Food Insecurity and Mental Health among Venezuelan Migrants and Refugees Living in Peru: Secondary Data Analysis of a Cross-Sectional Survey
Highlights
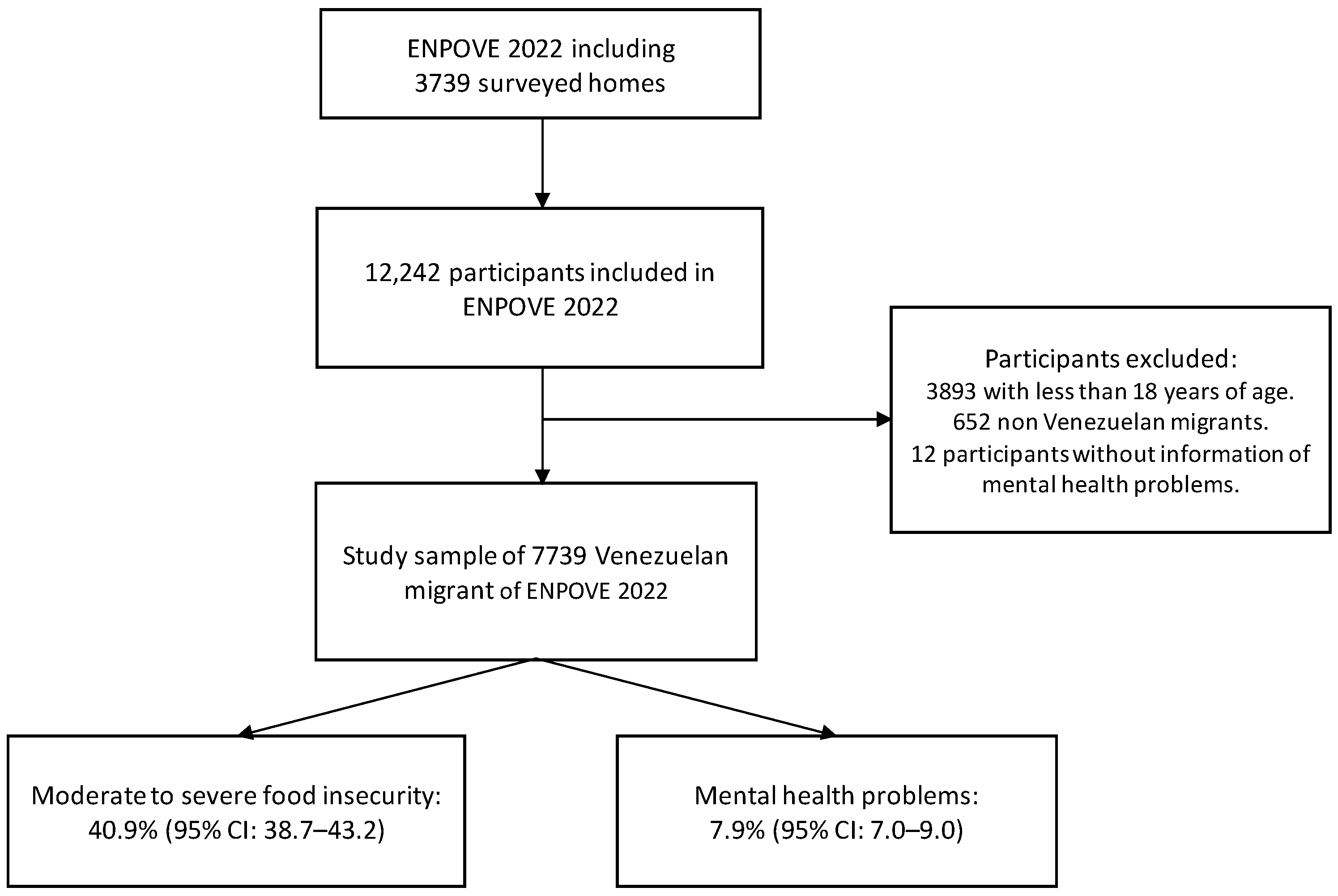
- This study found that 40.9% of Venezuelan migrants and refugees in Peru lived in households with moderate to severe food insecurity.
- Approximately 7.9% of the participants reported experiencing mental health problems, such as depression and anxiety, in the last month.
- There was a significant association between moderate to severe food insecurity and the likelihood of experiencing mental health problems, with a 2.16 times higher risk compared to food-secure households.
- These findings emphasize the need for comprehensive support for food-insecure households to prevent mental health problems. This includes food assistance, nutritional education, and access to affordable mental health services.
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Study Population
2.2. Variables and Measurements
2.2.1. Outcome Variable
2.2.2. Main Exposure
2.2.3. Covariables
2.3. Statistical Analysis
2.4. Ethical Considerations
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grupo de Trabajo para Refugiados y Migrantes (GTRM). GTRM Perú—Análisis Conjunto de Necesidades Para El RMRP 2022; Grupo de Trabajo para Refugiados y Migrantes (GTRM): Lima, Peru, 2021. [Google Scholar]
- Mendoza, W.; Miranda, J.J. La Inmigración Venezolana En El Perú: Desafíos y Oportunidades Desde La Perspectiva de La Salud. Rev. Peru. Med. Exp. Salud Pública 2019, 36, 497. [Google Scholar] [CrossRef] [PubMed]
- Uscategui, R. Una Oportunidad Para Todos: Los Migrantes y Refugiados Venezolanos y El Desarrollo Del Perú; The World Bank: Washington, DC, USA, 2019. [Google Scholar]
- Landaeta-Jiménez, M.; Herrera Cuenca, M.; Vásquez, M.; Ramírez, G. La alimentación y nutrición de los venezolanos: Encuesta Nacional de Condiciones de Vida 2014. In Anales Venezolanos de Nutrición; Fundación Bengoa: Caracas, Miranda, 2015; pp. 100–109. [Google Scholar]
- Vargas-Vásquez, A.; Aparco, J.P.; Hernández-Vásquez, A.; Pisfil-Benites, N.; Fuentes-Rivera, H. Food Insecurity among the Migrant Venezuelan Population in Peru during the COVID-19 Pandemic. Rev. Child. Nutr. 2022, 49, 524–525. [Google Scholar] [CrossRef]
- Coleman-Jensen, A.; Rabbitt, M.P.; Gregory, C.A.; Singh, A. Household Food Security in the United States in 2020. Available online: http://www.ers.usda.gov/publications/pub-details/?pubid=102075 (accessed on 25 February 2023).
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2022; FAO: Rome, Italy, 2022; ISBN 978-92-5-136499-4. [Google Scholar]
- Instituto Nacional de Estadística e Informática. Condiciones de Vida de la Población Venezolana que Reside en el Perú: Resultados de la “Encuesta Dirigida a la Polación Venezolana que Reside en el País” II ENPOVE 2022; Instituto Nacional de Estadística e Informática: Lima, Peru, 2023; Available online: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1666/libro.pdf (accessed on 14 February 2023).
- Mansour, R.; John, J.R.; Liamputtong, P.; Arora, A. Prevalence and Risk Factors of Food Insecurity among Libyan Migrant Families in Australia. BMC Public Health 2021, 21, 2156. [Google Scholar] [CrossRef]
- Pico, R.; del Castillo Matamoros, S.; Bernal, J. Food and Nutrition Insecurity in Venezuelan Migrant Families in Bogotá, Colombia. Front. Sustain. Food Syst. 2021, 5, 634817. [Google Scholar] [CrossRef]
- World Food Programme. Food Security Update on Venezuelan Migrants and Refugees in Colombia, Ecuador and Peru—February 2021. Available online: https://data.unhcr.org/en/documents/details/85361 (accessed on 25 February 2023).
- Schweitzer, R.; Melville, F.; Steel, Z.; Lacherez, P. Trauma, Post-Migration Living Difficulties, and Social Support as Predictors of Psychological Adjustment in Resettled Sudanese Refugees. Aust. N. Z. J. Psychiatry 2006, 40, 179–187. [Google Scholar] [CrossRef]
- Kavian, F.; Mehta, K.; Willis, E.; Mwanri, L.; Ward, P.; Booth, S. Migration, Stress and the Challenges of Accessing Food: An Exploratory Study of the Experience of Recent Afghan Women Refugees in Adelaide, Australia. Int. J. Environ. Res. Public Health 2020, 17, 1379. [Google Scholar] [CrossRef]
- Berggreen-Clausen, A.; Hseing Pha, S.; Mölsted Alvesson, H.; Andersson, A.; Daivadanam, M. Food Environment Interactions after Migration: A Scoping Review on Low- and Middle-Income Country Immigrants in High-Income Countries. Public Health Nutr. 2022, 25, 136–158. [Google Scholar] [CrossRef]
- Fang, D.; Thomsen, M.R.; Nayga, R.M. The Association between Food Insecurity and Mental Health during the COVID-19 Pandemic. BMC Public Health 2021, 21, 607. [Google Scholar] [CrossRef]
- Firth, J.; Gangwisch, J.E.; Borsini, A.; Wootton, R.E.; Mayer, E.A. Food and Mood: How Do Diet and Nutrition Affect Mental Wellbeing? BMJ 2020, 369, m2382. [Google Scholar] [CrossRef] [PubMed]
- Bernal, J.; Frongillo, E.A.; Jaffe, K. Food Insecurity of Children and Shame of Others Knowing They Are without Food. J. Hunger Environ. Nutr. 2016, 11, 180–194. [Google Scholar] [CrossRef]
- Nanama, S.; Frongillo, E.A. Altered Social Cohesion and Adverse Psychological Experiences with Chronic Food Insecurity in the Non-Market Economy and Complex Households of Burkina Faso. Soc. Sci. Med. 2012, 74, 444–451. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, J.A.; Garcia, T.; Leung, C.W. Food Insecurity Is Associated with Depression, Anxiety, and Stress: Evidence from the Early Days of the COVID-19 Pandemic in the United States. Health Equity 2021, 5, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.D. Food Insecurity and Mental Health Status: A Global Analysis of 149 Countries. Am. J. Prev. Med. 2017, 53, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Pourmotabbed, A.; Moradi, S.; Babaei, A.; Ghavami, A.; Mohammadi, H.; Jalili, C.; Symonds, M.E.; Miraghajani, M. Food Insecurity and Mental Health: A Systematic Review and Meta-Analysis. Public Health Nutr. 2020, 23, 1778–1790. [Google Scholar] [CrossRef]
- Rashki Kemmak, A.; Nargesi, S.; Saniee, N. Social Determinant of Mental Health in Immigrants and Refugees: A Systematic Review. Med. J. Islam. Repub. Iran 2021, 35, 196. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística e Informática. Segunda Encuesta Dirigida a la Población Venezolana que Reside en el País. II ENPOVE 2021–2022. Ficha Técnica; Instituto Nacional de Estadística e Informática: Lima, Peru, 2022; Available online: https://www.inei.gob.pe/media/encuestas/documentos/enpove/Ficha_Tecnica_2022_enpove.pdf (accessed on 14 February 2023).
- Cafiero, C.; Viviani, S.; Nord, M. Food Security Measurement in a Global Context: The Food Insecurity Experience Scale. Measurement 2018, 116, 146–152. [Google Scholar] [CrossRef]
- Food and Agriculture Organization of the United Nations SDG Indicator 2.1.2—Using the Food Insecurity Experience Scale (FIES). Lesson 3: Statistical Validation of FIES Data. Available online: https://elearning.fao.org/pluginfile.php/491591/mod_scorm/content/5/story_content/external_files/SDG2.1.2_lesson3.pdf (accessed on 1 May 2023).
- Cafiero, C.; Viviani, S.; Nord, M. RM. Weights: Weighted Rasch Modeling and Extensions Using Conditional Maximum Likelihood. 2018. Available online: https://cran.r-project.org/package=RM.weights (accessed on 25 February 2023).
- Food and Agriculture Organization of the United Nations SDG Indicator 2.1.2—Using the Food Insecurity Experience Scale (FIES). Lesson 4: Using FIES Data to Calculate Food Insecurity Prevalence Rates. Available online: https://elearning.fao.org/pluginfile.php/491591/mod_scorm/content/5/story_content/external_files/SDG2.1.2_lesson4.pdf (accessed on 1 May 2023).
- Jankhotkaew, J.; Chandrasiri, O.; Charoensit, S.; Vongmongkol, V.; Tangcharoensathien, V. Thailand Prevalence and Profile of Food Insecurity in Households with under Five Years Children: Analysis of 2019 Multi-Cluster Indicator Survey. Int. J. Environ. Res. Public Health 2022, 19, 5065. [Google Scholar] [CrossRef]
- Cañari-Casaño, J.L.; Cochachin-Henostroza, O.; Elorreaga, O.A.; Dolores-Maldonado, G.; Aquino-Ramírez, A.; Huaman-Gil, S.; Giribaldi-Sierralta, J.P.; Aparco, J.P.; Antiporta, D.A.; Penny, M.E. Social Predictors of Food Insecurity during the Stay-at-Home Order Due to the COVID-19 Pandemic in Peru. Results from a Cross-Sectional Web-Based Survey. MedRxiv 2021. [Google Scholar]
- Carle, A.C. Fitting Multilevel Models in Complex Survey Data with Design Weights: Recommendations. BMC Med. Res. Methodol. 2009, 9, 49. [Google Scholar] [CrossRef]
- Textor, J.; van der Zander, B.; Gilthorpe, M.S.; Liśkiewicz, M.; Ellison, G.T.H. Robust Causal Inference Using Directed Acyclic Graphs: The R Package ‘Dagitty’. Int. J. Epidemiol. 2017, 45, 1887–1894. [Google Scholar] [CrossRef]
- Jager, K.J.; Zoccali, C.; MacLeod, A.; Dekker, F.W. Confounding: What It Is and How to Deal with It. Kidney Int. 2008, 73, 256–260. [Google Scholar] [CrossRef]
- Alarcão, V.; Guiomar, S.; Oliveira, A.; Severo, M.; Correia, D.; Torres, D.; Lopes, C. Food Insecurity and Social Determinants of Health among Immigrants and Natives in Portugal. Food Secur. 2020, 12, 579–589. [Google Scholar] [CrossRef]
- Maury-Sintjago, E.; Rodríguez-Fernández, A.; García, D.E.; Parra-Flores, J. High Prevalence of Food Insecurity and Factors Associated with Haitian Immigrants in Southern Chile. J. Immigr. Minor. Health 2019, 21, 1436–1439. [Google Scholar] [CrossRef] [PubMed]
- Saint Ville, A.; Francis-Granderson, I.; Bhagwandeen, B.; Mohammed, M. Food Insecurity in Venezuelan Migrants in Trinidad and Tobago Using the Food Insecurity Experience Scale. Front. Public Health 2022, 10, 925813. [Google Scholar] [CrossRef] [PubMed]
- Mansour, R.; Liamputtong, P.; Arora, A. Prevalence, Determinants, and Effects of Food Insecurity among Middle Eastern and North African Migrants and Refugees in High-Income Countries: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 7262. [Google Scholar] [CrossRef] [PubMed]
- The United Nations Network on Migration towards Sustainable Food Systems: The Critical Role of Migrants. Available online: https://migrationnetwork.un.org/statements/towards-sustainable-food-systems-critical-role-migrants (accessed on 1 May 2023).
- Bromand, Z.; Temur-Erman, S.; Yesil, R.; Heredia Montesinos, A.; Aichberger, M.C.; Kleiber, D.; Schouler-Ocak, M.; Heinz, A.; Kastrup, M.C.; Rapp, M.A. Mental Health of Turkish Women in Germany: Resilience and Risk Factors. Eur. Psychiatry 2012, 27, S17–S21. [Google Scholar] [CrossRef]
- Heeren, M.; Wittmann, L.; Ehlert, U.; Schnyder, U.; Maier, T.; Müller, J. Psychopathology and Resident Status—Comparing Asylum Seekers, Refugees, Illegal Migrants, Labor Migrants, and Residents. Compr. Psychiatry 2014, 55, 818–825. [Google Scholar] [CrossRef] [PubMed]
- Leong, F.; Park, Y.S.; Kalibatseva, Z. Disentangling Immigrant Status in Mental Health: Psychological Protective and Risk Factors among Latino and Asian American Immigrants. Am. J. Orthopsychiatry 2013, 83, 361–371. [Google Scholar] [CrossRef]
- Chen, W.; Hall, B.J.; Ling, L.; Renzaho, A.M. Pre-Migration and Post-Migration Factors Associated with Mental Health in Humanitarian Migrants in Australia and the Moderation Effect of Post-Migration Stressors: Findings from the First Wave Data of the BNLA Cohort Study. Lancet Psychiatry 2017, 4, 218–229. [Google Scholar] [CrossRef]
- Bogic, M.; Ajdukovic, D.; Bremner, S.; Franciskovic, T.; Galeazzi, G.M.; Kucukalic, A.; Lecic-Tosevski, D.; Morina, N.; Popovski, M.; Schützwohl, M.; et al. Factors Associated with Mental Disorders in Long-Settled War Refugees: Refugees from the Former Yugoslavia in Germany, Italy and the UK. Br. J. Psychiatry 2012, 200, 216–223. [Google Scholar] [CrossRef]
- Correa-Velez, I.; Gifford, S.M.; McMichael, C.; Sampson, R. Predictors of Secondary School Completion Among Refugee Youth 8 to 9 Years After Resettlement in Melbourne, Australia. J. Int. Migr. Integr. 2017, 18, 791–805. [Google Scholar] [CrossRef]
- Beiser, M.; Hou, F. Mental Health Effects of Premigration Trauma and Postmigration Discrimination on Refugee Youth in Canada. J. Nerv. Ment. Dis. 2016, 204, 464–470. [Google Scholar] [CrossRef]
- Shedlin, M.G.; Decena, C.U.; Noboa, H.; Betancourt, Ó. Sending-Country Violence and Receiving-Country Discrimination: Effects on the Health of Colombian Refugees in Ecuador. J. Immigr. Minor. Health 2014, 16, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Allsopp, J.; Sigona, N.; Phillimore, J. Poverty among Refugees and Asylum Seekers in the UK: An Evidence and Policy Review; University of Birmingham, Institute for Research into Superdiversity Birmingham: Birmingham, UK, 2014. [Google Scholar]
- Porter, M.; Haslam, N. Predisplacement and Postdisplacement Factors Associated with Mental Health of Refugees and Internally Displaced Persons: A Meta-Analysis. JAMA 2005, 294, 602. [Google Scholar] [CrossRef] [PubMed]
- Bakker, L.; Dagevos, J.; Engbersen, G. The Importance of Resources and Security in the Socio-Economic Integration of Refugees. A Study on the Impact of Length of Stay in Asylum Accommodation and Residence Status on Socio-Economic Integration for the Four Largest Refugee Groups in the Netherlands. J. Int. Migr. Integr. 2014, 15, 431–448. [Google Scholar]
- Hynie, M. The Social Determinants of Refugee Mental Health in the Post-Migration Context: A Critical Review. Can. J. Psychiatry 2018, 63, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Weaver, L.J.; Hadley, C. Moving Beyond Hunger and Nutrition: A Systematic Review of the Evidence Linking Food Insecurity and Mental Health in Developing Countries. Ecol. Food Nutr. 2009, 48, 263–284. [Google Scholar] [CrossRef]
- Maharaj, V.; Tomita, A.; Thela, L.; Mhlongo, M.; Burns, J.K. Food Insecurity and Risk of Depression Among Refugees and Immigrants in South Africa. J. Immigr. Minor. Health 2017, 19, 631–637. [Google Scholar] [CrossRef]
| Code | Question | Answer | Categorization |
|---|---|---|---|
| P110_1 | Does your household have: Color TV? | 1 Yes | 1 Yes |
| 2 No | 0 No | ||
| P110_2 | Does your household have: Gas stove? | 1 Yes | 1 Yes |
| 2 No | 0 No | ||
| P110_3 | Does your household have: Blender? | 1 Yes | 1 Yes |
| 2 No | 0 No | ||
| P110_4 | Does your household have: Electric iron? | 1 Yes | 1 Yes |
| 2 No | 0 No | ||
| P110_5 | Does your household have: Computer/laptop/tablet? | 1 Yes | 1 Yes |
| 2 No | 0 No | ||
| P110_7 | Does your household have: Landline phone? | 1 Yes | 1 Yes |
| 2 No | 0 No | ||
| P110_8 | Does your household have: Radio? | 1 Yes | 1 Yes |
| 2 No | 0 No | ||
| P110_9 | Does your household have: Refrigerator/freezer? | 1 Yes | 1 Yes |
| 2 No | 0 No | ||
| P110_10 | Does your household have: Washing machine? | 1 Yes | 1 Yes |
| 2 No | 0 No | ||
| P108_1 | Does the water you use at home come mainly from: | Public network, inside the house? | 1 Yes |
| Public network, outside the house, but inside the building? | 0 No | ||
| Pilon or pool for public use? | 0 No | ||
| Truck-tanker or other similar? | 0 No | ||
| Other? | 0 No | ||
| P108_2 | Is the bathroom or toilet in your home connected to: | Public drainage network inside the house? | 1 Yes |
| Public drainage network outside the home, but inside the building? | 0 No | ||
| Latrine (with treatment)? | 0 No | ||
| Septic tank, septic tank or biodigester? | 0 No | ||
| Other? | 0 No | ||
| P108_4 | Does your home have internet service? | 1 Yes | 1 Yes |
| 2 No | 0 No | ||
| P102 | Is the predominant construction material for exterior walls: | Brick or cement block? | 1 Yes |
| Stone, ashlar with lime or cement? | 0 No | ||
| Adobe? | 0 No | ||
| Rammed earth? | 0 No | ||
| Quincha (cane with mud)? | 0 No | ||
| Stone with mud? | 0 No | ||
| Wood (pona, screw, etc.)? | 0 No | ||
| Plywood/calamine/mat? | 0 No | ||
| Other material? | 0 No | ||
| P103 | Is the predominant construction material in the roofs: | Reinforced concrete? | 1 Yes |
| Wood? | 0 No | ||
| Roof tiles? | 0 No | ||
| Calamine sheets, fiber cement or similar? | 0 No | ||
| Cane or mat with cake of mud or cement? | 0 No | ||
| Plywood/mat/reed? | 0 No | ||
| Straw, palm fronds, etc.? | 0 No | ||
| Other material? | 0 No | ||
| P104 | Is the predominant material in the floors: | Parquet or polished wood? | 1 Yes |
| Asphalt sheets, vinyl or similar? | 1 Yes | ||
| Tiles, terraces or similar? | 1 Yes | ||
| Wood (pona, screw, etc.)? | 0 No | ||
| Cement? | 0 No | ||
| Land? | 0 No | ||
| Other material? | 0 No | ||
| P105 | How many rooms in total does the house have, without counting the bathroom, kitchen, hallways, and garage? | Number of rooms | 1 More than one inhabitant per room 0 One or less than one inhabitant per room |
| P15 | Does anyone who came from Venezuela live in this home? (at least one person of Venezuelan nationality) | 1 Yes | |
| 2 No | |||
| P15_N | Number of people | Number of people |
| Characteristics | n | % (95% CI) | |
|---|---|---|---|
| Sex | |||
| Female | 3999 | 51.6 (50.7–52.6) | |
| Male | 3740 | 48.4 (47.4–49.3) | |
| Age group | |||
| 18 to 29 years | 3286 | 42.6 (41.1–44.0) | |
| 30 to 39 years | 2408 | 31.4 (30.1–32.7) | |
| 40 to 49 years | 1124 | 14.6 (13.6–15.5) | |
| 50 to more | 921 | 11.5 (10.7–12.4) | |
| Wealth index tertile | |||
| Lower | 2408 | 30.6 (28.6–32.7) | |
| Middle | 2668 | 34.0 (32.0–36.1) | |
| Higher | 2663 | 35.3 (33.1–37.6) | |
| Educational level | |||
| Higher | 3265 | 43.1 (41.5–44.8) | |
| Secondary | 3451 | 43.9 (42.3–45.7) | |
| Up to primary | 1023 | 12.9 (11.7–14.2) | |
| Worked the last week | |||
| No | 1900 | 24.1 (23.1–25.2) | |
| Yes | 5839 | 75.9 (74.8–76.9) | |
| Health Insurance | |||
| No | 6293 | 80.8 (79.4–82.1) | |
| Yes | 1446 | 19.2 (17.9–20.7) | |
| Rented house | |||
| No | 476 | 6.4 (5.5–7.5) | |
| Yes | 7263 | 93.6 (92.5–94.5) | |
| Children under 5 in the household | |||
| No | 4931 | 63.3 (61.3–65.4) | |
| Yes | 2808 | 36.7 (34.6–38.7) | |
| Older adults in the household | |||
| No | 6838 | 88.8 (87.2–90.2) | |
| Yes | 901 | 11.2 (9.8–12.8) | |
| Household size | |||
| 1 person | 697 | 8.9 (8.1–9.7) | |
| 2 to 5 persons | 5754 | 73.6 (71.5–75.6) | |
| 6 or more persons | 1288 | 17.5 (15.5–19.7) | |
| Mental health problem | |||
| No | 7140 | 92.0 (90.9–92.9) | |
| Yes | 599 | 7.9 (7.0–9.0) | |
| Household food insecurity | |||
| Food security | 1878 | 24.3 (22.4–26.3) | |
| Mild | 2721 | 34.8 (32.8–36.9) | |
| Moderate to severe | 3140 | 40.9 (38.7–43.2) | |
| Characteristics | Mental Health Problem in the Last Month | p-Value | ||
|---|---|---|---|---|
| No (n = 7140) n (%) | Yes (n = 599) n (%) | |||
| Sex | <0.001 | |||
| Female | 3617 (90.1) | 382 (9.9) | ||
| Male | 3523 (94.1) | 217 (5.9) | ||
| Age group | 0.079 | |||
| 18 to 29 years | 3028 (92.3) | 258 (7.7) | ||
| 30 to 39 years | 2237 (92.9) | 171 (7.1) | ||
| 40 to 49 years | 1022 (89.8) | 102 (10.2) | ||
| 50 to more | 853 (91.4) | 68 (8.6) | ||
| Wealth index tertile | 0.496 | |||
| Lower | 2230 (92.6) | 178 (7.4) | ||
| Middle | 2443 (91.4) | 225 (8.7) | ||
| Higher | 2467 (92.1) | 196 (7.9) | ||
| Educational level | <0.001 | |||
| Higher | 2956 (90.2) | 309 (9.8) | ||
| Secondary | 3226 (93.4) | 225 (6.6) | ||
| Up to primary | 958 (93.3) | 65 (6.7) | ||
| Worked the last week | 0.018 | |||
| No | 1723 (90.6) | 177 (9.4) | ||
| Yes | 5417 (92.5) | 422 (7.5) | ||
| Health Insurance | ||||
| No | 5803 (91.9) | 490 (8.1) | 0.414 | |
| Yes | 1337 (92.7) | 109 (7.3) | ||
| Rented house | 0.074 | |||
| No | 446 (94.4) | 30 (5.6) | ||
| Yes | 6694 (91.9) | 569 (8.1) | ||
| Children under 5 in the household | 0.87 | |||
| No | 4559 (92.1) | 372 (7.9) | ||
| Yes | 2581 (91.9) | 227 (8.1) | ||
| Older adults in the household | 0.259 | |||
| No | 6315 (92.3) | 523 (7.8) | ||
| Yes | 825 (90.2) | 76 (9.8) | ||
| Household size | 0.187 | |||
| 1 person | 628 (89.7) | 69 (10.3) | ||
| 2 to 5 persons | 5321 (92.1) | 433 (7.9) | ||
| 6 or more persons | 1191 (92.7) | 97 (7.3) | ||
| Household food insecurity | <0.001 | |||
| Food security | 1782 (94.8) | 96 (5.3) | ||
| Mild | 2549 (93.6) | 172 (6.4) | ||
| Moderate to severe | 2809 (89.0) | 331 (10.9) | ||
| Characteristics | Food Insecurity in the Last Month | p-Value | |||
|---|---|---|---|---|---|
| No (n = 1878) n (%) | Mild (n = 2721) n (%) | Moderate to Severe (n = 3140) n (%) | |||
| Sex | 0.005 | ||||
| Female | 924 (23.1) | 1413 (34.9) | 1662 (41.9) | ||
| Male | 954 (25.5) | 1308 (34.7) | 1478 (39.8) | ||
| Age group | 0.379 | ||||
| 18 to 29 years | 811 (25.1) | 1133 (33.6) | 1342 (41.3) | ||
| 30 to 39 years | 561 (23.4) | 867 (35.7) | 980 (40.9) | ||
| 40 to 49 years | 281 (25.1) | 382 (33.7) | 461 (41.2) | ||
| 50 to more | 225 (22.4) | 339 (38.2) | 357 (39.4) | ||
| Wealth index tertile | <0.001 | ||||
| Lower | 372 (15.7) | 699 (28.0) | 1337 (56.3) | ||
| Middle | 555 (20.9) | 1014 (37.3) | 1099 (41.8) | ||
| Higher | 951 (34.9) | 1008 (38.3) | 704 (26.8) | ||
| Educational level | <0.001 | ||||
| Higher | 944 (29.7) | 1177 (35.5) | 1144 (34.8) | ||
| Secondary | 772 (21.7) | 1187 (34.1) | 1492 (44.2) | ||
| Up to primary | 162 (14.9) | 357 (34.7) | 504 (50.3) | ||
| Worked the last week | <0.001 | ||||
| No | 373 (19.3) | 621 (32.7) | 906 (47.9) | ||
| Yes | 1505 (25.9) | 2100 (35.5) | 2234 (38.7) | ||
| Health Insurance | <0.001 | ||||
| No | 1403 (21.9) | 2232 (35.1) | 2658 (42.9) | ||
| Yes | 475 (34.4) | 489 (33.4) | 482 (32.3) | ||
| Rented house | 0.098 | ||||
| No | 139 (28.8) | 171 (38.1) | 166 (33.0) | ||
| Yes | 1739 (23.9) | 2550 (34.6) | 2974 (41.5) | ||
| Children under 5 in the household | <0.001 | ||||
| No | 1349 (27.6) | 1717 (34.3) | 1865 (38.1) | ||
| Yes | 529 (18.6) | 1004 (35.6) | 1275 (45.8) | ||
| Older adults in the household | 0.048 | ||||
| No | 1681 (24.7) | 2357 (33.8) | 2800 (41.4) | ||
| Yes | 197 (20.7) | 364 (42.3) | 340 (37.0) | ||
| Household size | <0.001 | ||||
| 1 person | 244 (36.6) | 203 (28.5) | 250 (34.9) | ||
| 2 to 5 persons | 1405 (24.6) | 2072 (35.7) | 2277 (39.7) | ||
| 6 or more persons | 229 (16.7) | 446 (34.2) | 613 (49.1) | ||
| Mental health problem | <0.001 | ||||
| No | 1782 (25.0) | 2549 (35.4) | 2809 (39.6) | ||
| Yes | 96 (15.9) | 172 (27.8) | 331 (56.2) | ||
| Characteristics | Bivariate Analysis | Multiple Regression * | |||||
|---|---|---|---|---|---|---|---|
| PR | 95% CI | p-Value | PR | 95% CI | p-Value | ||
| Household food insecurity | |||||||
| Food security | Ref. | Ref. | |||||
| Mild | 1.18 | 0.88–1.57 | 0.259 | 1.22 | 0.92–1.63 | 0.169 | |
| Moderate to severe | 2.05 | 1.55–2.69 | <0.001 | 2.16 | 1.63–2.86 | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernández-Vásquez, A.; Visconti-Lopez, F.J.; Rojas-Cueva, A.C.; Grendas, L.N.; Azañedo, D. Food Insecurity and Mental Health among Venezuelan Migrants and Refugees Living in Peru: Secondary Data Analysis of a Cross-Sectional Survey. Nutrients 2023, 15, 3102. https://doi.org/10.3390/nu15143102
Hernández-Vásquez A, Visconti-Lopez FJ, Rojas-Cueva AC, Grendas LN, Azañedo D. Food Insecurity and Mental Health among Venezuelan Migrants and Refugees Living in Peru: Secondary Data Analysis of a Cross-Sectional Survey. Nutrients. 2023; 15(14):3102. https://doi.org/10.3390/nu15143102
Chicago/Turabian StyleHernández-Vásquez, Akram, Fabriccio J. Visconti-Lopez, Alexandra C. Rojas-Cueva, Leandro Nicolás Grendas, and Diego Azañedo. 2023. "Food Insecurity and Mental Health among Venezuelan Migrants and Refugees Living in Peru: Secondary Data Analysis of a Cross-Sectional Survey" Nutrients 15, no. 14: 3102. https://doi.org/10.3390/nu15143102
APA StyleHernández-Vásquez, A., Visconti-Lopez, F. J., Rojas-Cueva, A. C., Grendas, L. N., & Azañedo, D. (2023). Food Insecurity and Mental Health among Venezuelan Migrants and Refugees Living in Peru: Secondary Data Analysis of a Cross-Sectional Survey. Nutrients, 15(14), 3102. https://doi.org/10.3390/nu15143102







