Association of Plant-Based Diet Indices and Abdominal Obesity with Mental Disorders among Older Chinese Adults
Abstract
1. Introduction
2. Methods
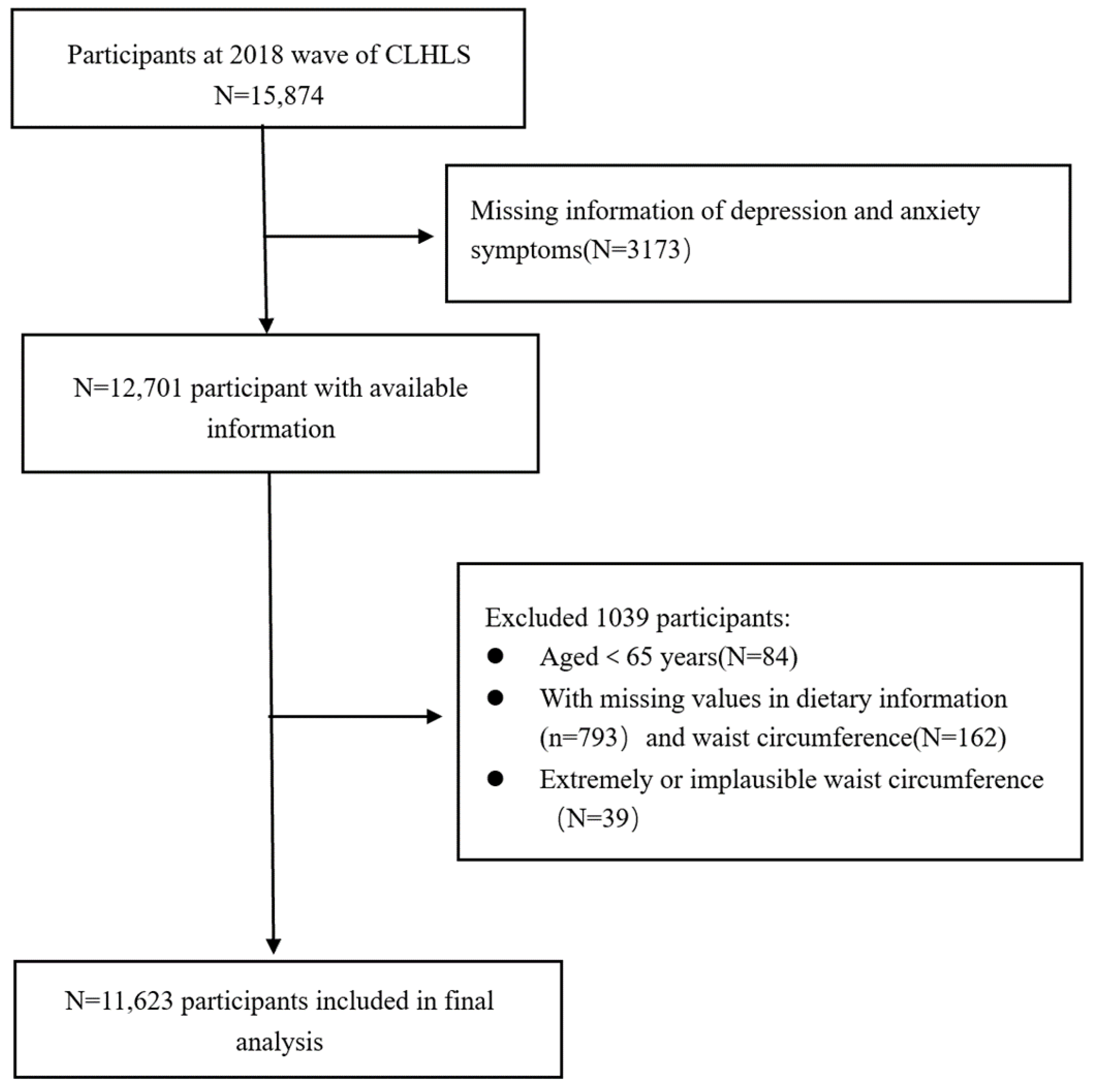
2.1. Data Sources and Study Population
2.2. Assessment of Abdominal Obesity
2.3. Calculation of Plant-Based Diet Indices
2.4. Assessment of Depression and Anxiety
2.5. Assessment of Covariates
2.6. Statistical Analysis
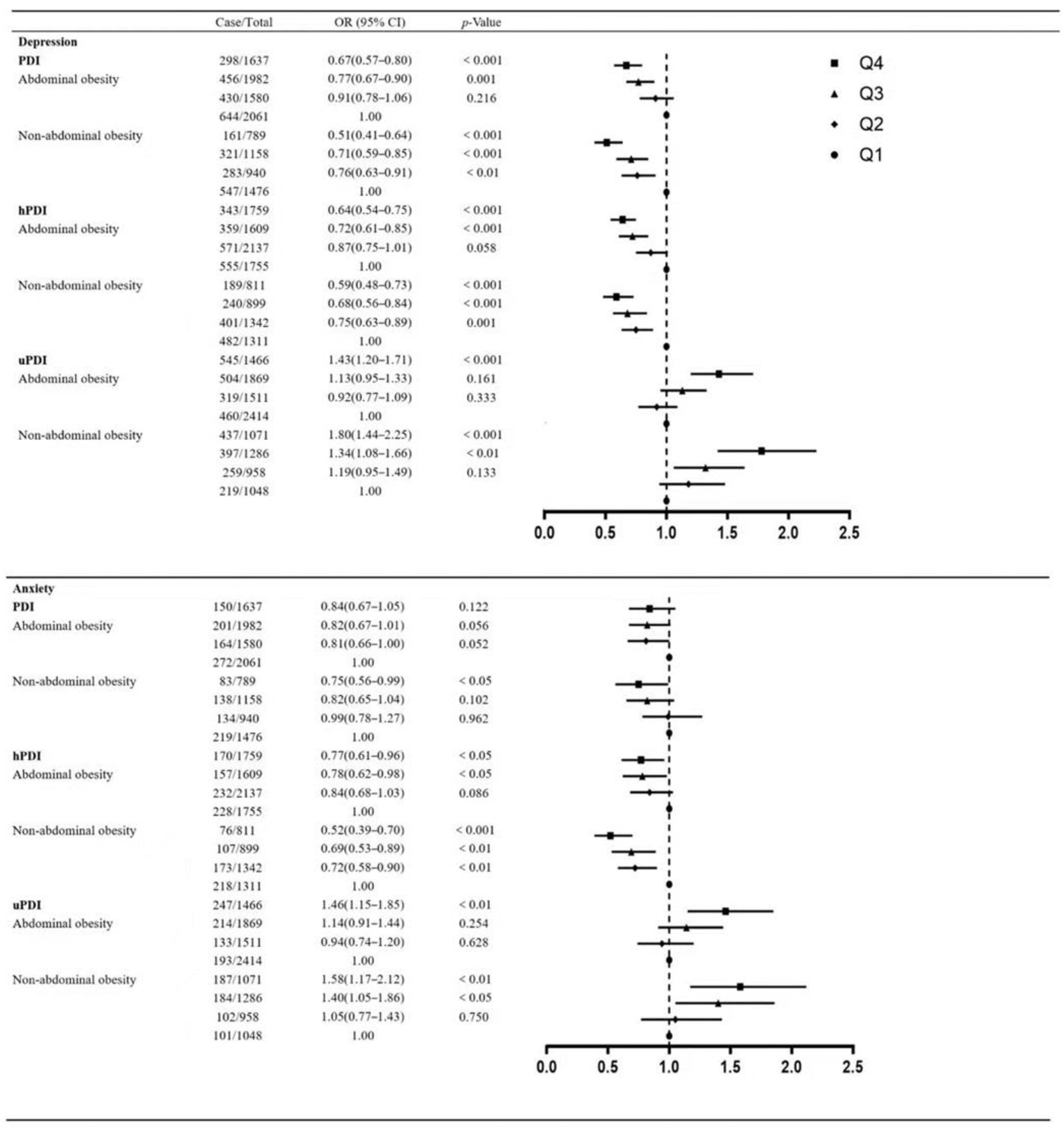
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chen, L.K. Urbanization and population aging: Converging trends of demographic transitions in modern world. Arch. Gerontol. Geriatr. 2022, 101, 104709. [Google Scholar] [CrossRef]
- Abdoli, N.; Salari, N.; Darvishi, N.; Jafarpour, S.; Solaymani, M.; Mohammadi, M.; Shohaimi, S. The global prevalence of major depressive disorder (MDD) among the elderly: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2022, 132, 1067–1073. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; He, H.; Yang, J.; Feng, X.; Zhao, F.; Lyu, J. Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. J. Psychiatr. Res. 2020, 126, 134–140. [Google Scholar] [CrossRef]
- Blazer, D.G. Depression in late life: Review and commentary. J. Gerontol. A Biol. Sci. Med. Sci. 2003, 58, 249–265. [Google Scholar] [CrossRef] [PubMed]
- Steel, Z.; Marnane, C.; Iranpour, C.; Chey, T.; Jackson, J.W.; Patel, V.; Silove, D. The global prevalence of common mental disorders: A systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 2014, 43, 476–493. [Google Scholar] [CrossRef] [PubMed]
- Malhi, G.S.; Mann, J.J. Depression. Lancet 2018, 392, 2299–2312. [Google Scholar] [CrossRef]
- Balsamo, M.; Cataldi, F.; Carlucci, L.; Fairfield, B. Assessment of anxiety in older adults: A review of self-report measures. Clin. Interv. Aging 2018, 13, 573–593. [Google Scholar] [CrossRef] [PubMed]
- Meng, R.; Yu, C.; Liu, N.; He, M.; Lv, J.; Guo, Y.; Bian, Z.; Yang, L.; Chen, Y.; Zhang, X.; et al. Association of Depression with All-Cause and Cardiovascular Disease Mortality Among Adults in China. JAMA Netw. Open 2020, 3, e1921043. [Google Scholar] [CrossRef] [PubMed]
- Kivimäki, M.; Lawlor, D.A.; Singh-Manoux, A.; Batty, G.D.; Ferrie, J.E.; Shipley, M.J.; Nabi, H.; Sabia, S.; Marmot, M.G.; Jokela, M. Common mental disorder and obesity: Insight from four repeat measures over 19 years: Prospective Whitehall II cohort study. BMJ 2009, 339, b3765. [Google Scholar] [CrossRef] [PubMed]
- Molendijk, M.; Molero, P.; Ortuño Sánchez-Pedreño, F.; Van Der Does, W.; Angel Martínez-González, M. Diet quality and depression risk: A systematic review and dose-response meta-analysis of prospective studies. J. Affect. Disord. 2018, 226, 346–354. [Google Scholar] [CrossRef]
- Lassale, C.; Batty, G.D.; Baghdadli, A.; Jacka, F.; Sánchez-Villegas, A.; Kivimäki, M.; Akbaraly, T. Healthy dietary indices and risk of depressive outcomes: A systematic review and meta-analysis of observational studies. Mol. Psychiatry 2019, 24, 965–986. [Google Scholar] [CrossRef] [PubMed]
- Aucoin, M.; Lachance, L.; Naidoo, U.; Remy, D.; Shekdar, T.; Sayar, N.; Cardozo, V.; Rawana, T.; Chan, I.; Cooley, K. Diet and Anxiety: A Scoping Review. Nutrients 2021, 13, 4418. [Google Scholar] [CrossRef] [PubMed]
- Grases, G.; Colom, M.A.; Sanchis, P.; Grases, F. Possible relation between consumption of different food groups and depression. BMC Psychol. 2019, 7, 14. [Google Scholar] [CrossRef]
- Parletta, N.; Zarnowiecki, D.; Cho, J.; Wilson, A.; Bogomolova, S.; Villani, A.; Itsiopoulos, C.; Niyonsenga, T.; Blunden, S.; Meyer, B.; et al. A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized controlled trial (HELFIMED). Nutr. Neurosci. 2019, 22, 474–487. [Google Scholar] [CrossRef]
- Sadeghi, O.; Keshteli, A.H.; Afshar, H.; Esmaillzadeh, A.; Adibi, P. Adherence to Mediterranean dietary pattern is inversely associated with depression, anxiety and psychological distress. Nutr. Neurosci. 2021, 24, 248–259. [Google Scholar] [CrossRef] [PubMed]
- López-Taboada, I.; González-Pardo, H.; Conejo, N.M. Western Diet: Implications for Brain Function and Behavior. Front. Psychol. 2020, 11, 564413. [Google Scholar] [CrossRef] [PubMed]
- Bu, T.; Tang, D.; Liu, Y.; Chen, D. Trends in Dietary Patterns and Diet-related Behaviors in China. Am. J. Health Behav. 2021, 45, 371–383. [Google Scholar] [CrossRef]
- Zhao, R.; Zhao, L.; Gao, X.; Yang, F.; Yang, Y.; Fang, H.; Ju, L.; Xu, X.; Guo, Q.; Li, S.; et al. Geographic Variations in Dietary Patterns and Their Associations with Overweight/Obesity and Hypertension in China: Findings from China Nutrition and Health Surveillance (2015–2017). Nutrients 2022, 14, 3949. [Google Scholar] [CrossRef]
- Baden, M.Y.; Liu, G.; Satija, A.; Li, Y.; Sun, Q.; Fung, T.T.; Rimm, E.B.; Willett, W.C.; Hu, F.B.; Bhupathiraju, S.N. Changes in Plant-Based Diet Quality and Total and Cause-Specific Mortality. Circulation 2019, 140, 979–991. [Google Scholar] [CrossRef]
- Loeb, S.; Fu, B.C.; Bauer, S.R.; Pernar, C.H.; Chan, J.M.; Van Blarigan, E.L.; Giovannucci, E.L.; Kenfield, S.A.; Mucci, L.A. Association of plant-based diet index with prostate cancer risk. Am. J. Clin. Nutr. 2022, 115, 662–670. [Google Scholar] [CrossRef]
- Gan, Z.H.; Cheong, H.C.; Tu, Y.K.; Kuo, P.H. Association between Plant-Based Dietary Patterns and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutrients 2021, 13, 3949. [Google Scholar] [CrossRef]
- Zhu, A.; Chen, H.; Shen, J.; Wang, X.; Li, Z.; Zhao, A.; Shi, X.; Yan, L.; Zeng, Y.; Yuan, C.; et al. Interaction between plant-based dietary pattern and air pollution on cognitive function: A prospective cohort analysis of Chinese older adults. Lancet Reg. Health-West. Pac. 2022, 20, 100372. [Google Scholar] [CrossRef]
- Liang, F.; Fu, J.; Turner-Mcgrievy, G.; Wang, Y.; Qiu, N.; Ding, K.; Zeng, J.; Moore, J.B.; Li, R. Association of Body Mass Index and Plant-Based Diet with Cognitive Impairment among Older Chinese Adults: A Prospective, Nationwide Cohort Study. Nutrients 2022, 14, 3132. [Google Scholar] [CrossRef]
- Kim, H.; Caulfield, L.E.; Garcia-Larsen, V.; Steffen, L.M.; Coresh, J.; Rebholz, C.M. Plant-Based Diets Are Associated with a Lower Risk of Incident Cardiovascular Disease, Cardiovascular Disease Mortality, and All-Cause Mortality in a General Population of Middle-Aged Adults. J. Am. Heart Assoc. 2019, 8, e012865. [Google Scholar] [CrossRef]
- Matsuda, M.; Shimomura, I. Increased oxidative stress in obesity: Implications for metabolic syndrome, diabetes, hypertension, dyslipidemia, atherosclerosis, and cancer. Obes. Res. Clin. Pract. 2013, 7, e330–e341. [Google Scholar] [CrossRef]
- Kinlen, D.; Cody, D.; O’shea, D. Complications of obesity. QJM 2018, 111, 437–443. [Google Scholar] [CrossRef]
- Dhawan, D.; Sharma, S. Abdominal Obesity, Adipokines and Non-communicable Diseases. J. Steroid. Biochem. Mol. Biol. 2020, 203, 105737. [Google Scholar] [CrossRef]
- Fulton, S.; Décarie-Spain, L.; Fioramonti, X.; Guiard, B.; Nakajima, S. The menace of obesity to depression and anxiety prevalence. Trends Endocrinol. Metab. 2022, 33, 18–35. [Google Scholar] [CrossRef]
- Chauvet-Gelinier, J.C.; Roussot, A.; Cottenet, J.; Brindisi, M.C.; Petit, J.M.; Bonin, B.; Vergès, B.; Quantin, C. Depression and obesity, data from a national administrative database study: Geographic evidence for an epidemiological overlap. PLoS ONE 2019, 14, e0210507. [Google Scholar] [CrossRef]
- He, Z.H.; Li, M.D.; Liu, C.J.; Ma, X.Y. Relationship between body image, anxiety, food-specific inhibitory control, and emotional eating in young women with abdominal obesity: A comparative cross-sectional study. Arch. Public Health 2021, 79, 11. [Google Scholar] [CrossRef]
- Luo, H.; Li, J.; Zhang, Q.; Cao, P.; Ren, X.; Fang, A.; Liao, H.; Liu, L. Obesity and the onset of depressive symptoms among middle-aged and older adults in China: Evidence from the CHARLS. BMC Public Health 2018, 18, 909. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Song, J.H.; Hwang, J.Y.; Ahn, K.; Kim, J.; Koh, Y.H.; Park, M.H.; Jo, S.A. Obesity and depressive symptoms in elderly Koreans: Evidence for the “Jolly Fat” hypothesis from the Ansan Geriatric (AGE) Study. Arch. Gerontol. Geriatr. 2010, 51, 231–234. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.B.; Ho, S.Y.; Chan, W.M.; Ho, K.S.; Li, M.P.; Leung, G.M.; Lam, T.H. Obesity and depressive symptoms in Chinese elderly. Int. J. Geriatr. Psychiatry 2004, 19, 68–74. [Google Scholar]
- Rivenes, A.C.; Harvey, S.B.; Mykletun, A. The relationship between abdominal fat, obesity, and common mental disorders: Results from the HUNT study. J. Psychosom. Res. 2009, 66, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Liao, W.; Luo, Z.; Hou, Y.; Cui, N.; Liu, X.; Huo, W.; Wang, F.; Wang, C. Age and gender specific association between obesity and depressive symptoms: A large-scale cross-sectional study. BMC Public Health 2020, 20, 1565. [Google Scholar] [CrossRef]
- Pouliot, M.C.; Després, J.P.; Lemieux, S.; Moorjani, S.; Bouchard, C.; Tremblay, A.; Nadeau, A.; Lupien, P.J. Waist circumference and abdominal sagittal diameter: Best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am. J. Cardiol. 1994, 73, 460–468. [Google Scholar] [CrossRef]
- Liu, E.; Feng, Y.; Yue, Z.; Zhang, Q.; Han, T. Differences in the health behaviors of elderly individuals and influencing factors: Evidence from the Chinese Longitudinal Healthy Longevity Survey. Int. J. Health Plan. Manag. 2019, 34, e1520–e1532. [Google Scholar] [CrossRef]
- Zeng, Y. Towards Deeper Research and Better Policy for Healthy Aging—Using the Unique Data of Chinese Longitudinal Healthy Longevity Survey. China Economic. J. 2012, 5, 131–149. [Google Scholar] [CrossRef]
- Zeng, Y.; Feng, Q.; Hesketh, T.; Christensen, K.; Vaupel, J.W. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: A cohort study. Lancet 2017, 389, 1619–1629. [Google Scholar] [CrossRef]
- Du, P.; Wang, H.J.; Zhang, B.; Qi, S.F.; Mi, Y.J.; Liu, D.W.; Tian, Q.B. Prevalence of abdominal obesity among Chinese adults in 2011. J. Epidemiol. 2017, 27, 282–286. [Google Scholar] [CrossRef]
- Chen, B.; Zeng, J.; Qin, M.; Xu, W.; Zhang, Z.; Li, X.; Xu, S. The Association between Plant-Based Diet Indices and Obesity and Metabolic Diseases in Chinese Adults: Longitudinal Analyses from the China Health and Nutrition Survey. Front. Nutr. 2022, 9, 881901. [Google Scholar] [CrossRef]
- Chen, Z.; Drouin-Chartier, J.P.; Li, Y.; Baden, M.Y.; Manson, J.E.; Willett, W.C.; Voortman, T.; Hu, F.B.; Bhupathiraju, S.N. Changes in Plant-Based Diet Indices and Subsequent Risk of Type 2 Diabetes in Women and Men: Three U.S. Prospective Cohorts. Diabetes Care 2021, 44, 663–671. [Google Scholar] [CrossRef]
- Yao, Y.; Chen, H.; Chen, L.; Ju, S.Y.; Yang, H.; Zeng, Y.; Gu, D.; Ng, T.P. Type of tea consumption and depressive symptoms in Chinese older adults. BMC Geriatr. 2021, 21, 331. [Google Scholar] [CrossRef]
- Yue, Z.; Liang, H.; Gao, X.; Qin, X.; Li, H.; Xiang, N.; Liu, E. The association between falls and anxiety among elderly Chinese individuals: The mediating roles of functional ability and social participation. J. Affect. Disord. 2022, 301, 300–306. [Google Scholar] [CrossRef]
- Ribeiro, S.M.L.; Malmstrom, T.K.; Morley, J.E.; Miller, D.K. Fruit and vegetable intake, physical activity, and depressive symptoms in the African American Health (AAH) study. J. Affect. Disord. 2017, 220, 31–37. [Google Scholar] [CrossRef]
- Dong, X.; Gu, Y.; Rayamajhi, S.; Thapa, A.; Meng, G.; Zhang, Q.; Liu, L.; Wu, H.; Zhang, S.; Zhang, T.; et al. Green tea consumption and risk of depressive symptoms: Results from the TCLSIH Cohort Study. J. Affect. Disord. 2022, 310, 183–188. [Google Scholar] [CrossRef]
- Hepsomali, P.; Groeger, J.A. Diet, Sleep, and Mental Health: Insights from the UK Biobank Study. Nutrients 2021, 13, 2573. [Google Scholar] [CrossRef]
- Shen, Y.C.; Chang, C.E.; Lin, M.N.; Lin, C.L. Vegetarian Diet Is Associated with Lower Risk of Depression in Taiwan. Nutrients 2021, 13, 1059. [Google Scholar] [CrossRef]
- Fox, M.E.; Lobo, M.K. The molecular and cellular mechanisms of depression: A focus on reward circuitry. Mol. Psychiatry 2019, 24, 1798–1815. [Google Scholar] [CrossRef]
- Suneson, K.; Lindahl, J.; Chamli Hårsmar, S.; Söderberg, G.; Lindqvist, D. Inflammatory Depression-Mechanisms and Non-Pharmacological Interventions. Int. J. Mol. Sci. 2021, 22, 1640. [Google Scholar] [CrossRef]
- González, R.; Ballester, I.; López-Posadas, R.; Suárez, M.D.; Zarzuelo, A.; Martínez-Augustin, O.; Sánchez De Medina, F. Effects of flavonoids and other polyphenols on inflammation. Crit. Rev. Food Sci. Nutr. 2011, 51, 331–362. [Google Scholar] [CrossRef]
- Ko, Y.H.; Kim, S.K.; Lee, S.Y.; Jang, C.G. Flavonoids as therapeutic candidates for emotional disorders such as anxiety and depression. Arch. Pharm. Res. 2020, 43, 1128–1143. [Google Scholar] [CrossRef] [PubMed]
- Poleszak, E.; Szewczyk, B.; Kedzierska, E.; Wlaź, P.; Pilc, A.; Nowak, G. Antidepressant-and anxiolytic-like activity of magnesium in mice. Pharmacol. Biochem. Behav. 2004, 78, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Bao, B.; Prasad, A.S.; Beck, F.W.; Fitzgerald, J.T.; Snell, D.; Bao, G.W.; Singh, T.; Cardozo, L.J. Zinc decreases C-reactive protein, lipid peroxidation, and inflammatory cytokines in elderly subjects: A potential implication of zinc as an atheroprotective agent. Am. J. Clin. Nutr. 2010, 91, 1634–1641. [Google Scholar] [CrossRef]
- King, L.E.; Osati-Ashtiani, F.; Fraker, P.J. Apoptosis plays a distinct role in the loss of precursor lymphocytes during zinc deficiency in mice. J. Nutr. 2002, 132, 974–979. [Google Scholar] [CrossRef] [PubMed]
- Sartori, S.B.; Whittle, N.; Hetzenauer, A.; Singewald, N. Magnesium deficiency induces anxiety and HPA axis dysregulation: Modulation by therapeutic drug treatment. Neuropharmacology 2012, 62, 304–312. [Google Scholar] [CrossRef]
- Wang, J.; Um, P.; Dickerman, B.A.; Liu, J. Zinc, Magnesium, Selenium and Depression: A Review of the Evidence, Potential Mechanisms and Implications. Nutrients 2018, 10, 584. [Google Scholar] [CrossRef]
- Calder, P.C.; Ahluwalia, N.; Brouns, F.; Buetler, T.; Clement, K.; Cunningham, K.; Esposito, K.; Jönsson, L.S.; Kolb, H.; Lansink, M.; et al. Dietary factors and low-grade inflammation in relation to overweight and obesity. Br. J. Nutr. 2011, 106 (Suppl. S3), S5–S78. [Google Scholar] [CrossRef]
- Lopez-Garcia, E.; Schulze, M.B.; Fung, T.T.; Meigs, J.B.; Rifai, N.; Manson, J.E.; Hu, F.B. Major dietary patterns are related to plasma concentrations of markers of inflammation and endothelial dysfunction. Am. J. Clin. Nutr. 2004, 80, 1029–1035. [Google Scholar] [CrossRef]
- Gomes, A.P.; Soares AL, G.; Menezes AM, B.; Assunção, M.C.; Wehrmeister, F.C.; Howe, L.D.; Gonçalves, H. Adiposity, depression and anxiety: Interrelationship and possible mediators. Rev. Saúde Pública 2019, 53, 103. [Google Scholar] [CrossRef]
- Zhao, G.; Ford, E.S.; Li, C.; Tsai, J.; Dhingra, S.; Balluz, L.S. Waist circumference, abdominal obesity, and depression among overweight and obese U.S. adults: National Health and Nutrition Examination Survey 2005–2006. BMC Psychiatry 2011, 11, 130. [Google Scholar] [CrossRef]
- Mulugeta, A.; Zhou, A.; Power, C.; Hyppönen, E. Obesity and depressive symptoms in mid-life: A population-based cohort study. BMC Psychiatry 2018, 18, 297. [Google Scholar] [CrossRef]
- Heidari-Beni, M.; Azizi-Soleiman, F.; Afshar, H.; Khosravi-Boroujeni, H.; Hassanzadeh Keshteli, A.; Esmaillzadeh, A.; Adibi, P. Relationship between obesity and depression, anxiety and psychological distress among Iranian health-care staff. East. Mediterr. Health J. 2021, 27, 327–335. [Google Scholar] [CrossRef]
- Crisp, A.H.; Mcguiness, B. Jolly fat: Relation between obesity and psychoneurosis in general population. Br. Med. J. 1976, 1, 7–9. [Google Scholar] [CrossRef]
- Lawlor, D.A.; Smith, G.D.; Ebrahim, S. Association of insulin resistance with depression: Cross sectional findings from the British Women’s Heart and Health Study. BMJ 2003, 327, 1383–1384. [Google Scholar] [CrossRef]
- Lipsett, D.; Madras, B.K.; Wurtman, R.J.; Munro, H.N. Serum tryptophan level after carbohydrate ingestion: Selective decline in non-albumin-bound tryptophan coincident with reduction in serum free fatty acids. Life Sci. 1973, 12, 57–64. [Google Scholar] [CrossRef]
- Bornstein, S.R.; Schuppenies, A.; Wong, M.L.; Licinio, J. Approaching the shared biology of obesity and depression: The stress axis as the locus of gene-environment interactions. Mol. Psychiatry 2006, 11, 892–902. [Google Scholar] [CrossRef]
- Andreyeva, T.; Puhl, R.M.; Brownell, K.D. Changes in perceived weight discrimination among Americans, 1995–1996 through 2004–2006. Obesity 2008, 16, 1129–1134. [Google Scholar] [CrossRef]
- Qian, J.; Li, N.; Ren, X. Obesity and depressive symptoms among Chinese people aged 45 and over. Sci. Rep. 2017, 7, 45637. [Google Scholar] [CrossRef]
- Joshi, S.; Mohan, V. Pros & cons of some popular extreme weight-loss diets. Indian J. Med. Res. 2018, 148, 642–647. [Google Scholar]
- Carnauba, R.A.; Chaves, D.F.; Baptistella, A.B.; Paschoal, V.; Naves, A.; Buehler, A.M. Association between high consumption of phytochemical-rich foods and anthropometric measures: A systematic review. Int. J. Food Sci. Nutr. 2017, 68, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Slavin, J.L.; Lloyd, B. Health benefits of fruits and vegetables. Adv. Nutr. 2012, 3, 506–516. [Google Scholar] [CrossRef] [PubMed]
- Marrone, G.; Guerriero, C.; Palazzetti, D.; Lido, P.; Marolla, A.; Di Daniele, F.; Noce, A. Vegan Diet Health Benefits in Metabolic Syndrome. Nutrients 2021, 13, 817. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.B.; Shivappa, N.; Hébert, J.R.; Page, A.J.; Gill, T.K.; Melaku, Y.A. Association between Dietary Inflammatory Index, Dietary Patterns, Plant-Based Dietary Index and the Risk of Obesity. Nutrients 2021, 13, 1536. [Google Scholar] [CrossRef]
- Millard, L.A.; Davies, N.M.; Tilling, K.; Gaunt, T.R.; Davey Smith, G. Searching for the causal effects of body mass index in over 300,000 participants in UK Biobank, using Mendelian randomization. PLoS Genet. 2019, 15, e1007951. [Google Scholar] [CrossRef]
| Characteristics | Total | Non-Depressed | Depressed | p-Value | Non-Anxiety | Anxiety | p-Value |
|---|---|---|---|---|---|---|---|
| N | 11,623 | 8483 (73.0) | 3140 (27.0) | 10,262 (88.3) | 1361 (11.7) | ||
| PDI score | 48.11 ± 5.50 | 48.55 ± 5.45 | 46.95 ± 5.47 | <0.001 | 48.22 ± 5.49 | 47.32 ± 5.48 | <0.001 |
| hPDI score | 46.66 ± 5.37 | 47.02 ± 5.33 | 45.68 ± 5.37 | <0.001 | 46.77 ± 5.33 | 45.79 ± 5.59 | <0.001 |
| uPDI score | 49.13 ± 6.92 | 48.44 ± 6.84 | 51.00 ± 6.79 | <0.001 | 48.86 ± 6.87 | 51.15 ± 6.97 | <0.001 |
| Abdominal obesity | 7260 (62.5) | 5432 (64.0) | 1828 (58.2) | <0.001 | 6473 (63.1) | 787 (57.8) | <0.001 |
| Age, years | 83.21 ± 10.98 | 82.72 ± 11.04 | 84.54 ± 10.71 | <0.001 | 83.26 ± 10.98 | 82.87 ± 11.01 | 0.188 |
| Sex, female | 6197 (53.3) | 4270 (50.3) | 1927 (61.4) | <0.001 | 5318 (51.8) | 879 (64.6) | <0.001 |
| Residence | <0.001 | <0.001 | |||||
| Urban | 2743 (23.6) | 2128 (25.1) | 615 (19.6) | 2498 (24.3) | 245 (18.0) | ||
| Town | 8880 (76.4) | 6355 (74.9) | 2525 (80.4) | 7764 (75.7) | 1116 (82.0) | ||
| Marital status | <0.001 | <0.01 | |||||
| Married/cohabitating | 5256 (45.2) | 4090 (48.2) | 1166 (37.1) | 4689 (45.7) | 567 (41.7) | ||
| Others | 6367 (54.8) | 4393 (51.8) | 1974 (62.9) | 5573 (54.3) | 794 (58.3) | ||
| Cohabitation status | <0.001 | 0.010 | |||||
| Solitude | 1946 (16.7) | 1280 (15.1) | 666 (21.2) | 1685 (16.4) | 261 (19.2) | ||
| Not living alone | 9677 (83.3) | 7203 (84.9) | 2474 (78.8) | 8577 (83.6) | 1100 (80.8) | ||
| Education | <0.001 | <0.001 | |||||
| Illiterate | 5309 (45.7) | 3521 (41.5) | 1788 (56.9) | 4545 (44.3) | 764 (56.1) | ||
| Primary | 3927 (33.8) | 3041 (35.8) | 886 (28.2) | 3533 (34.4) | 394 (28.9) | ||
| Secondary and above | 2387 (20.5) | 1921 (22.6) | 466 (14.8) | 2184 (21.3) | 203 (14.9) | ||
| Occupation | <0.001 | 0.001 | |||||
| Agricultural | 7287 (62.7) | 5156 (60.8) | 2131 (67.9) | 6380 (62.2) | 907 (66.6) | ||
| Others | 4336 (37.3) | 3327 (39.2) | 1009 (32.1) | 3882 (37.8) | 454 (33.4) | ||
| Economic situation | <0.001 | <0.001 | |||||
| Wealthy | 2424 (20.9) | 2051 (24.2) | 373 (11.9) | 2265 (22.1) | 159 (11.7) | ||
| Not wealthy | 9199 (79.1) | 6432 (75.8) | 2767 (88.1) | 7997 (77.9) | 1202 (88.3) | ||
| Sleep duration | <0.001 | <0.001 | |||||
| ≤6 h | 4398 (37.8) | 2678 (31.6) | 1720 (54.8) | 3616 (35.2) | 782 (57.5) | ||
| 7–8 h | 4345 (37.4) | 3495 (41.2) | 850 (27.1) | 4002 (39.0) | 343 (25.2) | ||
| ≥9 h | 2880 (24.8) | 2310 (27.2) | 570 (18.2) | 2644 (25.8) | 236 (17.3) | ||
| Smoking status | <0.001 | <0.001 | |||||
| Never | 7977 (68.6) | 5656 (66.7) | 2321 (73.9) | 6955 (67.8) | 1022 (75.1) | ||
| Former | 1761 (15.2) | 1364 (16.1) | 397 (12.6) | 1595 (15.5) | 166 (12.2) | ||
| Current | 1885 (16.2) | 1463 (17.2) | 422 (13.4) | 1712 (16.7) | 173 (12.7) | ||
| Alcohol consumption | <0.001 | <0.001 | |||||
| Never | 8467 (72.8) | 6052 (71.3) | 2415 (76.9) | 7410 (72.2) | 1057 (77.7) | ||
| Former | 1367 (11.8) | 1002 (11.8) | 365 (11.6) | 1209 (11.8) | 158 (11.6) | ||
| Current | 1789 (15.4) | 1429 (16.8) | 360 (11.5) | 1643 (16.0) | 146 (10.7) | ||
| Physical exercise | <0.001 | <0.001 | |||||
| Yes | 4049 (34.8) | 3339 (39.4) | 710 (22.6) | 3658 (35.6) | 391 (28.7) | ||
| No | 7574 (65.2) | 5144 (60.6) | 2430 (77.4) | 6604 (64.4) | 970 (71.3) | ||
| BMI (kg/m2) | <0.001 | <0.001 | |||||
| Underweight | 1720 (14.8) | 1121 (13.2) | 599 (19.1) | 1465 (14.3) | 255 (18.7) | ||
| Normal | 5985 (51.5) | 4365 (51.5) | 1620 (51.6) | 5297 (51.6) | 688 (50.6) | ||
| Overweight | 2901 (25.0) | 2231 (26.3) | 670 (21.3) | 2606 (25.4) | 295 (21.7) | ||
| Obese | 1017 (8.7) | 766 (9.0) | 251 (8.0) | 894 (8.7) | 123 (9.0) | ||
| Chronic disease | <0.001 | <0.001 | |||||
| Yes | 7005 (60.3) | 4951 (58.4) | 2054 (65.4) | 6101 (59.5) | 904 (66.4) | ||
| No | 4618 (39.7) | 3532 (41.6) | 1086 (34.6) | 4161 (40.5) | 457 (33.6) | ||
| Comorbidity | <0.001 | <0.001 | |||||
| Yes | 2947 (25.4) | 2009 (23.7) | 938 (29.9) | 2534 (24.7) | 413 (30.3) | ||
| No | 8676 (74.6) | 6474 (76.3) | 2202 (70.1) | 7728 (75.3) | 948 (69.7) | ||
| Sedentary leisure activities | <0.001 | <0.001 | |||||
| Yes | 7446 (64.1) | 5839 (68.8) | 1607 (51.2) | 6762 (65.9) | 684 (50.3) | ||
| No | 4177 (35.9) | 2644 (31.2) | 1533 (48.8) | 3500 (34.1) | 677 (49.7) | ||
| Active leisure activities | <0.001 | <0.05 | |||||
| Yes | 3717 (32.0) | 2939 (34.6) | 778 (24.8) | 3316 (32.3) | 401 (29.5) | ||
| No | 7906 (68.0) | 5544 (65.4) | 2362 (75.2) | 6946 (67.7) | 960 (70.5) |
| Q1 | Q2 | Q3 | Q4 | p for Trend | |
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |||
| PDI | |||||
| Cases/total | 1191/3537 | 713/2520 | 777/3140 | 459/2426 | |
| Model 1 a | 1.00 | 0.81 (0.72–0.90) | 0.69 (0.62–0.77) | 0.51 (0.45–0.58) | <0.001 |
| Model 2 b | 1.00 | 0.84 (0.75–0.94) | 0.73 (0.65–0.81) | 0.55 (0.48–0.62) | <0.001 |
| Model 3 c | 1.00 | 0.85 (0.76–0.96) | 0.75 (0.67–0.85) | 0.61 (0.54–0.70) | <0.001 |
| hPDI | |||||
| Cases/total | 1037/3066 | 972/3479 | 599/2508 | 532/2570 | |
| Model 1 | 1.00 | 0.80 (0.72–0.89) | 0.67 (0.59–0.75) | 0.57 (0.50–0.64) | <0.001 |
| Model 2 | 1.00 | 0.83 (0.74–0.92) | 0.71 (0.63–0.80) | 0.60 (0.53–0.68) | <0.001 |
| Model 3 | 1.00 | 0.82 (0.73–0.91) | 0.71 (0.63–0.81) | 0.62 (0.54–0.71) | <0.001 |
| uPDI | |||||
| Cases/total | 679/3462 | 578/2469 | 901/3155 | 982/2537 | |
| Model 1 | 1.00 | 1.18 (1.04–1.34) | 1.51 (1.33–1.70) | 2.30 (2.03–2.60) | <0.001 |
| Model 2 | 1.00 | 1.10 (0.97–1.26) | 1.35 (1.19–1.53) | 1.94 (1.71–2.21) | <0.001 |
| Model 3 | 1.00 | 1.02 (0.89–1.16) | 1.19 (1.04–1.36) | 1.55 (1.35–1.78) | <0.001 |
| Q1 | Q2 | Q3 | Q4 | p for Trend | |
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |||
| PDI | |||||
| Cases/total | 491/3537 | 298/2520 | 339/3140 | 233/2426 | |
| Model 1 a | 1.00 | 0.84 (0.72–0.99) | 0.76 (0.65–0.88) | 0.69 (0.58–0.81) | <0.001 |
| Model 2 b | 1.00 | 0.87 (0.74–1.02) | 0.79 (0.68–0.92) | 0.73 (0.61–0.86) | 0.001 |
| Model 3 c | 1.00 | 0.89 (0.76–1.05) | 0.83 (0.71–0.97) | 0.81 (0.68–0.96) | <0.05 |
| hPDI | |||||
| Cases/total | 446/3066 | 405/3479 | 264/2508 | 246/2570 | |
| Model 1 | 1.00 | 0.78 (0.67–0.90) | 0.71 (0.60–0.83) | 0.63 (0.54–0.75) | <0.001 |
| Model 2 | 1.00 | 0.80 (0.69–0.92) | 0.74 (0.63–0.87) | 0.66 (0.56–0.78) | <0.001 |
| Model 3 | 1.00 | 0.78 (0.67–0.91) | 0.74 (0.63–0.88) | 0.66 (0.56–0.79) | <0.001 |
| uPDI | |||||
| Cases/total | 294/3462 | 235/2469 | 398/3155 | 434/2537 | |
| Model 1 | 1.00 | 1.08 (0.90–1.30) | 1.44 (1.22–1.71) | 2.00 (1.68–2.37) | <0.001 |
| Model 2 | 1.00 | 1.03 (0.86–1.24) | 1.35 (1.14–1.61) | 1.80 (1.51–2.15) | <0.001 |
| Model 3 | 1.00 | 0.99 (0.82–1.20) | 1.25 (1.04–1.49) | 1.50 (1.25–1.80) | <0.001 |
| Non- Abdominal Obesity | Abdominal Obesity | ||
|---|---|---|---|
| OR (95% CI) | p-Value | ||
| Depression | |||
| Cases/total | 1312/4363 | 1828/7260 | |
| Model 1 a | 1.00 | 0.79 (0.72–0.86) | <0.001 |
| Model 2 b | 1.00 | 0.81 (0.74–0.88) | <0.001 |
| Model 3 c | 1.00 | 0.79 (0.72–0.87) | <0.001 |
| Anxiety | |||
| Cases/total | 574/4363 | 787/7260 | |
| Model 1 | 1.00 | 0.75 (0.67–0.84) | <0.001 |
| Model 2 | 1.00 | 0.77 (0.68–0.86) | <0.001 |
| Model 3 | 1.00 | 0.75 (0.66–0.85) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qi, R.; Sheng, B.; Zhou, L.; Chen, Y.; Sun, L.; Zhang, X. Association of Plant-Based Diet Indices and Abdominal Obesity with Mental Disorders among Older Chinese Adults. Nutrients 2023, 15, 2721. https://doi.org/10.3390/nu15122721
Qi R, Sheng B, Zhou L, Chen Y, Sun L, Zhang X. Association of Plant-Based Diet Indices and Abdominal Obesity with Mental Disorders among Older Chinese Adults. Nutrients. 2023; 15(12):2721. https://doi.org/10.3390/nu15122721
Chicago/Turabian StyleQi, Ran, Baihe Sheng, Lihui Zhou, Yanchun Chen, Li Sun, and Xinyu Zhang. 2023. "Association of Plant-Based Diet Indices and Abdominal Obesity with Mental Disorders among Older Chinese Adults" Nutrients 15, no. 12: 2721. https://doi.org/10.3390/nu15122721
APA StyleQi, R., Sheng, B., Zhou, L., Chen, Y., Sun, L., & Zhang, X. (2023). Association of Plant-Based Diet Indices and Abdominal Obesity with Mental Disorders among Older Chinese Adults. Nutrients, 15(12), 2721. https://doi.org/10.3390/nu15122721





