Association between Depressive Symptoms and Adherence to the Mediterranean Diet in Nursing Students
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Information Collection
2.3. Depressive and Anxiety Symptoms
2.4. Adherence to the Mediterranean Diet
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Study Sample
3.2. Consumption of Coffee, Cola, Tea, and Alcohol and Smoking
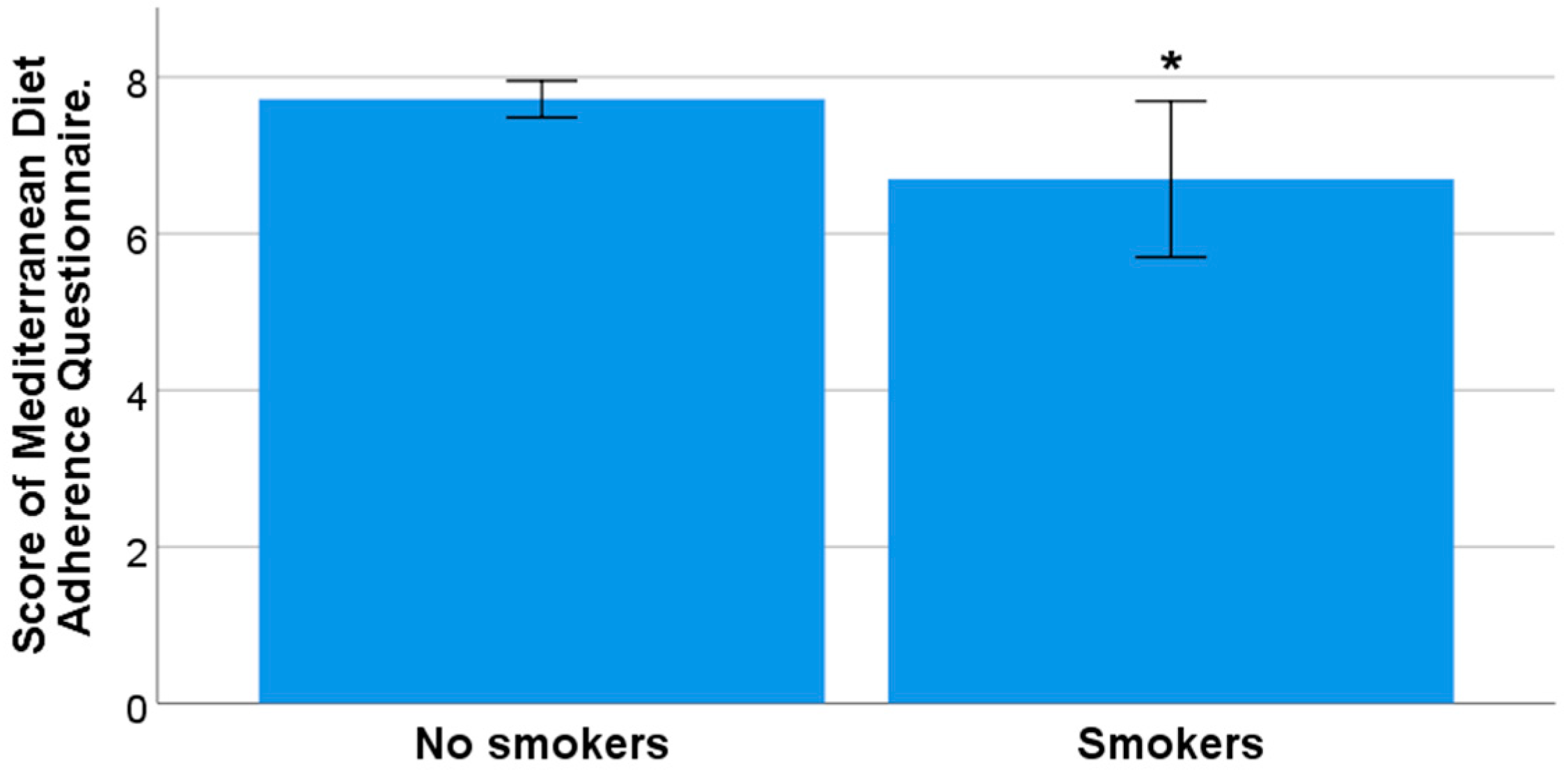
3.3. Adherence to the Mediterranean Diet and Its Relationship with Sociodemographic Characteristics, Lifestyle, and Health Conditions
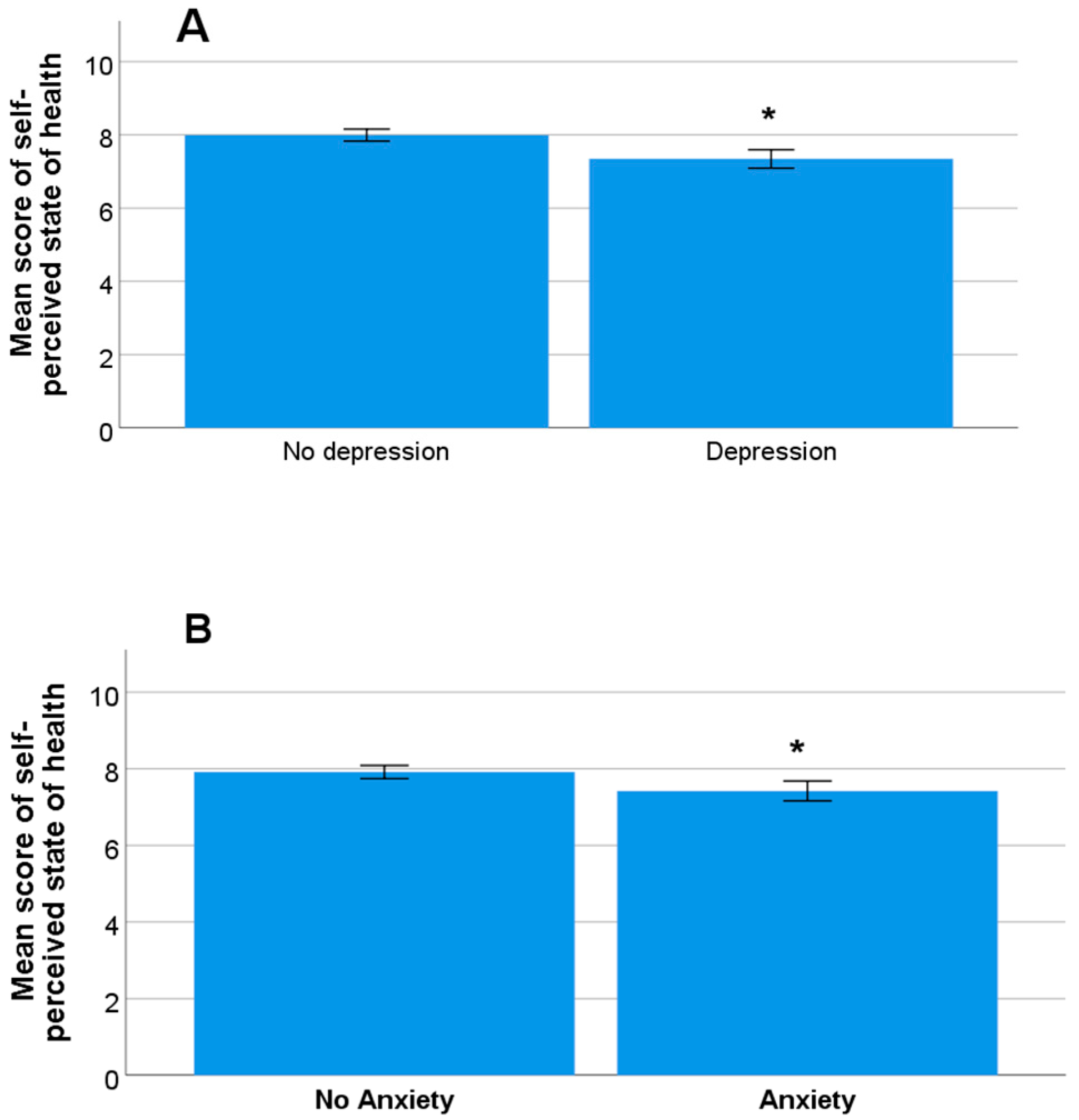
3.4. Symptoms of Anxiety and Depression and Their Relationship with Sociodemographic Characteristics, Lifestyle, and Health Conditions
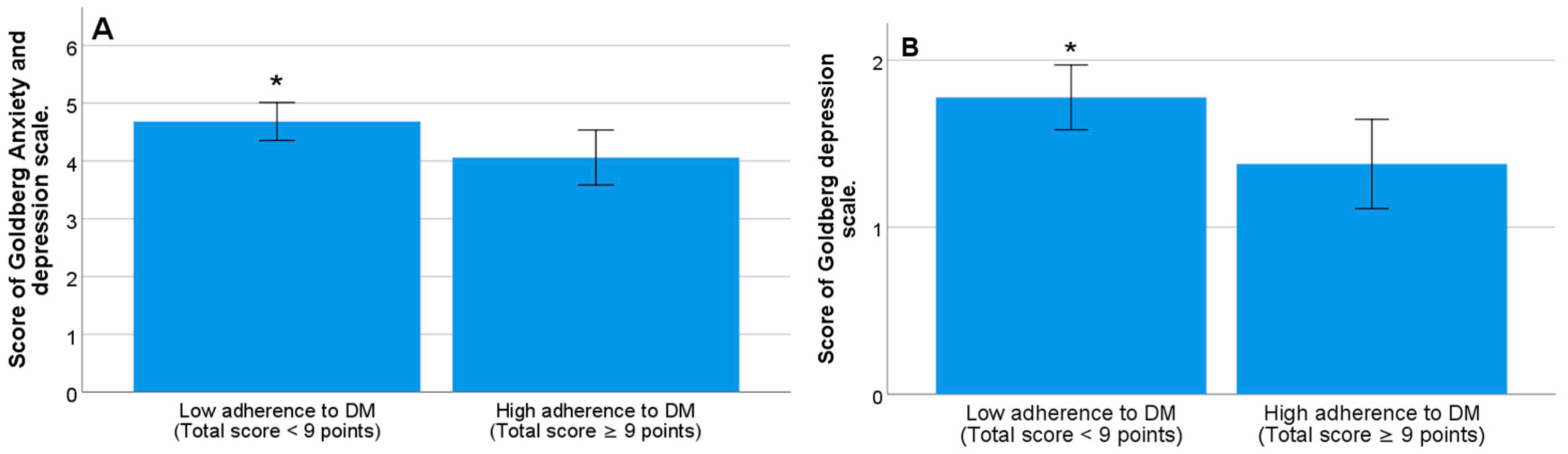
3.5. Relationship between Adherence to the Mediterranean Diet and Students’ Mood
3.6. Variables Associated with Low Adherence to MD: Logistic Regression Analysis
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D.; Willett, W.C.; Sacks, F.; Trichopoulou, A. Mediterranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. 1995, 61 (Suppl. S6), 1402S–1406S. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Sánchez-Villegas, A. The emerging role of Mediterranean diets in cardiovascular epidemiology: Monounsaturated fats, olive oil, red wine or the whole pattern? Eur. J. Epidemiol. 2004, 19, 9–13. [Google Scholar] [CrossRef]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean Diet; a Literature Review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013, 368, 1279–1290, Retraction in N. Engl. J. Med. 2018, 378, 2441–2442. [Google Scholar] [CrossRef] [PubMed]
- Nordmann, A.J.; Suter-Zimmermann, K.; Bucher, H.C.; Shai, I.; Tuttle, K.R.; Estruch, R.; Briel, M. Meta-analysis comparing Mediterranean to low-fat diets for modification of cardiovascular risk factors. Am. J. Med. 2011, 124, 841–851.e2. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G. Adherence to Mediterranean diet and risk of cancer: A systematic review and metaanalysis of observational studies. Int. J. Cancer 2014, 135, 1884–1897. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G. Adherence to Mediterranean diet and risk of cancer: An updated systematic review and meta-analysis of observational studies. Cancer Med. 2015, 4, 1933–1947. [Google Scholar] [CrossRef]
- Couto, E.; Boffetta, P.; Lagiou, P.; Ferrari, P.; Buckland, G.; Overvad, K.; Dahm, C.C.; Tjønneland, A.; Olsen, A.; Clavel-Chapelon, F.; et al. Mediterranean dietary pattern and cancer risk in the EPIC cohort. Br. J. Cancer 2011, 104, 1493–1499. [Google Scholar] [CrossRef]
- Esposito, K.; Giugliano, D. Mediterranean diet and type 2 diabetes. Diabetes Metab. Res. Rev. 2014, 30 (Suppl. S1), 34–40. [Google Scholar] [CrossRef]
- Esposito, K.; Maiorino, M.I.; Bellastella, G.; Chiodini, P.; Panagiotakos, D.; Giugliano, D. A journey into a Mediterranean diet and type 2 diabetes: A systematic review with meta-analyses. BMJ Open 2015, 5, e008222. [Google Scholar] [CrossRef]
- Parletta, N.; Zarnowiecki, D.; Cho, J.; Wilson, A.; Bogomolova, S.; Villani, A.; Itsiopoulos, C.; Niyonsenga, T.; Blunden, S.; Meyer, B.; et al. A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized controlled trial (HELFIMED). Nutr. Neurosci. 2019, 22, 474–487. [Google Scholar] [CrossRef]
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 2013 acute and chronic diseases and injuries in 188 countries, 1990–2103: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015, 386, 743–800. [Google Scholar] [CrossRef]
- World Health Organization. Available online: https://www.who.int/es/news-room/fact-sheets/detail/depression (accessed on 5 June 2023).
- Subdirección General de Información Sanitaria. Salud Mental en Datos: Prevalencia de los Problemas de Salud y Consumo de Psicofármacos y Fármacos Relacionados a Partir de Registros Clínicos de Atención Primaria. BDCAP Series 2; Ministerio de Sanidad: Madrid, Spain, 2021; Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SIAP/Salud_mental_datos.pdf (accessed on 20 May 2023).
- Zielińska, M.; Łuszczki, E.; Michońska, I.; Dereń, K. The Mediterranean Diet and the Western Diet in Adolescent Depression-Current Reports. Nutrients 2022, 14, 4390. [Google Scholar] [CrossRef] [PubMed]
- Institute for Health Metrics and Evaluation (IHME). Available online: https://www.healthdata.org/acting-data/new-ihme-analyses-show-depression-and-anxiety-among-top-causes-health-burden-worldwide (accessed on 5 June 2023).
- Burke, A.S.; Shapero, B.G.; Pelletier-Baldelli, A.; Deng, W.Y.; Nyer, M.B.; Leathem, L.; Namey, L.; Landa, C.; Cather, C.; Holt, D.J. Rationale, methods, feasibility, and preliminary outcomes of a transdiagnostic prevention program for at-risk college students. Front. Psychiatry 2020, 10, 1030. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Amminger, G.P.; Aguilar-Gaxiola, S.; Alonso, J.; Lee, S.; Ustün, T.B. Age of onset of mental disorders: A review of recent literature. Curr. Opin. Psychiatry 2007, 20, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Rotenstein, L.S.; Ramos, M.A.; Torre, M.; Segal, J.B.; Peluso, M.J.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of Depression, Depressive Symptoms, and Suicidal Ideation Among Medical Students: A Systematic Review and Meta-Analysis. JAMA 2016, 316, 2214–2236. [Google Scholar] [CrossRef]
- Mayne, S.L.; Hannan, C.; Davis, M.; Young, J.F.; Kelly, M.K.; Powell, M.; Dalembert, G.; McPeak, K.E.; Jenssen, B.P.; Fiks, A.G. COVID-19 and Adolescent Depression and Suicide Risk Screening Outcomes. Pediatrics 2021, 148, e2021051507. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística (INE). España. Nota de Prensa. Defunciones Según la Causa de Muerte. 19 de Diciembre de 2022. Available online: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176780&menu=ultiDatos&idp=1254735573175 (accessed on 8 June 2023).
- Buchanan, J.L. Prevention of depression in the college student population: A review of the literature. Arch. Psychiatr. Nurs. 2012, 26, 21–42. [Google Scholar] [CrossRef]
- Carrión-Pantoja, S.; Prados, G.; Chouchou, F.; Holguín, M.; Mendoza-Vinces, Á.; Expósito-Ruiz, M.; Fernández-Puerta, L. Insomnia Symptoms, Sleep Hygiene, Mental Health, and Academic Performance in Spanish University Students: A Cross-Sectional Study. J. Clin. Med. 2022, 11, 1989. [Google Scholar] [CrossRef]
- Benton, S.A.; Benton, S.L. College Student Mental Health: Effective Services and Strategies across Campus; NASPA: Washington, DC, USA, 2006. [Google Scholar]
- Watkins, D.C.; Hunt, J.B.; Eisenberg, D. Increased demand for mental health services on college campuses: Perspectives from administrators. Qual. Soc. Work 2012, 11, 319–337. [Google Scholar] [CrossRef]
- Ventriglio, A.; Sancassiani, F.; Contu, M.P.; Latorr, M.; Di Slavatore, M.; Fornaro, M.; Bhugra, D. Mediterranean Diet and its Benefits on Health and Mental Health: A Literature Review. Clin. Pract. Epidemiol. Ment. Health 2020, 16 (Suppl. S1), 156–164. [Google Scholar] [CrossRef] [PubMed]
- Jacka, F.N.; O’Neil, A.; Opie, R.; Itsiopoulos, C.; Cotton, S.; Mohebbi, M.; Castle, D.; Dash, S.; Mihalopoulos, C.; Chatterton, M.L.; et al. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med. 2017, 15, 23. [Google Scholar] [CrossRef]
- Mosteiro-Diaz, M.P.; Baldonedo-Mosteiro, C.; Campos Pavan Baptista, P.; Gamez-Fernandez, A.; Franco-Correia, S. Anxiety and depression among nursing students during the COVID-19 lockdown: A cross-sectional correlational study. J. Clin. Nurs. 2023, 32, 5065–5075. [Google Scholar] [CrossRef] [PubMed]
- Akinyemi, O.A.; Babatunde, O.; Weldeslase, T.A.; Akinyemi, I.; Akinwumi, B.; Oladunjoye, A.O.; Ogundare, T.; Bezold, M. Association Between Obesity and Self-Reported Depression Among Female University Students in the United States. Cureus 2022, 14, e31386. [Google Scholar] [CrossRef] [PubMed]
- Bombak, A.E. Self-rated health and public health: A critical perspective. Front. Public Health 2013, 1, 15. [Google Scholar] [CrossRef] [PubMed]
- Paúl, C.; Ribeiro, O.; Teixeira, L. Active Ageing: An Empirical Approach to the WHO Model. Curr. Gerontol. Geriatr. Res. 2012, 2012, 382972. [Google Scholar] [CrossRef]
- Bradley, K.A.; Bush, K.R.; Epler, A.J.; Dobie, D.J.; Davis, T.M.; Sporleder, J.L.; Maynard, C.; Burman, M.L.; Kivlahan, D.R. Two brief alcohol-screening tests From the Alcohol Use Disorders Identification Test (AUDIT): Validation in a female Veterans Affairs patient population. Arch. Intern. Med. 2003, 163, 821–829. [Google Scholar] [CrossRef]
- Bekar, C.; Goktas, Z. Validation of the 14-item mediterranean diet adherence screener. Clin. Nutr. ESPEN 2023, 53, 238–243. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Hillier, V.F. A scaled version of the General Health Questionnaire. Psychological Medicine. Psychol. Med. 1979, 9, 139–145. [Google Scholar] [CrossRef]
- Montón, C.; Pérez Echeverría, M.J.; Campos, R.; García Campayo, J.; Lobo, A. Anxiety scales and Goldberg’s depression: An efficient interview guide for the detection of psychologic distress. Aten. Primaria 1993, 12, 345–349. [Google Scholar] [PubMed]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvad, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- Dernini, S.; Berry, E.M. Mediterranean Diet: From a Healthy Diet to a Sustainable Dietary Pattern. Front. Nutr. 2015, 2, 15. [Google Scholar] [CrossRef]
- Ruggeri, S.; Buonocore, P.; Amoriello, T. New Validated Short Questionnaire for the Evaluation of the Adherence of Mediterranean Diet and Nutritional Sustainability in All Adult Population Groups. Nutrients 2022, 14, 5177. [Google Scholar] [CrossRef]
- Müller, C.; El-Ansari, K.; El Ansari, W. Cross-Sectional Analysis of Mental Health among University Students: Do Sex and Academic Level Matter? Int. J. Environ. Res. Public Health 2022, 19, 12670. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, A.M.; Hakami, A.; AlHadi, A.; Batais, M.A.; Alrasheed, A.A.; Almigbal, T.H. The interplay between mindfulness, depression, stress and academic performance in medical students: A Saudi perspective. PLoS ONE 2020, 15, e0231088. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Torrano, D.; Ibrayeva, L.; Sparks, J.; Lim, N.; Clementi, A.; Almukhambetova, A.; Nurtayev, Y.; Muratkyzy, A. Mental Health and Well-Being of University Students: A Bibliometric Mapping of the Literature. Front. Psychol. 2020, 11, 1226. [Google Scholar] [CrossRef] [PubMed]
- Gogoi, M.; Webb, A.; Pareek, M.; Bayliss, C.D.; Gies, L. University Students’ Mental Health and Well-Being during the COVID-19 Pandemic: Findings from the UniCoVac Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19, 9322. [Google Scholar] [CrossRef]
- Reneses, B.; Garrido, S.; Navalón, A.; Martín, O.; Ramos, I.; Fuentes, M.; Moreno, J.; López-Ibor, J.J. Psychiatric morbidity and predisposing factors in a primary care population in Madrid. Int. J. Soc. Psychiatry 2015, 61, 275–286. [Google Scholar] [CrossRef]
- Ramón-Arbués, E.; Gea-Caballero, V.; Granada-López, J.M.; Juárez-Vela, R.; Pellicer-García, B.; Antón-Solanas, I. The Prevalence of Depression, Anxiety and Stress and Their Associated Factors in College Students. Int. J. Environ. Res. Public Health 2020, 17, 7001. [Google Scholar] [CrossRef]
- Wong, J.G.; Cheung, E.P.; Chan, K.K.; Ma, K.K.; Tang, S.W. Web-based survey of depression, anxiety and stress in first-year tertiary education students in Hong Kong. Aust. N. Z. J. Psychiatry 2006, 40, 777–782. [Google Scholar] [CrossRef]
- Blanco, V.; Salmerón, M.; Otero, P.; Vázquez, F.L. Symptoms of Depression, Anxiety, and Stress and Prevalence of Major Depression and Its Predictors in Female University Students. Int. J. Environ. Res. Public Health 2021, 18, 5845. [Google Scholar] [CrossRef]
- García-Fernández, L.; Romero-Ferreiro, V.; Izquierdo-Izquierdo, M.; Rodríguez, V.; Alvarez-Mon, M.A.; Lahera, G.; Santos, J.L.; Rodriguez-Jimenez, R. Dramatic increase of suicidality in children and adolescents after COVID-19 pandemic start: A two-year longitudinal study. J. Psychiatr. Res. 2023, 163, 63–67. [Google Scholar] [CrossRef]
- Gruber, J.; Prinstein, M.J.; Clark, L.A.; Rottenberg, J.; Abramowitz, J.S.; Albano, A.M.; Aldao, A.; Borelli, J.L.; Chung, T.; Davila, J.; et al. Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. Am. Psychol. 2021, 76, 409–426. [Google Scholar] [CrossRef] [PubMed]
- Hawes, M.T.; Szenczy, A.K.; Klein, D.N.; Hajcak, G.; Nelson, B.D. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol. Med. 2022, 52, 3222–3230. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Hawkley, L.C.; Ernst, J.M.; Burleson, M.; Bertnson, G.G.; Nouriani, B.; Spiegel, D. Loneliness within a nomological net: An evolutionary perspective. J. Res. Pers. 2006, 40, 1054–1085. [Google Scholar] [CrossRef]
- Nolen-Hoeksema, S.; Ahrens, C. Age differences and similarities in the correlates of depressive symptoms. Psychol. Aging. 2002, 17, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Victor, C.R.; Yang, K.M. The prevalence of loneliness among adults: A case study of the United Kingdom. J. Psychol. 2012, 146, 85–104. [Google Scholar] [CrossRef] [PubMed]
- Casal Rodríguez, B.; Rivera Castiñeira, B.; Rodríguez-Míguez, E. Estudio el Coste de la Soledad no Deseada en España. Observatorio Estatal de la Soledad No Deseada. Fundación ONCE. Available online: https://www.soledades.es/ (accessed on 4 June 2023).
- Cyranowski, J.M.; Frank, E.; Young, E. Adolescent onset of the gender difference in lifetime rates of major depression: A theoretical model. Arch. Gen. Psychiatry 2000, 57, 21–27. [Google Scholar] [CrossRef]
- Ford, D.E.; Erlinger, T.P. Depression and C-reactive protein in US adults: Data from the Third National Health and Nutrition Examination Survey. Arch. Intern. Med. 2004, 164, 1010–1014. [Google Scholar] [CrossRef] [PubMed]
- Ghrouz, A.K.; Noohu, M.M.; Dilshad Manzar, M.; Warren Spence, D.; BaHammam, A.S.; Pandi-Perumal, S.R. Physical activity and sleep quality in relation to mental health among college students. Sleep Breath. 2019, 23, 627–634. [Google Scholar] [CrossRef] [PubMed]
- Ishida, M.; Montagni, I.; Matsuzaki, K.; Shimamoto, T.; Cariou, T.; Kawamura, T.; Tzourio, C.; Iwami, T. The association between depressive symptoms and self-rated health among university students: A cross-sectional study in France and Japan. BMC Psychiatry 2020, 20, 549. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Jiang, C.; Yang, Y.; Dzierzewski, J.M.; Spruyt, K.; Zhang, B.; Huang, M.; Ge, H.; Rong, Y.; Ola, B.A.; et al. Depression and Anxiety Mediate the Association between Sleep Quality and Self-Rated Health in Healthcare Students. Behav. Sci. 2023, 13, 82. [Google Scholar] [CrossRef] [PubMed]
- Villanueva-Blasco, V.J.; Villanueva-Silvestre, V.; Vázquez-Martínez, A.; de Vicente, L.P.; Pérez-Gálvez, B. Depression, Suicidal Ideation, and Consumption of Psychotropic Drugs During Lockdown by COVID-19 According to Gender and Age. Int. J. Ment. Health Addict. 2022, 1–17. [Google Scholar] [CrossRef]
- Cobo-Cuenca, A.I.; Garrido-Miguel, M.; Soriano-Cano, A.; Ferri-Morales, A.; Martínez-Vizcaíno, V.; Martín-Espinosa, N.M. Adherence to the Mediterranean Diet and Its Association with Body Composition and Physical Fitness in Spanish University Students. Nutrients 2019, 11, 2830. [Google Scholar] [CrossRef]
- López-Moreno, M.; Garcés-Rimón, M.; Miguel, M.; Iglesias López, M.T. Adherence to Mediterranean Diet, Alcohol Consumption and Emotional Eating in Spanish University Students. Nutrients 2021, 13, 3174. [Google Scholar] [CrossRef]
- Antonopoulou, M.; Mantzorou, M.; Serdari, A.; Bonotis, K.; Vasios, G.; Pavlidou, E.; Trifonos, C.; Vadikolias, K.; Petridis, D.; Giaginis, C. Evaluating Mediterranean diet adherence in university student populations: Does this dietary pattern affect students’ academic performance and mental health? Int. J. Health Plan. Manag. 2020, 35, 5–21. [Google Scholar] [CrossRef]
- Sánchez-Villegas, A.; Delgado-Rodríguez, M.; Alonso, A.; Schlatter, J.; Lahortiga, F.; Serra Majem, L.; Martínez-González, M.A. Association of the Mediterranean dietary pattern with the incidence of depression: The Seguimiento Universidad de Navarra/University of Navarra follow-up (SUN) cohort. Arch. Gen. Psychiatry 2009, 66, 1090–1098. [Google Scholar] [CrossRef]
- Pardavila-Belio, M.I.; Hershey, M.S.; Barbería-Latasa, M.; Toledo, E.; Martin-Moreno, J.M.; Martínez-González, M.Á.; Ruiz-Canela, M. Joint association of the Mediterranean diet and smoking with all-cause mortality in the Seguimiento Universidad de Navarra (SUN) cohort. Nutrition 2022, 103–104, 111761. [Google Scholar] [CrossRef]
- Zaragoza-Martí, A.; Ferrer-Cascales, R.; Hurtado-Sánchez, J.A.; Laguna-Pérez, A.; Cabañero-Martínez, M.J. Relationship between Adherence to the Mediterranean Diet and Health-Related Quality of Life and Life Satisfaction among Older Adults. J. Nutr. Health Aging 2018, 22, 89–96. [Google Scholar] [CrossRef]
- Popa, T.A.; Ladea, M. Nutrition and depression at the forefront of progress. J. Med. Life 2012, 5, 414–419. [Google Scholar]
- Rechenberg, K.; Humphries, D. Nutritional interventions in depression and perinatal depression. Yale J. Biol. Med. 2013, 86, 127–137. [Google Scholar]
- Duarte, R.; Escario, J.J.; Molina, J.A. Marijuana consumption and school failure among Spanish students. Econ. Educ. Rev. 2006, 25, 472–481. [Google Scholar] [CrossRef]
- Páramo, M.F.; Cadaveira, F.; Tinajero, C.; Rodríguez, M.S. Binge Drinking, Cannabis Co-Consumption and Academic Achievement in First Year University Students in Spain: Academic Adjustment as a Mediator. Int. J. Environ. Res. Public Health 2020, 17, 542. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Martínez, R.; Chover-Sierra, E.; Colomer-Pérez, N.; Vlachou, E.; Andriuseviciene, V.; Cauli, O. Sleep quality and its association with substance abuse among university students. Clin. Neurol. Neurosurg. 2020, 188, 105591. [Google Scholar] [CrossRef] [PubMed]
- Strickland, J.C.; Smith, M.A. The effects of social contact on drug use: Behavioral mechanisms controlling drug intake. Exp. Clin. Psychopharmacol. 2014, 22, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Birch, L.L.; Davison, K.K. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr. Clin. N. Am. 2001, 48, 893–907. [Google Scholar] [CrossRef]
- Story, M.; Neumark-Sztainer, D.; French, S.A. Individual and environmental influences on adolescent eating behaviors. J. Am. Diet. Assoc. 2002, 102, S40–S51. [Google Scholar] [CrossRef]
- Deliens, T.; Clarys, P.; de Bourdeaudhuij, I.; Deforche, B. Correlates of university students’ soft and energy drink consumption according to gender and residency. Nutrients 2015, 7, 6550–6566. [Google Scholar] [CrossRef]
- Pearson, T.; Timperio, A.; Salmon, J.; Crawford, D.; Biddle, S. Family influences on childrens’ physical activity and fruit and vegetable consumption. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 34. [Google Scholar] [CrossRef]
- Tanja, T.T.; Outi, N.; Sakari, S.; Jarmo, L.; Kaisa, P.; Leila, K. Preliminary Finnish measures of eating competence suggest association with health-promoting eating patterns and related psychobehavioral factors in 10–17-year-old adolescents. Nutrients 2015, 7, 3828–3846. [Google Scholar] [CrossRef] [PubMed]
- Sarmugam, R.; Worsley, A. Dietary Behaviours, Impulsivity and Food Involvement: Identification of Three Consumer Segments. Nutrients 2015, 7, 8036–8057. [Google Scholar] [CrossRef] [PubMed]
| Qualitative Variables | Frequency (n) | Percentage (%) | |
| Gender | Female | 250 | 86.5 |
| Male | 39 | 13.5 | |
| Nationality | Spanish | 276 | 95.5 |
| Other | 13 | 4.5 | |
| Marital status | Single | 276 | 95.5 |
| Married | 13 | 4.5 | |
| Children | No | 288 | 99.7 |
| Yes | 1 | 0.3 | |
| Cohabitation | Family | 198 | 69.5 |
| Friends | 67 | 23.2 | |
| Couple | 15 | 5.2 | |
| Other | 9 | 3.1 | |
| Chronic diseases | No | 238 | 82.4 |
| Yes | 51 | 17.6 | |
| BMI (kg/m2) | Underweight | 30 | 10.4 |
| Normal weight | 214 | 74.0 | |
| Overweight | 30 | 10.4 | |
| Obese | 11 | 3.8 | |
| Stimulating drinks daily (coffee, cola, tea) | No | 110 | 39.1 |
| Yes | 179 | 61.9 | |
| Tobacco | No | 266 | 92 |
| Yes | 23 | 8 | |
| Alcohol | No | 121 | 41.9 |
| Yes | 168 | 58.1 | |
| Psychoactive substances | No | 285 | 98.6 |
| Yes | 4 | 1.4 | |
| Psychotropic drugs daily | No | 276 | 95.5 |
| Yes | 13 | 4.5 | |
| Quantitative variable | Mean (±SD) | Range | |
| Age (years) | 20.60 (±2.56) | 17–30 | |
| Self-perceived health (0–10) | 7.69 (±1.29) | 1–10 | |
| Items of the Questionnaire Corresponding to Good Adherence to MD | % Individuals over the Total Sample Who Fulfilled the Recommended Pattern of Consumption of Each Food |
|---|---|
| Use olive oil as the principal source of fat for cooking | 92.7% |
| ≥4 tablespoons of oil/day | 41.2% |
| ≥2 servings of vegetables/day | 49.8% |
| ≥3 servings of fruit/day | 21.8% |
| <1 serving of red meat, hamburgers, sausage/day | 68.2% |
| <1 serving of butter, margarine, cream/day | 97.6% |
| <1 serving of carbonated sweetened beverages/day | 90.3% |
| ≥3 servings of legumes/week | 33.2% |
| ≥3 servings of fish or seafood/week | 21.5% |
| <2 servings of commercial pastries/week | 54.7% |
| ≥3 servings of nuts/week | 38.1% |
| Prefers white meat over red meat | 83% |
| ≥2 times/week homemade tomato sauce | 71.3% |
| Individuals with good adherence to MD based on proposed cut-off value (total score ≥ 9 points) | 35.6% |
| Variables | p-Value | Exp (B) | 95%CI EXP (B) | |
|---|---|---|---|---|
| LL | UL | |||
| BMI | 0.622 | 0.969 | 0.790 | 1.188 |
| Smoking | 0.198 | 0.508 | 0.181 | 1.424 |
| Goldberg total scale score | 0.761 | 1.019 | 0.947 | 1.096 |
| Depression subscale score | 0.021 | 0.803 | 0.666 | 0.968 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ibáñez-del Valle, V.; Navarro-Martínez, R.; Cauli, O. Association between Depressive Symptoms and Adherence to the Mediterranean Diet in Nursing Students. Nutrients 2023, 15, 3158. https://doi.org/10.3390/nu15143158
Ibáñez-del Valle V, Navarro-Martínez R, Cauli O. Association between Depressive Symptoms and Adherence to the Mediterranean Diet in Nursing Students. Nutrients. 2023; 15(14):3158. https://doi.org/10.3390/nu15143158
Chicago/Turabian StyleIbáñez-del Valle, Vanessa, Rut Navarro-Martínez, and Omar Cauli. 2023. "Association between Depressive Symptoms and Adherence to the Mediterranean Diet in Nursing Students" Nutrients 15, no. 14: 3158. https://doi.org/10.3390/nu15143158
APA StyleIbáñez-del Valle, V., Navarro-Martínez, R., & Cauli, O. (2023). Association between Depressive Symptoms and Adherence to the Mediterranean Diet in Nursing Students. Nutrients, 15(14), 3158. https://doi.org/10.3390/nu15143158







