Healthy Eating for All? The Challenge of Adhering to Dietary Guidelines for Low-Income Groups in China
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Methods
2.2.1. Calculation of the Minimum Cost Diet
2.2.2. Affordability of Diets
2.2.3. Assessment of Dietary Nutrition Quality
3. Results
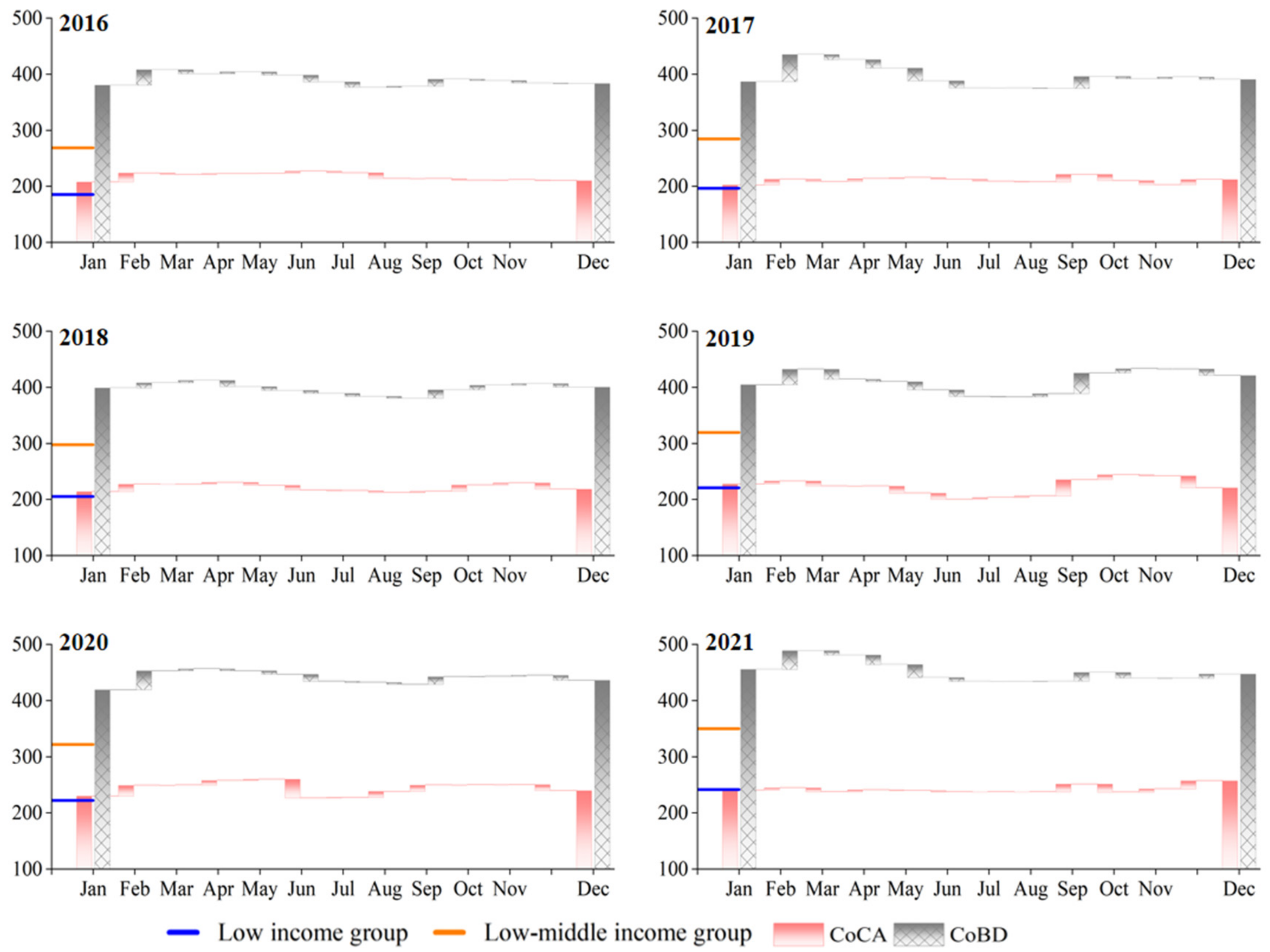
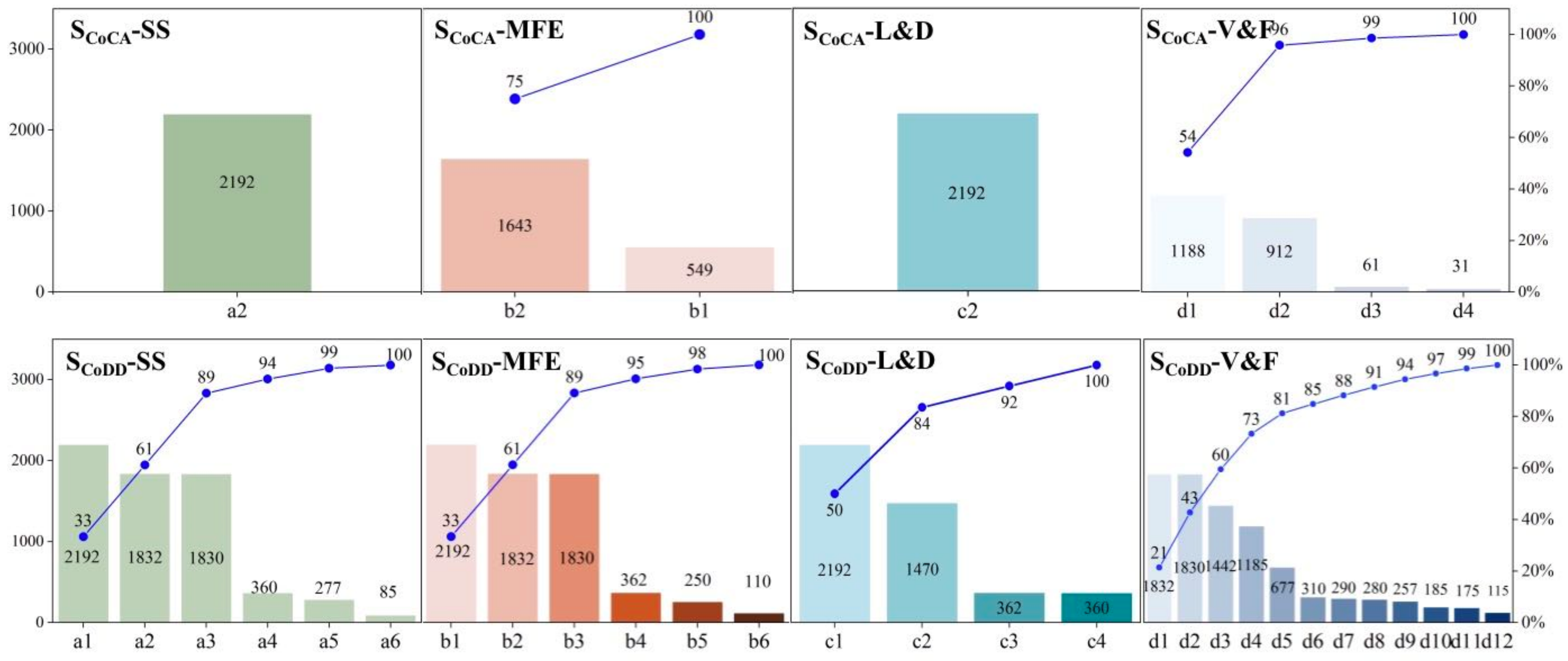
3.1. Dietary Affordability Assessment
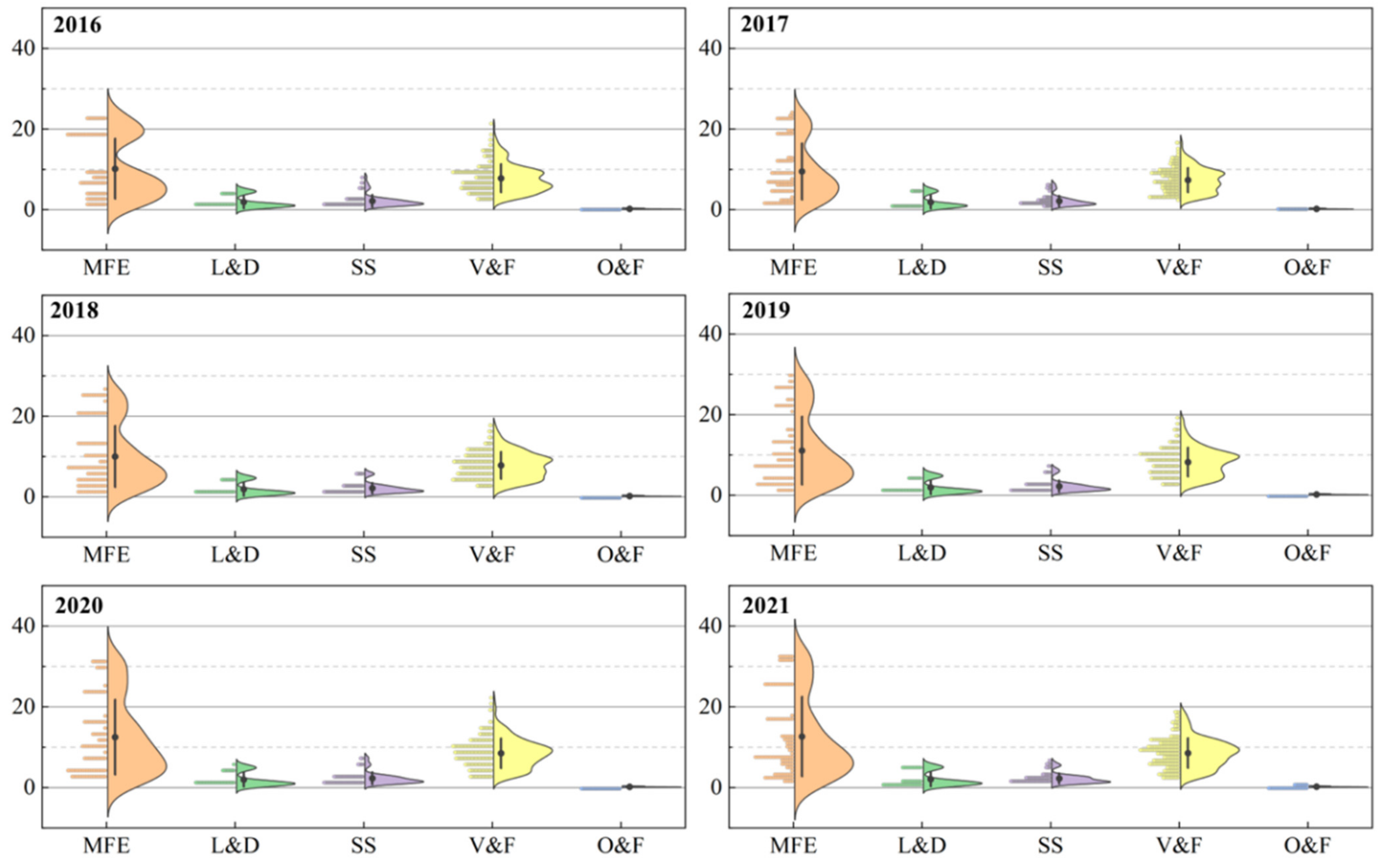
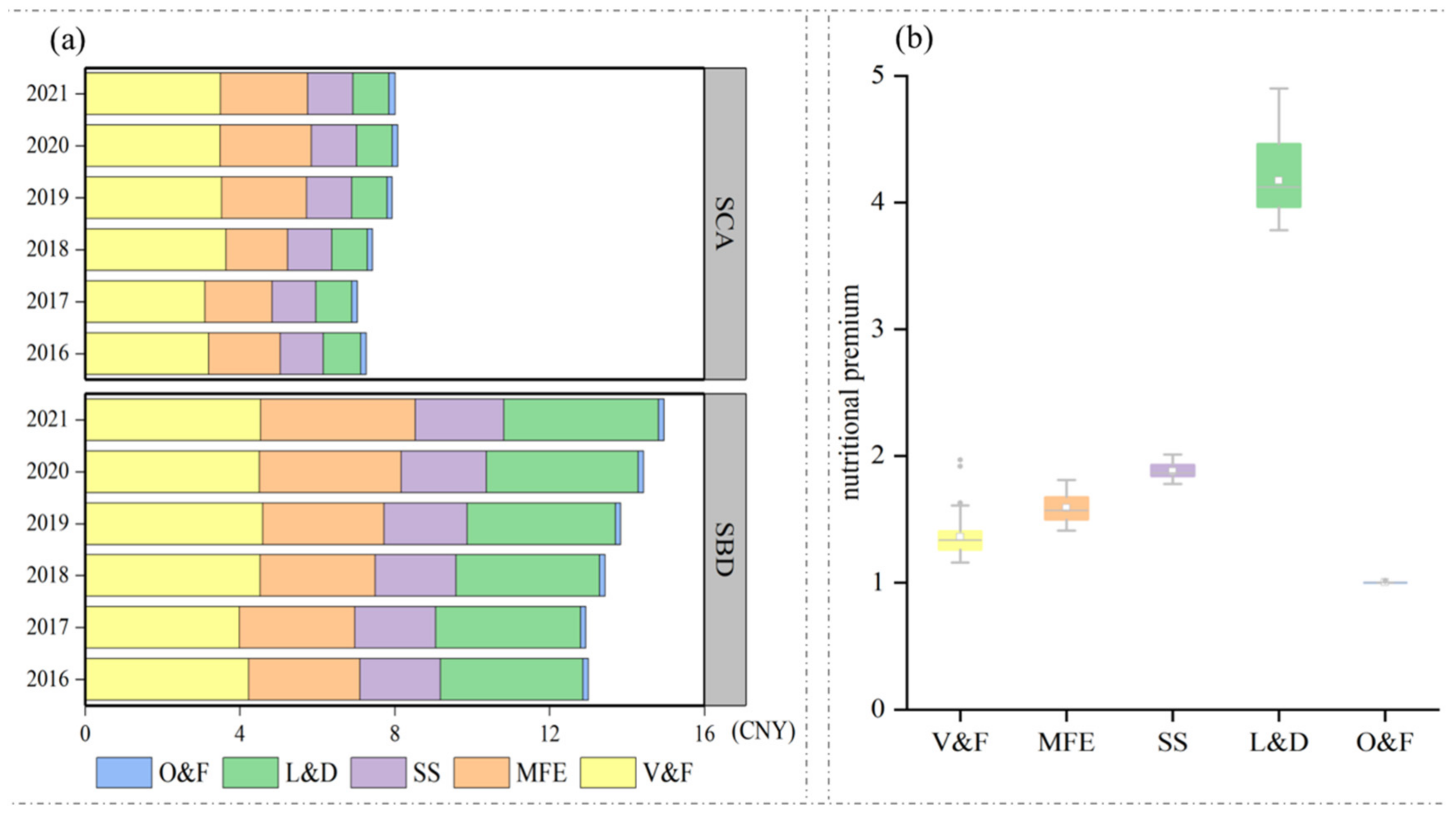
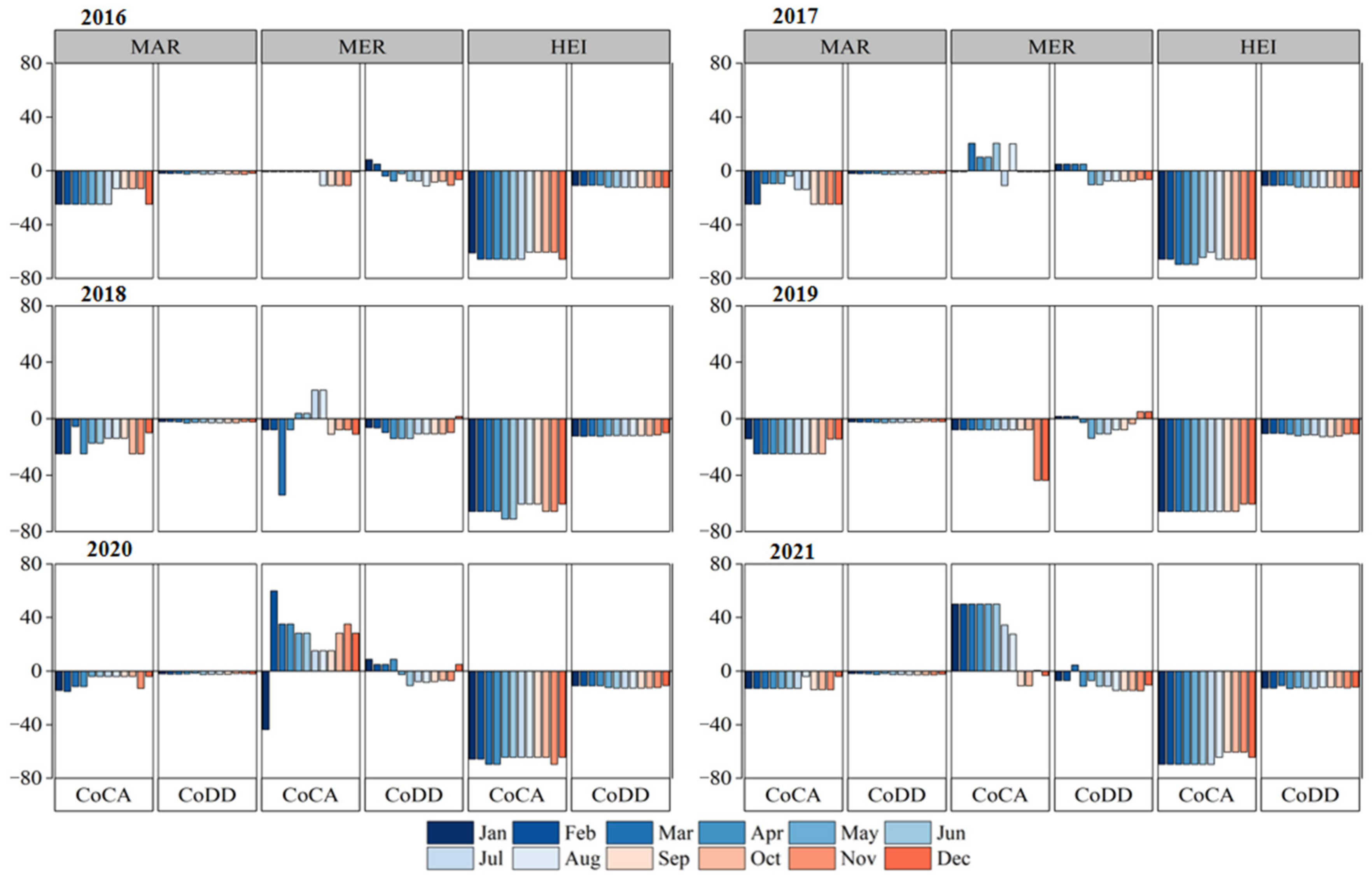
3.2. Dietary Composition Change
3.3. Dietary Nutrition Change
4. Discussion
4.1. Cost Differences of Diet Patterns
4.2. Policy Implications
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- FAO Rome. Declaration on World Food Security and World Food Summit Plan of Action; World Food Summit; FAO: Rome, Italy, 1996. [Google Scholar]
- Herforth, A.; Bai, Y.; Venkat, A.; Mahrt, K.; Ebel, A.; Masters, W.A. Cost and Affordability of Healthy Diets across and within Countries; Background Paper for the State of Food Security and Nutrition in the World 2020; FAO: Rome, Italy, 2020. [Google Scholar]
- Raghunathan, K.; Headey, D.; Herforth, A. Affordability of Nutritious Diets in Rural India. Food Policy 2021, 99, 101982. [Google Scholar] [CrossRef] [PubMed]
- Hirvonen, K.; Bai, Y.; Headey, D.; Masters, W.A. Affordability of the EAT–Lancet Reference Diet: A Global Analysis. Lancet Glob. Health 2020, 8, e59–e66. [Google Scholar] [CrossRef] [PubMed]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2020-Transforming Food Systems for Affordable Healthy Diets; FAO: Rome, Italy, 2020. [Google Scholar]
- Fan, S.; Si, W.; Zhang, Y. How to Prevent a Global Food and Nutrition Security Crisis under COVID-19? China Agric. Econ. Rev. 2020, 12, 471–480. [Google Scholar] [CrossRef]
- Akter, S. The Impact of COVID-19 Related ‘Stay-at-Home’ Restrictions on Food Prices in Europe: Findings from a Preliminary Analysis. Food Sec. 2020, 12, 719–725. [Google Scholar] [CrossRef] [PubMed]
- Headey, D.; Ruel, M. The COVID-19 Nutrition Crisis: What to Expect and How to Protect, IFPRI 2020. Available online: https://www.ifpri.org/blog/covid-19-nutrition-crisis-what-expect-and-how-protect (accessed on 7 February 2023).
- O’Connell, M.; Smith, K.; Stroud, R. The Dietary Impact of the COVID-19 Pandemic. J. Health Econ. 2022, 84, 102641. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Alemu, R.; Block, S.A.; Headey, D.; Masters, W.A. Cost and Affordability of Nutritious Diets at Retail Prices: Evidence from 177 Countries. Food Policy 2021, 99, 101983. [Google Scholar] [CrossRef]
- Headey, D.D.; Alderman, H.H. The Relative Caloric Prices of Healthy and Unhealthy Foods Differ Systematically across Income Levels and Continents. J. Nutr. 2019, 149, 2020–2033. [Google Scholar] [CrossRef]
- Masters, W.A.; Bai, Y.; Herforth, A.; Sarpong, D.B.; Mishili, F.; Kinabo, J.; Coates, J.C. Measuring the Affordability of Nutritious Diets in Africa: Price Indexes for Diet Diversity and the Cost of Nutrient Adequacy. Am. J. Agric. Econ. 2018, 100, 1285–1301. [Google Scholar] [CrossRef]
- Chastre, C.; Duffield, A.; Kindness, H.; LeJeune, S.; Taylor, A. The Minimum Cost of a Healthy Diet; Save the Children: London, UK, 2007. [Google Scholar]
- Beydoun, M.A.; Powell, L.M.; Chen, X.; Wang, Y. Food Prices Are Associated with Dietary Quality, Fast Food Consumption, and Body Mass Index among U. S. Children and Adolescents. J. Nutr. 2011, 141, 304–311. [Google Scholar] [CrossRef]
- Dizon, F.; Herforth, A.; Wang, Z. The Cost of a Nutritious Diet in Afghanistan, Bangladesh, Pakistan, and Sri Lanka. Glob. Food Secur. 2019, 21, 38–51. [Google Scholar] [CrossRef]
- Miller, V.; Yusuf, S.; Chow, C.K.; Dehghan, M.; Corsi, D.J.; Lock, K.; Popkin, B.; Rangarajan, S.; Khatib, R.; Lear, S.A.; et al. Availability, Affordability, and Consumption of Fruits and Vegetables in 18 Countries across Income Levels: Findings from the Prospective Urban Rural Epidemiology (PURE) Study. Lancet Glob. Health 2016, 4, e695–e703. [Google Scholar] [CrossRef] [PubMed]
- Clements, K.W.; Si, J. Engel’s Law, Diet Diversity, and the Quality of Food Consumption. Am. J. Agric. Econ. 2018, 100, 1–22. [Google Scholar] [CrossRef]
- Harris, J.; Tan, W.; Raneri, J.E.; Schreinemachers, P.; Herforth, A. Vegetables for Healthy Diets in Low- and Middle-Income Countries: A Scoping Review of the Food Systems Literature. Food Nutr. Bull. 2022, 43, 232–248. [Google Scholar] [CrossRef] [PubMed]
- Dolislager, M.; Liverpool-Tasie, L.S.O.; Mason, N.M.; Reardon, T.; Tschirley, D. Consumption of Healthy and Unhealthy Foods by the African Poor: Evidence from Nigeria, Tanzania, and Uganda. Agric. Econ. 2022, 53, 870–894. [Google Scholar] [CrossRef]
- Schneider, K.R.; Christiaensen, L.; Webb, P.; Masters, W.A. Assessing the Affordability of Nutrient-adequate Diets. Am. J. Agric. Econ. 2022, 105, 503–524. [Google Scholar] [CrossRef]
- Yin, J.; Zhang, X.; Huang, W.; Liu, L.; Zhang, Y.; Yang, D.; Hao, Y.; Chen, Y. The Potential Benefits of Dietary Shift in China: Synergies among Acceptability, Health, and Environmental Sustainability. Sci. Total Environ. 2021, 779, 146497. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Wang, Z.; Wang, H.; Zhao, L.; Jiang, H.; Zhang, B.; Ding, G. Nutrition Transition and Related Health Challenges over Decades in China. Eur. J. Clin. Nutr. 2021, 75, 247–252. [Google Scholar] [CrossRef]
- Chinese Nutrition Society. The Chinese Dietary Guidelines, 2022 ed.; People’s Medical Publishing House: Beijing, China, 2022; pp. 93–304. [Google Scholar]
- National Bureau of Statistics. China Urban Life and Price Yearbook; China Statistics Press: Beijing, China, 2013; pp. 38–41. [Google Scholar]
- Yang, Y. Chinese Food Composition Tables (Standard Edition) (Book 1); Peking University Medical Press: Beijing, China, 2019; pp. 27–226. [Google Scholar]
- Yang, Y. Chinese Food Composition Tables (Standard Edition) (Book 2); Peking University Medical Press.: Beijing, China, 2019; pp. 51–333. [Google Scholar]
- Stigler, G.J. The Cost of Subsistence. J. Farm Econ. 1945, 27, 303–314. [Google Scholar] [CrossRef]
- Bai, J.; Wang, L.; Wang, H.; Wang, Z.; Zhang, B. Intakes of energy and macronutrient from Chinese 15 provinces (autonomous regions and municipalities) adults aged 18 to 35 in 1989–2018. J. Hyg. Res. 2022, 51, 361–366+380. [Google Scholar] [CrossRef]
- Food Prices for Nutrition Technical Assistance Tools for Calculating the Cost of a Healthy Diet, Version 3.0. 2022. Available online: https://sites.tufts.edu/foodpricesfornutrition/tools/ (accessed on 20 September 2022).
- Ambikapathi, R.; Schneider, K.R.; Davis, B.; Herrero, M.; Winters, P.; Fanzo, J.C. Global Food Systems Transitions Have Enabled Affordable Diets but Had Less Favourable Outcomes for Nutrition, Environmental Health, Inclusion and Equity. Nat. Food 2022, 3, 764–779. [Google Scholar] [CrossRef]
- Li, L.; Bai, J.; Zhang, C. Impacts of Income on the Dietary Health of Chinese Rural Residents from the Perspective of Poverty-Line: Based on the China Nutrition and Health Survey Data. Res. Agric. Mod. 2020, 41, 93–103. [Google Scholar] [CrossRef]
- Yuan, Y.; Li, F.; Dong, R.; Chen, J.; He, G.; Li, S.; Chen, B. The Development of a Chinese Healthy Eating Index and Its Application in the General Population. Nutrients 2017, 9, 977. [Google Scholar] [CrossRef] [PubMed]
- Vieux, F.; Soler, L.; Touazi, D.; Darmon, N. High Nutritional Quality Is Not Associated with Low Greenhouse Gas Emissions in Self-Selected Diets of French Adults. Am. J. Clin. Nutr. 2013, 97, 569–583. [Google Scholar] [CrossRef]
- Perignon, M.; Sinfort, C.; El Ati, J.; Traissac, P.; Drogué, S.; Darmon, N.; Amiot, M.J.; Achir, N.; Alouane, L. How to Meet Nutritional Recommendations and Reduce Diet Environmental Impact in the Mediterranean Region? An Optimization Study to Identify More Sustainable Diets in Tunisia. Glob. Food Secur. 2019, 23, 227–235. [Google Scholar] [CrossRef]
- Chinese Nutrition Society. Chinese Dietary Nutrients Reference Intakes, 2013 ed.; China Science Press: Beijing China, 2014; pp. 652–658. [Google Scholar]
- Yu, X.; Liu, C.; Wang, H.; Feil, J. The Impact of COVID-19 on Food Prices in China: Evidence of Four Major Food Products from Beijing, Shandong and Hubei Provinces. China Agric. Econ. Rev. 2020, 12, 445–458. [Google Scholar] [CrossRef]
- Rozelle, S.; Rahimi, H.; Wang, H.; Dill, E. Lockdowns Are Protecting China’s Rural Families From COVID-19, But the Economic Burden Is Heavy. In COVID-19 and Global Food Security; International Food Policy Research Institute (IFPRI): Washington, DC, USA, 2020. [Google Scholar]
- Grosso, G.; Mateo, A.; Rangelov, N.; Buzeti, T.; Birt, C. Nutrition in the Context of the Sustainable Development Goals. Eur. J. Public Health 2020, 30, i19–i23. [Google Scholar] [CrossRef]
- FAO; WHO. Sustainable Healthy Diets—Guiding Principles; FAO: Rome, Italy, 2019. [Google Scholar]
- Biswas, A.K.; Tortajada, C. How China Eradicated Absolute Poverty? China Daily, 12 April 2021. Available online: https://www.chinadailyhk.com/article/a/162843#:~:text=Monday%2C%20April%2012%2C%202021%2C%2012%3A59%20By%20Asit%20K.,Brazil%20%28US%241%2C947.28%29%20and%2073%20percent%20of%20India%20%28US%24266.58%29. (accessed on 20 September 2022).
- Fanzo, J.; Haddad, L.; McLaren, R.; Marshall, Q.; Davis, C.; Herforth, A.; Jones, A.; Beal, T.; Tschirley, D.; Bellows, A.; et al. The Food Systems Dashboard Is a New Tool to Inform Better Food Policy. Nat. Food 2020, 1, 243–246. [Google Scholar] [CrossRef]
- Narayanan, S.; Saha, S. Urban Food Markets and the Lockdown in India; Indira Gandhi Institute of Development Research: New Delhi, India, 2020. [Google Scholar]
- Masters, W.A. COVID-19 Disruptions and Resilience of Retail Food Prices Around the World. 2020. Available online: https://poverty-action.org/recovr-study/covid-19-disruptions-and-resilience-retail-food-prices-around-world (accessed on 21 December 2022).
- The China Rural Work Conference. Available online: http://www.moa.gov.cn/ztzl/ncgzhy2015/zxdt/201512/t20151226_4966987.htm (accessed on 21 December 2022).
| Food Group Names | Recommended Consumption Group | Food Subgroup Names | Recommended Consumption Subgroup |
|---|---|---|---|
| Starchy staples (SS) | 250 | Refined cereals | 75 |
| Whole cereals and mixed beans | 100 | ||
| Tubers and roots | 75 | ||
| Vegetables and fruits (V&F) | 800 | Vegetables | 225 |
| Vegetables—DGLV or red/orange | 225 | ||
| Fruits | 300 | ||
| Meat, fish, and eggs (MFE) | 150 | Meat | 50 |
| Fish | 50 | ||
| Eggs | 50 | ||
| Legumes and dairy (L&D) | 325 | Dairy products | 300 |
| Legumes and nuts | 25 | ||
| Oils and fats (O&F) | 25 | Oils and fats | 25 |
| SCA (SBD), % | |||||
|---|---|---|---|---|---|
| SS | MFE | F&V | L&D | O&F | |
| Energy | 40.1 (39.9) | 16.6 (18.1) | 18.3 (17.4) | 13.6 (13.5) | 11.4 (11.1) |
| Protein | 43.4 (34.7) | 17.7 (34.7) | 8.3 (10.2) | 30.5 (20.4) | 0.0 (0.0) |
| Lipids | 7.6 (7.9) | 41.0 (38.0) | 1.5 (1.8) | 14.9 (17.8) | 35.0 (34.5) |
| Carbohydrate | 58.7 (60.9) | 0.7 (0.6) | 32.0 (29.7) | 8.5 (8.8) | 0.0 (0.0) |
| Dietary fiber | 0.0 (14.7) | 0.0 (0.0) | 48.2 (66.5) | 51.8 (18.8) | 0.0 (0.0) |
| Elements | |||||
| Calcium | 18.4 (16.0) | 12.7 (9.2) | 27.3 (25.4) | 40.8 (49.1) | 0.9 (0.2) |
| Phosphorus | 36.8 (36.5) | 14.1 (21.9) | 15.1 (13.1) | 33.8 (28.4) | 0.2 (0.1) |
| Magnesium | 24.6 (47.9) | 3.2 (7.5) | 35.3 (29.8) | 36.7 (14.7) | 0.2 (0.1) |
| Iron | 10.7 (47.5) | 13.5 (10.7) | 33.2 (27.9) | 38.4 (11.5) | 4.1 (2.4) |
| Zinc | 7.3 (37.2) | 21.9 (23.5) | 19.7 (20.4) | 46.5 (16.0) | 4.5 (3.0) |
| Selenium | 43.2 (26.7) | 33.4 (55.7) | 11.2 (13.7) | 12.1 (4.0) | 0.0 (0.0) |
| Vitamins | |||||
| Thiamin | 67.6 (60.6) | 12.7 (14.7) | 10.7 (15.2) | 9.0 (9.5) | 0.0 (0.0) |
| Riboflavin | 15.2 (18.1) | 27.4 (22.3) | 26.8 (22.9) | 30.7 (36.8) | 0.0 (0.0) |
| Niacin | 37.5 (43.0) | 19.5 (33.2) | 30.9 (21.2) | 12.0 (2.6) | 0.0 (0.0) |
| Folate | 11.9 (19.4) | 24.7 (18.7) | 30.6 (46.7) | 32.8 (15.2) | 0.0 (0.0) |
| Vitamin C | 0.0 (10.4) | 0.0 (0.0) | 100.0 (71.3) | 0.0 (0.0) | 0.0 (0.0) |
| Vitamin E | 1.9 (18.0) | 0.1 (6.0) | 3.0 (6.0) | 31.7 (9.3) | 63.4 (59.0) |
| Limited-intake nutrients | |||||
| SFA | 0.0 (0.4) | 100.0 (64.8) | 0.0 (0.0) | 0.0 (34.8) | 0.0 (0.0) |
| Cholesterol | 0.0 (0.0) | 100.0 (88.7) | 0.0 (0.0) | 0.0 (11.3) | 0.0 (0.0) |
| Na | 2.1 (1.4) | 41.8 (21.1) | 55.2 (28.6) | 0.6 (48.9) | 0.4 (0.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yin, J.; Hua, J.; Zhang, X.; Tuyishimire, A.; Yang, D. Healthy Eating for All? The Challenge of Adhering to Dietary Guidelines for Low-Income Groups in China. Nutrients 2023, 15, 2704. https://doi.org/10.3390/nu15122704
Yin J, Hua J, Zhang X, Tuyishimire A, Yang D. Healthy Eating for All? The Challenge of Adhering to Dietary Guidelines for Low-Income Groups in China. Nutrients. 2023; 15(12):2704. https://doi.org/10.3390/nu15122704
Chicago/Turabian StyleYin, Jingjing, Jingfen Hua, Xinhuan Zhang, Alexandre Tuyishimire, and Degang Yang. 2023. "Healthy Eating for All? The Challenge of Adhering to Dietary Guidelines for Low-Income Groups in China" Nutrients 15, no. 12: 2704. https://doi.org/10.3390/nu15122704
APA StyleYin, J., Hua, J., Zhang, X., Tuyishimire, A., & Yang, D. (2023). Healthy Eating for All? The Challenge of Adhering to Dietary Guidelines for Low-Income Groups in China. Nutrients, 15(12), 2704. https://doi.org/10.3390/nu15122704





