Alterations in Dietary Behavior, Appetite Regulation, and Health-Related Quality of Life in Youth with Obesity in Germany during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Nutritional Behavior
2.3. Health-Related Quality of Life (HrQoL)
2.4. Data Analysis
3. Results
3.1. Cohort Characteristics
3.2. Eating Habits
3.2.1. Food Content and Food Frequency
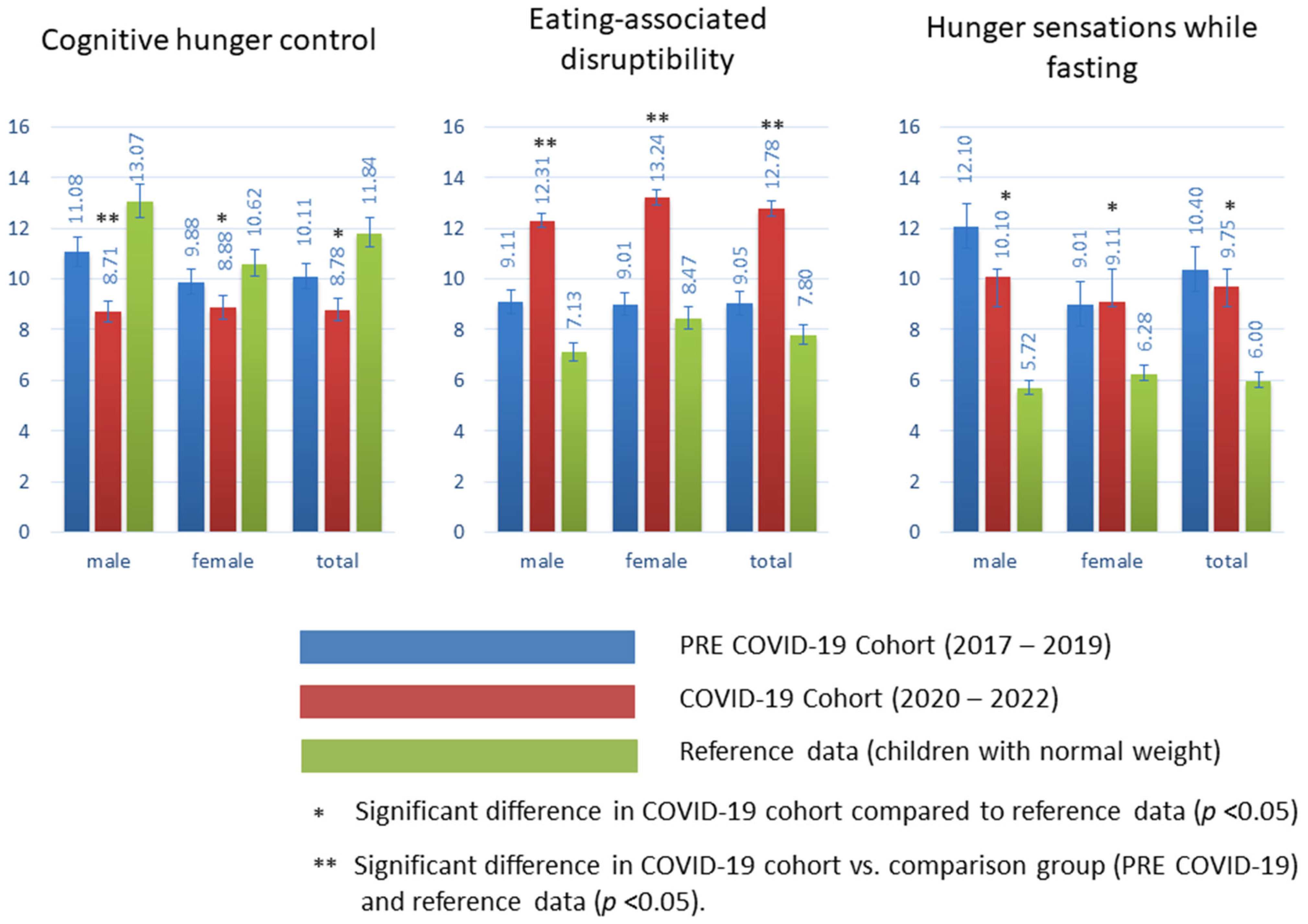
3.2.2. Nutritional Behavior
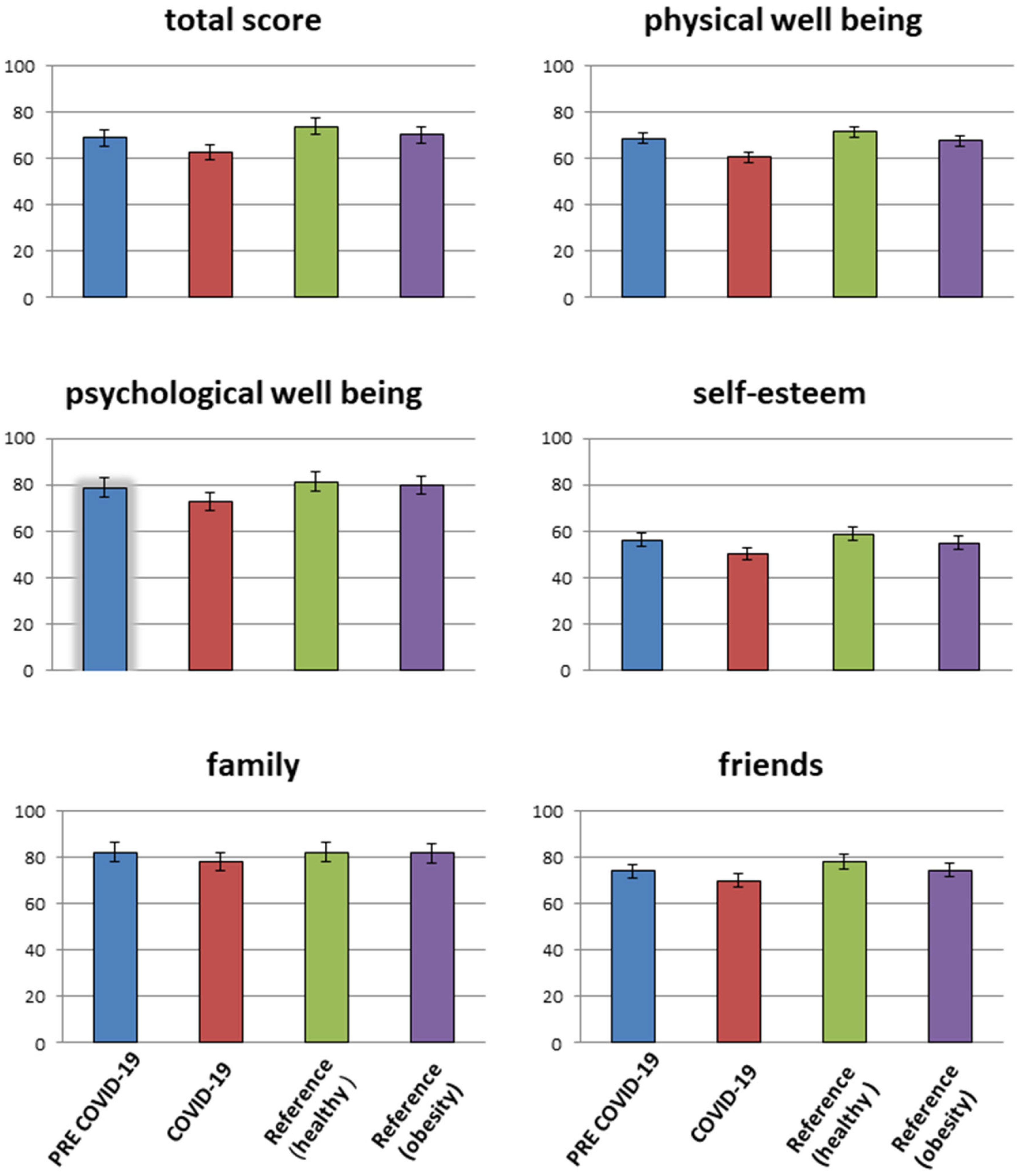
3.2.3. Health-Related Quality of Life (HR QoL)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SARS-CoV-2 | Severe-acute-respiratory-syndrome-related Coronavirus 2 |
| COVID-19 | Coronavirus disease 2019 |
| BMI | Body mass index |
| SDS | Standard deviation score |
| HrQoL | Health-related quality of life |
| HOMA | Homeostasis Model Assessment |
References
- Hosseini, S.H.; Jones, J.M.; Vatanparast, H. Association between Grain Intake, Nutrient Intake, and Diet Quality of Canadians: Evidence from the Canadian Community Health Survey–Nutrition 2015. Nutrients 2019, 11, 1937. [Google Scholar] [CrossRef]
- Kininmonth, A.R.; Smith, A.D.; Llewellyn, C.H.; Dye, L.; Lawton, C.L.; Fildes, A. The relationship between the home environment and child adiposity: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 4. [Google Scholar] [CrossRef]
- Oh, S.; Lee, S.Y.; Kim, D.-Y.; Woo, S.; Kim, Y.; Lee, H.-J.; Jang, H.B.; Park, S.I.; Park, K.H.; Lim, H. Association of Dietary Patterns with Weight Status and Metabolic Risk Factors among Children and Adolescents. Nutrients 2021, 13, 1153. [Google Scholar] [CrossRef]
- Grace, G.A.; Edward, S.; Gopalakrishnan, S. Dietary habits and obesity among adolescent school children: A case control study in an urban area of kancheepuram district. Indian J. Community Med. 2021, 46, 637–640. [Google Scholar] [CrossRef] [PubMed]
- Derks, I.P.M.; Sijbrands, E.J.G.; Wake, M.; Qureshi, F.; van der Ende, J.; Hillegers, M.H.J.; Jaddoe, V.W.V.; Tiemeier, H.; Jansen, P.W. Eating behavior and body composition across childhood: A prospective cohort study. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 96. [Google Scholar] [CrossRef] [PubMed]
- Davidson, T.L.; Jones, S.; Roy, M.; Stevenson, R.J. The Cognitive Control of Eating and Body Weight: It’s More Than What You “Think”. Front. Psychol. 2019, 10, 62. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, L.D.; Zuelch, M.L.; Dimitratos, S.M.; Scherr, R.E. Adolescent Obesity: Diet Quality, Psychosocial Health, and Cardiometabolic Risk Factors. Nutrients 2019, 12, 43. [Google Scholar] [CrossRef]
- Pearson, N.; Biddle, S.J.; Williams, L.; Worsley, A.; Crawford, D.; Ball, K. Adolescent television viewing and unhealthy snack food consumption: The mediating role of home availability of unhealthy snack foods. Public Health Nutr. 2014, 17, 317–323. [Google Scholar] [CrossRef]
- Marsh, S.; Ni Mhurchu, C.; Maddison, R. The non-advertising effects of screen-based sedentary activities on acute eating behaviours in children, adolescents, and young adults. A systematic review. Appetite 2013, 71, 259–273. [Google Scholar] [CrossRef]
- Nederkoorn, C.; Dassen, F.; Franken, L.; Resch, C.; Houben, K. Impulsivity and overeating in children in the absence and presence of hunger. Appetite 2015, 93, 57–61. [Google Scholar] [CrossRef]
- Loeber, S.; Grosshans, M.; Herpertz, S.; Kiefer, F.; Herpertz, S.C. Hunger modulates behavioral disinhibition and attention allocation to food-associated cues in normal-weight controls. Appetite 2013, 71, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Jebeile, H.; Kelly, A.S.; O’Malley, G.; Baur, L.A. Obesity in children and adolescents: Epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022, 10, 351–365. [Google Scholar] [CrossRef] [PubMed]
- Gil, E.G.; Fileh, S.; Miguel-Berges, M.L.; Aznar, L.A.M. Food portion sizes, obesity, and related metabolic complications in children and adolescents. Nutr. Hosp. 2021, 38, 169–176. [Google Scholar] [CrossRef]
- Tremmel, M.; Gerdtham, U.-G.; Nilsson, P.M.; Saha, S. Economic Burden of Obesity: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2017, 14, 435. [Google Scholar] [CrossRef] [PubMed]
- Handakas, E.; Lau, C.H.; Alfano, R.; Chatzi, V.L.; Plusquin, M.; Vineis, P.; Robinson, O. A systematic review of metabolomic studies of childhood obesity: State of the evidence for metabolic determinants and consequences. Obes. Rev. 2022, 23 (Suppl. S1), e13384. [Google Scholar] [CrossRef]
- Haraldstad, K.; Wahl, A.; Andenæs, R.; Andersen, J.R.; Andersen, M.H.; Beisland, E.; Borge, C.R.; Engebretsen, E.; Eisemann, M.; Halvorsrud, L.; et al. A systematic review of quality of life research in medicine and health sciences. Qual. Life Res. 2019, 28, 2641–2650. [Google Scholar] [CrossRef]
- Wu, X.Y.; Han, L.H.; Zhang, J.H.; Luo, S.; Hu, J.W.; Sun, K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS ONE 2017, 12, e0187668. [Google Scholar] [CrossRef]
- Haqq, A.M.; Kebbe, M.; Tan, Q.; Manco, M.; Salas, X.R. The Complexity and Stigma of Pediatric Obesity. Child. Obes. 2021, 17, 229–240. [Google Scholar] [CrossRef]
- Kenney, E.L.; Mozaffarian, R.S.; Ji, W.; Tucker, K.; Poole, M.K.; DeAngelo, J.; Bailey, Z.D.; Cradock, A.L.; Lee, R.M.; Frost, N. Moving from Policy to Practice for Early Childhood Obesity Prevention: A Nationwide Evaluation of State Implementation Strategies in Childcare. Int. J. Environ. Res. Public Health 2022, 19, 10304. [Google Scholar] [CrossRef]
- Available online: https://www.bundesgesundheitsministerium.de/coronavirus/chronik-coronavirus.html (accessed on 1 June 2023).
- Adıbelli, D.; Sümen, A. The effect of the coronavirus (COVID-19) pandemic on health-related quality of life in children. Child. Youth Serv. Rev. 2020, 119, 105595. [Google Scholar] [CrossRef]
- Truthmann, J.; Mensink, G.B.; Richter, A. Relative validation of the KiGGS Food Frequency Questionnaire among adolescents in Germany. Nutr. J. 2011, 10, 133. [Google Scholar] [CrossRef] [PubMed]
- Menrath, I.; Gminder, A.; Hiort, O.; Thyen, U. Gesundheitsbezogene Lebensqualität, Selbstwert und Gesundheitsverhalten durchschnittlich 6 Jahre nach einem ambulanten Adipositastherapieprogramm. Klin. Paediatr. 2017, 229, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Guthrie, C.A.; Sanderson, S.; Rapoport, L. Development of the Children’s Eating Behaviour Questionnaire. J. Child Psychol. Psychiatry 2001, 42, 963–970. [Google Scholar] [CrossRef] [PubMed]
- Pudel, V.; Westenhöfer, J. Fragebogen zum Essverhalten; Handanweisung; Hogrefe: Göttingen, Germany, 1989. [Google Scholar]
- Pudel, V. Bildung von Geschmackspräferenzen, Ernährung—Gewicht-Diät. Die Mythen und die Fakten. In Psychotherapie der Essstörungen: Krankheitsmodelle und Therapiepraxis störungsspezifisch—Schulenübergreifend, (Hrsg Günther Reich und Manfred Cierpka); 3te Auflage Georg Thieme Verlag Stuttgart: Stuttgart, Germany, 2010; pp. 11–12. [Google Scholar]
- Löffler, A.; Luck, T.; Then, F.S.; Luppa, M.; Sikorski, C.; Kovacs, P.; Tönjes, A.; Böttcher, Y.; Breitfeld, J.; Horstmann, A.; et al. Age- and gender-specific norms for the German version of the Three-Factor Eating-Questionnaire (TFEQ). Appetite 2015, 91, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Neuner, B.; Krampe, H.; McCarthy, W.J.; Reinke, S.; Kowalski, D.; Clausnizer, H.; Shneyder, M.; Rocke, A.; Nowak-Göttl, U. Psychometric Properties of a Modified KINDL-R Questionnaire for Adolescents and Adults, and Construction of a Brief Version, the KINDL-A(dult)B(rief) Questionnaire, KINDL-AB. Acta Haematol. 2018, 140, 1–9. [Google Scholar] [CrossRef]
- Erhart, M.; Ellert, U.; Kurth, B.-M.; Ravens-Sieberer, U. Measuring adolescents’ HRQoL via self reports and parent proxy reports: An evaluation of the psychometric properties of both versions of the KINDL-R instrument. Health Qual. Life Outcomes 2009, 7, 77. [Google Scholar] [CrossRef]
- Meixner, L.; Cohrdes, C.; Schienkiewitz, A.; Mensink, G.B.M. Health-related quality of life in children and adolescents with overweight and obesity: Results from the German KIGGS survey. BMC Public Health 2020, 20, 1722. [Google Scholar] [CrossRef]
- Tse, Y.; Darlington, A.-S.E.; Tyerman, K.; Wallace, D.; Pankhurst, T.; Chantziara, S.; Culliford, D.; Recio-Saucedo, A.; Nagra, A. COVID-19: Experiences of lockdown and support needs in children and young adults with kidney conditions. Pediatr. Nephrol. 2021, 36, 2797–2810. [Google Scholar] [CrossRef]
- McLoone, J.; Wakefield, C.E.; Marshall, G.M.; Pierce, K.; Jaffe, A.; Bye, A.; Kennedy, S.E.; Drew, D.; Lingam, R. It’s made a really hard situation even more difficult: The impact of COVID-19 on families of children with chronic illness. PLoS ONE 2022, 17, e0273622. [Google Scholar] [CrossRef]
- Logan, B.A. The impact of the COVID-19 pandemic on pediatric chronic illness groups. Brown Univ. Child Adolesc. Behav. Lett. 2022, 38, 1–4. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Erhart, M.; Devine, J.; Gilbert, M.; Reiss, F.; Barkmann, C.; Siegel, N.A.; Simon, A.M.; Hurrelmann, K.; Schlack, R.; et al. Child and Adolescent Mental Health During the COVID-19 Pandemic: Results of the Three-Wave Longitudinal COPSY Study. J. Adolesc. Health 2022, 71, 570–578. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, J.A.; Ashraf, A.P.; Becker, D.J.; Sen, B. Changes in Type 2 Diabetes Trends in Children and Adolescents During the COVID-19 Pandemic. J. Clin. Endocrinol. Metab. 2022, 107, e2777–e2782. [Google Scholar] [CrossRef] [PubMed]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Pujia, R.; Ferro, Y.; Maurotti, S.; Khoory, J.; Gazzaruso, C.; Pujia, A.; Montalcini, T.; Mazza, E. The Effects of COVID-19 on the Eating Habits of Children and Adolescents in Italy: A Pilot Survey Study. Nutrients 2021, 13, 2641. [Google Scholar] [CrossRef]
- Mikkelsen, H.T.; Skarstein, S.; Helseth, S.; Småstuen, M.C.; Haraldstad, K.; Rohde, G. Health-related quality of life, health literacy and COVID-19-related worries of 16- to 17-year-old adolescents and parents one year into the pandemic: A cross-sectional study. BMC Public Health 2022, 22, 1321. [Google Scholar] [CrossRef]
- Vogel, M.; Meigen, C.; Sobek, C.; Ober, P.; Igel, U.; Körner, A.; Kiess, W.; Poulain, T. Well-being and COVID-19-related worries of German children and adolescents: A longitudinal study from pre-COVID to the end of lockdown in Spring 2020. JCPP Adv. 2021, 1, e12204. [Google Scholar] [CrossRef]
- Sundar, T.K.B.; Riiser, K.; Småstuen, M.C.; Opheim, R.; Løndal, K.; Glavin, K.; Helseth, S. Health-related quality of life among 13–14 year old adolescents with overweight−a mixed methods approach. Health Qual. Life Outcomes 2020, 18, 161. [Google Scholar] [CrossRef]
- Ferreira, L.N.; Pereira, L.N.; Brás, M.D.F.; Ilchuk, K. Quality of life under the COVID-19 quarantine. Qual. Life Res. 2021, 30, 1389–1405. [Google Scholar] [CrossRef]
- Wright, L.; Steptoe, A.; Fancourt, D. Are we all in this together? Longitudinal assessment of cumulative adversities by socioeconomic position in the first 3 weeks of lockdown in the UK. J. Epidemiol. Community Health 2020, 74, 683–688. [Google Scholar] [CrossRef]
| PRE-COVID-19 (June 2017–June 2019) | COVID-19 (June 2020–June 2022) | p * Values | |||||
|---|---|---|---|---|---|---|---|
| Sex | ♀ | ♂ | total | ♀ | ♂ | total | |
| N (%) | 138 (52.0) | 127 (48.2) | 265 | 125 (47.6) | 139 (52.6) | 264 | ns |
| Age (years) [mean ± SD] | 12.9 ± 4.1 | 13.4 ± 3.7 | 13.2 ± 4.0 | 13.3 ± 4.7 | 12.7 ± 4.2 | 13.0 ± 4.1 | ns |
| Height (cm) [mean ± SD] | 159.9 ± 11.4 | 168.1 ± 16.5 | 162.1 ± 12.0 | 161.5 ± 17.9 | ns | ||
| Height z score | 0.10 | 0.53 | 0.15 | 0.62 | ns | ||
| Weight (kg) [mean ± SD] | 72.7 ± 11.9 | 88.4 ± 27.1 | 79.7 ± 9.8 | 87.5 ± 11.2 | ns | ||
| Weight z score | 2.21 ± 0.27 | 2.34 ± 0.33 | 2.27 ± 0.35 | 2.33 ± 0.18 | 2.64 ± 0.19 | ns | |
| BMI (kg/m2) [mean ± SD] | 29.8 ± 3.7 | 32.8 ± 4.1 | 30.03 ± 2.9 | 33.4 ± 4.3 | ns | ||
| BMI z score | 2.22 ± 0.39 | 2.28 ± 0.29 | 2.44 ± 0.69 | 2.65 ± 0.47 | <0.05 | ||
| Migration status (n; %) | 87 (63,04) | 79 (62.20) | 166 (62.64) | 68 (54.42) | 83 (59.71 | 151 (57.20) | ns |
| Proportion non-caucasian (n; %) | 78 (56.50%) | 75 (37.95%) | 153 (50.94%) | 63 (50.4%) | 81 (58.27%) | 144 (54,54%) | ns |
| Daily screen time (minutes) [mean ± SD] | 288 ± 41 | 302 ± 47 | 292 ± 43 | 337 ± 39 | 351 ± 54 | 348 ± 47 | <0.01 |
| HOMA index [95% CI] | 3.1 [3.0; 3.7] | 2.9 [2.7; 4.1] | 3.2 [3.0; 4.6] | 3.5 [3.2; 4.4] | 4.2 [3.3; 5.1] | 3.8 [3.3; 5.2] | <0.01 |
| HbA1c (%; mmol/mol Hb) | 5.27; 34.1 | 5,34; 34.86 | 5.31; 34.54 | 5.42; 35.74 | 5.39; 35.41 | 5.40; 35.52 | ns |
| Cholesterol (mg/dL) [95% CI) | 204.1 [187.4; 219.3] | 194.2 [188.4; 222.2] | 198.5 [168.0; 214.5] | 207.2 [191.7; 229.5] | 212.4 [189.9; 231.4] | 208.8 [196.7; 219.5] | <0.01 |
| GPT (U/l) [95% CI] | 89.3 [56.7; 99.5] | 63.3 [44.1; 79.9] | 72.8 [51.2; 88.2] | 102.4 [66.3; 109.5] | 83.3 [67.7; 99.8] | 93.4 [61.8; 101.2] | <0.01 |
| Food Content | Pre-COVID-19 (June 2017–June 2019) N = 265 | COVID-19 (June 2020–June 2022) N = 264 | Comparison between Pre-COVID-19 and COVID-19 | |||
|---|---|---|---|---|---|---|
| Healthy Consumption Frequency n; % (95% CI) | Unhealthy Consumption Frequency n; % (95% CI) | Healthy Consumption Frequency n; % (95% CI) | Unhealthy Consumption Frequency n; % (95% CI) | P * (Healthy Consumption) | P * (Unhealthy Consumption) | |
| Soft drinks | 133; 50.3% (34.9–66.7%) | 132; 49.7% (31.3–64.1%) | 91; 34.5% (20.5–44.7%) | 173; 65.5% (51.3–87.5%) | <0.05 | <0.001 |
| Mineral water, tea, water | 183; 69.2% (51.8–80.2%) | 82; 30.8% (19.2–49.8%) | 133; 50.4% (37.0–67.8%) | 131; 49.6% (28.2–61.2%) | <0.05 | <0.001 |
| Milk, cocoa | 148; 55.9% (40.1–71.2%) | 117; 44.1% (26.3–57.7%) | 128; 48.4% (30.6–55.3%) | 136; 51.6% (41.8–60.0%) | ns | p < 0.05 |
| Yoghurt, buttermilk, curd | 129; 48.5% (34.1–59.8%) | 136; 51.5% (34.3–61.2%) | 133; 50.3% (37.9–66.7%) | 131; 49.7% (38.0–59.8%) | ns | ns |
| Cheese | 120; 45.3% (31.4–57.8%) | 145; 54.7% (37.9–72.5%) | 158; 59.8% (48.5–72.2%) | 106; 40.2% (31.2–57.8%) | <0.05 | <0.05 |
| Meat/suasages | 74; 27.8% (11.2–45.3%) | 191; 72.2% (56.4–87.8%) | 34; 12.8% (2.5–31.2%) | 230; 87.2% (62.9–95.4%) | <0.05 | <0.01 |
| Fish | 23; 8.7% (1.9–16.5%) | 242; 91.3% (84.8–99.9%) | 10; 3.7% (0.4–8.2%) | 254; 96.3% (82.8–99.9%) | <0.05 | ns |
| Mixed bar, white bread, rolls | 126; 47.4% (33.6–61.2%) | 139; 52.6% (33.1–63.7%) | 154; 58.4% (41.1–70.7%) | 110; 41.6% (37.9–66.0%) | ns | ns |
| Wholemeal bread, wholemeal rolls | 74; 27.8% (14.9–44.7%) | 191; 72.2% (57.9–82.1%) | 62; 23.5% (11.7–45.2%) | 202; 76.5% (57.2–82.1%) | ns | ns |
| Rice/pasta | 76; 28.7% (14.7–42.6%) | 189; 72.3% (56.2–88.2%) | 28; 10.7% (2.8–22.1%) | 236; 89.3 (76.7–98.6%) | ns | <0.05 |
| Fresh fruit | 100; 37.9% (19.9–44.3%) | 165; 62.1% (45.0–76.3%) | 166; 62.9% (45.1–78.5%) | 98; 37.1% (13.8–47.9%) | <0.05 | <0.05 |
| Vegetables/fresh/frozen) | 97; 36.5% (23.1–51.4%) | 168; 63.5% (44.2–71.9%) | 28; 10.5% (2.8–20.1%) | 236; 89.5% (77.6–98.4%) | <0.05 | <0.01 |
| Fast food/delivery food | 83, 31.2% (24.6–43.2%) | 182; 68.8% (58.3–77.8%) | 12; 4.7% (0.1–10.9%) | 252; 95.3% (87.8–99.9%) | <0.05 | <0.01 |
| Chocolate/sweets | 61; 22.9% (11.6– 30.2%) | 204; 77.1% (51.2–85.4%) | 21; 7.8% (3.2–16.4%) | 243; 92.2% (69.7–98.9%) | <0.05 | <0.001 |
| Chips, salty nuts, snack biscuits | 77; 28.9% (20.7–39.8%) | 188; 71.1% (59.9–78.5%) | 11; 4.2% (0.0–14.2%) | 253; 95.8% (87.3–99.9%) | <0.05 | <0.01 |
| Gummi bears, wine gum | 100; 37.8% (24.3–55.1%) | 165; 62.2% (47.2–73.0%) | 36; 13.8% (5.4–17.1%) | 228; 86.2% (78.0% -92.1%) | <0.05 | <0.01 |
| Cakes, tarts, biscuits | 145; 54.7% (39.8–70.1%) | 120; 45.3% (42.6–67.1%) | 208; 78.9% (66.1–88.4%) | 56; 21.1% (8.7–34.8%) | <0.05 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Struckmeyer, N.; Biester, T.; Kordonouri, O.; Weiner, C.; Sadeghian, E.; Guntermann, C.; Kapitzke, K.; Weiskorn, J.; Galuschka, L.; von Stuelpnagel, K.; et al. Alterations in Dietary Behavior, Appetite Regulation, and Health-Related Quality of Life in Youth with Obesity in Germany during the COVID-19 Pandemic. Nutrients 2023, 15, 2936. https://doi.org/10.3390/nu15132936
Struckmeyer N, Biester T, Kordonouri O, Weiner C, Sadeghian E, Guntermann C, Kapitzke K, Weiskorn J, Galuschka L, von Stuelpnagel K, et al. Alterations in Dietary Behavior, Appetite Regulation, and Health-Related Quality of Life in Youth with Obesity in Germany during the COVID-19 Pandemic. Nutrients. 2023; 15(13):2936. https://doi.org/10.3390/nu15132936
Chicago/Turabian StyleStruckmeyer, Nora, Torben Biester, Olga Kordonouri, Chantal Weiner, Evelin Sadeghian, Cathrin Guntermann, Kerstin Kapitzke, Jantje Weiskorn, Laura Galuschka, Kisa von Stuelpnagel, and et al. 2023. "Alterations in Dietary Behavior, Appetite Regulation, and Health-Related Quality of Life in Youth with Obesity in Germany during the COVID-19 Pandemic" Nutrients 15, no. 13: 2936. https://doi.org/10.3390/nu15132936
APA StyleStruckmeyer, N., Biester, T., Kordonouri, O., Weiner, C., Sadeghian, E., Guntermann, C., Kapitzke, K., Weiskorn, J., Galuschka, L., von Stuelpnagel, K., Meister, D., Lange, K., Danne, T., & Reschke, F. (2023). Alterations in Dietary Behavior, Appetite Regulation, and Health-Related Quality of Life in Youth with Obesity in Germany during the COVID-19 Pandemic. Nutrients, 15(13), 2936. https://doi.org/10.3390/nu15132936





