Impact of Pasta Intake on Body Weight and Body Composition: A Technical Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Observational Studies on Pasta Intake and Body Weight Outcomes
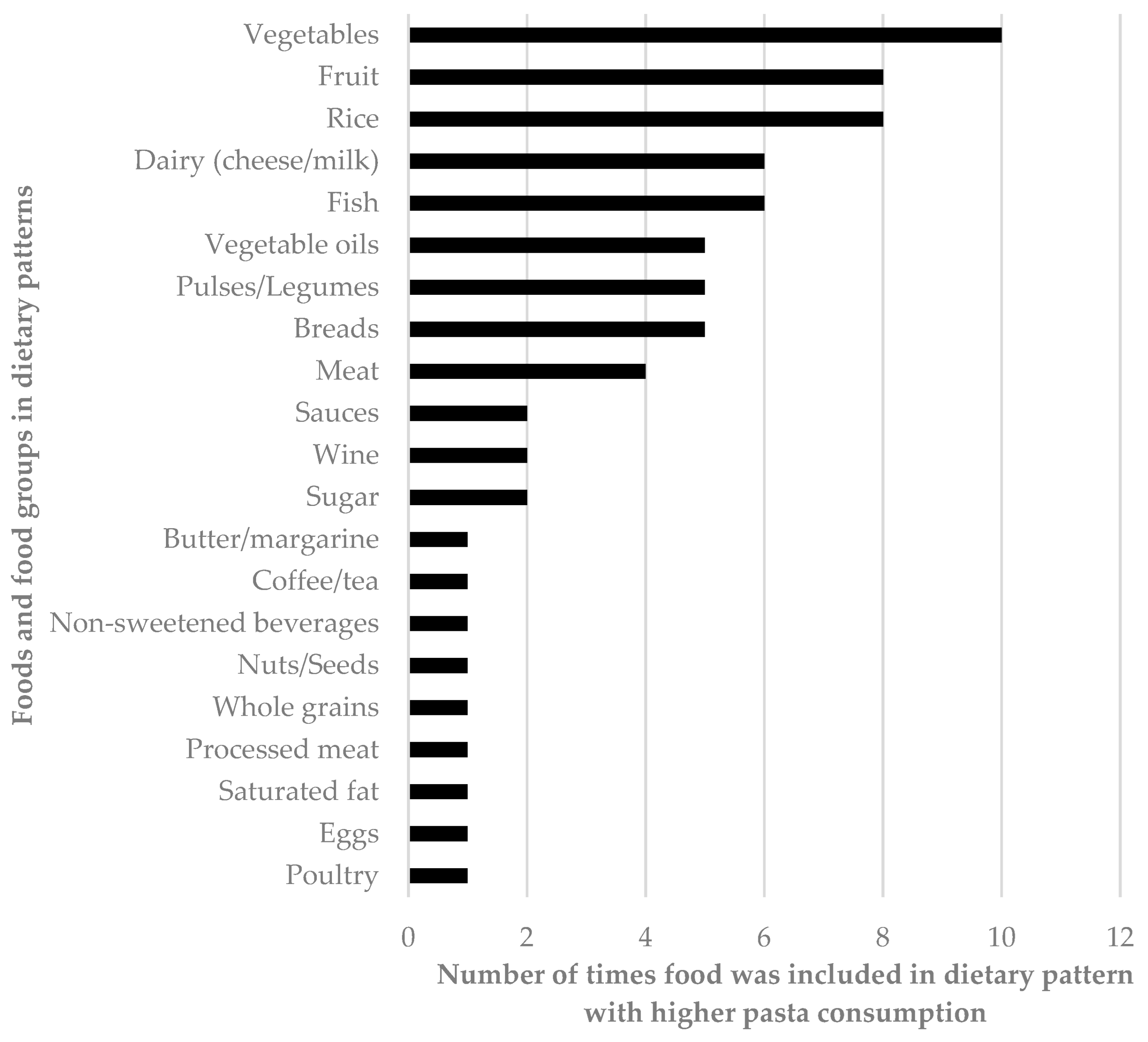
3.2. Observational Studies of Dietary Patterns Higher in Pasta Compared to Dietary Patterns Lower in Pasta and Body Weight/Composition Outcomes
3.3. Clinical Trials on Pasta Intake and Body Weight/Composition Outcomes
3.4. Clinical Trials on Potential Mechanisms by Which Pasta May Influence Body Weight and Body Composition
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Slining, M.M.; Mathias, K.C.; Popkin, B.M. Trends in food and beverage sources among US children and adolescents: 1989–2010. J. Acad. Nutr. Diet. 2013, 113, 1683–1694. [Google Scholar] [CrossRef] [PubMed]
- Toselli, S.; Brasili, P.; Di Michele, R.; Spiga, F. Perception of fattening foods in Italian children and adolescents. Springerplus 2014, 3, 402. [Google Scholar] [CrossRef] [PubMed]
- Altamore, L.; Ingrassia, M.; Columba, P.; Chironi, S.; Bacarella, S. Italian Consumers’ Preferences for Pasta and Consumption Trends: Tradition or Innovation? J. Int. Food Agribus. Mark. 2019, 32, 337–360. [Google Scholar] [CrossRef]
- Pereira, J.L.; Félix, P.V.; Mattei, J.; Fisberg, R.M. Differences over 12 Years in Food Portion Size and Association with Excess Body Weight in the City of São Paulo, Brazil. Nutrients 2018, 10, 696. [Google Scholar] [CrossRef]
- Webb, D. Pasta’s History and Role in Healthful Diets. Nutr. Today 2019, 54, 213–220. [Google Scholar] [CrossRef]
- Martinez-Lacoba, R.; Pardo-Garcia, I.; Amo-Saus, E.; Escribano-Sotos, F. Mediterranean diet and health outcomes: A systematic meta-review. Eur. J. Public Health 2018, 28, 955–961. [Google Scholar] [CrossRef]
- Esposito, K.; Kastorini, C.; Panagiotako, D.; Giugliano, D. Mediterranean Diet and Weight Loss: Meta-Analysis of Randomized Controlled Trials. Metab. Syndr. Relat. Disord. 2011, 9, 1–12. [Google Scholar] [CrossRef]
- Simopoulos, A.P. The Mediterranean diets: What is so special about the diet of Greece? The scientific evidence. J. Nutr. 2001, 131, 3065s–3073s. [Google Scholar] [CrossRef]
- Fulgoni, V.L.; Bailey, R. Association of Pasta Consumption with Diet Quality and Nutrients of Public Health Concern in Adults: National Health and Nutrition Examination Survey 2009–2012. Curr. Dev. Nutr. 2017, 1, e001271. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hobl, L.P.; Hoffmann, G. Effects of low glycaemic index/low glycaemic load vs. high glycaemic index/high glycaemic load diets on overweight/obesity and associated risk factors in children and adolescents: A systematic review and meta-analysis. Nutr. J. 2015, 14, 87. [Google Scholar] [CrossRef]
- Zafar, M.I.; Mills, K.E.; Zheng, J.; Regmi, A.; Hu, S.Q.; Gou, L.; Chen, L.-L. Low-glycemic index diets as an intervention for diabetes: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2019, 110, 891–902. [Google Scholar] [CrossRef] [PubMed]
- Chiavaroli, L.; Kendall, C.W.C.; Braunstein, C.R.; Blanco Mejia, S.; Leiter, L.A.; Jenkins, D.J.A.; Sievenpiper, J.L. Effect of pasta in the context of low-glycaemic index dietary patterns on body weight and markers of adiposity: A systematic review and meta-analysis of randomised controlled trials in adults. BMJ Open 2018, 8, e019438. [Google Scholar] [CrossRef] [PubMed]
- Bergia, R.E.; Giacco, R.; Hjorth, T.; Biskup, I.; Zhu, W.; Costabile, G.; Vitale, M.; Campbell, W.W.; Landberg, R.; Riccardi, G. Differential Glycemic Effects of Low- versus High-Glycemic Index Mediterranean-Style Eating Patterns in Adults at Risk for Type 2 Diabetes: The MEDGI-Carb Randomized Controlled Trial. Nutrients 2022, 14, 706. [Google Scholar] [CrossRef] [PubMed]
- Mancino, L.; Kuchler, F.; Leibtag, E. Getting consumers to eat more whole-grains: The role of policy, information, and food manufacturers. Food Policy 2008, 33, 489–496. [Google Scholar] [CrossRef]
- de Pedro-Jiménez, D.; Romero-Saldaña, M.; Molina-Recio, G.; de Diego-Cordero, R.; Cantón-Habas, V.; Molina-Luque, R. Relationships between work, lifestyles, and obesity: Cross-sectional study based on the 2017 Spanish National Health Survey. Eur. J. Cardiovasc. Nurs. 2022, 21, 243–253. [Google Scholar] [CrossRef]
- Palmer, K.; Bschaden, A.; Stroebele-Benschop, N. Changes in lifestyle, diet, and body weight during the first COVID 19 ‘lockdown’ in a student sample. Appetite 2021, 167, 105638. [Google Scholar] [CrossRef]
- Hörmann-Wallner, M.; Krause, R.; Alfaro, B.; Jilani, H.; Laureati, M.; Almli, V.L.; Sandell, M.; Sandvik, P.; Zeinstra, G.G.; Methven, L. Intake of Fibre-Associated Foods and Texture Preferences in Relation to Weight Status Among 9-12 Years Old Children in 6 European Countries. Front. Nutr. 2021, 8, 633807. [Google Scholar] [CrossRef]
- Androutsos, O.; Perperidi, M.; Georgiou, C.; Chouliaras, G. Lifestyle Changes and Determinants of Children’s and Adolescents’ Body Weight Increase during the First COVID-19 Lockdown in Greece: The COV-EAT Study. Nutrients 2021, 13, 930. [Google Scholar] [CrossRef]
- Papanikolaou, Y. Pasta Consumption Is Linked to Greater Nutrient Intakes and Improved Diet Quality in American Children and Adults, and Beneficial Weight-Related Outcomes Only in Adult Females. Front. Nutr. 2020, 7, 112. [Google Scholar] [CrossRef]
- Pounis, G.; Castelnuovo, A.D.; Costanzo, S.; Persichillo, M.; Bonaccio, M.; Bonanni, A.; Cerletti, C.; Donati, M.B.; de Gaetano, G.; Iacoviello, L. Association of pasta consumption with body mass index and waist-to-hip ratio: Results from Moli-sani and INHES studies. Nutr. Diabetes 2016, 6, e218. [Google Scholar] [CrossRef]
- Mostad, I.L.; Langaas, M.; Grill, V. Central obesity is associated with lower intake of whole-grain bread and less frequent breakfast and lunch: Results from the HUNT study, an adult all-population survey. Appl. Physiol. Nutr. Metab. 2014, 39, 819–828. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Marventano, S.; Buscemi, S.; Scuderi, A.; Matalone, M.; Platania, A.; Giorgianni, G.; Rametta, S.; Nolfo, F.; Galvano, F.; et al. Factors associated with adherence to the Mediterranean diet among adolescents living in Sicily, Southern Italy. Nutrients 2013, 5, 4908–4923. [Google Scholar] [CrossRef] [PubMed]
- Shay, C.M.; Van Horn, L.; Stamler, J.; Dyer, A.R.; Brown, I.J.; Chan, Q.; Miura, K.; Zhao, L.; Okuda, N.; Daviglus, M.L.; et al. Food and nutrient intakes and their associations with lower BMI in middle-aged US adults: The International Study of Macro-/Micronutrients and Blood Pressure (INTERMAP). Am. J. Clin. Nutr. 2012, 96, 483–491. [Google Scholar] [CrossRef]
- Krachler, B.; Eliasson, M.; Stenlund, H.; Johansson, I.; Hallmans, G.; Lindahl, B. Reported food intake and distribution of body fat: A repeated cross-sectional study. Nutr. J. 2006, 5, 34. [Google Scholar] [CrossRef] [PubMed]
- Kelishadi, R.; Pour, M.H.; Sarraf-Zadegan, N.; Sadry, G.H.; Ansari, R.; Alikhassy, H.; Bashardoust, N. Obesity and associated modifiable environmental factors in Iranian adolescents: Isfahan Healthy Heart Program-Heart Health Promotion from Childhood. Pediatr. Int. 2003, 45, 435–442. [Google Scholar] [CrossRef]
- Ng, A.P.; Jessri, M.; L’Abbe, M.R. Using partial least squares to identify a dietary pattern associated with obesity in a nationally-representative sample of Canadian adults: Results from the Canadian Community Health Survey-Nutrition 2015. PLoS ONE 2021, 16, e0255415. [Google Scholar] [CrossRef]
- Cacau, L.T.; De Miguel-Etayo, P.; Santaliestra-Pasías, A.M.; Giménez-Legarre, N.; Marchioni, D.M.; Molina-Hidalgo, C.; Censi, L.; González-Gross, M.; Grammatikaki, E.; Breidenassel, C.; et al. Breakfast Dietary Pattern Is Inversely Associated with Overweight/Obesity in European Adolescents: The HELENA Study. Children 2021, 8, 1044. [Google Scholar] [CrossRef]
- Barros, N.; Moreno, L.A.; Arruda, S.P.M.; de Assis, R.C.; Celedonio, R.F.; Silva, F.R.A.; Pinto, F.J.M.; Maia, C.S.C. Association between Eating Patterns and Excess Body Weight in Adolescents. Child. Obes. 2021, 17, 400–407. [Google Scholar] [CrossRef]
- Hosseini, S.H.; Papanikolaou, Y.; Isalm, N.; Rashmi, P.; Shamloo, A.; Vatanparast, H. Consumption Patterns of Grain-Based Foods among Children and Adolescents in Canada: Evidence from Canadian Community Health Survey-Nutrition 2015. Nutrients 2019, 11, 623. [Google Scholar] [CrossRef]
- Agnoli, C.; Sieri, S.; Ricceri, F.; Giraudo, M.T.; Masala, G.; Assedi, M.; Panico, S.; Mattiello, A.; Tumino, R.; Giurdanella, M.C.; et al. Adherence to a Mediterranean diet and long-term changes in weight and waist circumference in the EPIC-Italy cohort. Nutr. Diabetes 2018, 8, 22. [Google Scholar] [CrossRef]
- Biazzi Leal, D.; Altenburg de Assis, M.A.; Hinnig, P.F.; Schmitt, J.; Soares Lobo, A.; Bellisle, F.; Di Pietro, P.F.; Vieira, F.K.; de Moura Araujo, P.H.; de Andrade, D.F. Changes in Dietary Patterns from Childhood to Adolescence and Associated Body Adiposity Status. Nutrients 2017, 9, 1098. [Google Scholar] [CrossRef] [PubMed]
- Voortman, T.; Leermakers, E.T.; Franco, O.H.; Jaddoe, V.W.; Moll, H.A.; Hofman, A.; van den Hooven, E.H.; Kiefte-de Jong, J.C. A priori and a posteriori dietary patterns at the age of 1 year and body composition at the age of 6 years: The Generation R Study. Eur. J. Epidemiol. 2016, 31, 775–783. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.D.; Emmett, P.M.; Newby, P.K.; Northstone, K. Dietary patterns and changes in body composition in children between 9 and 11 years. Food Nutr. Res. 2014, 58, 22769. [Google Scholar] [CrossRef] [PubMed]
- Navarro-González, I.; López-Nicolás, R.; Rodríguez-Tadeo, A.; Ros-Berruezo, G.; Martínez-Marín, M.; Doménech-Asensi, G. Adherence to the Mediterranean diet by nursing students of Murcia (Spain). Nutr. Hosp. 2014, 30, 165–172. [Google Scholar] [CrossRef]
- Flores, M.; Macias, N.; Rivera, M.; Lozada, A.; Barquera, S.; Rivera-Dommarco, J.; Tucker, K.L. Dietary patterns in Mexican adults are associated with risk of being overweight or obese. J. Nutr. 2010, 140, 1869–1873. [Google Scholar] [CrossRef] [PubMed]
- Robinson, S.M.; Marriott, L.D.; Crozier, S.R.; Harvey, N.C.; Gale, C.R.; Inskip, H.M.; Baird, J.; Law, C.M.; Godfrey, K.M.; Cooper, C.; et al. Variations in infant feeding practice are associated with body composition in childhood: A prospective cohort study. J. Clin. Endocrinol. Metab. 2009, 94, 2799–2805. [Google Scholar] [CrossRef]
- López, E.P.; Rice, C.; Weddle, D.O.; Rahill, G.J. The relationship among cardiovascular risk factors, diet patterns, alcohol consumption, and ethnicity among women aged 50 years and older. J. Am. Diet. Assoc. 2008, 108, 248–256. [Google Scholar] [CrossRef]
- Pala, V.; Sieri, S.; Masala, G.; Palli, D.; Panico, S.; Vineis, P.; Sacerdote, C.; Mattiello, A.; Galasso, R.; Salvini, S.; et al. Associations between dietary pattern and lifestyle, anthropometry and other health indicators in the elderly participants of the EPIC-Italy cohort. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 186–201. [Google Scholar] [CrossRef]
- Bamia, C.; Orfanos, P.; Ferrari, P.; Overvad, K.; Hundborg, H.H.; Tjønneland, A.; Olsen, A.; Kesse, E.; Boutron-Ruault, M.C.; Clavel-Chapelon, F.; et al. Dietary patterns among older Europeans: The EPIC-Elderly study. Br. J. Nutr. 2005, 94, 100–113. [Google Scholar] [CrossRef]
- Williams, D.E.; Prevost, A.T.; Whichelow, M.J.; Cox, B.D.; Day, N.E.; Wareham, N.J. A cross-sectional study of dietary patterns with glucose intolerance and other features of the metabolic syndrome. Br. J. Nutr. 2000, 83, 257–266. [Google Scholar] [CrossRef]
- Rosi, A.; Tesan, M.; Cremonini, A.; Biasini, B.; Bicchieri, L.; Cossu, M.; Brighenti, F.; Dall’Aglio, E.; Scazzina, F. Body weight of individuals with obesity decreases after a 6-month high pasta or low pasta Mediterranean diet weight-loss intervention. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 984–995. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Venn, B.J.; Monro, J.; Mishra, S. Subjective Satiety Following Meals Incorporating Rice, Pasta and Potato. Nutrients 2018, 10, 1739. [Google Scholar] [CrossRef]
- Diaz-Toledo, C.; Kurilich, A.C.; Re, R.; Wickham, M.S.; Chambers, L.C. Satiety Impact of Different Potato Products Compared to Pasta Control. J. Am. Coll. Nutr. 2016, 35, 537–543. [Google Scholar] [CrossRef]
- Akilen, R.; Deljoomanesh, N.; Hunschede, S.; Smith, C.E.; Arshad, M.U.; Kubant, R.; Anderson, G.H. The effects of potatoes and other carbohydrate side dishes consumed with meat on food intake, glycemia and satiety response in children. Nutr. Diabetes 2016, 6, e195. [Google Scholar] [CrossRef]
- Geliebter, A.; Lee, M.I.; Abdillahi, M.; Jones, J. Satiety following intake of potatoes and other carbohydrate test meals. Ann. Nutr. Metab. 2013, 62, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Erdmann, J.; Hebeisen, Y.; Lippl, F.; Wagenpfeil, S.; Schusdziarra, V. Food intake and plasma ghrelin response during potato-, rice-and pasta-rich test meals. Eur. J. Nutr. 2007, 46, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Mourot, J.; Thouvenot, P.; Couet, C.; Antoine, J.M.; Krobicka, A.; Debry, G. Relationship between the rate of gastric emptying and glucose and insulin responses to starchy foods in young healthy adults. Am. J. Clin. Nutr. 1988, 48, 1035–1040. [Google Scholar] [CrossRef]
- Dickinson, S.; Hancock, D.P.; Petocz, P.; Ceriello, A.; Brand-Miller, J. High–glycemic index carbohydrate increases nuclear factor-κB activation in mononuclear cells of young, lean healthy subjects. Am. J. Clin. Nutr. 2008, 87, 1188–1193. [Google Scholar] [CrossRef] [PubMed]
- Chiavaroli, L.; Di Pede, G.; Dall’Asta, M.; Cossu, M.; Francinelli, V.; Goldoni, M.; Scazzina, F.; Brighenti, F. The importance of glycemic index on post-prandial glycaemia in the context of mixed meals: A randomized controlled trial on pasta and rice. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 615–625. [Google Scholar] [CrossRef]
- Vanhatalo, S.; Dall’Asta, M.; Cossu, M.; Chiavaroli, L.; Francinelli, V.; Pede, G.D.; Dodi, R.; Närväinen, J.; Antonini, M.; Goldoni, M.; et al. Pasta Structure Affects Mastication, Bolus Properties, and Postprandial Glucose and Insulin Metabolism in Healthy Adults. J. Nutr. 2021, 152, 994–1005. [Google Scholar] [CrossRef]
- Camps, S.G.; Lim, J.; Koh, M.X.N.; Henry, C.J. The Glycaemic and Insulinaemic Response of Pasta in Chinese and Indians Compared to Asian Carbohydrate Staples: Taking Spaghetti Back to Asia. Nutrients 2021, 13, 451. [Google Scholar] [CrossRef] [PubMed]
- Dexter, J.E. Grain, paste products: Pasta and Asian noodles. In Food Processing: Principles and Applications; Smith, J.S., Hui, Y., Eds.; Blackwell Publishing: Ames, IA, USA, 2004; pp. 249–271. [Google Scholar]
- Fuad, T.; Prabhasankar, P. Role of ingredients in pasta product quality: A review on recent developments. Crit. Rev. Food Sci. Nutr. 2010, 50, 787–798. [Google Scholar] [CrossRef] [PubMed]
- Rouhani, M.H.; Salehi-Abargouei, A.; Surkan, P.J.; Azadbakht, L. Is there a relationship between red or processed meat intake and obesity? A systematic review and meta-analysis of observational studies. Obes. Rev. 2014, 15, 740–748. [Google Scholar] [CrossRef] [PubMed]
- Schlesinger, S.; Neuenschwander, M.; Schwedhelm, C.; Hoffmann, G.; Bechthold, A.; Boeing, H.; Schwingshackl, L. Food Groups and Risk of Overweight, Obesity, and Weight Gain: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Adv. Nutr. 2019, 10, 205–218. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.; Li, J.; Ha, M.A.; Riccardi, G.; Liu, S. A systematic review on the relations between pasta consumption and cardio-metabolic risk factors. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 939–948. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, D.S.; Aronne, L.J.; Astrup, A.; de Cabo, R.; Cantley, L.C.; Friedman, M.I.; Heymsfield, S.B.; Johnson, J.D.; King, J.C.; Krauss, R.M.; et al. The carbohydrate-insulin model: A physiological perspective on the obesity pandemic. Am. J. Clin. Nutr. 2021, 114, 1873–1885. [Google Scholar] [CrossRef]
- Perin, L.; Camboim, I.G.; Lehnen, A.M. Low glycaemic index and glycaemic load diets in adults with excess weight: Systematic review and meta-analysis of randomised clinical trials. J. Hum. Nutr. Diet. 2022, 35, 1124–1135. [Google Scholar] [CrossRef]
- Wee, M.S.M.; Henry, C.J. Reducing the glycemic impact of carbohydrates on foods and meals: Strategies for the food industry and consumers with special focus on Asia. Compr. Rev. Food Sci. Food Saf. 2020, 19, 670–702. [Google Scholar] [CrossRef]
- Hodges, C.; Archer, F.; Chowdhury, M.; Evans, B.L.; Ghelani, D.J.; Mortoglou, M.; Guppy, F.M. Method of Food Preparation Influences Blood Glucose Response to a High-Carbohydrate Meal: A Randomised Cross-over Trial. Foods 2020, 9, 23. [Google Scholar] [CrossRef]
- Reynolds, A.N.; Akerman, A.P.; Mann, J. Dietary fibre and whole grains in diabetes management: Systematic review and meta-analyses. PLoS Med. 2020, 17, e1003053. [Google Scholar] [CrossRef]
- Tsitsou, S.; Athanasaki, C.; Dimitriadis, G.; Papakonstantinou, E. Acute Effects of Dietary Fiber in Starchy Foods on Glycemic and Insulinemic Responses: A Systematic Review of Randomized Controlled Crossover Trials. Nutrients 2023, 15, 2383. [Google Scholar] [CrossRef] [PubMed]
| Reference | Design | Population | Dataset and Location | Outcomes | Key Findings |
|---|---|---|---|---|---|
| De Pedro-Jiminez et al. (2022) [15] | Cross-sectional | 9097 adults (18–65 years) | Spain Spanish National Health Survey 2017 | Odds of ow/ob | OR ow/ob 1.2 (1.03–1.4) for low (<1 time/week) consumption. OR ow/ob 1.16 (1–1.34) for moderate (1–3 times/week) consumption of pasta/potatoes/rice compared to high consumption. |
| Palmer et al. (2021) [16] | Cross-sectional | 827 university students | Germany During 2020 COVID-19 lockdown | BMI | Self-reported increase in pasta intake positively associated with self-reported increase in BMI (β = 0.097, p < 0.005). |
| Hormann-Wallner et al. (2021) [17] | Cross-sectional | 330 children (9–12 years) | Six European countries | BMI | Inverse association of BMI for age and pasta intake (r = −0.127, p = 0.021). |
| Androutsos et al. (2021) [18] | Cross-sectional | 397 children (2–18 years) | Greece | Change in body weight | No association of pasta intake with parent-reported changes in body weight. |
| Papanikolaou (2020) [19] | Cross-sectional | 400 adults 323 children (2–18 years) | United States NHANES 2001–2012 | Body weight BMI WC Skinfolds | No association across quartiles of pasta intake with body weight, BMI, WC, or skinfolds in adults or children. Subgroup analysis of women 19–50 years demonstrated inverse association across quartiles of pasta intake with body weight, BMI, and WC. |
| Pereira et al. (2018) [4] | Cross-sectional | 5270 individuals (≥12 years) | Brazil Health Survey of Sao Paulo 2003–2015 | Odds of ow/ob | Portion sizes of pasta have decreased from 2003 (mean = 238.5 g) to 2015 (mean = 192.1 g). No association of pasta portion size with odds of ow/ob. |
| Pounis et al. (2016) [20] | Cross-sectional | 14,402 adults | Italy Moli-sani cohort and Italian Nutrition and Health Survey (INHES) | BMI WC HC WHR | Moli-sani cohort Inverse association of pasta intake with BMI and HC in women, but not men (women βBMI = −0.007, p = 0.003; women βHC = −0.01, p = 0.03). No association of pasta intake with WC or WHR. INHES No association of pasta intake and self-reported BMI (did not assess WC, HC, or WHR). |
| Mostad et al. (2014) [21] | Cross-sectional | 541,093 adults | Norway HUNT3 survey 2006–2008 | WHR | Inverse association of pasta/rice intake frequency and WHR. |
| Grosso et al. (2013) [22] | Cross-sectional | 1135 adolescents (13–16 years) | Spain | Odds of ow/ob | Positive association of pasta/rice intake with Mediterranean diet adherence (β = 0.019, p < 0.001). No association of pasta/rice intake with OR of ow/ob. |
| Shay et al. (2012) [23] | Cross-sectional | 2195 adults (40–59 years) | United States INTERMAP | BMI | Inverse association of BMI and pasta/rice intake in men only (β = −0.64, p < 0.01). |
| Krachler et al. (2006) [24] | Cross-sectional | 5915 adults | Sweden MONICA cohort | WC HC | Positive association of pasta intake with HC in men (+1.59 mm, p = 0.02). No association of pasta intake with WC in both genders or HC in women. |
| Kelishadi et al. (2003) [25] | Cross-sectional | 2000 adolescents (11–18 years) | Iran | BMI | Positive association of pasta intake and BMI (β = 0.03, p = 0.04). |
| Outcome | Reported Outcomes with Inverse Association | Reported Outcomes with No Association | Reported Outcomes with Positive Association |
|---|---|---|---|
| BMI or BMI z-score | 0 | 4 | 2 |
| OR overweight/obesity | 2 | 2 | 1 |
| Abdominal obesity (WC, WHR, or OR) | 4 | 1 | 1 |
| Fat mass, % body fat | 2 | 1 | 0 |
| Fat-free mass | 0 | 0 | 1 |
| Lean mass | 1 | 0 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanders, L.M.; Slavin, J. Impact of Pasta Intake on Body Weight and Body Composition: A Technical Review. Nutrients 2023, 15, 2689. https://doi.org/10.3390/nu15122689
Sanders LM, Slavin J. Impact of Pasta Intake on Body Weight and Body Composition: A Technical Review. Nutrients. 2023; 15(12):2689. https://doi.org/10.3390/nu15122689
Chicago/Turabian StyleSanders, Lisa M., and Joanne Slavin. 2023. "Impact of Pasta Intake on Body Weight and Body Composition: A Technical Review" Nutrients 15, no. 12: 2689. https://doi.org/10.3390/nu15122689
APA StyleSanders, L. M., & Slavin, J. (2023). Impact of Pasta Intake on Body Weight and Body Composition: A Technical Review. Nutrients, 15(12), 2689. https://doi.org/10.3390/nu15122689





