racial/Ethnic Birth Cohort in US. Nutrients 2023, 15, 3287. https://doi.org/10.3390/nu15153287
Li L-J, Du R, Ouidir M, Lu R, Chen Z, Weir NL, Tsai MY, Albert PS, Zhang C. Early Pregnancy Maternal Plasma Phospholipid Saturated Fatty Acids and Fetal Growth: Findings from a Multi-Racial/Ethnic Birth Cohort in US. Nutrients. 2023; 15(15):3287. https://doi.org/10.3390/nu15153287
Chicago/Turabian StyleLi, Ling-Jun, Ruochen Du, Marion Ouidir, Ruijin Lu, Zhen Chen, Natalie L. Weir, Michael Y. Tsai, Paul S. Albert, and Cuilin Zhang. 2023. "Early Pregnancy Maternal Plasma Phospholipid Saturated Fatty Acids and Fetal Growth: Findings from a Multi-Racial/Ethnic Birth Cohort in US" Nutrients 15, no. 15: 3287. https://doi.org/10.3390/nu15153287
APA StyleLi, L.-J., Du, R., Ouidir, M., Lu, R., Chen, Z., Weir, N. L., Tsai, M. Y., Albert, P. S., & Zhang, C. (2023). Early Pregnancy Maternal Plasma Phospholipid Saturated Fatty Acids and Fetal Growth: Findings from a Multi-Racial/Ethnic Birth Cohort in US. Nutrients, 15(15), 3287. https://doi.org/10.3390/nu15153287









